Abstract
Blood tests (BTs), specifically liver and/or kidney function tests, are employed in Korean Medicine (KM) practice to ensure the safety of herbal medicine. The widespread concomitant use of conventional and herbal medicines in South Korea requires BTs due to the unpredictable liver injury and drug–herb interactions. However, BTs ordered by Korean Medicine doctors (KMDs) are currently not covered by the National Health Insurance (NHI), which further leads to a lack of data on the demographics and utilization of BT in KM practice. This study surveys the frequency and features of BT utilization through a national sampling of KMDs. Between February 10 and 20, 2023, a questionnaire was developed and electronically distributed to 25,574 KMDs across the nation, comprising all licensed and qualified to practice KM at the time of the survey. We assessed respondents’ characteristics, perceptions, current use and usage patterns, including frequency and indication of BT, and unmet BT needs. Of the 830 KMD (3.25% of all the licensed) respondents, 363 incorporate BTs in their workups, while 467 do not. Liver function tests (n = 351) are the most common, followed by kidney function (n = 235) and diabetes (n = 188) tests. The time of ordering BT varied by institution, with KM hospitals most often in “the patient’s first visit” (45.71%), and KM clinics “before and after prescription of herbal medicine.” (43.75% in specialized clinics; 36.95% in non-specialized). The purposes of ordering BTs were to complement the assessment of health conditions (67.22%), monitor herb-induced liver injury (58.68%), and follow up after KM treatment (55.10%). Meanwhile, 97% of the current non-users of BT hope to use it in the future, with 90.36% suggesting that BTs be covered by the NHI. Understanding the current BT practice pattern may guide the creation of guidelines for proper BT usage in KM practice. In addition, stakeholders must recognise the importance of BTs in real-world KM practice to monitor patients’ condition or reactions after herbal medicine administration.
Similar content being viewed by others
Introduction
Blood tests (BTs) are integrated into the practice of traditional East Asian medicine to assess the safety of herbal medicine (HM) and treatment outcomes when deemed appropriate. BT indicates that HM has demonstrated effectiveness in the treatment of inflammation and infection, as well as in the improvement of endocrine and metabolic disorders1,2,3,4. Liver function tests (LFTs) are highly valued and recommended as routine tests in daily Traditional Chinese Medicine (TCM) practice owing to their potential for detecting herb-induced liver injury (HILI)5. In South Korea, where HM is prescribed by licensed Korean Medicine doctors (KMDs), concomitant use of conventional and herbal medicines is widespread6. Within the cohorts of liver injury cases in which herbs were indicated as one of the causative agents, the proportion of HILI was approximately 25% of all cases of drug-induced liver injury (DILI)7. In principle, DILI may occur with any drug, even if used appropriately8. Furthermore, HILI mostly occurs in idiosyncratic types, which are dose-independent and unpredictable7. In light of this, a growing number of practices that administer HM choose to run LFTs to monitor HILI and drug–herb interactions. Insurance entities, however, consider liver or kidney function tests non-essential procedures in Korean Medicine (KM) practice, causing users to pay the associated fees out of pocket. Some competing medical bodies argue that KMDs’ use of BTs will lead to unnecessary duplication of tests and increased costs9,10.
As KMDs seek to incorporate BTs into their practice, following the 2014 authoritative interpretation from the Ministry of Health and Welfare that KMDs could use BT devices11, the Association of Korean Medicine has launched a campaign to encourage using BTs in KM clinics. According to the Korean Medicine policy research center of Korea Institute of Oriental Medicine, diagnostic medical devices were used in 64.2% of KM clinical studies between 2017 and 2019, with the most common tests being BTs (23.5%)12. BTs have also been the predominant medical tool featured in job analysis and license exams for KMDs12. However, regarding BTs, there is a discrepancy between the demand on KM clinics and the coverage provided by National Health Insurance (NHI). Furthermore, the absence of KMDs from the BT claim has resulted in a lack of demographic information on both patients and KMDs who use BT in KM practice, despite the fact that the NHI system in South Korea offers extensive claim data for the entire population. This survey aims to understand the nationwide frequency of BTs and their characteristics in KM clinics. We also aim to survey the perceptions of BT and identify KMDs’ needs for BTs. The present study may provide evidence for the use of BTs to ensure the safety of KM treatment, thus promoting the use of BTs in KM practice and improving the NHI system in South Korea.
