Abstract
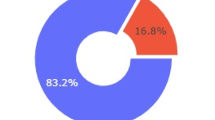
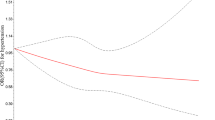
Hypertension is an emerging public health problem in Bhutan due to epidemiological and nutritional transitions in the last two decades. This study aimed to quantify risk factors of hypertension in Bhutan using nationally representative data. This was a secondary data analysis of a nationally representative World Health Organization Non-Communicable Disease STEP-wise Survey of Bhutan carried out in 2019. Multivariable logistic regression analysis was conducted to identify the risk factors of hypertension in the population 40–69 years age group. The Bayesian network (BN) analysed the influencing factors on the prevalence of hypertension. Of the 2,574 individuals aged 40–69 years sampled, 56.8% were women. The prevalence of hypertension was 44.3% (1,140). In multivariable logistic regression, participants in 55–59 and 60–64 years were 44% (adjusted odds ratio [AOR] = 1.44; 95% confidence interval [CI] 1.06, 2.14) and 65% (AOR = 1.65; 95% CI 1.17, 2.42) higher odds of developing hypertension than 40–44 years old. Compared to non-formal education, certificate and bachelor, and year 12 educated were 77% (AOR = 1.77; 95% CI 1.01, 3.12) and 54% (AOR = 1.54; 95% CI 1.02, 2.32) odds of reporting hypertension. The higher wealth index had lower odds of hypertension than those in the lower wealth index. Alcohol use was associated with developing hypertension (AOR = 1.73; 95% CI 1.39, 2.15) compared to non-drinkers. Those who chewed betel quid were 38% (AOR = 0.62; 95% CI 0.50, 0.76) less odds of reporting hypertension than those who did not chew betel quid. Individuals with obesity (AOR = 2.39; 95% CI 1.84, 3.12) and overweight (AOR = 1.44; 95% CI 1.04, 1.98) had more than twice and 44% higher odds of developing hypertension compared to those with normal body mass index (BMI). Borderline (AOR = 2.0; 95% CI 1.05, 3.81) and high cholesterol levels (AOR = 1.84; 95% CI 1.32, 2.57) were associated with an increased odds of hypertension compared to normal blood cholesterol levels. The conditional probability of hypertension using BN showed that obese and border blood cholesterol was associated with an increased odds of hypertension. While use alcohol use and chewing betel quid lowered the odds of hypertension. These findings highlight the need for targeted hypertension prevention strategies that address both behavioural and socioeconomic factors such as older age, alcohol use, pre-obesity and obesity, and high cholesterol levels. Therefore, the Ministry of Health, Bhutan should implement a comprehensive prevention and management program that include both clinical care and non-pharmacological strategies such as promoting healthy lifestyles, maintaining optimal body weight, and conducting regular screenings for hypertension and related conditions like high cholesterol.
Similar content being viewed by others
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
WHO. Global Status Report on Noncommunicable Diseases 2010 (World Health Organization, 2011).
Collaboration, N. C. D. R. F. Worldwide trends in hypertension prevalence and progress in treatment and control from 1990 to 2019: a pooled analysis of 1201 population-representative studies with 104 million participants. Lancet 398, 957–980 (2021).
Hypertension [https://www.who.int/news-room/fact-sheets/detail/hypertension]
WHO. Causes of death 2008: data sources and methods. vol. Online database, edition2011. (2011).
Mills, K. T., Stefanescu, A. & He, J. The global epidemiology of hypertension. Nat. Rev. Nephrol. 16, 223–237 (2020).
Ha, S. K. Dietary salt intake and hypertension. Electrolytes Blood Pressure: E BP. 12, 7–18 (2014).
Messerli, F. H., Williams, B. & Ritz, E. Essential hypertension. The Lancet, 370:591–603 .
Fuchs, F. D., Chambless, L. E., Whelton, P. K., Nieto, F. J. & Heiss, G. Alcohol consumption and the incidence of hypertension: the atherosclerosis risk in communities study. Hypertension 37, 1242–1250 (2001).
Husain, K., Ansari, R. A. & Ferder, L. Alcohol-induced hypertension: mechanism and prevention. World J. Cardiol. 6, 245–252 (2014).
Lloyd-Sherlock, P., Beard, J., Minicuci, N., Ebrahim, S. & Chatterji, S. Hypertension among older adults in low- and middle-income countries: prevalence, awareness and control. Inter. J. Epidemiol. (2014).
