Abstract
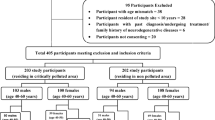
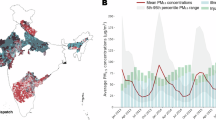
In this study, outpatient data of pediatric neurological diseases together with air pollutants data and meteorological factors were collected in SJZ from 2013 to 2021 to study the correlation between exposure to PM2.5 and pediatric neurological diseases. A Poisson regression GLM was employed to assess the risk associated with both a single time lag and a moving average time lag of 0–7 days. The Poisson regression GLM was evaluated with respect to sex, age, seasons, and disease types. For per IQR (75.2 µg/m3) increase in PM2.5 concentration over a 7-day period (lag07) was correlated with a 2.047% increase in the overall count of pediatric outpatient visits for nervous system-related issues. As PM2.5 concentration increased, its impact was more obvious among girls or children aged < 6 years. Moreover, the adverse effects on nervous systems of children were more pronounced during the warm season (ER: 4.875%). A preliminary exposure assessment revealed a significant correlation between PM2.5 and both the overall outpatient visits for pediatric neurological diseases and the number of various outpatient visits for neurological disorders in children. Additionally, girls < 6 years old were identified as a group particularly sensitive to PM2.5 exposure.
Similar content being viewed by others
Data availability
Ambient air quality data during the study period (PM2.5 , PM10 , O3 , CO, SO2 , NO2 ) were obtained from the China National Urban Air Quality Real-time Publishing Platform (https://air.cnemc.cn:18007/). The meteorological data (e.g., daily average temperature, relative humidity, atmospheric pressure, sunshine duration, and wind speed) during the study period were obtained from the National Meteorological Science Data Center (http://data.cma.cn/). The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
Abbreviations
- SJZ:
-
Shijiazhuang
- GLM:
-
Generalized linear model
- NSDs:
-
Nervous system diseases
- CNS:
-
Central nervous system
- BBB:
-
Blood–brain barrier
- SO2 :
-
Sulfur dioxide
- NO2 :
-
Nitrogen dioxide
- O3 :
-
Ozone
- GLM:
-
Generalized linear model
- ER:
-
Excess risk
- ANOVA:
-
Analysis of variance
- CI:
-
Confidence interval
- IQR:
-
Interquartile range
References
Vos, T. et al. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the global burden of disease study 2019. Lancet 396, 1204–1222. https://doi.org/10.1016/s0140-6736(20)30925-9 (2020).
Wang, Y. et al. Burden of common neurologic diseases in Asian countries, 1990–2019: an analysis for the global burden of disease study 2019. Neurology 100, e2141–e2154. https://doi.org/10.1212/wnl.0000000000207218 (2023).
Wang, Y. et al. Associations of daily mortality with short-term exposure to PM2. 5 and its constituents in Shanghai, China. Chemosphere 233, 879–887. https://doi.org/10.1016/j.chemosphere.2019.05.249 (2019).
Wang, C. et al. Effects of using different exposure data to estimate changes in premature mortality attributable to PM2. 5 and O3 in China. Environ. Pollut. 285, 117242. https://doi.org/10.1016/j.envpol.2021.117242 (2021).
Huang, Y. et al. Exploring health effects under specific causes of mortality based on 90 definitions of PM2. 5 and cold spell combined exposure in Shanghai, China. Environ. Sci. Technol. 57, 2423–2434. https://doi.org/10.1021/acs.est.2c06461.s001 (2023).
Sharma, S., Chandra, M. & Kota, S. H. Health effects associated with PM2. 5: A systematic review. Curr. Pollut Rep. 6, 345–367. https://doi.org/10.1007/s40726-020-00155-3 (2020).
Zhao, H., Wang, Y. & Zhang, Z. Increased ground-level O3 during the COVID-19 pandemic in China aggravates human health risks but has little effect on winter wheat yield. Environ. Pollut. 338, 122713. https://doi.org/10.1016/j.envpol.2023.122713 (2023).
Peng, W., Li, H., Peng, L., Wang, Y. & Wang, W. Effects of particulate matter on hospital admissions for respiratory diseases: an ecological study based on 12.5 years of time series data in Shanghai. Environ. Health. 21, 12. https://doi.org/10.1186/s12940-021-00828-6 (2022).
