Abstract
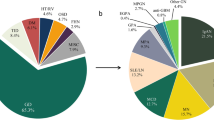
Dense deposit disease (first reported in 1962) was classified as subtype II of membranoproliferative glomerulonephritis in the early 1970s. Over the last 30 years, marked differences in etiology and pathogenesis between type I membranoproliferative glomerulonephritis and dense deposit disease have become apparent. The sporadic observation that dense deposit disease can be seen with markedly different light microscopy appearances prompted this study. The goal was to examine a large number of renal biopsies from around the world to characterize the histopathologic features of dense deposit disease. Eighty-one cases of dense deposit disease were received from centers across North America, Europe and Japan. Biopsy reports, light microscopy materials and electron photomicrographs were reviewed and histopathologic features scored. Sixty-nine cases were acceptable for review. Five patterns were seen: (1) membranoproliferative n=17; (2) mesangial proliferative n=30; (3) crescentic n=12; (4) acute proliferative and exudative n=8 and (5) unclassified n=2. The age range was 3–67 years, with 74% in the range of 3–20 years; 15% 21–30 years and 11% over 30 years. Males accounted for 54% and females 46%. All patients with either crescentic dense deposit disease or acute proliferative dense deposit disease were between the ages of 3 and 18 years. The essential diagnostic feature of dense deposit disease is not the membranoproliferative pattern but the presence of electron dense transformation of the glomerular basement membranes. Based upon this study and the extensive data developed over the past 30 years, dense deposit disease is clinically distinct from membranoproliferative glomerulonephritis and is morphologically heterogeneous with only a minority of cases having a membranoproliferative pattern. Therefore, dense deposit disease should no longer be regarded as a subtype of membranoproliferative glomerulonephritis.
Similar content being viewed by others
Main
Membranoproliferative glomerulonephritis is a histologic pattern associated with an eclectic assortment of diseases ranging from sickle cell anemia through hepatitis C infection to transplant glomerulopathy (reviewed by Appel et al,1 Rennke,2 and Zhou and Silva3). The hypothesis of this work is that membranoproliferative glomerulonephritis type II is a separate disease entity and should be separated from the membranoproliferative glomerulonephritis category and called dense deposit disease in reference to its unique and diagnostically unifying morphologic finding.
Membranoproliferative glomerulonephritis type II is rare and only a relatively small number of studies of this disease have been published.4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16, 17, 18, 19, 20, 21 In these reports, the histologic description of membranoproliferative glomerulonephritis II is usually a membranoproliferative pattern, although other light microscopy changes including a crescentic form and a mesangial proliferative form are included in some of the reports.6, 7, 8, 12, 13, 15, 16, 17, 20, 21, 22, 23 However, the frequency, variability and definition of the light microscopy patterns present in patients with dense deposit disease are not apparent from previous reports. Thus, the purpose of this study was to examine a large number of renal biopsies from patients with dense deposit disease in order to characterize the light microscopic patterns seen in association with the diagnostic feature of dense deposit disease, electron dense transformation of the glomerular basement membranes.
Materials and methods
Cases were received from North America, Japan and the European Union. The slides and reports were coded and patient data removed at the local center before being sent to the authors for review. Clinical information was gathered from the surgical pathology report form and entered onto coded standardized score sheets. Representative slides, immunohistochemistry or immunofluorescence photomicrographs and electron microscopy photographs were examined and scored using a standardized score sheet. All materials were reviewed without knowledge of the clinical history. This study complied with all human subject protection requirements at each submitting institution and was approved by the local institutional review board.
Pathology Review
The light microscopy material was reviewed and scored by compartment. Glomeruli were counted and the number with global and/or segmental sclerosis was determined. The number and type of crescents (cellular, fibrocellular or fibrous) were determined. The presence or absence of hypercellularity was ascertained and then specified as to the presence of infiltrating cells and/or endocapillary proliferation. Mesangial matrix expansion was also recorded. The basement membranes of glomeruli, tubules and Bowman's capsules were graded for the presence of PAS-positive ribbons. Tubular atrophy, interstitial fibrosis and interstitial inflammation were graded. Blood vessel changes, if any, were recorded. For semiquantitative analysis, a scoring system of 0–3 was used.
Immunohistochemistry information was obtained from the report including immunoreactant, intensity and location. Thioflavin T staining, when available, was also recorded.
