Abstract
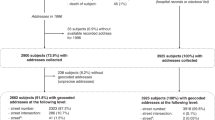
Prostate cancer is always regarded as ‘we’ disease with unavoidable influence within the couples, particularly during the early post-diagnosis period. Thus, this qualitative research is to explore the psychosocial experiences of prostate cancer couples coping within six months of diagnosis in China. The study was conducted through semi-structured interviews between June 2023 and June 2024. All interviews were recorded, transcribed, and analyzed following Braun and Clarke’s reflective thematic analysis approach. Fourteen couples were enrolled using purposive sampling with variation in sociodemographic information. The participants’ normal lives were disrupted, and couples adopted both individual and joint coping strategies to regain a new sense of balance. The overarching theme “Refine and Regain” was proposed during this process. This emerged from five main themes: “Unrecognized distress and emotional fluctuation,” “Lost in frustration,” “Interrupted family and social connections,” “Striving for survival,” and “Growth and adaption.” Couples got through physical and emotional difficulties during the anti-cancer treatment, starting from accepting the fact they got the cancer. Some participants showed a progressive adaptation to cancer over time, while others experienced a dynamic, non-linear adjustment process. The findings revealed variations in couples’ psychosocial adaptation to prostate cancer, highlighting the need for tailored interventions to enhance mutual coping.
Similar content being viewed by others
Data availability
The datasets generated and/or analyzed during the current study are available from the first author upon reasonable request.
References
Bray, F. et al. Global cancer statistics 2022: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 74, 229–263. https://doi.org/10.3322/caac.21834 (2024).
Xia, X. F. et al. The relationship between urologic cancer outcomes and National human development index: trend in recent years. BMC Urol. 22 https://doi.org/10.1186/s12894-022-00953-5 (2022).
Han, B. et al. Cancer incidence and mortality in China, 2022. J. Natl. Cancer Cent. 4, 47–53 (2024). https://doi.org/10.1016/j.jncc.2024.01.006
Ferlay, J. et al. Cancer Today. (International Agency for Research on Cancer, 2024); https://gco.iarc.who.int/today
Xia, C. et al. Cancer statistics in China and united States, 2022: profiles, trends, and determinants. Chin. Med. J. (Engl). 135, 584–590. https://doi.org/10.1097/CM9.0000000000002108 (2022).
Gu, X. Y. et al. Analysis on the trend of prostate cancer incidence and age change in cancer registration areas of China, 2000 to 2014. Chin. Prev. Med. 52, 586–592. https://doi.org/10.3760/cma.j.issn.0253-9624.2018.06.006 (2018).
Salter, C. A., Mulhall, J. P. & Oncosexology Sexual issues in the male cancer survivor. Urol. Clin. North. Am. 48, 591–602. https://doi.org/10.1016/j.ucl.2021.07.001 (2021).
Wittmann, D. et al. Guidelines for sexual health care for prostate cancer patients: recommendations of an international panel. J. Sex. Med. 19, 1655–1669. https://doi.org/10.1016/j.jsxm.2022.08.197 (2022).
Shevach, J., Weiner, A. & Morgans, A. K. Quality of Life-Focused Decision-Making for prostate cancer. Curr. Urol. Rep. 20 https://doi.org/10.1007/s11934-019-0924-2 (2019).
Beyer, M., Bischoff, C., Lässing, J., Gockel, I. & Falz, R. Effects of postoperative physical exercise rehabilitation on cardiorespiratory fitness, functional capacity and quality of life in patients with colorectal, breast, and prostate cancer - a systematic review and meta-analysis. J. Cancer Res. Clin. Oncol. 151, 13. https://doi.org/10.1007/s00432-024-06064-y (2024).
Van den Broeck, T. et al. Prognostic value of biochemical recurrence following treatment with curative intent for prostate cancer: A systematic review. Eur. Urol. 75, 967–987. https://doi.org/10.1016/j.eururo.2018.10.011 (2019).
Schulz, R., Beach, S. R., Czaja, S. J., Martire, L. M. & Monin, J. K. Family caregiving for older adults. Annu. Rev. Psychol. 71, 635–659. https://doi.org/10.1146/annurev-psych-010419-050754 (2020).
Schantz Laursen, B. Sexuality in men after prostate cancer surgery: a qualitative interview study. Scand. J. Caring Sci. 31, 120–127. https://doi.org/10.1111/scs.12328 (2017).
