Abstract
Background
Ovarian cancer is a major female reproductive health issue with heterogeneous biological features on its subtypes, which may require different therapeutic strategies. Glucagon-like peptide-1 receptor (GLP-1R) agonists were reported to be beneficial for ovarian cancer, but the causal effects and mechanisms on its heterogeneous subtypes remain unclear.
Methods
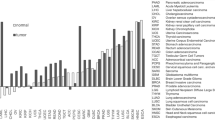
We used genetic variants robustly associated with gene expression, protein level, splicing event, and DNA methylation of GLP-1R in six endocrine-related tissues (N ≤ 35,431) as genetic instruments to proxy the effect of GLP-1R agonism. To increase power, we conducted a meta-analysis of genome-wide association studies of ovarian cancer (29,066 cases, 461,542 controls), and identified 12 genome-wide associated variants, including two previously unreported variants: rs77247401 (MIR1208) and rs56159231 (PLEKHM1).
Results
Here we show that gene expression of GLP-1R in pancreas is associated with a reduced risk of overall ovarian cancer risk odds ratio ([OR] = 0.94, 95% confidence interval [CI] 0.89-1.00) and endometrioid ovarian cancer (ENOC; OR = 0.83, 95% CI = 0.72-0.95), which the finding is validated using splicing event of GLP-1R in pancreas (OR = 0.13, 95% CI = 0.02-0.86). However, null association is found for GLP-1R expression in pancreas with other ovarian cancer subtypes. The phenome-wide MR followed by mediation MR identifies six body composition and metabolic factors as mediators, including 18:2 linoleic acid.
Conclusions
The protective effect of GLP-1R agonists on ovarian cancer, especially ENOC, needs further validation in large-scale and well-conducted clinical trials.
Plain language summary
The class of drugs known as GLP-1 receptor (GLP-1R) agonists are known to have a range of health benefits. However, their effect on ovarian cancer, which is a significant health concern for women worldwide, has been unclear. GLP-1R agonists act on a protein expressed in the outside of cells, called the GLP-1 receptor. In our study, we used human genetic data to predict activity of the GLP-1 receptor in over 490,000 individuals. We found that GLP-1R activity in the pancreas was associated with a lower risk of a specific subtype of ovarian cancer called endometrioid ovarian cancer. This protective effect appeared to be partly influenced by changes in body composition and molecules in the blood, such as linoleic acid. Our results suggest that GLP-1R agonists could help prevent certain forms of ovarian cancer. Further clinical studies are needed to confirm this possibility.
Similar content being viewed by others
Data availability
The data of molecular traits used to proxy GLP-1R expression were available via deCODE genetics website (https://www.decode.com/summarydata/), the eQTL Gen website (https://www.eqtlgen.org), the GoDMC website (http://mqtldb.godmc.org.uk), the MetaBrain website (https://metabrain.nl/) and the Genotype-Tissue Expression (GTEx) Portal website (https://www.gtexportal.org). The summary statistics of ovarian cancer for GWAS meta-analyses used in this study are deposited in the IEU OpenGWAS database (GWAS IDs ieu-a-1120 and ieu-b-4963) and FinnGen r12 defined as II Neoplasms, from cancer register (ICD-O-3) (https://r12.finngen.fi/pheno/C3_OVARY_EXALLC). The GWAS summary statistics for the ovarian cancer subtypes are available at https://gwas.mrcieu.ac.uk with their GWAS IDs listed in the Supplementary Data. The GWAS summary statistics for positive control outcomes are downloaded from the GWAS Catalog (https://www.ebi.ac.uk/gwas/) and the accession codes are as follows: body mass index (GCST90029007) and type 2 diabetes (GCST90018926). The GWAS summary statistics for mediators were derived from EpiGraphDB database (https://www.epigraphdb.org/). No additional permissions or applications are required to access these datasets. The drug information utilized in this study was obtained from the Citeline database (https://clinicalintelligence.citeline.com/). Full access to the Citeline platform is commercially licensed and not freely available to all researchers. The source data for Figs. 1, 2 and 3 are available in Supplementary Data.
Code availability
The MR pipeline assessing the effect of GLP-1R expression on ovarian cancer is publicly available on the Omics Harbor GitHub repository (https://github.com/geneinmylife/GLP1R-OC-project) and has been permanently archived on Zenodo (https://doi.org/10.5281/zenodo.17994065).
