Abstract
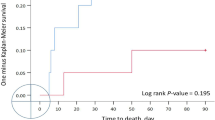
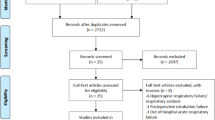
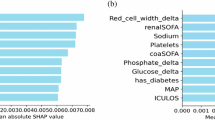
High-flow nasal cannula (HFNC) and non-invasive ventilation(NIV) are commonly used for hypoxemic respiratory failure, but their comparative efficacy remains unclear. This prospective cohort study enrolled 259 non-hypercapnic hypoxemic respiratory failure patients (PaO₂ <60 mmHg, PaCO₂ <50 mmHg, pH ≥ 7.30) in a Chinese ICU. Patients were allocated to HFNC (n = 128) or NIV (n = 131) based on physician judgment. Primary outcome was 28-day intubation rate; secondary outcomes included 28-day mortality, treatment withdrawal, and ICU/hospital stay duration. Baseline characteristics were similar except for higher respiratory/heart rates and disease severity in the NIV group. Before adjustment, the HFNC group had a lower intubation rate (P < 0.05) and fewer events of death or treatment withdrawal(P<0.01). After propensity score matching, all group differences became non-significant: intubation(aOR 2.61,95%CI 0.58–11.68,P = 0.21), hospital mortality (aOR 0.91,95%CI 0.31–2.62,P = 0.86),death or withdrawing treatment༈aOR 0.54,95%CI 0.26–1.13,P = 0.10),and the composite endpoint (aOR = 1.14,95%CI 0.42–3.08, P = 0.80).The durations of ICU stay (8 vs. 8 days, P = 0.87) and hospital stay (13 vs. 12 days, P = 0.10) showed no significant differences both before and after matching.Patients transitioning from HFNC to NIV had longer ICU stays than NIV-only patients (12 vs. 8 days, P < 0.05). Outcomes did not differ between HFNC-failure patients transitioning to NIV or intubation (P > 0.05). HFNC and NIV show similar efficacy in preventing intubation and reducing mortality. NIV may shorten ICU stay in severe cases, but escalation to NIV or intubation after HFNC failure does not improve outcomes. Treatment should be individualized based on disease severity and patient response. However, given the non-randomized design and potential for residual confounding despite multivariate adjustment, these findings should be interpreted with caution and require validation in randomized controlled trials.
Similar content being viewed by others
Data availability
All the data analysed during this study are included in this published article.
References
Bellani, G. et al. Epidemiology, patterns of care, and mortality for patients with acute respiratory distress syndrome in intensive care units in 50 countries. JAMA 315 (8), 788–800 (2016).
Ferreyro, B. L. et al. Association of noninvasive oxygenation strategies with all-cause mortality in adults with acute hypoxemic respiratory failure. JAMA 324 (1), 57 (2020).
Global Initiative for Chronic Obstructive Lung Disease (GOLD). Global Strategy for Prevention, Diagnosis and Management of COPD: 2023 Report. https://goldcopd.org/2023-gold-report-2/
Nava, S., Navalesi, P. & Gregoretti, C. Interfaces and humidification for noninvasive mechanical ventilation. Respir Care. 54 (1), 71–84 (2009).
Cuquemelle, E. et al. Heated and humidified high-flow oxygen therapy reduces discomfort during hypoxemic respiratory failure. Respir Care. 57, 1571–1577 (2012).
Frat, J. P. et al. Sequential application of oxygen therapy via high-flow nasal cannula and noninvasive ventilation in acute respiratory failure: an observational pilot study. Respir Care. 60, 170–178 (2015).
Maggiore, S. M. et al. Nasal high-flow versus venturi mask oxygen therapy after extubation: effects on oxygenation, comfort, and clinical outcome. Am. J. Respir Crit. Care Med. 190, 282–288 (2014).
Ricard, J. D. et al. Use of nasal high flow oxygen during acute respiratory failure. Intensive Care Med. 46, 2238–2247 (2020).
