Abstract
Diabetic retinopathy (DR) is one of the major complications of diabetes, resulting in severe vision loss. Traction retinal detachment (TRD) is the main factor affecting the effect of proliferative diabetic retinopathy (PDR) surgery. Liquid Chromatography with tandem mass spectrometry (LC-MS/MS) was adopted to analyze the proteomes of the vitreous in the TRD, vitreous hemorrhage (VH) and macular hole (MH) groups. By employing bioinformatics tools for GO and KEGG pathway annotation, as well as conducting protein-protein interaction(PPI) network analysis, we investigated the functional enrichment of proteins in the TRD vitreous and their associated pathways. Additionally, peptide center analysis was performed on the proteomic data to identify key differentially expressed proteins based on screening results. Bioinformatics analysis showed that DEPs is mainly enriched in the complement, the coagulation cascade systems and regulation of actin cytoskeleton. The protein interaction network analysis showed that the central proteins were mainly related to sphingolipid metabolism. APOA4, CHI3L1, LTBP2 were significantly up-regulated in TRD, which were related to the complement system, coagulation cascade and platelet activation, sphingolipid metabolism and other pathways. APOA4 and CHI3L1 protein in patients with TRD group raised significantly in the vitreous humor, shows the potential biomarkers for TRD.
Similar content being viewed by others
Introduction
Diabetic retinopathy (DR) is the leading causes of visual impairment and one of the main causes of vision loss worldwide, and also brings a huge public health burden to the world1. Clinically, the main types of diabetic retinopathy are non-proliferative diabetic retinopathy (NPDR) and proliferative diabetic retinopathy (PDR) according to the disease process. NPDR is known as early DR, which is characterized by clinical manifestations such as retinal microaneurysms, cotton wool spots, hemorrhages, and exudates2. PDR is also known as late DR, which is typically characterized by the formation of new blood vessels that are very fragile and can thus rupture and bleed profusely.Progression towards PDR leads to severe complications such as vitreous hemorrhage (VH) and tractional retinal detachment (TRD) that may require surgical intervention in the form of pars plana vitrectomy (PPV). Given the crucial role of TRD in the visual prognosis and management of eyes with PDR, it is essential to conduct meticulous screening for its presence.
Vitreoretinal disease will cause changes in the level of vitreous specific proteins1. The changes of biochemical components in vitreous are believed to be closely related to the changes of retinal homeostasis3. Proteomics technology facilitates the detection of anomalous proteins within the vitreous, made it possible to evaluate entire proteome sets in different disease conditions to understand the interplay among various proteins and how they affect disease progression and therapy4. Barba et al.5 found that lactic acid increased and ascorbic acid decreased in the vitreous fluids of DR Patients. Paris et al.6 reported an increase in arginine, proline and allantoin; Zou et al. studied the changes induced by ranibizumab in the vitreous proteome of patients with PDR and found that platelet degranulation and integrin cell surface interaction pathways are severely affected7. Kaku et al.8found the fatty acid-binding protein4 (FABP4) and vascular endothelial growth factor A (VEGFA) play key roles in the PDR. Ocular proteomics provide new possibilities for discovering new biomarkers, which could help to unveil the underlying mechanism of PDR development.
Vitreoretinal disease will cause changes in the level of vitreous specific proteins9. The changes of biochemical components in vitreous are believed to be closely related to the changes of retinal homeostasis3,10. With the progress of science and technology, the study of proteins and genomics has become a research hotspot, providing new possibilities for further research on the pathogenesis and treatment of DR. Barba et al.5 found that lactic acid increased and ascorbic acid decreased in the vitreous fluids of DR Patients. Paris et al.6 reported an increase in arginine, proline and allantoin; And Haines et al.3 reported an increase in pyruvate and purine-related pathways. Vitreo-retinal interface plays an important role in reflecting the state of retinal diseases. Vitreous metabolism is closely related to the pathological process of DR. Proteomics technology facilitates the detection of anomalous proteins within the vitreous, made it possible to evaluate entire proteome sets of different disease conditions to understand the interplay among various proteins and how they affect disease expression4. Such insights can elucidate the pathogenesis of diabetic retinopathy and identify novel therapeutic targets.
To date, studies into the vitreoretinal proteome within diabetic retinopathy and proliferative diabetic retinopathy (PDR) has significantly contributed to the identification of potential biomarkers and the guidance of diagnostic and therapeutic approaches10. Nonetheless, the preponderance of prior research has focused on PDR or diabetic macular edema (DME) as primary points of investigation, while comparatively neglecting the underlying etiology of irreversible visual loss due to tractional retinal detachment. In the present study, we have categorized PDR into two distinct groups: VH group and TRD group, utilizing the patients with macular hole (MH) as a control. we first performed vitreous protein profiling of patients with VH, TRD and MH using label-free quantitative proteomics. A comprehensive bioinformatics analysis revealed several altered pathways and target protein candidates. Our results identify novel protein candidates and these findings may serve as a theoretical foundation for a more comprehensive understanding of DR pathogenesis and development of novel treatment options. (Fig. 1).
Results
Differentially expressed proteins (DEPs) compared between TRD, vitreous hemorrhage (VH) and controls
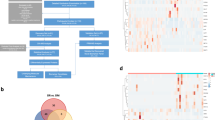
Proteomic analysis revealed a total of 634 proteins in the vitreous humor samples from all groups, of these, 487 proteins were quantified (Fig. 2). There were 87 differentially expressed proteins (DEPs) found between TRD and control group by the LC-MS/MS platform, with 40 of them being downregulated and 47 being upregulated. A total of 141 DEPs were found between the vitreous hemorrhage (VH) and control groups, including 78 downregulated proteins and 63 upregulated proteins. Interestingly, in our analysis, 36 DEPs (13 downregulated and 23 up-regulated proteins) were identified compared TRD with vitreous hemorrhage (VH) (Fig. 2). In the hierarchical clustering analysis between the different groups, the expression pattern of DEP was determined (Fig. 3A,D,G). To identify the key factors for developing TRD, we identified differential proteins between TRD and vitreous hemorrhage (VH), TRD and control group, and the top 10 proteins with elevated differential proteins were selected for analysis, as detailed in Tables 1 and 2.
