Abstract
Atopic dermatitis (AD) is the most common chronic inflammatory skin disease. Massive cohort studies revealed that AD was associated with allergic diseases, inflammatory diseases, autoimmune diseases, cardiovascular diseases, and mental disorders. We comprehensively and systematically analyzed the correlation between AD and diseases to identify AD-associated diseases (ADADs). We involved 17,924 individuals from the National Health and Nutrition Examination Survey (NHANES) (2013–2018) dataset, and analyzed the correlation between AD and 422 diseases classified by International Classification of Diseases-10 (ICD-10) using four logistic regression models. We found that AD is significantly associated with 33 diseases: (1) allergic diseases, including urticaria, allergic rhinitis, allergy, asthma, other seasonal allergic rhinitis; (2) inflammatory diseases, including noninfective gastroenteritis and colitis, acute atopic conjunctivitis, osteoarthritis, and unspecified chronic bronchitis; (3) mental disorders with impairment (MDI), including comorbid mental disorders, schizophrenia and sleep disorder; (4) malignant tumors, including malignant neoplasm of prostate, malignant (primary) neoplasm and malignant neoplasm of breast; (5) other symptoms and diseases, other symptoms and diseases, such as wheezing, pruritus and gout. Notably, non-infective gastroenteritis and colitis showed the strongest correlation (OR: 38.39, 95% CI: 3.08-478.01) among the 33 ADADs. We identified 33 ADADs based on the NHANES (2013–2018) dataset, which provide new insights into understanding the development of these ADADs associated with AD.
Similar content being viewed by others
Introduction
Atopic dermatitis (AD) is one of the most common chronic relapsing inflammatory skin diseases, characterized by persistent itching of the skin1. Within the past decades, the incidence of AD increased steadily in both urbanized and developing countries2,3. Currently, AD impact 15–20% of children and up to 10% adults worldwide, causing significant economic burden and reduced life quality to patients and their family4,5,6. It is noteworthy that AD primarily affects pediatric demographic and leading to life-long recurrent course, wherein approximately 24% of children suffer from AD, and the prevalence rate increases from 15 to 38% between children aged 1 and children aged 4–57. Many adults suffering AD experienced childhood onset of the disease, and this long-term persistent itching of skin can interfere their occupations, sleeping quality and even intimate relationships, causing life-long burdens both physically and mentally7,8.
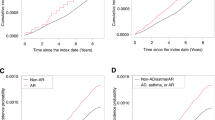
More importantly, growing evidence suggested robust correlations between AD and various allergic diseases, such as allergic asthma (AA), allergic rhinitis (AR), and food allergy (FA)4,9,10. The progressing onset of allergic diseases follow a time-based-order, as AD and FA in infancy can evolve into AS and AR in childhood, this evolution from skin to gastrointestinal and respiratory tract was defined as “atopic march”11,12. Elevated comorbidities were also noticed between AD and autoimmune diseases, cardiovascular diseases (CVD), MDI and other disorders: recent meta-analysis showed increased possibility of comorbidities between AD and multiple autoimmune diseases, including rheumatoid arthritis (RA) and systemic lupus erythematosus (SLE)13,14,15. Increased risk of CVD including ischemic stroke, hypertension and myocardial infarction (MI) were observed in AD patients16,17,18,19. Patients suffering mental disorders, particularly depression, anxiety, sleep disorders and suicidal ideation also show higher prevalence of AD than normal20.
To identify the risk of AD and conduct interventions to improve health-related outcomes, we proposed that the patients suffered from AD and a certain disease that is demonstrated to be associated with AD should be diagnosed as AD associated disease (ADAD). Herein, we comprehensively and systematically analysis the correlation between AD and 422 diseases using the National Health and Nutrition Examination Survey (NHANES) (2013–2018) dataset to provide a useful guideline for clinics to diagnose ADADs.