Grieco, D. L. et al. Non-invasive ventilatory support and high-fow nasal oxygen as frst-line treatment of acute hypoxemic respiratory failure and ARDS.Intensive. Care Med. 47, 851–866 (2021).
Frat, J. P. et al. High-flow oxygen through nasal cannula in acute hypoxemic respiratory failure. N Engl. J. Med. 372 (23), 2185–2196 (2015).
Rochwerg, B. et al. .Offcial ERS/ATS clinical practice guidelines: noninvasive ventilation for acute respiratory failure. Eur. Respir J. 50 (2), 1602426 (2017).
Chanques, G. et al. Comparison of three high flow oxygen therapy delivery devices: a clinical physiological cross-over study. Minerva Anestesiol. 79, 1344–1355 (2013).
Corley, A., Caruana, L. R., Barnett, A. G., Tronstad, O. & Fraser, J. F. Oxygen delivery through high-flow nasal cannulae increase end-expiratory lung volume and reduce respiratory rate in post-cardiac surgical patients. Br. J. Anaesth. 107, 998–1004 (2011).
Parke, R. L., Eccleston, M. L. & McGuinness, S. P. The effects of flow on airway pressure during nasal high-flow oxygen therapy. Respir Care. 56, 1151–1155 (2011).
Spicuzza, L. & Schisano, M. High-flow nasal cannula oxygen therapy as an emerging option for respiratory failure: the present and the future. Ther. Adv. Chronic Dis. 11, 2040622320920106 (2020).
Xu, C., Yang, F., Wang, Q. & Gao, W. Comparison of high flow nasal therapy with Non-Invasive ventilation and conventional oxygen therapy for acute hypercapnic respiratory failure: A Meta-Analysis of randomized controlled trials. Int. J. Chron. Obstruct Pulmon Dis. 18, 955–973 (2023).
Frat, J. P., Coudroy, R. & Thille, A. W. Non-invasive ventilation or high-flow oxygen therapy: when to choose one over the other? Respirol. (Carlton Vic). 24 (8), 724–731 (2019).
Munroe, E. S. et al. High-flow nasal cannula vs non-invasive ventilation in acute hypoxia: propensity score matched study. Crit. Care Explor. 6 (5), e1092 (2024).
Ana Carolina Etrusco Zaroni Santos & Caiado, C. M. Alessandra geisler Daud Lopes,et al.Comparison between high-flow nasal cannula (HFNC) therapy and noninvasive ventilation (NIV) in children with acute respiratory failure by bronchiolitis: a randomized controlled trial.BMC pediatrics. 24:595 (2024).
Acknowledgements
The authors would like to thank all the staffs in RICU to participate in data collection.
Funding
This study was supported by the Chongqing Joint Medical Research Program of Science & Health(Project No. 2020FYYX138). The funder had no role in the study design, data collection, statistical analysis, or manuscript writing.
Author information
Authors and Affiliations
Contributions
All the authors participated in the article preparation. The authors read and approved the final manuscript.1.Literature search: Zhao Qianru, Jiang Heyue.2.Data collection: Zhao Qianru, Liu Qiao.3.Study design: Hong Yueling,PanLongfan.4.Data analysis: Duan Jun.5.Manuscript preparation: Hong Yueling, Zhao Qianru, Jiang Heyue.6.Manuscript review: Hong Yueling, Pan Longfang.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
The study was approved by the Ethics Committee of the First Affiliated Hospital of Chongqing Medical University. Written informed consent was obtained from all participants prior to their inclusion in the study.Ethics Number:2020-1.
Consent for publication
The authors confirm that no identifiable personal data are presented in this manuscript. Therefore, consent for publication was not required.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Qianru, Z., Heyue, J., Longfang, P. et al. High-flow nasal cannula versus noninvasive ventilation in patients with hypoxemic respiratory failure: a prospective cohort study. Sci Rep (2026). https://doi.org/10.1038/s41598-026-38516-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-026-38516-5