Abstract
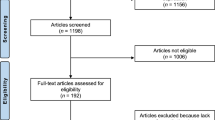
Low back pain (LBP) is a leading cause of disability worldwide, and manual therapy (MT) is commonly used in its management. However, utilization patterns and perceived effectiveness vary according to training and clinical context, with limited national-level evidence describing how Saudi physical therapists apply MT in routine LBP care. To examine national patterns of MT utilization for LBP among licensed Saudi physical therapists, to identify commonly applied techniques, and to evaluate professional and educational factors associated with perceived effectiveness and frequency of use. A cross-sectional survey was conducted from January to March 2025 using a structured online questionnaire distributed nationwide via professional and social-media platforms. Eligible participants were Saudi Commission for Health Specialties (SCFHS)–licensed physical therapists actively managing LBP. The questionnaire assessed demographics, MT training exposure, frequency and type of MT use, perceived effectiveness, and outcome-measurement practices. Content validity was confirmed by six experts (S-CVI/Avg = 0.96). Data were analyzed using descriptive statistics, chi-square tests, Spearman’s rho correlation, and multivariable ordinal logistic regression (SPSS v28; α < 0.05). Of 182 responses received, 173 met the inclusion criteria. Most participants reported using MT for LBP management, with 89% employing it at least occasionally and 20% reporting routine use. MT was rated as important or very important by 87.9% of respondents, and more than half assigned a perceived usefulness score ≥ 6/10. Greater exposure to MT training was independently associated with higher MT utilization and stronger perceived effectiveness (p < 0.001; Nagelkerke R² = 0.47), whereas years of experience and clinical specialization were not significantly associated. MT is widely used and positively perceived by Saudi physical therapists managing LBP. Variability in its utilization and perceived effectiveness appears primarily related to differences in training exposure. These findings describe current practice patterns and professional perceptions and may inform future educational planning, without inferring clinical effectiveness.
Similar content being viewed by others
Data availability
The dataset supporting the findings of this study has been deposited in the Open Science Framework (OSF) repository and is openly available at https://osf.io/p2s69/overview? view_only=99d6801264334cd896e30278631f3093 under the title “MT Utilization and Perceived Effectiveness Dataset.”
Abbreviations
- LBP:
-
Low back pain
- MT:
-
Manual Therapy
- SCFHS:
-
Saudi Commission for Health Specialties
- CPD:
-
Continuing-professional-development
- IFOMPT:
-
International Federation of Orthopaedic Manipulative Physical Therapists
- S-CVI:
-
Scale-Level Content Validity Index
- VAS:
-
Visual Analog Scale
- NPRS:
-
Numeric Pain Rating Scale
- RMDQ:
-
Roland–Morris Disability Questionnaire
- QBPDS:
-
Quebec Back-Pain Disability Scale
- SF-12/SF-36:
-
Short Form Health Survey
- SPSS:
-
Statistical Package for the Social Sciences
- CHERRIES:
-
Checklist for Reporting Results of Internet E-Surveys
- STROBE:
-
Strengthening the Reporting of Observational Studies in Epidemiology
- OSF:
-
Open Science Framework
References
Vos, T. et al. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the global burden of disease study 2019. Lancet 396 (10258), 1204–1222. https://doi.org/10.1016/S0140-6736(20)30925-9 (2020).
Ferreira, M. L. et al. Global, regional, and National burden of low back pain, 1990–2020, its attributable risk factors, and projections to 2050: a systematic analysis of the global burden of disease study 2021. Lancet Rheumatol. 5 (6), e316–e329. https://doi.org/10.1016/S2665-9913(23)00098-X (2023).
Hoy, D., Brooks, P., Blyth, F. & Buchbinder, R. The epidemiology of low back pain. Best Pract. Res. Clin. Rheumatol. 24 (6), 769–781. https://doi.org/10.1016/j.berh.2010.10.002 (2010).
Hartvigsen, J. et al. What low back pain is and why we need to pay attention. Lancet 391 (10137), 2356–2367. https://doi.org/10.1016/S0140-6736(18)30480-X (2018).
Yang, Y. et al. Focus on the impact of social factors and lifestyle on the disease burden of low back pain: findings from the global burden of disease study 2019. BMC Musculoskelet. Disord. 24 (1), 679 (2023).