Electron microscopy photographs were examined and scored for endocapillary proliferation, discrete electron dense deposits and dense transformation of the glomerular basement membrane. Electron dense transformation was characterized by density and location. The basement membranes of Bowman's capsule and tubules were also examined and scored for dense transformation when available.
Clinical Review
Clinical data available at the time of biopsy was abstracted from the original renal biopsy reports, but was usually very limited in scope. The patient's age and gender were noted. Other clinical information was not present in most cases eliminating analysis of presenting symptoms, initial laboratory data, treatment or follow-up.
Statistics
Nonparametric semiquantitative data were analyzed using the Kruskal–Wallis nonparametric analysis of variance followed by post hoc testing with Dunn's multiple comparisons test. The data were collated onto a Microsoft® Excel spreadsheet (Microsoft Corporation, Redmond, WA, USA) and statistical analysis was carried out using GraphPad InStat® (GraphPad Software Inc., San Diego, CA, USA) using an Apple® Macintosh Mac Mini computer (Apple Computer, Cupertino, CA, USA).
Results
Eighty-one cases were received. Twelve were eliminated from further examination because they were either repeat biopsies, transplant biopsies or because electron photomicrographs were not available.
Pathology
Five histologic patterns were identified by their light microscopic appearance: membranoproliferative, mesangial proliferative, crescentic, acute proliferative and exudative and unclassified (Table 1, Figures 1, 2, 3, 4, 5, 6 and 7). Only two cases were categorized as unclassified, so this group, although described below, was not included in comparative analysis. The unifying diagnostic feature of all five patterns is the presence of electron dense transformation of the glomerular basement membranes (Figure 4). Still, there was variation in the frequency and distribution of the basement membrane changes (Table 2). Some glomeruli were diffusely affected, while others had an interrupted linear pattern, or a ‘linked sausage’ appearance. Occasional dense deposits were found in the subendothelial space separate from the lamina densa. These discrete deposits were as electron dense as the linear electron dense transformation seen in other areas. Subepithelial ‘hump-like’ dense transformations of the glomerular basement membrane were sometimes seen (Figure 7). Electron dense transformation of the tubular basement membranes was found in 24% and the basement membranes of Bowman's capsule in 30% of cases where examined (Table 2).
Dense deposit disease, light microscopy patterns. (a) Membranoproliferative dense deposit disease pattern 1: hypercellularity and lobular appearance, × 400 PAS. (b) Mesangial proliferative dense deposit disease pattern 2 mild mesangial cell and matrix increase, × 400 PAS. (c) Crescentic dense deposit disease pattern 3 cellular crescent, × 400 PAS. (d) Acute proliferative and exudative dense deposit disease pattern 4 diffuse endocapillary proliferation with numerous macrophages and neutrophils × 400 PAS.
Dense deposit disease, distinctive features by light microscopy. (a) Strongly PAS-positive ‘ribbons’ along glomerular basement membranes × 400 PAS. (b) Thioflavin T positive in glomerular basement membranes and Bowman's capsule basement membranes, × 400 thioflavin T. (c) Toluidine blue stain intermittently accentuated in glomerular basement membranes and Bowman's capsule basement membranes (normal area single arrowhead, accentuated area double arrowhead, boxed area shown at higher magnification in d), × 600 toluidine blue. (d) High power of toluidine blue stained area of Bowman's capsule showing normal basement membrane thickness and density (single arrowhead) and accentuated basement membrane (double arrowhead), × 1200 toluidine blue.
Dense deposit disease crescentic pattern (a, b); dense deposit disease unclassified pattern (c, d), electron microscopy, uranyl acetate and lead citrate. (a) Ribbons of electron dense transformation of glomerular basement membranes, sometimes forming subepithelial ‘humps’, paramesangial areas and ‘waist’ areas, × 5000. (b) Electron dense transformation of glomerular basement membranes forming subepithelial ‘humps’, × 20 000 uranyl acetate and lead citrate. (c, d) Intermediate electron dense transformation in ribbons along glomerular basement membranes and mesangial regions, × 5000.
Dense deposit disease unclassified pattern. Mild PAS-positive mesangial matrix increase. (a) PAS stain × 200, (b) PAS stain × 400, (c) C3-positive staining in loops and mesangial regions with ‘ring’ pattern, fluorescein-conjugated anti-C3 antibody × 400. (d) Thioflavin T-positive staining in glomerular basement membranes, mesangial areas, Bowman's capsule basement membranes and tubular basement membranes, thioflavin T stain × 200.
