Abstract
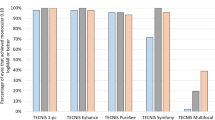
In this single-center retrospective study, we compared visual performance and optical quality between a new refractive extended depth-of-focus intraocular lens (EDoF IOL, Model ZEN00V, n = 44), with a slightly myopic target, and an enhanced monofocal IOL (Model ICB00, n = 44), with the target refraction closest to emmetropia on the myopic side. The IOL power for the EDoF IOL was selected to achieve postoperative refraction of -0.50 to -1.00 D. Monocular distance visual acuity (VA) and iTrace aberrometry were assessed. Bilateral cases were analyzed to evaluate intermediate and near VA, and photic phenomena. Preoperative target diopter and postoperative spherical equivalent were more myopic in the EDoF IOL group than in the monofocal IOL group (all p < 0.001). Uncorrected and corrected distance VA were comparable between the two groups (all p > 0.05). Higher order aberrations were comparable between the two groups (all p > 0.05) except for spherical aberrations, which were lower in the monofocal group (p = 0.002). Subgroup analysis revealed superior near VA (p = 0.02) and an extended range of defocus in the EDoF IOL group with comparable photic phenomena. Implantation of the new refractive EDoF IOL, the TECNIS PureSee™, with myopic target diopter may be a viable option for improving intermediate and near visual performance while preserving distance vision and visual quality.
Similar content being viewed by others
Data availability
The datasets used during the current study are available from the corresponding author on reasonable request. All data generated or analyzed during this study are included in this published article.
Abbreviations
- ACD:
-
Anterior chamber depth
- AL:
-
Axial length
- CCT:
-
Central corneal thickness
- CDVA:
-
Corrected distance visual acuity
- D:
-
Diopter
- ETDRS:
-
Early treatment diabetic retinopathy study
- EDoF IOL:
-
Extended depth-of-focus intraocular lens
- HOA:
-
High-order aberration
- IOL:
-
Intraocular lens
- logMAR:
-
Logarithm of the minimum angle of resolution
- RMS:
-
Root mean square
- UDVA:
-
Uncorrected distance
- VA:
-
Visual acuity
- WTW:
-
White-to-white
- SE:
-
Spherical equivalent
References
Obstbaum, S. A. Utilization, appropriate care, and quality of life for patients with cataracts: American academy of ophthalmology, American society of cataract and refractive surgery, and European society of cataract and refractive surgeons. Ophthalmology 113(10), 1878–1882. https://doi.org/10.1016/j.ophtha.2006.07.016 (2006).
Congdon, N. et al. Causes and prevalence of visual impairment among adults in the United States. Arch. Ophthalmol. 122(4), 477–485. https://doi.org/10.1001/archopht.122.4.477 (2004).
Gonglore, B. & Smith, R. Extracapsular cataract extraction to phacoemulsification: Why and how?. Eye 12(6), 976–982. https://doi.org/10.1038/eye.1998.253 (1998).
Minassian, D. C. et al. Extracapsular cataract extraction compared with small incision surgery by phacoemulsification: A randomised trial. Br. J. Ophthalmol. 85(7), 822–829. https://doi.org/10.1136/bjo.85.7.822 (2001).
Atima, M. O. et al. Long-term outcomes of phacoemulsification surgeries at ECWA eye hospital: A prospective clinical cohort study. J. Ophthalmol. 2024(1), 2562064. https://doi.org/10.1155/2024/2562064 (2024).
Nanavaty, M. A. Evolving generation of new extended depth of focus intraocular lenses. Eye 38(Suppl 1), 1–3 (2024).
Kanclerz, P., Toto, F., Grzybowski, A. & Alio, J. L. Extended depth-of-field intraocular lenses: an update. Asia-Pacific J. Ophthalmol. 9(3), 194–202 (2020).
Galvis, V. et al. Visual and satisfaction results with implantation of the trifocal Panoptix® intraocular lens in cataract surgery. J. Optometry 15(3), 219–227 (2022).
D. Zamora-de La Cruz, J. Bartlett, M. Gutierrez, S.M. Ng, Trifocal intraocular lenses versus bifocal intraocular lenses after cataract extraction among participants with presbyopia, Cochrane Database Syst. Rev. (1) (2023).
Kawamura, J. et al. Comparison of visual performance between diffractive bifocal and diffractive trifocal intraocular lenses. Sci. Rep. 14(1), 5292 (2024).
Zhuo, B. et al. Binocular visual performance and optical quality of trifocal intraocular lens in Chinese patients with high myopic cataract. PLoS ONE 20(8), e0330473 (2025).
de Vries, N. E. et al. Dissatisfaction after implantation of multifocal intraocular lenses. J. Cataract Refract. Surg. 37(5), 859–865. https://doi.org/10.1016/j.jcrs.2010.11.032 (2011).
Masket, S. et al. Symptoms and satisfaction levels associated with intraocular lens implants in the monofocal and premium IOL patient-reported outcome measure study. Ophthalmology 130(7), 726–734. https://doi.org/10.1016/j.ophtha.2023.02.027 (2023).
Breyer, D. R. et al. Multifocal intraocular lenses and extended depth of focus intraocular lenses. Asia-Pacific J. Ophthalmol. 6(4), 339–349 (2017).
Montrimas, A., Žemaitienė, R., Yao, K. & Grzybowski, A. Chord mu and chord alpha as postoperative predictors in multifocal intraocular lens implantation. Graefe’s Arch. Clin. Exp. Ophthalmol. 262(2), 367–380 (2024).