Al Amer, H. S. Low back pain prevalence and risk factors among health workers in Saudi Arabia: a systematic review and meta-analysis. J. Occup. Health 62(1), e12155. https://doi.org/10.1002/1348-9585.12155 (2020).
Aldera, M. A., Alexander, C. M. & McGregor, A. H. Prevalence and incidence of low back pain in the Kingdom of Saudi Arabia: a systematic review. J. Epidemiol. Glob Health 10(4), 269–279. https://doi.org/10.2991/jegh.k.200417.001 (2020).
George, S. Z. et al. Interventions for the management of acute and chronic low back pain: revision 2021. J. Orthop. Sports Phys. Ther. 51 (11), CPG1–CPG60. https://doi.org/10.2519/jospt.2021.0304 (2021).
Qaseem, A., Wilt, T. J., McLean, R. M. & Forciea, M. A. Noninvasive treatments for acute, subacute, and chronic low back pain: a clinical practice guideline from the American college of physicians. Ann. Intern. Med. 166 (7), 514–530. https://doi.org/10.7326/M16-2367 (2017).
Delitto, A. et al. Low back pain. J. Orthop. Sports Phys. Ther. 42 (4), A1–A57. https://doi.org/10.2519/jospt.2012.42.4.A1 (2012).
Oliveira, C. B. et al. Clinical practice guidelines for the management of non-specific low back pain in primary care: an updated overview. Eur. Spine J. 27 (11), 2791–2803. https://doi.org/10.1007/s00586-018-5673-2 (2018).
Nicol, V. et al. Chronic low back pain: a narrative review of recent international guidelines for diagnosis and conservative treatment. J. Clin. Med. 12(4), 1685. https://doi.org/10.3390/jcm12041685 (2023).
Zhou, T., Salman, D. & McGregor, A. H. Recent clinical practice guidelines for the management of low back pain: a global comparison. BMC Musculoskelet. Disord. 25 (1), 344. https://doi.org/10.1186/s12891-024-07468-0 (2024).
Bronfort, G., Haas, M., Evans, R., Leininger, B. & Triano, J. Effectiveness of manual therapies: the UK evidence report. Chiropr. Osteopat. 18, 3. https://doi.org/10.1186/1746-1340-18-3 (2010).
Chitale, N., Patil, D. S., Phansopkar, P. & Joshi, A. A review on treatment approaches for chronic low back pain via mulligan’s movement with mobilization and physical therapy. Cureus 14 (8), e28127. https://doi.org/10.7759/cureus.28127 (2022).
Cankaya, M. S. & Pala, O. O. Outcomes of Mulligan concept applications in obese individuals with chronic mechanical low back pain: a randomized controlled trial. Life (Basel). 14 (6), 754. https://doi.org/10.3390/life14060754 (2024).
Cyriax, J. Textbook of Orthopaedic Medicine 11th edn (Baillière Tindall, 1984).
Neto, T. et al. Effects of lower body quadrant neural mobilization in healthy and low back pain populations: a systematic review and meta-analysis. Musculoskelet. Sci. Pract. 27, 14–22. https://doi.org/10.1016/j.msksp.2016.11.014 (2017).
Bailly, F. et al. Clinical guidelines and care pathway for management of low back pain with or without radicular pain. Jt. Bone Spine 88(6), 105227. https://doi.org/10.1016/j.jbspin.2021.105227 (2021).
Shipton, E. A. Physical therapy approaches in the treatment of low back pain. Pain Ther. 7 (2), 127–137. https://doi.org/10.1007/s40122-018-0105-x (2018).
Ladeira, C. E., Cheng, M. S. & Hill, C. J. Physical therapists’ treatment choices for non-specific low back pain in florida: an electronic survey. J. Man. Manip Ther. 23 (2), 109–118. https://doi.org/10.1179/2042618613Y.0000000065 (2015).
Foster, N. E., Thompson, K. A., Baxter, G. D. & Allen, J. M. Management of non-specific low back pain by physiotherapists in Britain and Ireland. Spine 24 (13), 1332–1342. https://doi.org/10.1097/00007632-199907010-00011 (1999).