Wittmann, D. et al. TrueNTH sexual recovery intervention for couples coping with prostate cancer: randomized controlled trial results. Cancer 128 (7), 1513–1522. https://doi.org/10.1002/cncr.34076 (2022).
Wang, T., Cheng, H. L., Li, K. W., Wong, P. K. K. & Dong, W. The experiences of female partners of patients with erectile dysfunction due to prostate cancer treatment in china: A qualitative exploration. Cancer Nurs. 48, 131–137. https://doi.org/10.1097/NCC.0000000000001282 (2025).
Yang, Y. et al. Does caring for patients with advanced non-small cell lung cancer affect health-related quality of life of caregivers? A multicenter, cross-sectional study. BMC Public. Health. 24, 224. https://doi.org/10.1186/s12889-024-17669-w (2024).
Ninnoni, J. P. K. & Owoo, B. Psychosocial experiences of caring by family caregivers of patients living with prostate cancer in a teaching hospital: A descriptive phenomenological study. Nurs. Open. 10, 6268–6281. https://doi.org/10.1002/nop2.1869 (2023).
Song, L., Rini, C., Ellis, K. R. & Northouse, L. L. Appraisals, perceived dyadic communication, and quality of life over time among couples coping with prostate cancer. Support Care Cancer. 24, 3757–3765. https://doi.org/10.1007/s00520-016-3188-0 (2016).
Coyne, I., Holmström, I. & Söderbäck, M. Centeredness in healthcare: A concept synthesis of family-centered care, person-centered care and child-centered care. J. Pediatr. Nurs. 42, 45–56. https://doi.org/10.1016/j.pedn.2018.07.001 (2018).
Lim, J. W., Shon, E. J., Paek, M. & Daly, B. The dyadic effects of coping and resilience on psychological distress for cancer survivor couples. Support Care Cancer. 22, 3209–3217. https://doi.org/10.1007/s00520-014-2334-9 (2014).
Rentscher, K. E. Communal coping in couples with health problems. Front. Psychol. 10, 398. https://doi.org/10.3389/fpsyg.2019.00398 (2019).
Manne, S. L. et al. Relationship communication and the course of psychological outcomes among couples coping with localised prostate cancer. Eur. J. Cancer Care (Engl). 30, e13401. https://doi.org/10.1111/ecc.13401 (2021).
Lim, J. W., Paek, M. S. & Shon, E. J. Gender and role differences in couples’ communication during cancer survivorship. Cancer Nurs. 38, E51–E60. https://doi.org/10.1097/NCC.0000000000000191 (2015).
Chen, M. et al. A literature review of the relationship between dyadic coping and dyadic outcomes in cancer couples. Eur. J. Oncol. Nurs. 54, 102035. https://doi.org/10.1016/j.ejon.2021.102035 (2021).
Chan, F., da Silva Cardoso, E., Chronister, J. & Hiatt, E. Psychosocial adjustment. In Encyclopedia of Behavioral Medicine (eds Gellman, M. D. & Turner, J. R.) (Springer, 2013). https://doi.org/10.1007/978-1-4419-1005-9_917.
Sanabria, G. et al. Navigating norms and expectations: the influence of culture on Latino couples and their interpersonal communication and coping post-breast cancer diagnosis. Ethn. Health. 29, 164–178. https://doi.org/10.1080/13557858.2023.2279482 (2024).
Creswell, J. W. Research Design: International Student Edition 4th edn (Sage, Thousand Oaks, CA, 2014).
Thorne, S. Interpretive Description: Qualitative Research for Applied Practice 2nd edn (Routledge, 2016). https://doi.org/10.4324/9781315545196
Kusi, H. Doing Qualitative Research: A Guide for Researchers (Emmpong Press, Accra, Ghana, 2012).
O’Brien, B. C., Harris, I. B., Beckman, T. J., Reed, D. A. & Cook, D. A. Standards for reporting qualitative research: a synthesis of recommendations. Acad. Med. 89, 1245–1251. https://doi.org/10.1097/ACM.0000000000000388 (2014).
Hill, C. E. Consensual Qualitative Research: A Practical Resource for Investigating Social Science Phenomena 1st edn (American Psychological Association, 2012).
Buote, R., Cameron, E., Collins, R. & McGowan, E. Understanding men’s experiences with prostate cancer stigma: a qualitative study. Oncol. Nurs. Forum. 47, 577–585. https://doi.org/10.1188/20.ONF.577-585 (2020).