Compares the Venn plots and the volcano plots of the different groups of DEPs. (A) Bar graph of the quantitative difference results in different histones. (B) Venn plots identified between all sample groups, 422 co-expressed DEPs in TRD, vitreous hemorrhage (VH) and Control, 54 unique DEPs in Control Group, 25 unique DEPs in TRD, and 13 unique DEPs in vitreous hemorrhage (VH). (C–E) Volcano plot shows the distribution of differentially expressed proteins in each comparison. The horizontal axis represents the multiple (FC) and the vertical axis represents the p value. Red dots are upregulated DEPs, blue dots are downregulated DEPs, and grey dots are proteins not significantly differentially expressed.(| log2 (FC) |> 0.58; p-value < 0.05).
Functional analysis of the identified TRD and VH associated proteins
Results of cluster analysis and GO analysis of differentially expressed proteins between groups. The left column (A, B, C) shows the results of the cluster analysis. The horizontal axis represents sample information, while the vertical axis represents significantly differentially expressed proteins. The expression of significantly different proteins in different samples is standardized by Z-Score method and displayed in the heat map, where red representing significantly up-regulated proteins and blue representing significantly downregulated proteins. The middle column (D, E, F) shows the GO annotation statistics (Levle 2) of differentially expressed proteins, including BP, MF and CC, shown as in blue, red and orange, and the horizontal axis indicates the number of differentially expressed proteins under each group. The column on the left shows the Top 20 enriched GO terms of significantly DEPs in each comparison. Cluster analysis of differentially expressed proteins between TRD and vitreous hemorrhage (VH) groups, GO statistical analysis map (Level 2), string GO-term enrichment (A, D, G). Hierarchical clustering analysis and GO-term enrichment of differentially expressed proteins between vitreous hemorrhage (VH) and control groups (B, E, H).Hierarchical cluster analysis and string GO-term enrichment of differentially expressed proteins between TRD and control groups (C, F, I) .(|log2(FC)| > 0.58; P < 0.05).
Layer clustering analysis results in the tree heat map (Fig. 3A,B,C), each column represents a set of samples, horizontal axis for sample information, each row represents a protein, significant protein expression in different samples in Z-Score method in different color heat map, where red represents significantly increased protein, blue represents significantly downregulated protein, gray part represents no protein quantitative information.
In order to fully understand the function, localization and involved biological pathways of proteins, the proteins are annotated through the Gene Ontology (Gene Ontology, GO). GO function annotation is mainly divided into three categories: biological processes (Biological Process, BP), molecular functions (Molecular Function, MF) and cellular components (Cellular Component, CC), which are distinguished in blue, red and orange. BP analysis showed that the main biological process in TRD and control groups was platelet degranulation, lipid metabolic process for VH and control, and regulated exocytosis and exocytosis for TRD and vitreous hemorrhage (VH). The MF results showed that the main molecular functions of the TRD and control groups were endopeptidase inhibitor activity, serine-type endopeptidase inhibitor activity, peptidase inhibitor activity, endopeptidase regulator activity, and peptidase regulator activity. vitreous hemorrhage (VH) and control group were serine-type endopeptidase inhibitor activity, and TRD and vitreous hemorrhage (VH) group were phosphoprotein binding. The CC results showed that the main cellular component of the TRD and control groups was platelet alpha granule, fibrinogen complex and platelet alpha granule lumen, That of the VH and control group were the extracellular space, fibrinogen complex and extracellular region part, The TRD and vitreous hemorrhage (VH) groups were the intracellular vesicle, cytoplasmic vesicle, And cytoplasmic vesicle and secretory vesicle (Fig. 3).
KEGG pathways enrichment for DEPs in the different comparisons. The KEGG pathway enrichment analysis is represented as bar plots and bubble plots, respectively. For the upregulated deg, the top-enriched pathways are indicated in red. For the down-regulated degs, the top-enriched pathways are shown in blue. In the bubble plot, the horizontal axis is the enrichment factor, and the vertical axis is the name of the KEGG pathway. The bubble color is the significance level of the enrichment, and more red represents the more significant enrichment. The size of the bubbles is proportional to the number of the protein. Bar graph and bubble plot of KEGG pathway enrichment for TRD and vitreous hemorrhage (VH) (A, D), VH and control group (B, E), TRD and control group (C, F).
In order to analyze the biological process, the mechanism of disease, this project will all differentially expressed proteins KEGG pathway annotation, at the same time, the number of differentially expressed proteins, the statistics, the protein expression increased pathway in red, expression down pathways in blue, and the first few pathways with the largest number of differentially expressed proteins as shown in Fig. 4A,B,C. Compared between the TRD group and the control group (Fig. 4C), the most differentially expressed proteins were mainly Complement and coagulation cascade (17 DEPs) and Regulation of actin cytoskeleton (7 DEPs). Compared with the vitreous hemorrhage (VH) group and control group (Fig. 4B), the most differentially expressed proteins were mainly Complement and coagulation cascade (23 DEPs) and Regulation of actin cytoskeleton (12 DEPs). Comparing the TRD group with the vitreous hemorrhage (VH) (Fig. 4A), the pathways with the most differentially expressed proteins were concentrated in Complement and coagulation cascade (5 DEPs) and Platelet activation (4 DEPs). The above pathways are mainly correlated with the complement system and the coagulation cascade and platelet activation.
KEGG pathway enrichment analysis between the group, expressed in the form of bubble chart (Fig. 4D,E,F), where bubble color indicates the significance of KEGG pathway enrichment, color gradient represents the P-value (-log10), the closer the red represents the smaller the P value, the higher the significance level of enrichment of metabolic pathways. As can be seen from Fig. 4, the TRD group (Fig. 4F) and the VH group (Fig. 4E). Compared with the TRD and vitreous hemorrhage (VH) groups (Fig. 4D), there were significant changes in the Platelet activation pathway .
Analysis of protein interaction networks and functional clusters between different groups
PPI network and functional cluster analysis results of DEPs in different comparisons. After the functional classification of the interaction network map, the proteins in the same network module often have similar biological functions, and the proteins within the functional module of interest can be selected as the focus of subsequent research. (A, B) Differential protein PPI network and major functional clusters in groups of TRD and control group. (C, D) differential protein PPI networks and major functional clusters in groups VH and B. (E) Network diagram of differentially expressed protein interactions between TRD and vitreous hemorrhage (VH) groups.
