Abstract
Type 2 diabetes mellitus (T2DM) is closely associated with an increased risk and adverse event of acute coronary syndrome (ACS). The present study aims to investigate the association between differential urinary metabolites and major adverse cardiovascular events (MACEs) in patients with ACS co-morbid T2DM with preserved renal function, and to explore the potential value of the metabolites as prognostic biomarkers in this population. Ultra-high performance liquid chromatography-mass spectrometry (UHPLC/MS) was used to analyze urine samples from ACS co-morbid T2DM. Spearman’s correlation was used to examine the association between differential metabolites and serum fasting blood glucose (FBG), glycated hemoglobin (HbA1c), Syntax score I, and MACE. The Cox proportional hazards models and Kaplan–Meier survival curves were used to identify MACE risk factors. A total of 101 differential urinary metabolites were identified, of which seven showed a correlation with FBG, HbA1c, Syntax score I and MACE. In particular, myo-inositol and (E)-Monocrotophos emerged as significant indicators of poor prognosis in ACS co-morbid with T2DM. Urinary metabolomic alteration is closely associated with clinical manifestation of ACS co-morbid T2DM. Urinary myo-inositol and (E)-Monocrotophos may be considered as prognostic biomarkers of ACS co-morbid T2DM.
Similar content being viewed by others
Introduction
Acute coronary syndrome (ACS) is characterized by rapid onset, severe manifestation, and high mortality1,2. ACS is considered a severe type of coronary artery disease (CAD). Its basic pathologic profile involves the vulnerability and/or rupture of atherosclerotic plaque, often accompanied by complete or incomplete coronary artery occlusion. It has been confirmed that type 2 diabetes mellitus (T2DM) is an independent risk factor of ACS3, and the latter is a prevalent complication of T2DM4. Coronary angiography and autopsy studies have shown that patients with ACS and co-morbid T2DM exhibit more severe and diffuse coronary artery lesions5,6,7,8. Multiple studies have indicated that the risk of all-cause mortality and major adverse cardiovascular event (MACE) is much higher in ACS co-morbid T2DM patients than those with ACS alone9,10. These findings suggest that T2DM and ACS are closely related as well as interlinked. Therefore, exploring the underlying mechanisms by which T2DM accelerates ACS is vital for precision intervention and may help to reduce the incidence of MACE in co-morbid patients.
Metabolomics studies are powerful tools for qualitatively and quantitatively characterizing metabolite (molecular weight lower than 1000 Dalton) disturbance caused by to endogenous and exogenous stimuli in organisms. These studies reveal patterns of disease pathogenesis, progression, and outcomes11,12. A prospective cohort study noted that impaired plasma branched-chain amino acids (BCAAs) metabolism denotes a mutual pathway of metabolic dysfunction between T2DM and CAD13; altered asparagine and glutamate homeostasis precedes the onset of CAD and T2DM14. A series of serum potential metabolite biomarkers of ACS and T2DM have been identified15,16,17,18,19. However, metabolic studies on urine in ACS co-morbid T2DM patients are quite limited. Urine, produced by filtration of blood along with water homeostasis, contains diverse metabolites that are passively filtered or actively secreted into the urine. Urine offers comprehensive information about physiological and pathophysiological conditions, organ functions, and metabolic dynamics, making it a vital bio-sample studying the organism.
In the present study, we profiled the urinary differential metabolites in ACS co-morbid T2DM patients using ultra-high performance liquid chromatography-mass spectrometry (UHPLC/MS) measurement and bioinformatics analysis. We then examined the correlation between these differential metabolites and serum fasting blood glucose (FBG), glycated hemoglobin (HbA1c), and Syntax score I, and MACE in ACS co-morbid T2DM subjects. This work illustrated the relationship between urinary metabolic traits and the manifestation of ACS co-morbid T2DM, identifying urinary myo-inositol and (E)-Monocrotophos as potential prognostic biomarkers for ACS co-morbid T2DM. Our findings provide new insights into the underlying mechanisms of ACS co-morbid T2DM and offer a novel perspective for interpreting its specific manifestations.
Materials and methods
Subjects and grouping
This study followed the Helsinki Declaration and was approved by the Research Ethics Review Committee of Ningxia Medical University (Ethics No. 2022-1342). All subjects provided informed consent. A power analysis was conducted using MetaboAnalyst 5.0 to determine the final sample size. As shown in Supplemental Fig. S1, a sample size of 40 per group would give a power of more than 80% to detect discriminating metabolites, increasing this number to 60 would raise the power up to 85%. Based on the power analysis, we enrolled 105 hospitalized ACS patients, including 64 with ACS alone (named as ACS group) and 41 patients with ACS comorbid T2DM (named as ACS + T2DM group).
Diagnostic criteria
The diagnostic criteria were the 2021 AHA/ACC/ASE/CHEST/SAE/SCCT/SCMR chest pain assessment and diagnostic guidelines for ACS20. T2DM was defined according to the American Diabetes Association (ADA)21.
Inclusion and exclusion criteria
We included patients who met the diagnostic criteria for ACS and T2DM. Exclusion criteria included: ① History of myocardial infarction or unstable angina or undergoing coronary artery revascularization within 3 months, myocarditis, pericarditis, valvular heart disease, and arrhythmia. ② High blood pressure (systolic blood pressure ≥ 130 mmHg and/or diastolic blood pressure ≥ 80 mmHg) despite treatment with antihypertensive drugs. ③ Severe cardiac insufficiency, aortic coarctation, or aneurysm. ④ Chronic obstructive pulmonary disease (COPD), Pulmonary insufficiency, bronchial asthma, pulmonary embolism. ⑤ Cushing’s syndrome, hyperthyroidism, and other endocrine/metabolic disorders. ⑥ Active liver disease, or unexplained elevated serum aminotransferases, or aspartate transaminase (AST), alanine transaminase (ALT) > normal reference values. ⑦ Chronic kidney disease (CKD) with current estimate glomerular filtration rate (eGFR) < 90 mL/min/1.73 m2. ⑧ Hematologic disorders, malignancies, autoimmune disorders, and connective tissue disorders. ⑨ Mental or neurological disorders, surgery, severe trauma, severe infectious disease in the last 6 months. ⑩ Other type of diabetes.