Methods
Participants and recruitment
All licensed KMDs were invited to participate in the email survey (n = 25,574) through the Association of Korean Medicine. Identifying the precise target population posed challenges due to the presence of licensed KMDs who are not practicing. This study required a sample size of 830 participants to estimate the expected proportion with a margin of error for estimated rates of ± 3.4% points, conservatively assuming a population rate of 50% and a 95% confidence level13. The cross-sectional survey was conducted between February 10 and February 20, 2023. The questionnaire was based on voluntary responses without sampling. A gift card worth 3 USD was given as a reward to 300 participants (the first 100 and 200 randomly selected participants) who completed the survey.
Survey design
Two KMD researchers created the questionnaire by reviewing previous literature14,15. The draft was finalised after content validity was assessed by a panel of 10 KMDs, including those who use BT in clinics and professors at the College of KM who have experience with survey studies. Only items with a content validity ratio ≥ 0.8 were retained in the final questionnaire16. The questionnaire comprised 47 questions in 6 sections: sociodemographic characteristics of the participants, BT perception, current BT use, usage pattern, unmet needs of BTs, and perceptions of the campaign to use BT. To assess participant eligibility, a question to confirm whether each participant was currently working as a clinician and practising KM was included at the beginning of the questionnaire; the survey automatically closed when the answer was “no.” The survey was supposed to be completed within a maximum of ten minutes.
Survey questions were entered into an online survey tool (SurveyMonkey, San Mateo, CA, USA), and responses were limited to once per participant. A single pilot test participating four KMDs, consisting of three practicing KMDs and one researcher with expertise in survey research, was conducted to verify the completeness and comprehensibility of the survey.
Ethical considerations
Informed consent was obtained from all participants before they completed the survey. Consent included information on the purpose and target of the study, voluntary participation, and confidentiality. Only respondents who voluntarily agreed to participate were permitted to proceed with the survey. This study was approved by the institutional review board (IRB) of the Korea Institute of Oriental Medicine (I-2212/012 − 001). All methods were performed in accordance with the Declaration of Helsinki and the relevant guidelines and regulations in human research of the IRB of the Korea Institute of Oriental Medicine. The surveys were conducted anonymously. The mobile phone number collected to provide the reward was managed separately from the response data and deleted immediately after the reward was provided. The raw data of the survey response were accessible only to one researcher, and the research results were shared only with the researchers and kept confidential. This study complied with the Checklist for Reporting of Survey Studies17.
Statistical analysis
Incomplete responses were excluded from the analysis to ensure reliability. The characteristics of survey respondents were presented as frequency (%), classified according to the experience of using BT. A Chi-squared test was performed to identify significant differences in the experience of using BTs according to the characteristics of the survey respondents, including sex, age, medical experience after obtaining a license, occupation, employment region, type of medical institution, highest academic degree, and qualification. Perceptions of whether BTs are actively used in KM practice and they are required in clinical practice were analysed using the Cochran–Armitage Trend test. Data were analysed using SAS software, version 9.4 (SAS Institute Inc., Cary, NC, USA). Statistical significance was set at p < 0.05. Two-tailed comparisons were performed.