Mardani, A., Farahani, M. A., Khachian, A. & Vaismoradi, M. Fear of cancer recurrence and coping strategies among prostate cancer survivors: a qualitative study. Curr. Oncol. 30, 6720–6733. https://doi.org/10.3390/curroncol30070493 (2023).
Collaço, N. et al. Prostate cancer and the impact on couples: a qualitative metasynthesis. Support Care Cancer. 26, 1703–1713. https://doi.org/10.1007/s00520-018-4134-0 (2018).
Kallio, H., Pietilä, A. M., Johnson, M. & Kangasniemi, M. Systematic methodological review: developing a framework for a qualitative semi-structured interview guide. J. Adv. Nurs. 72, 2954–2965. https://doi.org/10.1111/jan.13031 (2016).
Chen, H. Y. & Boore, J. R. Translation and back-translation in qualitative nursing research: methodological review. J. Clin. Nurs. 19, 234–239. https://doi.org/10.1111/j.1365-2702.2009.02896.x (2010).
Byrne, D. A worked example of Braun and clarke’s approach to reflexive thematic analysis. Qual. Quant. 56, 1391–1412 (2022).
Braun, V. & Clarke, V. Thematic Analysis: A Practical Guide (Sage, 2022).
Braun, V. & Clarke, V. One size fits all? What counts as quality practice in (reflexive) thematic analysis? Qualitative Res. Psychol. 18, 328–352. https://doi.org/10.1080/14780887.2020.1769238 (2021).
World Medical Association. World medical association declaration of helsinki: ethical principles for medical research involving human participants. JAMA 333, 71–74. https://doi.org/10.1001/jama.2024.21972 (2025).
Manne, S. & Badr, H. Intimacy and relationship processes in couples’ psychosocial adaptation to cancer. Cancer , 112(Suppl. 11), 2541–2555. https://doi.org/10.1002/cncr.23450 (2008).
Mizuno, M., Kataoka, J. & Oishi, F. Longitudinal study on quality of life and psychosocial conditions in light of responses to illness-related information in postoperative cancer patients. Asia Pac. J. Oncol. Nurs. 5, 208–216 (2018).
Watts, S. et al. Depression and anxiety in prostate cancer: a systematic review and meta-analysis of prevalence rates. BMJ Open. 4, e003901. https://doi.org/10.1136/bmjopen-2013-003901 (2014).
Oba, A. et al. Psychological distress in men with prostate cancer and their partners before and after cancer diagnosis: a longitudinal study. Jpn J. Clin. Oncol. 47, 735–742. https://doi.org/10.1093/jjco/hyx066 (2017).
Varner, S. et al. Illness uncertainty, partner support, and quality of life: a dyadic longitudinal investigation of couples facing prostate cancer. Psychooncology 28, 2188–2194. https://doi.org/10.1002/pon.5205 (2019).
Lehto, U. S., Aromaa, A. & Tammela, T. Psychological recovery and well-being of spouses of patients with prostate cancer 5 years after primary treatment in finland: a follow-up survey. BMJ Open. 13, e063435. https://doi.org/10.1136/bmjopen-2022-063435 (2023).
Lafaye, A. et al. Dyadic effects of coping strategies on emotional state and quality of life in prostate cancer patients and their spouses. Psychooncology 23, 797–803. https://doi.org/10.1002/pon.3483 (2014).
Mullen, L. et al. Psychosocial care for cancer survivors: a global review of National cancer control plans. Psychooncology 32, 1684–1693. https://doi.org/10.1002/pon.6218 (2023).
Lee, H., Higgins, M. K. & Song, M. K. Sexual satisfaction and associated factors among older cancer survivors. Res. Nurs. Health. 48, 85–94. https://doi.org/10.1002/nur.22430 (2025).
Jitaru, M. & Turliuc, M. N. The moderator role of interpersonal emotion regulation on the associations between commitment, intimacy, and couple satisfaction. Int. J. Environ. Res Public. Health. 19, 10506. https://doi.org/10.3390/ijerph191710506 (2022).
Tagai, E. K. et al. Social and medical risk factors associated with supportive needs in the first year following localized prostate cancer treatment. J. Cancer Surviv. 15, 110–118. https://doi.org/10.1007/s11764-020-00916-5 (2021).
Alexis, O. & Worsley, A. J. A meta-synthesis of qualitative studies exploring men’s sense of masculinity post–prostate cancer treatment. Cancer Nurs. 41, 298–310. https://doi.org/10.1097/NCC.0000000000000509 (2018).
