Abstract
The effectiveness of digital health management (DM) in post-discharge care for patients with coronary artery disease (CAD) remains insufficiently explored, particularly across public health emergencies. A total of 24,129 patients with CAD enrolled in the HeartMed Digital Management System were divided into DM or conventional management groups based on patient preference, and categorized into pre-COVID-19 (n = 13,473; 16.7% DM), COVID-19 (n = 5173; 80.3% DM), and post-COVID-19 (n = 5483; 86.2% DM) eras according to enrollment dates. For the primary endpoint, digital healthcare was significantly associated with lower all-cause mortality risk across all three periods after adjustment (HR: pre-COVID 0.23; COVID 0.52; post-COVID 0.58; all p < 0.001). No significant interaction was found in the protective effect of DM among the three eras (all interaction p > 0.05). Similar trends were observed for the secondary endpoints—readmission, MACE, and MACCE. Across all three pandemic phases, DM was consistently associated with improved clinical outcomes in post-discharge CAD populations.
Similar content being viewed by others
Introduction
Coronary artery disease (CAD) is one of the leading causes of mortality and disability worldwide, continually imposing a substantial burden on healthcare systems across countries1,2. Although the intensified efforts in prevention and significant advancements in diagnosis and treatment in recent years have effectively reduced adverse events among CAD patients, the discharged patients under the traditional outpatient care model still face numerous challenges—inadequate health education, persistent unhealthy lifestyle behaviours, suboptimal risk factor control, and poor medication adherence—all of which significantly impact the long-term prognosis of patients with CAD3,4.
In recent years, digital healthcare has demonstrated tremendous potential in the management of chronic diseases5,6. Studies have suggested that digital health management, leveraging mobile devices or online software, can effectively enhance self-management behaviours and improve clinical outcomes among patients with CAD7,8. Nonetheless, existing evidence is primarily derived from high-income countries and remains limited by factors such as singular intervention strategies, small sample sizes, short intervention durations, and inadequate follow-up periods8. With ongoing technological advancements, digital post-discharge management is evolving toward greater refinement, long-term implementation, and comprehensive coverage. Throughout the management process, it is also essential to account for the diversity of cultural differences, lifestyle habits, geographic distances, and economic conditions across various regions9. Consequently, large-scale real-world studies are still needed to comprehensively assess the clinical effectiveness of electronic post-discharge management, thereby addressing the current gaps in secondary prevention for CAD patients.
The outbreak of COVID-19 has posed unprecedented challenges to global healthcare systems10. In addition to straining medical resources, the COVID-19 pandemic has significantly disrupted and hindered traditional face-to-face outpatient follow-up management models. Against this unique backdrop, utilizing digital and intelligent approaches for post-discharge management has become particularly crucial11,12,13. Despite the considerable potential of digital health management in improving the long-term prognosis of patients with CAD, systematic research specifically evaluating its role during public health emergencies remain lacking. Notably, the end of the COVID-19 pandemic does not signify the complete elimination of its threats. Ongoing preparedness for potential public health emergencies remains in future essential.
Therefore, this study aims to investigate the impact of digital post-discharge management on the clinical outcomes of post-discharge CAD patients across different periods—pre-COVID-19 pandemic era, COVID-19 pandemic era, and post-COVID-19 pandemic era—to evaluate its applicability and prospects for broader implementation in the context of public health emergencies. Our study not only contributes to evaluating the role and effectiveness of digital management in post-discharge patients with CAD but also provides practical evidence and theoretical support for utilizing an efficient and sustainable post-discharge digital management system under similar future public health emergencies.
Results
Baseline characteristics
The study cohort comprised 24,129 participants, with a median age of 63 years (IQR, 55–71), and 70.0% were male. Of these, 346 participants (1.4%) were lost to follow-up. A total of 13,473 participants were in the pre-COVID-19 Pandemic Era, with 2256 (16.7%) selecting Digital Health Management. In the COVID-19 Pandemic Era, there were 5173 participants, of whom 4156 (80.3%) chose Digital Health Management. 5483 participants were included in the post-COVID-19 Pandemic Era, with 4724 (86.2%) in DM group (Table 1). Moreover, individuals opting for Digital Health Management tended to be younger, have fewer comorbidities, and exhibit healthier lifestyle habits, yet they had more severe coronary artery conditions and a higher proportion underwent PCI in general (Table S3).
