Abstract
Nuclear factor-κB (NF-κB) plays a central role in myocardial ischemia-reperfusion (MI/R) injury. The inhibitory protein IκBα prevents its activation. We investigated the effects of adeno-associated viral vector-mediated IκBα gene transfer in MI/R injury. Male C57BL/6 mice were randomized to receive a recombinant adeno-associated virus (rAAV) encoding the gene for the NF-κB inhibitory protein IκBα (rAAV- IκBα) or the β-galactosidase gene (a control and inert gene; rAAV-LacZ), both at a dose of 1011 copies. Four weeks later anesthetized animals were subjected to total occlusion (45 minutes) of the left main coronary artery followed by 5 hours of reperfusion. MI/R produced a wide infarct size (IF/area-at-risk = 56 ± 8%; IF/left ventricle = 44 ± 5%) and tissue neutrophil infiltration, studied by means of elastase activity (area-at-risk = 2.5 ± 0.4 μg/gm tissue; infarct area = 2.9 ± 0.6 μg/gm tissue). Furthermore MI/R caused peak message for intercellular adhesion molecule-1 (ICAM-1) in the area-at-risk at 3 hours of reperfusion (1.2 ± 0.4 relative amount of cardiac ICAM-1 mRNA). NF-κB activation was evident at 0.5 hours of reperfusion and reached its maximum increase at 2 hours of reperfusion. rAAV-IκBα injection reduced infarct size (IF/area-at-risk = 19 ± 3%; IF/left ventricle = 10 ± 2%; p < 0.001), blocked NF-κB activation, diminished cardiac ICAM-1 expression (0.4 ± 0.02 relative amount of cardiac ICAM-1 mRNA; p < 0.001), and blunted leukocyte accumulation (area-at-risk = 0.6 ± 0.05 μg/gm tissue; infarct area = 0.4 ± 0.02 μg/gm tissue; p < 0.001). Our data indicate that rAAV-IκBα may be useful for MI/R gene therapy.
Similar content being viewed by others
Introduction
Reperfusion of coronary arteries with thrombolytic agents (Stampfer et al, 1982) or angioplasty (Stone et al, 1998; Zahn et al, 1997) markedly reduces mortality and improves left ventricular function in acute myocardial infarction. However acute myocardial infarction is still the leading cause of death in developed countries. Reperfusion after even brief periods of ischemia is associated with pathologic changes that represent either an acceleration of processes initiated during ischemia, per se, or new changes initiated during the reperfusion (Braun, 1985; Lucchesi, 1990; Muller et al, 1990).
Indeed ischemia-reperfusion triggers a release of reactive oxygen species (McCord, 1987), cytokines (Ikeda et al, 1994; Squadrito et al, 1993), and other proinflammatory mediators that activate leukocytes, endothelial cells, and myocytes. Such activation promotes the expression of adhesion molecules on the endothelium and myocardium (Altavilla et al, 1994; Ioculano et al, 1994); adhesion molecules recruit neutrophils to the surface of the endothelium and myocardium and prompt a specific cascade of cell-cell interaction, leading first to the adherence of neutrophils to the endothelium and then to trans-endothelial migration and direct interaction with myocytes (Lucchesi, 1991; Mullane, 1991).
Nuclear factor-κB (NF-κB) is an early transcription factor that modulates gene expression in various situations that require rapid and sensitive immune and inflammatory response. The prototypic inducible form of NF-κB is composed of NF-κB1 and Rel A, which both belong to the NF-κB/Rel family of proteins. Inactive NF-κB is present in the cytoplasm complexed with the inhibitory protein IκBα. NF-κB is activated by a number of incoming signals from the cell surface. Released from IκBα inhibition, NF-κB translocates into the nucleus and binds to the κB motif of the target gene, in turn causing activation of several factors (cell adhesion molecules, cytokines) involved in the inflammatory response (Ghosh et al, 1998; Gius et al, 1999; Lee and Burckart, 1998).
It has been suggested that in myocardial ischemia-reperfusion (MI/R) injury, NF-κB activates the inflammatory cascade, leading to the expression of cell adhesion molecules and cytokines and finally culminating in the deleterious accumulation of leukocytes in the ischemic myocardium (Chandrasekar et al, 2001a; Sun et al, 2001; Thourani et al, 2000). This suggests that this transcription factor may represent a new therapeutic target for myocardial protection (Valen et al, 2001). Indeed blockade of NF-κB activation by using several pharmacologic strategies has been successful in reducing myocardial damage and attenuating leukocyte infiltration in the ischemic myocardium (Valen et al, 2001).
