Abstract
South Asians experience disproportionately elevated cardiometabolic disease risk yet remain underrepresented in genomic research. The OurHealth Study builds a digital biobank of US South Asian adults, integrating remote surveys, mailed biospecimens for sequencing, and electronic health record sharing to identify genetic and non-genetic drivers of cardiometabolic disease. By pairing remote participation with culturally tailored outreach, OurHealth enhances accessibility, supports granular phenotyping, and addresses logistical barriers to genomic research inclusion.
Similar content being viewed by others
Data availability
No datasets were generated or analyzed during the current study.
References
Talegawkar, S. A., Jin, Y., Kandula, N. R. & Kanaya, A. M. Cardiovascular health metrics among South Asian adults in the United States: prevalence and associations with subclinical atherosclerosis. Prev. Med. 96, 79–84 (2017).
Joshi, P. et al. Risk factors for early myocardial infarction in South Asians compared with individuals in other countries. JAMA 297, 286–294 (2007).
Rana, A., de Souza, R. J., Kandasamy, S., Lear, S. A. & Anand, S. S. Cardiovascular risk among South Asians living in Canada: a systematic review and meta-analysis. CMAJ Open 2, E183–E191 (2014).
Patel, A. P., Wang, M., Kartoun, U., Ng, K. & Khera, A. V. Quantifying and understanding the higher risk of atherosclerotic cardiovascular disease among South Asians—results from the UK Biobank prospective cohort study. Circulation 144, 410–422 (2021).
Kuppuswamy, V. C. & Gupta, S. Excess coronary heart disease in South Asians in the United Kingdom. BMJ 330, 1223–1224 (2005).
Beckles, G. L. A. et al. High total and cardiovascular disease mortality in adults of Indian descent in Trinidad, unexplained by major coronary risk factors. Lancet 327, 1298–1301 (1986).
Wainwright, J. Cardiovascular disease in the Asiatic (Indian) population of Durban. SA Med. J. 43, 136–138 (1969).
Walker, A. R. P. The epidemiology of ischaemic heart disease in the different ethnic populations in Johannesburg. SA Med. J. 57, 748–752 (1980).
Volgman, A. S. et al. Atherosclerotic cardiovascular disease in South Asians in the United States: epidemiology, risk factors, and treatments: a scientific statement from the American Heart Association. Circulation 138, e1–e34 (2018).
Arnett, D. K. et al. 2019 ACC/AHA guideline on the primary prevention of cardiovascular disease: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation 140, e596–e646 (2019).
Daniel, M., Wilbur, J., Fogg, L. F. & Miller, A. M. Correlates of lifestyle physical activity among South Asian Indian immigrants. J. Community Health Nurs. 30, 185–200 (2013).
Shah, A. D., Vittinghoff, E., Kandula, N. R., Srivastava, S. & Kanaya, A. M. Correlates of pre-diabetes and type 2 diabetes in US South Asians: findings from the mediators of atherosclerosis in South Asians Living in America (MASALA) study. Ann. Epidemiol. 25, 77–83 (2015).
Lauderdale, D. S. & Rathouz, P. J. Body mass index in a US national sample of Asian Americans: effects of nativity, years since immigration and socioeconomic status. Int. J. Obes. 24, 1188–1194 (2000).
Chow, C. K. et al. Association of diet, exercise, and smoking modification with risk of early cardiovascular events after acute coronary syndromes. Circulation 121, 750–758 (2010).
Lear, S. A., Chockalingam, A., Kohli, S., Richardson, C. G. & Humphries, K. H. Elevation in cardiovascular disease risk in South Asians is mediated by differences in visceral adipose tissue. Obesity 20, 1293–1300 (2012).
Martin, A. R. et al. Clinical use of current polygenic risk scores may exacerbate health disparities. Nat. Genet. 51, 584–591 (2019).