Clinical outcome evaluation
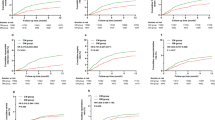
In all stages of the pandemic, the incidence and risk of endpoint events in the DM group was lower than those in the CM group (Table S4, Fig. 1, Fig. S3). In the pre-COVID-19 era, the adverse event rates in the Digital Health Management group compared to the Conventional outpatient group were as follows: readmission (9.31% vs 11.71%), all-cause mortality (1.91% vs 2.67%), MACE (3.99% vs 4.97%), and MACCE (6.96% vs 9.25%). During the COVID-19 era, the event rates for the Digital Health Management group, in contrast with the Conventional outpatient group, were as follows: readmission (8.78% vs 12.00%), all-cause mortality (1.28% vs 2.26%), MACE (2.33% vs 4.62%), and MACCE (5.82% vs 7.47%). Regarding the post-COVID-19 era, the event rates for the Digital Health Management group were as follows, in comparison to the Conventional outpatient group: readmission (9.14% vs 13.57%), all-cause mortality (1.59% vs 2.77%), MACE (3.56% vs 5.93%), and MACCE (6.52% vs 9.09%). To further quantify the clinical benefits, the absolute risk reduction (ARR) and number needed to treat (NNT) were calculated for each endpoint. For the primary endpoint, the ARR of all-cause mortality was 0.76%, 0.98%, and 1.18% in the pre-COVID-19, COVID-19, and post-COVID-19 periods, respectively, corresponding to NNTs of 132, 102, and 85. Meanwhile, for the composite endpoint MACCE, the ARR across the same periods was 2.29%, 1.65%, and 2.57%, with corresponding NNTs of 44, 61, and 39 (Table S4).
This figure illustrates the cumulative incidence of adverse clinical events, unadjusted for covariates. Group differences were evaluated using the log-rank test. The adverse events, arranged from top to bottom, are: readmission, all-cause mortality, MACE, and MACCE. The pandemic phases, arranged from left to right, are: pre-COVID-19 pandemic era, COVID-19 pandemic era, and post-COVID-19 pandemic era.
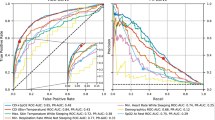
According to univariate Cox analysis, digital health management was associated with a significant reduction in the primary endpoint, all-cause mortality, compared to conventional follow-up. Specifically, in the pre-COVID-19 pandemic era (HR, 0.70; 95% CI, 0.51–0.97), COVID-19 pandemic era (HR, 0.56; 95% CI, 0.34–0.91), and post-COVID-19 pandemic era (HR, 0.57; 95% CI, 0.35–0.92). Significant associations were also observed between digital health management and low risks of secondary endpoints, including readmission, MACE, and MACCE. After fully adjusting for demographic indicators, physical examination, lifestyle factors, comorbidities, laboratory parameters, and coronary interventions, the associations remained significant (Fig. 2). In the pre-pandemic era, compared to conventional follow-up, digital health management was linked to a reduced incidence of clinical events, including readmission (HR, 0.76; 95% CI, 0.65–0.88), all-cause mortality (HR, 0.23; 95% CI, 0.16–0.33), MACE (HR, 0.64; 95% CI, 0.51–0.81), and MACCE (HR, 0.56; 95% CI, 0.47–0.67). Similarly, digital health management was associated with a lower risk of readmission (HR, 0.72; 95% CI, 0.58–0.89), all-cause mortality (HR, 0.52; 95% CI, 0.31–0.86), MACE (HR, 0.51; 95% CI, 0.36–0.73), and MACCE (HR, 0.70; 95% CI, 0.54–0.91) during the pandemic era. After the COVID-19 pandemic, digital health management remained associated with reduced risks of readmission (HR, 0.66; 95% CI, 0.53–0.82), all-cause mortality (HR, 0.58; 95% CI, 0.36–0.94), MACE (HR, 0.62; 95% CI, 0.44–0.86), and MACCE (HR, 0.71; 95% CI, 0.55–0.93).
Sensitivity analyses and interaction analysis
The primary finding—digital health management was associated with reduced risk of readmission, all-cause mortality, MACE, and MACCE events in CAD patients—remained robust across sensitivity analyses (Table S5). With respect to the primary endpoint, all-cause mortality, similar associations were observed after excluding participants with missing data in the pre-COVID-19 pandemic era (HR, 0.24; 95% CI, 0.16–0.36), COVID-19 pandemic era (HR, 0.46; 95% CI, 0.27–0.79), and post-COVID-19 pandemic era (HR, 0.58; 95% CI, 0.36–0.94). Meanwhile, after further adjusting for medication use, the effect remained significant in the pre-COVID-19 pandemic era (HR, 0.24; 95% CI, 0.17–0.34), COVID-19 pandemic era (HR, 0.54; 95% CI, 0.33–0.89), and post-COVID-19 pandemic era (HR, 0.57; 95% CI, 0.35–0.82). Similarly, the three secondary endpoints retained their significance in these sensitivity analyses. Additionally, PSM was performed separately within each pandemic phase to balance baseline characteristics between the DM and CM groups. After matching, all SMDs were below 0.01, indicating excellent covariate balance (Table S6). Multivariable Cox regression models were re-applied to the matched cohorts, and the associations between digital management and clinical outcomes remained consistent with the primary analyses across all phases. Specifically, digital management was associated with a lower risk of all-cause mortality in the pre-COVID-19 pandemic era (HR, 0.54; 95% CI, 0.34–0.86), the COVID-19 pandemic era (HR, 0.37; 95% CI, 0.17–0.81), and the post-COVID-19 pandemic era (HR, 0.38; 95% CI, 0.17–0.86). Similar patterns were observed for three secondary endpoints, further supporting the robustness of the findings.