Results
Sociodemographic characteristics of participants
Of the 25,574 registered KMDs, 931 initiated the survey. A total of 830 (3.25%) survey responses were analysed after excluding two individuals who did not consent to participate in the study, four who were not currently practising, and 95 who did not complete the survey. The demographics and practice characteristics of the survey respondents are presented in Table 1. A total of 363 (43.73%) KMDs responded that they currently use BTs, while 467 (56.27%) responded that they do not. The 830 respondents were most likely to be 30–39 years old (36.14%) and self-employed (60.0%). Of the 830, 629 (75.78%) were general practitioners (GPs), and 201 (24.22%) were specialists. The 76 specialities of the KM clinics included skin diseases (30.26%), obesity (28.95%), paediatric growth (19.74%), women’s diseases (18.42%), digestive diseases (18.42%), rhinitis (11.84%), autoimmune diseases (11.84%), cancer (7.89%), psychiatric diseases (6.58%), and neurological diseases (3.95%) (including duplicates). The percentage of BT users was higher in KMDs who mainly treat middle-aged (30–49 years old) patients (38.57%, p < 0.0001), who were specialists (31.68%, p < 0.0001), held a PhD (27.55%) or Master’s degree (26.45%) (p < 0.0001), worked in a KM hospital (27.27%, p < 0.0001), worked in city (commercial areas) (27%, p < 0.0001), were interns or residents (10.19%) and clinical faculty (6.34%) (p < 0.0001). There were no differences in the current use of BTs according to sex, age, years of medical experience after licensure, employment region, or KM area of speciality (Table 1).
Perception on BTs
When asked whether BTs were actively used in KM clinical practice, 76.63% disagreed. The percentage of negative responses was higher among BT non-users (p < 0.0001), those who work in KM clinics (p < 0.0001), and GPs (p = 0.0296). Most BT users (98.9%) and non-users (93.58%) believed that BT is essential in their clinical practices. There were 622 (74.94%) who were aware that BT can be used to monitor the progress of KM treatment, with a significantly high proportion of BT users (62.59%) that “strongly agree” with this statement (p < 0.0001; Table 2).
BT frequency and indications in KM practice
Among the 363 users, BTs were predominantly ordered 1–9 times (41.32%) in the past month. Most BT users in KM hospitals (98.10%) were referred by KMDs to a medical doctor (MD), whereas 87.7% in KM clinics were not. Peripheral fingerstick (55.92%) and venipuncture (53.44%) were the most common blood sampling methods and were predominantly performed by nurses or nursing assistants (77.84%). BT analysis was more likely to be performed using an automated analyser (76.31%) than by transferring to a specialised laboratory (35.54%). Centrifuges were more likely to be used in KM hospitals (64.76%) than in KM clinics (25.5%) or other institutions (14.29%; p < 0.0001) (Table 3).
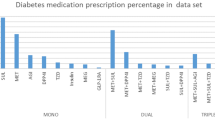
Most BT users (96.69%) ordered LFTs, followed by kidney function tests (KFTs; 64.74%), diabetes tests (51.79%), lipid panels (51.52%), and complete blood counts (CBCs; 51.24%). Other parameters suggested by respondents were prothrombin time, hepatitis tests (amylase, lipase, IgE, live blood tests), and anti-Müllerian hormone, D-dimer, procalcitonin, and uric acid levels. The main purposes of BTs were to determine the basic health condition (67.22%), monitor HILI (58.68%), follow up after KM treatment (55.10%), decide whether or not to prescribe HM (42.98%), and rule out severe or acute diseases (32.78%). In total, 80.95% of BT users in KM hospitals ordered blood testing as a basic examination upon admission. Other purposes included checking BT levels before prescribing HM to avoid “the misunderstanding of existing illnesses as being caused by HM,” diagnosing and treating “precocious puberty,” and participating in a government “infertility support program.” Most BT users (93.67%) replied that BTs are important in their practice (Table 3). According to the survey, the average percentage of patients undergoing blood testing was 24.29% (± 30.02%) (median 10%, mode 10%) (Supplementary Table S1).
BTs were ordered by 51.52% of BT users regardless of the patient’s chief complaint or disease, while 36.09% ordered when patients complained of fatigue or decreased stamina. Among the International Classification of Diseases − 10 categories, ‘Endocrine, nutritional, and metabolic diseases (Chapter IV)’ (25.90%), ‘Diseases of the digestive system (Chapter XI)’ (21.76%), and ‘Diseases of the circulatory system (Chapter IX)’ (15.43%) were the most common disease factors that determined BT use. The medical history of patients receiving BTs included liver disease (51.79%), diabetes (33.61%), and kidney disease (31.13%), whereas 50.41% underwent blood testing regardless of their medical history (Table 4).