To explore the interactions between the differentially expressed proteins of the different groups, based on the protein interaction relationships in the STRING or IntAct databases, we constructed a protein interaction network map on the differentially expressed proteins of the comparison groups using CytoScape software. As shown in Fig. 5, the circle represent the differential expression protein, the line represents protein interaction between proteins, the circle color represents protein expression difference (down in blue, up in red), the circle size indicates the protein connectivity. Generally speaking, the greater the connectivity, and the more likely to be the key to maintaining the balance and stability of the system, as a candidate protein for subsequent key research. These proteins were tightly linked to each other, and the central proteins in TRD, vitreous hemorrhage (VH) and control groups were primarily associated with sphingolipid metabolism.We compared TRD and vitreous hemorrhage (VH) with the control group, and selected the top 10 differentially expressed proteins that demonstrated increased expression and were associated with sphingolipid metabolism. Among these, we focused on validating three specific proteins: CHI3L1, LTBP2, and APOA4 (Tables 1 and 2).
APOA4, CHI3L1 as discriminatory biomarkers of TRD
To verify the expression of APOA4 and CHI3L1 in different vitreous fluids, the proteomics results of the collected vitreous were verified by enzyme-linked immunosorbent assay (ELISA). There was no significant difference in sex (p = 0.81) and age (p = 0.12) between the two groups (Table 3). APOA4 expression in TRD(131.92 ± 19.71 ng/mL) was significantly increased compared to control group (98.46 ± 10.55 ng/mL) (p = 0.003), and no significant difference between vitreous hemorrhage (VH) (117.99 ± 16.77ng/mL) and control group (98.46 ± 10.55 ng/mL) (p = 0.160) (Fig. 6A). CHI3L1 in TRD group expression (45.87 ± 4.61ng/mL) was significantly increased compared to control (29.58 ± 4.86 ng/mL) (p = 0.006) and VH group (35.47 ± 4.09 ng/mL) (p = 0.006), there was significant difference between VH (35.47 ± 4.09 ng/mL) and control group too (29.58 ± 4.86 ng/mL) (p = 0.006) (Fig. 6B). There was no significant difference among each group of the results of LTBP2. In addition, the receiver operating curve (ROC) curve of APOA4 and CHI3L1 displayed in Fig. 6.
Results of the candidate biomarkers in one-way ANOVA analysis, including the ROC curves for statistically significant comparisons between groups and respective plots. (A).Comparison of Apo-A4 protein abundance between groups measured by ELISA; (B) ROC curves depicting the classification power of Apo-A4; (C).Comparison of CHI3L1 protein abundance between groups measured by ELISA; (D).ROC curves depicting the classification power of CHI3L1. Data is presented in the plots as median ± SD, with asterisk determining the statistical significance: *p-value < 0.05, ** p-value < 0.01, ***p-value < 0.001, and ****p-value ≤ 0.0001.
Discussion
In recent years, the incidence of diabetic retinopathy (DR), as a serious complication of diabetic patients, has been increasing year by year11,and it has become one of the main causes of vision loss worldwide. The pathogenesis of DR is closely related to long-term hyperglycemia. Sustained hyperglycemia can lead to retinal microcirculation disorder and a large number of microvascular formation12, which makes the retina in a state of hypoxia and chronic inflammatory stimulation for a long time13,14,15. In this process, oxidative stress increase16, PKC pathway activation17,18,19, PI3K/Akt signaling pathway9,14,15activation mechanism plays a key role. Under the condition of hyperglycemia, the activation of PI3K/Akt pathway in the retina leads to the increased expression of downstream target genes such as VEGF, which further aggravates retinal capillary ischemia and promotes the formation of pathological neovascularization. In addition, under hyperglycemia, ROS production in retinal cells increases20,which leads to increased oxidative stress, destroys the integrity of cell membrane, induces apoptosis, microvascular damage and barrier damage, and then promotes the development of DR21,22. The presence of oxidative stress can also trigger local inflammation and cellular apoptosis, establishing a detrimental feedback loop that exacerbates the pathology of diabetic retinopathy21. Furthermore, there have been additional studies that have yielded EndoMT may underlie the pathogenesis of PDR, and the induction and regulation correlate with autophagy defects and the inflammatory response.
With the rapid development of proteomics technologies23,24,the study of protein expression changes in DR vitreous fluid has improved significantly. By collecting the vitreous humor from DR and non-diabetic retinopathy (NDR) patients for proteomics analysis, we found significant changes in the proteome profile in the vitreous fluid of DR patients. These differentially expressed proteins are closely related to immune response, oxidative stress and glucose metabolism, which provides effective information and new ideas for solving the clinical problems of DR25.Previous studies mostly compared PDR or DME with the control group. In order to observe the causes and initiation factors of TRD in DR, this study was divided into TRD and vitreous hemorrhage (VH) groups and compared with MH patients. By performing the GO enrichment and the KEGG pathway analysis, TRD versus control differential proteins were concentrated in Complement and coagulation cascade and Regulation of actin cytoskeleton, While comparing the TRD with the vitreous hemorrhage (VH) group, Differential proteins were mainly concentrated in Complement and coagulation cascade and Platelet activation, This is consistent with previous literature reports, the complement and coagulation cascade are the most important routes of PDR26.
Compared with control group, KDR, CA1, FGG, FGB, CHI3L1, FGA, CFD, APOA4, C2, SERPINA7 were the most significantly differentially expressed proteins in TRD. The KDR belonging to the tyrosine kinase family, encoding vascular endothelial growth factor receptor 2, mainly involved in angiogenesis and vascular permeability regulation26. CA1, carbonic anhydrase I, is an enzyme involved in the regulation of acid-base balance27. FGG, FGB, and FGA encode the three distinct chains of fibrinogen, a pivotal protein in hemostasis, with significant implications for wound healing, thrombosis development, and inflammatory responses28,29. CHI3L1 encodes chitinase-like protein3, a secreted glycoprotein expressed in the context of inflammation, tissue remodeling, and cancer. It is involved in diverse biological processes such as cell proliferation, migration, and angiogenesis30.CFD encodes the complement factor D in the complement system, which is a serine protease involved in the activation of the alternative complement replacement pathway, with an important contribution to the innate immune and inflammatory responses31. APOA4 encodes apolipoprotein A-IV, a protein associated with high-density lipoprotein (HDL) and involved in lipid metabolism and cholesterol transport, thereby influencing the risk of cardiovascular disease32. Component 2 of the C2 complement system, a pivotal protein in the classical complement activation pathway, exerts a crucial role in immune defense and is implicated in the eradication of pathogens and damaged cells33.SERPINA7 coding serine protease inhibitors A7, which is a kind of plasma serine protease inhibitors, may participate in regulating blood coagulation, fibrinolysis and inflammatory process34. It can be speculated that they may interact in certain common biological processes or disease states, such as inflammation, immune response, angiogenesis, or lipid metabolism. These processes often involve a complex network of multiple molecules and signaling pathways.