The results of the interaction analysis revealed no significant interaction between pandemic phase and digital health management (all P for interaction >0.05; Table S7). This suggests that the observed reductions in readmission, all-cause mortality, MACE, and MACCE associated with digital health management remained consistent across all phases of the COVID-19 pandemic.
Discussion
Digital health management, utilizing technologies such as the internet, mobile terminals, and intelligent cloud platforms, stands as a highly promising approach to post-discharge chronic disease management. To the best of our knowledge, HeartMed is currently the largest reported cohort on the long-term management of CAD patients using a digital healthcare system, and this study is the first to evaluate the clinical benefits of digital post-discharge management on long-term outcomes across different phases of the COVID-19 pandemic, specifically focusing on the effectiveness of digital health management during public health emergencies. In this study, which thoroughly evaluates the role of digital health management in post-discharge management for the CAD population across different pandemic phases, we found: (I) With the evolving times, the advancement of internet technology, and the experience of the COVID-19 pandemic, there has been an increasing recognition and adoption of digital health management, leading to growing acceptance and proactive selection of digital health management shift from traditional outpatient follow-up. (II) Digital health management consistently showed associations with reduced risks of all-cause mortality, readmission, MACE, and MACCE across all pandemic phases in patients with CAD. (III) In addition, the associations between digital health management and clinical outcomes did not differ significantly across different pandemic periods, suggesting its potential as an effective strategy for managing chronic disease populations during public health crises.
In the past decade, the application of digital technologies for improving chronic disease management has been preliminarily explored, demonstrating promising results and proving effective in enhancing symptom management and patient adherence as research advances5,6,14. In recent years, digital health management technologies have benefited from advancements in information technology—such as Internet Plus, big data, cloud computing—gradually evolving from text messages (SMS)—and call-based management to well-designed, sophisticated online programs, with current efforts exploring the integration of AI technologies12,15. During the COVID-19 pandemic, both in China and worldwide, the integration of internet technologies into existing healthcare systems accelerated significantly, leading to a wide range of practical applications. Even in the post-pandemic era, these technologies continue to evolve and advance15,16,17. Our research indicates that as society advances, particularly after experiencing the COVID-19 pandemic—a period that catalysed broader exposure to Internet-based healthcare—the acceptance and preference for digital health management have been increasing year by year in the Chinese population, especially among younger individuals. Meanwhile, a 2024 survey conducted in Germany revealed that approximately 84% of cardiovascular patients, particularly those under the age of 63, were willing to use health-related mobile applications (apps) as a form of health support, aligning with our research findings16,18. Objective factors, such as technological advancements and the accumulation of early user experience feedback data, have contributed to the continued refinement of more user-friendly and precise digital health management systems. Meanwhile, pandemic-driven adaptation and increasing user acceptance have supported the broader adoption and continued use of digital health management platforms19,20. Consequently, driven by these factors, an increasing number of post-discharge patients are opting for digital health management as a replacement for traditional outpatient follow-ups.
The implementation of digital healthcare in the long-term management of CAD still faces several challenges worldwide. A meta-analysis suggests that digital health programs were associated with lower hospital readmissions among post-discharge CAD patients, yet no significant decrease has been observed in MACE or mortality8. Nevertheless, in currently published relevant studies, the main method of digital health interventions remains SMS or telephone-based, and the intervention duration is generally not sustained throughout the entire course, most commonly lasting 12 to 24 weeks8,21,22. Additionally, the follow-up period is relatively short, with most studies covering six months or less23,24. In contrast, the present study exhibits several noteworthy and innovative strengths. Chief among them is its large sample size, extended temporal span, and long-term follow-up, enabling a more comprehensive evaluation of the real-world effectiveness of digital health interventions. As is well established, standard post-discharge management of CAD typically consists of lifestyle modifications, risk factor control, secondary preventive medication use, and symptom management25. Across these critical domains, this study adopts multidimensional and continuous intervention strategies that could help address the potential limitations observed in prior research and shows promise in enhancing patient adherence and improving long-term outcomes, through thoughtfully incorporating and integrating the following key elements: (1) Personalization: Given the variability in patients’ risk factors and disease conditions, a personalized management approach—encompassing tailored rehabilitation frequency, intensity, and specific targets—is crucial. However, many digital health solutions still follow a ‘one-size-fits-all’ model, where all patients adhere to similar programmes26, with limited adaptation based on real-time patient feedback27. Notably, several innovative personalized management strategies—such as individualized action planning, graded task assignments, and peer-supported interventions—have recently revealed strong feasibility and acceptability, pointing to promising directions for enhancing digital intervention effectiveness28,29. (2) Continuous Long-Term Management: Post-discharge management for CAD patients is a prolonged and complex process, yet many studies provide health-related information only during the initial months after discharge, without extending support throughout the full follow-up period. This limited coverage may contribute to diminished patient adherence and even the neglect or loss of critical medical guidance and information30,31. (3) Diversified and Targeted Information Delivery: Relying solely on SMS and push notifications, as seen in many current studies, is far from sufficient. Effective digital health management requires a multi-format and multi-channel approach to information delivery, and direct online access to professional cardiologists, when needed, can significantly improve patient awareness and adherence to recommended health advice. Otherwise, monotonous and excessive medical advice risks becoming overwhelming ‘information overload’ with limited practical value8,24,32. (4) Dynamic Monitoring and Real-Time Feedback: CAD can progress rapidly, so in addition to actively reporting symptoms, connecting patients to daily and professional monitoring devices is crucial for tracking activity levels and vital signs enables dynamic tracking of health status. By consistently observing these parameters and promptly alerting healthcare professionals when abnormalities arise, potential crises can be anticipated, and adverse events mitigated. A meta-analysis has also demonstrated that integrating remote consultation with remote monitoring significantly reduces cardiovascular mortality and hospitalizations in heart failure patients33. This supports the emerging view in current research that digital health technologies—particularly remote monitoring—when deeply integrated with enhanced clinician-patient interaction frameworks, may play a pivotal role in improving intervention efficacy21,34. In addition, this digital management model may offer several potential benefits that are not easily quantify. For instance, features such as campaign reminders, risk stratification, two-way information exchange, and video-based educational content likely play a role in improving the quality of post-discharge management. It is worth noting that, with advancements in internet-related technologies and the integration of AI, digital health management systems could undergo continuous upgrades. Our findings indicate that current digital health management systems are associated with favourable clinical outcomes inpatients with CAD. Along with further advancements in internet and AI technologies, future iterations of these systems may hold the potential to further improve CAD patient outcomes.
