Abstract
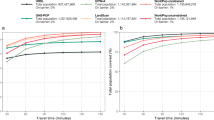
There is consensus that urban residents have better access to healthcare than rural residents in the USA, yet this knowledge is based mostly on primary care services. Here we put forward a multidimensional examination of healthcare access to 75 medical specialties in 898 US cities. Leveraging urban scaling theory, economic geography and network science, we confirm the expectation that residents in large cities have access to a more diverse range of specialists. Concurrently, we register a surprising sublinear scaling of the prevalence of most specialty providers: the larger the city, the less the provision of specialized healthcare per capita and per unit area. We propose that the trade-off between diversity and provision is related to economic clustering in the healthcare sector and high patient loading of providers in large cities. These findings suggest the need for city-specific strategies to address emerging inequalities in healthcare services.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
Data availability
Datasets that are allowed to be shared are available via GitHub at https://github.com/dynamicalsystemslaboratory/Healthcare-Disparities-in-the-United-States/.
Code availability
Scripts that are allowed to be shared are available via GitHub at https://github.com/dynamicalsystemslaboratory/Healthcare-Disparities-in-the-United-States/.
References
Fullman, N. et al. Measuring performance on the Healthcare Access and Quality Index for 195 countries and territories and selected subnational locations: a systematic analysis from the Global Burden of Disease Study 2016. Lancet 391, 2236–2271 (2018).
Cu, A., Meister, S., Lefebvre, B. & Ridde, V. Assessing healthcare access using the Levesque’s conceptual framework—a scoping review. Int. J. Equity Health 20, 116 (2021).
Fiscella, K. & Williams, D. R. Health disparities based on socioeconomic inequities: implications for urban health care. Acad. Med. 79, 1139–1147 (2004).
Mackenbach, J. P. et al. Trends in health inequalities in 27 European countries. Proc. Natl Acad. Sci. USA 115, 6440–6445 (2018).
Dickman, S. L., Himmelstein, D. U. & Woolhandler, S. Inequality and the health-care system in the USA. Lancet 389, 1431–1441 (2017).
Nelson, A. Unequal treatment: confronting racial and ethnic disparities in health care. J. Natl Med. Assoc. 94, 666 (2002).
Douthit, N., Kiv, S., Dwolatzky, T. & Biswas, S. Exposing some important barriers to health care access in the rural USA. Public Health 129, 611–620 (2015).
Mahajan, S. et al. Trends in differences in health status and health care access and affordability by race and ethnicity in the United States, 1999–2018. JAMA 326, 637–648 (2021).
Zhao, P., Li, J. & Zhang, M. Unequal roles of cities in the intercity healthcare system. Nat. Cities 2, 198–209 (2025).
Meit, M. et al. The 2014 Update of the Rural–Urban Chartbook (Rural Health Reform Policy Research Center, 2014).
Zhang, D. et al. Assessment of changes in rural and urban primary care workforce in the United States from 2009 to 2017. JAMA Netw. Open 3, e2022914 (2020).
Chen, X. et al. Differences in rural and urban health information access and use. J. Rural Health 35, 405–417 (2019).
Rydin, Y. et al. Shaping cities for health: complexity and the planning of urban environments in the 21st century. Lancet 379, 2079–2108 (2012).
Bettencourt, L. M. Introduction to Urban Science Evidence and Theory of Cities as Complex Systems (MIT Press, 2021).
Gayon, J. History of the concept of allometry. Am. Zool. 40, 748–758 (2000).
Bettencourt, L. M., Lobo, J., Helbing, D., Kühnert, C. & West, G. B. Growth, innovation, scaling, and the pace of life in cities. Proc. Natl Acad. Sci. USA 104, 7301–7306 (2007).
Lu, M., Zhou, C., Wang, C., Jackson, R. B. & Kempes, C. P. Worldwide scaling of waste generation in urban systems. Nat. Cities 1, 126–135 (2024).
Boeing, G. Street network models and indicators for every urban area in the world. Geogr. Anal. 54, 519–535 (2022).
Succar, R. & Porfiri, M. Urban scaling of firearm violence, ownership and accessibility in the United States. Nat. Cities 1, 216–224 (2024).
McCulley, E. M. et al. Urban scaling of health outcomes: a scoping review. J. Urban Health 99, 409–426 (2022).
Bilal, U. et al. Scaling of mortality in 742 metropolitan areas of the Americas. Sci. Adv. 7, eabl6325 (2021).