Tcheandjieu, C. et al. Large-scale genome-wide association study of coronary artery disease in genetically diverse populations. Nat. Med. 28, 1679–1692 (2022).
Aragam, K. G. et al. Discovery and systematic characterization of risk variants and genes for coronary artery disease in over a million participants. Nat. Genet. 54, 1803–1815 (2022).
Bureau, U. C. American Community Survey Data. Census.gov. https://www.census.gov/programs-surveys/acs/data.html.
Kathiresan, N. et al. Representation of race and ethnicity in the contemporary US Health Cohort All of Us Research Program. JAMA Cardiol. 8, 859–864 (2023).
Saleheen, D. et al. The Pakistan Risk of Myocardial Infarction Study: a resource for the study of genetic, lifestyle and other determinants of myocardial infarction in South Asia. Eur. J. Epidemiol. 24, 329–338 (2009).
Magavern, E. F. et al. CYP2C19 genotype prevalence and association with recurrent myocardial infarction in British–South Asians treated with clopidogrel. JACC Adv. 2, 100573 (2023).
Bilen, O., Kamal, A. & Virani, S. S. Lipoprotein abnormalities in South Asians and its association with cardiovascular disease: current state and future directions. World J. Cardiol. 8, 247–257 (2016).
Paré, G. et al. Lipoprotein(a) levels and the risk of myocardial infarction among 7 ethnic groups. Circulation 139, 1472–1482 (2019).
Patel, D. et al. Role of lipoprotein(a) in atherosclerotic cardiovascular disease in South Asian individuals. J. Am. Heart Assoc. 14, eJAHA/2024/040361–T (2025).
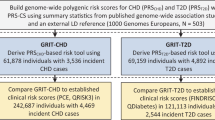
Patel, A. P. et al. A multi-ancestry polygenic risk score improves risk prediction for coronary artery disease. Nat. Med. 29, 1793–1803 (2023).
Rausell, A. et al. Common homozygosity for predicted loss-of-function variants reveals both redundant and advantageous effects of dispensable human genes. Proc. Natl. Acad. Sci. USA 117, 13626–13636 (2020).
Narasimhan, V. M. et al. Health and population effects of rare gene knockouts in adult humans with related parents. Science 352, 474–477 (2016).
Saleheen, D. et al. Human knockouts and phenotypic analysis in a cohort with a high rate of consanguinity. Nature 544, 235–239 (2017).
Wall, J. D. et al. South Asian medical cohorts reveal strong founder effects and high rates of homozygosity. Nat. Commun. 14, 3377 (2023).
Inan, O. T. et al. Digitizing clinical trials. NPJ Digit. Med. 3, 1–7 (2020).
Jean-Louis, G. & Seixas, A. A. The value of decentralized clinical trials: inclusion, accessibility, and innovation. Science 385, eadq4994 (2024).
Natarajan, P. Exceptional genetics, generalizable therapeutics, and coronary artery disease. N. Engl. J. Med. 391, 957–959 (2024).
Flores, L. E. et al. Assessment of the inclusion of racial/ethnic minority, female, and older individuals in vaccine clinical trials. JAMA Netw. Open 4, e2037640 (2021).
Warren, R. C., Forrow, L., Hodge, D. A. & Truog, R. D. Trustworthiness before trust - COVID-19 vaccine trials and the black community. N. Engl. J. Med. 383, e121 (2020).
Kasahara, A. et al. Digital technologies used in clinical trial recruitment and enrollment including application to trial diversity and inclusion: a systematic review. Digit. Health 10, 20552076241242390 (2024).
Smith, J. L. et al. Data sharing in the PRIMED Consortium: design, implementation, and recommendations for future policymaking. Am. J. Hum. Genet. 112, 754–1768 (2025).
The All of Us Research Program Investigators The “All of Us” Research Program. N. Engl. J. Med. 381, 668–676 (2019).
Survey Explorer – All of Us Research Hub. https://www.researchallofus.org/data-tools/survey-explorer/.
