Abstract
Telomerase activity was examined by the telomeric repeat amplification protocol assay in 25 cases of lung adenocarcinoma, in relation to cancer cell differentiation, proliferation, and chromosome alterations. Telomerase activity, chromosome alterations, and cell proliferation assessed by Ki-67 labeling were significantly lower (P < .001 to .05) in well-differentiated (10 cases) than in moderately differentiated (8 cases) or poorly differentiated (7 cases) lesions. Telomerase activity by semiquantitative analysis with scoring of 0 to 3 was significantly correlated with similarly graded chromosome alterations (P < .05) and Ki-67 labeling indices (P < .002). Telomerase activity and chromosome alteration (T-C) indices generated by multiplication of telomerase activity and chromosome alteration scores also showed a significant correlation with cell differentiation. The Clara cell subtype, confirmed by electron microscopic analysis, significantly predominated in the well-differentiated group, showing a low grade of telomerase activity and chromosome alterations and low Ki-67 labeling indices, suggesting clinical relevance. No significant association of telomerase activity was found with p53 protein accumulation or Bcl-2 protein expression. The good correlation of telomerase activity with chromosome alterations, cell differentiation, and Ki-67 labeling indices suggests that this parameter might have potential application in estimation of prognosis.
Similar content being viewed by others
INTRODUCTION
The activity of telomerase, an enzyme that contributes to immortality of cells by allowing continued cell proliferation, has been shown to be increased in carcinomas of various sites, including the prostate (1), lung (2), stomach (3), colorectum (4, 5), liver (6), pancreas (7), brain (8, 9), breast (10, 11), hematopoietic system (12), and thyroid (13, 14). Regarding human colorectal tumors, this is reported to be associated with acquisition of malignant potential (4). However, our recent data on changes that occur in thyroid and colorectal tumors suggest that telomerase activity is not a critical marker for cancer development, although it has a strong correlation with tumor differentiation and progression and tumor cell proliferation (5, 14). The present study was conducted to ascertain whether telomerase activity is linked to chromosome alterations, cell differentiation, proliferation, and tumor staging in lung adenocarcinomas. A comparison of clinicopathologic features and the level of cell proliferation, assessed by Ki-67 immunohistochemistry, was therefore performed. Furthermore, because precursor cells of lung adenocarcinomas are heterogeneous, ultrastructural subtypes confirmed by electron microscopic observation were also compared for these markers.
MATERIALS AND METHODS
Patients and Histologic Diagnosis
Fresh-frozen tumor and nontumor regions were stored in all cases of lung adenocarcinomas in the Japanese Red Cross Medical Center, if good-sized tissues were available, after getting histopathologic diagnosis at surgical operation. Simultaneously, chromosome alteration and electron microscopic analyses were performed. In the present study, a total of 25 cases of surgically resected lung adenocarcinomas were randomly selected from the records in which fresh-frozen tissues for telomerase activity test were available and cytogenetic and ultramicroscopic analyses were also successful. Histologic observations were performed on hematoxylin and eosin–stained 4-μm-thick sections of 10% buffered formalin-fixed and paraffin-embedded tissues. Adenocarcinomas were divided into well-, moderately, and poorly differentiated subtypes on the basis of histologic features according to the World Health Organization classification (15). The tumor staging was performed based on the TNM classification (15).
Electron Microscopic Analysis
Fresh cancer tissues were fixed with 2.5% glutaraldehyde for 2 h at 4° C and postfixed with 1% osmium tetroxide for 1 h. The samples were then dehydrated in graded ethanols up to 100% and embedded in a gelatin capsule of fresh epoxy resin. After polymerization, ultrathin sections were cut and stained with 3.5% uranyl acetate and Reynolds’ lead citrate and examined with a transmission electron microscope (JEM 2000; Nippondenshi, Tokyo, Japan). According to ultrastructural features (16), adenocarcinomas were classified as being of Clara cell type (more than 95%, peg-shaped cells or low columnar epithelial cells having many dense secretory granules and rough endoplasmic reticulum in their cytoplasm), fuzzy Clara cell type (predominantly Clara cells having several dense secretory granules, partially including bronchial surface or type II alveolar epithelial cells), bronchial surface cell type (tall columnar cells, cytoplasm rich in mitochondria and smooth-surfaced vesicles but devoid of secretory granules), type II alveolar epithelial cell type (many osmiophilic lamellar bodies in the cytoplasm) or mixed cell type (two or more types of cells).