Meirelles, J., Neto, C. R., Ferreira, F. F., Ribeiro, F. L. & Binder, C. R. Evolution of urban scaling: evidence from Brazil. PLoS ONE 13, e0204574 (2018).
Gan, T., Succar, R., Macri, S. & Porfiri, M. Investigating the link between impulsivity and obesity through urban scaling laws. PLoS Complex Syst. 2, e0000046 (2025).
Ortman, J. M., Velkoff, V. A. & Howard, H. An aging nation: the older population in the United States. US Census Bureau https://www.census.gov/content/dam/Census/library/publications/2014/demo/p25-1140.pdf (2014).
Jin, K., Simpkins, J. W., Ji, X., Leis, M. & Stambler, I. The critical need to promote research of aging and aging-related diseases to improve health and longevity of the elderly population. Aging Dis. 6, 1–5 (2014).
Densen, P. Challenges and opportunities facing medical education. Trans. Am. Clin. Climatol. Assoc. 122, 48–58 (2011).
Durneva, P., Cousins, K. & Chen, M. The current state of research, challenges, and future research directions of blockchain technology in patient care: systematic review. J. Med. Internet Res. 22, e18619 (2020).
Guagliardo, M. F. Spatial accessibility of primary care: concepts, methods and challenges. Int. J. Health Geogr. 3, 3 (2004).
Roth, G. A. et al. Global and regional patterns in cardiovascular mortality from 1990 to 2013. Circulation 132, 1667–1678 (2015).
Barnett, K. et al. Epidemiology of multimorbidity and implications for health care, research, and medical education: a cross-sectional study. Lancet 380, 37–43 (2012).
Shaw, J. & Glover, W. The political economy of digital health equity: structural analysis. J. Med. Internet Res. 26, e46971 (2024).
Cyr, M. E., Etchin, A. G., Guthrie, B. J. & Benneyan, J. C. Access to specialty healthcare in urban versus rural US populations: a systematic literature review. BMC Health Serv. Res. 19, 974 (2019).
Breschi, S. & Malerba, F. The geography of innovation and economic clustering: some introductory notes. Ind. Corp. Change 10, 817–833 (2001).
Specialty & subspecialty certificates. American Board of Medical Specialties https://www.abms.org/member-boards/specialty-subspecialty-certificates/ (2025).
Rocha, L. E., Thorson, A. E. & Lambiotte, R. The non-linear health consequences of living in larger cities. J. Urban Health 92, 785–799 (2015).
Petterson, S. M. et al. Projecting US primary care physician workforce needs: 2010–2025. Ann. Fam. Med. 10, 503–509 (2012).
Naylor, M. D. & Kurtzman, E. T. The role of nurse practitioners in reinventing primary care. Health Aff. 29, 893–899 (2010).
Youn, H. et al. Scaling and universality in urban economic diversification. J. R. Soc. Interface 13, 20150937 (2016).
Wait times surge: physician appointment delays reach record highs. Advisory.com https://www.advisory.com/daily-briefing/2025/06/02/wait-times-ec (2025).
Porter, M. E. Location, competition, and economic development: Local clusters in a global economy. Econ. Dev. Q. 14, 15–34 (2000).
Lee, A. A., James, A. S. & Hunleth, J. M. Waiting for care: chronic illness and health system uncertainties in the United States. Soc. Sci. Med. 264, 113296 (2020).
Hanna, T. P. et al. Mortality due to cancer treatment delay: systematic review and meta-analysis. BMJ 371, m4087 (2020).
Epstein, A. J., Gray, B. H. & Schlesinger, M. Racial and ethnic differences in the use of high-volume hospitals and surgeons. Arch. Surg. 145, 179–186 (2010).
Peen, J., Schoevers, R. A., Beekman, A. T. & Dekker, J. The current status of urban–rural differences in psychiatric disorders. Acta Psychiatr. Scand. 121, 84–93 (2010).
Sutradhar, U., Spearing, L., Zou, B., Chester, M. & Derrible, S. Evolution of infrastructure burden for US cities by 2100. Preprint at Research Square https://doi.org/10.21203/rs.3.rs-5505742/v1 (2025).
Xiao, Y. & Gong, P. Removing spatial autocorrelation in urban scaling analysis. Cities 124, 103600 (2022).