References
Ajayi, A. F., Oyovwi, M. O., Akano, O. P., Akanbi, G. B. & Adisa, F. B. Molecular pathways in reproductive cancers: a focus on prostate and ovarian cancer. Cancer Cell Int. 25, 33 (2025).
Webb, P. M. & Jordan, S. J. Global epidemiology of epithelial ovarian cancer. Nat. Rev. Clin. Oncol. 21, 389–400 (2024).
Cho, K. R. & Shih, I.-M. Ovarian cancer. Annu. Rev. Pathol. 4, 287–313 (2009).
Phelan, C. M. et al. Identification of 12 new susceptibility loci for different histotypes of epithelial ovarian cancer. Nat. Genet. 49, 680–691 (2017).
Wentzensen, N. et al. Ovarian cancer risk factors by histologic subtype: an analysis from the ovarian cancer cohort consortium. J. Clin. Oncol. 34, 2888–2898 (2016).
Lincoff, A. M. et al. Semaglutide and cardiovascular outcomes in obesity without diabetes. N. Engl. J. Med. 389, 2221–2232 (2023).
Wharton, S. et al. Daily Oral GLP-1 receptor agonist orforglipron for adults with obesity. N. Engl. J. Med. 389, 877–888 (2023).
Srivastava, G. & Kumar, R. B. Once-weekly semaglutide in adults with overweight or obesity. N. Engl. J. Med. 385, e4 (2021).
American Diabetes Association Primary Care Advisory Group Standards of Care in Diabetes—2025 Abridged for Primary Care. Clin. Diab. 43, 182 (2025).
Ibrahim, S. S. et al. The effect of GLP-1R agonists on the medical triad of obesity, diabetes, and cancer. Cancer Metastasis Rev. 43, 1297–1314 (2024).
Pasternak, B. et al. Glucagon-like peptide 1 receptor agonist use and risk of thyroid cancer: scandinavian cohort study. BMJ 385, e078225 (2024).
Zheng, Z. et al. Glucagon-like peptide-1 receptor: mechanisms and advances in therapy. Signal Transduct. Target Ther. 9, 234 (2024).
Wang, L., Xu, R., Kaelber, D. C. & Berger, N. A. Glucagon-like peptide 1 receptor agonists and 13 obesity-associated cancers in patients with type 2 diabetes. JAMA Netw. Open 7, e2421305 (2024).
Montastruc, J.-L. GLP 1 receptor agonists and obesity-associated cancers: a disproportionality analysis in Vigibase®. Eur. J. Clin. Pharm. 80, 1999–2001 (2024).
Pratley, R. et al. Oral semaglutide versus subcutaneous liraglutide and placebo in type 2 diabetes (PIONEER 4): a randomised, double-blind, phase 3a trial. Lancet 394, 39–50 (2019).
Marso, S. P. et al. Liraglutide and cardiovascular outcomes in type 2 diabetes. N. Engl. J. Med. 375, 311–322 (2016).
O’Neil, P. M. et al. Efficacy and safety of semaglutide compared with liraglutide and placebo for weight loss in patients with obesity: a randomised, double-blind, placebo and active controlled, dose-ranging, phase 2 trial. Lancet 392, 637–649 (2018).
Smith, G. D. & Ebrahim, S. Mendelian randomization’: can genetic epidemiology contribute to understanding environmental determinants of disease? Int. J. Epidemiol. 32, 1–22 (2003).
Zheng, J. et al. Recent developments in mendelian randomization studies. Curr. Epidemiol. Rep. 4, 330–345 (2017).
Sun, Y. et al. Association of glucagon-like peptide-1 receptor agonists with risk of cancers-evidence from a drug target Mendelian randomization and clinical trials. Int. J. Surg. 110, 4688–4694 (2024).
Yarmolinsky, J. et al. Genetically proxied glucose-lowering drug target perturbation and risk of cancer: a Mendelian randomisation analysis. Diabetologia 66, 1481–1500 (2023).
Riedinger, C. J. et al. Glucagon-like peptide-1 (GLP-1) receptor agonists for weight management: a review for the gynecologic oncologist. Gynecol. Oncol. 190, 1–10 (2024).