The heart is an ideal organ for in vivo gene transfer (Su et al, 2000). Several gene delivery procedures have been used to investigate myocardial gene transfer in vivo, including the use of viral and nonviral methods. Among the novel strategies that hold promise for therapeutic gene therapy application is the use of vectors based on the adeno-associated virus (AAV). These vectors are derived from a nonpathogenetic and widespread defective parvovirus and are able to transfect both dividing and nondividing cells including cardiac muscle cells. These vectors have been found to be highly efficient for in vivo gene transfer to the mouse heart (Su et al, 2000). Furthermore, because recombinant adeno-associated virus (rAAV) vectors are devoid of any viral genes, which are expressed in trans for the packaging process, they elicit virtually no inflammatory or immune response in the sites of injection (Grimm et al, 1998).
In the present study we investigated the effect of AAV-mediated IκBα (the inhibitory protein of NF-κB) delivery in mice subjected to MI/R injury.
Results
Transgene Expression of rAAV- IκBα in the Mouse Heart
In a effort to determine the time course of rAAV-IκBα expression in mouse heart, mice were treated with an intracardiac injection of rAAV-LacZ or rAAV- IκBα. Animals were killed 4 and 8 weeks after treatment, and a Western blotting analysis was performed with an antibody reacting with IκBα. Animals treated with rAAV- IκBα showed an enhanced expression of the inhibitory protein (Fig. 1).
Western blot analysis of IκBα protein. Hearts were transduced with recombinant adeno-associated virus (rAAV)-IκBα or rAAV-LacZ, and analysis was performed 4 and 8 weeks after treatment. High level expression of IκBα is detectable. A = rAAV-LacZ; B = rAAV-IκBα after 4 weeks; C = rAAV-IκBα after 8 weeks. Data represent mean ± sd of seven experiments.
Reduced Myocardial Infarct Size After Treatment with rAAV- IκBa
The area-at-risk (AAR) showed no significant differences between each of the experimental group (Fig. 2), indicating that a similar amount of tissue was jeopardized by the occlusion of the left anterior descending artery (LAD) in each group. In the MI/R rAAV-LacZ and PBS groups, the infarct size, expressed either as a percentage of AAR or as a percentage of the left ventricle, was significantly increased. Administration of rAAV- IκBα markedly reduced the extension of infarct size (Fig. 2).
Myocardial infarct size after coronary occlusion and reperfusion in mice treated with PBS, rAAV-LacZ, or rAAV-IκBα. Infarct size is expressed as a ratio of weight of infarct tissue to weight of area-at risk (IF/AAR) or of left ventricle (IF/LV). Data represent mean ± sd of seven experiments. # p < 0.01 compared with rAAV-LacZ.
Serum creatinine phosphokinase showed a marked and significant increase in MI/R animals treated with the reporter gene LacZ or PBS. In contrast the gene transfer of the IκBα protein blunted the rise in serum creatinine phosphokinase (Table 1).
Myocardial Elastase (ELA) Levels in Mice Subjected to the rAAV-Mediated Gene Transfer of IκBa
High ELA activities were found both in the AAR and in the infarct area of the MI/R group treated with rAAV-LacZ or PBS. However, rAAV-mediated gene transfer of IκBα reduced tissue ELA levels in both the AAR and the infarct area (Table 1). ELA values, in the nonischemic myocardium, ranged between 0.22 and 0.33 μg/gm tissue in each group. There were no significant differences in ELA contents among groups (Table 1).
Increased Transgene Expression of IκBα and Blunted NF-κB Activation in the Myocardium-at-Risk After Treatment with rAAV- IκBa
Basal expression of IκBα was significantly augmented in mice subjected to rAAV- IκBα administration, thus strongly confirming the high efficiency of the rAAV for gene transfer to the heart. In mice treated with the reporter gene LacZ or PBS, the IκBα levels in the cytoplasm began to decrease at 45 minutes of occlusion and peak reduction was observed at 1 hour of reperfusion. Thereafter IκBα levels in cytoplasm increased, and after 5 hours of reperfusion the cardiac levels of the inhibitory protein were not significantly different from those of sham-operated animals (Fig. 3). The rAAV-mediated gene transfer of IκBα blunted the consistent loss of IκBα protein from the cytoplasm (Fig. 3). NF-κB activation in the nuclear extracts of myocardium was determined by electrophoretic mobility shift assay (EMSA) in the myocardium-at-risk at different time points.
Western blot analysis of IκBα protein levels in the cytoplasm of mice myocardium. Samples were normal myocardium of sham-operated mice (Sham MI/R; A) and myocardium-at-risk of mice subjected to myocardial ischemia-reperfusion (MI/R) injury and treated with PBS (B), rAAV-LacZ (C), or rAAV-IκBα (D). (Top) Representative autoradiograms highlighting IκBα protein levels at time 0 (basal) and 1 hour. (Bottom) Quantitative data and integrated intensity of IκBα protein levels. Each point represents the mean ± sd of seven experiments. *p < 0.05 versus the corresponding basal value; §p < 0.05 versus time 0.5 hours; #p < 0.05 versus rAAV-LacZ.
