Abstract
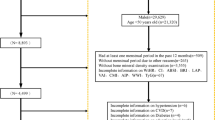
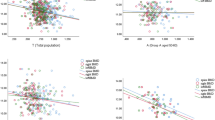
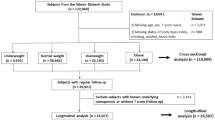
To evaluate the associations and comparative performance of novel anthropometric and metabolic indices with osteopenia and osteoporosis among middle-aged and older Chinese adults. A cross-sectional study was conducted among 10,142 Chinese adults aged ≥ 45 years who underwent quantitative computed tomography (QCT) for lumbar spine BMD assessment. Participants were categorized as normal, osteopenia, and osteoporosis. Associations and predictive capabilities of anthropometric indices were analyzed using multivariable logistic regression and receiver operating characteristic (ROC) curve analyses. The prevalences of osteopenia and osteoporosis were 35.14% and 14.05%, respectively. After adjusting for confounders, weight-adjusted waist index (WWI), relative fat mass (RFM), a body shape index (ABSI), triglyceride–glucose (TyG) index, and glycated hemoglobin (HbA1c) were found to be independently associated with osteopenia and osteoporosis. Among all indices, WWI demonstrated the strongest predictive value for osteoporosis (area under the curve = 0.726), followed by RFM and ABSI. In contrast, BMI and the visceral adiposity index (VAI) showed no significant associations with low BMD. Indices associated with central adiposity and metabolic dysfunction, especially WWI, may provide more precise prediction of osteoporosis risk. Incorporating such indices into early risk stratification for osteoporosis among older Chinese adults may have potential clinical utility.
Similar content being viewed by others
Data availability
The datasets generated and analyzed during the current study are not publicly available due to institutional restrictions but are available from the corresponding author upon reasonable request.
Abbreviations
- BMD:
-
Bone mineral density
- QCT:
-
Quantitative computed tomography
- DXA:
-
Dual-energy X-ray absorptiometry
- ISCD:
-
International Society for Clinical Densitometry
- SD:
-
Standard deviation
- IQR:
-
Interquartile range
- VIF:
-
Variance inflation factor
- BMI:
-
Body mass index
- WWI:
-
Weight-adjusted waist index
- ABSI:
-
A body shape index
- RFM:
-
Relative fat mass
- VAI:
-
Visceral adiposity index
- TyG:
-
Triglyceride-glucose index
- HbA1c:
-
Hemoglobin A1c
- ROC:
-
Receiver operating characteristic
- AUC:
-
Area under the curve
- OR:
-
Odds ratio
- CI:
-
Confidence interval
- MASLD:
-
Metabolic-associated steatotic liver disease
- SBP:
-
Systolic blood pressure
- DBP:
-
Diastolic blood pressure
- UA:
-
Uric acid
- BUN:
-
Blood urea nitrogen
- SCr:
-
Serum creatinine
- FPG:
-
Fasting plasma glucose
- HDLC:
-
High-density lipoprotein cholesterol
- LDLC:
-
Low-density lipoprotein cholesterol
- NHHR:
-
Non-HDL-C to HDL-C ratio
- MCH:
-
Mean corpuscular hemoglobin
- MCHC:
-
Mean corpuscular hemoglobin concentration
- HGB:
-
Hemoglobin
- PLT:
-
Platelet
- WBC:
-
White blood cell count
- ALB:
-
Albumin
- ALT:
-
Alanine aminotransferase
- AST:
-
Aspartate aminotransferase
- 5-NT:
-
5’-nucleotidase
- DBiL:
-
Direct bilirubin
- IDBiL:
-
Indirect bilirubin
- TBil:
-
Total bilirubin
- LFC:
-
Liver fat content
- VAA:
-
Visceral adipose area
- RANKL:
-
Receptor activator of nuclear kB ligand
References
Lekamwasam, S., Chandran, M. & Subasinghe, S. Revised FRAX®-based intervention thresholds for the management of osteoporosis among postmenopausal women in Sri Lanka. Arch. Osteoporos. 14(1), 33 (2019).
Drake, M. T. & Khosla, S. Mechanisms of age-related bone loss. Nat. Rev. Endocrinol. 18(9), 539–554 (2022).
