Abstract
The detection of thyroglobulin in lymph node (LN) fine needle aspirates (FNA-Tg) is an effective supplement to ultrasound and fine needle aspiration cytology (FNAC) in diagnosis of cervical LN metastases for patients with papillary thyroid carcinoma (PTC). However, there is no unique cutoff value of FNA-Tg in practice. We aimed to determine the optimal cutoff of FNA-Tg and evaluate the interfering factors of FNA-Tg. A serial of 405 lateral cervical LN samples from 317 patients with PTC were analyzed retrospectively. Receiver operating characteristic (ROC) curve was used to determine the optimal cutoff of FNA-Tg. The factors that impact FNA-Tg were evaluated. Serum Tg, serum thyroglobulin antibody (TgAb) and serum thyroid stimulating hormone (TSH) level, and thyroid status did not differ between the malignant and benign LN groups. The median FNA-Tg was 3.81 ng/mL (0.16–33.40 ng/mL) in LNs without metastasis and 310.32 ng/mL (124.41–500.00 ng/mL) in LNs with metastasis, and the differences reached statistical significance (P < 0.01). The optimal cutoff of FNA-Tg was 36.22 ng/mL, and the values of area under the curve (AUC), sensitivity, specificity, positive predictive value (PPV) and negative predictive value (NPV) was 0.88, 0.89, 0.75, 0.91 and 0.71, respectively. The diagnostic accuracy of FNA-Tg cutoff of 36.22ng/mL was 85%. When FNAC and the present FNA-Tg cutoff of 36.22 ng/mL were combined together, the diagnostic sensitivity, specificity, PPV, NPV and diagnostic accuracy was 0.96, 0.75, 0.92, 0.87 and 91%, respectively. FNA-Tg improves the diagnostic efficacy of FNAC for PTC lateral cervical LN metastasis, and the optimal cutoff value of FNA-Tg was 36.22 ng/mL. FNA-Tg was affected by LN status but was not associated with serum Tg, serum TgAb, serum TSH and thyroid status.
Similar content being viewed by others
Introduction
Papillary thyroid carcinoma (PTC) is one of the most common endocrine system tumors, accounting for about 90% of thyroid carcinomas. The rate of cervical lymph node metastasis is high in PTC patients, about half of the patients when diagnosed, and the rate of lymph node micro-metastasis can even reach 70–90%1,2. Cervical lymph node metastasis is an important factor that affects the prognosis of PTC and its clinical treatment decisions, especially the extent of surgical operation3,4. The location and number of cervical lymph node metastasis are important factors in determining the extent of surgical operation and postoperative adjuvant treatment for patients with PTC5. In addition, clinical studies found that one of the main reasons for postoperative recurrence in PTC patients was insufficient evaluation of cervical lymph nodes (LNs) before initial operation6,7. Patients with LN metastases are involved in higher rates of recurrence and cancer mortality8. Accurate evaluation of the lymph nodes in the lateral cervical region before operation can avoid insufficient treatment caused by missed diagnosis or insufficient diagnosis, and also reduce the unnecessary expansion of the extent of surgery. Therefore, preoperative cervical lymph node evaluation is critical for the management of patients with PTC.