Presence of ‘humps’ (deeply electron dense, hillock-shaped transformations along the subepithelial side of the glomerular basement membrane) by dense deposit disease histologic pattern: 1, membranoproliferative dense deposit disease; 2, mesangial proliferative dense deposit disease; 3, crescentic dense deposit disease; 4, acute proliferative and exudative dense deposit disease; 5, unclassified dense deposit disease had only two cases and was not used for further analysis. Data expressed as mean semiquantitative score × 100.
By light microscopy, the number of glomeruli, percentage global sclerosis, percentage segmental sclerosis, and interstitial and vascular changes were similar among the four major histologic patterns. Immunohistochemical examination revealed that mesangial C3 was present in every case (Table 3) and mesangial ‘rings’ were seen in all cases when immunofluorescence photomicrographs were available for review (Figure 3).
Histologic Patterns
Membranoproliferative dense deposit disease is characterized by endocapillary proliferation producing a mesangial lobular appearance (Figure 1), sometimes in association with a markedly eosinophilic and PAS-positive alteration (so-called ribbons) along glomerular, tubular and other basement membranes (Figure 2a). Capillary closure was not a criterion for endocapillary proliferation. These membranoproliferative features were most often focal and segmental and only rarely were diffuse. Four of the 17 patients had mild or moderate mesangial sclerosis, while the remaining 13 had minimal or none. Endocapillary proliferation was significantly greater in membranoproliferative dense deposit disease than in mesangial proliferative dense deposit disease or crescentic dense deposit disease (Table 4). Glomerular basement membrane double contours were present on PAS and silver stain in many capillary loops. The degree of glomerular basement membrane thickening and/or duplication was most pronounced in this pattern (Table 4). The capillary loop ribbons were thioflavin-T positive, and accentuated by toluidine blue staining of plastic-embedded tissue for electron microscopy (Figure 2). Tubular basement membranes and the basement membranes of Bowman's capsule also showed similar ribbons in a segmental pattern. Immunofluorescence microscopy revealed deposits of C3 in a diffuse or segmental pattern along the glomerular, tubular and Bowman's capsule basement membranes (Figure 3). C3 staining frequently formed a distinctive ring-like pattern in the mesangial regions that suggested the diagnosis of dense deposit disease (Figure 3). Immunoglobulins were usually absent and staining for more than one immunoglobulin was not seen in membranoproliferative dense deposit disease (Table 3). Electron microscopy showed the characteristic diffuse to segmental, linear very dense transformation of the lamina densa (Figure 4). Spherical electron dense transformation was common in the mesangium.
Mesangial proliferative dense deposit disease is characterized by focal segmental mesangial hypercellularity. Mesangial hypercellularity was defined as more than three cells in any mesangial region in one or more glomeruli. Some glomeruli appeared normal by light microscopy (Figure 1). Endocapillary proliferation was generally absent and, when present, was focal and mild. Immunoglobulins were more often present in mesangial proliferative dense deposit disease both singly and in combination (Table 3). The one case that stained for all three immunoglobulins tested, IgG, IgM and IgA, was a mesangial proliferative dense deposit disease case. C3 positivity was universal, while C1q was present in a third of the cases examined. The characteristic very dense transformation of the glomerular basement membranes was present but was more intermittent when compared to membranoproliferative dense deposit disease (Table 2). On the other hand, subendothelial dense transformation and subepithelial ‘humps’ were more common.
Crescentic dense deposit disease is defined by the presence of crescents in 50% or more of the glomeruli available for examination (Figure 1). The average number of glomeruli in this group was 30 with a range of 6–83. The two cases out of 12 cases with less than 10 glomeruli for examination had crescents in five of six and seven of eight glomeruli, respectively. Cellular crescents and total crescents were much more frequent in crescentic dense deposit disease than in the other patterns (Table 4). The underlying histologic pattern was either membranoproliferative dense deposit disease or mesangial proliferative dense deposit disease with endocapillary proliferation varying from essentially normal (five of 12 cases) to focal and segmental endocapillary proliferation (four of 12 cases) to diffuse endocapillary proliferation (three of 12 cases). The immunofluorescence findings were similar to membranoproliferative dense deposit disease. Staining for immunoglobulins was rare and the presence of more than one immunoglobulin was not seen in crescentic dense deposit disease (Table 3). By electron microscopy, the typical dense transformation of the basement membranes was present. In addition, electron dense material was also present as large subepithelial hump-like transformations in the outer portions of the glomerular basement membranes, at the junction of the glomerular basement membrane and the mesangial area (‘waist’ deposits) and extending from the mesangium itself (Figure 5a and b).