Immunohistochemistry
Immunohistochemistry for Ki-67 labeling, p53 accumulation, and Bcl-2 expression was performed by a combination of the ordinary streptavidin-biotin peroxidase complex method (Histofine SAB-PO [M and R] kit; Nichirei Co., Tokyo, Japan) and microwave oven heating. Briefly, after deparaffinization, histologic slides bearing 4-μm-thick sections were heated in 10 mm citrate buffer (pH 6.0) for three 5-min cycles using a microwave oven and then incubated overnight at 4° C with optimum dilutions of primary antibodies: rabbit antihuman Ki-67 (150 × dilution; DAKO, Copenhagen, Denmark), Do-7 monoclonal for p53 protein (500 × dilution; Novocastra Laboratories, Newcastle, UK), and antihuman Bcl-2 monoclonal antibody (100 × dilution; DAKO). As positive controls, infiltrating lymphocytes were applied for Bcl-2 and a p53-positive esophageal carcinoma for p53. Ki-67 labeling indices (LI) were calculated as percentage values by counting more than 1000 nuclei of cancer cells. Immunopositivity for Bcl-2 was defined as negative (0), weak (1+), moderate (2+), or strong (3+), in comparison with the positive controls, regarded as strong. On the basis of the percentages of Bcl-2–positive cells in the tumors, the lesions were subdivided into four categories according to scoring method of Sinicrope et al. (17) as follows: negative, no or fewer than 5% positive cells; 1+, more than 5% but fewer than 30% positive cells; 2+, more than 30% but fewer than 50% positive cells; 3+, more than 50% positive cells. Immunoreactive scores for Bcl-2 indices were calculated by multiplication of the values for the two parameters. Positivity for p53 protein in cancer cells was defined as diffuse (>30%), focal (6 to 30%), or negative (0 to 5%) according to the previously reported method (18).
Telomerase Assay
Fresh tumor and nontumor tissues were immediately frozen in dry ice isopentane and stored at −80° C until subjected to the telomeric repeat amplification protocol (TRAP) assay, as described by Kim et al. (1) and Wright et al. (19). Briefly, lysates were prepared by powdering tissues frozen in liquid nitrogen, followed by homogenization in 200 μ/L ice-cold lysis buffer (10 mm Tris-HCl [pH 7.5], 1 mm MgCl2, 1 mm EGTA, 0.1 mm phenylmethylsulfonyl fluoride, 5 mm β-mercaptoethanol, 0.5% CHAPS-10% glycerol) and incubation for 30 min on ice. The lysates were then centrifuged at 10,000 g for 20 min at 4° C, and the supernatants and precipitates were rapidly frozen separately and stored at −80° C. The protein concentration of each supernatant was determined by the Bradford assay (Bio-Rad, Hercules, CA).
Assay tubes were prepared by sequestering 0.1 μg CX primer (5′-CCCTTACCCTTACCCTTACCCTAA-3′) under a wax barrier (Ampliwax; Perkin-Elmer Cetus, Foster City, CA). Supernatant samples equivalent to 6 μg protein were assayed in 50 μL reaction mixture (20 mm Tris-HCl [pH 8.3], 1.5 mm MgCl2, 63 mm KCl, 0.005% Tween 20, 1 mm EGTA, 50 μm dNTPs, 150 kBq[α-32P]dCTP, 0.1 μg TS primer [5′-AATCCGTCGAGCAGAGTT-3′], 1 μg T4gene32 protein [Boehringer Mannheim, Mannheim, Germany], and 2 units of Taq DNA polymerase [GIBCO-BRL, Gaithersburg, MD]). After a 30-min incubation at 23° C for telomerase-mediated extension of the TS primer, the reaction mixture was heated at 90° C for 90 seconds and then subjected to 31 polymerase chain reaction cycles of 94° C for 30 seconds, 50° C for 30 seconds, and 72° C for 45 seconds. The polymerase chain reaction products were then electrophoresed on 10% polyacrylamide gels.