Broad Clinical Laboratories, The Broad Institute. Juniper [Hosted Computer Software]. (2023).
Bhakhri, P. et al. Count Me In: patient-partnered research to address disparities for rare cancer patients. Ther. Adv. Rare Dis. 5, 26330040241304440 (2024).
The Heart Hive. HeartHive. https://thehearthive.org/.
DeFelice, M. et al. Blended Genome Exome (BGE) as a cost efficient alternative to deep whole genomes or arrays. Preprint at https://doi.org/10.1101/2024.04.03.587209 (2024).
Martin, A. R. et al. Low-coverage sequencing cost-effectively detects known and novel variation in underrepresented populations. Am. J. Hum. Genet. 108, 656–668 (2021).
Boltz, T. A. et al. A blended genome and exome sequencing method captures genetic variation in an unbiased, high-quality, and cost-effective manner. Preprint at https://doi.org/10.1101/2024.09.06.611689 (2024).
Khera, R. et al. Assessment of health conditions from patient electronic health record portals vs self-reported questionnaires: an analysis of the INSPIRE study. J. Am. Med. Inform. Assoc. 32, 784–794 (2025).
Hugo Health. Hugo Health https://hugo.health.
Hugo Health, Inc. Hugo Connect.
Broad Data Sciences Platform, The Broad Institute. Terra [Hosted Computer Software] (2023).
UW Genetic Analysis Center. Primed Data Models. (2025).
Chaudhary, N., Vyas, A. & Parrish, E. B. Community based organizations addressing South Asian American Health. J. Community Health 35, 384–391 (2010).
Satagopan, J. M. et al. Experiences and lessons learned from community-engaged recruitment for the South Asian breast cancer study in New Jersey during the COVID-19 pandemic. PLoS ONE 18, e0294170 (2023).
Kanaya, A. M. et al. Recruitment and retention of US South Asians for an epidemiologic cohort: Experience from the MASALA study. J. Clin. Transl. Sci. 3, 97–104 (2019).
Islam, N. S. et al. Evaluation of a community health worker pilot intervention to improve diabetes management in Bangladeshi immigrants with type 2 diabetes in New York City. Diab. Educ. 39, 478–493 (2013).
Mukherjea, A., Ivey, S. L., Shariff-Marco, S., Kapoor, N. & Allen, L. Overcoming challenges in recruitment of South Asians for health disparities research in the United States. J. Racial Ethn. Health Disparities 5, 195–208 (2018).
Lambert, S. A. et al. The Polygenic Score Catalog as an open database for reproducibility and systematic evaluation. Nat. Genet. 53, 420–425 (2021).
Auton, A. et al. A global reference for human genetic variation. Nature 526, 68–74 (2015).
Truong, B. et al. Integrative polygenic risk score improves the prediction accuracy of complex traits and diseases. Cell Genomics 4, 100523 (2024).
Misra, A. et al. Instability of high polygenic risk classification and mitigation by integrative scoring. Nat. Commun. 16, 1584 (2025).
Koyama, S. et al. Genetics and context for precision health in Greater Boston. Nat. Commun. 16, 11661 (2025).
Abu-El-Haija, A. et al. The clinical application of polygenic risk scores: a points to consider statement of the American College of Medical Genetics and Genomics (ACMG). Genet. Med. https://www.gimjournal.org/article/S1098-3600(23)00816-X/fulltext (2023).
Wand, H. et al. Clinical genetic counseling and translation considerations for polygenic scores in personalized risk assessments: A Practice Resource from the National Society of Genetic Counselors. J. Genet. Couns. 32, 558–575 (2023).
National Human Genome Research Institute. Polygenic Risk Scores. https://www.genome.gov/Health/Genomics-and-Medicine/Polygenic-risk-scores (2020).
Broad Institute. Polygenic Scores Explained. http://polygenicscores.org/explained/ (2025).