Hu, J. et al. Fine particulate matter air pollution and subclinical cardiovascular outcomes: A longitudinal study in 15 Chinese cities. Environ. Int. 163, 107218. https://doi.org/10.1016/j.envint.2022.107218 (2022).
Li, D. et al. Multiple organ injury in male C57BL/6J mice exposed to ambient particulate matter in a real-ambient PM exposure system in Shijiazhuang, China. Environ. Pollut. 248, 874–887. https://doi.org/10.1016/j.envpol.2019.02.097 (2019).
Genc, S., Zadeoglulari, Z., Fuss, S. H. & Genc, K. The adverse effects of air pollution on the nervous system. J. Toxicol. 2012 (782462). https://doi.org/10.1155/2012/782462 (2012).
Shin, J., Han, S. H. & Choi, J. Exposure to ambient air pollution and cognitive impairment in community-dwelling older adults: the Korean frailty and aging cohort study. Int. J. Environ. Res. Public. Health. 16, 3767. https://doi.org/10.3390/ijerph16193767 (2019).
Xu, M., Zhu, Y., Chang, H. & Liang, Y. Nanoceria restrains PM2. 5-induced metabolic disorder and hypothalamus inflammation by Inhibition of astrocytes activation related NF-κB pathway in Nrf2 deficient mice. Adv. Free Radical Biol. Med. 99, 259–272. https://doi.org/10.1016/j.freeradbiomed.2016.08.021 (2016).
Fu, P., Guo, X., Cheung, F. M. H. & Yung, K. K. L. The association between PM2. 5 exposure and neurological disorders: a systematic review and meta-analysis. Sci. Total Environ. 655, 1240–1248. https://doi.org/10.1016/j.scitotenv.2018.11.218 (2019).
Cipriani, G., Danti, S., Carlesi, C. & Borin, G. Danger in the air: air pollution and cognitive dysfunction. Am. J. Alzheimers Dis. Other Dementias. 33, 333–341. https://doi.org/10.1177/1533317518777859 (2018).
Zanobetti, A., Dominici, F., Wang, Y. & Schwartz, J. D. A National case-crossover analysis of the short-term effect of PM2. 5 on hospitalizations and mortality in subjects with diabetes and neurological disorders. Environ. Health. 13, 38. https://doi.org/10.1186/1476-069X-13-38 (2014).
Armas, F. V. & D’Angiulli, A. Neuroinflammation and neurodegeneration of the central nervous system from air pollutants: A scoping review. Toxics 10, 666. https://doi.org/10.3390/toxics10110666 (2022).
Zhu, X. et al. Risks of hospital admissions from a spectrum of causes associated with particulate matter pollution. Sci. Total Environ. 656, 90–100. https://doi.org/10.1016/j.scitotenv.2018.11.240 (2019).
Cheng, J., Su, H., Song, J. & Wang, X. Short-term effect of air pollution on childhood epilepsy in Eastern china: a space–time-stratified case-crossover and pooled analysis. Environ. Int. 170, 107591. https://doi.org/10.1016/j.envint.2022.107591 (2022).
Tokuda, N. et al. Association of air pollution exposure during pregnancy and early childhood with children’s cognitive performance and behavior at age six. Environ. Res. 236, 116733. https://doi.org/10.1016/j.envres.2023.116733 (2023).
Julvez, J. et al. Early life multiple exposures and child cognitive function: A multi-centric birth cohort study in six European countries. Environ. Pollut. 284, 117404. https://doi.org/10.1016/j.envpol.2021.117404 (2021).
Li, M., Huang, T., Zhang, S. & Li, D. Effects of household indoor air pollution on children’s cognitive function: a systematic review. Chin. J. Women Child. Health. 14, 22–29. https://doi.org/10.19757/j.cnki.issn1674-7763.2023.06.005 (2023).
Calderón Garcidueñas, L., Kulesza, R. J., Doty, R. L. & D’Angiulli, A. Torres-Jardón, R. Megacities air pollution problems: Mexico City metropolitan area critical issues on the central nervous system pediatric impact. Environ. Res. 137, 157–169. https://doi.org/10.1016/j.envres.2014.12.012 (2015).