Extracts from 103, 102, and 101 SiHa cells were applied with controls (internal telomerase standard [ITAS]) in every TRAP assay. The intensity of individual electrophoresed bands was measured with computer assistance using NIH Image version 1.58 software. To evaluate relative activity, values were compared with that for ITAS in each case and then semiquantitatively scored as 3, 2, and 1, respectively. Negative telomerase activity was scored as 0.
Analysis of Chromosome Alterations
Fresh tumor samples were examined with the method described elsewhere (20). Briefly, after fine mincing without collagenase in a petri dish covered with 3 to 5 mL RPMI 1640 medium, disaggregated cells were cultured in RPMI 1640 medium supplemented with 10% fetal bovine serum plus antibiotics and antimycotics for 1 to 30 days. Metaphase cells arrested by exposure overnight to Colcemid (0.01 mg/mL) were treated with 0.075 m KCl hypotonic solution for 30 min at 37° C and then fixed in a 3:1 mixture of methanol:acetic acid. Chromosomes were analyzed using Q-band technique. Chromosome identification and karyotype designations were performed in accordance with the International System for Human Cytogenetic Nomenclature (21). After 10 or more metaphase cells were analyzed, chromosome alterations were classified and scored as follows: high-grade alteration, score 3 (>15 structure abnormalities, including marker chromosomes); medium-grade, score 2 (6–15 abnormalities); low-grade, score 1 (1–5 abnormalities); no abnormalities, score 0.
T-C indices were calculated by multiplication of telomerase activity and chromosome alteration scores as an indirect marker of DNA abnormalities.
Statistical Analysis
Differences in telomerase activity, chromosome alteration scores, T-C indices, Ki-67 LI, and tumor staging between groups were statistically analyzed by the χ2 test and the nonparametric Mann-Whitney U test, respectively. Multivariate analysis was performed with PSS logistic regression. Statistical significance was concluded with P values less than 0.05.
RESULTS
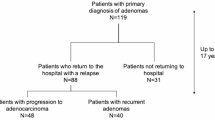
Results of the clinicopathologic comparison of lung adenocarcinomas for the various analytical categories are summarized in Table 1. No significant differences were observed with regard to age, although male cases significantly predominated for the poorly differentiated as compared to the well-differentiated type (P < .05). No significant associations were found between tumor differentiation and stage (P = .2481 between well- and moderately and P = .0971 between well- and poorly differentiated adenocarcinomas, by comparisons of numerical values of each stage between two groups) or tumor sizes. Stage 1 lesions were significantly (P = .0484) smaller than the others (2.8 ± 0.9±4.3 ± 1.7 cm). In the well-differentiated group, the Clara cell type significantly predominated, compared with moderately or poorly differentiated groups, respectively (P < .05, .01).
Telomerase activity was detected in 22 of 25 lung adenocarcinomas (92%) (Table 1, Fig. 1) but was negative in all paired samples of non-neoplastic lung tissue. Telomerase activity scores were 1.0 ± 0.8 (mean ± SD) in well-differentiated, 2.0 ± 0.8 in moderately differentiated, and 2.4 ± 0.5 in poorly differentiated types, respectively, the difference being significant between well- and moderately or poorly differentiated types (P = .0330, .0047; Table 1). Telomerase activity was 1.3 ± 0.9 in Stage 1 (n = 12) and 2.1 ± 0.9 in more advanced stages (n = 13), respectively (not significant).