NF-κB binding activity was present at low levels in sham-operated animals during occlusion and reperfusion. In mice treated with the reporter gene LacZ or PBS, NF-κB rapidly increased at 0.5 hours of reperfusion and reached its peak increase after 2 hours of reperfusion (Fig. 4). In fact NF-κB binding activity was significantly higher at 2 hours than at 1 hour. The administration of rAAV- IκBα markedly reduced NF-κB binding activity (Fig. 4). No significant changes of the p65/50 subunits versus 50/50 subunits were observed.
Electrophoretic mobility shift assay (EMSA) of NF-κB in mice myocardium. Samples were normal myocardium of sham-operated mice (Sham MI/R; A) and myocardium-at-risk of mice subjected to MI/R injury and treated with PBS (B), rAAV-LacZ (C), or rAAV-IκBα (D). (Top) Representative EMSA picture highlighting NF-κB binding activity. (Bottom) Quantitative data and integrated intensity of NF-κB binding activity. Each point represents the mean ± sd of seven experiments. *p < 0.01 versus the corresponding basal value; §p < 0.05 versus time 1 hour; #p < 0.05 versus rAAV-LacZ.
Intercellular Adhesion Molecule-1 (ICAM-1) mRNA Expression in the Myocardium-at-Risk of Mice Subjected to the rAAV-Mediated Gene Transfer of IκBa
No significant change in cardiac ICAM-1 mRNA expression was observed during occlusion of the coronary artery. In mice treated with rAAV-LacZ or PBS, cardiac mRNA levels for ICAM-1 were significantly elevated during reperfusion (Fig. 5) and peak levels for adhesion molecule message were reached at 3 hours of reperfusion. ICAM-1 mRNA levels were, in fact, higher at 3 hours than at 2 hours. Administration of rAAV- IκBα blunted cardiac ICAM-1 mRNA expression (Fig. 5).
Cardiac intercellular adhesion molecule-1 (ICAM-1) mRNA expression in samples of normal myocardium of sham-operated mice (Sham MI/R; A) and myocardium-at-risk from mice subjected to MI/R injury and treated with PBS (B), rAAV-LacZ (C) or rAAV-IκBα (D). Representative autoradiograms highlighting ICAM-1 expression and quantitative data indicating relative amount of ICAM-1 mRNA. Each point represents the mean ± sd of seven experiments. *p < 0.05 versus the corresponding basal value; §p < 0.05 versus time 2 hours; #p < 0.02 versus rAAV-LacZ.
Discussion
Ischemia and reperfusion of the myocardium causes activation of NF-κB, liberation of TNF-α, and up-regulation of ICAM-1, an adhesion molecule involved in the accumulation of leukocytes in the ischemic tissues. As a consequence neutrophil adhesion may lead to aggravation and prolongation of the reperfusion injury (Kupatt et al, 1999). NF-κB is therefore critical for the transcription of multiple genes involved in MI/R injury, and it can be hypothesized that blocking NF-κB would attenuate tissue damage. Using double-stranded oligodeoxynucleotides with a specific affinity for NF-κB (decoy transfection against the transcription factor), a significant protection has been shown in experimental models of MI/R (Morishita et al, 1997; Sakaguchi et al, 2001; Sawa et al, 1997).
Regulation of NF-κB occurs through complex formation of the heterodimer with the cytoplasmic inhibitor IκBα. IκBα retains the p50/p65 complex in the cytoplasm by masking its nuclear localization sequence (Zabel et al, 1993). In addition to retaining NF-κB in the cytoplasm, a second function has been demonstrated for IκBα: it can prevent DNA binding of NF-κB, namely of the p50/p65 heterodimer (Brown et al, 1993).
Taking advantage of this physiologic regulation of the early transcription factor, an approach to study the role of NF-κB is the blockade of its activation by the transgene overexpression of its inhibitory protein IκBα. This approach may also be important to verify the potential of a gene therapy aimed at overexpressing the IκBα protein for the treatment of myocardial ischemia.