Reflecting on successful experience in combating the COVID-19 outbreak in China, various digital healthcare initiatives—Internet Plus Health Care Service Pattern, Internet Hospitals, and Telemedicine—were implemented to meet patient needs amid restrictions on movement and social activities. These digital health models were reported to provide patients with accessible and high-quality medical services, offering valuable support for pandemic control efforts12,35. However, limited evidence exists regarding performance of digital health management for post-discharge CAD patients during the COVID-19 pandemic. Digital health management approach under pandemic conditions shares similarities with the previously mentioned Internet Plus-based healthcare strategies, while also providing more comprehensive symptom and vital sign monitoring, and offering more personalized, and timely medical advice in certain aspects. Our findings fill this gap by demonstrating that, even during the COVID-19 pandemic, digital health management was associated with lower readmission rates and fewer cardiovascular adverse events in patients with CAD. This presents a viable strategy for optimizing post-discharge management and enhancing CAD patient outcomes in future public health emergencies.
Several limitations should still be considered when interpreting our conclusions. Firstly, the inherent limitations of observational studies restrict the ability to confirm the causal relationship between digital health management and the reduction of clinical endpoint events under different phases of the pandemic. Moreover, the nature of observational studies also prevents completely ruling out the possibility of residual confounding. Secondly, from the perspective of baseline characteristics, the potential for selection bias must be considered. Consistent with previous studies, participants in the DM group may have been younger and more health-conscious36,37. Although relevant factors were adjusted in Cox regression models and a sensitivity analysis using PSM was performed to confirm the robustness of the findings, the influence of these factors could not be fully eliminated. Meanwhile, the findings of this study may remain susceptible to unmeasured or residual confounders that were not accounted for in the present analysis, either due to their absence in the dataset or the lack of validated assessment tools—such as participants’ socioeconomic status, educational attainment, digital literacy, trust in the healthcare system, and communication preferences. As reported in previous studies, these factors may not only shape an individual’s willingness or ability to engage with digital health services, but also impact how frequently and effectively digital healthcare tools are used36,38,39. Therefore, when interpreting the actual effects of DM interventions, the potential dual impact of these variables—both on the likelihood of selecting into DM and on subsequent clinical outcomes—should be carefully considered. In light of the above two points, subsequent randomized controlled trials required to be designed to further explore and validate the causal relationship of digital health management models in populations with chronic diseases. Thirdly, regarding the generalizability of the study’s conclusions, the study sample is confined to a Chinese population. As a result, the applicability of the findings to patients in other countries and regions is constrained. The implementation and dissemination of digital health management across different countries and populations are profoundly influenced by variations in cultural contexts, healthcare system structures, and digital infrastructure. In low- and middle-income countries, low-income individuals, immigrants, and ethnic minorities are particularly at greater risk of “digital exclusion” due to limited access to digital devices, unstable internet connections, and inadequate digital literacy40,41. Compounding these challenges are healthcare providers’ insufficient digital competencies and outdated organizational models of healthcare delivery, which collectively hinder the integration of digital health strategies42,43. Addressing these barriers requires not only strengthening technological infrastructure but also optimizing the organization and delivery of healthcare services. Bridging the digital divide and promoting digital equity remain critical global challenges21. Consequently, further studies across diverse countries and populations are warranted to validate the transferability and broader applicability of digital management strategies beyond the Chinese setting. In addition, as this study focuses solely on CAD, the observed benefits of digital health management are limited to this population. Digital health management systems for other chronic diseases require further design and their effectiveness still needs exploration.