Elliott, S. & Matthew, A. Sexual recovery following prostate cancer: recommendations from two established Canadian sexual rehabilitation clinics. Sex. Med. Rev. 6, 279–294. https://doi.org/10.1016/j.sxmr.2017.09.001 (2018).
Sun, W. N., Hsu, H. T., Ko, N. Y. & Huang, Y. T. Decision-making processes in surrogates of cancer patients in a Taiwan intensive care unit. Int. J. Environ. Res. Public. Health. 17, 4443. https://doi.org/10.3390/ijerph17124443 (2020).
Mardani, A., Farahani, M. A., Khachian, A., Maleki, M. & Vaismoradi, M. Qualitative exploration of sexual dysfunction and associated coping strategies among Iranian prostate cancer survivors. Support Care Cancer. 32, 360. https://doi.org/10.1007/s00520-024-08548-6 (2024).
Kobayashi, K. et al. How do Japanese patients really feel about losing potency after radical prostatectomy? (MAJI study). Int. J. Urol. 32, 69–72. https://doi.org/10.1111/iju.15597 (2025).
Ng, K. S. & Wei, M. Cultural differences in the associations between attachment, coping strategies, and emotional regulation. J. Couns. Psychol. 67, 417–428 (2020).
Moynihan, C. Theories in health care and research: theories of masculinity. BMJ 324, 409–412 (2002).
Chan, A. et al. A systematic review: sexual well-being and perceived barriers to seeking professional help among Chinese adults living with cancer. Eur. J. Cancer Care (Engl. 30, e13519. https://doi.org/10.1111/ecc.13519 (2021).
Chen, W. et al. Effectiveness of couple-based interventions for prostate cancer patients and their spouses on their quality of life: a systematic review and meta-analysis. Support Care Cancer. 31, 34. https://doi.org/10.1007/s00520-022-07532-2 (2022).
Ihrig, A. et al. Couples coping with advanced prostate cancer: an explorative study on treatment decision making, mental deterioration, partnership, and psychological burden. Urol. Oncol. 40, 58.e17–58.e25. https://doi.org/10.1016/j.urolonc.2021.07.016 (2022).
Donachie, K. et al. What interventions affect the psychosocial burden experienced by prostate cancer patients undergoing active surveillance? A scoping review. Support Care Cancer. 30, 4699–4709. https://doi.org/10.1007/s00520-022-06830-z (2022).
Chien, C. H. et al. Psychosocial adjustments in patients with prostate cancer from pre-diagnosis to six months post-treatment. Int. J. Nurs. Pract. 22, 70–78. https://doi.org/10.1111/ijn.12360 (2016).
Lashbrook, M. et al. Coping strategies used by breast, prostate, and colorectal cancer survivors: a literature review. Cancer Nurs. 41, E23–E39. https://doi.org/10.1097/NCC.0000000000000528 (2018).
Chen, J. J. et al. Family resilience, perceived social support, and individual resilience in cancer couples: analysis using the actor-partner interdependence mediation model. Eur. J. Oncol. Nurs. 52, 101932. https://doi.org/10.1016/j.ejon.2021.101932 (2021).
Luo, Z. et al. Effect of spouse-based self-disclosure intervention on psychological distress and intimate relationship in patients with prostate cancer during radiotherapy. Chin. Nurs. Manag. 22, 1020–1025. https://doi.org/10.3969/j.issn.1672-1756.2022.07.012 (2022).
Yang, H. et al. A qualitative study on care experience of postoperative caregivers of patients with prostatic cancer. Chin. J. Mod. Nurs. 28, 739–744. https://doi.org/10.3760/cma.j.cn115682-20210524-02234 (2022).
Acknowledgements
Thanks to all participants involved in our research for your time, support, and understanding.
Funding
This work was supported by the National Natural Science Foundation of China [72174120].
Author information
Authors and Affiliations
Contributions
Xiuqun Yuan: Data collection and analysis, writing the original draft; Zhiyuan Yu: writing: review and editing; Hongfan Yin: data collection and analysis; Zhihong Yang: data analysis; Min Chen: investigation; Yan Yang: review and editing, project administration.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Yuan, X., Yu, Z., Yin, H. et al. Psychosocial experience of couples coping with prostate cancer: a qualitative study. Sci Rep (2026). https://doi.org/10.1038/s41598-026-38068-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-026-38068-8