Telomerase activity in lung adenocarcinomas by the telomeric repeat amplification protocol assay. Extracts from SiHa cells (as a positive control) were analyzed as an internal telomerase standard. Lane 1, 103 SiHa cells with positive telomerase activity; lane 2, lysis buffer (as negative control); lanes 3 and 4, lung adenocarcinoma (T; poorly differentiated type) and noncancer lung tissue (N) from Case 23; lanes 5 and 6, lung adenocarcinoma (T; moderately differentiated type) and noncancer lung tissue (N) from Case 18; lanes 7 and 8, lung adenocarcinoma (T; well-differentiated type) and noncancer lung tissue (N) from Case 8. According to the relative intensity to internal telomerase standard, the telomerase activity was scored as 3, 2, and 1 in lanes 3, 5, and 7, respectively.
Chromosome alterations were detected in 21 of 25 adenocarcinomas (Fig. 2), with scores of 1.0 ± 1.1 in well-differentiated, 2.3 ± 0.9 in moderately differentiated, and 2.1 ± 0.9 in poorly differentiated types, respectively. Significant differences were evident between well- and moderately or poorly differentiated types (P = .0368, .0248; Table 1).
Chromosome alterations in a lung adenocarcinoma (Case 21). The chromosome alteration score was 3 as follows: The modal chromosome number was 80. 73∼81 less than 4n more than, XX, −Y, −Y, −1, −1, add(2)(q37 × 2, +5, add(5)(q31 × 3, del(6)(q25 × 2, der(6)t(6;9)(q13;q12) × 2, +7, +7, −9, −9, −12, −13, −13, del(13)(q32q33 × 2, −14, −14, add(15)(p13 × 2, add(15)(q26 × 2, −17, −17, −19, −20, add(21)(p13 × 2, −22, −22, −22, −22, +mar1x2, +mar2x2, +mar3, +0∼3mar [cp10]
T-C indices were 1.0 ± 1.2 for well-differentiated, 4.6 ± 2.6 for moderately differentiated, and 5.1 ± 2.3 for poorly differentiated types, with significant differences between well- and moderately or poorly differentiated types (P = .0039, .0018; Table 1).
Ki-67 LI were 9.1 ± 5.5% for well-differentiated, 22.4 ± 6.5% for moderately differentiated, and 43.8 ± 18.1% for poorly differentiated types, with the differences being significant between well- and moderately or poorly differentiated types (P = .0019, .0006; Figs. 3 and 4).
p53 indices were 1.3 ± 1.2 for well-differentiated, 2.6 ± 0.7 for moderately differentiated, and 1.6 ± 1.3 for poorly differentiated types, respectively, the differences not being significant. Bcl-2 indices were 1.9 ± 2.1 for well-differentiated, 1.1 ± 1.6 for moderately differentiated, and 0.7 ± 1.5 for poorly differentiated types, respectively. Although not reaching significance, indices were decreased in the sequence leading from well-to poorly differentiated types.
A significant correlation between telomerase activity scores and Ki-67 LI was found in adenocarcinomas (Y = 3.889 + 11.169X, r = .592, P = .0018; Fig. 5), as well as chromosome alteration scores (Y = .852 + .551X, r = .462, P = .0202; Fig. 6). No link was apparent between chromosome alteration scores and Ki-67 LI (data not shown).
Clara cell type adenocarcinomas (n = 7; Fig. 7) showed significantly lower telomerase activity (0.9 ± 0.9/2.1 ± 0.7, P = .0110), chromosome alterations (0.7 ± 0.8/2.1 ± 1.0; P = .0065), T-C indices (0.7 ± 1.0/4.3 ± 2.6; P = .0015), and Ki-67 LI (7.8 ± 5.3/29.1 ± 17.2; P = .0011), compared with other types (n = 18).