In conclusion, with the evolving times and advancements in internet technology, coupled with having experienced the COVID-19 pandemic, there has been a growing preference for digital health management follow-up over conventional outpatient follow-up. Regardless of the pandemic phase—whether pre-COVID-19, during the COVID-19 pandemic, or post-COVID-19—consistent associations were observed between digital health management and reduced risks of all-cause mortality, readmission, MACE, and MACCE in CAD populations. Moreover, the impact of digital health management remained stable across different pandemic phases, highlighting its potential role in providing an effective approach to managing chronic disease populations in the face of public health crises. These findings suggest that digital health management follow-up is a practical and feasible approach, with superior management outcomes compared to conventional follow-up in CAD populations, both under routine and exceptional circumstances.
Methods
Data source and sample
The “HeartMed Digital Management System” is a nationwide post-discharge management platform designed for cardiovascular disease patients, primarily those with coronary artery disease (CAD). Depending on the participants’ preferences and selection, the system offers a one-year follow-up either through conventional outpatient visits or Digital Health Management. Patient visits and follow-up data are recorded through connected medical records, digital management systems and telephone consultations.
Data from 26,402 participants were available in the current HeartMed Digital Management System. This study primarily focuses on patients with coronary artery disease (Table S1). Based on strict inclusion and exclusion criteria (detailed in the Supplementary Material), a total of 24,129 participants were included in the main analysis (Fig. 3). Subsequently, through standardized procedures and permissions, the following data for this population were obtained for further analysis: diagnoses, demographic information, physical examination findings, lifestyle factors, comorbidities, laboratory and examination parameters, coronary interventions, and follow-up records.
Ethics review
The Ethics Committee of Fuwai Hospital, Chinese Academy of Medical Sciences, approved this study (Approval No. 2023-2210). The study has been designed and conducted in accordance with the principles outlined in the Declaration of Helsinki and other relevant ethical guidelines.
Follow-up management approaches
Based on participants’ selection, participants were divided into the digital management group (DM group) and the conventional management group (CM group), each receiving a different follow-up approach over the one-year period. Patients in the DM group primarily received systematic and refined post-discharge electronic health management through an internet-based platform, which offers medical assistance and interventions in various aspects, including (Fig. 4):
The HeartMed Medical Digital Management System integrates smartphones, wearable devices, and medical data platforms to enhance secondary prevention of CAD. By enabling bidirectional data exchange between participants and caregivers, the system facilitates educational knowledge transmission, real-time risk factor assessment, personalized lifestyle and rehabilitation reminders, medication tracking, and follow-up appointment alerts. Additionally, the system can dynamically modify health management strategies in accordance with risk stratification and provide personalized disease management plans along with healthy lifestyle recommendations.
(I) Symptom management: health managers provided regular health education to improve patients’ disease awareness and adherence to post-discharge management. Patients were also monitored through a digital platform, with a chip-implanted sphygmomanometer for real-time tracking of blood pressure and pulse. New or worsening symptoms, when reported by patients in real-time, triggered alerts to health managers. Clinical evaluations were conducted through telemedicine, with decision support from cardiologists sought when needed.
(II) Clinical evaluation: The system stratified patients by risk level to tailor management frequency and intensity, with regular monitoring of vital signs and symptom surveys. Abnormal data were automatically transmitted to health managers and the doctor’s assistant for early detection of life-threatening complications, such as bleeding and heart failure. Any abnormal data or potential risks would be promptly addressed, with the patient contacted either through the system or by phone.
(III) Lifestyle intervention: Patients received regular follow-up calls to monitor progress and adjust lifestyle interventions. Tailored daily exercise programs were provided based on physical activity levels and disease status, while personalized meal plans generated by artificial intelligence (AI) were provided. Smart devices tracked dietary intake and exercise levels accurately, facilitating better assessment and management. Personalized guidance was provided for different patient groups, such as psychological counselling, therapy, and medication for those with mental health issues, as well as sleep hygiene education for patients with sleep disturbances.
(IV) Risk factor control: For smokers, the system provided smoking cessation guidance and relevant educational materials. It also updated dietary and exercise plans in real-time based on blood glucose and lipid levels uploaded, with treatment reviewed as appropriate.
(V) Medication management: The system tracked medication types, names, and dosages daily, sending reminders to ensure correct usage. It recorded medication adherence, flagged potential adverse drug reactions, and made timely adjustments as needed.
Regarding the CM group, which followed the current conventional clinical process, patients received routine outpatient visits based on discharge instructions. Doctors provided education on CAD secondary prevention, guided proper medication use, and recommended regular follow-ups.
COVID-19 pandemic era
The classification of participants into different eras is based on two key milestones in the COVID-19 epidemic in China. The government implemented the Wuhan lockdown on January 23, 2020, marking the start of the COVID-19 epidemic, while the National Health Commission of China lifted preventive and control measures on January 8, 2023, signalling the end of the epidemic10,44. Accordingly, participants enrolled before January 23, 2020, are considered part of the pre-COVID-19 pandemic era, those enrolled after January 8, 2023, as the post-COVID-19 pandemic era, and the period between these two dates is defined as the COVID-19 pandemic era.