Methods
Study population
We utilized the data extracted from the National Health and Nutrition Examination Survey dataset of the United States (NHANES)21. 12,226 individuals were excluded from the study due to missing or incomplete data on body mass index (BMI), education level, AD records, and uncertain or incomplete information. Additionally, 24 individuals who lacked ICD-10 diagnosis information were also rule out in this study. A total of 17,924 subjects remained for the final analysis. The entire study was performed according to the guidelines approved by the Research Ethics Review Board of the National Center for Health Statistics (Protocol #2011-17, #2018-01). Moreover, written informed consent was duly obtained from all participants involved in this project spanning 2013 to 2018.
Population characteristics
The sample population age, BMI, sex, race and education were examined. Race characteristics include Mexican American, Non-Hispanic Black, Non-Hispanic White and others. Education characteristics include college graduate or above, college or above, high school or equivalent and less than high school (Table 1).
Clinical markers measurement
In the NHANES MEC, samples of whole blood undergo meticulous analysis. The NHANES Laboratory Procedures Manual (LPM) thoroughly expounds on the collection and processing of specimens. As a fundamental gauge of inflammation, we utilized the platelet count (PLT), neutrophil count (NEU), monocyte count (MO), and lymphocyte count (LYM). To gain a more comprehensive understanding of the correlation between inflammation-related indices and sex hormones, we derived the neutrophil-to-lymphocyte ratio (NLR), monocyte-to-lymphocyte ratio (MLR), systemic immune-inflammation index (SII), and systemic immune response index (SIRI). The measurements of PLT, NEU, and LYM were taken at a concentration of 1000 cells/uL. SIRI was computed by (NEU × Mo) / LYM. SII was determined by dividing NEU by LYM. MLR was obtained by the ratio of MO to LYM. The detection limits remained consistent for all analytes in the dataset, and none of the results fell below the limits of detection.
The Collaborative Laboratory Services (Ottumwa, IA) used a Beckman Synchron LX20 analyzer to measure biochemistry profile, including levels of ALT, AST, ALP and GGT. For NHANES cycles prior to 2015, serum CRP levels were determined by latex-enhanced nephelometry on a Behring Nephelometer, with a lower limit of detection (LLOD) of 0.2 mg/L. For NHANES cycles 2015 and 2017, CRP levels were assayed on Beckman Coulter Synchron analyzers, with LLODs of 0.11 mg/L (for 2015) and 0.15 mg/L (for 2017).
Soluble klotho levels (pg/ml) were analyzed with a commercially available ELISA kit produced by IBL International, Japan during the period 2019–2020. All analyses were performed at the University of Washington research laboratories. A description of the laboratory methodology can be found at https://wwwn.cdc.gov/Nchs/Nhanes/.
Model categories
The association between AD and each disease was assessed through four multivariable logistic regression models: one unadjusted and three adjusted models. Model 1 did not include any covariate adjustments. Model 2 was adjusted for core demographic covariates (sex, age, race). Model 3 was expanded upon Model 2 by incorporating additional socioeconomic covariates (education level and household income). Finally, Model 4 comprehensively adjusted for demographic variables, lifestyle factors and comorbidities. The model construction was informed by established methodologies from prior epidemiological studies, specifically adopting a sequential adjustment approach to progressively account for potential confounding effects22,23.
Statistical analyses
We have performed all statistical analysis with the R software (Version 4.2.2) according to the CDC guidelines (https://wwwn.cdc.gov/nchs/nhanes/tutorials). Sample weights were taken into account in all of the estimates to produce representative data of the civilian noninstitutionalized US population. Population characteristics of the sample were analyzed using parametric and nonparametric methods according to variable types and distribution assumptions. For continuous variables with normal distribution and homogeneity of variance across groups, one-way Analysis of Variance (ANOVA) was employed to detect between-group differences. The normality assumption was verified through Shapiro-Wilk tests (p > 0.05), while Levene’s test (p > 0.10) confirmed variance homogeneity. When ANOVA revealed significant differences (p < 0.05), post-hoc pairwise comparisons were conducted with Bonferroni correction. For categorical variables, the Pearson Chi-square test was primarily applied. In cases where small sample sizes led to expected frequencies < 5, Fisher’s exact test was substituted to ensure validity.
