Abstract
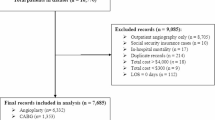
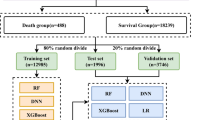
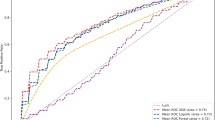
Cardiac tamponade is a rare yet catastrophic complication during atrial fibrillation (AF) catheter ablation. Influenced by multiple procedural and patient-related factors, its prediction remains highly challenging. This study aimed to develop and interpret a machine learning-based predictive model for cardiac tamponade during AF catheter ablation. Data were retrospectively collected from 1481 patients who underwent AF catheter ablation at a tertiary hospital in Nanjing, China, between October 2014 and December 2024. After identifying key predictors of intraoperative cardiac tamponade via least absolute shrinkage and selection operator (LASSO) regression, eight machine learning algorithms were trained using Python libraries. Model performance was evaluated through cross-validation, and SHapley Additive exPlanations (SHAP) analysis was performed to interpret the best-performing model. The XGBoost model exhibited the optimal overall performance, with an area under the curve (AUC) of 0.972 in the training set and 0.908 in internal validation, demonstrating excellent calibration and the highest clinical net benefit. SHAP analysis identified five major predictors: operator experience, D-dimer level, total heparin dose, AF type, and left atrial diameter. These predictors represent multidimensional determinants associated with procedural technique, coagulation status, and cardiac anatomy. The XGBoost-based predictive model showed strong discriminative ability and interpretability for predicting cardiac tamponade during AF catheter ablation, which supports accurate preoperative risk stratification and guides intraoperative management to enhance procedural safety and precision. External validation across multiple centers is required to confirm the generalizability of the model.
Similar content being viewed by others
Data availability
The data used in this study contain sensitive patient information and therefore cannot be made publicly available. However, the corresponding author (BAO Zhipeng) can provide access to the data upon reasonable request.
References
Joglar, J. A. et al. ACC/AHA/ACCP/HRS Guideline for the diagnosis and management of atrial fibrillation: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation 149, e1-e156. https://doi.org/10.1161/cir.0000000000001193 (2024).
Goulart, A. C. et al. The impact of atrial fibrillation and long-term oral anticoagulant use on all-cause and cardiovascular mortality: A 12-year evaluation of the prospective Brazilian study of stroke mortality and morbidity. Int. J. Stroke. 17, 48–58. https://doi.org/10.1177/1747493021995592 (2022).
Farwati, M. et al. Impact of Redo ablation for atrial fibrillation on patient-reported outcomes and quality of life. J. Cardiovasc. Electrophysiol. 34, 54–61. https://doi.org/10.1111/jce.15710 (2023).
Benali, K. et al. Procedure-related complications of catheter ablation for atrial fibrillation. J. Am. Coll. Cardiol. 81, 2089–2099. https://doi.org/10.1016/j.jacc.2023.03.418 (2023).
Deshpande, S. et al. Predictors of morbidity and in-hospital mortality following procedure-related cardiac tamponade. J. Arrhythm. 39, 790–798. https://doi.org/10.1002/joa3.12911 (2023).
du Lavallaz, F. Severe periprocedural complications after ablation for atrial fibrillation: An international collaborative individual patient data registry. JACC Clin. Electrophysiol. 10, 1353–1364. https://doi.org/10.1016/j.jacep.2024.03.024 (2024).
Hamaya, R. et al. Management of cardiac tamponade in catheter ablation of atrial fibrillation: Single-centre 15 year experience on 5222 procedures. Europace 20, 1776–1782. https://doi.org/10.1093/europace/eux307 (2018).
Wu, N. et al. Surgical intervention for cardiac tamponade during atrial fibrillation ablation: Who and when?-A single-center experience. J. Interv. Card Electrophysiol. 62, 373–380. https://doi.org/10.1007/s10840-020-00907-7 (2021).
Arina, P. et al. Prediction of complications and prognostication in perioperative medicine: A systematic review and PROBAST assessment of machine learning tools. Anesthesiology 140, 85–101. https://doi.org/10.1097/aln.0000000000004764 (2024).
Shelley, B. & Shaw, M. Machine learning and preoperative risk prediction: The machines are coming. Br. J. Anaesth. 133, 925–930. https://doi.org/10.1016/j.bja.2024.07.015 (2024).
Bansal, A. et al. Machine learning prediction of pericardial tamponade after atrial fibrillation ablation. Am. J. Cardiol. 175, 179–180. https://doi.org/10.1016/j.amjcard.2022.04.002 (2022).
Li, R. et al. Machine learning-based risk models for procedural complications of radiofrequency ablation for atrial fibrillation. BMC Med. Inf. Decis. Mak. 23, 257. https://doi.org/10.1186/s12911-023-02347-5 (2023).
Riley, R. D. et al. Calculating the sample size required for developing a clinical prediction model. Bmj 368, m441. https://doi.org/10.1136/bmj.m441 (2020).
Collins, G. S. et al. TRIPOD + AI statement: Updated guidance for reporting clinical prediction models that use regression or machine learning methods. Bmj 385, e078378. https://doi.org/10.1136/bmj-2023-078378 (2024).
Doebler, P., Doebler, A., Buczak, P. & Groll, A. Interactions of scores derived from two groups of variables: Alternating Lasso regularization avoids overfitting and finds interpretable scores. Psychol. Methods. 28, 422–437. https://doi.org/10.1037/met0000461 (2023).