Wright, N. C., Saag, K. G. & Curtis, J. R. Epidemiology of osteoporosis and fracture in men and women. Clin. Geriatr. Med. 38(3), 427–443 (2022).
International Osteoporosis Foundation. Osteoporos. Global Fact. Sheet https://www.osteoporosis.foundation (2021).
Oliveira, T. et al. Trends in osteoporotic fracture and related in-hospital complications during the COVID-19 pandemic in Alberta, Canada. Arch. Osteoporos. 17(1), 109 (2022).
Cauley, J. A., Chalhoub, D., Kassem, A. M. & Fuleihan, G. E. Osteoporosis: current clinical perspectives. Lancet Diabetes Endocrinol. 10(6), 421–435 (2022).
Zhang, F. et al. FAR591 promotes the pathogenesis and progression of SONFH by regulating Fos expression to mediate the apoptosis of bone microvascular endothelial cells. Bone Res. 11(1), 27 (2023).
Rachner, T. D., Khosla, S. & Hofbauer, L. C. Osteoporosis: now and the future. Lancet 377(9773), 1276–1287 (2011).
Yedavally-Yellayi, S., Ho, A. M. & Patalinghug, E. M. Update on osteoporosis. Prim. Care. 46(1), 175–190 (2019).
Assessment of fracture risk. And its application to screening for postmenopausal osteoporosis. Report of a WHO study group. World Health Organ. Tech. Rep. Ser. 843, 1–129 (1994).
Armbrecht, G. et al. Degenerative inter-vertebral disc disease osteochondrosis intervertebralis in europe: prevalence, geographic variation and radiological correlates in men and women aged 50 and over. Rheumatol. (Oxford). 56(7), 1189–1199 (2017).
Schultz, K. & Wolf, J. M. Emerging technologies in osteoporosis diagnosis. J. Hand Surg. Am. 44(3), 240–243 (2019).
Engelke, K. Quantitative computed tomography-current status and new developments. J. Clin. Densitom. 20(3), 309–321 (2017).
Mao, S. S. et al. Thoracic quantitative computed tomography (QCT) can sensitively monitor bone mineral metabolism: comparison of thoracic QCT vs lumbar QCT and dual-energy x-ray absorptiometry in detection of age-relative change in bone mineral density. Acad. Radiol. 24(12), 1582–1587 (2017).
Jia, L. & Cheng, M. Correlation analysis between risk factors, BMD and serum osteocalcin, CatheK, PINP, β-crosslaps, TRAP, lipid metabolism and BMI in 128 patients with postmenopausal osteoporotic fractures. Eur. Rev. Med. Pharmacol. Sci. 26(21), 7955–7959 (2022).
Sun, A., Hu, J., Wang, S., Yin, F. & Liu, Z. Association of the visceral adiposity index with femur bone mineral density and osteoporosis among the U.S. older adults from NHANES 2005–2020: a cross-sectional study. Front. Endocrinol. 14, 1231527 (2023).
Liu, Z. et al. Central obesity indices as predictors of osteoporosis risk. Osteoporos. Int. 34(4), 675–684 (2023).
Mattioli, D. et al. Behavior during aging of bone-marrow fatty-acids profile in women’s calcaneus to search for early potential osteoporotic biomarkers: a 1H-MR spectroscopy study. Bone 164, 116514 (2022).
Li, Y. et al. Visceral adiposity and its relationship with bone health. Metabolism 130, 155156 (2022).
Koo, H. Y. et al. Fracture risk in parkinson’s disease according to its severity and duration. Osteoporos. Int. 34(1), 81–89 (2023).
Wang, Y. et al. Cardiovascular risk and osteoporosis: shared mechanisms and clinical insights. J. Bone Min. Res. 38(2), 190–202 (2023).
Lin, S. Y. et al. Glycemic control and bone health: a systematic review. Diabetes Metab. Syndr. 16(7), 102547 (2022).
Xu, H., Li, J., Guo, S. & Yang, J. Triglyceride-glucose index and osteoporosis in postmenopausal women. Endocrine 80(3), 608–615 (2023).
Castiblanco-Rubio, G. A. & Martinez-Mier, E. A. Fluoride metabolism in pregnant women: A narrative review of the literature. Metabolites 12(4), 324 (2022).