Results
Baseline information of study participants
A total of 17,924 participants (mean age 53.90 ± 0.35, 46% males) were included in this study. A total of 47.88 ± 2.9 patients with AD (51.93% female, 48.07% male) were compared to 46.97 ± 0.29 individuals without AD (51.82% female, 48.18% male). The weighted distribution of the characteristics according to AD was shown in Table 1. A two-sided P-value < 0.05 was considered a significant association between AD and ADADs. The average age and body mass index in these two groups did not have a significant difference. Males and Non-Hispanic Whites were more likely to have a higher rate of AD.
Laboratory examination of AD patients
We conducted a study examining the disparities in clinical indexes between AD and non-AD group in Table 2. 15 clinical parameters were analyzed, the majorities of clinical-related indexes were no significantly different compared to the non-AD population, only white blood cell count (WBC), lymphocyte count (LYM) and SII are slightly elevated in the AD population. Interestingly, there were notable increases in metabolic indicators, especially Gamma-Glutamyl Transferase (GGT) (AD: 41.35 ± 4.43 compared to non-AD group: 27.72 ± 0.34, p = 0.004) and Fe (AD: 316.53 ± 83.82 compared to non-AD group: 126.10 ± 2.99, p = 0.03) are significantly enhanced in the AD population.
The association analysis of AD with 422 diseases
Within this investigation, we delved into the association between AD and various diseases. We examined a comprehensive collection of 422 prevalent illnesses categorized by the ICD-10 classification system and calculated the disparities in disease incidence between AD and non-AD group. In the model1, we identified 33 diseases that exhibited a significant positive correlation with AD (Fig. 1). In analysis, we observed that AD comorbid allergy diseases, such as urticaria (L50, OR: 49.67, 95% CI: 4.90-503.62), acute atopic conjunctivitis (H10.1, OR: 31.26, 95% CI: 4.44-219.93), rash and other nonspecific skin eruption (R21, OR: 21.47, 95% CI: 5.96–77.34), allergic rhinitis (J30.9), allergy (T78.4) and asthma(J45). Moreover, comorbid mental disorders (F99, OR:11.94, 95% CI: 1.46–97.68) were increased in prevalence in AD patients, including schizophrenia (F20) and sleep disorder (G47.9). Interestingly, we found evidence for statistically significant interaction between atopic dermatitis and inflammatory diseases, including non-infective diseases and infective diseases (K52.9). Among non-infective diseases, noninfective gastroenteritis and colitis (K52.9, OR:38.39, 95% CI: 3.08-478.01) has strongest association with AD, secondly are osteoarthritis (M19.9) and chronic bronchitis (J42). Among infective diseases include HIV disease (B20), dermatophytosis (B35.9) and local infection of the skin and subcutaneous tissue (L08.9). In addition, we found AD was associated with malignant diseases, particularly malignant neoplasm of prostate (C61, OR:38.52, 95% CI: 5.32-278.74). Interestingly, some metabolic diseases, such as gout (M10.9, OR:12.11, 95% CI: 2.08–70.65), overweight and obesity (E66, OR:9, 95% CI: 1.10-73.94), hyperuricemia without signs of inflammatory arthritis and prevent high cholesterol (E79) and renal disease, such as dependence on renal dialysis (Z99.2) and other specified urinary incontinence (N39.4) are significantly associated with atopic dermatitis. What’s more, AD is also associated with other diseases, including other chest pain (R07.89), wheezing (R06.2), disorder of ear (H93.9), abnormal sputum (R09.3), nasal congestion (R09.81) and enlarged prostate (N40).