Klein, D. et al. Building a digital health research platform to enable recruitment, enrollment, data collection, and follow-up for a highly diverse longitudinal US cohort of 1 million people in the All of Us Research Program: design and implementation study. J. Med. Internet Res. 27, e60189 (2025).
Naz-McLean, S. et al. Feasibility and lessons learned on remote trial implementation from TestBoston, a fully remote, longitudinal, large-scale COVID-19 surveillance study. PLoS ONE 17, e0269127 (2022).
Tomiwa, T. et al. Leveraging digital tools to enhance diversity and inclusion in clinical trial recruitment. Front. Public Health 12, 1483367 (2024).
Goodson, N. et al. Opportunities and counterintuitive challenges for decentralized clinical trials to broaden participant inclusion. NPJ Digit. Med. 5, 58 (2022).
Rebbeck, T. R. et al. A framework for promoting diversity, equity, and inclusion in genetics and genomics research. JAMA Health Forum 3, e220603 (2022).
Guo, X., Vittinghoff, E., Olgin, J. E., Marcus, G. M. & Pletcher, M. J. Volunteer participation in the Health eHeart study: a comparison with the US population. Sci. Rep. 7, 1956 (2017).
Acknowledgements
We gratefully acknowledge the participants of the OurHealth study, without whom this research would not be possible. Research reported in this publication was supported by the National Institutes of Health for the project “Polygenic Risk Methods in Diverse Populations (PRIMED) Consortium”, with grant funding for Study Site FFAIR-PRS (U01HG011719) to P.N., and the Coordinating Center (U01HG011697) to P.N., M.P.C., and K.R. R.B. is supported by the Harvard Catalyst K12/CMeRIT Award (1K12TR004381-01). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Author information
Authors and Affiliations
Contributions
P.N. conceived and supervised the study. S.G., R.B., W.E.H., and R.M. drafted the manuscript. S.G. and R.M. contributed graphical illustrations. A.B., C.R., S.H., B.O., H.B., P.S., S.P., N.U., N.S., K.R., M.P.C., R.D., A.K., A.P.P., K.P., Y.L., S.S.P., R.K., M.G., A.V.K., and L.P. reviewed the manuscript and provided comments. All authors read and approved the final version of the manuscript.
Corresponding authors
Ethics declarations
Competing interests
P.N. reports research grants from Allelica, Amgen, Apple, Boston Scientific, Cleerly, Genentech / Roche, Ionis, Novartis, and Silence Therapeutics, personal fees from Allelica, Apple, AstraZeneca, Bain Capital, Blackstone Life Sciences, Bristol Myers Squibb, Creative Education Concepts, CRISPR Therapeutics, Eli Lilly & Co, Esperion Therapeutics, Foresite Capital, Foresite Labs, Genentech / Roche, GV, HeartFlow, Magnet Biomedicine, Merck, Novartis, Novo Nordisk, TenSixteen Bio, and Tourmaline Bio, equity in Bolt, Candela, Mercury, MyOme, Parameter Health, Preciseli, and TenSixteen Bio, royalties from Recora for intensive cardiac rehabilitation, and spousal employment at Vertex Pharmaceuticals, all unrelated to the present work. A.V.K. is an employee and holds equity in Verve Therapeutics and has received consulting fees from Arboretum Therapeutics. R.B. received consulting fees from Casana Care, Inc, and Novartis unrelated to the present work. M.G. received consulting fees from Medtronic, Bayer and New Amsterdam, and serves on a DSMB for Merck; all unrelated to this present work. N.U. has worked at the American Cancer Society unrelated to the submitted work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Ganesh, S., Bhattacharya, R., Bhatnagar, A. et al. The OurHealth Study: A digital genomic cohort for cardiometabolic risk mechanisms in US South Asians. npj Digit. Med. (2026). https://doi.org/10.1038/s41746-025-02335-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41746-025-02335-1