Among the novel strategies that hold promise for gene therapy applications is the use of vectors based on the AAV. These vectors are derived from a nonpathogenic and widespread defective parvovirus and are able to transduce both dividing and nondividing cells in a variety of tissue including the heart (Monahan and Samulski, 2000). More specifically it has been suggested that rAAV vectors show an exquisite tropism for cardiomyocytes (Melo et al, 2002; Phillips et al, 2002). Because rAAV vectors are devoid of any viral genes (which are expressed in trans for the packaging process), they elicit virtually no inflammatory or immune response in the sites of injections. This represents an appealing feature for such a viral vector. In agreement with this hypothesis, our study confirms this idea: in fact rAAV-LacZ–treated animals and PBS-treated mice had the same degree and extent of MI/R injury.
Ischemic and reperfused hearts treated with control vector (rAAV-LacZ) or PBS showed a marked nuclear binding of NF-κB and reduced expression of the inhibitory protein IκBα. Maximum reduction of the cytoplasmic inhibitory protein was observed at 1 hour after the release of the coronary artery, whereas peak NF-κB activation was achieved at 2 hours of reperfusion. Thereafter IκBα protein levels and NF-κB returned to basal levels, thus confirming that the transcription factor represents a rapid and early signal for controlling gene expression during reperfusion, as previously shown in an in vitro model of MI/R injury (Li et al, 1999).
In keeping with this hypothesis, cardiac ICAM-1 mRNA levels started to increase at 1 hour of reperfusion and the peak for the adhesion molecule was reached after 3 hours of reperfusion. This confirms the hypothesis that NF-κB activates an inflammatory cascade leading to the expression of cell adhesion molecules and cytokines, and, finally, culminating in the deleterious accumulation of leukocytes in the ischemic tissues. This latter event amplifies organ damage.
rAAV-mediated gene transfer of IκBα efficiently caused a transgene expression of the inhibitory protein in the myocardium. Enhanced protein expression was still present 8 weeks after administration. This finding suggests that our rAAV-VEGF may be able to achieve a long-lasting effect that could confer long-term protection after myocardial ischemia with subsequent reperfusion. The feasibility of such a gene therapy for myocardial ischemia is further underlined and straightened by the exquisite tropism of rAAV for cardiomyocytes (Melo et al, 2002; Phillips et al, 2002).
AAV-mediated gene delivery of IκBα significantly reduced NF-κB binding activity. Furthermore the IκBα gene transfer blunted cardiac ICAM-1 expression, decreased leukocyte infiltration in the myocardium, and attenuated infarct size.
Therefore, this experimental evidence led us to hypothesize that gene delivery of the IκBα protein may represent a promising strategy to interrupt the inflammatory cascade triggered by the transcription factor NF-κB during MI/R injury. Indeed, this approach might represent an interesting alternative to the “pharmacological blockade” of NF-κB in myocardial ischemia (Altavilla et al, 2000; Chandrasekar et al, 2001b; Squadrito et al, 2000; Yoshiyama et al, 2001).
Collectively, these data strongly support a key role of the early transcription factor NF-κB in the development of myocardial injury after ischemia and reperfusion of the coronary arteries. Furthermore rAAV-mediated gene transfer of IκBα represents an interesting strategy for halting the inflammatory damage after myocardial reperfusion. However further studies on the efficacy and safety of rAAV-IκBα must be performed before proposing this approach in the clinical setting.
Materials and Methods
Animals
All procedures complied with the standards for care and use of animal subjects as stated in the Guide for the Care and Use of Laboratory Animals (Institute of Laboratory Animal Resources, National Academy of Sciences, Bethesda, Maryland). Male C57BL/6 mice weighing 20 to 25 gm were used. The animals were bred in the Messina University School of Medicine Animal Facility.
rAAV Vector Preparation and Characterization
Two rAAV vectors were obtained in this study, expressing the LacZ reporter gene and the cDNA for IκBα under the control of the strong and constitutive CMV immediate early promoter. These vectors were prepared as previously shown (Grimm et al, 1998; Zolotukhin et al, 1996).