Generally, the indication for lateral cervical lymph node dissection recommended by guidelines is cytologically confirmed lateral lymph node metastasis5,9. The main diagnostic methods for lateral cervical lymph node metastasis are ultrasound and fine needle aspiration cytology (FNAC). Lymph nodes suspicious of metastasis in the lateral cervical region should be further examined by ultrasound (US)-guided FNAC. However, due to the limited number of cells in lymph node fine needle aspirates, there are 20–30% misdiagnosis, which affects clinical decision-making10,11. The detection of thyroglobulin in lymph node fine needle aspirates (FNA-Tg) is an effective supplement to FNAC, and the increase of FNA-Tg in lymph nodes probably indicates differentiated thyroid carcinoma metastasis. Clinical studies showed that the sensitivity of positive FNA-Tg in the diagnosis of lateral cervical lymph node metastasis in PTC patients can reach 80–100%12,13. However, there are still several problems to be solved in the clinical application of this parameter, the most important of which is the lack of a unified diagnostic cutoff value14,15,16,17. Some clinical centers use the absolute value of FNA-Tg in LN as the diagnostic standard, but the cutoff value of each center varies greatly, ranging from 1 ng/mL to 50 ng/mL13,18,19. In other centers, the positive criteria for LN metastasis are defined when the ratio of FNA-Tg in LN to serum Tg was greater than 0.1 or 115,17. In addition, the values of FNA-Tg in lymph nodes are also affected by a variety of factors, including serum Tg (sTg), the level of serum thyroglobulin antibody (sTgAb), whether total thyroidectomy has been performed or not, and the level of serum thyroid stimulating hormone (TSH)20,21. The conclusions from different studies are not consistent. However, there is still a lack of large-sample clinical studies on this issue.
The present study evaluated the diagnostic value of FNA-Tg for lateral cervical lymph node metastases, especially when FNAC did not find cancer cells, in patients with PTC through a large retrospective study. We also evaluated the factors that may affect the FNA-Tg result in clinical practice. We aimed to provide practical help for clinical diagnosis and treatment for PTC patients, especially for those who were suspicious of lateral cervical lymph node metastasis.
Materials and methods
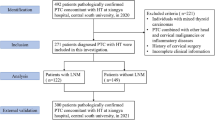
Patients diagnosed with PTC and suspected lateral cervical LN metastasis, and undergone surgical treatment between July 2019 and April 2022 at the Department of Otorhinolaryngology-Head and Neck Surgery, The First Affiliated Hospital of Xi’an Jiaotong University (Xi’an, Shaanxi, China) were enrolled retrospectively. The inclusion criterion was histologically confirmed PTC, regardless of initial treatment or disease recurrence. According to clinical guidelines, the patients with suspicious lateral cervical LN metastasis were given US-guided FNAC with or without FNA-Tg detection for the LNs. Patients undergone FNAC without FNA-Tg detection and those without complete data for analysis were excluded. A total of 405 LN samples from 317 patients were included in the study. The study was approved by the Institutional Review board of The First Affiliated Hospital of Xi’an Jiaotong University (XJTU-2019-ZD10). Informed written consent was obtained from the enrolled patients and participants received assurances that the information would only be used for research. The study was conducted in accordance with the Declaration of Helsinki, as well as any later modifications or equivalent ethical standards.
Ultrasound and US-guided fine-needle aspiration (FNA)
All 317 patients underwent US using a 10–12 MHz linear transducer by two experienced radiologists. The ultrasonic characteristics of suspicious LNs included a round shape (longitudinal/transverse diameter ratio < 1.5), hyperechogenicity or heterogeneous echogenicity, cystic changes, calcification, unclear boundary between the cortex and medulla, peripheral vascularity or a loss of echogenic hilum. The locations (levels II–V) of lateral cervical LNs were recorded according to the guidelines of the American Joint Committee on Cancer (AJCC) classification.
US-guided FNA was performed by a skilled and experienced physician, using 22-gauge needles. Each suspicious LN was aspirated twice to obtain adequate samples for analysis. The needle was inserted into the LN repeatedly until the needle hub was filled with sufficient material. Then, the aspirates were expelled onto glass and 5 µL of the sample was added to 195 µL Tg-free serum for FNA-Tg measurement. The remaining aspirate was smeared, fixed in 95% ethanol and sent for Papanicolaou staining and cytopathological examination. FNAC results were classified into three categories—malignant, benign, and inconclusive. Malignant was defined by the clear detection of cancer cells, benign was defined by the absence of cancer cells, and FNAC inconclusive was defined when suspicious cell morphology, necrosis, or poor epithelial cellularity was reported.