Analysis of the differentially expressed proteins between TRD and vitreous hemorrhage (VH) groups reveals that KDR, MYOC, LTBP2, CHI3L1, SPARC, PPIA, CST3, PFN1, RNASET2, and SPP1 exhibit the most significant alterations. Although KDR has been discussed in the comparison between TRD and Group B, it was not included in the subsequent analysis due to previous literature indicating that KDR expression is significantly influenced by anti-VEGF treatment post-surgery, and considering that both TRD and VH patients in this study had received anti-VEGF intravitreal injection prior to surgery35. MYOC is closely related to the occurrence of hereditary glaucoma and is one of the main genetic risk factors for glaucoma. MYOC gene mutation can lead to the obstruction of the aqueous humor discharge pathway, increase the intraocular pressure, and thus cause glaucoma36,37. LTBP2 binds to transforming growth factor β (TGF-β), participates in collagen synthesis and biological processes, and plays an important role in the formation and stability of extracellular matrix, cell adhesion and migration38. CHI3L1 is a kind of secreted glycoprotein30, also expressed in the TRD and control group. SPARC is a stromal cell protein, which is involved in the construction and remodeling of extracellular matrix and plays an important role in embryonic development, tissue repair and tumor growth39. PPIA, also known as cyclosporin A binding protein, is implicated in protein folding and signal transduction. It exhibits widespread expression across various cell types and plays a pivotal role in maintaining cellular homeostasis40. CST3 is a cysteine proteinase inhibitor that plays a pivotal role in modulating intracellular protein degradation processes and holds potential as a biomarker for renal function and the risk of cardiovascular disease41,42. PFN1 is involved in actin polymerization and dynamic changes of the cytoskeleton, and plays an important role in processes such as cell migration, division and morphology maintenance43. RNASET2 is a ribonuclease involved in RNA degradation and may play a role in immune defense and regulation of cell homeostasis44,45.SPP1 is a secreted phosphorylated glycoprotein involved in bone metabolism, immune regulation and tumor progression46,47. Despite the distinctive functions and roles of these proteins within their respective domains, specific information regarding their direct interactions may be somewhat limited. Nevertheless, it is conceivable that they could engage in shared biological processes or pathological conditions. For instance, KDR promotes angiogenesis and CHI3L1 involved in inflammation and tumor growth might synergistically facilitate cell proliferation and metastasis. In the context of tissue repair and inflammatory processes, LTBP2, CHI3L1, SPP1, along with other proteins, such as periostin (PN) and tenascin-C (TNC)48may collaborate to regulate the interplay between the extracellular matrix and immune cells.
The major DEP of TRD, VH and control groups are mainly related to sphingolipid metabolism, which is a novel finding in this paper. Lipid metabolism and sheath of phospholipids metabolic abnormalities are linked to many diseases. For example, in diabetic retinopathy (DR), lipid metabolism disorder is considered to be one of the important risk factors, and sphingomyelin metabolic abnormalities may also through affecting the stability of the retinal blood vessels and promote the progress of new angiogenesis to aggravate the DR. Based on this, we chose the TRD and vitreous hemorrhage (VH) compared with control group in the top 10 differentially expressed proteins and associated with sphingolipid metabolism and proteins associated with eye (CHI3L1 LTBP2, APOA4) for verification. Verification results show that the differences between CHI3L1 in three groups was statistically significant, APOA4 difference was statistically significant between TRD and the control group, while LTBP2 differences had no statistical significance between each group.
The literature reports that the role of inflammatory factors in the occurrence and development of DR cannot be ignored, so DR is considered to be an inflammatory disease49,50. A growing body of research has indicated that CHI3L1 participated in acute or chronic inflammation and angiogenesis. Previous studies have confirmed the serum or vitreous humor CHI3L1 levels changes associated with diabetic vascular complications51,suggesting CHI3L1 exerts an influence on the progression of DR. Xu Ying believe that the serum levels of CHI3L1 in patients with type 2 diabetes are significantly lower compared to those with DR, and CHI3L1 levels increased with the increase of DR severity, DR occurrence and progress of risk also increases with the increase of expression of CHI3L1. Kaya, et al.30 found CHI3L1 participated in the serous retinal detachment occurred in diabetic macular edema. CHI3L1 also plays a key role in inflammatory and immune responses. It can be combined with cell surface receptor, activation of downstream signaling pathways, which regulates the activity of immune cells and functions. In addition, the CHI3L1 can also promote the release of inflammatory mediators, further aggravate the inflammatory response. In a variety of inflammatory diseases such as rheumatoid arthritis, asthma, inflammatory bowel disease, the expression of CHI3L1 levels tend to rise significantly52. In the process of fibrosis, CHI3L1 also plays an important role. CHI3L1 can affect the structure and function of tissues by regulating the synthesis and degradation of extracellular matrix. In some fibrosis diseases, such as pulmonary fibrosis, liver fibrosis, the expression of CHI3L1 levels will rise. High expression of CHI3L1 may increase after laser induced ERK1/2 phosphorylation level so as to activate the MAPK pathway to promote choroidal neovascularization53. Interestingly, CHI3L1 also contributes to ameliorating the progression of certain diseases. It was reported that CHI3L1 played a protective role in injury by ameliorating inflammation and cell death, and a profibrotic role54. CHI3L1 was also shown to contributes to the amelioration of LPS-induced atherosclerotic reactions via PPARδ-mediated suppression of inflammation and endoplasmic reticulum stress. CHI3L1’s dual role as both a protective and pathogenic factor underscores its complexity in inflammatory diseases. Its functional outcomes depend on the interplay of disease stage, tissue microenvironment, and molecular interactions. Our result in here shows that the potential significance of CHI3L1 as a predictive factor for TRD, future research should focus on elucidating context-specific mechanisms to develop targeted therapies.