Kuik, M., Calley, D., Buus, R. & Hollman, J. Beliefs and practice patterns of spinal thrust manipulation for mechanical low back pain of physical therapists in Minnesota. J. Man. Manip Ther. 32 (4), 421–428. https://doi.org/10.1080/10669817.2023.2279821 (2024).
Alghadir, A. H., Iqbal, Z. A. & Iqbal, A. Knowledge and utilization of manual therapy in the management of knee osteoarthritis by physical therapists in Saudi arabia: a cross-sectional study. BMC Public. Health. 24 (1), 3379. https://doi.org/10.1186/s12889-024-20923-w (2024).
Fairbank, J. C. T. & Pynsent, P. B. The Oswestry disability index. Spine 25 (22), 2940–2953. https://doi.org/10.1097/00007632-200011150-00017 (2000).
Roland, M. & Fairbank, J. The Roland–Morris disability questionnaire and the Oswestry disability questionnaire. Spine 25 (24), 3115–3124. https://doi.org/10.1097/00007632-200012150-00006 (2000).
Roland, M. & Morris, R. A study of the natural history of back pain. Spine 8 (2), 141–144. https://doi.org/10.1097/00007632-198303000-00004 (1983).
Kopec, J. A. et al. The Quebec back pain disability scale. Spine 20 (3), 341–352. https://doi.org/10.1097/00007632-199502000-00016 (1995).
Jenkinson, C. & Layte, R. Development and testing of the UK SF-12. J. Health Serv. Res. Policy. 2 (1), 14–18. https://doi.org/10.1177/135581969700200105 (1997).
Ware, J. E. SF-36 health survey update. Spine 25 (24), 3130–3139. https://doi.org/10.1097/00007632-200012150-00008 (2000).
Waddell, G., Newton, M., Henderson, I., Somerville, D. & Main, C. J. A Fear-Avoidance beliefs questionnaire (FABQ) and the role of fear-avoidance beliefs in chronic low back pain and disability. Pain 52 (2), 157–168. https://doi.org/10.1016/0304-3959(93)90127-B (1993).
Snaith, R. P. & Zigmond, A. S. The hospital anxiety and depression scale. BMJ 292 (6516), 344. https://doi.org/10.1136/bmj.292.6516.344 (1986).
Podsiadlo, D. & Richardson, S. The timed up and go: a test of basic functional mobility for frail elderly persons. J. Am. Geriatr. Soc. 39 (2), 142–148. https://doi.org/10.1111/j.1532-5415.1991.tb01616.x (1991).
Butland, R. J., Pang, J., Gross, E. R., Woodcock, A. A. & Geddes, D. M. Two-, six-, and 12-minute walking tests in respiratory disease. BMJ 284 (6329), 1607–1608. https://doi.org/10.1136/bmj.284.6329.1607 (1982).
Chiarotto, A. et al. Measurement properties of VAS, NRS, and the pain severity subscale of the brief pain inventory in patients with low back pain: a systematic review. J. Pain. 20 (3), 245–263. https://doi.org/10.1016/j.jpain.2018.07.009 (2019).
Alghadir, A., Anwer, S., Iqbal, A. & Iqbal, Z. Test–retest reliability, validity, and minimum detectable change of VAS, NRS and VRS for Osteoarthritic knee pain. J. Pain Res. 11, 851–856. https://doi.org/10.2147/JPR.S158847 (2018).
Yusoff, M. S. B. ABC of content validation and content validity index calculation. Educ. Med. J. 11 (2), 49–54. https://doi.org/10.21315/eimj2019.11.2.6 (2019).
World Medical Association. World medical association declaration of helsinki: ethical principles for medical research involving human subjects. JAMA 310 (20), 2191–2194. https://doi.org/10.1001/jama.2013.281053 (2013).
Algarni, A. S., Ghorbel, S., Jones, J. G. & Guermazi, M. Validation of an Arabic version of the Oswestry index in Saudi Arabia. Ann. Phys. Rehabil Med. 57 (9–10), 653–663. https://doi.org/10.1016/j.rehab.2014.06.006 (2014).
Jenks, A. et al. RMDQ, ODI, and QBPDS: which has superior measurement properties in older adults with low back pain? J. Orthop. Sports Phys. Ther. 52 (7), 457–469. https://doi.org/10.2519/jospt.2022.10802 (2022).