Thyroglobulin examination
Tg was assayed using a monoclonal antibody immunoradiometric assay (IRMA; CIS Bios International, Gif-surYvette, France). The detection range of Tg was 0.16 to 500.00 ng/mL. When the concentration exceeded 500.00 ng/mL, the value was recorded as > 500 ng/mL, and was counted as 500.00 µg/L during data processing. When the concentration was less than 0.16 ng/mL, the value was recorded as < 0.16 ng/mL, and was counted as 0.16 ng/mL during data processing. Serum Tg autoantibodies were measured using the Siemens IMMULITE 2000 assay (New York, NY, USA).
Definition of benign and metastatic lymph nodes and surgical protocol
Based on previous results and clinical experiences, when FNAC indicated benign LN and FNA-Tg was less than serum Tg, it was identified as benign LN. According to clinical guidelines, there was no evidence of lateral cervical lymph nodes metastasis and lateral lymph node dissection was not performed. When FNAC detected cancer cells in LNs, therapeutic lateral lymph node dissection was performed. When FNAC result was benign or inconclusive, but FNA-Tg was higher than 10ng/mL or higher than serum Tg level14,22, as metastasis could not be ruled out in these lymph nodes with elevated FNA-Tg, so selective lymph node dissection and intraoperative rapid freezing histologic examination were performed to determine whether these suspected lymph nodes were malignant or not (Fig. 1). And then, the data of these lymph nodes were added to different groups respectively after histological confirmation for final statistical analysis. Malignant FNAC results or positive histopathological results (intraoperative rapid freezing and postoperative pathological confirmation of cancer metastasis) were defined as the gold standard for cervical lymph node metastasis, otherwise they were considered non-metastatic lymph nodes. During the follow-up, there was no puncture-related needle tract implantation metastasis in the present group of patients.
Data collection and histopathological analyses
Data collected of each case included basic demographic data, FNAC results or histopathological results of LNs, serum Tg value (sTg), FNA-Tg, serum TgAb, TSH, whether total thyroidectomy has been performed or not, and ultrasonic characteristics of suspicious lateral cervical lymph nodes.
Statistical analyses
Median (lower quartile, upper quartile) was used for continuous variables, while composition ratio was used for categorical variables. The intergroup differences of variables were assessed using the “Mann-Whitney U Test” for continuous variables and the “Chi-Squared Test” for categorical variables. Linear regression analysis was used to explore the relationship between multiple factors and the dependent, which is FNA-Tg. The independent variables include gender, age, histopathology of tissue, serum Tg, TSH, serum TgAb, whether total thyroidectomy has been performed, and lymph node short-axis size. Statistical analysis is conducted using Python. Receiver operating characteristic (ROC) curves and area under the curve (AUC) were used to evaluate the diagnostic efficacy of FNA-Tg. A significance level of P < 0.05 indicated statistical significance.
Results
Comparison of FNA-Tg levels between metastatic lateral cervical lymph nodes and benign lymph nodes
A total of 405 LN samples from 317 patients were included in the study, with 106 males and 211 females. The median age for cases without metastasis was 43 years (37.25, 51.75). The median age for cases with metastasis was 40 years (32.00, 50.50). Among the 405 LNs, 258 LNs (63.70%) were diagnosed as malignant after FNAC and the patients were given therapeutic cervical lymph node dissection (Table 1; Fig. 1). In the remaining 147 LNs (36.30%), no cancer cells were observed through FNAC. Among the 147 LNs, 93 LNs were detected with elevated FNA-Tg level, and they were given selective lymph node dissection and intraoperative rapid freezing examination (Fig. 1). As a result, forty-six LNs (46/147, 31.29%) were confirmed as malignant by intraoperative rapid freezing examination and the patients were thus given therapeutic lateral cervical lymph node dissection, 47 (47/147, 31.97%) LNs were found without cancer metastasis. Fifty-four LNs (54/147, 36.73%) were found with neither positive FNAC result nor elevated FNA-Tg level, and were diagnosed as benign, and they were not given selective lymph node dissection. Therefore, the diagnostic rate of metastatic LNs was increased from 63.70% by FNAC alone to 75.06% by combination of FNAC and FNA-Tg detection, and 11.36% LNs (46/405) missing microscopic metastasis undetected with FNA cytology were avoided.