Apolipoproteins have been reported as a more significant marker for diabetic retinopathy (DR) and also was involving with the pathology of PDR. Apolipoprotein A-IV (ApoA-IV or APOA4) is synthesized by the small intestine and liver, serving as a plasma lipoprotein involved in regulating various metabolic functions in the body, such as appetite inhibition, lipid absorption promotion, cholesterol reverse transport, etc. APOA4 was found reduced in the PDR patients compared with the macular hole patients55, which had conflicts with Jianqing Li’s result56.Additionally, Ouchi et al. study suggested that the increase in apolipoprotein A-IV is associated with the deposition of hard exudates, seen in DME patients, as they are composed of lipids57. Our study found that APOA4 levels were elevated in the TRD group, which is consistent with previous reports, suggesting that APOA4 may be an indicator of DR secondary changes. Inflammation is a crucial mechanism in the development of DR. APOA4 has been reported to regulate inflammatory responses in certain disease states, although direct research on APOA4’s inflammatory modulation in DR is limited. It is speculated that APOA4 may be involved in the pathological process of DR by influencing the expression or activity of inflammatory factors.
This study revealed significant alterations in the proteome profile of vitreous fluid from DR patients, as determined by LC-MS/MS analysis. Bioinformatics analysis indicated that the differentially expressed proteins were closely associated with the Complement and coagulation cascade, Regulation of actin cytoskeleton, sphingolipid metabolism and Platelet activation pathways; however, further investigation is required to elucidate their specific mechanisms of action. The expression of inflammatory factors such as CHI3L1 increases during the course of diabetic retinopathy (DR), contributing to both acute and chronic inflammation as well as angiogenesis. The levels of these factors are closely associated with the severity of DR lesions. Furthermore, abnormal expression of APOA4, a plasma lipoprotein with anti-inflammatory and antioxidant properties, is also observed in DR, potentially implicating its role in the pathogenesis of DR. While this study provides novel insights into DR proteomics, several limitations warrant consideration. The single-center design and restricted sample size may limit generalizability. Future studies will focus on three synergistic directions: (1) Longitudinal mapping of disease progression through multimodal biomarkers coupled with temporal proteomic profiling to decode dynamic molecular trajectories; (2) Mechanistic validation using complementary animal models (genetic and induced DR systems) with parallel in vivo imaging and in vitro functional assays to elucidate causal pathways; (3) Translational optimization focusing on prioritized candidate proteins, establishing preclinical-efficacy benchmarks via dose-response studies and primate model validations to accelerate therapeutic development.
Materials and methods
Subject
This study was approved by the Medical Ethics Committee of Tianjin Eye Hospital (Approval No.: TJYYLL-2018-01) and performed under the guidance of the Declaration of Helsinki. Written informed consent was obtained from all subjects to publish this paper. A total of 14 patients were recruited for LC-MS/MS analysis, and these patients were divided into 3 groups, including 4 patients with idiopathic macular hole (Control Group), 5 patients with vitreous hemorrhage (VH Group), and 5 patients with traction retinal detachment (TRD Group)(Fig. 1). Inclusion criteria included patients aged 18–85 years, with indications for vitrectomy surgery and consent to surgery. Exclusion criteria included: systemic or ocular infectious diseases; systemic use of corticosteroids, immunosuppressive agents or antimetabolites; a history of other ocular surgery or laser treatment; and other ocular diseases such as pathological myopia, retinal neovascularization, glaucoma, retinal vascular occlusion, etc. There were no significant differences in baseline data including sex and age comparison between the two groups (all p > 0.05) (Table 3).
Sample collection and Preparation
All patients underwent a standard 25G vitrectomy, and all procedures were performed by the three experienced surgeons. The patients underwent intravitreal anti-VEGF medication (Conbercept) 3–5 days before surgery.Vitreous samples were collected during standard three-port vitrectomy, before connecting the infusion and then immediately transferred to a sterilized Eppendorf tube in the-80℃ refrigerator.
SDT(4%SDS, 100mM Tris-HCl, 1mM DTT, pH7.6) buffer was used for sample lysis and protein extraction. The amount of protein was quantified with the BCA Protein Assay Kit (Bio-Rad, USA). Protein digestion by trypsin was performed according to filter-aided sample preparation (FASP) procedure described by Matthias Mann. The digest peptides of each sample were desalted on C18 Cartridges(Empore™ SPE Cartridges C18 (standard density), concentrated by vacuum centrifugation and reconstituted in 40 µl of 0.1% (v/v) formic acid.
LC-MS/MS analysis
A Q Exactive mass spectrometer (Thermo Scientific) coupled with Easy nLC (Thermo Fisher Scientific) was used for comprehensive LC-MS/MS analysis. Peptides loaded onto a reverse phase trap column linked to a C18 analytical column (Thermo Scientific Easy Column,10 cm, 75 μm ID, 3 μm resin) in Buffer A (0.1% FA), separated with a linear gradient of Buffer B (84% ACN + 0.1% FA) at 300 nl/min via IntelliFlow. In this study, the mass spectrometer was operated in the positive ion modality. During data acquisition, the most abundant precursor ions within the survey scan range of 300–1800 m/z were dynamically selected using a data-dependent top10 approach for subsequent HCD fragmentation to generate MS data. The target for the Automatic Gain Control (AGC) was established at 3e6, while the maximum injection time was limited to 10 milliseconds. Additionally, the duration of dynamic exclusion was configured to last for 40.0 s.The survey scans were collected with a resolution of 70,000 at an m/z value of 200, while the resolution for the HCD spectra was specifically set to 17,500 at m/z 200. Additionally, the isolation width was maintained at 2 m/z. The normalized collision energy was set to 30 eV, while the underfill ratio, determining the minimum percentage of the target value likely to be achieved at the maximum fill time, was defined as 0.1%.