Discussion
Genetic predisposition, epidermal dysfunction, skin microbiome abnormalities and immune dysregulation jointly contribute to the development of AD. Th2 inflammation mediates the most typical symptom of AD, atopic pruritus, and causing consistent itching to the patients24. Epidermis destructing factors such as skin damage, infections and inflammation can activate keratinocytes and exaggerate production of proinflammatory factors, such as thymic stromal lymphopoietin (TSLP), IL-25 and IL-33, adding to recruitment of immune cells especially Th2 cells. Th2 cells, eosinophils, neutrophils and mast cells therefore release pro-inflammatory cytokines and peptides to stimulate pruritoceptive pathways, in which IL-31 expressed by Th2 cells acts as the most significant pruritus mediator. IL-31 can bind to IL-31 A receptor and activate transient receptor potential vanilloid 1 (TRPV1) and transient receptor potential ankyrin 1 (TRPA1) to awake sensory neurons and exacerbate pruritus. Excessive production of Th2 lymphocytes lead to elevation in IL-4, IL-5 and IL-13 levels to recruit and activate immune cells and trigger B cells to generate allergen-specific IgE, adding to defections in epidermal barrier and stimulate type 2 inflammatory responses25.
Immunological aberrations are believed to be significant in triggering disruptions of the epidermal barrier, microbial dysbiosis and disorders of immune responses in AD. Our analysis indicated that innate and adaptive immune system were activated in AD patients. We observed infiltration of inflammatory cells and noticed that GGT, an enzyme in antioxidant system (AOS), was significantly increased in AD. Oxidative stress (OS) causes direct damage to the cell membrane and DNA to establish skin barrier defection, as well as activating NF-κB pathway to stimulate IL-6, IL-8, IL-9 and IL-33 releasing26,27. These factors jointly contribute to dermal inflammation, elevated histamine releasing and itching, which in turn determine a vicious cycle that exaggerate OS and add to epidermal barrier disruption. Considering the fact GGT level was notably increased in AD patients, it may act as a potential clinical diagnosis and prognostic indicators for OS in AD.
In our analysis, no differences among the clinical characteristics of age, sex and race were reflected on the morbidity of AD. In association analysis, we found that AD individuals show positive correlations among a series of allergy diseases, including urticaria, allergic rhinitis, allergy, asthma and other seasonal allergic rhinitis. These findings show consistence with previous researches that the early onset of AD increases co-occurrence of other allergic diseases and establish the pathogenesis of atopic march28,29.
AD also show correlations with various inflammatory diseases, including noninfective gastroenteritis and colitis, acute atopic conjunctivitis, osteoarthritis, and unspecified chronic bronchitis, in which noninfective gastroenteritis and colitis show the most robust correlation in our analysis. The possible mechanisms of AD increasing comorbidity of these diseases are complex. First, one possible pathway is the inflammatory pathway: The imbalance of Th2 to Th1 cytokines, such as IL-4, IL-5, IL-9 and IL-13, observed in AD can create alterations in the cell mediated immune responses30. These inflammatory cytokines circulate to the different tissues through related anatomical pathways and triggering inflammation. Of note, inflammatory bowel disease (IBD) is caused by an abnormal adaptive immune response. In particular, ulcerative colitis (UC) has been rather related to a non-conventional Th2 response31. Therefore, Th2 inflammatory cytokines created by AD enters into bowels and contribute to a vicious inflammatory cycle, finally exacerbating colitis. The potential mechanisms of AD increasing atopic conjunctivitis and osteoarthritis maybe consistent with this. Second, some studies proposed the hypothesis of the interplay of intestinal dysbacteria in AD patients. Li et al. has reported that differential abundance of genera in the skin, oral and gut32. Accordingly, we speculate that abnormal oral microbiota through oral-gut axis or intestinal dysbacteria probably impact the risk of colitis.