Serum Tg, TgAb and TSH level, and the percentage of previous history of total thyroidectomy did not differ between the malignant LN group and the benign LN group (Table 1). The median FNA-Tg was 3.81 ng/mL (0.16–33.40 ng/mL) in cases without metastasis and 310.32 ng/mL (124.41–500.00 ng/mL) in cases with metastasis, and the differences reached statistical significance (P < 0.01) (Table 1; Fig. 2). While there was no significant difference (P = 0.99) in serum Tg level between the benign LNs (median 11.62 ng/mL, 0.60-31.66 ng/mL) and the malignant LNs (median 12.29 ng/mL, 0.20-32.56 ng/mL) (Table 1; Fig. 3). The median LN short-axis size of cases with metastasis (5.10 mm, 4.00–7.60 mm) is significantly greater than that of cases without metastasis (4.70 mm, 3.80–5.50 mm) (P < 0.01). Refer to Table 1; Fig. 1, and Fig. 2 for details. Therefore, these data indicated that FNA-Tg levels of metastatic lateral cervical lymph nodes are higher than those of benign lymph nodes in PTC patients regardless of serum Tg, TgAb or TSH level, whether total thyroidectomy had been performed or not. And FNA-Tg measurement increased the diagnostic efficacy of FNAC in PTC patients.
Correlation between FNA-Tg and other factors
To evaluate the factors that correlate FNA-Tg level in the lateral cervical LNs, Spearman correlation analysis was performed. FNA-Tg was used as the dependent variable, incorporating TgAb, serum Tg, TSH, lymph node long-axis size, lymph node short-axis size, and lymph node long-axis size/short-axis size as independent variables. The correlation coefficient of TgAb was − 0.10, indicating a very weak negative correlation with FNA-Tg, with statistical significance at P = 0.05. The correlation coefficient of lymph node short-axis size was 0.10, indicating a very weak positive correlation with FNA-Tg, with statistical significance at P = 0.04. The correlation coefficient of lymph node long-axis size/short-axis size was − 0.18, indicating a very weak negative correlation with FNA-Tg, with statistical significance at P < 0.01. Serum Tg, TSH, and lymph node long-axis size showed no statistical significance. Refer to Table 2.
Univariate and multivariate linear regression analysis of multiple factors and FNA-Tg in cervical lateral lymph nodes metastasis
FNA-Tg was used for the dependent variable, incorporating gender, age, definite lymph node status (malignant or benign), serum Tg, TSH, serum TgAb, whether total thyroidectomy has been performed, and lymph node short-axis size as independent variables. In the univariate analysis, the regression coefficient for definite lymph node status was − 32.74, with statistical significance at P < 0.01. The average FNA-Tg value for cases with cancer metastasis was increased by 250.09 ng/mL compared to cases without metastasis. The regression coefficient for total thyroidectomy was 56.12, with statistical significance at P = 0.09. The average FNA-Tg value for cases with total thyroidectomy was increased by 56.12 ng/mL compared to cases without total thyroidectomy. The regression coefficient for lymph node short-axis size was 6.33, with statistical significance at P = 0.03. For every 1 mm increase in lymph node short-axis size, FNA-Tg increased by 6.33 ng/mL. Gender, age, serum Tg, TSH, and serum TgAb showed no statistical significance in this analysis. The variables with statistical significance in the univariate analysis, including definite lymph node status, whether total thyroidectomy has been performed, and lymph node short-axis size, were included in the multivariate analysis. In the multivariate analysis, the regression coefficient for definite lymph node status was 247.65, with statistical significance at P < 0.01. The average FNA-Tg value for cases with cancer metastasis was increased by 247.65 ng/mL compared to cases without metastasis. Total thyroidectomy and lymph node short-axis size showed no statistical significance. Refer to Table 3.