Coronary lesions quantitative assessment
All subjects were administered coronary angiography (CAG) by certificated and experienced cardiologists. Results of CAG were entered into Syntax score system (https://Syntaxscore.org/) by a cardiologist who remained blind to patient’s information. Syntax score I is used to quantify coronary artery lesions based on CAG. By means of Syntax scoring, site and degree of stenosis, lesions of bifurcation, calcification, and diffuse were documented22,23.
Demography, laboratories and outcomes documentation
The age, gender, body mass index (BMI), systolic and diastolic blood pressure, hypertension and stroke, and medications of all subjects were recorded. Results of the first blood test were documented, including levels of uric acid (UA), creatinine (CREA), blood urea nitrogen (BUN), AST, ALT, white blood cell (WBC) and neutrophils (NEUT) counts, triglyceride (TG), low-density lipoprotein cholesterol (LDL-C), high-density lipoprotein cholesterol (HDL-C), total cholesterol (TC), brain natriuretic peptide (BNP), FBG, and HbA1c. The left ventricular ejection fraction (LVEF), measured by echocardiogram, was also included. The beginning of follow-up was defined as the next day of percutaneous coronary intervention (PCI), and the end was defined as the occurrence of MACE or June 30, 2023, whichever is earlier. The patients were followed up by phone and/or face-to-face interviews. The median duration of follow-up was 28 months. MACE includes cardiovascular death, acute myocardial infarction, recurrent angina, heart failure, or severe arrhythmias.
Metabolomics study
Metabolite extraction
Fasting clean midstream urine was collected and rapidly centrifuged at 4000 rpm/min at 4 °C for 10 min, then filtrated by 0.22 μm membrane packaging. The samples were aliquoted and frozen at − 80 °C for further measurement.
For the assay, urine osmolality (OSM) was determined by freezing point depression method and used for normalization of urine concentration to ensure metabolite measurements were not affected by the patients’ hydration status. Then, 50 μL of urine was combined with 200 μL of an extraction solvent (acetonitrile: methanol in 1:1 ratio with added internal standards), vortexed for 30 s, sonicated in an ice-water bath for 10 min, and incubated at − 40 °C for an hour to precipitate proteins. After another centrifugation at 12,000 rpm (RCF = 13,800 (× g), R = 8.6 cm) for 15 min at 4 °C, the clear supernatant was collected. A quality control (QC) sample was prepared by pooling equal parts of each supernatant.
LC–MS/MS analysis
A comprehensive metabolomic investigation was conducted through the UHPLC Vanquish platform (developed by Thermo Fisher Scientific), paired with a UPLC BEH Amide analytical column (dimensions of 2.1 mm by 100 mm, with particle size 1.7 μm) linked to the Q Exactive HFX Orbitrap mass spectrometer (provided by Thermo). The chromatographic separation employed a mobile phase comprising both 25 mmol/L ammonium acetate/ammonia hydroxide (pH = 9.75) as solvent A, and pure acetonitrile as solvent B. The auto-sampling device was kept at 4 °C, with a set injection volume of 3 μL. The state-of-the-art QE HFX mass spectrometry apparatus was operated under the information-dependent acquisition (IDA) mode, which is regulated by Xcalibur software (Thermo). This mode allows for the continuous assessment of the entire MS spectral range in real-time. Settings for the ESI source included a sheath gas flow at a rate of 30 arbitrary units, auxiliary gas at 25 arbitrary units (Arb), capillary heating at 350 °C, a full-scan MS resolving power of 60,000, MS/MS resolution set to 7500, with the collision energy optimized to 10, 30, and 60 for the NCE setting, and ion spray voltages set at 3.6 kV for the positive mode and − 3.2 kV for the negative mode.
Data processing
The raw mass spectrometry data was converted to mzXML format using the ProteoWizard software. Subsequent analysis, including peak identification, extraction, alignment, and quantification, was performed using the R programming and the XCMS kernel. To mitigate the impact of system errors on the results and to better highlight biological significance, a series of data preparation and processing steps were performed on the original data. ① Data quality control criterion: A relative standard deviation (RSD) of less than or equal to 30% of the compounds in a sample demonstrates that the experimental method is stable and reproducible, and that the metabolic data obtained are reliable. ② Filtering criterion for deviation: Filtering of individual peaks in QC samples with an RSD greater than 30%. ③ Missing values: Peak areas with > 50% missing values in a single group or > 50% missing values in all groups were removed. Remaining missing values are filled with 1/2 of the minimum value. ④ Data normalization was conducted using internal standards (IS) to ensure the retention of peak values and guarantee data quality (Supplemental Table S1)24,25.
The comprehensive database BiotreeDB, which integrates information from several well-known public metabolite databases, including HMDB (https://hmdb.ca/), MONA (https://mona.fiehnlab.ucdavis.edu/), and METLIN (https://metlin.scripps.edu/)26,27,28,29,30, was used in the annotation of our standard product-generated secondary mass spectrometry data. Metabolite annotation was conducted using a qualitative analysis method based on Euclidean distance and dot product algorithms, with an annotation threshold set at 0.3. Data was then converted to a logarithmic scale, centralized, and analyzed using SIMCA software (version 16.0.2)31. Principal component analysis (PCA) and orthogonal projections to latent structures-discriminant analysis (OPLS-DA) were employed to distinguish metabolic patterns. The quality of the OPLS-DA model was confirmed by sevenfold cross-validation, and the interpretability and predictability of the model were assessed using R2Y (explanatory power of the model for categorical variable Y) and Q2 (predictability of the model) obtained after cross-validation. Finally, the order of categorical variable Y was changed randomly several times (number of times n = 200) by permutation test to further test the validity of the model.