Additionally, our analysis also emphasized correlation between AD and MDI, including comorbid mental disorders, schizophrenia and sleep disorder. Corresponding to our findings, previous studies showed that elevated prevalence of MDI and relatively severe phenotype were noticed in children suffering AD, including mental health disturbances including anxiety, depression, ADHD, conduct disorder, and autism33,34. Although the underlying mechanisms between AD and MDI remain unclear, correlation between diseases severity, eczema area and wake experiences after sleep onset were notice in AD children, highlighting lower sleep efficiency and sleep disorder. Sleep disturbance along with consistent itching may add to daily anxiety and depression and drive the association between neuropsychiatric disorders and AD34. Therefore, the concept of ADAD may offer therapeutic guidance to take AD into consideration when faced with mental disorders of unknown origins, especially in children with allergic history.
Previous research reached contrary results about the correlations between AD and multiple cancers due to substantial heterogeneity and severe bias between studies35,36. However, our analysis found correlation between AD and malignant tumor, including malignant neoplasm of prostate, malignant (primary) neoplasm and malignant neoplasm of breast. Wherein the effect of AD in the pathogenesis of malignant tumor are likely multifactorial. Other than genetic predispositions and systemic inflammation, another pathway could be psychosocial disease20. Besides, our result also found correlations between AD and other diseases, including dermatophytosis, dependence on renal dialysis, other chest pain, wheezing, rash and other nonspecific skin eruption, pruritus, gout, nasal congestion, hyperuricemia without signs of inflammatory arthritis and tophaceous disease, unspecified disorder of ear, abnormal sputum, prevent high cholesterol, overweight and obesity, local infection of the skin and subcutaneous tissue, enlarged prostate, other specified urinary incontinence, and other acute postprocedural pain, emphasizing the overall affection of AD. Previous studies have proved that allergic diseases mediated type 2 immunity induced atherosclerosis, which affects arteries of different organs such as the heart and the kidney37,38, which the underlying cause of metabolic diseases and renal disease.
Of note, we should diagnose the patient suffered from AD and a certain disease that is demonstrated to be associated with AD as AD associated disease (ADAD). Compared with previous studies, our report first explored the association between AD and related diseases via analyzing the NHANES database and successfully revealed a cluster of 33 diseases positively correlating to AD. However, limitations still exist as our research examined no obvious correlation among the prevalence of cardiovascular disease, autoimmune disease and AD due to insufficiency in sample size. Besides, as a cross-sectional studies, our findings may have uncovered correlations but could not disentangle noncausal or causal associations, thus there might still be bidirectional correlations between AD and other diseases. Recommendations should be made with caution when guiding clinical practice.
Limitations
This study has several important limitations that should be considered when interpreting the results. First, the diagnosis of atopic dermatitis (AD) in the National Health and Nutrition Examination Survey (NHANES) dataset is based on self-reported data and clinical assessments by general practitioners, rather than specialists such as dermatologists or allergists. As a result, the accuracy of the AD diagnosis may be limited, and misclassification could have influenced the findings. While this limitation is inherent in the use of large-scale, population-based datasets like NHANES, future studies that include more detailed clinical evaluations by specialists would help to improve the diagnostic accuracy and reduce the risk of misclassification bias.
Second, the control group in this study is not a true “normal” control group, but rather a heterogeneous group of participants who may have various other diseases or treatments. Therefore, the comparison of AD patients with this group should be interpreted with caution, as it includes individuals who may have received treatment for other conditions. The use of participants receiving treatment for different diseases may contribute to the observed associations between AD and comorbidities, as these treatments (e.g., immunosuppressive therapies like cyclosporine, azathioprine, and methotrexate) could independently influence the risk of developing certain conditions. This raises the possibility that some of the comorbidities identified in this study may reflect the effects of AD treatments rather than the disease pathology itself. To address this, further research is needed to separate the impact of AD from the potential confounding effects of treatment-related factors.