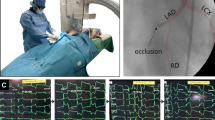
MI/R Injury
Male C57BL/6 mice were randomized to receive an rAAV encoding the gene for the NF-κB inhibitory protein IκBα (rAAV- IκBα) or the β-galactosidase gene (a control and inert gene; rAAV-LacZ), both at a dose of 1011 copies. rAAV vectors in 50 μl of PBS were injected into normal hearts at the left ventricle through the diaphragm via an incision on the upper abdomen (subdiaphragmatic approach). An additional group of animals received PBS alone (50 μl). Three injections were performed under an echocardiographic guide that allowed the exact localization of the needle in the left ventricular myocardium. The echocardiographic study was performed by an ultrasonographer experienced in rodent imaging using commercially available equipment (Sonos 5500; Hewlett Packard Medical Products, Asndover, Massachusetts) and an 8- to12-MHz transducer. Four weeks later, animals were subjected to MI/R injury. After premedication with 0.04 mg/kg atropine sulfate im, animals were anesthetized with 100 mg/kg sodium pentobarbital ip. The animals were placed in a supine position with their paws and tails taped to the operating table. The head was retracted with a thin rubber band fastened to the upper incisors. The upper portion of the trachea was exposed through a middle incision in the neck, and the pretracheal muscles were bluntly dissected. A black tipped endotracheal tube, made with PE-50 tubing, was inserted by way of the mouth into the trachea with the black tip placed 5 to 8 mm below the thyroid cartilage. Artificial respiration was maintained through the use of a respirator with an Fio2 of 0.80, a frequency of 100 strokes per minute, and a tidal volume of 0.8 to 1.2 mL, to maintain normal arterial Pao2, Paco2, and pH. The middle skin incision in the neck was extended down to the xiphoid. The left pectoris major muscle and the muscle beneath it were dissected longitudinally, without cutting these muscles, to expose the left third and fourth ribs. A parasternal incision was made to open the chest by cutting the left third and fourth ribs with a cautery pen. Dissection was aided by a microscope (Zeiss, Jena, Germany). The animal was slightly rotated to the right through the release of the left upper paw to fully expose the left ventricle. The pericardial sac was then removed, and the LAD was visualized under microscope and ligated with a 7-0 silk suture using a snare occluder. To avoid injuring the LAD, a small patch was attached to its surface. Ischemia and reperfusion were accomplished by first tightening the snare occluder (45 minutes) and then loosening it. Significant electrocardiogram changes including widening of the QRS complex, peak S-T elevation in lead II (monitored with a MacLab/4E ECG module; AD Instruments, Hastings, UK), and color changes of the AAR were considered indicative of successful coronary occlusion and reperfusion. Once the reperfusion was started, the chest was closed in layers. The respirator was weaned and the endotracheal tube was removed when the animal recovered spontaneous breathing and began to move. Five percent dextrose and whole blood from animals with the same genotype were administered ip or iv to replace the fluid and blood loss that occurred during surgery. Reperfusion lasted 5 hours. Control animals underwent all of the previously described surgical procedures apart from the fact that the snare occluder was not tied (Sham MI/R).
Evaluation of Infarct Size
At the end of reperfusion period, the thoracotomies were reopened, the LAD was reoccluded, and 1 ml of 1.0% Evans Blue (Sigma Chemical Company, St. Louis, Missouri) was injected from the apex to each heart to delineate the nonischemic tissue. The AAR was therefore determined by negative staining. The heart were then excised, washed with PBS, and cut into five transverse slices. Sections were placed between two Plexiglas plates, and the outlines of the entire areas of the left ventricle and the unstained areas of the myocardium (ie, the AAR) were traced on transparencies. The slices were then placed in a 96-well culture plate, stained for 15 minutes at room temperature with 1.0 ml of 1.5% 2,3,5-triphenyltetrazolium chloride (Sigma Chemical Company) solution to determine the infarct size, weighed, and photographed under a microscope (Olimpus Company, Tokyo, Japan). Viable tissues stained deep red, and infarcted areas depleted of coenzyme and dehydrogenases were unstained. Left ventricle area, AAR, and infarct size were determined by computerized planimetry using Adobe Photoshop. The weight of the nonischemic area, AAR, and the infarction area were then calculated as a percentage of corresponding area multiplied by the weight of the slice.
Serum Creatine Phosphokinase Activity
Serum levels of creatine phosphokinase and its myocardium-specific isoform (CK-MB) were measured with the use of commercial kits (Sigma Chemical).
Cardiac ELA Content
ELA levels were evaluated as an index of polymorphonuclear neutrophil accumulation and activation in the jeopardized tissue because this enzyme is released from the stimulated granulocytes at the site of injury. The analysis was performed in the nonischemic area, AAR, and infarction area by using a specific immunoassay kit (PMN ELA, IMAC, Catalog No. 11332; Merck, Darmstadt, Germany). ELA activity was expressed in microgram per gram (μg/gm) of tissue.
Isolation of Nuclear and Cytoplasmic Proteins
Briefly 70 mg of pulverized myocardial samples (obtained from the AAR at different time points) were homogenized in 0.8 ml of ice cold hypotonic buffer [10 mm HEPES, pH 7.9; 0.1 mm EDTA; 0.1 mm EGTA; 1 mm dithiothreitol; protease inhibitors: 0.5 mm phenyl methylsulfonyl fluoride, aprotinin, pepstatin, leupeptin (10 μg/ml each); and phosphatase inhibitors: 50 mm NAF, 30 mm β-glycerophosphate, 1 mm Na3VO4, and 20 mm ρ-nitrophenyl phosphate]. Nuclear and cytoplasmic proteins were isolated as previously reported (Altavilla et al, 2001).