Among the different treatment modalities in KM, BTs were ordered by 75.21% considering the use of HM, and 28.93% used BTs regardless of treatment. When to use and how often to follow up with BTs varied by type of medical institution (p < 0.0001). The rate of “patient’s first visit (except for prescription of HM) (45,71%),” and “before and after prescription of HM” (43.75%) were relatively high among BT users inKM hospitals and specialised KM clinic, respectively. The follow-up periods for BT were 3 to < 8 weeks (43.53%), less than 3 weeks (18.18%), and 12 weeks to < 6 months (8.82%). A total of 20.11% of patients had no specific follow-up period. More than 80% of BT users in specialised KM clinics retested BT after more than three weeks, while BT users in KM hospitals had a relatively high rate of retesting within three weeks (33.33%; Table 4). Of the 363 BT users, 11 (3.03%) experienced patient safety incidents related to BTs, including bleeding, bruising, hematoma, angioedema, pain, delayed haemostasis after blood sampling, hypotension, and dizziness after fasting (Supplementary Table S1).
Requirements for BT implementation
BT users identified the “cost of a BT” (65.56%), “lack of legal and institutional safeguards” (57.02%), and “cost of a blood tester” (40.50%) as the primary difficulties in using BTs in KM institutions. Meanwhile, BT non-users most commonly cited the “cost of a blood tester” (61.46%) as a reason for not using BT. Moreover, synthesising the responses of BT users and non-users, “burden in manpower expansion in charge of BT” (n = 274), “patients’ lack of awareness about BT in KM clinics” (n = 216), “difficulties in using referral laboratories” (n = 189), and “time charge in collecting blood and check the results” (n = 133) were identified as barriers to using BT (Fig. 1). The most popular opinion was that “BT should be covered by NHI” to promote the use of BTs in KM institutions. “Education on the interpretation of the BT results” was valued more by BT non-users (41.54%), while “improving awareness of the legitimacy of BTs by KMDs” was valued by BT users (43.53%; Fig. 2). Most BT non-users (n = 453, 97.0%) hoped to use BTs in their future care, with demands for BT coverage by NHI (89.85%) and cost support for BTs (57.62%; Fig. 3).
A total of 419 (50.48%) KMDs were aware of the campaign to use BT in KM clinics; 118 (14.22%) individuals have participated in the campaign. Overall, 98.31% of campaign participants reported that the campaign was important, and 73.73% were satisfied with it.
Discussion
This is a reflective summary of the prevalence and characteristics of BT use in KM practice. Although less than half of respondents use BTs, 95.9% responded that BTs are necessary for their KM practice. KMDs currently order BTs to assess their patients’ basic health condition, typically before prescribing HM, with 3–8 weeks follow-up. This suggests that BTs are now practically used in KM institutions to check the basic condition of patients and understand their progress after KM treatment, including HM.
Most BT users order LFTs and KFTs before or after prescribing HM in KM clinics. The findings suggest that BTs in KM clinics are primarily ordered to monitor HILI rather than for general screening purposes18. Interestingly, KM clinics have a markedly higher rate of LFT use than CBC testing; 70.12% of BT users in KM clinics used BTs to monitor HILI after prescribing HM. KMDs’ awareness of HILI was also presented in the survey responses, with more than 50% of BT users ordering these tests regardless of the patient’s chief complaint and medical history and over 75% deciding to test considering the use of HM. The survey comment regarding the use of BTs to “prevent misinterpretation of pre-existing conditions as being caused by HM” is reflective of a long history of HM being criticised for causing HILI by competing positions19 and rebuttal by KMDs20,21,22,23. Adverse hepatotoxic events associated with HM have been reported in South Korea, but they are mostly resulted from the non-professional use of dietary supplements and folk remedies rather than from HM under the direction of qualified KMDs21. Meanwhile, a nationwide multicentre, prospective study including 1,001 patients showed that the incidence of HILI was 0.60% based on the Roussel Uclaf Causality Assessment Method scale, including BTs24. Although several reviews25,26,27 and prospective studies28,29 have shown that the incidence of HILI is not high, many KMDs still use BTs to ensure the safety of HM and provide an objective demonstration to their safety to patients18. In South Korea, while manufactured herbal medicinal products’ adverse events are monitored by the regional pharmacovigilance center, there is currently no nationwide pharmacovigilance system for personalized herbal prescriptions by KMDs. Recently, efforts have been made to develop a specialized adverse event reporting form, which includes BT results, to reflect the unique characteristics of individualized herbal formulas prescribed by KMDs30. KMDs, like all medical professionals, are responsible for monitoring and managing adverse events from their herbal prescriptions. However, when medical disputes occur due to adverse events, they are mediated and arbitrated by the Korea Medical Dispute Mediation and Arbitration Agency, where medical professional negligence and causality are thoroughly evaluated31.