Covariates and endpoints design
To analyze the association between digital management and clinical outcomes, five main groups of potential confounders were considered according to a priori defined directed acyclic graphs (Fig. S1): (I) Demographic Indicators & Physical Examination: Age, Sex, Body Mass Index (BMI), Heart Rate (HR); (II) Lifestyle Factors: Smoking Status, Alcohol Consumption Status; (III) Comorbidities: Acute Coronary Syndrome, Hypertension, Hyperlipidemia, Diabetes Mellitus, Heart Failure, Stroke, Chronic Kidney Disease; (IV) Laboratory Parameters: Ejection Fraction (EF), Estimated Glomerular Filtration Rate (eGFR), Low-Density Lipoprotein Cholesterol (LDL-C); (V) Coronary Intervention: Multi-Vessel Disease, Percutaneous Coronary Intervention (PCI).
All patients were followed for 12 months as scheduled. The primary endpoint was defined as all-cause mortality, while secondary endpoints included readmission, major adverse cardiovascular events (MACE, composite cardiovascular mortality, non-fatal myocardial infarction, and non-fatal stroke), and major adverse cardiac and cerebrovascular events (MACCE, composite endpoint event of all-cause mortality, non-fatal myocardial infarction, revascularization, and non-fatal stroke)45 (detailed in Supplementary Material).
Statistical analyses
The baseline characteristics of the study population were presented from two classification perspectives: participants grouped by different phases of the COVID-19 pandemic (Table 1, Table S2) and participants categorized by follow-up method (Table S3). Data are presented as mean (SD), median (IQR), or counts (percentages), as appropriate. Differences between variables were evaluated using the Kruskal-Wallis rank sum test, Wilcoxon rank sum test, or Pearson’s chi-squared test, depending on the data type and distribution. Follow-up time was defined as the period from enrollment to the occurrence of the corresponding endpoint or one year of event-free follow-up. To minimize bias due to missing data, covariates with more than 5% missingness were excluded from the analysis (Fig. S2). For the remaining variables, missing values were imputed using multiple imputation by chained equations, generating five complete datasets. Subsequent analyses were performed on each dataset, and results were pooled using Rubin’s rules to produce valid statistical inferences (detailed in Supplementary Material). The imputed datasets served as the primary dataset for subsequent analyses.
Cumulative risk curves were used to compare the risk of the four endpoint events in CM group and DM group. The log-rank test was applied to assess group differences. Hazard ratios (HRs) and 95% confidence intervals (CIs) were calculated through Cox proportional hazard regression analyses. The proportional hazards assumption was assessed using Schoenfeld residuals, and no significant violations were detected (all p-values > 0.05). After that, to adequately control for potential confounders, the aforementioned covariates were fully adjusted in the multivariate analyses. Additionally, three sensitivity analyses were conducted: (1) Participants with missing covariate data were excluded instead of imputing the missing values, thereby limiting our analysis to the population with complete data; (2) Medication use was further included in the adjustment model to account for its potential influence on the observed associations; (3) Although covariate adjustment was performed in the multivariable Cox models, the baseline differences between the DM and CM groups may still introduce residual confounding. To further reduce potential selection bias, propensity score matching (PSM) was conducted as a sensitivity analysis. Matching was performed separately within each of the three pandemic phases to ensure within-phase comparability. For each of the three pandemic phases, 1:1 nearest neighbor matching without replacement was conducted between DM and CM patients. The propensity score was estimated using a logistic regression model with management group (DM vs. CM) as the outcome variable and baseline demographic indicators, physical examination findings, lifestyle factors, comorbidities, laboratory measurements, and coronary intervention history as predictors. Matching quality was assessed using standardized mean differences (SMDs), with an SMD < 0.1 indicating acceptable balance between groups (detailed in Supplementary Material). Cox regression models were then re-applied to the matched datasets to assess the robustness of the primary findings.
To further investigate the relationship between different pandemic phases and digital health management, an interaction analysis was performed. Specifically, the interaction between COVID-19 pandemic phases and digital health management was assessed in relation to the risk of clinical events. The interaction term between the pandemic phase and digital health management was incorporated into multivariate Cox proportional hazards regression models. The significance of the interaction effect was evaluated by examining the p-value of the interaction term46. Statistical significance was set at a two-tailed P-value < 0.05. All analyses were conducted using R version 4.2.2 (R Project for Statistical Computing, Vienna, Austria).
Data availability
The datasets generated and analyzed in the study are not publicly available due to institutional policy and the privacy of study individuals, but are available from the corresponding author upon request under the data-sharing agreements between institutions.
References
Malakar, A. K. et al. A review on coronary artery disease, its risk factors, and therapeutics. J. Cell. Physiol. 234, 16812–16823 (2019).
Stolpe, S., Kowall, B. & Stang, A. Decline of coronary heart disease mortality is strongly effected by changing patterns of underlying causes of death: an analysis of mortality data from 27 countries of the WHO European region 2000 and 2013. Eur. J. Epidemiol. 36, 57–68 (2021).
Magnussen, C. et al. Global effect of modifiable risk factors on cardiovascular disease and mortality. N. Engl. J. Med. 389, 1273–1285 (2023).