Statistical analysis
The data was processed using SPSS 26.0. Continuous variables followed a normal distribution were expressed as mean ± standard deviation (mean ± SD); otherwise, variables were expressed as median (quartile) [M (Q1, Q3)]. The appropriate statistical tests, either the t-test or the Mann–Whitney U test, were used for comparisons between groups. Categorical variables were expressed as absolute frequencies and percentages. The x2 test or Fisher’s exact test was employed to assess significance between the two groups. The significance level was α = 0.05, and p ≤ 0.05 was considered statistically significant. Differential metabolites screening between groups required the simultaneous fulfillment of two criteria: ① variable important in the prediction (VIP) > 1.0 using the first principal component variable of the OPLS-DA model, ② calibrated p < 0.05. Heatmap and hierarchical cluster analyses were performed using the heatmap package of the R package (https://CRAM.R-project.org/package=pheatmap). Correlation analyses were conducted using Spearman’s correlation. The Cox proportional hazards model was employed to filter the factors associated with MACE. Variables were selected through backward stepwise elimination based on the Akaike Information Criterion (AIC), with a significance threshold of p < 0.05. Endpoint event curves were plotted by using Kaplan–Meier.
Results
Comparisons of demography and laboratories
No statistical difference was found in age, gender, BMI, smoking status, lipid levels, comorbidities, or medications between the ACS + T2DM group and the ACS group (p > 0.05). The ACS + T2DM group exhibited significantly higher levels of serum FBG and HbA1c compared to the ACS group (either p < 0.05), consistent with the expected characteristics of the disease. The Syntax score I in the ACS + T2DM group was also significantly higher compared with the ACS group (p < 0.001, Table 1). Therefore, we considered serum FBG, HbA1c, and Syntax score I as the parameters representing the clinical manifestation of ACS co-morbid T2DM.
Outcome comparison between the groups
During a median follow-up of 28 months, 10 subjects of the ACS + T2DM group experienced MACE (4 cardiovascular death, 3 recurrent anginas, 2 heart failure, 1 atrial fibrillation), compared to 4 subjects in the ACS group (2 cardiovascular death, 1 recurrent angina, 1 premature ventricular beat). The incidence of MACE was significantly higher among the ACS + T2DM group compared to the ACS group [24.4% (10/41) vs. 6.2% (4/64), p = 0.016] (Table 1, Fig. 1A,B).
The incidence of MACE and Kaplan–Meier survival curves (A). MACE in the ACS group. Four subjects experienced MACE (2 cardiovascular deaths, 1 recurrent angina, 1 premature ventricular beat). (B). MACE in the ACS + T2DM group. Ten subjects suffered from MACE (4 cardiovascular deaths, 3 recurrent anginas, 2 heart failure, 1 atrial fibrillation). (C). Kaplan–Meier survival curves (Log-rank test, p = 0.011).
Furthermore, using an independent sample t-test and Fisher’s exact test, we found no significant difference in T2DM duration (p = 0.49) or medication use (p = 0.53) between subjects with MACE and those without MACE, suggesting that the duration and medication had no detectable impact on MACE incidence in this cohort (Supplemental Table S2).
The cumulative survival rate over the follow-up period was presented using the Kaplan–Meier survival curve (Fig. 1C). The survival rate of the ACS + T2DM group was lower than that of the ACS group (75.6% vs. 93.8%, Log-rank test, p = 0.011).
Metabolomics analysis
PCA score plot
A total of 1006 features were screened using UHPLC/MS. An unsupervised PCA model was used to describe the overall distribution of the data matrices for each group. As shown in the PCA score plot (Fig. 2A), all samples were located within the 95% confidence interval (CI). The QC samples (red dots) were well clustered and the internal standard RSD of the QC sample was ≤ 15% (median), which indicating that the system we used was stable and repeatable, thereby ensuring the reliability of the metabolomic results (Supplemental Fig. S2A-B)24,25.
Distribution of metabolites (A). PCA scores plot. The horizontal and vertical coordinates PCt [1] and PCt [2] represent the scores of the first and second-ranked principal components, respectively; each scatter represents a sample, and the colors represent subgroups. (B). OPLS-DA scores plot. The horizontal axis t [1] P represents the predicted principal component score of the first principal component, displaying differences between groups. The vertical axis t [1] O represents the orthogonal principal component score. Different groups are separated by scatter points in different colors and shapes. (C). Volcano plot. A dot represents a metabolite, the blue represents up-regulation, the green represents down-regulation, and the gray represents no change. The horizontal axis represents the multiple differences in log2 of the metabolite, the vertical axis represents the—log10p value of the Student’s t-test, and the size of the dot represents the VIP value, the larger the dot, the higher the VIP value. (D). Circular diagram of superclass composition in 101 urinary metabolites.
OPLS-DA analysis and replacement test
The OPLS-DA model was used to differentiate between non-orthogonal and orthogonal variables, providing insights into the metabolite differences between the groups. The quality of the OPLS-DA model was confirmed by sevenfold cross-validation, as shown in Fig. 2B, both groups exhibited good intra-group aggregation and significant inter-group separation, indicating the intrinsic metabolic characteristics and distinctive metabolite distributions within the two groups. The replacement test demonstrated that the original model’s R2Y value approached 1, and the intercept of the Q2 regression line was less than 0, indicating that the original model was not overfitted (Supplemental Fig. S3). Collectively, the multivariate pattern recognition analyses were robust and sufficient for distinguishing the metabolites between the two groups.
Identification of differential expressed metabolites
Based on VIP > 1 and p < 0.05, 101 metabolites were identified as distinguishing between the ACS + T2DM group and the ACS group (Supplemental Table S3). As shown in the volcano plot (Fig. 2C), hierarchical clustering heatmap (Supplemental Fig. S4A) and Supplemental Table S4&5, 67 of these differential metabolites were up-regulated and 34 were down-regulated in the ACS + T2DM group. This suggests that these differential metabolites can potentially distinguish the two clusters. The superclass of these 101 metabolites is depicted in Fig. 2D and Supplemental Fig. S4B. As shown in Fig. 2D, organic acids and their derivatives were the most abundant, accounting for nearly 50% of the differential expressed molecules. This indicates that disturbance of urinary organic compound was the most prominent in the ACS co-morbid T2DM individuals.