Li, G. et al. Obesity and its complex relationship with osteoporosis. Obes. Rev. 20(9), 1279–1290 (2019).
Ferbebouh, M. et al. The pathophysiology of immunoporosis: innovative therapeutic targets. Inflamm. Res.(12), 1–17. (2021).
Meng, C. et al. Contemporary kidney transplantation has a limited impact on bone microarchitecture. Bone Rep. 16, 101172 (2022).
Cheng, X. G. et al. The use of QCT in China: progress and challenges. Osteoporos. Int. 33(5), 865–874 (2022).
Li, N. et al. Age-related changes of QCT lumbar and hip BMD in Chinese adults. Arch. Osteoporos. 14, 92 (2019).
Cui, L. et al. Osteoporosis diagnosis using QCT in Chinese adults. Osteoporos. Int. 28(1), 151–162 (2017).
Lee, J. J. et al. Quantification of abdominal adipose tissue by CT: a practical standardized approach. Radiology 303(1), 131–140 (2022).
Hofmann, P. et al. Quantitative CT for evaluating liver fat: current techniques and clinical applications. Abdom. Radiol. (NY). 47, 1985–1997 (2022).
Albala, C. et al. Obesity as a protective factor for postmenopausal osteoporosis. Int. J. Obes. Relat. Metab. Disord. 20(11), 1027–1032 (1996).
Reid, I. R., Plank, L. D. & Evans, M. C. Fat mass is an important determinant of whole body bone density in premenopausal women but not in men. J. Clin. Endocrinol. Metab. 75(3), 779–782 (1992).
Bredella, M. A. et al. Determinants of bone mineral density in obese premenopausal women. Bone 48(4), 748–754 (2011).
Salamat, M. R., Salamat, A. H. & Janghorbani, M. Association between obesity and bone mineral density by gender and menopausal status. Endocrinol. Metab. (Seoul). 31(4), 547–558 (2016).
Fu, X. et al. Associations of fat mass and fat distribution with bone mineral density in pre- and postmenopausal Chinese women. Osteoporos. Int. 22(1), 113–119 (2011).
Zhang, L., Sun, J., Li, Z. & Zhang, D. The relationship between serum folate and grip strength in American adults. Arch. Osteoporos. 16(1), 97 (2021).
Wang, X., Yang, S., He, G. & Xie, L. The association between weight-adjusted-waist index and total bone mineral density in adolescents: NHANES 2011–2018. Front. Endocrinol. (Lausanne). 14, 1191501 (2023).
Chen, P. J. et al. Association between osteoporosis and adiposity index reveals nonlinearity among postmenopausal women and linearity among men aged over 50 years. J. Epidemiol. Glob. Health. 14(3) (2024).
Engelke, K., Libanati, C., Fuerst, T., Zysset, P. & Genant, H. K. Advanced CT based in vivo methods for the assessment of bone density, structure, and strength. Curr. Osteoporos. Rep. 11(3), 246–255 (2013).
ISCD official positions–QCT. International Society for clinical densitometry. https://iscd.org/official-positions/2019-iscd-official-positions-adult/.
Cao, J. J. Effects of obesity on bone metabolism. J. Orthop. Surg. Res. 6(1), 30 (2011).
Ding, J. et al. The association of inflammatory markers with bone mineral density. J. Bone Min. Res. 23(7), 1124–1133 (2008).
Upadhyay, J., Farr, O. M. & Mantzoros, C. S. The role of leptin in regulating bone metabolism. Metabolism 64(1), 105–113 (2015).
Ilich, J. Z. et al. Marrow adiposity and osteoblastogenesis. J. Gerontol. Biol. Sci. Med. Sci. 75(5), 901–909 (2020).
Karsenty, G. & Ferron, M. The contribution of bone to whole-organism physiology. Nature 481(7381), 314–320 (2012).
Ramdas Nayak, V. K., Satheesh, P., Shenoy, M. T. & Kalra, S. Triglyceride glucose (TyG) index: A surrogate biomarker of insulin resistance. J. Pak Med. Assoc. 72(5), 986–988 (2022).