Nicol/Oliveira/George. (refs 7–12) — multimodal recommendation cited in Results/Discussion (already listed; no duplicate entry).
Rubinstein, S. M. et al. Benefits and harms of spinal manipulative therapy for chronic low back pain: systematic review and meta-analysis of RCTs. BMJ 364, l689. https://doi.org/10.1136/bmj.l689 (2019).
Thomas, J. S. et al. Effect of spinal manipulative and mobilization therapies in young adults with mild to moderate chronic low back pain. JAMA Netw. Open. 3 (8), e2012589. https://doi.org/10.1001/jamanetworkopen.2020.12589 (2020).
Guzmán Pavón, M. J. et al. Comparative effectiveness of manual therapy interventions on pain and pressure pain threshold in patients with myofascial trigger points. Clin. J. Pain. 38 (12), 749–760. https://doi.org/10.1097/AJP.0000000000001079 (2022).
Pensri, P., Foster, N. E., Srisuk, S., Baxter, G. D. & McDonough, S. M. Physiotherapy management of low back pain in thailand: a study of practice. Physiother Res. Int. 10 (4), 201–212. https://doi.org/10.1002/pri.16 (2005).
Poitras, S., Blais, R., Swaine, B. & Rossignol, M. Practice patterns of physiotherapists in the treatment of work-related back pain. J. Eval Clin. Pract. 13 (3), 412–421. https://doi.org/10.1111/j.1365-2753.2006.00725.x (2007).
Ladeira, C. E., Cheng, M. S. & da Silva, R. A. Clinical specialization and adherence to Evidence-Based practice guidelines for low back pain management: A survey of US physical therapists. J. Orthop. Sports Phys. Ther. 47 (5), 347–358. https://doi.org/10.2519/jospt.2017.6561 (2017).
Agnus Tom, A., Rajkumar, E., John, R. & Joshua George, A. Determinants of quality of life in individuals with chronic low back pain: a systematic review. Health Psychol. Behav. Med. 10 (1), 124–144. https://doi.org/10.1080/21642850.2021.2022487 (2022).
Maughan, E. F. & Lewis, J. S. Outcome measures in chronic low back pain. Eur. Spine J. 19 (9), 1484–1494. https://doi.org/10.1007/s00586-010-1353-6 (2010).
Hansen, A., Nim, C. G., O’Sullivan, K. & O’Neill, S. Testing walking performance in patients with low back pain: will two minutes do instead of six minutes? Disabil. Rehabil. 46 (6), 1173–1177. https://doi.org/10.1080/09638288.2023.2194683 (2024).
Alanazi, F., Gleeson, P., Olson, S. & Roddey, T. Translation and validation of the Arabic version of the Fear-Avoidance beliefs questionnaire in patients with low back pain. Spine (Phila Pa. 1976). 42 (7), E411–E416. https://doi.org/10.1097/BRS.0000000000001802 (2017).
Hallegraeff, J. M., Van Zweden, L., Oostendorp, R. A. & Van Trijffel, E. Psychological assessments by manual physiotherapists in the Netherlands in patients with nonspecific low back pain. J. Man. Manip Ther. 29 (5), 310–317. https://doi.org/10.1080/10669817.2021.1919283 (2021).
Holopainen, R., Piirainen, A., Karppinen, J., Linton, S. J. & O’Sullivan, P. Physiotherapists’ conceptions of learning and integrating cognitive functional therapy into clinical practice. Physiother Theory Pract. 38 (2), 309–326. https://doi.org/10.1080/09593985.2020.1753271 (2022).
Mourad, F. et al. Knowledge, beliefs, and attitudes of spinal manipulation: a cross-sectional survey of Italian physiotherapists. Chiropr. Man. Th. 30 (1), 33. https://doi.org/10.1186/s12998-022-00449-x (2022).
Ali, M., Uddin, Z. & Hossain, A. Clinical practice pattern of managing low back pain among physiotherapists in bangladesh: a cross-sectional study. Physiother Pract. Res. 43 (2), 93–100 (2022). (If volume/pages differ in your thesis file, keep your originals.).