In order to conduct BTs in KM clinics, blood testers and consumable supplies for each BT are needed. The cost of BTs, currently borne entirely by the user, is a barrier to their use. Nevertheless, over 87% of BT users in KM clinics chose not to refer BT orders to MDs, due to the restriction on employing MDs at these clinics32 and the hassle for patients to attend other medical institutions for BTs33. Considering that the number of BTs ordered within one month was most often 1–10 times, it is clear that the utilization34 of BT in KM clinics is limited due to the aforementioned challenges9,10. Meanwhile, BTs were implemented in most university hospitals where clinical faculty, interns, and residents work. Indeed, 98.1% of responders in KM hospitals referred BTs to MDs based on established conditions of cooperation with MDs. In South Korea, since 2010, KM hospitals have been allowed to hire MDs to establish and operate additional medical specialities for collaboration32,35; by 2021, 492 MDs were working in 472 KM hospitals nationwide36. Therefore, BTs are used more actively in KM hospitals as routine testing upon admission, as they can be referred to MDs for insurance claims.
In South Korea, MDs and KMDs operate under separate licensing systems. While MDs can order BTs under NHI coverage, KMDs’ authority to order BTs remains controversial. The limited implementation of BTs in KM practice appears to be influenced by unclear policy guidelines regarding KMDs’ authority to use BTs. Survey results demonstrated that one barrier is possible legal violations. On the one hand, in 2014, The Ministry of Health and Welfare in South Korea presented an authoritative interpretation that KMDs could use BTs11. On the other hand, in 2020, the court ruled that the order to perform a BT and urine test by KMDs was a medical practice outside the scope of the license (Gwangju District Court 2020No141, Decided Apr. 29, 2021). The certainty of the authority to utilize medical devices for BT is not assured in these conflicting statements. In contrast, healthcare systems in most East Asian countries allow doctors who use HM to order BTs. TCM doctors have no restrictions regarding accessing diagnostic tools originating from conventional medicine37. Despite Taiwan’s dualised medical system, post-graduation training entitles TM doctors to various diagnostic tools of MDs38. With a unified healthcare system in Japan, MDs may prescribe Kampo medicine based on BT results39,40. Thus, based on current East Asian practices, it is considered outdated to regulate BT in KM practice. A policy to guarantee BT use in KM practice should be urgently considered. If BT is covered by the NHI in the future, as requested by most KMDs, the use of BTs may expand significantly, thus ensuring patient safety.
This survey showed that the usage rate of capillary blood was similar to that of intravenous sampling in KM institutions, while venipuncture for BT sampling is dominant procedure in primary healthcare settings41. Only 3.03% of BT users experienced patient safety incidents, such as bleeding, bruising, and pain, which are common side effects of invasive venipuncture and do not constitute serious adverse events. The South Korean Supreme Court decided new criteria for the use of diagnostic medical devices by KMDs in 2022, including whether the use of a medical device by a KMD as an aid to diagnosis is likely to result in health and hygiene hazards beyond normal practices42. Our results suggest that the use of BTs in KM institutions does not pose a health and hygiene risk beyond the usual level.
The KM education curriculum also supports the legitimacy of the use of diagnostic medical devices by KMDs42. Currently, KM undergraduate students learn to interpret BT results in diagnostic laboratory medicine courses43 and practice venipuncture techniques44 in the undergraduate curriculum. The survey results showed that it is necessary to expand education on interpreting the results and distribute a newly developed manual on using BTs in KM practice. BT non-users stated that they require further education on BT methods and interpretation of BT results, indicating that KM treatments based on BT should be provided through the manual.