ROC analysis for cutoff values of FNA-Tg
To evaluate the optimal cutoff value for metastatic lateral lymph nodes diagnosis in PTC patients, definite lymph node status (malignant or benign) was used as the dependent variable, and FNA-Tg was used as the independent variable for conducting ROC analysis. When FNA-Tg reached 36.22 ng/mL, the Youden’s index reached its maximum value. The values of AUC, sensitivity, specificity, positive predictive value (PPV) and negative predictive value (NPV) was 0.88, 0.89, 0.75, 0.91 and 0.71, respectively. And the diagnostic accuracy of FNA-Tg cutoff of 36.22ng/mL was 85%. Refer to Table 4; Fig. 4. Therefore, ROC analysis indicates the optimal FNA-Tg cutoff of 36.22 ng/mL for diagnosing lateral cervical lymph nodes metastasis in PTC patients.
When FNAC was used alone to assess the suspicious lymph nodes was metastatic or not, the diagnostic sensitivity, specificity, PPV, NPV and diagnostic accuracy was 0.86, 1.00, 1.00, 0.71 and 0.90, respectively. When FNAC and the present FNA-Tg cutoff of 36.22 ng/mL were combined together, the diagnostic sensitivity, specificity, PPV, NPV and diagnostic accuracy was 0.96, 0.75, 0.92, 0.87 and 0.91, respectively (Table 5). Therefore, the sensitivity of diagnosis was significantly improved and the misdiagnosis was correspondingly reduced.
ROC: receiver operating characteristic; AUC: area under the curve; FNA-Tg: thyroglobulin in lymph node fine needle aspirates; PPV: positive predictive value; NPV: negative predictive value.
ROC curve of FNA-Tg for diagnosing lateral lymph nodes metastasis in PTC patients. Definite lymph node status was used as the dependent variable, and FNA-Tg was used as the independent variable for conducting ROC analysis. The best cutoff of FNA-Tg was 36.22ng/mL, and the corresponding AUC value was 0.88. ROC: receiver operating characteristic; AUC: area under the curve; FNA-Tg: thyroglobulin in lymph node fine needle aspirates.
Discussion
The use of FNA-Tg in the diagnosis of suspicious metastatic LN for PTC patients was initially proposed by Pacini et al. in 199223. It has gradually become a reliable tool and an excellent partner of FNAC in clinical practice24. Both of the sensitivity and specificity of FNA-Tg for diagnosing metastatic LN can reach 80–100%, respectively14. The main deficiency of FNA-Tg usage is lack of standard cutoff value which ranged from 1 to 50.0 µg/L in different centers13,18. Also, the values of FNA-Tg are affected by multiple influencing factors which may interfere with clinical interpretation15,25. In the present study, we retrospectively analyzed a large sample of suspicious lateral cervical LNs which were given FNAC and simultaneous FNA-Tg measurement in PTC patients. As a result, the median FNA-Tg level in metastatic LNs was significantly higher than that in non-metastatic LNs (310.32 ng/mL vs. 3.81 ng/mL) regardless of serum Tg, serum TgAb, serum TSH level and previous history of total thyroidectomy. FNA-Tg detection increased the diagnostic rate of metastatic LNs from 63.70% by FNAC alone to 75.06%, and thus 11.36% LNs misdiagnosis were avoided. FNA-Tg detection also helped FNAC exclude 13.33% of non-metastatic lymph nodes. Indeed, FNA-Tg measurement increased the diagnostic sensitivity and efficacy of FNAC in diagnosis of suspicious lateral cervical LNs for PTC patients. The result agreed with most previous studies26,27,28.
In previous studies, the variation and inconsistency of FNA-Tg cutoff values may be due to different detection methods for Tg, which included immunometric assay, radioimmunoassay, immunoradiometric and immunochemiluminescence assays14. In addition, the studies were carried out in different populations, and most of the sample sizes were small. In the present study, a total of 405 suspicious LNs were enrolled in study which may produce more convinced results. ROC analysis indicates the optimal FNA-Tg cutoff value for diagnosing lateral cervical LNs metastasis in PTC patients was 36.22 ng/mL and the corresponding diagnostic accuracy was 85%. Because FNA-Tg does not differ between the patients with and without previous medical history of total thyroidectomy, the cutoff value can be used no matter thyroid is absent or not. The result was consistent with recent studies26. In Liu’s study, the best cutoff values of FNA-Tg in nonsurgery group and surgery group were similar, 25.17 and 28.30 µg/L, respectively26.