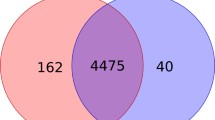
Identification of the candidate metabolites related to clinical manifestation
Using Spearman correlation analysis, we identified a series of urinary molecules that correlated with serum FBG, HbA1c, Syntax score I, and MACE. The result was depicted in a correlation clustering heatmap (Fig. 3A), with the corresponding correlation coefficients were shown in the Supplemental Table S6. There are 69, 85, 29, and 54 molecules correlate with FBG, HbA1c, Syntax score I, and MACE, respectively (Supplemental Table S7). Seven (myo-Inositol, dimethylethanolamine, (E)-Monocrotophos, (Â ±)-2- (1-Methylpropyl)-4,6- dinitrophenol, N-acetyl-5-aminosalicylic acid, phenylpyruvate acid, and 1-hexanediol) of these molecules correlate with FBG, HbA1c, Syntax score I, and MACE simultaneously. This data is presented as a Venn diagram (Fig. 3B). Of these seven, myo-Inositol, (Â ±)-2- (1-Methylpropyl)-4,6-dinitrophenol, phenylpyruvic acid, and 1-Hexanethiol were up-regulated in the ACS + T2DM group and positively correlated with these clinical parameters; Dimethylethanolamine, (E)-Monocrotophos, and N-acetyl-5-aminosalicylic acid were down-regulated and negatively correlated with these parameters. These results are illustrated in a correlation network diagram and box plot (Fig. 3C,D and Table 2). Based on these findings, we considered these seven metabolites as potential indicators of prognosis for ACS + T2DM patients. Furthermore, super classifying analysis revealed that all seven metabolites are organic compounds (organic oxygen, organosulfur, organonitrogen, organophosphorus compounds, and benzenoids, Table 3), suggesting that disturbances in organic metabolism contribute to the complex manifestation of ACS co-morbid T2DM.
Metabolites correlated with clinical manifestation (A). Clustered heatmap. The 101 urinary differential metabolites that correlate with FBG, HbA1c, Syntax score I, and MACE (Spearman’s correlation, p < 0.05). The red represents positive correlation, the blue represents negative correlation. Group-row represents the category to which the metabolite belongs. (B). Venn diagram. Metabolites correlated with serum FBG, HbA1c, and Syntax Score I and MACE. (C). Network plot. Correlation between the seven metabolites and clinical manifestation (Spearman’s correlation, p < 0.05). The yellow lines represent positive correlation, and the purple dashed lines represent negative correlation. (D). Box plot. Expression of the seven candidate metabolites (Mann–Whitney U test, * p < 0.05, ** p < 0.01, *** p < 0.001, **** p < 0.0001).
MACE risk scoring
To visualize the contributions of the seven candidate metabolites to MACE risk, we constructed a risk model, with the risk score depicted in Fig. 4. Based on the cutoff value of 0.33, patients were categorized into high and low risk groups of MACE. During the follow-up period, MACEs predominantly occurred in the high-risk group. The metabolites myo-inositol, (Â ±)-2- (1-Methylpropyl)-4,6-dinitrophenol and phenylyruvic acid, and 1-hexanethiol were identified as contributors to high-risk, while N-acetyl-5-aminosalicylic acid, dimethylethanolamine and (E)-Monocrotophos were associated with low-risk.
Risk score triple chart (A). The scatterplot. The risk scores developed from the Cox regression are in ascending order, the y-axis represents the risk scores and the x-axis represents the sample sequence numbers. The median risk score 0.33 is used as the cutoff value (Cutoff = 0.33). (B). Survival time (months) graph. (C). Heatmap. Expressions of 1-hexanethiol, phenylyruvic acid, and (Â ±)-2- (1-Methylpropyl)-4, 6-dinitrophenol are increased in the high-risk group, N-acetyl-5-aminosalicylic acid, (E)-Monocrotophos and dimethylethanolamine are increased in the low-risk group.
The Cox proportional hazards regression model
To identify independent predictors of MACE in ACS co-morbid T2DM, the Cox proportional hazards regression model was developed through a structured variable selection process. Initial covariates included traditional cardiovascular risk factors (age, smoking, TC, LDL-C, TG) and FBG, HbA1c, the Syntax Score I, alongside seven candidate metabolites. A backward stepwise elimination approach, guided by the AIC, was employed to optimize model parsimony while minimizing overfitting. Variables were retained in the final model if they met the statistical significance threshold of p < 0.05. The refined model (ΔAIC = 93.65) demonstrated that elevated myo-Inositol levels (HR = 1.003, 95% CI 1.001–1.004; p < 0.001) and reduced (E)-Monocrotophos concentrations (HR = 0.48, 95% CI 0.24–0.96; p = 0.041) independently predicted MACE risk (Table 4). The baseline levels of these two metabolites are provided in Supplemental Table S8.
Given the modest per-unit hazard ratio (HR = 1.003) for urinary myo-Inositol, we performed concentration-dependent risk recalibration across the interquartile range (IQR) in our ACS + T2DM cohort. This analysis revealed a clinically significant 25% increase in MACE risk (HR = 1.25, 95% CI 1.12–1.40) when comparing the 25th versus 75th percentile concentrations (IQR: 8.23 × 10–5–6.05 × 10–4 μmol/L), which supported myo-Inositol’s role as a cumulative metabolic risk factor. Therefore, we consider that urinary myo-Inositol and (E)-Monocrotophos may be considered as prognostic biomarkers of ACS co-morbid T2DM.
Discussion
CAD is one of the most prevalent complications of T2DM, as well as the main cause of death in T2DM. Conversely, T2DM is an independent risk factor for CAD, accelerating the development of atherosclerosis and CAD3,4,8. ACS is a severe type of CAD, which includes unstable angina, non-ST-segment elevated myocardial infarction, and ST-segment elevated myocardial infarction. It heralds a more serious and complicated process and worse prognosis once an ACS patient is companied with T2DM. Understanding the underlying mechanisms by which T2DM exacerbates ACS is crucial for the precision management of ACS co-morbid T2DM patients.
In the present study, we observed that MACE occurred significantly more frequently in the ACS comorbid T2DM group compared to the ACS group (24.4% vs. 6.2%, p = 0.016; Table 1, Fig. 1A,B). Additionally, the survival rate in the ACS comorbid T2DM group was lower than in the ACS group (75.6% vs. 93.8%, p = 0.011; Fig. 1C), highlighting the worse prognosis of ACS comorbid T2DM patient.
