Abstract
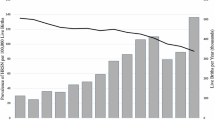
We aimed to describe the magnitude and population burden of inequality in adverse birth outcomes by maternal education (five categories). Data from 639,007 singleton births of gestational age ≥ 24 weeks or, if missing, birthweight ≥ 500 g were included from the National registry of the Netherlands, 2016–2019. One in six Dutch births had an adverse outcome. Each step down the educational ladder was associated with higher adverse outcome rates. Inequalities in stillbirth and neonatal mortality rates were large between the highest (Master’s or higher) and lowest (primary) educated groups (rate ratio [RR] = 2.94 [95%CI: 2.33–3.55] and 2.25 [1.71–2.79], respectively). Inequalities were smaller for preterm birth, small-for-gestational-age, low Apgar score, neonatal intensive care unit admission, and severe congenital anomalies (RR range = 1.32–1.77; PAF range = 13.8–17.7%). Mortality would reduce by a third if the entire population had the mortality rates of the highest educated (population attributable fraction [PAF]stillbirth=35.0% [24.4–45.6%]; PAFneonatal mortality=27.1% [14.4–39.7%]). The middle education category (higher secondary) was the largest group, contributing most to the population burden of inequality despite only having a moderately elevated risk of adverse outcomes. Population health gains would be largest if addressed through preventive approaches targeting the entire health gradient rather than by only focussing on those at highest risk.
Similar content being viewed by others
Data availability
The data that has been used is confidential. Access to the DIAPER linked data-infrastructure can be requested by contacting [diaper@rivm.nl] , access to Perined data can be requested by contacting [info@perined.nl] , and access to the CBS microdata can be requested by following the instructions at [https://www.cbs.nl/en-gb/our-services/customised-services-microdata/microdata-conducting-your-own-research/applying-for-access-to-microdata] .
References
Marmot, M., Friel, S., Bell, R., Houweling, T. A. & Taylor, S. Closing the gap in a generation: health equity through action on the social determinants of health. Lancet 372(9650), 1661–1669. https://doi.org/10.1016/S0140-6736(08)61690-6 (2008).
Kuh, D. & Ben-Schlomo, Y. (eds) A Life Course Approach To Chronic Disease Epidemiology 1st edn (Oxford University Press, 1997).
Shenkin, S. D., Starr, J. M. & Deary, I. J. Birth weight and cognitive ability in childhood: A systematic review. Psychol. Bull. 130(6), 989–1013. https://doi.org/10.1037/0033-2909.130.6.989 (2004).
Silva, A., Metha, Z. & O’Callaghan, F. J. The relative effect of size at Birth, postnatal growth and social factors on cognitive function in late childhood. Ann. Epidemiol. 16(6), 469–476. https://doi.org/10.1016/j.annepidem.2005.06.056 (2006).
Oudgenoeg-Paz, O., Mulder, H., Jongmans, M. J., van der Ham, I. J. M. & Van der Stigchel, S. The link between motor and cognitive development in children born preterm and/or with low birth weight: A review of current evidence. Neurosci. Biobehav Rev. 80, 382–393. https://doi.org/10.1016/j.neubiorev.2017.06.009 (2017).
Pillas, D. et al. Social inequalities in early childhood health and development: a European-wide systematic review. Pediatr. Res. 76(5), 418–424. https://doi.org/10.1038/pr.2014.122 (2014).
Houweling, T. A. J. & Grünberger, I. Intergenerational transmission of health inequalities: research agenda for a life course approach to socioeconomic inequalities in health. J. Epidemiol. Commun. H. https://doi.org/10.1136/jech-2022-220163 (2023).
Mackenbach, J. P. & Kunst, A. E. Measuring the magnitude of socio-economic inequalities in health: an overview of available measures illustrated with two examples from Europe. Soc. Sci. Med. 44(6), 757–771. https://doi.org/10.1016/S0277-9536(96)00073-1 (1997).
Rom, A. L. et al. A comparative study of educational inequality in the risk of stillbirth in Denmark, Finland, Norway and Sweden 1981–2000. J. Epidemiol. Community Health (1978). 66(3), 240–246. https://doi.org/10.1136/jech.2009.101188 (2012).