Primatesta, P., Falaschetti, E., Gupta, S., Marmot, M. G. & Poulter, N. R. Association between smoking and blood pressure: evidence from the health survey for England. Hypertension 37, 187–193 (2001).
Kokkinos, P. et al. Exercise capacity and 24-h blood pressure in prehypertensive men and women. Am. J. Hypertens. 19, 251–258 (2006).
Pinto, E. Blood pressure and ageing. Postgrad. Med. J. 83, 109–114 (2007).
Sun, Z. Aging, arterial Stiffness, and hypertension. Hypertension 65, 252–256 (2015).
Skurnick, J. H., Aladjem, M. & Aviv, A. Sex differences in pulse pressure trends with age are Cross-Cultural. Hypertension 55, 40–47 (2010).
Coffman, T. M. & Crowley, S. D. Kidney in hypertension: Guyton redux. Hypertension 51, 811–816 (2008).
Hall, J. E. Pathophysiology of obesity hypertension. Curr. Hypertens. Rep. 2, 139–147 (2000).
Hall, J. E., Crook, E. D., Jones, D. W., Wofford, M. R. & Dubbert, P. M. Mechanisms of obesity-associated cardiovascular and renal disease. Am. J. Med. Sci. 324, 127–137 (2002).
P, B. M., K: The nutritional transition, S. H. S. & Diet-related chronic diseases in and Asia: implications for prevention. (Food Consumption and Nutrition Division IFPRI ed., vol. FCND Discussion paper NO. 105. Washington, D.C. (2001).
Popkin, B. M., Adair, L. S. & Ng, S. W. NOW AND THEN: the global nutrition transition: the pandemic of obesity in developing countries. Nutr. Rev. 70, 3–21 (2012).
Turin, T. C. et al. Burden of Cardio- and Cerebro-vascular diseases and the conventional risk factors in South Asian population. Global Heart. 8, 121–130 (2013).
Giri, B. R., Sharma, K. P., Chapagai, R. N. & Palzom, D. Diabetes and hypertension in urban Bhutanese men and women. Indian J. Commun. Med. 38, 138–143 (2013).
Sithey, G., Wen, L. M., Dzed, L. & Li, M. Noncommunicable diseases risk factors in bhutan: A secondary analysis of data from bhutan’s nationwide STEPS survey 2014. PLoS One. 16, e0257385 (2021).
MoH: Noncommunicable Disease Risk Factors: Bhutan STEPS Survey Report. Thimphu, Bhutan: Department of Public Health, Ministry of Health, Bhutan; (2019).
Chhezom, K., Gurung, M. S. & Wangdi, K. Comparison of laboratory and Non-Laboratory-Based 2019 world health organization cardiovascular risk charts in the Bhutanese population. Asia Pac. J. Public. Health. 36, 29–35 (2024).
Witteveen, A., Nane, G. F., Vliegen, I. M. H., Siesling, S. & MJ, I. J. Comparison of logistic regression and bayesian networks for risk prediction of breast cancer recurrence. Med. Decis. Mak. 38, 822–833 (2018).
Liu, Y. et al. A gentle introduction to bayesian network Meta-Analysis using an automated R package. Multivar. Behav. Res. 58, 706–722 (2023).
Pan, J. et al. Prevalence of hyperlipidemia in Shanxi Province, China and application of bayesian networks to analyse its related factors. Sci. Rep. 8, 3750 (2018).
Zhao, L. et al. A bayesian network for estimating hypertension risk due to occupational aluminum exposure. Chronic Dis. Transl Med. 10, 130–139 (2024).
WHO. Guideline for the Pharmacological Treatment of Hypertension in Adults (World Health Organization, 2021).
A healthy lifestyle - WHO recommendations [https://www.who.int/europe/news-room/fact-sheets/item/a-healthy-lifestyle---who-recommendations]
WHO. Classification of Diabetes Mellitus (World Health Organization, 2019).
Mancini, F. et al. Classification of postural profiles among mouth-breathing children by learning vector quantization. Methods Inf. Med. 50, 349–357 (2011).
Kumar, B. S. & Venkateswarlu, C. Inverse modeling approach for evaluation of kinetic parameters of a biofilm reactor using Tabu search. Water Environ. Res. 86, 675–686 (2014).
Scutari, M. Dirichlet bayesian network scores and the maximum relative entropy principle. Behaviormetrika 45, 337–362 (2018).