Salzwedel, A. et al. Effectiveness of comprehensive cardiac rehabilitation in coronary artery disease patients treated according to contemporary evidence based medicine: update of the Cardiac Rehabilitation Outcome Study (CROS-II). Eur. J. Prev. Cardiol. 27, 1756–1774 (2020).
Zhang, P. et al. Improving the management of type 2 diabetes in China using a multifaceted digital health intervention in primary health care: the SMARTDiabetes cluster randomised controlled trial. Lancet Reg. Health West. Pac. 49, 101130 (2024).
Zhang, X., Luo, Z., Yang, M., Huang, W. & Yu, P. Efficacy and safety of digital therapeutics-based cardiac rehabilitation in heart failure patients: a systematic review. ESC Heart Fail. 9, 3751–3760 (2022).
Akinosun, A. S. et al. Digital technology interventions for risk factor modification in patients with cardiovascular disease: systematic review and meta-analysis. JMIR mHealth uHealth 9, e21061 (2021).
Braver, J., Marwick, T. H., Oldenburg, B., Issaka, A. & Carrington, M. J. Digital health programs to reduce readmissions in coronary artery disease. A Syst. Rev. Meta-Anal. Jacc. Adv. 2, 100591 (2023).
Ramasawmy, M., Khan, N., Sunkersing, D. & Banerjee, A. Understanding ethnic inequalities in the design and implementation of digital health interventions for cardiometabolic disease: a qualitative study. Lancet 402(Suppl 1), S78 (2023).
Zhang, Z. et al. Trajectory of COVID-19 response and management strategy in China: scientific rationale driven strategy adjustments. Front. Med. 18, 19–30 (2024).
Digital health and COVID-19. Bull. World Health Organ. 98, 731–732 (2020).
Huang, M., Wang, J., Nicholas, S., Maitland, E. & Guo, Z. Development, status quo, and challenges to China’s health informatization during COVID-19: evaluation and recommendations. J. Med. Internet Res. 23, e27345 (2021).
Whitelaw, S., Mamas, M. A., Topol, E. & Van Spall, H. G. C. Applications of digital technology in COVID-19 pandemic planning and response. Lancet Digit. Health 2, e435–e440 (2020).
Li, Y. et al. Effects on adherence to a mobile app-based self-management digital therapeutics among patients with coronary heart disease: pilot randomized controlled trial. JMIR mHealth uHealth 10, e32251 (2022).
Ting, D. S. W., Carin, L., Dzau, V. & Wong, T. Y. Digital technology and COVID-19. Nat. Med. 26, 459–461 (2020).
Buhr, L., Schicktanz, S. & Nordmeyer, E. Attitudes toward mobile apps for pandemic research among smartphone users in Germany: national survey. JMIR mHealth uHealth 10, e31857 (2022).
Zhang, G. W. et al. In-depth examination of the functionality and performance of the internet hospital information platform: development and usability study. J. Med. Internet Res. 26, e54018 (2024).
Oettinger, V. et al. Development of a patient-centered app in Germany as a special health and organizational support by surveying patients with cardiovascular diseases. Clin. Res. Cardiol. https://doi.org/10.1007/s00392-024-02542-y (2024).
Zeng, B., Rivadeneira, N. A., Wen, A., Sarkar, U. & Khoong, E. C. The impact of the COVID-19 pandemic on internet use and the use of digital health tools: secondary analysis of the 2020 health information national trends survey. J. Med. Internet Res. 24, e35828 (2022).
Győrffy, Z., Boros, J., Döbrössy, B. & Girasek, E. Older adults in the digital health era: insights on the digital health related knowledge, habits and attitudes of the 65 year and older population. BMC Geriatr. 23, 779 (2023).
Braver, J. et al. Effects of a digitally enabled cardiac rehabilitation intervention on risk factors, recurrent hospitalization and mortality. Eur. Heart J. Digit. Health 6, 688–703 (2025).
Hernandez, M. F. & Rodriguez, F. Health techequity: opportunities for digital health innovations to improve equity and diversity in cardiovascular care. Curr. Cardiovasc. Risk Rep. 17, 1–20 (2023).
Chow, C. K. et al. Effect of lifestyle-focused text messaging on risk factor modification in patients with coronary heart disease: a randomized clinical trial. JAMA 314, 1255–1263 (2015).
Pfaeffli Dale, L. et al. Text message and internet support for coronary heart disease self-management: results from the Text4Heart randomized controlled trial. J. Med. Internet Res. 17, e237 (2015).
Sigamani, A. & Gupta, R. Revisiting secondary prevention in coronary heart disease. Indian Heart J. 74, 431–440 (2022).
Brouwers, R. W. M., Scherrenberg, M., Kemps, H. M. C., Dendale, P. & Snoek, J. A. Cardiac telerehabilitation: current status and future perspectives. Neth. Heart J. 32, 31–37 (2024).
Scherrenberg, M. et al. Development and internal validation of the digital health readiness questionnaire: prospective single-center survey study. J. Med. Internet Res. 25, e41615 (2023).
Ellis, T. et al. Effect of a nurse-avatar guided discharge education smartphone application in people after acute coronary syndrome: a randomized controlled trial. Eur. Heart J. Digit. Health 6, 772–782 (2025).
