Abstract
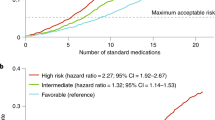
Polypharmacy is increasingly prevalent among people living with HIV (PLWH), especially as they age and manage multiple comorbidities. This cross-sectional study analyzed data from 268 PLWH in Vigo, Spain (2020–2023), revealing an aging cohort (mean age 49.8 years) and a 51.9% prevalence of multimorbidity. Descriptive, bivariate, and multivariable logistic regression analyses were performed. Polypharmacy, defined as the chronic use of ≥ 5 non-antiretroviral drugs, was observed in 35.7% of participants, increasing among older adults (≥ 50 years, 50.7%; p < 0.001) and those living with HIV for > 10 years (43.0%; p = 0.004). Nervous system medications (47.0%), alimentary tract/metabolism drugs (36.2%), and cardiovascular drugs (34.3%) were the most common. Psychotropic drugs were frequent, particularly anxiolytics (24.8%) and antidepressants (22.9%). In multivariable analysis, anxiolytic use was associated with older age (OR = 1.03; p = 0.038), female sex (OR = 1.97; p = 0.042), current smoking (OR = 3.74; p = 0.002), and past cocaine use (OR = 2.52; p = 0.008); antidepressant use with past (OR = 3.46; p = 0.015) and current smoking (OR = 4.46; p = 0.001). These findings highlight the complexity of managing polypharmacy in aging PLWH and underscore the need for strategies to optimize medication use.
Similar content being viewed by others
Data availability
The datasets generated and analyzed during the current study are not publicly available, but are available from the corresponding author on reasonable request. Access will require adherence to appropriate ethical guidelines and approval from the relevant institutional review board.
References
Trickey, A. et al. Life expectancy after 2015 of adults with HIV on long-term antiretroviral therapy in Europe and North America: A collaborative analysis of cohort studies. Lancet HIV 10, e295–e307 (2023).
Mahy, M., Autenrieth, C. S., Stanecki, K. & Wynd, S. Increasing trends in HIV prevalence among people aged 50 years and older. AIDS 28, S453–S459 (2014).
Guaraldi, G., Milic, J. & Mussini, C. Aging with HIV. Curr HIV/AIDS Rep 16, 475–481 (2019).
Zicari, S. et al. Immune activation, inflammation, and non-AIDS Co-morbidities in HIV-infected patients under long-term ART. Viruses 11, 200 (2019).
Feinstein, M. J. et al. Characteristics, prevention, and management of cardiovascular disease in people living with HIV: A scientific statement from the American Heart Association. Circulation 140, (2019).
Van Epps, P. & Kalayjian, R. C. Human immunodeficiency virus and aging in the era of effective antiretroviral therapy. Infect. Dis. Clin. North Am. 31, 791–810 (2017).
Fragkou, P. C. et al. Cardiovascular disease and risk assessment in people living with HIV: Current practices and novel perspectives. Hellenic J. Cardiol. 71, 42–54 (2023).
Collins, L. F. et al. Aging-related comorbidity burden among women and men with or at-risk for HIV in the US, 2008–2019. JAMA Netw. Open 6, e2327584 (2023).
Fuster-RuizdeApodaca, M. J. et al. Prevalence and patterns of illicit drug use in people living with HIV in Spain: A cross-sectional study. PLoS ONE 14, e0211252 (2019).
Remien, R. H. et al. Mental health and HIV/AIDS. AIDS 33, 1411–1420 (2019).
Eshun-Wilson, I. et al. Antidepressants for depression in adults with HIV infection. Cochrane Database Syst. Rev. 2018, (2018).
Mudra Rakshasa-Loots, A. Depression and HIV: a scoping review in search of neuroimmune biomarkers. Brain Commun. 5, (2023).
Mudra Rakshasa-Loots, A., Whalley, H. C., Vera, J. H. & Cox, S. R. Neuroinflammation in HIV-associated depression: evidence and future perspectives. Mol. Psychiatry 27, 3619–3632 (2022).
Earnshaw, V. A. et al. HIV stigma, depressive symptoms, and substance use. AIDS Patient Care STDS 34, 275–280 (2020).
World Health Organization. Medication Safety in Poly-Pharmacy. https ://apps.who.int/iris/bitst ream/handl e/10665 /32545 4/WHO-UHC-SDS-2019.11-eng.pdf?ua=1 (2019).
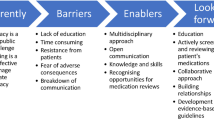
Edelman, E. J., Rentsch, C. T. & Justice, A. C. Polypharmacy in HIV: recent insights and future directions. Curr. Opin. HIV AIDS 15, 126–133 (2020).