Acute proliferative and exudative dense deposit disease shows diffuse glomerular hypercellularity due to endocapillary proliferation with prominent neutrophilic infiltration (Figure 1). The proliferative changes led to occlusion of most capillary lumens. Endocapillary proliferation was significantly greater in acute proliferative and exudative dense deposit disease compared to either mesangial proliferative dense deposit disease or crescentic dense deposit disease (Table 4). Glomerular inflammatory cell infiltration was also significantly more common in acute proliferative and exudative dense deposit disease compared to the other patterns (Table 4). By light microscopy, this variant can be difficult to distinguish from post-infectious glomerulonephritis. However, by immunofluorescence, the presence of ring-like deposits of C3 suggests dense deposit disease. In addition, immunoglobulin deposits were frequently absent and, when present, were often focal and sparse. Staining for more than one immunoglobulin was not seen in acute proliferative and exudative dense deposit disease (Table 3). Five of six biopsies classified as acute proliferative and exudative dense deposit disease were positive for C1q, significantly more common than in either membranoproliferative dense deposit disease or crescentic dense deposit disease (Table 3). Electron microscopy showed the typical very dense linear transformation of glomerular basement membranes and similar electron dense material in the mesangium. About half of the cases also had subepithelial ‘hump-like’ dense transformations of the glomerular basement membrane similar to changes seen in crescentic dense deposit disease (Table 2).
Unclassified dense deposit disease is defined by the presence of intermediately electron dense transformation of the glomerular basement membranes and mesangial regions (Figure 5c and d). Often this transformation had a granular appearance. There was variable focal, segmental endocapillary proliferation with PAS and thioflavin T-positive ribbons present in loops and mesangial areas (Figure 6) similar to the other patterns of dense deposit disease and corresponding to the intermediately electron dense transformation seen by electron microscopy. Immunoglobulins were negative by immunohistochemistry but C3 staining was present along basement membranes and within the mesangium forming typical ‘mesangial rings’ (Figure 6). Although the electron dense transformation of the basement membranes was not as deep as that seen in the other forms of dense deposit disease, the pattern and distribution of the transformation along the basement membranes was similar. Only two cases were categorized as unclassified dense deposit disease, so this group was not included in comparative analysis.
Clinical Data
Gender was specified in 57 cases. There were 31 male and 26 female subjects with no differences between the various dense deposit disease patterns (Table 5). Age at presentation was given in all cases. The overall median age was 14 years with a range of 3–67 years (Figure 8). All patients with either pattern 3 (crescentic) or pattern 4 (acute proliferative and exudative) were 18 years or younger.
Age at presentation by dense deposit disease histologic pattern: 1, membranoproliferative dense deposit disease; 2, mesangial proliferative dense deposit disease; 3, crescentic dense deposit disease; 4, acute proliferative and exudative dense deposit disease; 5, unclassified dense deposit disease had only two cases and was not used for further analysis. Median age=14 years (line).
Discussion
In 1975, Habib et al6 noted the similarity by light microscopy of dense deposit disease and membranoproliferative glomerulonephritis, and classified dense deposit disease as a variant of membranoproliferative glomerulonephritis, calling dense deposit disease membranoproliferative glomerulonephritis, type II. Interestingly, the classic light microscopic features of membranoproliferative glomerulonephritis I were present in just 11 of 44 patients (25%). The majority of patients had mild (11/44, 25%) or moderate (22/44, 50%) mesangial hypercellularity.
The single defining or unifying feature of dense deposit disease in the current study is the presence of electron dense transformation of the glomerular basement membranes by electron microscopy. Alterations similar to those seen within the glomerular basement membrane were often present along tubular basement membranes and the basement membrane of Bowman's capsule, when examined.9, 24 The major finding from this international series of dense deposit disease cases is that the light microscopy pattern is variable and that the presence of a membranoproliferative pattern is seen in only one of four patients with dense deposit disease (similar to Habib et al above6).
