Abstract
Introduction
Injecting drug users often extract morphine from slow-release oral tablets, potentially leading to harmful particle contamination upon injection. This study assesses the efficiency of morphine extraction and particle content of filtrates produced by various methods employed by drug users in Trondheim, Norway. The findings provide important insights that can inform harm-reduction services and healthcare providers in efforts to reduce injection-related morbidity among people who already inject drugs.
Methods
Four extraction methods were evaluated using 60 mg Dolcontin tablets: Method A (no coating removal, 3-minute boiling), Method B (coating removal, crushing, 3-minute boiling), Method C (coating removal, 3-minute boiling), and Method D (coating removal, 10-minute boiling). Resulting solutions were filtered using cotton balls, and morphine content was quantified using LC-MS/MS. Particle content of filtrates was analyzed using slide scanning, deep learning-based particle segmentation, and QuPath image analysis software.
Results
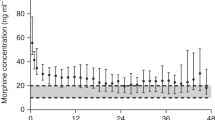
Morphine recovery ranged from 81.2% (Method D) to 91.3% (Method B). Method A yielded a significant presence of small insoluble particles (<100 μm), while Method B yielded the highest density of the largest particles (>500 μm). Method C exhibited the highest density of medium-sized particles (100-500 μm). Method D generated the fewest particles across all size categories.
Conclusion
The extraction methods used by injecting drug users result in significant variability in morphine recovery and particle content of filtrates. Method D (10-minute vs. 3-minute boiling) demonstrated the highest efficiency in particle reduction, with only 10% less morphine recovery. Lack of coat removal significantly increases the number of primarily small (<100 μm) fragments. These findings highlight the importance of evidence-based harm-reduction measures to mitigate risks associated with injecting tablet-derived solutions. The results may support harm-reduction counselling and service design aimed at reducing particulate exposure and related complications, without endorsing or facilitating drug use.
Similar content being viewed by others
Data availability
The scanned slides, raw MS-data and segmentation masks for the particle content analyses are available from the corresponding author upon reasonable requests.
References
United Nations Office on Drugs and Crime. World drug report 2023 (Technical report, United Nations Office on Drugs and Crime, Vienna, 2023).
Mathers, B. M. et al. Mortality among people who inject drugs: A systematic review and meta-analysis. Bull. World Health Organ. 91(2), 102–123 (2013).
Edvardsen, H. E. et al. Differences in combinations and concentrations of drugs of abuse in fatal intoxication and driving under the influence cases. Forensic Sci. Int. 281, 127–133 (2017).
Folkehelseinstituttet. Narkotika i norge. Technical report, Folkehelseinstituttet (Norwegian Institute of Public Health), Oslo, (2021)
World Health Organization. Opioid overdose fact sheet, (2023)
Dahlman, D., Berge, J., Bjorkman, P., Nilsson, A. C. & Hakansson, A. Both localized and systemic bacterial infections are predicted by injection drug use: A prospective follow-up study in Swedish criminal justice clients. PLoS One 13(5), e0196944 (2018).
Kammersgaard, T. From punishment to help? Continuity and change in the Norwegian decriminalization reform proposal. The International journal on drug policy 113, 103963 (2023).
Marks, L. R., Durkin, M. J., Ayres, K. & Ellis, M. Drug preparation, injection-related infections, and harm reduction practices among a national sample of individuals entering treatment for opioid use disorder. Harm reduction journal 21(1), 16 (2024).
Des Jarlais, D. C. Harm reduction in the USA: The research perspective and an archive to David Purchase. Harm reduction journal 14(1), 51 (2017).
Robertson, R., Broers, B. & Harris, M. Injecting drug use, the skin and vasculature. Addiction (Abingdon, England) 116(7), 1914–1924 (2021).
Hanoa, K., Bilgrei, O. R., Buvik, K. & Gjersing, L. “Hooked on the needle’’: Exploring the paradoxical attractions towards injecting drug use. Drugs Educ. Prev. Policy 29(6), 667–674 (2022).
McLean, S., Bruno, R., Brandon, S. & de Graaff, B. Effect of filtration on morphine and particle content of injections prepared from slow-release oral morphine tablets. Harm reduction journal 6, 37 (2009).
Puzhko, S. et al. Effectiveness of interventions for prevention of common infections among opioid users: A systematic review of systematic reviews. Front. Pub. Health 10, 749033 (2022).