Using an untargeted UHPLC/MS approach, we discovered differences in urinary metabolic distributions between ACS patients with comorbid T2DM and those with ACS alone (Fig. 2B). A total of 101 differentially expressed urine metabolites were identified from the two cohorts. Approximately 50% of these differential molecules were organic acids, their derivatives, or organic heterocyclic compounds (Fig. 2D), suggesting that the perturbance of urinary organic compounds was a notable metabolic feature in ACS comorbid T2DM individuals. Correlation analysis identified several organic compounds, myo-Inositol, (Â ±)-2- (1-Methylpropyl)-4, 6-dinitrophenol and phenylpyruvic acid, and 1-Hexanethiol,to be positively correlated with serum FBG,HbA1c, Syntax score I, and MACE, while Dimethylethanolamine, (E)-Monocrotophos, and N-acetyl-5-aminosalicylic acid were negatively correlated with serum FBG,HbA1c, Syntax score I, and MACE (Table 2, Fig. 3C,D). Furthermore, myo-inositol, (Â ±)-2- (1-Methylpropyl)-4,6-dinitrophenol, phenylyruvic acid, and 1-hexanethiol were identified as contributors to MACE (Fig. 4). These findings suggest that these seven metabolites may serve as candidate biomarkers for the prognosis of ACS with comorbid T2DM. This proposes a robust link between urine metabolites and the pathophysiological changes in ACS comorbid T2DM.
Among the potential candidates, (Â ±)-2- (1-methylpropyl)-4,6-dinitrophenol, phenylpyruvate acid, and N-acetyl-5-aminosalicylic acid are benzene compounds. Benzene is a widely used industrial solvent and a significant indoor and outdoor air pollutant. Most studies on benzene have primarily focused on occupational exposure32, with only a few exploring its metabolic effects. A study of 210 individuals with mild to high risk of cardiovascular disease indicated that urinary levels of benzene metabolites correlate with the Framingham Risk Score. In addition, in T2DM participants, urinary benzene metabolites positively correlate with HbA1c levels33,34. A recent study found a significant accumulation of phenylpyruvate acid in the foot ulcers of T2DM patients, with a positive correlation between phenylpyruvate acid and the inflammatory protein nucleotide-binding oligomerization domain-like receptor family pyrin domain-containing 3 (NLRP3)35. These results suggest benzene metabolites are involved in the development of T2DM. In our study, we observed correlations between urinary benzene metabolites, coronary plaque load, and MACE, further supporting the involvement of benzene compounds in the development and outcomes of ACS comorbid with T2DM. Recent reports have shown that benzene-based organic compounds, as measured by LC/MS, are associated with depletion of circulating angiogenic cells, which may impair endothelial repair and angiogenesis, thereby increasing the risk of CAD36. Additionally, production of benzene increases CAD risk by enhancing platelet reactivity and thrombotic potential through adrenergic receptor signaling37. While these studies, along with our findings, provide evidence of benzene metabolites’ involvement in both T2DM and CAD, the detailed mechanisms remain uncertain. The role of benzene compounds in the interplay between T2DM and CAD also requires further investigation.
Our MACE risk scoring results indicate that urine myo-Inositol is a contributor to MACE, as well as a predictor of poorer outcomes. In contrast, (E)-Monocrotophos is a contributor to low risk of MACE. Combined with the findings from the COX regression analysis, we conclude that myo-Inositol and (E)-Monocrotophos are potential prognostic biomarkers for ACS comorbid T2DM.
Myo-Inositol is a naturally occurring molecule that contributes to multiple biochemical and metabolic processes in various tissues and organs. In the context of T2DM pathogenesis, hyperglycemia is associated with insulin resistance and β-cell dysfunction38. Some insulin actions are mediated by inositol phosphate glycan (IPG)39,40. The majority of IPG exists in the form of inositol. Therefore, disturbances in myo-Inositol metabolism can significantly influence diabetes development. Under hyperglycemic circumstances, IPG increases myo-Inositol degradation and inhibits its biosynthesis and adsorption, leading to reduced inositol availability41. The kidneys serves as the primary site for myo-inositol synthesis, reabsorption, and degradation, and plays a crucial role in regulating plasma myo-inositol concentrations42. Myo-Inositol is catabolized and degraded to glucuronide via the renal-specific myo-inositol oxygenase (MIOX) and glucuronate-xylulose (GX) pathways, ultimately transforming into glucuronic acid, which is excreted by the kidneys43. Chang and colleagues have concluded that the excretion of urinary myo-Inositol is notably increased in diabetic patients, potentially serving as a predictor of response to glycemic control44. These findings have been further confirmed by animal experiments45,46,47. While Kwon et al.48 highlighted myo-Inositol’s diagnostic utility in cohorts with heterogeneous renal function, our study specifically analyzed a preserved renal function cohort, thereby isolating intrinsic metabolic effects from chronic kidney disease-related confounders. This stratification improved detection sensitivity for early metabolic dysregulation. In the present study, subjects with ACS comorbid T2DM exhibited elevated levels of urinary myo-Inositol, which may indicate ineffective glycemic control. This condition likely impacts both the clinical characteristics and prognosis of these patients.
(E)-Monocrotophos, a water-soluble dimethoxycarbonyl compound, is an organophosphorus insecticide (OPI) with significant toxicity to mammals49. (E)-Monocrotophos has a propensity to accumulate in organs responsible for its metabolism50. Research has demonstrated that (E)-Monocrotophos is primarily broken down through N-demethylation, O-demethylation, and vinyl phosphate bond cleavage51, with the majority (70–90%) eliminated via the urinary tract52. Studies have shown that prolonged exposure to OPIs in rats is often associated with dyslipidemia, glucose intolerance, and insulin resistance. A notable upsurge in the expression level of diglycerol acyltransferase 1 (DGAT1), an indispensable enzyme that regulates triglyceride synthesis, in rat adipose tissue continually exposed to (E)-Monocrotophos was described53,54,55. Enhanced DGAT1 activity or expression poses a risk of metabolic syndrome56,57. Similar findings have been reported in a prospective study in humans58. However, the underlying mechanisms require further investigation through via in vivo and in vitro studies.