Lastly, while the study identifies a cluster of diseases associated with AD, it is difficult to definitively establish the directionality or causal relationships between AD and these comorbidities due to the cross-sectional nature of the NHANES dataset. Longitudinal studies with more detailed clinical and treatment information would provide a more comprehensive understanding of how AD and its treatments interact with other diseases over time.
Conclusion
Our data revealed a cluster of 33 diseases positively correlating to AD and proposed the concept of AD-associated disease (ADAD). Given the influence of AD, the concept of ADADs may add to early prediction, diagnosis and treatment of AD among ADADs, providing clinical guidance in comorbidities analysis and advanced treatment. Further replication in larger samples is needed to validate our findings, and experimental studies are needed to explore the underlying mechanisms.
Data availability
The survey data are publicly available on the NHANES website for all researchers worldwide (www.cdc.gov/nchs/nhanes/).
Abbreviations
- AD:
-
atopic dermatitis
- ADAD:
-
AD-associated disease
- NHANES:
-
national health and nutrition examination survey
- BMI:
-
body mass index
- ICD-10:
-
international classification of diseases-10
- MDI:
-
mental disorders with impairment
- HIV:
-
human immunodeficiency virus
- OR:
-
odds ratio
- AA:
-
allergic asthma
- AR:
-
allergic rhinitis
- FA:
-
food allergy
- CVD:
-
cardiovascular diseases
- RA:
-
rheumatoid arthritis
- SLE:
-
systemic lupus erythematosus
- LPM:
-
laboratory procedures manual
- PLT:
-
platelet count
- NEU:
-
neutrophil count
- MO:
-
monocyte count
- LYM:
-
lymphocyte count
- NLR:
-
neutrophil-to-lymphocyte ratio
- MLR:
-
monocyte-to-lymphocyte ratio
- SII:
-
systemic immune-inflammation index
- SIRI:
-
systemic immune response index
- LLOD:
-
lower limit of detection
- WBC:
-
white blood cell count
- LYM:
-
lymphocyte count
- GGT:
-
gamma-Glutamyl Transferase
- TSLP:
-
thymic stromal lymphopoietin
- TRPV1:
-
transient receptor potential vanilloid 1
- TRPA1:
-
transient receptor potential ankyrin 1
- IBD:
-
inflammatory bowel disease
- UC:
-
ulcerative colitis
References
David Boothe, W., Tarbox, J. A. & Tarbox, M. B. Atopic dermatitis: pathophysiology. Adv. Exp. Med. Biol. 1027, 21–37 (2017).
Bylund, S., Kobyletzki, L. B., Svalstedt, M. & Svensson, A. Prevalence and incidence of atopic dermatitis: A systematic review. Acta Derm Venereol. Jun. 9 (12), adv00160 (2020).
Kim, J., Kim, B. E. & Leung, D. Y. M. Pathophysiology of atopic dermatitis: Clinical implications. Allergy Asthma Proc. Mar 1. ;40(2):84–92. (2019).
Nutten, S. Atopic dermatitis: global epidemiology and risk factors. Ann. Nutr. Metab. 66 (Suppl 1), 8–16 (2015).
Silverberg, J. I. et al. Patient burden and quality of life in atopic dermatitis in US adults: A population-based cross-sectional study. Ann. Allergy Asthma Immunol. Sep. 121 (3), 340–347 (2018).
Schuler, C. F., Billi, A. C., Maverakis, E., Tsoi, L. C. & Gudjonsson, J. E. Novel insights into atopic dermatitis. J. Allergy Clin. Immun. May. 151 (5), 1145–1154 (2023).
Abuabara, K. et al. Clinical onset of atopic eczema: results from 2 nationally representative British birth cohorts followed through midlife. J. Allergy Clin. Immun. Sep. 144 (3), 710–719 (2019).