Li, P., Stuart, E. A. & Allison, D. B. Multiple imputation: A flexible tool for handling missing data. Jama 314, 1966–1967 (2015). https://doi.org/10.1001/jama.2015.15281
Wang, L., Han, M., Li, X., Zhang, N. & Cheng, H. Review of classification methods on unbalanced data sets. Ieee Access. 9, 64606–64628. https://doi.org/10.1109/ACCESS.2021.3074243 (2021).
Klement, W. & El Emam, K. Consolidated reporting guidelines for prognostic and diagnostic machine learning modeling studies: Development and validation. J. Med. Internet Res. 25, e48763. https://doi.org/10.2196/48763 (2023).
Friedman, D. J. et al. Predictors of cardiac perforation with catheter ablation of atrial fibrillation. JACC Clin. Electrophysiol. 6, 636–645. https://doi.org/10.1016/j.jacep.2020.01.011 (2020).
Tsiachris, D. et al. Effectiveness and safety of a time to isolation strategy of cryoballoon ablation of atrial fibrillation: A systematic review and meta-analysis. J. Cardiovasc. Electrophysiol. 33, 2640–2648. https://doi.org/10.1111/jce.15697 (2022).
Loh, P. et al. Feasibility and safety of single-pulse ablation in 20 patients with atrial fibrillation. Heart Rhythm. https://doi.org/10.1016/j.hrthm.2025.05.054 (2025).
Luo, A. et al. Machine learning in the management of patients undergoing catheter ablation for atrial fibrillation: Scoping review. J. Med. Internet Res. 27, e60888. https://doi.org/10.2196/60888 (2025).
Shade, J. K. et al. Preprocedure application of machine learning and mechanistic simulations predicts likelihood of paroxysmal atrial fibrillation recurrence following pulmonary vein isolation. Circ. Arrhythm. Electrophysiol. 13, e008213. https://doi.org/10.1161/circep.119.008213 (2020).
Tang, S. et al. Machine learning-enabled multimodal fusion of intra-atrial and body surface signals in prediction of atrial fibrillation ablation outcomes. Circ. Arrhythm. Electrophysiol. 15, e010850. https://doi.org/10.1161/circep.122.010850 (2022).
Zhong, X. et al. Development and interpretation of a machine learning risk prediction model for post-stroke depression in a Chinese population. Sci. Rep. 15, 28602. https://doi.org/10.1038/s41598-025-09322-2 (2025).
Talbot, H. et al. Interactive training system for interventional electrocardiology procedures. Med. Image Anal. 35, 225–237. https://doi.org/10.1016/j.media.2016.06.040 (2017).
Fink, T. et al. Outcome of cardiac tamponades in interventional electrophysiology. Europace 22, 1240–1251. https://doi.org/10.1093/europace/euaa080 (2020).
Samuel, M., Rienstra, M. & Van Gelder, I. C. Ablation of persistent atrial fibrillation: Never say never again. Eur. Heart J. 45, 2617–2619. https://doi.org/10.1093/eurheartj/ehae374 (2024).
Liu, N. et al. Association between the use of contact force-sensing catheters and cardiac tamponade in atrial fibrillation ablation. J. Interv Card Electrophysiol. 55, 137–143. https://doi.org/10.1007/s10840-019-00516-z (2019).
Deshpande, S. et al. Impact of intracardiac echocardiography on readmission morbidity and mortality following atrial fibrillation ablation. J. Cardiovasc. Electrophysiol. 33, 2496–2503. https://doi.org/10.1111/jce.15683 (2022).
Acknowledgements
We sincerely thank all the medical staff and participants from the First Affiliated Hospital with Nanjing Medical University for their valuable contributions.
Funding
This study was supported by the National Natural Science Foundation of China (No. 72074124), the Jiangsu Youth Science and Technology Talent Promotion Project (JSTJ-2025-386), the Institute for Hospital Reform and Development of Nanjing University (NDYG052), and the Youth Foundation Cultivation Program of the National Natural Science Foundation at Jiangsu Provincial People’s Hospital (PY2022002).
Author information
Authors and Affiliations
Contributions
Z.B. and L.Z. served as the primary coordinators of this project, overseeing the study design and overall project management. L.Z. and H.G. were responsible for drafting the manuscript. Y.Z. and W.S. contributed to data collection and stratification supervision. Y.L. and J.W. assisted with data compilation and statistical analysis. Z.B. and G.S. were involved in manuscript revision and securing research funding. All authors made substantial contributions to the study and approved the final submitted manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
This study was approved by the Ethics Committee of the First Affiliated Hospital with Nanjing Medical University (2024-SRFA-210). As this was a retrospective observational study, the requirement for informed consent was waived, and all patient identifiers were rigorously anonymized. All procedures in this study adhered to the ethical standards of the institutional committee and to the 1964 Declaration of Helsinki and its subsequent amendments. The prediction model was developed in line with the latest TRIPOD + AI statement (Transparent Reporting of a Multivariable Prediction Model for Individual Prognosis or Diagnosis + Artificial Intelligence)14.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Zhou, L., Zhao, Y., Song, W. et al. Explainable machine learning for risk prediction of acute cardiac tamponade during atrial fibrillation ablation. Sci Rep (2026). https://doi.org/10.1038/s41598-026-40302-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-026-40302-2