Cainelli, E., Vedovelli, L., Trevisanuto, D., Suppiej, A. & Bisiacchi, P. Prospective assessment of early developmental markers and their association with neuropsychological impairment. Eur. J. Pediatr. 182, 5181–5189. https://doi.org/10.1007/s00431-023-05182-y (2023).
Sun, H. et al. Platelet mitochondrial DNA methylation as epigenetic biomarker of short-term air pollution exposure in healthy subjects. Front. Mol. Biosci. 8, 803488. https://doi.org/10.3389/fmolb.2021.803488 (2022).
Gao, A. et al. Health and economic losses attributable to PM2. 5 and Ozone exposure in Handan, China. Air Qual. Atmos. Health. 14, 605–615. https://doi.org/10.1007/s11869-020-00964-x (2021).
Zhang, Q. et al. Overview of particulate air pollution and human health in china: Evidence, challenges, and opportunities. Innovation 3 https://doi.org/10.1016/j.xinn.2022.100312 (2022).
Moshammer, H. et al. Acute effects of air pollution and noise from road traffic in a panel of young healthy adults. Int. J. Environ. Res. Public. Health. 16, 788. https://doi.org/10.3390/ijerph16050788 (2019).
Bhaskaran, K., Gasparrini, A., Hajat, S., Smeeth, L. & Armstrong, B. Time series regression studies in environmental epidemiology. Int. J. Epidemiol. 42, 1187–1195. https://doi.org/10.1093/ije/dyt092 (2013).
Dominici, F., Sheppard, L. & Clyde, M. Health effects of air pollution: a statistical review. Int. Stat. Rev. 71, 243–276. https://doi.org/10.1111/j.1751-5823.2003.tb00195.x (2003).
Vatcheva, K. P., Lee, M., McCormick, J. B. & Rahbar, M. H. Multicollinearity in regression analyses conducted in epidemiologic studies. Epidemiol. (Sunnyvale Calif). 6, 227. https://doi.org/10.4172/2161-1165.1000227 (2016).
Liu, X. et al. Neurodevelopmental toxicity induced by PM2. 5 exposure and its possible role in neurodegenerative and mental disorders. Hum. Exp. Toxicol. 42, 09603271231191436. https://doi.org/10.1177/09603271231191436 (2023).
Liu, F. et al. Neurotoxicity of the air-borne particles: from molecular events to human diseases. J. Hazard. Mater. 457, 131827. https://doi.org/10.1016/j.jhazmat.2023.131827 (2023).
Qin, S. et al. Neurotoxicity of fine and ultrafine particulate matter: A comprehensive review using a toxicity pathway-oriented adverse outcome pathway framework. Sci. Total Environ. 947, 174450. https://doi.org/10.1016/j.scitotenv.2024.174450 (2024).
Aderinto, N. et al. The impact of air pollution on neurodegenerative diseases: a narrative review of current evidence. Egypt. J. Intern. Med. 37 https://doi.org/10.1186/s43162-025-00403-2 (2025).
Zeka, A., Zanobetti, A. & Schwartz, J. Individual-level modifiers of the effects of particulate matter on daily mortality. Am. J. Epidemiol. 163, 849–859. https://doi.org/10.1093/aje/kwj116 (2006).
Picillo, M. et al. The relevance of gender in parkinson’s disease: a review. J. Neurol. 264, 1583–1607. https://doi.org/10.1007/s00415-016-8384-9 (2017).
Lenroot, R. K. & Giedd, J. N. Brain development in children and adolescents: insights from anatomical magnetic resonance imaging. Neurosci. Biobehav Rev. 30, 718–729. https://doi.org/10.1016/j.neubiorev.2006.06.001 (2006).
Ni, Y. et al. Associations of pre-and postnatal air pollution exposures with child behavioral problems and cognitive performance: a US multi-cohort study. Environ. Health Perspect. 130, 067008. https://doi.org/10.1289/EHP10248 (2022).
Zhang, Y. et al. Genetic and epigenetic susceptibility of airway inflammation to PM2. 5 in school children: new insights from quantile regression. Environ. Health. 16, 88. https://doi.org/10.1186/s12940-017-0285-6 (2017).