There are currently no statistics on the extent to which BTs are used in KM institutions across South Korea; however, this study provides an estimate. However, this study has certain limitations. The survey was distributed online, which introduces the possibility of selection bias and may have resulted in biased responses. Additionally, formal face validity testing and reliability analysis of the survey items were not conducted, which could affect the robustness of our findings. Nevertheless, this study is significant as it is the first nationwide survey to specifically examine the use of BTs in national KM practice. Hence, this study makes an important contribution to the literature by providing detailed insights into the patterns and characteristics of BT utilization in KM clinical practice.
Conclusions
BTs are currently used by KMDs to assess the basic health status of patients and objectively monitor the progress of KM treatment. Current practice patterns regarding BT use may inform the development of standardized guidelines for BT utilization in KM practice. In addition, stakeholders must recognise the importance of BTs in real world KM practice to monitor patients’ condition or reaction to HM. To further investigate the detailed use of BTs and interpretation of the associated results in KM practice, future qualitative studies are needed to examine the experiences of KMDs who use BTs, as well as the satisfaction and needs of patients who receive KM care, including BTs in KM institutions.
Data availability
Data is provided within the manuscript or supplementary information files.
References
Liu, F. et al. Herbal medicines for asthmatic inflammation: from basic researches to clinical applications. Mediators Inflamm. 2016, 6943135. https://doi.org/10.1155/2016/6943135 (2016).
Ang, L., Song, E., Lee, H. W. & Lee, M. S. Herbal medicine for the treatment of coronavirus disease 2019 (COVID-19): A systematic review and meta-analysis of randomized controlled trials. J. Clin. Med. 9, 1583. https://doi.org/10.3390/jcm9051583 (2020).
Lee, H. Y., Hwang, S. I., Park, J. K. & Yoon, Y. J. A review of randomized controlled trials of herbal medicine treatment for hyperthyroidism. J. Korean Obstet. Gynecol. 34, 114–136. https://doi.org/10.15204/jkobgy.2021.34.3.114 (2021).
Lu, Z., Zhong, Y., Liu, W., Xiang, L. & Deng, Y. The efficacy and mechanism of Chinese herbal medicine on diabetic kidney disease. J. Diabetes Res. 2019, 2697672. https://doi.org/10.1155/2019/2697672 (2019).
Zhang, P., Ye, Y., Yang, X. & Jiao, Y. Systematic review on Chinese herbal medicine induced liver injury. Evid. Based Complement. Alternat Med. 2016, 3560812. https://doi.org/10.1155/2016/3560812 (2016).
Bae, S., Park, S., Kang, C. & Hong, S.-H. Safety of Korean herbal medicine used with Western medicin on liver function: prospective observational study. Korean J. Orient. Int. Med. 34, 192–203 (2013).
Byeon, J. H., Kil, J. H., Ahn, Y. C. & Son, C. G. Systematic review of published data on herb induced liver injury. J. Ethnopharmacol. 233, 190–196 (2019).
Nebeker, J. R., Barach, P. & Samore, M. H. Clarifying adverse drug events: a clinician’s guide to terminology, documentation, and reporting. Ann. Intern. Med. 140, 795–801. https://doi.org/10.7326/0003-4819-140-10-200405180-00009 (2004).
Park, K. Problems with the use of modern medical devices by Korean medicine doctors. Med. Policy Forum. 12, 159–163 (2014).
Kim, S. Public safety is the highest value: Korean medicine doctors’ use of modern medical devices and telemedicine. Med. Policy Forum. 14, 14–18 (2016).
Park, J., Oh, K., Kwon, S., Chu, H. & Kim, J. A study on the precedents changing related to using medical devices of Korean medicine doctors. J. Int. Korean Med. 42, 1303–1318. https://doi.org/10.22246/jikm.2021.42.6.1303 (2021).
Korea Institute of Oriental Medicine Korean Medicine Policy Research Center. A study on ways to improve social norms regarding the use of modern medical devices by Korean Medicine doctors. (2020).