Western Blot Analysis of IκBα in Cytoplasm
Cytoplasmic proteins (20 μg) from each sample were mixed with 2 × SDS sample buffer [62 mm Tris (pH 6.8), 10% glycerol, 2% SDS, 5% β-mercaptoethanol, 0.003% bromophenol blue], heated at 95° C for 5 minutes, and separated by SDS-PAGE. Western blot analysis of IκBα in the cytoplasm was performed as previously reported Sawa et al (1997). The IκBα protein signal was quantified by scanning densitometry using a bio-image analysis system (BIO-PROFIL; Celbio, Milan, Italy). The results from each experimental group were expressed as relative integrated intensity compared with the sham MI/R group measured in the same batch.
EMSA
NF-κB binding activity was performed in a 15-μl binding reaction mixture containing 1% binding buffer [50 μg/ml of double-stranded poly(dI-dC), 10 mm Tris HCl (pH 7.5), 50 mm NaCl, 0.5 mm EDTA, 0.5 mm dithiothreitol, 1 mm MgCl2, and 10% glycerol], 15 μg of nuclear proteins, and 35 fmol (50,000 cpm, Cherenkov counting) of double-stranded NF-κB consensus oligonucleotide (5′-AGT TGA GGG GAC TTT CCC AGG C-8′; Promega, Madison, Wisconsin) which was end-labeled with [γ32P]ATP (3000 Ci/mmol at 10 mCi/ml; Amersham Life Sciences, Arlington Heights, Illinois) using T4 polynucleotide kinase. This methodology has been previously described (Sawa et al, 1997). The binding bands were quantified by scanning densitometry of a bio-image analysis system (BIO-PROFIL). The results for each time point from each group were expressed as relative integrated intensity compared with the sham MI/R group measured in the same batch because the integrated intensity of group samples from different EMSA batches would be affected by the half-life of the isotope, exposure time, and background levels.
RNA Isolation and RT-PCR
To evaluate the message for the ICAM-1, total cellular RNA was extracted from heart specimens (AAR) harvested from mice killed at different time points. The methodology has been previously reported (Sawa et al, 1997).
The following oligonucleotide pairs were used (5′ oligo/3′ oligo), each sequence as 5′ to 3′: ICAM-1: AGGTGGATATCCGGTAGA/CCTTCTAAGTCCTCCAACA; GAPDH: ACCACCATGGAGAAGGTCGG/CTCAGTGTAGCCCAGGATGGC. The optimal cycle number for ICAM-1 was 25, and we used a PCR-negative and a PCR-positive control without cDNA or with a known cDNA, respectively. A portion of the PCR product was subjected to electrophoresis and transferred to a nylon membrane, which was prehybridized with oligonucleotide probes, radiolabeled with [32P]ATP by a T4 oligonucleotide kinase. After an overnight hybridization at 55° C, filters underwent autoradiography in a dark room with a fixed camera. The captured image, sent to image analysis software (BIO-PROFIL) was subjected to densitometric analysis.
Statistical Analysis
Data are expressed as means ± sd. The difference between the means of two groups was evaluated with an ANOVA followed by Bonferroni's test and was considered significant when p < 0.05.
References
Altavilla D, Deodato B, Campo GM, Arlotta M, Miano M, Squadrito G, Saitta A, Cucinotta D, Ceccarelli S, Ferlito M, Tringali M, Minutoli L, Caputi AP, and Squadrito F (2000). IRFI 042, a novel dual vitamin E-like antioxidant, inhibits activation of nuclear factor-κB and reduces the inflammatory response in myocardial ischemia-reperfusion injury. Cardiovasc Res 47: 515–528.
Altavilla D, Saitta A, Guarini S, Galeano M, Squadrito G, Cucinotta D, Santamaria LB, Mazzeo AT, Campo GM, Ferlito M, Minutoli L, Bazzani C, Bertolini A, Caputi A, and Squadrito F (2001). Oxidative stress causes nuclear factor-kappaB activation in acute hypovolemic hemorrhagic shock. Free Radic Biol Med 30: 1055–1066.
Altavilla D, Squadrito F, Ioculano M, Canale P, Campo GM, Zingarelli B, and Caputi AP (1994). E-selectin in the pathogenesis of experimental myocardial ischaemia-reperfusion injury. Eur J Pharmacol 3: 45–51.
Braun E (1985). Myocardial reperfusion: A double-edged sword? J Clin Invest 35: 1713–1719.
Brown K, Park S, Kanno T, Franzoso G, and Sienbelist U (1993). Mutual regulation of the transcriptional activator NF-κB and its inhibitor, IκB-α. Proc Natl Acad Sci USA 90: 2532–2536.