Bioinformatics analysis
The MS raw data for each sample were combined and searched using the MaxQuant software (version: 1.5.3.17), and the quantitative information of the target protein set was normalized (normalized to the interval (-1,1)). The DEPs presented more than 2.0 Fold Change (FC) and P value < 0.05. The Complexheatmap R package (Version:3.4) is used to generate hierarchical clustering heat maps.The Gene Ontology (GO) terms were assigned and the sequences were annotated utilizing the Blast2GO software application. Subsequently, the outcomes of these GO annotations were visually represented using R scripts. The studied proteins were blasted against the online Kyoto Encyclopedia of Genes and Genomes (KEGG) database (http://geneontology.org/)58,59,60. GO function annotation and KEGG pathway analysis were performed for all DEPs. GO functional annotations are mainly divided into three categories: Biological Process (BP), Molecular Function (MF), and Cellular Component (CC).The protein-protein interaction (PPI) data for the proteins under investigation was obtained from the IntAct molecular interaction database (accessible at http://www.ebi.ac.uk/intact/) using their respective gene symbols as identifiers. The outcomes were transferred into the Cytoscape software platform (accessible at http://www.cytoscape.org/, version 3.9.1) for the purpose of visualizing and conducting a deeper analysis of the functional protein-protein interaction networks. The volcano plots were created using R (version 3.4.1) in figures.
ELISA measurement
APOA4, YKL 40, and LTBP2 (Jiangsu Meilian industrial Co., Ltd) was selected as the target proteins, and the measured ELISA method was applied for the validation of these proteins expression in the samples of individual patients, including 6 patients with idiopathic macular hole (Control Group), 7 patients treated with vitreous hemorrhage (VH Group), and 9 patients with traction retinal detachment (TRD Group). The enrollment criteria and vitreous humour collection methods were consistent with the LC-MS/MS analysis method described above. In these ELISA assays, each sample was tested in triplicate according to the ELISA kit protocol. (Fig. 1)
Statistical analysis
For statistical analysis, clinical data were performed by the standard deviation of mean ± SD and analyzed between groups using Student’s test and one-way analysis of variance. For all analyses, p < 0.05 was considered statistically significant, and all p values were derived from 2-sided tests.
Data availability
Data is provided within the supplementary information files.
References
Lechner, J., O’Leary, O. E. & Stitt, A. W. The pathology associated with diabetic retinopathy. Vis. Res. 139, 7–14. https://doi.org/10.1016/j.visres.2017.04.003 (2017).
Fong, D. S., Ferris, F. L. 3, Davis, M. D., Chew, E. Y. & rd, & Causes of severe visual loss in the early treatment diabetic retinopathy study: ETDRS report 24. Early treatment diabetic retinopathy study research group. Am. J. Ophthalmol. 127, 137–141. https://doi.org/10.1016/s0002-9394(98)00309-2 (1999).
Haines, N. R., Manoharan, N., Olson, J. L., D’Alessandro, A. & Reisz, J. A. Metabolomics analysis of human vitreous in diabetic retinopathy and rhegmatogenous retinal detachment. J. Proteome Res. 17, 2421–2427. https://doi.org/10.1021/acs.jproteome.8b00169 (2018).
Weber, S. R. et al. Proteomic analyses of vitreous in proliferative diabetic retinopathy: prior studies and future outlook. J. Clin. Med. 10 https://doi.org/10.3390/jcm10112309 (2021).
Barba, I. et al. Metabolic fingerprints of proliferative diabetic retinopathy: an 1H-NMR-based metabonomic approach using vitreous humor. Invest. Ophthalmol. Vis. Sci. 51, 4416–4421. https://doi.org/10.1167/iovs.10-5348 (2010).
Paris, L. P. et al. Global metabolomics reveals metabolic dysregulation in ischemic retinopathy. Metabolomics 12 https://doi.org/10.1007/s11306-015-0877-5 (2016).
Zou, C. et al. Change of ranibizumab-induced human vitreous protein profile in patients with proliferative diabetic retinopathy based on proteomics analysis. Clin. Proteom. 15 https://doi.org/10.1186/s12014-018-9187-z (2018).
Itoh, K. et al. Detection of significantly high vitreous concentrations of fatty acid-binding protein 4 in patients with proliferative diabetic retinopathy. Sci. Rep. 11 https://doi.org/10.1038/s41598-021-91857-1 (2021).
Antonetti, D. A., Silva, P. S. & Stitt, A. W. Current Understanding of the molecular and cellular pathology of diabetic retinopathy. Nat. Rev. Endocrinol. 17, 195–206. https://doi.org/10.1038/s41574-020-00451-4 (2021).
Lauwen, S., de Jong, E. K., Lefeber, D. J. & den Hollander, A. Omics biomarkers in ophthalmology. Invest. Ophthalmol. Vis. Sci. 58, Bio88–bio. https://doi.org/10.1167/iovs.17-21809 (2017).
Ejigu, T. & Tsegaw, A. Prevalence of diabetic retinopathy and risk factors among diabetic patients at university of Gondar tertiary eye care and training center, North-West Ethiopia. Middle East. Afr. J. Ophthalmol. 28, 71–80. https://doi.org/10.4103/meajo.meajo_24_21 (2021).
Gaonkar, B. et al. Plasma angiogenesis and oxidative stress markers in patients with diabetic retinopathy. Biomarkers 25, 397–401. https://doi.org/10.1080/1354750x.2020.1774654 (2020).
Rezzola, S. et al. Angiogenesis-Inflammation cross talk in diabetic retinopathy: novel insights from the chick embryo Chorioallantoic membrane/human vitreous platform. Front. Immunol. 11, 581288. https://doi.org/10.3389/fimmu.2020.581288 (2020).
Yang, Q. et al. Silencing Nogo-B improves the integrity of blood-retinal barrier in diabetic retinopathy via regulating Src, PI3K/Akt and ERK pathways. Biochem. Biophys. Res. Commun. 581, 96–102. https://doi.org/10.1016/j.bbrc.2021.10.024 (2021).
Zhang, Y., Wang, W. & Yang, A. The involvement of ACO3 protein in diabetic retinopathy through the PI3k/Akt signaling pathway. Adv. Clin. Exp. Med. 31, 407–416. https://doi.org/10.17219/acem/121930 (2022).