Mesangial proliferative dense deposit disease is much more common than the membranoproliferative pattern, accounting for 45% of our cases. Twenty-nine of 30 mesangial proliferative cases showed only minimal to mild proliferation, changes easily confused on light microscopy with minimal changes by light microscopy or diffuse mesangial hypercellularity. However, the unique immunofluorescence pattern with mesangial ‘rings’ on C3 staining and the diagnostic electron dense transformation of the glomerular basement membrane by electron microscopy leads to the correct diagnosis. The mesangial proliferative pattern was described by Sibley and Kim22 in 1984 and, in a follow-up paper, Kashtan et al demonstrated that the patients with the mesangial proliferative pattern had significantly better long-term outcome.16
Crescentic dense deposit disease, pattern 3, occurred only in patients less than 17 years and may be a unique form of dense deposit disease. In 1982, a case of crescentic dense deposit disease treated with high-dose steroids, azothioprine, dipyridamole and heparin with complete resolution of disease was presented by Kher et al.23 West et al20 described a group of children with crescentic glomerulonephritis, many of which had electron dense transformation of glomerular basement membranes, but all responded to high-dose steroid treatment. The West group did not characterize their cases as dense deposit disease, but concluded that these cases represented a new entity, juvenile acute nonproliferative glomerulitis or JANG. In a more recent study, Hoschek et al21 described two patients with crescentic dense deposit disease that were treated with high-dose steroids and went into complete remission. These studies stand in contrast to the previous literature concerning crescentic glomerulonephritis in childhood including extensive crescent formation in dense deposit disease, where end-stage renal disease is the usual outcome.12, 15, 25, 26, 27, 28 Overall, this pattern requires further clinical study to determine if the expected universally dismal outcome is reversible with high-dose steroid treatment in some subset of patients.20, 21
Previous studies have described the presence of increased neutrophils in otherwise typical membranoproliferative or mesangial proliferative lesions.6, 15, 29 In addition, the diffuse endocapillary proliferation with neutrophilic infiltration seen in our study has been previously reported.17 This pattern is easily mistaken for a postinfectious glomerulonephritis on light microscopy examination alone. Complicating a correct diagnosis even further is the finding of either IgG or IgM by immunofluorescence in six of eight cases and C3 in all cases. Electron microscopy is required for a correct diagnosis of dense deposit disease in these patients.
The unclassified pattern of dense deposit disease was seen in two cases and because of the limited number, no further statistical analysis was carried out. Unclassified dense deposit disease was similar to the mesangial proliferative pattern by light microscopy and immunofluorescence, differing only in the intensity of the glomerular basement membrane transformation by electron microscopy. Given the similarity to dense deposit disease in almost all respects, it is likely that this unclassified form is a rare pattern of dense deposit disease in need of further study.
Many of the early reports on dense deposit disease presented compelling evidence that membranoproliferative glomerulonephritis I and dense deposit disease are different disease entities all together.5, 9, 10, 22, 30 More recently, Appel et al1 published a detailed review of dense deposit disease documenting the unique characteristics of dense deposit disease that separate it from membranoproliferative glomerulonephritis I and other forms of glomerular disease. Briefly, dense deposit disease is almost exclusively a disease of children and teens presenting primarily with the acute nephritic syndrome, whereas membranoproliferative glomerulonephritis I, although it occurs as an idiopathic disease in childhood, occurs much more commonly in adults presenting primarily with the nephrotic syndrome (Table 6). Patients with membranoproliferative glomerulonephritis I may have systemic manifestations associated with an underlying associated condition, while those with dense deposit disease primarily display only the symptoms of renal disease. Blood levels of complement reflect the different complement components involved in the two entities (reviewed by Nakopoulou31). In addition, C3 nephritic factor is much more commonly found in patients with dense deposit disease. Membranoproliferative glomerulonephritis I is considered to be an immune complex mediated glomerular disease, while dense deposit disease is related to abnormalities in complement cascade control (reviewed by Appel et al1 and Nakopoulou31). Membranoproliferative glomerulonephritis I is commonly associated with hepatitis C and other infections with or without cryoglobulinemia.