Chandrasekar B, Nelson JF, Colston JT, and Freeman GL (2001a). Calorie restriction attenuates inflammatory responses to myocardial ischemia-reperfusion injury. Am J Physiol 280: H2094–H20102.
Chandrasekar B, Smith JB, and Freeman GL (2001b). Ischemia-reperfusion of rat myocardium activates nuclear factor KappaB and induces neutrophil infiltration via lipopolysaccharide-induced CXC chemokine. Circulation 103: 2296–2302.
Ghosh S, May MJ, and Kopp EB (1998). NF-kappa B and Rel proteins: Evolutionarily conserved mediators of immune responses. Annu Rev Immunol 16: 225–260.
Gius D, Botero A, Shah S, and Curry HA (1999). Intracellular oxidation/reduction status in the regulation of transcription factor NF-kappa B and AP-1. Toxicol Lett 106: 93–106.
Grimm D, Kern A, Rittner K, and Kleinschmidt JA (1998). Novel tools for production and purification of recombinant adenoassociated virus vectors. Hum Gene Ther 9: 2745–2760.
Kupatt C, Habazetti H, Goedecke A, Wolf DA, Zahler S, Boekstegers P, Kelly RA, and Becker BF (1999). Tumor necrosis factor-alpha contributes to ischaemia- and reperfusion-induced endothelial activation in isolated hearts. Circ Res 84 (4): 392–400.
Ikeda U, Ikeda M, Kano S, and Shimada K (1994). Neutrophil adherence to rat cardiac myocytes by pro-inflammatory cytokines. J Cardiovasc Pharmacol 23: 647–652.
Ioculano M, Squadrito F, Altavilla D, Canale P, Squadrito G, Campo GM, Saitta A, and Caputi AP (1994). Antibodies against intercellular adhesion molecule 1 protect against myocardial ischaemia-reperfusion injury in rat. Eur J Pharmacol 264: 143–149.
Lee J and Burckart GJ (1998). Nuclear factor kappa B: Important transcription factor and therapeutic target. J Clin Pharmacol 38: 981–993.
Li C, Browder W, and Kao RL (1999). Early activation of transcription factor NF-kappa B during ischaemia in perfused rat heart. Am J Physiol 276: H543–H552.
Lucchesi BR (1990). Modulation of leukocyte mediated myocardial reperfusion injury. Annu Rev Physiol 52: 561–576.
Lucchesi BR (1991). Modulation of leukocyte-mediated myocardial ischaemia reperfusion injury. Annu Rev Physiol 84: 400–411.
McCord JM (1987). Oxygen-derived radicals: A link between reperfusion injury and inflammation. Fed Proc 46: 2402–2406.
Melo LG, Agrawal R, Zhang L, Rezvani M, Mangi AA, Ehsan A, Griese DP, Dell'Acqua G, Mann MJ, Oyama J, Yet SF, Layne MD, Perrella MA, and Dzau VJ (2002). Gene therapy strategy for long term myocardial protection using adeno-associated virus mediated delivery of heme oxygenase gene. Circulation 105 (5): 602–607.
Monahan PE and Samulski RJ (2000). AAV vectors: Is clinical success on the horizon? Gene Ther 7: 24–30.
Morishita R, Sugimoto T, Aoki M, Kida I, Tomita N, Moriguchi A, Maeda K, Sawa Y, Kaneda Y, Higaki J, and Ogihara T (1997). In vivo transfection of cis element “decoy” against nuclear factor kappaB binding site prevents myocardial infarction. Nat Med 3 (8): 894–899.
Mullane K (1991). Neutrophil and endothelial changes in reperfusion injury. Trends Cardiovasc Med 1: 282–289.
Muller DW, Topo EJ, Califf RM, Sigmon KN, Gorman L, George BS, Kereiakes DJ, Lee KL, and Ellis SG (1990). Relationship between antecedent angina pectoris and prognosis after thrombolytic therapy for acute myocardial infarction. Thrombolysis and Angioplasty in Myocardial Infarction (TAMI) Study Group. Am Heart J 119: 224–231.
Phillips MI, Tang Y, Schmidt-Ott K, Qian K, and Kagiyana S (2002). Vigilant vector: Heart-specific promoter in an adeno-associated virus vector for cardioprotection. Hypertension 39 (2): 651–655.
Sakaguchi T, Sawa Y, Fukushima N, Nishimura M, Ichikawa H, Kaneda Y, and Matsuda H (2001). A novel strategy of decoy transfection against nuclear factor-kappaB in myocardial preservation. Ann Thorac Surg 71 (82): 624–629.