In conclusion, in ACS comorbid T2DM subjects, the most prominent perturbance is in urinary organic acid metabolism. Among these, urine Myo-Inositol and (E)-Monocrotophos may serve as robust biomarkers and have significant impacts on the manifestation and prognosis of ACS comorbid T2DM. Our work provides novel insights into the comprehensive understanding of the specific phenotype of ACS comorbid T2DM.
Further optimization is warranted. Targeted metabolic analysis and larger sample size case–control studies are crucial for metabolic profiling. A validation cohort study is essential to strengthen the validity of the findings. Monitoring of metabolite changes or tracer metabolic fluxes is necessary for gain further insights into the pathophysiology of ACS comorbid T2DM.
Data availability
Data is provided within the manuscript or supplementary information files.
Abbreviations
- ACS:
-
Acute coronary syndrome
- CAD:
-
Coronary artery disease
- T2DM:
-
Type 2 diabetes mellitus
- MACE:
-
Major adverse cardiovascular event
- UHPLC/MS:
-
Ultra-high performance liquid chromatography–mass spectrometry
- FBG:
-
Fasting blood glucose
- HbA1c:
-
Glycated hemoglobin
- CAG:
-
Coronary angiography
- ADA:
-
American Diabetes Association
- ALT:
-
Alanine transaminase
- COPD:
-
Chronic obstructive pulmonary disease
- AST:
-
Aspartate transaminase
- CREA:
-
Creatinine
- BMI:
-
Body mass index
- BUN:
-
Blood urea nitrogen
- UA:
-
Uric acid
- WBC:
-
White blood cell
- NEUT:
-
Neutrophils
- TG:
-
Triglyceride
- TC:
-
Total cholesterol
- LVEF:
-
Left ventricular ejection fraction
- LDL-C:
-
Low-density lipoprotein cholesterol
- BNP:
-
Brain natriuretic peptide
- Myo:
-
Myoglobin
- cTnI:
-
Cardiac troponin I
- CK-MB:
-
Creatine Kinase MB isoenzyme
- HDL-C:
-
High-density lipoprotein cholesterol
- PCI:
-
Percutaneous coronary intervention
- QC:
-
Quality control
- IDA:
-
Information-dependent acquisition
- VIP:
-
Variable important in the prediction
- CI :
-
Confidence interval
- RSD:
-
Relative standard deviation
- IS:
-
Internal standards
- IPG:
-
Inositol phosphate glycan
- MIOX:
-
Myo-inositol oxygenase
- GX:
-
Glucuronate-xylulose
- DGAT1:
-
Diglycerol acyltransferase 1
- PCA:
-
Principal component analysis
- OPLS-DA:
-
Orthogonal projections to latent structures-discriminant analysis
- BCAA:
-
Branched chain amino acids
- ACS:
-
Acute coronary syndrome
References
Libby, P. Mechanisms of acute coronary syndromes and their implications for therapy. N. Engl. J. Med. 368, 2004–2013. https://doi.org/10.1056/NEJMra1216063 (2013).
Byrne, R. A. et al. 2023 ESC Guidelines for the management of acute coronary syndromes. Eur. Heart J. Acute Cardiovasc. Care 13(1), 55–161. https://doi.org/10.1093/ehjacc/zuad107 (2023).
Braunwald, E. Diabetes, heart failure, and renal dysfunction: The vicious circles. Prog. Cardiovasc. Dis. 62, 298–302. https://doi.org/10.1016/j.pcad.2019.07.003 (2019).
Naito, R. & Miyauchi, K. Coronary artery disease and type 2 diabetes mellitus. Int. Heart J. 58, 475–480. https://doi.org/10.1536/ihj.17-191 (2017).
Hamedifard, Z. et al. The effects of combined magnesium and zinc supplementation on metabolic status in patients with type 2 diabetes mellitus and coronary heart disease. Lipids Health Dis. 19, 112. https://doi.org/10.1186/s12944-020-01298-4 (2020).
Shah, A. D. et al. Type 2 diabetes and incidence of cardiovascular diseases: A cohort study in 1·9 million people. Lancet Diabetes Endocrinol. 3, 105–113. https://doi.org/10.1016/S2213-8587(14)70219-0 (2015).
Stratton, I. M. et al. Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35): Prospective observational study. BMJ (Clin. Res. ed.) 321, 405–412. https://doi.org/10.1136/bmj.321.7258.405 (2000).
Marx, N. et al. 2023 ESC Guidelines for the management of cardiovascular disease in patients with diabetes. Eur. Heart J. 44, 4043–4140. https://doi.org/10.1093/eurheartj/ehad192 (2023).
Shehab, A. et al. Diabetes and mortality in acute coronary syndrome: Findings from the gulf COAST registry. Curr. Vasc. Pharmacol. 18, 68–76. https://doi.org/10.2174/1570161116666181024094337 (2020).
Zhou, M. et al. Prevalence and in-hospital outcomes of diabetes among patients with acute coronary syndrome in China: findings from the Improving Care for Cardiovascular Disease in China-Acute Coronary Syndrome Project. Cardiovasc. Diabetol. 17, 147. https://doi.org/10.1186/s12933-018-0793-x (2018).
Griffin, J. L., Atherton, H., Shockcor, J. & Atzori, L. Metabolomics as a tool for cardiac research. Nat. Rev. Cardiol. 8, 630–643. https://doi.org/10.1038/nrcardio.2011.138 (2011).
Singh, A. Tools for metabolomics. Nat. Methods 17, 24. https://doi.org/10.1038/s41592-019-0710-6 (2020).
Tobias, D. K. et al. Circulating branched-chain amino acids and incident cardiovascular disease in a prospective cohort of US women. Circ. Genom. Precis. Med. 11, e002157. https://doi.org/10.1161/CIRCGEN.118.002157 (2018).
Ottosson, F., Smith, E., Melander, O. & Fernandez, C. Altered asparagine and glutamate homeostasis precede coronary artery disease and type 2 diabetes. J. Clin. Endocrinol. Metab. 103, 3060–3069. https://doi.org/10.1210/jc.2018-00546 (2018).
Ferrannini, G. et al. coronary artery disease and type 2 diabetes: A proteomic study. Diabetes Care 43, 843–851. https://doi.org/10.2337/dc19-1902 (2020).