Mortensen, L. H., Diderichsen, F., Smith, G. D. & Andersen, A. M. N. Time is on whose side? Time trends in the association between maternal social disadvantage and offspring fetal growth. A study of 1 409 339 births in Denmark, 1981–2004. J. Epidemiol. Community Health (1978). 63(4), 281–285. https://doi.org/10.1136/jech.2008.076364 (2009).
Mortensen, L. H. et al. Social inequality in fetal growth: a comparative study of Denmark, Finland, Norway and Sweden in the period 1981–2000. J. Epidemiol. Community Health (1978). 62(4), 325–331. https://doi.org/10.1136/jech.2007.061473 (2008).
Petersen, C. B. et al. Socio-economic inequality in preterm birth: a comparative study of the nordic countries from 1981 to 2000. Paediatr. Perinat. Epidemiol. 23(1), 66–75. https://doi.org/10.1111/j.1365-3016.2008.00977.x (2009).
Currie, J. & Gruber, J. Public health insurance and medical treatment: the equalizing impact of the medicaid expansions. J. Public. Econ. 82(1), 63–89. https://doi.org/10.1016/S0047-2727(00)00140-7 (2001).
Rauscher, E. & Rangel, D. E. Rising inequality of infant health in the U.S. SSM Popul. Health. 12, 100698. https://doi.org/10.1016/j.ssmph.2020.100698 (2020).
Aizer, A. & Currie, J. The intergenerational transmission of inequality: maternal disadvantage and health at birth. Sci. (1979). 344(6186), 856–861. https://doi.org/10.1126/science.1251872 (2014).
Jansen, P. W. et al. Explaining educational inequalities in birthweight: the generation R study. Paediatr. Perinat. Epidemiol. 23(3), 216–228. https://doi.org/10.1111/j.1365-3016.2009.01023.x (2009).
van den Berg, G., van Eijsden, M., Vrijkotte, T. G. M. & Gemke, R. J. B. J. Educational inequalities in perinatal outcomes: the mediating effect of smoking and environmental tobacco exposure. PLoS One. 7(5), e37002. https://doi.org/10.1371/journal.pone.0037002 (2012).
Ruiz, M. et al. Mother’s education and the risk of preterm and small for gestational age birth: a DRIVERS meta-analysis of 12 European cohorts. J. Epidemiol. Community Health (1978). 69(9), 826–833. https://doi.org/10.1136/jech-2014-205387 (2015).
Jaddoe, V. W. V. et al. The generation R study: design and cohort profile. Eur. J. Epidemiol. 21(6), 475–484. https://doi.org/10.1007/s10654-006-9022-0 (2006).
Bertens, L. C. M., Burgos Ochoa, L., Van Ourti, T., Steegers, E. A. P. & Been, J. V. Persisting inequalities in birth outcomes related to neighbourhood deprivation. J. Epidemiol. Community Health (1978). 74(3), 232–239. https://doi.org/10.1136/jech-2019-213162 (2020).
Burgos Ochoa, L. et al. Association of neighbourhood socioeconomic trajectories with preterm birth and small-for-gestational-age in the netherlands: a nationwide population-based study. Lancet Reg. Health - Europe. 10, 100205. https://doi.org/10.1016/j.lanepe.2021.100205 (2021).
Vos, A. A., Posthumus, A. G., Bonsel, G. J., Steegers, E. A. P. & Denktaş, S. Deprived neighborhoods and adverse perinatal outcome: a systematic review and meta-analysis. Acta Obstet. Gynecol. Scand. 93(8), 727–740. https://doi.org/10.1111/aogs.12430 (2014).
Vos, A. A., Denktaş, S., Borsboom, G. J., Bonsel, G. J. & Steegers, E. A. Differences in perinatal morbidity and mortality on the neighbourhood level in Dutch municipalities: a population based cohort study. BMC Pregnancy Childbirth. 15(1), 201. https://doi.org/10.1186/s12884-015-0628-7 (2015).
Agyemang, C. et al. The effect of neighbourhood income and deprivation on pregnancy outcomes in Amsterdam, the Netherlands. J. Epidemiol. Community Health (1978). 63(9), 755–760. https://doi.org/10.1136/jech.2008.080408 (2009).
Poeran, J., Denktas, S., Birnie, E., Bonsel, G. J. & Steegers, E. A. P. Urban perinatal health inequalities. J. Maternal-Fetal Neonatal Med. 24(4), 643–646. https://doi.org/10.3109/14767058.2010.511341 (2011).