Rubin, L. H. et al. Degree of polypharmacy and cognitive function in older women with HIV. AIDS Res. Hum. Retrovir. 38, 571–579 (2022).
Psomas, C. K. et al. Polypharmacy is associated with falls in women with and without HIV. JAIDS J. Acquir. Immune Defic. Syndr. 90, 351–359 (2022).
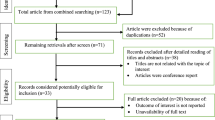
Danjuma, M. I. et al. Prevalence and global trends of polypharmacy among people living with HIV: A systematic review and meta-analysis. Ther. Adv. Drug Saf. 13, 204209862210807 (2022).
López-Centeno, B. et al. Polypharmacy and drug-drug interactions in people living with human immunodeficiency virus in the region of Madrid, Spain: A population-based study. Clin. Infect. Dis. 71, 353–362 (2020).
Paudel, M. et al. Comorbidity and comedication burden among people living with HIV in the United States. Curr. Med. Res. Opin. 38, 1443–1450 (2022).
Gimeno-Gracia, M., Crusells-Canales, M. J., Armesto-Gomez, F. J., Compaired-Turlan, V. & Rabanaque-Hernandez, M. J. Polypharmacy in older adults with human immunodeficiency virus infection compared with the general population. Clin. Interv. Aging 11, 1149–1157 (2016).
Naito, T. et al. Comorbidities and co-medications among 28 089 people living with HIV: A nationwide cohort study from 2009 to 2019 in Japan. HIV Med. 23, 485–493 (2022).
Altice, F. L., Kamarulzaman, A., Soriano, V. V, Schechter, M. & Friedland, G. H. Treatment of medical, psychiatric, and substance-use comorbidities in people infected with HIV who use drugs. The Lancet 376, 367–387 (2010).
Harris, P. A. et al. Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. J. Biomed. Inform. 42, 377–381 (2009).
Harris, P. A. et al. The REDCap consortium: Building an international community of software platform partners. J. Biomed. Inform. 95, 103208 (2019).
Gutiérrez Ibarzábal, M. L., Berraondo Zabalegui, I., Bilbao Madariaga, J. L. & Gorroñogoitia Iturbe, A. I. Análisis y desarrollo del plan de actividades preventivas de atención primaria. Revisión de la oferta preferente y del programa informático de soporte. Vitoria-Gasteiz: Departamento de Sanidad y Consumo, Gobierno Vasco (2011).
Silla Stoel, M. & Rosón Hernández, B. Evaluación del consumo de alcohol y diagnóstico de patrón de consumo. Trastor. Adict. 11, 191–199 (2009).
University of Liverpool. HIV drug interactions. https://www.hivdruginteractions. org.
Smit, M. et al. Future challenges for clinical care of an ageing population infected with HIV: A modelling study. Lancet Infect. Dis. 15, 810–818 (2015).
Subdirección General de Información Sanitaria. Salud Mental en datos: Prevalencia de los Problemas de Salud y Consumo de Psicofármacos y Fármacos Relacionados a Partir de Registros Clínicos de Atención Primaria. https://www.sanidad.gob.es/estadEstudios/estadisticas/estadisticas/estMinisterio/SIAP/Salud_mental_datos.pdf (2021).
Rasmussen, L. et al. Utilization of psychotropic drugs prescribed to persons with and without <scp>HIV</scp> infection: a <scp>D</scp> Anish nationwide population-based cohort study. HIV Med. 15, 458–469 (2014).
Cholera, R. et al. Mind the Gap: Gaps in antidepressant treatment, treatment adjustments, and outcomes among patients in routine HIV care in a multisite U.S. clinical cohort. PLoS One 12, e0166435 (2017).
Kiely, K. M., Brady, B. & Byles, J. Gender, mental health and ageing. Maturitas 129, 76–84 (2019).
Xu, Y. et al. Association between depression and HIV infection vulnerable populations in United States adults: A cross-sectional analysis of NHANES from 1999 to 2018. Front. Public Health 11, (2023).
de Pinho, C. S. N., Santana, R. D., Campos, E. de M. & Pires Neto, R. da J. Prevalence and factors associated with depression in people living with HIV/AIDS in a Brazilian metropolitan region. AIDS Care 34, 1580–1585 (2022).
Mitra, P., Jain, A. & Kim, K. HIV and AIDS in older adults: Neuropsychiatric changes. Curr. Psychiatry Rep. 24, 463–468 (2022).
Skogen, V. et al. Prevalence of mental distress and factors associated with symptoms of major depression among people living with HIV in Norway. AIDS Care 36, 173–180 (2024).