Based on all of the above, it is important to consider the classification of dense deposit disease in the overall scheme of glomerular diseases. Correct morphological classification remains critical in the study of disease and if a classification system is to remain useful, it must be modified as more information is obtained about the specific diseases included under its umbrella.32 As discussed by Foucar,32 measures of both ‘accuracy’ and ‘precision’ are important, but very different methods of determining the utility of any classification system. Precision, the measure of the degree of intra- and interobserver variability in assigning a specific biopsy to a given diagnostic category is at least moderate when using the general term membranoproliferative glomerulonephritis. However, the accuracy, a measure of the closeness of the diagnosis to the actual clinical situation, is quite low given the variability of clinical conditions associated with a membranoproliferative pattern. Thus, as it becomes possible, disease subsets that can be recognized as distinct entities must be removed from the generic category of membranoproliferative glomerulonephritis. Given the extensive information compiled over the last 30 years including the histopathologic data provided by this study, it can be said with a high degree of certainty that dense deposit disease is not a subtype of membranoproliferative glomerulonephritis.
References
Appel GB, Cook HT, Hageman G, et al. Membranoproliferative glomerulonephritis type II (dense deposit disease): an update. J Am Soc Nephrol 2005;16:1392–1404.
Rennke HG . Secondary membranoproliferative glomerulonephritis. Kidney Int 1995;47:643–656.
Zhou XJ, Silva FG . Membranoproliferative Glomerulonephritis. In: Jennette JC, Olson JL, Schwartz MM, Silva FG (eds). Heptinstall's Pathology of the Kidney. Lippincott Williams & Wilkins: Philadelphia, 2007, pp 253–319.
Galle P . Mise en évidence au microscope électronique d'une lésion singulière des membranes basales du rein et de la substance hyaline. Thesis Med, Paris, 1962.
Galle P, Mahieu P . Electron dense alteration of kidney basement membranes: a renal lesion specific of a systemic disease. Am J Med 1975;58:749–764.
Habib R, Gubler M, Loirat C, et al. Dense deposit disease: a variant of membranoproliferative glomerulonephritis. Kidney Int 1975;7:204–215.
Lamb V, Tisher CC, McCoy RC, et al. Membranoproliferative glomerulonephritis with dense intramembranous alterations. Lab Invest 1977;36:607–617.
Davis AE, Schneeberger EE, Grupe WE, et al. Membranoproliferative glomerulonephritis (MPGN type I) and dense deposit disease (DDD) in children. Clin Nephrol 1978;9:184–193.
Churg J, Duffy JL, Bernstein J . Identification of dense deposit disease. Arch Pathol Lab Med 1979;103:67–72.
Kim Y, Vernier RL, Fish AJ, et al. Immunofluorescence studies of dense deposit disease: the presence of railroad tracks and mesangial rings. Lab Invest 1979;40:474–480.
Cameron JS, Turner DR, Heaton J, et al. Idiopathic mesangiocapillary glomerulonephritis: comparison of types I and II in children and adults and long-term prognosis. Am J Med 1983;74:175–192.
Klein M, Poucell S, Arbus GS, et al. Characteristics of a benign subtype of dense deposit disease: comparison with the progressive form of this disease. Clin Nephrol 1983;20:163–171.
Dense deposit disease in children: prognostic value of clinical and pathologic indicators. A report of the Southwest Pediatric Nephrology Study Group. Am J Kid Dis 1985;6:161–169.
Muda AO, Barsotti P, Marinozzi V . Ultrastructural histochemical investigations of ‘dense deposit disease’. Pathogenetic approach to a special type of mesangiocapillary glomerulonephritis. Virchows Arch 1988;413:529–537.
Bennett WM, Fassett RG, Walker RG, et al. Mesangiocapillary glomerulonephritis type II (dense deposit disease): clinical features of a progressive disease. Am J Kid Dis 1989;13:469–476.
Kashtan CE, Burke B, Burch G, et al. Dense intramembranous deposit disease: a clinical comparison of histological subtypes. Clin Nephrol 1990;33:1–6.
Joh K, Aizawa S, Matsuyama N, et al. Morphologic variations of dense deposit disease: light and electron microscopic, immunohistochemical and clinical findings in 10 patients. Acta Pathol Japon 1993;43:552–565.
Ikeda M, Honda M, Hasegawa O . Another example of spontaneous improvement in a case of dense deposit disease. Pediatr Nephrol 2000;16:609–610.