The potential factors that may influence FNA-Tg value and its clinical interpretation mainly include serum Tg, serum TgAb and whether total thyroidectomy has been performed or not20,21,25,29,30. In several previous studies, the presence of thyroid may increase serum Tg level and lead to higher FNA-Tg cutoff values for diagnosing cervical LNs metastasis in DTC patients19,31. However, other studies got different results and showed that the presence of thyroid and serum Tg level did not influence FNA-Tg cutoff values in clinical practice18,32. In the present study, there was no significant difference in serum Tg level between the patients with benign LNs and malignant LNs (median 11.62 ng/mL vs. 12.29 ng/mL, P = 0.99). In the univariate and multivariate linear regression analysis, serum Tg level and thyroid status were not independent factors that influence FNA-Tg. As for serum TgAb, it mainly decreases the detected serum Tg level. As a result, it did not influence FNA-Tg neither in the present results. Therefore, our results indicated that serum Tg, serum TgAb and thyroid status do not influence FNA-Tg level and its clinical interpretation when determining lymph node status in clinical practice.
Another influential factor that deserves our attention is the difference in the detection methods of different institutions, especially some details of which may affect the FNA-Tg value. For example, in different hospitals, when researchers take samples of puncture eluent, the dosage of solvent used to wash the puncture needle is different, including 1 mL or 1.5 mL, some may less than 1 mL13,22,26. This may increase the differences between the diagnostic cutoff values derived from different studies, and also makes it difficult to obtain a uniform standard that can be generalized. Therefore, unified detection methods will facilitate the communication of clinical data from different institutions.
Our study provides strengthened data for the value of FNA-Tg in diagnosing lateral cervical LN metastasis accompanied by FNAC for patients with PTC. However, there are still some limitations that need to be improved. Firstly, although the sample size was large, the data were from one single center. The results need to be validated by multicenter clinical trials especially with uniform criteria and the same patient cohort. Secondly, the benign LN was defined when FNAC indicated benign LN and FNA-Tg was less than 10 ng/mL based on previous results and clinical experiences14,22. Some benign LNs were not verified by histopathological examination. Thus, a large prospective study may be needed. Another inevitable issue in this subject is that FNA-Tg might be contaminated by patient blood in patients with high serum Tg14. Thus, strict and standardized procedure is vital in clinical practice. Meanwhile, the interpretation of the results should be combined with clinical factors including serum Tg, ultrasonic characteristics of LNs, characteristics of thyroid lesions and previous history.
Conclusions
In conclusion, FNA-Tg improves the diagnostic efficacy of FNAC for PTC lateral cervical lymph node metastasis, and the optimal cutoff value of FNA-Tg was 36.22 ng/mL at our center. FNA-Tg was affected by lymph node status but was not associated with serum Tg, serum TgAb and serum TSH level, and thyroid status.
Data availability
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
References
Qubain, S. W. et al. Distribution of lymph node micrometastasis in pN0 well-differentiated thyroid carcinoma. Surgery 131 (3), 249–256 (2002).
Shirley, L. A., Jones, N. B. & Phay, J. E. The role of central neck lymph node dissection in the management of papillary thyroid Cancer. Front. Oncol. 7, 122 (2017).
Sapuppo, G. et al. Latero-cervical lymph node metastases (N1b) represent an additional risk factor for papillary thyroid cancer outcome. J. Endocrinol. Invest. 40 (12), 1355–1363 (2017).
Sapuppo, G. et al. Lymph node location is a risk factor for papillary thyroid cancer-related death. J. Endocrinol. Invest. 41 (11), 1349–1353 (2018).