Mahajan, N., Arora, P. & Sandhir, R. Perturbed biochemical pathways and associated oxidative stress lead to vascular dysfunctions in diabetic retinopathy. Oxid. Med. Cell Longev. 2019 8458472. https://doi.org/10.1155/2019/8458472 (2019).
Amadio, M. et al. The PKCbeta/HuR/VEGF pathway in diabetic retinopathy. Biochem. Pharmacol. 80, 1230–1237. https://doi.org/10.1016/j.bcp.2010.06.033 (2010).
Titchenell, P. M. & Antonetti, D. A. Using the past to inform the future: anti-VEGF therapy as a road map to develop novel therapies for diabetic retinopathy. Diabetes 62, 1808–1815. https://doi.org/10.2337/db12-1744 (2013).
Birkenfeld, A. L. & Shulman, G. I. Nonalcoholic fatty liver disease, hepatic insulin resistance, and type 2 diabetes. Hepatology 59, 713–723. https://doi.org/10.1002/hep.26672 (2014).
Rudraraju, M., Narayanan, S. P. & Somanath, P. R. Regulation of blood-retinal barrier cell-junctions in diabetic retinopathy. Pharmacol. Res. 161 https://doi.org/10.1016/j.phrs.2020.105115 (2020).
Li, C. et al. Oxidative stress-related mechanisms and antioxidant therapy in diabetic retinopathy. Oxid. Med. Cell Longev. 2017 9702820. https://doi.org/10.1155/2017/9702820 (2017).
Kang, Q. & Yang, C. Oxidative stress and diabetic retinopathy: molecular mechanisms, pathogenetic role and therapeutic implications. Redox Biol. 37 https://doi.org/10.1016/j.redox.2020.101799 (2020).
Aslam, B., Basit, M., Nisar, M. A., Khurshid, M. & Rasool, M. H. Proteomics: technologies and their applications. J. Chromatogr. Sci. 55, 182–196. https://doi.org/10.1093/chromsci/bmw167 (2017).
Rotello, R. J. & Veenstra, T. D. Mass spectrometry techniques: principles and practices for quantitative proteomics. Curr. Protein Pept. Sci. 22, 121–133. https://doi.org/10.2174/1389203721666200921153513 (2021).
Zou, C. et al. Difference in the vitreal protein profiles of patients with proliferative diabetic retinopathy with and without intravitreal conbercept injection. J. Ophthalmol. 2018 7397610. https://doi.org/10.1155/2018/7397610 (2018).
Santos, F. M. et al. Proteomics profiling of vitreous humor reveals complement and coagulation components, adhesion factors, and neurodegeneration markers as discriminatory biomarkers of vitreoretinal eye diseases. Front. Immunol. 14, 1107295. https://doi.org/10.3389/fimmu.2023.1107295 (2023).
Gao, B. B. et al. Extracellular carbonic anhydrase mediates hemorrhagic retinal and cerebral vascular permeability through prekallikrein activation. Nat. Med. 13, 181–188. https://doi.org/10.1038/nm1534 (2007).
Youngblood, H., Robinson, R., Sharma, A. & Sharma, S. Proteomic biomarkers of retinal inflammation in diabetic retinopathy. Int. J. Mol. Sci. 20 https://doi.org/10.3390/ijms20194755 (2019).
Alli-Shaik, A. et al. System-wide vitreous proteome dissection reveals impaired Sheddase activity in diabetic retinopathy. Theranostics 12, 6682–6704. https://doi.org/10.7150/thno.72947 (2022).
Kaya, M. et al. A novel biomarker in diabetic macular edema with serous retinal detachment: serum Chitinase-3-Like protein 1. Ophthalmologica 241, 90–97. https://doi.org/10.1159/000490534 (2019).
Shahulhameed, S. et al. A systematic investigation on complement pathway activation in diabetic retinopathy. Front. Immunol. 11, 154. https://doi.org/10.3389/fimmu.2020.00154 (2020).
Zhang, Y. et al. Proteomic analysis of aqueous humor reveals novel regulators of diabetic macular edema. Exp. Eye Res. 239 https://doi.org/10.1016/j.exer.2023.109724 (2024).
Cehofski, L. J. et al. Central subfield thickness of diabetic macular edema: correlation with the aqueous humor proteome. Mol. Vis. 30, 17–35 (2024).
Wang, T., Chen, H., Li, N., Zhang, B. & Min, H. Aqueous humor proteomics analyzed by bioinformatics and machine learning in PDR cases versus controls. Clin. Proteom. 21 https://doi.org/10.1186/s12014-024-09481-w (2024).
Rezzola, S. et al. 3D endothelial cell spheroid/human vitreous humor assay for the characterization of anti-angiogenic inhibitors for the treatment of proliferative diabetic retinopathy. Angiogenesis 20, 629–640. https://doi.org/10.1007/s10456-017-9575-4 (2017).
Huang, X. et al. Mutation analysis of seven known glaucoma-associated genes in Chinese patients with glaucoma. Invest. Ophthalmol. Vis. Sci. 55, 3594–3602. https://doi.org/10.1167/iovs.14-13927 (2014).
Vergaro, A. et al. Primary open-angle glaucoma due to mutations in the myoc gene. Cesk. Slov. Oftalmol. 78, 242–248, https://doi.org/10.31348/2022/25 (2022).
Rifkin, D. B., Rifkin, W. J. & Zilberberg, L. LTBPs in biology and medicine: LTBP diseases. Matrix Biol. 71–72, 90–99. https://doi.org/10.1016/j.matbio.2017.11.014 (2018).
Cho, W. J. et al. Involvement of SPARC in in vitro differentiation of skeletal myoblasts. Biochem. Biophys. Res. Commun. 271, 630–634. https://doi.org/10.1006/bbrc.2000.2682 (2000).
Wu, Y. et al. Cyclophilin A regulates the apoptosis of A549 cells by stabilizing Twist1 protein. J. Cell. Sci. 135 https://doi.org/10.1242/jcs.259018 (2022).
t Hart, L. M. et al. Small RNA sequencing reveals snornas and piRNA-019825 as novel players in diabetic kidney disease. Endocrine https://doi.org/10.1007/s12020-024-03884-3 (2024).
Zhu, Y. Z. et al. Genome-Wide search links senescence-associated secretory proteins with susceptibility for coronary artery disease in mouse and human. J. Gerontol. Biol. Sci. Med. Sci. 79 https://doi.org/10.1093/gerona/glae070 (2024).