Qin, A. et al. Does unequal economic development contribute to the inequitable distribution of healthcare resources? evidence from China spanning 2001–2020. Global Health 20, 20 (2024).
Ono, T., Schoenstein, M. & Buchan, J. Geographic Imbalances in Doctor Supply and Policy Responses (OECD, 2014); https://doi.org/10.1787/5jz5sq5ls1wl-en
Provider Data: National Downloadable File (Centers for Medicare and Medicaid Services, 2025); https://data.cms.gov/provider-data/dataset/mj5m-pzi6
Google Maps Geocoding API (Google Developers Console, 2023); https://developers.google.com/maps/documentation/geocoding/start
HUD USPS ZIP Code Crosswalk Files (National Bureau of Economic Research, 2023); https://www.huduser.gov/portal/datasets/usps_crosswalk.html
Office of Management and Budget. 2020 standards for delineating core-based statistical areas. Federal Register https://www.federalregister.gov/documents/2021/07/16/2021-15159/2020-standards-for-delineating-core-based-statistical-areas (2021).
Dieleman, J. L. et al. Drivers of variation in health care spending across US counties. JAMA Health Forum 6, e245220 (2025).
Bettencourt, L. M., Lobo, J., Strumsky, D. & West, G. B. Urban scaling and its deviations: revealing the structure of wealth, innovation and crime across cities. PLoS ONE 5, e13541 (2010).
Gomez-Lievano, A., Patterson-Lomba, O. & Hausmann, R. Explaining the prevalence, scaling and variance of urban phenomena. Nat. Hum. Behav. 1, 0012 (2016).
Yin, C., He, Q., Liu, Y., Chen, W. & Gao, Y. Inequality of public health and its role in spatial accessibility to medical facilities in China. Appl. Geogr. 92, 50–62 (2018).
Ricke, K., Drouet, L., Caldeira, K. & Tavoni, M. Country-level social cost of carbon. Nat. Clim. Change 8, 895–900 (2018).
Gastwirth, J. L. The estimation of the Lorenz curve and Gini index. Rev. Econ. Stat. 54, 306–316 (1972).
Metadata glossary. World Bank Group https://databank.worldbank.org/metadataglossary/gender-statistics/series/SI.POV.GINI#:~:text=Gini%20index,of%20100%20implies%20perfect%20inequality (2024).
Virtanen, P. et al. SciPy 1.0: fundamental algorithms for scientific computing in Python. Nat. Methods 17, 261–272 (2020).
Liu, W.-C., Huang, L.-C., Liu, C. W.-J. & Jordán, F. A simple approach for quantifying node centrality in signed and directed social networks. Appl. Netw. Sci. 5, 46 (2020).
Seabold, S. & Perktold, J. statsmodels: econometric and statistical modeling with Python. R version 0.14.0 (2010).
MacKinnon, J. G. & White, H. Some heteroskedasticity-consistent covariance matrix estimators with improved finite sample properties. J. Econometrics 29, 305–325 (1985).
Hosmer, D. W. Jr, Lemeshow, S. & Sturdivant, R. X. Applied Logistic Regression (John Wiley & Sons, 2013).
Pedregosa, F. et al. Scikit-learn: machine learning in Python. J. Mach. Learn. Res. 12, 2825–2830 (2011).
TIGER/Line Shapefiles and TIGER/Line Files Technical Documentation. US Census Bureau https://www.census.gov/geographies/mapping-files/time-series/geo/tiger-line-file.2020.html (2020).
Acknowledgements
We acknowledge support from National Science Foundation grant numbers ECCS-1928614 and DUE-2129076 (both granted to M.P.). We thank A. Boldini, R. Barak Ventura, P. De Lellis, S. Macrì, O. Nov, R. Succar and T. Yabe for constructive input.
Author information
Authors and Affiliations
Contributions
T.G. and M.P. designed research; T.G. and M.P. performed research; T.G. and T.D. analyzed data; T.G. led software; M.P. acquired funding; T.D. led data curation; M.P. provided resources and supervision; T.G. handled visualization; and T.G. and M.P. wrote the paper.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Cities thanks the anonymous reviewers for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary Information
Supplementary Figs. 1–9, Discussions 1–8 and Tables 1–5.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Gan, T., Dighe, T. & Porfiri, M. Trade-off between diversity and provision of specialized healthcare in US cities. Nat Cities 2, 980–989 (2025). https://doi.org/10.1038/s44284-025-00326-7
Received:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s44284-025-00326-7