Ring, J. et al. Atopic eczema: burden of disease and individual suffering - results from a large EU study in adults. J. Eur. Acad. Dermatol. Venereol. Jul. 33 (7), 1331–1340 (2019).
Martinez, A., de la Rosa, R., Mujahid, M. & Thakur, N. Structural racism and its pathways to asthma and atopic dermatitis. J. Allergy Clin. Immunol. Nov. 148 (5), 1112–1120 (2021).
Sugita, K. & Akdis, C. A. Recent developments and advances in atopic dermatitis and food allergy. Allergol. Int. Apr. 69 (2), 204–214 (2020).
Tsuge, M., Ikeda, M., Matsumoto, N., Yorifuji, T. & Tsukahara, H. Current insights into atopic March. Children-Basel Nov ;8(11). (2021).
Yang, L., Fu, J. & Zhou, Y. Research progress in atopic March. Front. Immunol. 11, 1907 (2020).
Floca, E. et al. A new autoimmune disease: atopic dermatitis in children. Allergol. Immunopathol. (Madr). 50 (6), 17–21 (2022).
Williams, R. C. et al. The uni-directional association of atopic dermatitis and rheumatoid arthritis: a systematic review and meta-analysis. Arch. Dermatol. Res. Apr 12 (2023).
Ponvilawan, B., Charoenngam, N., Wongtrakul, W. & Ungprasert, P. Association of atopic dermatitis with an increased risk of systemic lupus erythematosus: A systematic review and meta-analysis. J. Postgrad. Med. Jul-Sep. 67 (3), 139–145 (2021).
Brunner, P. M. et al. The atopic dermatitis blood signature is characterized by increases in inflammatory and cardiovascular risk proteins. Sci. Rep. Aug. 18 (1), 8707 (2017).
Huang, J., Gui, Y., Wu, J. & Xie, Y. Investigating the association of atopic dermatitis with ischemic stroke and coronary heart disease: A Mendelian randomization study. Front. Genet. 13, 956850 (2022).
Yousaf, M. et al. Association between atopic dermatitis and hypertension: a systematic review and meta-analysis. Br. J. Dermatol. Feb. 186 (2), 227–235 (2022).
Drucker, A. M. et al. Atopic dermatitis is not independently associated with nonfatal myocardial infarction or stroke among US women. Allergy Oct. 71 (10), 1496–1500 (2016).
Kage, P., Simon, J. C. & Treudler, R. Atopic dermatitis and psychosocial comorbidities. J. Dtsch. Dermatol. Ges Feb. 18 (2), 93–102 (2020).
Sommers, T. et al. Prevalence of chronic constipation and chronic diarrhea in diabetic individuals in the united States. Am. J. Gastroenterol. Jan. 114 (1), 135–142 (2019).
Li, H. et al. Association of dietary patterns with chronic respiratory health among US adults. Front. Immunol. Dec. 6, 15 (2024).
Shen, R. H. & Zou, T. The association between cardiovascular health and depression: results from the 2007–2020 NHANES. Psychiat Res. Jan ;331. (2024).
Li, H., Zhang, Z., Zhang, H., Guo, Y. & Yao, Z. Update on the pathogenesis and therapy of atopic dermatitis. Clin. Rev. Allergy Immunol. Dec. 61 (3), 324–338 (2021).
Sroka-Tomaszewska, J. & Trzeciak, M. Molecular mechanisms of atopic dermatitis pathogenesis. Int. J. Mol. Sci. Apr 16 ;22(8). (2021).
Bertino, L. et al. Oxidative stress and atopic dermatitis. Antioxid. (Basel) Feb 26 ;9(3). (2020).
Borgia, F. et al. Oxidative stress and phototherapy in atopic dermatitis: mechanisms, role, and future perspectives. Biomolecules Dec. 19 ;12(12). (2022).