Carter, A. R. et al. Mendelian randomisation for mediation analysis: current methods and challenges for implementation. Eur. J. Epidemiol. 36, 465–478 (2021).
Garrido-Martín, D., Borsari, B., Calvo, M., Reverter, F. & Guigó, R. Identification and analysis of splicing quantitative trait loci across multiple tissues in the human genome. Nat. Commun. 12, 727 (2021).
GTEx Consortium The GTEx Consortium atlas of genetic regulatory effects across human tissues. Science 369, 1318–1330 (2020).
Võsa, U. et al. Large-scale cis- and trans-eQTL analyses identify thousands of genetic loci and polygenic scores that regulate blood gene expression. Nat. Genet. 53, 1300–1310 (2021).
de Klein, N. et al. Brain expression quantitative trait locus and network analyses reveal downstream effects and putative drivers for brain-related diseases. Nat. Genet. 55, 377–388 (2023).
Min, J. L. et al. Genomic and phenotypic insights from an atlas of genetic effects on DNA methylation. Nat. Genet. 53, 1311–1321 (2021).
Robins, C. et al. Genetic control of the human brain proteome. Am. J. Hum. Genet. 108, 400–410 (2021).
Wingo, T. S. et al. Brain proteome-wide association study implicates novel proteins in depression pathogenesis. Nat. Neurosci. 24, 810–817 (2021).
Sun, B. B. et al. Genomic atlas of the human plasma proteome. Nature 558, 73–79 (2018).
Hansson, O. et al. The genetic regulation of protein expression in cerebrospinal fluid. EMBO Mol. Med. 15, e16359 (2022).
Sun, B. B. et al. Plasma proteomic associations with genetics and health in the UK Biobank. Nature 622, 329–338 (2023).
Pietzner, M. et al. Mapping the proteo-genomic convergence of human diseases. Science 374, eabj1541 (2021).
Ferkingstad, E. et al. Large-scale integration of the plasma proteome with genetics and disease. Nat. Genet. 53, 1712–1721 (2021).
Zhang, J. et al. Plasma proteome analyses in individuals of European and African ancestry identify cis-pQTLs and models for proteome-wide association studies. Nat. Genet. 54, 593–602 (2022).
Yang, C. et al. Genomic atlas of the proteome from brain, CSF and plasma prioritizes proteins implicated in neurological disorders. Nat. Neurosci. 24, 1302–1312 (2021).
Western, D. et al. Proteogenomic analysis of human cerebrospinal fluid identifies neurologically relevant regulation and implicates causal proteins for Alzheimer’s disease. Nat. Genet. 56, 2672–2684 (2024).
Mitchell, R. et al. UK Biobank Genetic Data: MRC-IEU Quality Control, version 2. University of Bristol https://doi.org/10.5523/BRIS.1OVAAU5SXUNP2CV8RCY88688V (2019).
Kurki, M. I. et al. FinnGen provides genetic insights from a well-phenotyped isolated population. Nature 613, 508–518 (2023).
Elsworth, B. & Gaunt, T. R. MELODI Presto: a fast and agile tool to explore semantic triples derived from biomedical literature. Bioinformatics 37, 583–585 (2021).
Skrivankova, V. W. et al. Strengthening the reporting of observational studies in epidemiology using mendelian randomisation (STROBE-MR): explanation and elaboration. BMJ 375, n2233 (2021).
Skrivankova, V. W. et al. Strengthening the reporting of observational studies in epidemiology using mendelian randomization: the STROBE-MR statement. JAMA 326, 1614–1621 (2021).
Willer, C. J., Li, Y. & Abecasis, G. R. METAL: fast and efficient meta-analysis of genomewide association scans. Bioinformatics 26, 2190–2191 (2010).
Winkler, T. W. et al. Quality control and conduct of genome-wide association meta-analyses. Nat. Protoc. 9, 1192–1212 (2014).
Bulik-Sullivan, B. K. et al. LD Score regression distinguishes confounding from polygenicity in genome-wide association studies. Nat. Genet. 47, 291–295 (2015).
Yang, J. et al. Conditional and joint multiple-SNP analysis of GWAS summary statistics identifies additional variants influencing complex traits. Nat. Genet. 44, 369–375 (2012).
Dong, S. et al. Annotating and prioritizing human non-coding variants with RegulomeDB v.2. Nat. Genet. 55, 724–726 (2023).