Hunter, W. G. et al. Metabolomic profiling identifies novel circulating biomarkers of mitochondrial dysfunction differentially elevated in heart failure with preserved versus reduced ejection fraction: Evidence for shared metabolic impairments in clinical heart failure. J. Am. Heart Assoc. 5, e003190. https://doi.org/10.1161/JAHA.115.003190 (2016).
Liu, W. et al. Metabolic interactions and differences between coronary heart disease and diabetes mellitus: A pilot study on biomarker determination and pathogenesis. J. Proteome Res. 20, 2364–2373. https://doi.org/10.1021/acs.jproteome.0c00879 (2021).
Qin, Y. et al. Relationship between random blood glucose, fasting blood glucose, and gensini score in patients with acute myocardial infarction. Biomed. Res. Int. 2019, 9707513. https://doi.org/10.1155/2019/9707513 (2019).
Stratmann, B. et al. Metabolomic signature of coronary artery disease in type 2 diabetes mellitus. Int. J. Endocrinol. 2017, 7938216. https://doi.org/10.1155/2017/7938216 (2017).
Gulati, M. et al. 2021 AHA/ACC/ASE/CHEST/SAEM/SCCT/SCMR guideline for the evaluation and diagnosis of chest pain: A report of the American College of Cardiology/American Heart Association joint committee on clinical practice guidelines. Circulation 144, e368–e454. https://doi.org/10.1161/CIR.0000000000001029 (2021).
Updates to the Standards of Medical Care in Diabetes-2018. Diabetes Care 41, 2045–2047. https://doi.org/10.2337/dc18-su09 (2018).
Cavalcante, R. et al. Impact of the SYNTAX scores I and II in patients with diabetes and multivessel coronary disease: A pooled analysis of patient level data from the SYNTAX, PRECOMBAT, and BEST trials. Eur. Heart J. 38, 1969–1977. https://doi.org/10.1093/eurheartj/ehx138 (2017).
Mavromatis, K. & King, S. B. SYNTAX scoring: growing stronger. Eur. Heart J. 38, 1978–1979. https://doi.org/10.1093/eurheartj/ehx231 (2017).
Dunn, W. B. et al. Procedures for large-scale metabolic profiling of serum and plasma using gas chromatography and liquid chromatography coupled to mass spectrometry. Nat. Protoc. 6, 1060–1083. https://doi.org/10.1038/nprot.2011.335 (2011).
Want, E. J. et al. Global metabolic profiling procedures for urine using UPLC-MS. Nat. Protoc. 5, 1005–1018. https://doi.org/10.1038/nprot.2010.50 (2010).
Fu, M. et al. Multinomial machine learning identifies independent biomarkers by integrated metabolic analysis of acute coronary syndrome. Sci. Rep. 13, 20535. https://doi.org/10.1038/s41598-023-47783-5 (2023).
Xiao, Y. et al. Comprehensive metabolomics expands precision medicine for triple-negative breast cancer. Cell Res. 32, 477–490. https://doi.org/10.1038/s41422-022-00614-0 (2022).
Zhang, X. et al. Dietary cholesterol drives fatty liver-associated liver cancer by modulating gut microbiota and metabolites. Gut 70, 761–774. https://doi.org/10.1136/gutjnl-2019-319664 (2021).
Liu, Q. et al. Altered faecal microbiome and metabolome in IgG4-related sclerosing cholangitis and primary sclerosing cholangitis. Gut 71, 899–909. https://doi.org/10.1136/gutjnl-2020-323565 (2022).
Gong, Y. et al. Metabolic-pathway-based subtyping of triple-negative breast cancer reveals potential therapeutic targets. Cell Metab. 33, 51–64. https://doi.org/10.1016/j.cmet.2020.10.012 (2021).
Smith, C. A., Want, E. J., O’Maille, G., Abagyan, R. & Siuzdak, G. XCMS: processing mass spectrometry data for metabolite profiling using nonlinear peak alignment, matching, and identification. Anal. Chem. 78, 779–787. https://doi.org/10.1021/ac051437y (2006).
Bahadar, H., Mostafalou, S. & Abdollahi, M. Current understandings and perspectives on non-cancer health effects of benzene: A global concern. Toxicol. Appl. Pharmacol 276, 83–94. https://doi.org/10.1016/j.taap.2014.02.012 (2014).
Caro, A. A. & Cederbaum, A. I. Oxidative stress, toxicology, and pharmacology of CYP2E1. Annu. Rev. Pharmacol. Toxicol. 44, 27–42. https://doi.org/10.1146/annurev.pharmtox.44.101802.121704 (2004).
Shen, Y., Shen, H. M., Shi, C. Y. & Ong, C. N. Benzene metabolites enhance reactive oxygen species generation in HL60 human leukemia cells. Hum. Exp. Toxicol. 15, 422–427. https://doi.org/10.1177/096032719601500510 (1996).
Lv, D. et al. Targeting phenylpyruvate restrains excessive NLRP3 inflammasome activation and pathological inflammation in diabetic wound healing. Cell Rep. Med. 4, 101129. https://doi.org/10.1016/j.xcrm.2023.101129 (2023).
Riggs, D. W. et al. Environmental exposure to volatile organic compounds is associated with endothelial injury. Toxicol. Appl. Pharmacol 437, 115877. https://doi.org/10.1016/j.taap.2022.115877 (2022).
Dludla, P. V. et al. The combination effect of aspalathin and phenylpyruvic acid-2-O-β-D-glucoside from rooibos against hyperglycemia-induced cardiac damage: An in vitro study. Nutrients 12, 1151. https://doi.org/10.3390/nu12041151 (2020).
Kahn, S. E. The relative contributions of insulin resistance and beta-cell dysfunction to the pathophysiology of Type 2 diabetes. Diabetologia 46, 3–19. https://doi.org/10.1007/s00125-002-1009-0 (2003).
Petersen, M. C. & Shulman, G. I. Mechanisms of insulin action and insulin resistance. Physiol. Rev. 98, 2133–2223. https://doi.org/10.1152/physrev.00063.2017 (2018).
Saltiel, A. R. Second messengers of insulin action. Diabetes Care 13, 244–256. https://doi.org/10.2337/diacare.13.3.244 (1990).