Rea, L. M. & Parker, R. A. Designing and Conducting Survey Research: A Comprehensive Guide 4th edn (Jossey-Bass, 1992).
van Bokhoven, M. A. et al. Why do patients want to have their blood tested? A qualitative study of patient expectations in general practice. BMC Fam Pract. 7 https://doi.org/10.1186/1471-2296-7-75 (2006).
Sung, S. H. et al. The utilization of medical devices by traditional Korean medicine doctors investigated through traditional Korean medicine clinical studies. Evid. Based Complement. Alternat. Med. 2018, 3987019. https://doi.org/10.1155/2018/3987019 (2018).
Ayre, C. & Scally, A. J. Critical values for Lawshe’s content validity ratio: revisiting the original methods of calculation. Meas. Evaluation Couns. Dev. 47, 79–86. https://doi.org/10.1177/0748175613513808 (2014).
Sharma, A. et al. A consensus-based checklist for reporting of survey studies (CROSS). J. Gen. Intern. Med. 36, 3179–3187. https://doi.org/10.1007/s11606-021-06737-1 (2021).
Yang, Y. et al. A review of herb-induced liver injury in Mainland China. Front. Pharmacol. 13, 813073. https://doi.org/10.3389/fphar.2022.813073 (2022).
Young doctor newspaper. Herbal medicine, ‘Causes of hepatotoxic injury’… Is herbal medicine safe? A serious lie, (2015).
Jang, I. A review of the report about drug-induced hepatitis published by the National Institute of toxicological research. J. Korean Orient. Med. 25, 78–89 (2004).
Park, H., Jang, I. & Lee, S. Hepatotoxic events associated with herbal medicinal products, folk remedies and food supplements in Korea. J. Korean Orient. Med. 26, 152–165 (2005).
Cheon, J. H., Min, S. Y. & Kim, J. H. A clinical study on the modified RUCAM application to liver injury induced by herbal medicine. J. Korean Orient. Pediatr. 22, 83–94 (2008).
Lee, J. et al. Battle over herb-induced liver injury: low prevalence confirmed through secondary evaluation and research team’s clarifying rebuttal to unwarranted public claims. J. Altern. Complement. Med. 25, 260–264. https://doi.org/10.1089/acm.2018.0253 (2019).
Cho, J. H. et al. A nationwide study of the incidence rate of herb-induced liver injury in Korea. Arch. Toxicol. 91, 4009–4015. https://doi.org/10.1007/s00204-017-2007-9 (2017).
Yun, Y. et al. Korean herbal medicine on liver function: A systematic review in Korean literature. Korean J. Orient. Int. Med. 30, 153–172 (2009).
Lee, J., Son, C., Lee, J. A., Choi, J. & Lee, M. S. Do herbal medicines negatively affect liver tests? A systematic review of Korean clinical studies on safety. Eur. J. Integr. Med. 6, 441–450. https://doi.org/10.1016/j.eujim.2014.06.006 (2014).
Oh, S. J., Cho, J. H. & Son, C. G. Systematic review of the incidence of herbal drug-induced liver injury in Korea. J. Ethnopharmacol. 159, 253–256. https://doi.org/10.1016/j.jep.2014.11.027 (2015).
Jeong, T. Y. et al. A prospective study on the safety of herbal medicines, used alone or with conventional medicines. J. Ethnopharmacol. 143, 884–888. https://doi.org/10.1016/j.jep.2012.08.016 (2012).
Yun, Y. J. et al. Safety of prescribed Korean herbal medicine on liver function: prospective multi-center pilot study. Korean J. Orient. Physiol. Pathol. 23, 715–722 (2009).
Cho, E. et al. Development of an adverse event reporting form for herbal medicine: A Delphi expert consensus study. Pharmacoepidemiol. Drug Saf. 34, e70116. https://doi.org/10.1002/pds.70116 (2025).
Hwang, H. W., Lee, J. S. & Kim, K. H. Claimed adverse events of Korean medicine in South Korea: analysis of cases in the Korea medical dispute mediation and arbitration agency databases. Korean J. Acupunct. 34, 126–135 (2017).