Brunner, P. M. et al. Increasing comorbidities suggest that atopic dermatitis is a systemic disorder. J. Invest. Dermatol. Jan. 137 (1), 18–25 (2017).
Paller, A. S., Spergel, J. M., Mina-Osorio, P. & Irvine, A. D. The atopic March and atopic Multimorbidity: many trajectories, many pathways. J. Allergy Clin. Immun. Jan. 143 (1), 46–55 (2019).
Dubin, C., Del Duca, E. & Guttman-Yassky, E. The IL-4, IL-13 and IL-31 pathways in atopic dermatitis. Expert Rev. Clin. Immunol. Aug. 17 (8), 835–852 (2021).
Fuss, I. J. et al. Disparate CD4 + lamina propria (LP) lymphokine secretion profiles in inflammatory bowel disease. Crohn’s disease LP cells manifest increased secretion of IFN-gamma, whereas ulcerative colitis LP cells manifest increased secretion of IL-5. J. Immunol. Aug. 1 (3), 1261–1270 (1996).
Li, W. et al. Inverse association between the skin and oral microbiota in atopic dermatitis. J. Invest. Dermatol. Aug. 139 (8), 1779–1787e1712 (2019).
Wan, J., Takeshita, J., Shin, D. B. & Gelfand, J. M. Mental health impairment among children with atopic dermatitis: A united States population-based cross-sectional study of the 2013–2017 National health interview survey. J. Am. Acad. Dermatol. Jun. 82 (6), 1368–1375 (2020).
Fishbein, A. B. et al. Sleep disturbance in children with moderate/severe atopic dermatitis: A case-control study. J. Am. Acad. Dermatol. Feb. 78 (2), 336–341 (2018).
Wang, L., Bierbrier, R., Drucker, A. M. & Chan, A. W. Noncutaneous and cutaneous Cancer risk in patients with atopic dermatitis: A systematic review and Meta-analysis. Jama Dermatol. Feb. 1 (2), 158–171 (2020).
Halling-Overgaard, A. S., Ravnborg, N., Silverberg, J. I., Egeberg, A. & Thyssen, J. P. Atopic dermatitis and cancer in solid organs: a systematic review and meta-analysis. J. Eur. Acad. Dermatol. Venereol. Feb. 33 (2), e81–e82 (2019).
Fernandez-Gallego, N. et al. The impact of type 2 immunity and allergic diseases in atherosclerosis. Allergy Nov. 77 (11), 3249–3266 (2022).
Schonmann, Y. et al. Inflammatory skin diseases and the risk of chronic kidney disease: population-based case-control and cohort analyses. Br. J. Dermatol. Oct. 185 (4), 772–780 (2021).
Acknowledgements
We would like to thank Zhang Jing (Shanghai Tongren Hospital) for his work on the NHANES database, which makes it easier for us to explore. Thanks to those who contributed to NHANES data, including all anonymous participants in the study.
Funding
This work was supported by the Significant Science and Technology Project of Beijing Life Science Academy [grant number 2024500CB0030, 2023000CA0040]; the National Natural Science Foundation of China [grant number 81603119]; the Natural Science Foundation of Beijing Municipality [grant number 7174316]; the Peking University Medicine Seed Fund for Interdisciplinary Research supported by “the Fundamental Research Funds for the Central Universities” [grant number No. BMU2022MX017, No. BMU2022MX003].
Author information
Authors and Affiliations
Contributions
X.C., Y. L. and ZY. S analyzed the data and wrote the manuscript; All authors help to revise this manuscript and approved it to publish.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
The ethics review board of the National Center for Health Statistics approved all NHANES protocols and written informed consent was obtained from all participants.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Liu, Y., Chen, X., Su, Z. et al. Identification of atopic dermatitis-associated diseases based on the National health and nutrition examination survey (NHANES) 2013–2018. Sci Rep 15, 13778 (2025). https://doi.org/10.1038/s41598-025-98551-6
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-98551-6