Funes, S. et al. Expression of ALS-PFN1 impairs vesicular degradation in iPSC-derived microglia. Nat. Commun. 15 https://doi.org/10.1038/s41467-024-46695-w (2024).
Mukai, N., Nakanishi, T., Shimizu, A., Takubo, T. & Ikeda, T. Identification of phosphotyrosyl proteins in vitreous humours of patients with vitreoretinal diseases by sodium Dodecyl sulphate-polyacrylamide gel electrophoresis/western blotting/matrix-assisted laser desorption time-of-flight mass spectrometry. Ann. Clin. Biochem. 45, 307–312. https://doi.org/10.1258/acb.2007.007151 (2008).
Li, Z. et al. RNA-Seq revealed novel Non-proliferative retinopathy specific Circulating MiRNAs in T2DM patients. Front. Genet. 10, 531. https://doi.org/10.3389/fgene.2019.00531 (2019).
Giachelli, C. M. & Steitz, S. Osteopontin: a versatile regulator of inflammation and biomineralization. Matrix Biol. 19, 615–622. https://doi.org/10.1016/s0945-053x(00)00108-6 (2000).
Rejas-González, R. et al. Proteomics analyses of small extracellular vesicles of aqueous humor: identification and validation of GAS6 and SPP1 as Glaucoma markers. Int. J. Mol. Sci. 25 https://doi.org/10.3390/ijms25136995 (2024).
Kubo, Y. et al. Periostin and tenascin-C interaction promotes angiogenesis in ischemic proliferative retinopathy. Sci. Rep. 10 https://doi.org/10.1038/s41598-020-66278-1 (2020).
Forrester, J. V., Kuffova, L. & Delibegovic, M. The role of inflammation in diabetic retinopathy. Front. Immunol. 11, 583687. https://doi.org/10.3389/fimmu.2020.583687 (2020).
Spencer, B. G., Estevez, J. J., Liu, E., Craig, J. E. & Finnie, J. W. Pericytes, inflammation, and diabetic retinopathy. Inflammopharmacology 28, 697–709. https://doi.org/10.1007/s10787-019-00647-9 (2020).
Rathcke, C. N., Persson, F., Tarnow, L., Rossing, P. & Vestergaard, H. YKL-40, a marker of inflammation and endothelial dysfunction, is elevated in patients with type 1 diabetes and increases with levels of albuminuria. Diabetes Care. 32, 323–328. https://doi.org/10.2337/dc08-1144 (2009).
Yu, J. E. et al. Significance of chitinase-3-like protein 1 in the pathogenesis of inflammatory diseases and cancer. Exp. Mol. Med. 56, 1–18. https://doi.org/10.1038/s12276-023-01131-9 (2024).
Xu, N. et al. Chitinase-3-Like-1 promotes M2 macrophage differentiation and induces choroidal neovascularization in neovascular Age-Related macular degeneration. Invest. Ophthalmol. Vis. Sci. 60, 4596–4605. https://doi.org/10.1167/iovs.19-27493 (2019).
Zhou, Y. et al. Chitinase 3-like 1 suppresses injury and promotes fibroproliferative responses in mammalian lung fibrosis. Sci. Transl Med. 6 (ra276), 240. https://doi.org/10.1126/scitranslmed.3007096 (2014).
Kim, S. J. et al. Differential expression of vitreous proteins in proliferative diabetic retinopathy. Curr. Eye Res. 31, 231–240. https://doi.org/10.1080/02713680600557030 (2006).
Li, J., Lu, Q. & Lu, P. Quantitative proteomics analysis of vitreous body from type 2 diabetic patients with proliferative diabetic retinopathy. BMC Ophthalmol. 18 https://doi.org/10.1186/s12886-018-0821-3 (2018).
Ouchi, M., West, K., Crabb, J. W., Kinoshita, S. & Kamei, M. Proteomic analysis of vitreous from diabetic macular edema. Exp. Eye Res. 81, 176–182. https://doi.org/10.1016/j.exer.2005.01.020 (2005).
Kanehisa, M. & Goto, S. KEGG: Kyoto encyclopedia of genes and genomes. Nucleic Acids Res. 28, 27–30. https://doi.org/10.1093/nar/28.1.27 (2000).
Kanehisa, M. Toward Understanding the origin and evolution of cellular organisms. Protein Sci. 28, 1947–1951. https://doi.org/10.1002/pro.3715 (2019).
Kanehisa, M., Furumichi, M., Sato, Y., Matsuura, Y. & Ishiguro-Watanabe, M. KEGG: biological systems database as a model of the real world. Nucleic Acids Res. 53, D672–d677. https://doi.org/10.1093/nar/gkae909 (2025).
Funding
This study was supported by Tianjin Key Medical Discipline (Specialty) Construction Project (grant number TJYXZDXK-016 A), Tianjin Health Research Project (Grant No.TJWJ2024MS033), Science Foundation of Tianjin Educational Commission Fund(Grant No.2020KJ157), Science and Technology Foundation of Tianjin Eye Hospital (Grant No.YKPY2208).
Author information
Authors and Affiliations
Contributions
Conceived and designed the experiments: Yuyan Liu, Rongjie Wei, Xiujuan Zhao and Yanhua Chu; Performed the experiments: Yuyan Liu, Rongjie Wei; funding acquisition: Yanhua Chu, Yuyan Liu, Wei Zhang and Zhenhua Pan; software and formal analysis: Shuo Sun, Yong Tang and Wei Zhang; investigation, data curation, original draft: Yuyan Liu, Rongjie Wei and Yu Zhou; review & editing: Yanhua Chu, Xiujuan Zhao and Quanhong Han. All authors contributed to the article and approved the submitted version.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics statement
The study was conducted in accordance with the Declaration of Helsinki, and was approved by the Medical Ethics Committee of Tianjin Eye Hospital (Approval No.: TJYYLL-2018-01).
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Liu, Y., Wei, R., Tang, Y. et al. Identification of unique biomarkers for proliferative diabetic retinopathy with tractional retinal detachment by proteomics profiling of vitreous humor. Sci Rep 15, 13456 (2025). https://doi.org/10.1038/s41598-025-98327-y
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-98327-y