Marks SD, Rees L . Spontaneous clinical improvement in dense deposit disease. Pediatr Nephrol 2000;14:322–324.
West CD, McAdams AJ, Witte DP . Acute non-proliferative glomerulitis: a cause of renal failure unique to children. Pediatr Nephrol 2000;14:786–793.
Hoschek JC, Dreyer P, Dahal S, et al. Rapidly progressive renal failure in childhood. Am J Kid Dis 2002;40:1342–1347.
Sibley RK, Kim Y . Dense intramembranous deposit disease: new pathologic features. Kidney Int 1984;25:660–670.
Kher KK, Makker SP, Aikawa M, et al. Regression of dense deposits in type II membranoproliferative glomerulonephritis: case report of clinical course in a child. Clin Nephrol 1982;17:100–103.
Campbell-Boswell MV, Linder D, Naylor BR, et al. Kidney tubule basement membrane alterations in type II membranoproliferative glomerulonephritis. Virchows Arch 1979;382:49–61.
A clinico-pathologic study of crescentic glomerulonephritis in 50 children. A report of the Southwest Pediatric Nephrology Study Group. Kidney Int 1985;27:450–458.
Miller MN, Baumal R, Poucell S, et al. Incidence and prognostic importance of glomerular crescents in renal diseases of childhood. Am J Nephrol 1984;4:244–247.
Neild GH, Cameron JS, Ogg SS, et al. Rapidly progressive glomerulonephritis with extensive glomerular crescent formation. Quart J Med 1983;52:395–416.
Sethi S, Sahani M, Oei LS, et al. Crescentic glomerulonephritis and dense deposit disease in a woman with breast carcinoma on immunosuppressive chemotherapy. Am J Kid Dis 2004;44:E33–E37.
Vargas R, Thompson KJ, Wilson D, et al. Mesangiocapillary glomerulonephritis with dense ‘deposits’ in the basement membranes of the kidney. Clin Nephrol 1976;5:73–82.
Droz D, Zanetti M, Laure-Hélène N, et al. Dense deposits disease. Nephron 1977;19:1–11.
Nakopoulou L . Membranoproliferative glomerulonephritis. Nephrol Dial Transplant 2001;16S:71–73.
Foucar E . Classification in anatomic pathology. Am J Clin Pathol 2001;116 (Suppl 1):S5–S20.
Acknowledgements
This study was supported by a grant from the Kidneeds Foundation (Iowa City, IA). We thank the members of the Renal Pathology Society for their input and encouragement.
The following physicians kindly submitted their renal biopsy materials for review: North America: Stephen M Bonsib, MD, Indianapolis, IN, USA; Andrey V Cybulsky, MD, Montreal, Quebec, Canada; Helen Liapis, MD, St Louis, MO, USA; Neriman Gokden, MD, Little Rock, AR, USA; Regina R Verani, MD, Houston, TX, USA; Patrick D Walker, MD, Little Rock, AR, USA. Europe: Franco Ferrario, MD, Milan, Italy; Marisa Giani, MD, Milan, Italy; Laura Furci, MD, Modena, Italy; Giovanni Frascà, MD, Bologna, Italy; Maurizio Manganaro, MD, Torino, Italy; Giacomo Garibotto, MD, Genova, Italy; Leonardo Cagnoli, MD, Rimini, Italy; Alexei Sukhanov, MD, Moskow, Russia. Japan: Kensuke Joh, MD, Chiba City, Japan.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Walker, P., Ferrario, F., Joh, K. et al. Dense deposit disease is not a membranoproliferative glomerulonephritis. Mod Pathol 20, 605–616 (2007). https://doi.org/10.1038/modpathol.3800773
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/modpathol.3800773
Keywords
This article is cited by
-
Komplementvermittelte seltene Glomerulonephritis(GN)-Formen
Die Nephrologie (2023)
-
A clinical approach to children with C3 glomerulopathy
Pediatric Nephrology (2022)
-
Immunglobulin- und komplementvermittelte glomeruläre Erkrankungen mit MPGN-Muster
Der Nephrologe (2020)
-
Dominant C3 glomerulopathy: new roles for an old actor in renal pathology
Journal of Nephrology (2018)
-
C3 glomerulopathy and current dilemmas
Clinical and Experimental Nephrology (2017)