Haugen, B. R. et al. 2015 American thyroid association management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: the American thyroid association guidelines task force on thyroid nodules and differentiated thyroid Cancer. Thyroid 26 (1), 1–133 (2016).
Mulla, M. G. et al. Lateral cervical lymph node metastases in papillary thyroid cancer: a systematic review of imaging-guided and prophylactic removal of the lateral compartment. Clin. Endocrinol. (Oxf). 77 (1), 126–131 (2012).
Wang, Y. et al. Risk factors and a prediction model of lateral lymph node metastasis in CN0 papillary thyroid carcinoma patients with 1–2 central lymph node Metastases. Front. Endocrinol. (Lausanne). 12, 716728 (2021).
Liu, F. H. et al. Postoperative recurrence of papillary thyroid carcinoma with lymph node metastasis. J. Surg. Oncol. 112 (2), 149–154 (2015).
Filetti, S. et al. Thyroid cancer: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann. Oncol. 30 (12), 1856–1883 (2019).
Cáp, J. et al. Sensitivity and specificity of the fine needle aspiration biopsy of the thyroid: clinical point of view. Clin. Endocrinol. (Oxf). 51 (4), 509–515 (1999).
Leonard, N. & Melcher, D. H. To operate or not to operate? The value of fine needle aspiration cytology in the assessment of thyroid swellings. J. Clin. Pathol. 50 (11), 941–943 (1997).
Kahramangil, B. et al. Thyroglobulin washout from cervical lymph node fine needle aspiration biopsies in patients with differentiated thyroid cancer: an analysis of different expressions to use in post-total thyroidectomy follow-up. Surgery 167 (1), 34–39 (2020).
Zhu, X. H. et al. Diagnostic values of thyroglobulin in lymph node fine-needle aspiration washout: a systematic review and meta-analysis diagnostic values of FNA-Tg. Endocr. J. 67 (2), 113–123 (2020).
Torres, M. R. et al. Thyroglobulin in the washout fluid of lymph-node biopsy: what is its role in the follow-up of differentiated thyroid carcinoma?. Thyroid 24 (1), 7–18 (2014).
Jeon, M. J. et al. Thyroglobulin level in fine-needle aspirates for preoperative diagnosis of cervical lymph node metastasis in patients with papillary thyroid carcinoma: two different cutoff values according to serum thyroglobulin level. Thyroid 25 (4), 410–416 (2015).
Grani, G. & Fumarola, A. Thyroglobulin in lymph node fine-needle aspiration washout: a systematic review and meta-analysis of diagnostic accuracy. J. Clin. Endocrinol. Metab. 99 (6), 1970–1982 (2014).
Jiang, H. J. & Hsiao, P. J. Clinical application of the ultrasound-guided fine needle aspiration for thyroglobulin measurement to diagnose lymph node metastasis from differentiated thyroid carcinoma-literature review. Kaohsiung J. Med. Sci. 36 (4), 236–243 (2020).
Kim, D. W., Jeon, S. J. & Kim, C. G. Usefulness of thyroglobulin measurement in needle washouts of fine-needle aspiration biopsy for the diagnosis of cervical lymph node metastases from papillary thyroid cancer before thyroidectomy. Endocrine 42 (2), 399–403 (2012).
Zhai, L. et al. Impact of thyroid tissue status on the Cut-Off value of lymph node Fine-Needle aspiration thyroglobulin measurements in papillary thyroid Cancer. Br. J. Biomed. Sci. 79, 10210 (2022).
Martins-Costa, M. C. et al. Clinical impact of thyroglobulin (Tg) and Tg autoantibody (TgAb) measurements in needle washouts of neck lymph node biopsies in the management of patients with papillary thyroid carcinoma. Arch. Endocrinol. Metab. 61 (2), 108–114 (2017).
Sobrinho-Simões, M. et al. Impact of serum TSH and Anti-Thyroglobulin antibody levels on lymph node Fine-Needle aspiration thyroglobulin measurements in differentiated thyroid Cancer Patients. Mod. Pathol. 6 (6), 292–297 (2017).