Pérez-Valero, I., Blanch, J. & Martínez, E. Perception of HIV physicians in Spain towards diagnosis and management of neuropsychiatric comorbidities in people with HIV. HIV Med. 23, 969–977 (2022).
Brown, L. A., Mu, W., McCann, J., Durborow, S. & Blank, M. B. Under-documentation of psychiatric diagnoses among persons living with HIV in electronic medical records. AIDS Care 33, 311–315 (2021).
Ballester-Arnal, R. et al. A Spanish study on psychological predictors of quality of life in people with HIV. AIDS Behav. 20, 281–291 (2016).
GeSIDA. Consenso de GeSIDA sobre comorbilidad neuropsiquiátrica – cognitiva y VIH. https://gesida-seimc.org/wp-content/uploads/2020/07/Guia_GESIDA_ManejoClinicoComorbilidad.pdf (2020).
Crane, H. M. et al. Prevalence and factors associated with hazardous alcohol use among persons living with HIV across the US in the current era of antiretroviral treatment. AIDS Behav. 21, 1914–1925 (2017).
Langan, K., Wall, M., Potts, W. & Himelhoch, S. Prevalence and potential predictors of gambling disorder among people living with HIV. AIDS Care 31, 421–426 (2019).
Shiau, S., Arpadi, S. M., Yin, M. T. & Martins, S. S. Patterns of drug use and HIV infection among adults in a nationally representative sample. Addict. Behav. 68, 39–44 (2017).
Fluharty, M., Taylor, A. E., Grabski, M. & Munafò, M. R. The association of cigarette smoking with depression and anxiety: A systematic review. Nicotine Tob. Res. 19, 3–13 (2017).
Fiorentini, A. et al. Substance-induced psychoses: An updated literature review. Front. Psychiatry 12, (2021).
Ma, L., Steinberg, J. L., Moeller, F. G., Johns, S. E. & Narayana, P. A. Effect of cocaine dependence on brain connections: Clinical implications. Expert Rev. Neurother. 15, 1307–1319 (2015).
Mena, Á. Central nervous system disorders in HIV-infected individuals using distinct antiretroviral drugs. AIDS Rev. 23, (2023).
Hoffmann, C. & Llibre, J. M. Neuropsychiatric adverse events with Dolutegravir and other integrase strand transfer inhibitors. AIDS Rev. 21, (2019).
Cid-Silva, P. et al. Clinical experience with the integrase inhibitors Dolutegravir and Elvitegravir in <scp>HIV</scp> -infected patients: Efficacy, safety and tolerance. Basic Clin. Pharmacol. Toxicol. 121, 442–446 (2017).
Elzi, L. et al. Adverse events of raltegravir and dolutegravir. AIDS 31, 1853–1858 (2017).
European Pharmacovigilance Assessment Report. European Medicines Agency (EMA). Prezista. 68–69 https://www.ema.europa.eu/en/documents/product-information/prezista-epar-product-information_en.pdf (2024).
European Public Assessment Report. European Medicines Agency (EMA). Symtuza. 48 https://www.ema.europa.eu/en/documents/product-information/symtuza-epar-product-information_en.pdf (2024).
Altunal, L. N. et al. Prevalence of polypharmacy and potential drug-drug interactions associated with risk factors in the era of HIV integrase inhibitors: A prospective clinical study. AIDS Patient Care STDS 37, 138–145 (2023).
Deutschmann, E. et al. Prevalence of potential drug-drug interactions in patients of the Swiss HIV cohort study in the era of HIV integrase inhibitors. Clin. Infect. Dis. 73, e2145–e2152 (2021).
Acknowledgements
We want to particularly acknowledge the patients and the Biobank at the Galicia Sur Health Research Institute for their collaboration.
Funding
A.L.L. was supported by a Río Hortega contract (CM22/00243) from the Instituto de Salud Carlos III (ISCIII), Spanish Ministry of Science and Innovation. J.A.D. was supported by a predoctoral contract for research training in health (PFIS) (FI23/00006) from the Instituto de Salud Carlos III (ISCIII), Spanish Ministry of Science and Innovation.
Author information
Authors and Affiliations
Contributions
A.L.L. contributed to the formal analysis, investigation, methodology, and writing of the original draft. A.P.G., J.A.D., A.O., C.M., L. M., and N.M.L.C. were responsible for investigation. J.A.A. contributed to methodology. E.P. contributed to conceptualization, investigation, and writing of the original draft. All authors reviewed and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
López López, A., Pérez González, A., Alonso Domínguez, J. et al. High prevalence of polypharmacy and nervous system medications in people with HIV: a cross-sectional analysis. Sci Rep (2026). https://doi.org/10.1038/s41598-026-36832-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-026-36832-4