Calderón Garcidueñas, L. et al. Air pollution, combustion and friction derived nanoparticles, and alzheimer’s disease in urban children and young adults. J. Alzheimers Dis. 70, 343–360. https://doi.org/10.3233/JAD-190331 (2019).
Cory-Slechta, D. A., Merrill, A. & Sobolewski, M. Air pollution–related neurotoxicity across the life span. Annu. Rev. Pharmacol. Toxicol. 63, 143–163. https://doi.org/10.1146/annurev-pharmtox-051921-020812 (2023).
Kim, H., Kim, W. H., Kim, Y. Y. & Park, H. Y. Air pollution and central nervous system disease: a review of the impact of fine particulate matter on neurological disorders. Front. Public. Health. 8, 575330. https://doi.org/10.3389/fpubh.2020.575330 (2020).
Kang, Y. J., Tan, H. Y., Lee, C. Y. & Cho, H. An air particulate pollutant induces neuroinflammation and neurodegeneration in human brain models. Adv. Sci. 8, 2101251. https://doi.org/10.1002/advs.202101251 (2021).
Calderón-Garcidueñas, L. et al. Prefrontal white matter pathology in air pollution exposed Mexico City young urbanites and their potential impact on neurovascular unit dysfunction and the development of alzheimer’s disease. Environ. Res. 146, 404–417. https://doi.org/10.1016/j.envres.2015.12.031 (2016).
Vlachogiannis, D. M., Xu, Y., Jin, L. & González, M. C. Correlation networks of air particulate matter (PM2.5): a comparative study. Appl. Netw. Sci. 6, 32. https://doi.org/10.1007/s41109-021-00373-8 (2021).
Qiu, H., Wang, L., Zhou, L. & Pan, J. Coarse particles (PM2. 5–10) and cause-specific hospitalizations in Southwestern china: Association, attributable risk and economic costs. Environ. Res. 190, 110004. https://doi.org/10.1016/j.envres.2020.110004 (2020).
Culqui, D., Linares, C., Ortiz, C., Carmona, R. & Díaz, J. Association between environmental factors and emergency hospital admissions due to alzheimer’s disease in Madrid. Sci. Total Environ. 592, 451–457. https://doi.org/10.1016/j.scitotenv.2017.03.089 (2017).
Chen, J. et al. Association between temperature variability and global meningitis incidence. Environ. Int. 171, 107649. https://doi.org/10.1016/j.envint.2022.107649 (2023).
Lee, H. et al. Ambient air pollution exposure and risk of migraine: synergistic effect with high temperature. Environ. Int. 121, 383–391. https://doi.org/10.1016/j.envint.2018.09.022 (2018).
Wan, D., Du, L. & Song, L. Research progress in relationships and mechanisms between fine particles and nervous system diseases. Mil Med. Sci. 47, 544–550 (2023).
Cakmak, S., Dales, R. E. & Vidal, C. B. Air pollution and hospitalization for epilepsy in Chile. Environ. Int. 36, 501–505. https://doi.org/10.1016/j.envint.2010.03.008 (2010).
Liang, Z. et al. The association between short-term ambient air pollution and daily outpatient visits for schizophrenia: a hospital-based study. Environ. Pollut. 244, 102–108. https://doi.org/10.1016/j.envpol.2018.09.142 (2019).
Acknowledgements
We thank LetPub (www.letpub.com.cn) for its linguistic assistance during the preparation of this manuscript.
Funding
This work was supported by Medical Science Research Project of Hebei (No. 20250203).
Author information
Authors and Affiliations
Contributions
Z. L. and A. G. conducted relevant research and wrote the paper, Y. Z. was responsible for determining the research direction, conducting academic review and revision of the manuscript, and provided guidance on experimental design and data analysis methods. H. K., F. C., H. M., X. Z., X. S., X. Y., Y. S. assisted in conducting research and revised the paper together.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Liang, Z., Gao, A., Kang, H. et al. Short-term effect of PM2.5 exposure on pediatric neurological outpatient visits in Shijiazhuang China 2013–2021. Sci Rep (2026). https://doi.org/10.1038/s41598-026-36877-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-026-36877-5