Valderrábano, R. J. & Linares, M. I. The TyG index and osteoporosis. J. Clin. Med. 10(3), 583 (2021).
Arikan, D. C. et al. TyG index, insulin resistance and bone health in postmenopausal women. J. Investig Med. 70(5), 1030–1036 (2022).
Ferron, M. et al. Insulin signaling in osteoblasts integrates bone remodeling and energy metabolism. Cell 142(2), 296–308 (2010).
Zhou, M. et al. Advanced glycation end products and bone fragility. J. Bone Min. Metab. 39(1), 90–97 (2021).
Ueland, T. et al. Increased serum and bone matrix levels of the secreted Wnt antagonist DKK-1 in patients with growth hormone deficiency in response to growth hormone treatment. J. Clin. Endocrinol. Metab. 100(2), 736–743 (2015).
Napoli, N. et al. Mechanisms of diabetes mellitus-induced bone fragility. Nat. Rev. Endocrinol. 13(4), 208–219 (2017).
Yeap, B. B. et al. HbA1c and incident fracture risk. J. Clin. Endocrinol. Metab. 99(6), 2329–2336 (2014).
Vestergaard, P. Discrepancies in bone mineral density and fracture risk in diabetes. Curr. Osteoporos. Rep. 5(3), 139–145 (2007).
Manolagas, S. C. et al. From Estrogen to oxidative stress: endocrine mechanisms of bone loss. Nat. Rev. Endocrinol. 6(11), 593–601 (2010).
Zhou, Y. et al. Metabolomic profiling reveals biomarkers associated with osteoporosis. Metabolomics 19, 56 (2023).
Palacios-González, B. et al. Serum metabolite profile associated with sex-dependent visceral adiposity index and low bone mineral density in a Mexican population. Metabolites. 11(9) (2021).
Riggs, B. L. et al. Sex steroids and adult skeleton homeostasis. Endocr. Rev. 23(3), 279–302. https://doi.org/10.1210/edrv.23.3.0465 (2002).
Khosla, S. et al. Sex hormones and the skeleton: A primer. J. Clin. Endocrinol. Metab. 105(12), dgaa718. https://doi.org/10.1210/clinem/dgaa718 (2020).
Wang, Y. et al. Abdominal obesity and low bone mass in Chinese older adults. BMJ Open. 6(9), e012694 (2016).
Schousboe, J. T., Riekkinen, O. & Karjalainen, J. Prediction of hip osteoporosis by DXA using a novel pulse-echo ultrasound device. Osteoporos. Int. 28(1), 85–93 (2017).
Ruan, Z. et al. Metformin accelerates bone fracture healing by promoting type H vessel formation through Inhibition of YAP1/TAZ expression. Bone Res. 11 (2023).
Cao, Y. M. et al. Association of type 2 diabetes with osteoporosis and fracture risk: A systematic review and meta-analysis. Medicine 104(6), 7 (2025).
Eastell, R. & Szulc, P. Use of bone turnover markers in postmenopausal osteoporosis. Lancet Diabetes Endocrinol. 5(11), 908–923 (2017).
Vasikaran, S. et al. Markers of bone turnover for the prediction of fracture risk and monitoring of osteoporosis treatment: a need for international reference standards.Osteoporos. Int. 22(2) (2011).
Acknowledgements
The authors would like to thank all the participants and staff of the Health Management Center of the Second Affiliated Hospital of Chongqing Medical University for their cooperation and support during data collection.
Author information
Authors and Affiliations
Contributions
All the authors contributed significantly to this study. LHW designed and supervised the study. PPY and MXC performed data collection and statistical analysis. JD interpreted the results and drafted the manuscript. LHY and YC critically revised the manuscript for intellectual content. All the authors have read and approved the final version of this manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This study was conducted in accordance with the Declaration of Helsinki and approved by the Ethics Committee of the Second Affiliated Hospital of Chongqing Medical University (Approval Number: 2022(129)). Written informed consent was obtained from all participants prior to enrollment.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Wang, L., Yu, P., Chen, Y. et al. Association of central adiposity and metabolic markers with osteopenia and osteoporosis in Chinese adults: a QCT-based cross-sectional study. Sci Rep (2026). https://doi.org/10.1038/s41598-026-37749-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-026-37749-8