Dinicola, S. et al. Nutritional and acquired deficiencies in inositol bioavailability. Correlations with metabolic disorders. Int. J. Mol. Sci. 18, 2187. https://doi.org/10.3390/ijms18102187 (2017).
Chang, H. H. et al. Renal depletion of myo-inositol is associated with its increased degradation in animal models of metabolic disease. Am. J. Physiol. Renal Physiol. 309, F755–F763. https://doi.org/10.1152/ajprenal.00164.2015 (2015).
von Toerne, C. et al. MASP1, THBS1, GPLD1 and ApoA-IV are novel biomarkers associated with prediabetes: The KORA F4 study. Diabetologia 59, 1882–1892. https://doi.org/10.1007/s00125-016-4024-2 (2016).
Chang, H. H., Choong, B., Phillips, A. R. & Loomes, K. M. The diabetic rat kidney mediates inosituria and selective urinary partitioning of D-chiro-inositol. Exp. Biolo. Med. (Maywood, NJ) 240, 8–14. https://doi.org/10.1177/1535370214543064 (2015).
Croze, M. L., Géloën, A. & Soulage, C. O. Abnormalities in myo-inositol metabolism associated with type 2 diabetes in mice fed a high-fat diet: Benefits of a dietary myo-inositol supplementation. Br. J. Nutr. 113, 1862–1875. https://doi.org/10.1017/S000711451500121X (2015).
Kawa, J. M., Przybylski, R. & Taylor, C. G. Urinary chiro-inositol and myo-inositol excretion is elevated in the diabetic db/db mouse and streptozotocin diabetic rat. Exp. Biol. Med.(Maywood, N. J.) 228, 907–914. https://doi.org/10.1177/153537020322800806 (2003).
Sun, T. H., Heimark, D. B., Nguygen, T., Nadler, J. L. & Larner, J. Both myo-inositol to chiro-inositol epimerase activities and chiro-inositol to myo-inositol ratios are decreased in tissues of GK type 2 diabetic rats compared to Wistar controls. Biochem. Biophys. Res. Commun. 293, 1092–1098. https://doi.org/10.1016/S0006-291X(02)00313-3 (2002).
Kwon, S. et al. Urine myo-inositol as a novel prognostic biomarker for diabetic kidney disease: A targeted metabolomics study using nuclear magnetic resonance. Kidney Res. Clin. Pract. 42, 445–459. https://doi.org/10.23876/j.krcp.22.152 (2023).
Singh, S. et al. Toxicity and detoxification of monocrotophos from ecosystem using different approaches: A review. Chemosphere 275, 130051. https://doi.org/10.1016/j.chemosphere.2021.130051 (2021).
Peter, J. V. et al. Clinical profile and outcome of patients hospitalized with dimethyl and diethyl organophosphate poisoning. Clin. Toxicol. (Philadelphia, Pa) 48, 916–923. https://doi.org/10.3109/15563650.2010.528425 (2010).
Mücke, W. Metabolism of monocrotophos in animals. Rev. Environ. Contam. Toxicol. 139, 59–65. https://doi.org/10.1007/978-1-4684-7071-0_5 (1994).
Jose, A. et al. Estimation of Monocrotophos renal elimination half-life in humans. Clin. Toxicol. (Philadelphia, Pa) 53, 629–632. https://doi.org/10.3109/15563650.2015.1054500 (2015).
Nagaraju, R., Joshi, A., Vamadeva, S. & Rajini, P. S. Effect of chronic exposure to monocrotophos on white adipose tissue in rats and its association with metabolic dyshomeostasis. Hum. Exp. Toxicol. 39, 1190–1199. https://doi.org/10.1177/0960327120913080 (2020).
Nagaraju, R., Joshi, A., Vamadeva, S. G. & Rajini, P. S. Deregulation of hepatic lipid metabolism associated with insulin resistance in rats subjected to chronic monocrotophos exposure. J. Biochem. Mol. Toxicol. 34, e22506. https://doi.org/10.1002/jbt.22506 (2020).
Perry, R. J., Zhang, D., Zhang, X. M., Boyer, J. L. & Shulman, G. I. Controlled-release mitochondrial protonophore reverses diabetes and steatohepatitis in rats. Science 347, 1253–1256. https://doi.org/10.1126/science.aaa0672 (2015).
Chen, H. C., Stone, S. J., Zhou, P., Buhman, K. K. & Farese, R. V. Jr. Dissociation of obesity and impaired glucose disposal in mice overexpressing acyl coenzyme a:diacylglycerol acyltransferase 1 in white adipose tissue. Diabetes 51, 3189–3195. https://doi.org/10.2337/diabetes.51.11.3189 (2002).
Kazi, A. I. & Oommen, A. Monocrotophos induced oxidative damage associates with severe acetylcholinesterase inhibition in rat brain. Neurotoxicology 33, 156–161. https://doi.org/10.1016/j.neuro.2012.01.008 (2012).
Gifford, R. M. et al. Short-term glucose dysregulation following acute poisoning with organophosphorus insecticides but not herbicides, carbamate or pyrethroid insecticides in South Asia. Clin. Toxicol. (Philadelphia, Pa) 57, 254–264. https://doi.org/10.1080/15563650.2018.1515438 (2019).
Funding
This study was supported by Ningxia Key Research and Development Plan Project (2021BEG03115 to JH), Ningxia Health Commission Project (2023-NWKYT-020 to JH) and Ningxia Natural Science Foundation (2023AAC02070 to JH).
Author information
Authors and Affiliations
Contributions
J.H.: supervision, project administration, funding acquisition, conceptualization, validation, and critically revising the manuscript. M.Y.D.: Conceptualization, investigation, formal analysis, visualization, writing-original draft. Z.H.Z.: conceptualization, investigation, formal analysis. R.H.H.: investigation. Y.M.Z.: investigation. X.Y.Z.: visualization. M.D.: visualization.All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Duan, M., Zhang, Z., He, R. et al. Urinary metabolomics reveals myo-inositol and (E)-Monocrotophos associate with prognosis in ACS comorbid with T2DM and preserved renal function. Sci Rep 15, 12905 (2025). https://doi.org/10.1038/s41598-025-96010-w
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-96010-w