Ward, L. D. & Kellis, M. HaploReg v4: systematic mining of putative causal variants, cell types, regulators and target genes for human complex traits and disease. Nucleic Acids Res. 44, D877–D881 (2016).
Ward, L. D. & Kellis, M. HaploReg: a resource for exploring chromatin states, conservation, and regulatory motif alterations within sets of genetically linked variants. Nucleic Acids Res. 40, D930–D934 (2012).
Watanabe, K., Taskesen, E., van Bochoven, A. & Posthuma, D. Functional mapping and annotation of genetic associations with FUMA. Nat. Commun. 8, 1826 (2017).
Rentzsch, P., Witten, D., Cooper, G. M., Shendure, J. & Kircher, M. CADD: predicting the deleteriousness of variants throughout the human genome. Nucleic Acids Res. 47, D886–D894 (2019).
Zheng, J. et al. Phenome-wide Mendelian randomization mapping the influence of the plasma proteome on complex diseases. Nat. Genet. 52, 1122–1131 (2020).
Oliva, M. et al. The impact of sex on gene expression across human tissues. Science 369, eaba3066 (2020).
Loh, P.-R., Kichaev, G., Gazal, S., Schoech, A. P. & Price, A. L. Mixed-model association for biobank-scale datasets. Nat. Genet. 50, 906–908 (2018).
Sakaue, S. et al. A cross-population atlas of genetic associations for 220 human phenotypes. Nat. Genet. 53, 1415–1424 (2021).
Hemani, G. et al. The MR-Base platform supports systematic causal inference across the human phenome. Elife 7, e34408 (2018).
Liu, Y. et al. EpiGraphDB: a database and data mining platform for health data science. Bioinformatics 37, 1304–1311 (2021).
Davies, N. M., Holmes, M. V. & Davey Smith, G. Reading Mendelian randomisation studies: a guide, glossary, and checklist for clinicians. BMJ 362, k601 (2018).
Giambartolomei, C. et al. Bayesian test for colocalisation between pairs of genetic association studies using summary statistics. PLoS Genet 10, e1004383 (2014).
An efficient and robust tool for colocalisation: Pair-wise Conditional and Colocalisation (PWCoCo) | bioRxiv. https://doi.org/10.1101/2022.08.08.503158v1.
Davey Smith, G. & Hemani, G. Mendelian randomization: genetic anchors for causal inference in epidemiological studies. Hum. Mol. Genet. 23, R89–R98 (2014).
Woolf, B. et al. MRSamePopTest: introducing a simple falsification test for the two-sample mendelian randomisation ‘same population’ assumption. BMC Res Notes 17, 27 (2024).
Patel, A. et al. Robust use of phenotypic heterogeneity at drug target genes for mechanistic insights: Application of cis-multivariable Mendelian randomization to GLP1R gene region. Genet. Epidemiol. 48, 151–163 (2024).
Zuber, V., Colijn, J. M., Klaver, C. & Burgess, S. Selecting likely causal risk factors from high-throughput experiments using multivariable Mendelian randomization. Nat. Commun. 11, 29 (2020).
Zheng, J. & Liu, J. Mendelian randomization study of GLP-1R effects on ovarian cancer subtypes mediated by metabolic factors. Zenodo https://doi.org/10.5281/zenodo.17994065 (2025).
Chen, Y. et al. Plasma metabolites and risk of seven cancers: a two-sample Mendelian randomization study among European descendants. BMC Med. 22, 90 (2024).
Feng, Y. et al. Causal effects of genetically determined metabolites on cancers included lung, breast, ovarian cancer, and glioma: a Mendelian randomization study. Transl. Lung Cancer Res. 11, 1302–1314 (2022).
Freuer, D. et al. Body fat distribution and risk of breast, endometrial, and ovarian cancer: a two-sample mendelian randomization study. Cancers 13, 5053 (2021).
Nieto, M. A. Epithelial plasticity: a common theme in embryonic and cancer cells. Science 342, 1234850 (2013).
Xing, Q.-Q. et al. Global burden of common cancers attributable to metabolic risks from 1990 to 2019. Medicine 4, 168–181 (2023).
Wang, H. et al. DLAT is involved in ovarian cancer progression by modulating lipid metabolism through the JAK2/STAT5A/SREBP1 signaling pathway. Cancer Cell Int. 25, 25 (2025).