Stafford, M., Duke-Williams, O. & Shelton, N. Small area inequalities in health: are we underestimating them? Soc. Sci. Med. 67(6), 891–899. https://doi.org/10.1016/j.socscimed.2008.05.028 (2008).
de Kluiver, E., Offringa, M., Walther, F. J., Duvekot, J. J. & de Laat, M. W. M. Perinataal Beleid Bij extreme vroeggeboorte. Ned Tijdschr Geneeskd. A6362, 154 (2013).
Van de Voorde, P. et al. European resuscitation Council guidelines 2021: paediatric life support. Resuscitation 161, 327–387. https://doi.org/10.1016/j.resuscitation.2021.02.015 (2021).
Perined Perinatale zorg in Nederland anno 2020 [Internet]. Utrecht (2021).
Prins, K. Population register data, basis for the Netherlands population statistics. Statistics Netherlands (2017).
Scheefhals, Z. T. M., De Vries, E. F., Molenaar, J. M., Numans, M. E. & Struijs, J. N. Observational data for integrated maternity care: experiences with a data-Infrastructure for parents and children in the Netherlands. Int. J. Integr. Care. 23, 20. https://doi.org/10.5334/ijic.7012 (2023).
Hoftiezer, L. et al. From population reference to National standard: new and improved birthweight charts. Am. J. Obstet. Gynecol. 220(4), 383.e1-383.e17. https://doi.org/10.1016/j.ajog.2018.12.023 (2019).
Prins, M., van Roosmalen, J., Smit, Y., Scherjon, S. & van Dillen, J. Praktische Verloskunde (Bohn Stafleu van Loghum, 2019). https://doi.org/10.1007/978-90-368-2279-4
UNESCO Institute for Statistics. International Standard Classification of Education: ISCED 2011 (Montreal, 2012).
van Buuren, S. & Groothuis-Oudshoorn, K. Mice: multivariate imputation by chained equations in R. J. Stat. Softw. 45(3). https://doi.org/10.18637/jss.v045.i03 (2011).
Rubin, D. B. Multiple Imputation for Nonresponse in Surveys (Wiley, 1987). https://doi.org/10.1002/9780470316696
Kozuki, N. et al. The associations of parity and maternal age with small-for-gestational-age, preterm, and neonatal and infant mortality: a meta-analysis. BMC Public. Health. 13(S3), S2. https://doi.org/10.1186/1471-2458-13-S3-S2 (2013).
Brady, A. Adjusted population attributable fractions from logistic regression. Stata Tech. Bull. 42, 8–12 (1998).
R Core Team. R: A Language and Environment for Statistical Computing. R Foundation for Statistical Computing, Vienna, Austria. https://www.R-project.org/ (2021).
Rose, G. Strategy of prevention: lessons from cardiovascular disease. BMJ 282(6279), 1847–1851. https://doi.org/10.1136/bmj.282.6279.1847 (1981).
McCowan, L. & Horgan, R. P. Risk factors for small for gestational age infants. Best Pract. Res. Clin. Obstet. Gynaecol. 23(6), 779–793. https://doi.org/10.1016/j.bpobgyn.2009.06.003 (2009).
Reno, R. & Hyder, A. The evidence base for social determinants of health as risk factors for infant mortality: A systematic scoping review. J. Health Care Poor Underserved. 29(4), 1188–1208. https://doi.org/10.1353/hpu.2018.0091 (2018).
Flenady, V. et al. Major risk factors for stillbirth in high-income countries: a systematic review and meta-analysis. Lancet 377(9774), 1331–1340. https://doi.org/10.1016/S0140-6736(10)62233-7 (2011).
Vogel, J. P. et al. The global epidemiology of preterm birth. Best Pract. Res. Clin. Obstet. Gynaecol. 52, 3–12. https://doi.org/10.1016/j.bpobgyn.2018.04.003 (2018).
Silva, L. M. et al. Maternal educational level and risk of gestational hypertension: the generation R study. J. Hum. Hypertens. 22(7), 483–492. https://doi.org/10.1038/jhh.2008.22 (2008).