Wang, J. et al. Excellent Diagnostic Performance of FNA-Tg in Detecting Lymph Nodes Metastases from Papillary Thyroid cancer (Future Oncol, 2020).
Pacini, F. et al. Detection of thyroglobulin in fine needle aspirates of nonthyroidal neck masses: a clue to the diagnosis of metastatic differentiated thyroid cancer. J. Clin. Endocrinol. Metab. 74 (6), 1401–1404 (1992).
Xiao, J. et al. Optimal method for detecting cervical lymph node metastasis from papillary thyroid cancer. Endocrine 79 (2), 342–348 (2023).
Sun, J. et al. The influence of thyroid status, serum Tg, TSH, and TgAb on FNA-Tg in cervical metastatic lymph nodes of papillary thyroid carcinoma. Laryngoscope Investig Otolaryngol. 7 (1), 274–282 (2022).
Liu, Q. et al. Diagnostic efficacy of FNA-Tg in DTC cervical LN metastasis and its impact factors: A large retrospective Study. J. Clin. Endocrinol. Metab., (2023).
Jia, X. et al. Thyroglobulin measurement through Fine-Needle aspiration for optimizing neck node dissection in papillary thyroid Cancer. Ann. Surg. Oncol. 29 (1), 88–96 (2022).
Jeon, S. J. et al. Diagnostic benefit of thyroglobulin measurement in fine-needle aspiration for diagnosing metastatic cervical lymph nodes from papillary thyroid cancer: correlations with US features. Korean J. Radiol. 10 (2), 106–111 (2009).
Blazekovic, I. et al. Thyroglobulin measurement in needle aspiration for detection of recurrences and neck metastases in patients with differentiated thyroid carcinoma: significance of Anti-Tg Antibodies. Acta Clin. Croat. 59 (Suppl 1), 9–17 (2020).
Zhao, H. et al. Influence of presence/absence of thyroid gland on the cutoff value for thyroglobulin in lymph-node aspiration to detect metastatic papillary thyroid carcinoma. BMC Cancer. 17 (1), 296 (2017).
Lee, J. H. et al. Influence of thyroid gland status on the thyroglobulin cutoff level in washout fluid from cervical lymph nodes of patients with recurrent/metastatic papillary thyroid cancer. Head Neck. 38 (Suppl 1), E1705–1712 (2016).
Bournaud, C. et al. Thyroglobulin measurement in fine-needle aspirates of lymph nodes in patients with differentiated thyroid cancer: a simple definition of the threshold value, with emphasis on potential pitfalls of the method. Clin. Chem. Lab. Med. 48 (8), 1171–1177 (2010).
Acknowledgements
We sincerely thank the staff members at the Department of Medical Ultrasonics, The First Affiliated Hospital of Xi’an Jiaotong University, for their support.
Funding
This work was supported by the Basic Natural Science Research Program of Shaanxi Province (grant number 2022JM-552).
Author information
Authors and Affiliations
Contributions
Junsong Liu and Shaoqiang Zhang designed the study; Junsong Liu collected data and drafted the manuscript; Rui Wang and Chongwen Xu analyzed the data and reviewed the manuscript; Ruimin Zhao, Shiyang Wang, Qian Zhao and Honghui Li did surgical operation and collected data, Xiaobao Yao and Rui Gao interpreted the data and edited the manuscript; Shaoqiang Zhang and Yanxia Bai reviewed the manuscript and contributed for final approval. All authors have reviewed and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
The study was approved by the Institutional Review board of The First Affiliated Hospital of Xi’an Jiaotong University (XJTU-2019-ZD10). Informed written consent was obtained from the enrolled patients.
Consent for publication
Written informed consents for publication were obtained from all participants.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Liu, J., Wang, R., Xu, C. et al. FNA-Tg improves the diagnostic efficacy of FNAC for PTC lateral cervical LN metastasis. Sci Rep 15, 14057 (2025). https://doi.org/10.1038/s41598-025-99169-4
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-99169-4