Gilchrist, H. et al. Use of behavior change techniques in physical activity programs and services for older adults: findings from a rapid review. Ann. Behav. Med. 58, 216–226 (2024).
Yudi, M. B. et al. SMARTphone-based, early cardiac REHABilitation in patients with acute coronary syndromes: a randomized controlled trial. Coron. Artery Dis. 32, 432–440 (2021).
McElroy, I. et al. Use of digital health kits to reduce readmission after cardiac surgery. J. Surg. Res. 204, 1–7 (2016).
Khonsari, S. et al. Effect of a reminder system using an automated short message service on medication adherence following acute coronary syndrome. Eur. J. Cardiovasc. Nurs. 14, 170–179 (2015).
Kuan, P. X. et al. Efficacy of telemedicine for the management of cardiovascular disease: a systematic review and meta-analysis. Lancet Digit. Health 4, e676–e691 (2022).
Gallegos-Rejas, V. M., Rawstorn, J. C., Gallagher, R., Mahoney, R. & Thomas, E. E. Key features in telehealth-delivered cardiac rehabilitation required to optimize cardiovascular health in coronary heart disease: a systematic review and realist synthesis. Eur. Heart J. Digit. Health 5, 208–218 (2024).
Han, Y., Lie, R. K. & Guo, R. The internet hospital as a telehealth model in China: systematic search and content analysis. J. Med. Internet Res. 22, e17995 (2020).
Bhatla, A. et al. Patterns of telehealth visits after the COVID-19 pandemic among individuals with or at risk for cardiovascular disease in the United States. J. Am. Heart Assoc. 13, e036475 (2024).
Lee, J. S., Lowe Beasley, K., Schooley, M. W. & Luo, F. Trends and costs of US telehealth use among patients with cardiovascular disease before and during the COVID-19 pandemic. J. Am. Heart Assoc. 12, e028713 (2023).
Predmore, Z. S., Roth, E., Breslau, J., Fischer, S. H. & Uscher-Pines, L. Assessment of patient preferences for telehealth in post-COVID-19 pandemic health care. JAMA Netw. open 4, e2136405 (2021).
Qian, A. S. et al. Disparities in telemedicine during COVID-19. Cancer Med. 11, 1192–1201 (2022).
Angelovská, O., Dobiášová, K. & Těšinová, J. K. Pandemic COVID-19 as a challenge for telemedicine in the Czech Republic. Int. J. Health Plan. Manag. 40, 271–286 (2025).
Masterson Creber, R. et al. Telehealth and health equity in older adults with heart failure: a scientific statement from the American Heart Association. Circ. Cardiovasc. Qual. Outcomes 16, e000123 (2023).
Krackhardt, F. et al. Results from the “Me & My Heart” (eMocial) study: a randomized evaluation of a new smartphone-based support tool to increase therapy adherence of patients with acute coronary syndrome. Cardiovasc. Drugs Ther. 37, 729–741 (2023).
Zisis, G. et al. An m-Health intervention to improve education, self-management, and outcomes in patients admitted for acute decompensated heart failure: barriers to effective implementation. Eur. Heart J. Digit. Health 2, 649–657 (2021).
Xiang, D. et al. Management and outcomes of patients with STEMI during the COVID-19 pandemic in China. J. Am. Coll. Cardiol. 76, 1318–1324 (2020).
Yang, J. et al. The impact of the stress hyperglycemia ratio on short-term and long-term poor prognosis in patients with acute coronary syndrome: insight from a large cohort study in Asia. Diabetes Care 45, 947–956 (2022).
Corraini, P., Olsen, M., Pedersen, L., Dekkers, O. M. & Vandenbroucke, J. P. Effect modification, interaction and mediation: an overview of theoretical insights for clinical investigators. Clin. Epidemiol. 9, 331–338 (2017).
Acknowledgements
This work was supported by the National High Level Hospital Clinical Research Funding (2024-GSP-GG-4), CAMS Innovation Fund for Medical Sciences (CIFMS) (2024-I2M-C&T-B-040), CAMS Innovation Fund for Medical Sciences (CIFMS) (2024-I2M-ZH-004), Noncommunicable Chronic Diseases-National Science and Technology Major Project (2023ZD0504000), Artificial Intelligence and Information Technology Application Fund of Fuwai Hospital and Chinese Academy of Medical Sciences (2024-AI22).
Author information
Authors and Affiliations
Contributions
All authors read and approved the final version of the manuscript. Z.W. proposed the idea, performed the data analyses, and drafted the manuscript. L.Y., Z.B., M.L., Y.Z., and H.C. checked the integrity and plausibility of data analysis. X.G., S.Z., and Y.W. revised the manuscript and was responsible for the integrity of data acquisition and statistical analyses. X.G. and Y.W. verified the underlying data.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Wang, Z., Yang, L., Zhao, S. et al. Trends and effectiveness of digital health management in postdischarge coronary artery disease across COVID19 pandemic. npj Digit. Med. 8, 721 (2025). https://doi.org/10.1038/s41746-025-02099-8
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41746-025-02099-8