Silva, L. M. et al. Mother’s educational level and fetal growth: the genesis of health inequalities. Int. J. Epidemiol. 39(5), 1250–1261. https://doi.org/10.1093/ije/dyq069 (2010).
Baron, R. et al. Socio-demographic inequalities across a range of health status indicators and health behaviours among pregnant women in prenatal primary care: a cross-sectional study. BMC Pregnancy Childbirth. 15(1), 261. https://doi.org/10.1186/s12884-015-0676-z (2015).
Field, T. Prenatal depression risk Factors, developmental effects and interventions: A review. J. Pregnancy Child. Health. 04(01). https://doi.org/10.4172/2376-127X.1000301 (2017).
Holowko, N., Mishra, G. & Koupil, I. Social inequality in excessive gestational weight gain. Int. J. Obes. 38(1), 91–96. https://doi.org/10.1038/ijo.2013.62 (2014).
Camier, A. et al. Social inequalities in prenatal folic acid supplementation: results from the ELFE cohort. Nutrients 11(5), 1108. https://doi.org/10.3390/nu11051108 (2019).
Houweling, T. A. J. & Grünberger, I. Intergenerational transmission of health inequalities: towards a life course approach to socioeconomic inequalities in health – a review. J. Epidemiol. Community Health (1978). https://doi.org/10.1136/jech-2022-220162
Pearce, A. et al. Causal mediation approaches for Understanding pathways to inequalities and policy entry points: examples from early years health and development. J. Epidemiol. Community Health (1978). jech-2025-224260 https://doi.org/10.1136/jech-2025-224260 (2025).
Morton, S. M., de Stavola, B. L. & Leon, D. A. Intergenerational determinants of offspring size at birth: a life course and graphical analysis using the Aberdeen children of the 1950s study (ACONF). Int. J. Epidemiol. 43(3), 749–759. https://doi.org/10.1093/ije/dyu028 (2014).
Naylor, R. & Mifsud, N. Structural Inequality in Higher Education: Creating Institutional Cultures that Enable all Students (Perth, 2019).
Siddiqi, A., Irwin, L. & Hertzman, C. Total environment assessment model for early child development. WHO organisation mondiale de la santé. (2007).
Grunberg, V. A., Geller, P. A., Bonacquisti, A. & Patterson, C. A. NICU infant health severity and family outcomes: a systematic review of assessments and findings in psychosocial research. J. Perinatol. 39(2), 156–172. https://doi.org/10.1038/s41372-018-0282-9 (2019).
Kraljevic, M. & Warnock, F. F. Early educational and behavioral RCT interventions to reduce maternal symptoms of psychological trauma following preterm birth. J. Perinat. Neonatal Nurs. 27(4), 311–327. https://doi.org/10.1097/JPN.0b013e3182a8bfe2 (2013).
Bergstra, A. D., Brunekreef, B. & Burdorf, A. The influence of industry-related air pollution on birth outcomes in an industrialized area. Environ. Pollut. 269, 115741. https://doi.org/10.1016/j.envpol.2020.115741 (2021).
Sonnenschein-van der Voort, A. M. et al. Air pollution, fetal and infant tobacco smoke exposure, and wheezing in preschool children: a population-based prospective birth cohort. Environ. Health. 11(1), 91. https://doi.org/10.1186/1476-069X-11-91 (2012).
Acknowledgements
We thank Jeroen Struijs and Anouk Klootwijk for granting access to their DIAPER linked data-infrastructure (29).
Funding
This work was funded by a grant from the Dutch Research Council (NWO grant number NWA.1238.18.001).
Author information
Authors and Affiliations
Contributions
A.S., W.K., and T.A.J.H. conceptualized and designed the study, A.S. and R.M.K.D. prepared the data, D.K., L.B., A.N.R., W.K. and T.A.J.H. supervised data preparation and analyses, A.S. carried out the analyses, A.S. and T.A.J.H. drafted the initial manuscript, and all authors critically reviewed, revised, and approved the manuscript as submitted and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
The proposal for this study was reviewed by the Medical Ethics Committee (METC) of Erasmus MC, Rotterdam, The Netherlands.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Schreuder, A., van Klaveren, D., van Dijk, R.M.K. et al. The magnitude and population burden of educational inequalities in adverse birth outcomes. Sci Rep (2026). https://doi.org/10.1038/s41598-026-37601-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-026-37601-z