Sawa Y, Morishita R, Suzuki K, Kagisaki K, Kaneda Y, Maeda K, Kadoba K, and Matsuda H (1997). A novel strategy for myocardial protection using in vivo transfection of cis element “decoy” against NFkappaB binding site: evidence for a role of NFkappaB in ischemia-reperfusion injury. Circulation 96 (Suppl 9): II280–II284.
Squadrito F, Altavilla D, Squadrito G, Saitta A, Deodato B, Arlotta M, Minutoli L, Quartarone C, Ferlito M, and Caputi AP (2000). Tacrolimus limits polymorphonuclear leukocyte accumulation and protects against myocardial ischaemia-reperfusion injury. J Mol Cell Cardiol 32: 429–440.
Squadrito F, Altavilla D, Zingarelli B, Ioculano M, Calapai G, Campo GM, Miceli A, and Caputi AP (1993). Tumor necrosis factor involvement in myocardial ischaemia-reperfusion injury. Eur J Pharmacol 237: 223–230.
Stampfer MJ, Goldhaber SZ, Yusuf S, Peto R, and Hennekens CH (1982). Effect of intravenous streptokinase on acute myocardial infarction: Pooled results from randomized trials. N Engl J Med 307: 1180–1182.
Stone GW, Brodie BR, Griffin JJ, Morice MC, Costantini C, St Goar FG, Overlie PA, Popma JJ, McDonnell J, Jones D, O'Neill WW, and Grines CL (1998). Prospective, multicenter study of the safety and feasibility of primary stenting in acute myocardial infarction: in-hospital and 30-day results of the PAMI stent pilot trial. Primary Angioplasty in Myocardial Infarction Stent Pilot Trial Investigators. J Am Coll Cardiol 31 (1): 23–30.
Su H, Lu R, and Kan YW (2000). Adeno-associated viral vector-mediated vascular endothelial growth factor gene transfer induces neovascular formation in ischemic heart. Proc Natl Acad Sci USA 97: 13801–13806.
Sun B, Fan H, Honda T, Fujimaki R, Lafond-Walker A, Masui Y, Lowenstein CJ, and Becker LC (2001). Activation of NF kappa B and expression of ICAM-1 in ischemic-reperfused canine myocardium. J Mol Cell Cardiol 33: 109–119.
Thourani VH, Brar SS, Kennedy TP, Thornton LR, Watts JA, Ronson RR, Zhao Z, Sturrock AL, Hoidal JR, and Vinten-Johansen J (2000). Nonanticoagulant heparin inhibits NF-κB activation and attenuates myocardial reperfusion injury. Am J Physiol Heart Circ Physiol 48: H2084–H2093.
Valen G, Yan ZQ, and Hansson GK (2001). Nuclear factor kappa-B and the heart. J Am Coll Cardiol 38: 307–314.
Yoshiyama M, Omura T, Takeuchi K, Kim S, Shimasa K, Yamagishi H, Teragaki M, Akioka K, Iwao H, and Yoshikawa J (2001). Angiotensin blockade inhibits increased JNKs, AP-1 and NF-kappa B DNA-binding activities in myocardial infarcted rats. J Mol Cell Cardiol 33: 799–810.
Zabel U, Henkel T, Dos Santos Silva M, and Baeuerle PA (1993). Nuclear uptake control of NF-κB by MAD-3 and IκB protein present in the nucleus. EMBO J 12: 201–211.
Zahn R, Koch A, Rustige J, Schiele R, and Wirtzfeld A (1997). Primary angioplasty versus thrombolysis in the treatment of acute myocardial infarction. ALKK Study Group. Am J Cardiol 79: 264–269.
Zolotukhin S, Potter M, Hauswirth WW, Guy J, and Muzyczka N (1996). A “humanized” green fluorescent cDNA adapted for high-level expression in mammalian cells. J Virol 70: 4646–4654.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Squadrito, F., Deodato, B., Squadrito, G. et al. Gene Transfer of IκBα Limits Infarct Size in a Mouse Model of Myocardial Ischemia-Reperfusion Injury. Lab Invest 83, 1097–1104 (2003). https://doi.org/10.1097/01.LAB.0000082060.39079.A6
Received:
Published:
Issue date:
DOI: https://doi.org/10.1097/01.LAB.0000082060.39079.A6
This article is cited by
-
Promise of adeno-associated virus as a gene therapy vector for cardiovascular diseases
Heart Failure Reviews (2017)
-
AAV Vectors for Cardiac Gene Transfer: Experimental Tools and Clinical Opportunities
Molecular Therapy (2011)
-
Culture of skeletal myoblasts from human donors aged over 40 years: dynamics of cell growth and expression of differentiation markers
Journal of Translational Medicine (2005)