Kuroki, L. & Guntupalli, S. R. Treatment of epithelial ovarian cancer. BMJ 371, m3773 (2020).
Chen, S. et al. A review of the clinical characteristics and novel molecular subtypes of endometrioid ovarian cancer. Front. Oncol. 11, 668151 (2021).
Guidozzi, F. Endometriosis-associated cancer. Climacteric 24, 587–592 (2021).
Wang, L. et al. Endometriosis and epithelial ovarian cancer: a two-sample Mendelian randomization analysis. Sci. Rep. 13, 21992 (2023).
Krasnyi, A. M. et al. The levels of ghrelin, glucagon, visfatin and Glp-1 are decreased in the peritoneal fluid of women with endometriosis along with the increased expression of the CD10 protease by the macrophages. Int. J. Mol. Sci. 23, 10361 (2022).
Zheng, Z. et al. Glucagon-like peptide-1 receptor: mechanisms and advances in therapy. Sig Transduct. Target Ther. 9, 1–29 (2024).
Sanders, T. A. B. Omega-6 fatty acids and cardiovascular disease. Circulation 139, 2437–2439 (2019).
Zhu, T., Lu, X.-T., Liu, Z.-Y. & Zhu, H.-L. Dietary linoleic acid and the ratio of unsaturated to saturated fatty acids are inversely associated with significant liver fibrosis risk: a nationwide survey. Front. Nutr. 9, 938645 (2022).
Jeyapal, S. et al. Substitution of linoleic acid with α-linolenic acid or long chain n-3 polyunsaturated fatty acid prevents Western diet induced nonalcoholic steatohepatitis. Sci. Rep. 8, 10953 (2018).
Juárez-Hernández, E., Chávez-Tapia, N. C., Uribe, M. & Barbero-Becerra, V. J. Role of bioactive fatty acids in nonalcoholic fatty liver disease. Nutr. J. 15, 72 (2016).
Koundouros, N. et al. Direct sensing of dietary ω-6 linoleic acid through FABP5-mTORC1 signaling. Science 387, eadm9805 (2025).
Acknowledgements
This work was supported by grants from the Noncommunicable Chronic Diseases–National Science and Technology Major Project (2024ZD0531500, 2024ZD0531502) and the National Key Research and Development Program of China (2022YFC2505203). J.L.L., M.X., W.Q.W., Y.F.B. and G.N. are supported by the National Natural Science Foundation of China (82088102, 81970728 and 81941017) and the Shanghai Municipal Education Commission–Gaofeng Clinical Medicine Grant Support (20161307 and 20152508 Round 2). J.L.L., M.X., W.Q.W., Y.F.B. and G.N. are members of the Innovative Research Team of High-level Local Universities in Shanghai.
Author information
Authors and Affiliations
Contributions
Conceptualization: J.Z.; Formal analysis: J.J.L. and Z.H.C.; Methodology: J.Z.; Investigation: J.J.L., Z.H.C., Q.Y., H.L., S.Y.W., M.L., T.G.W., Z.Y.Z., M.X., Y.H.C., Y.X., J.L.L., and Q.H.G.; Visualization: J.J.L. and Z.H.C.; Funding acquisition: L.M.W., M.X., J.Z., J.L.L., W.Q.W., Y.F.B., and G.N.; Project administration: G.N. and W.Q.W.; Supervision: L.M.W., W.Q.W., Y.F.B., and J.Z.; Writing—original draft: J.J.L.; Writing—review and editing: Q.Y. and J.Z.; L.M.W., W.Q.W., Y.F.B., and J.Z. are the guarantors of this work and shall take responsibility for the full access and integrity of the data. All authors have approved the final version of the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests. The funding sources had no role in the design of the study, collection and analysis of data, interpretation of results, and decision to publish.
Peer review
Peer review information
Communications Medicine thanks Yiwen Liang, Benjamin Woolf and the other, anonymous, reviewer(s) for their contribution to the peer review of this work. A peer review file is available.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Liu, J., Chen, Z., Yang, Q. et al. Mendelian randomization study of GLP-1R effects on ovarian cancer subtypes mediated by metabolic factors. Commun Med (2026). https://doi.org/10.1038/s43856-026-01379-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s43856-026-01379-y