Platt L. et al. Needle and syringe programmes and opioid substitution therapy for preventing HCV transmission among people who inject drugs: Findings from a Cochrane Review and meta-analysis. Addiction (Abingdon, England) 113(3), 545–563 (2018).
Fernandes, R. M. et al. Effectiveness of needle and syringe Programmes in people who inject drugs - An overview of systematic reviews. BMC Public Health 17(1), 309 (2017).
Melby, K. et al. International perspectives on opioid use disorder and treatment: Results from an online convenience sample. Heroin Addict. Relat. Clin. Probl. 26(5), (2024)
Javid, S., Rahmanulla, A., Ahmed, M. G., Sultana, R. & Prashantha Kumar, B. R. Machine learning & deep learning tools in pharmaceutical sciences: A comprehensive review. Intell. Pharm. 3(3), 167–180 (2025).
Koutroumpa, N. M., Papavasileiou, K. D., Papadiamantis, A. G., Melagraki, G. & Afantitis, A. A systematic review of deep learning methodologies used in the drug discovery process with emphasis on in vivo validation. International journal of molecular sciences 24(7), 6573 (2023).
Cao, Y., Geddes, T. A., Yang, J. Y. H. & Yang P. Ensemble deep learning in bioinformatics. Nat. Mach. Intell. 2(9), 500–508 (2020).
Hegstad, S., Hermansson, S., Betner, I., Spigset, O. & Falch, B. M. Screening and quantitative determination of drugs of abuse in diluted urine by UPLC-MS/MS. Journal of chromatography. B, Analytical technologies in the biomedical and life sciences 947–948, 83–95 (2014).
Belevich, I., Joensuu, M., Kumar, D., Vihinen, H. & Jokitalo, E. Microscopy image browser: A platform for segmentation and analysis of multidimensional datasets. PLoS biology 14(1), e1002340 (2016).
Belevich, I. & Jokitalo, E. DeepMIB: User-friendly and open-source software for training of deep learning network for biological image segmentation. PLoS computational biology 17(3), e1008374 (2021).
Pettersen, H. S. et al. Code-free development and deployment of deep segmentation models for digital pathology. Front. Med. 8, 816281 (2022).
Vermeire, A. & Remon, J. P. Stability and compatibility of morphine. International Journal of Pharmaceutics 187(1), 17–51 (1999).
Perez, M., Maiguy-Foinard, A., Barthélémy, C., Décaudin, B. & Odou, P. Particulate matter in injectable drugs: Evaluation of risks to patients. Pharm. Technol. Hosp. Pharm. 1(2), 91–103 (2016).
Shah, M. et al. Risk factors of infective endocarditis in persons who inject drugs. Harm Reduction J. 17(1), 35 (2020).
Maghsoudi, N. et al. Drug checking services for people who use drugs: A systematic review. Addiction 117(3), 532–544 (2022).
Higgs, P., Moore, D. & Aitken, C. Engagement, reciprocity and advocacy: Ethical harm reduction practice in research with injecting drug users. Drug and alcohol review 25(5), 419–23 (2006).
Acknowledgements
We would like to acknowledge the technical help of scanning and preparation for scanning by Cellular & Molecular Imaging Core Facility (CMIC), NTNU.
Funding
Open access funding provided by NTNU Norwegian University of Science and Technology (incl St. Olavs Hospital - Trondheim University Hospital). This research was partly funded by Research Fund for the Center for Laboratory Medicine, St. Olavs Hospital, Trondheim University Hospital.
Author information
Authors and Affiliations
Contributions
HSP performed the image analysis and statistical analysis of images data and participated in the preparation and scanning of samples. POMG designed and performed morphine extraction and participated in the preparation and scanning of samples. KM contributed to the design of the study, morphine extraction, the preparation of the manuscript, and contributed to the preparation and scanning of samples. TOAA contributed to the design of the study. All authors contributed to the writing and editing of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors report there are no competing interests to declare.
Ethical approval
Not applicable.
Consent for publication
All authors consent to publication.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Pettersen, H.S., Gundersen, P.O.M., Aamo, T.O. et al. Deep learning analysis of particle content in extracted slow-release morphine: longer boiling reduces large fragments while retaining morphine extraction. Sci Rep (2026). https://doi.org/10.1038/s41598-026-35870-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-026-35870-2