Lee, E. J. et al. Attitude and recognition of medical doctors who employed by university hospital on traditional Korean medicine. Kor J. Ori Med. Physiol. Pathol. 26, 773–777 (2012).
Kim, J. et al. Should Korean medicine doctors use modern diagnostic medical devices? Survey result of public perspectives. J. Korean Med. 43, 94–105. https://doi.org/10.13048/jkm.22033 (2022).
Cho, E., Kim, S. & Son, M. J. Common adverse events of herbal formulas for developing reporting forms for clinical practice and research: an overview of systematic reviews. Integr. Med. Res. 14, 101118. https://doi.org/10.1016/j.imr.2024.101118 (2025).
Korean Law Information Center. Medical Law, Article 43, https://law.go.kr/LSW/lsSc.do?section=&menuId=1&subMenuId=15&tabMenuId=81&eventGubun=060101&query=%EC%9D%98%EB%A3%8C%EB%B2%95#undefined (2023).
37 National Health Insurance Service & Service, H. I. R. A. Status of healthcare institution, (2022).
Wang, F. A comparative study on qualification system of Korean medicine doctors and traditional Chinese medicine doctors. HUFS Law Rev. 45, 455–491 (2021).
Kim, D. S., Choi, B. H., Lee, H. J., Kwon, S. H. & Kwon, Y. K. Study on dual medical system of traditional Chinese medicine and Western medicine in Taiwan. Kor J. Ori Med. Physiol. Pathol. 28, 9–15 (2014).
Park, Y. L. et al. Comparative study on the education system of traditional medicine in China, Japan, Korea, and Taiwan. Explore (NY). 12, 375–383. https://doi.org/10.1016/j.explore.2016.06.004 (2016).
Hijikata, Y. & Ikemoto, Y. Kampo medicines improved blood test and QOL in two vasculitis cases of Churg–Strauss syndrome and Henoch–Shönlein purpura after inadequate treatment with conventional therapies. Int. J. Gen. Med. 3, 93–99. https://doi.org/10.2147/ijgm.s8018 (2010).
Cornes, M., Ibarz, M., Ivanov, H. & Grankvist, K. Blood sampling guidelines with focus on patient safety and identification - a review. Diagnosis (Berl). 6, 33–37. https://doi.org/10.1515/dx-2018-0042 (2019).
Supreme court of Korea. A doctor of Korean Medicine was charged with practicing medicine without a license for using an ultrasound diagnostic device to make a Korean medicine diagnosis., https://www.scourt.go.kr/supreme/news/NewsViewAction2.work?pageIndex=1&searchWord=&searchOption=&seqnum=8967&gubun=4&type=5 (2022).
Kang, Y. S. et al. A study for improvement of the National examination of Doctors of Korean medicine. 39, 49–53 (2017).
Sim, S. B., Kweon, J. H., Kim, H. W., Hong, J. W. & Shin, S. W. Student satisfaction study of clinical skills training in Korean medical education. J. Korean Med. 34, 37–53. https://doi.org/10.13048/jkm.13011 (2013).
Acknowledgements
We thank all the Korean Medicine doctors who participated in the survey and shared their clinical experiences and perspectives.
Funding
This work is supported by the Korea Institute of Oriental Medicine (grant no. KSN2122211). The funding source had no input regarding the interpretation or publication of the study’s results.
Author information
Authors and Affiliations
Contributions
EC designed and investigated the survey and drafted the manuscript in collaboration with SK. MMK performed the data analyses. CSY administered the project. SK conceptualised the study and provided supervision. All authors revised the manuscript and approved the final.
Corresponding author
Ethics declarations
Ethics approval
This study was approved by the institutional review board of the Korea Institute of Oriental Medicine (I-2212/012 − 001). We obtained informed consent to participate in this study from all participants.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Cho, E., Ko, M.M., Yang, C. et al. Blood test use in Korean Medicine for monitoring herbal medicine safety. Sci Rep 15, 13692 (2025). https://doi.org/10.1038/s41598-025-98501-2
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-98501-2