J.J. Moreno, V. Galvis, M. Salazar, J.S. Villamizar, N. Leal, A. Tello, Presentation of a New Method for Quantitative Determination of Trifocal Intraocular Lens Decentration, Ceska a slovenska oftalmologie: casopis Ceske oftalmologicke spolecnosti a Slovenske oftalmologicke spolecnosti 81 (Ahead of Print) (2025) 1–12.
Rampat, R. & Gatinel, D. Multifocal and extended depth-of-focus intraocular lenses in 2020. Ophthalmology 128(11), e164–e185 (2021).
MacRae, S. et al. Special report: American academy of ophthalmology task force consensus statement for extended depth of focus intraocular lenses. Ophthalmology 124(1), 139–141 (2017).
Chang, D. H. et al. Visual outcomes and safety of an extended depth-of-focus intraocular lens: Results of a pivotal clinical trial. J. Cataract. Refract. Surg. 48(3), 288–297. https://doi.org/10.1097/j.jcrs.0000000000000747 (2022).
Zhong, Y., Wang, K., Yu, X., Liu, X. & Yao, K. Comparison of trifocal or hybrid multifocal-extended depth of focus intraocular lenses: A systematic review and meta-analysis. Sci. Rep. 11(1), 6699. https://doi.org/10.1038/s41598-021-86222-1 (2021).
Kenia, V. P., Kenia, R. V., Mudaliya, L. & Pirdankar, O. H. Visual outcomes and higher-order aberrations in eyes implanted with hybrid extended depth of focus intraocular lens. Taiwan J. Ophthalmol. 13(3), 341–345. https://doi.org/10.4103/tjo.tjo_16_22 (2023).
S. Tavassoli, H. Ziaei, M.E. Yadegarfar, A. Gokul, A. Kernohan, J.R. Evans, M. Ziaei, Trifocal versus extended depth of focus (EDOF) intraocular lenses after cataract extraction, Cochrane Database Syst. Rev. (7) (2024).
Alarcon, A. et al. Optical and clinical simulated performance of a new refractive extended depth of focus intraocular lens. Eye 38(Suppl 1), 4–8 (2024).
Corbett, D. et al. Quality of vision clinical outcomes for a new fully-refractive extended depth of focus Intraocular Lens. Eye 38(1), 9–14. https://doi.org/10.1038/s41433-024-03039-8 (2024).
Kim, D. Y. et al. Comparative outcomes of the next-generation extended depth-of-focus intraocular lens and enhanced monofocal intraocular lens in cataract surgery. J. Clin. Med. 14(14), 4967 (2025).
Bernardes, J., Raimundo, M., Lobo, C. & Murta, J. N. A comparison of intraocular lens power calculation formulas in high myopia. J. Refract. Surg. 37(3), 207–211 (2021).
Stopyra, W., Langenbucher, A. & Grzybowski, A. Intraocular lens power calculation formulas—A systematic review. Ophthalmol. Therapy 12(6), 2881–2902 (2023).
Holladay, J. T. et al. The relationship of visual acuity, refractive error, and pupil size after radial keratotomy. Arch. Ophthalmol. 109(1), 70–76 (1991).
R. Schmid, A.F. Borkenstein, Optical bench evaluation of the latest refractive enhanced depth of focus intraocular lens, Clin. Ophthalmol. (2024) 1921–1932.
Alfonso-Bartolozzi, B. et al. Optical and visual outcomes of a new refractive extended depth of focus intraocular lens. J. Refract. Surg. 41(4), e333–e341 (2025).
Megiddo-Barnir, E. & Alió, J. L. Latest development in extended depth-of-focus intraocular lenses: an update. Asia-Pacific J. Ophthalmol. 12(1), 58–79 (2023).
Yi, F., Iskander, D. R. & Collins, M. Depth of focus and visual acuity with primary and secondary spherical aberration. Vision. Res. 51(14), 1648–1658 (2011).
Zhou, S. et al. Characteristics and influencing factors of corneal higher-order aberrations in patients with cataract. BMC Ophthalmol. 23(1), 313. https://doi.org/10.1186/s12886-023-03067-0 (2023).
Cheng, X., Bradley, A., Hong, X. & Thibos, L. N. Relationship between refractive error and monochromatic aberrations of the eye. Optom Vis. Sci. 80(1), 43–49. https://doi.org/10.1097/00006324-200301000-00007 (2003).
Mohammadpour, M. et al. Correlation of higher order aberrations and components of astigmatism in myopic refractive surgery candidates. J. Curr. Ophthalmol. 28(3), 112–116. https://doi.org/10.1016/j.joco.2016.04.007 (2016).
Xu, Z., Hua, Y., Qiu, W., Li, G. & Wu, Q. Precision and agreement of higher order aberrations measured with ray tracing and Hartmann-Shack aberrometers. BMC Ophthalmol. 18(1), 18 (2018).
Acknowledgements
This work was supported by a grant of the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health &Welfare, Republic of Korea (Grant number: RS-2023-00302193).
Author information
Authors and Affiliations
Contributions
Conceptualization with study design and hypothesis generation, H.L., D.Y.K., H.W.P., J.O., I.H.J., K.Y.S., A.E. and T.I.K.; Data collection and screening, H.L., D.Y.K., H.W.P., J.O. and T..K.; investigation including literature research and evidence synthesis, H.L., D.Y.K., A.E., and T.I.K., formal analysis, H.L., D.Y.K., and T.I.K.; writing—original draft preparation, H.L., D.Y.K., and T.I.K.; writing—review and editing with contributions from all co-authors. All authors have reviewed and agreed to the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Lee, H., Kim, D.Y., Oh, J. et al. Higher-order aberrations and visual outcomes of a new refractive extended depth-of-focus intraocular lens with a target of slight myopia. Sci Rep (2026). https://doi.org/10.1038/s41598-026-37674-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-026-37674-w