Adabor, E. S., Acquaah-Mensah, G. K. & Oduro, F. T. SAGA: a hybrid search algorithm for bayesian network structure learning of transcriptional regulatory networks. J. Biomed. Inf. 53, 27–35 (2015).
Broom, B. M., Do, K. A. & Subramanian, D. Model averaging strategies for structure learning in bayesian networks with limited data. BMC Bioinform. 13 (Suppl 13), S10 (2012).
Wangdi, K. & Jamtsho, T. Prevalence and predisposing factors for self-reported hypertension in Bhutanese adults. Nepal. J. Epidemiol. 10, 830–840 (2020).
MoH. Annual Health Bulletin. (Ministry of Health B ed. Thimphu2023. (2022).
Delivering NCD services with care. and compassion in Bhutan [https://www.who.int/bhutan/news/feature-stories/detail/delivering-ncd-services-with-care-and-compassion-in-bhutan]
Tripathy, J. P. & Mishra, S. How effective was implementation of the package of essential non-communicable disease (PEN) interventions: A review of evidence? Diabetes Metab. Syndr. 15, 102266 (2021).
Kempers, J. et al. Does training on the WHO package of essential noncommunicable (PEN) disease interventions enhance consultation quality? A real-world assessment of adherence to PEN protocol in primary health centres in the Republic of Moldova. Global Health Action. 16, 2285619 (2023).
Rahman, M. et al. Prevalence, treatment patterns, and risk factors of hypertension and pre-hypertension among Bangladeshi adults. J. Hum. Hypertens. 32, 334–348 (2018).
Franklin, S. S. et al. Hemodynamic patterns of age-related changes in blood pressure. The Framingham heart study. Circulation 96, 308–315 (1997).
Wangdi, K. & Jamtsho, T. Prevalence and correlates of current alcohol use among Bhutanese adults: A nationally representative survey data analysis. Indian J. Psychol. Med. 41, 38–45 (2019).
RGoB. National Policy and Strategic Framework To Reduce Harmful Use of Alcohol: 2015–2020. (2015).
MoH. Annual Health Bulletin 2015. (Ministry of Health B ed. Thimphu, Bhutan (2015).
MoH. Annual Health Bulletin 2016. Thimphu (2016).
BNCA. Drug and Controlled Substance Use in Bhutan- at a Glance (Bhutan Narcotic Control Agency and United Nations Office on Drugs and Crime, 2009).
Williams, B. Treating hypertension in patients with diabetes: when to start and how low to go? JAMA 313, 573–574 (2015).
Cheung, B. M. Y. & Li, C. Diabetes and hypertension: is there a common metabolic pathway? Curr. Atheroscler. Rep. 14, 160–166 (2012).
Ferrannini, E. & Cushman, W. C. Diabetes and hypertension: the bad companions. Lancet, 380:601–610 .
WHO. WHO Global InfoBase (Database). (2009).
Leng, B., Jin, Y., Li, G., Chen, L. & Jin, N. Socioeconomic status and hypertension: a meta-analysis. J. Hypertens. 33, 221–229 (2015).
Qin, Z. et al. Association of socioeconomic status with hypertension prevalence and control in nanjing: a cross-sectional study. BMC Public. Health. 22, 423 (2022).
Wang, X. et al. Application of a novel hybrid algorithm of bayesian network in the study of hyperlipidemia related factors: a cross-sectional study. BMC Public. Health. 21, 1375 (2021).
Acknowledgements
The authors would like to acknowledge the Ministry of Health, for allowing us to use the data of STEPS 20192 for this study. We would also like to thank all the study participants.
Funding
This study did not receive any funding. KW is funded by the Australian National Health and Medical Research Council (NHMRC) Investigator Grant (2008697).
Author information
Authors and Affiliations
Contributions
KC and KW conceptualized the idea and analysis plan for this paper. KW performed the statistical analysis and drafted the manuscript. KC was involved in the WHO NCD STEPS survey 2019. Both authors reviewed and approved the final draft of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
The ethical approval for the study was provided by the Research Ethics Board of Health (REBH), Ministry of Health Bhutan vide letter number Ref.No.REBH/PO/2023/005 dated 03/03/2023.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Chhezom, K., Wangdi, K. Determinants of hypertension among Bhutanese adults: evidence from a national WHO STEPS survey. Sci Rep (2026). https://doi.org/10.1038/s41598-026-35911-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-026-35911-w