Anggiat, L. & Rahmansyah, B. Trends in the use of manual therapy among physiotherapists in jakarta: a survey study. Int. J. Sport Exerc. Health Res. 6 (2), 121–125. https://doi.org/10.31254/sportmed.6205 (2022).
Chavula, G. Level of knowledge and practice of manual therapy among physiotherapy practitioners at the university teaching Hospital, Lusaka, Zambia. Int. J. Clin. Exp. Med. Res. 6 (2), 103–110. https://doi.org/10.26855/ijcemr.2022.04.001 (2022).
Hamm, L. et al. Danish physiotherapists’ management of low back pain. Adv. Physiother. 5 (3), 125–131 (2003).
Poitras, S., Blais, R., Swaine, B. & Rossignol, M. Management of work-related low back pain: a population-based survey of physical therapists. Phys. Ther. 85 (11), 1168–1181 (2005).
Rubinstein, S. M. & van Tulder, M. A best-evidence review of diagnostic procedures for neck and low-back pain. Best Pract. Res. Clin. Rheumatol. 22 (3), 471–482. https://doi.org/10.1016/j.berh.2007.12.003 (2008).
Anderson, D. B. & Shaheed, C. A. Medications for treating low back pain in adults: overview for musculoskeletal clinicians. J. Orthop. Sports Phys. Ther. 52 (7), 425–431. https://doi.org/10.2519/jospt.2022.10788 (2022).
Hiroshi, Takasaki Takahiro, Ueno Japanese Clinical Physical Therapists With the Mechanical Diagnosis and Therapy License Are More Competent and Confident in Pain Management Than Those Without It: A Cross-Sectional Study. Cureus. 16:e70652. https://doi.org/10.7759/cureus.70652 (2024).
Birgitta, Widerström Eva, Rasmussen-Barr Carina, Boström. Aspects influencing clinical reasoning and decision-making when matching treatment to patients with low back pain in primary healthcare Musculoskeletal Science and Practice 416-14. http://doi.org/10.1016/j.msksp.2019.02.003 (2019).
Ismail, Saracoglu Meltem Isintas, Arik Emrah, Afsar Hasan Huseyin, Gokpinar. The effectiveness of pain neuroscience education combined with manual therapy and home exercise for chronic low back pain: A single-blind randomized controlled trial. Physiotherapy Theory and Practice. 38(7), 868-878. 10.1080/09593985.2020.1809046 (2022).
Acknowledgements
The authors extend their appreciation to the Ongoing Research Funding program – Research Chairs (ORF-RC-2025-1000), King Saud University, Riyadh, Saudi Arabia for funding this research.
Funding
This study was funded by the Ongoing Research Funding program – Research Chairs (ORF-RC-2025-1000), King Saud University, Riyadh, Saudi Arabia. The funding body played no role in the design, execution, analysis and interpretation of data, or writing of the study.
Author information
Authors and Affiliations
Contributions
Y.M.Z. A.H.A. S.A.A. F.A.A. A.S.A. and A.I. proposed the study conception and design. Y.M.Z. A.H.A and A.I. completed the methodological work and collected data. Y.M.Z. A.H.A. S.A.A. F.A.A. A.S.A. and A.I. contributed to the data analysis and its interpretation. Y.M.Z. and A.I. prepared the manuscript’s initial draft. Y.M.Z. A.H.A. S.A.A. F.A.A. A.S.A. and A.I. critically reviewed and edited the manuscript’s intellectual content. All authors read and approved the manuscript’s final version to be submitted or published and took responsibility for the intellectual content of the same manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
Ethical approval for this study was conducted by the Institutional Review Board Ethics Committee of the College of Medicine at King Saud University (approval number 25/0010/IRB on 07/01/2025). The study was conducted in accordance with the ethical principles outlined in the Declaration of Helsinki (2010). All participants were informed about the purpose of the study, assured of confidentiality, and provided written consent prior to participation. Participation was voluntary, and respondents could withdraw at any time without consequence.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Zubayni, Y.M., Alhammad, S.A., Alodaibi, F.A. et al. Utilization patterns and perceived effectiveness of manual therapy for low back pain among Saudi physical therapists: a national cross-sectional study. Sci Rep (2026). https://doi.org/10.1038/s41598-026-38025-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-026-38025-5