Electron microscopic features of a Clara cell type (A) (Case 6) and a mixed type adenocarcinoma (B) (Case 5). A, peg-shaped or low columnar epithelial cells have many dense secretory granules and rough endoplasmic reticulum in their cytoplasm. B, carcinoma tissue comprises type II alveolar epithelial cells containing lamellar bodies in the cytoplasm (arrowheads) and Clara cells having dense secretory granules (small arrows) (double staining with uranium acetate and lead citrate; original magnification, × 2500).
Multivariate analysis revealed significant differences between scores for chromosome alterations and telomerase activity (P = .0331), chromosome alterations and p53 scores (P = .0352), cell differentiation and T-C indices (P = .0251), cell differentiation and Ki-67 LI (P = .0151), and stage and tumor size (P = .0484).
DISCUSSION
Recent work on telomerase activity in germline cells and cancers has demonstrated that this enzyme, thought to be involved in maintaining telomere length and stability, is associated with immortalization and continuous growth of cells (4, 22). Furthermore, increased telomerase activity has been found in most, if not all, types of cancers. In the present study, telomerase activity by the standard TRAP assay was positive in 22 of 25 (88%) lung adenocarcinoma cases, in line with previous reports (84 of 99 [84.8%] non–small cell lung cancers by Albanell et al. (23) and 45 of 65 [69.2%] lung adenocarcinoma cases by Hiyama et al. (2)). Telomerase expression with our scoring system was not found to be linked to cancer cell progression, although in the report of Albanell et al. (22), significantly higher scores were observed for nodal metastasis than in nonmetastatic cases. In the present study, the difference between Stage 1 and more advanced stage did not reach significance, possibly because of the small number of cases. However, our findings for telomerase activity of lung adenocarcinomas pointed for the first time to a significant relation with tumor cell differentiation, as observed for thyroid tumors (14) and colorectal carcinomas (5).
The positive association between telomerase activity and cancer cell proliferation as assessed by the Ki-67 labeling (24) found here is in line with data for non–small cell lung cancers (23), breast cancers (8), thyroid tumors (14), and colorectal carcinomas (5). Furthermore, normal human lymphocytes and hematopoietic progenitor cells strongly express telomerase after mitogenic stimulation (25, 26). It was also recently shown (27) that the endometrium in the proliferative phase expresses telomerase activity, similarly suggesting a link with cellular proliferation and dedifferentiation.
The grading score of telomerase activity showed a significant correlation with chromosome alterations that also have an intimate relation with tumor progression (28, 29, 30). This fact suggests that the acquisition and increase of telomerase activity correlate well with genetic alterations in lung tumorigenesis that might be responsible for allowing continued proliferation. Accordingly, T-C indices generated by multiplication of the two scores might be a good parameter for prognostic estimation, although assessment of the clinical outcome was not possible, because most of the cases examined in the present work were obtained in 1995–1997.
In the present work, Clara cell type carcinomas showed significantly lower scores for telomerase activity, chromosome alterations, and T-C indices than other types of carcinomas, suggesting that they constitute a relatively benign entity.
Although an inverse correlation between p53 and Bcl-2 expression during progression of colorectal carcinomas has been reported (17), there was no significant correlation with telomerase activity scores in our lung adenocarcinoma series. Although this indicates a lack of any intimate relationship with regulation of the cell cycle, this point remains to be clarified, for example by p53 gene mutation analysis.
In conclusion, the present data for lung adenocarcinomas point to a special relationship among telomerase activity and chromosome alterations, tumor cell differentiation, and proliferation.
References
Kim NW, Piatyszek MA, Prowse KR, Harley CB, West MD, Ho PL, et al. Specific association of human telomerase activity with immortal cells and cancer. Science 1994; 266: 2011–2015.
Hiyama K, Hiyama E, Ishioka S, Ymakido M, Inai K, Gazdar AF, et al. Telomerase activity in small-cell and non-small-cell lung cancers. J Natl Cancer Inst 1995; 87: 895–902.
Hiyama E, Yokoyama T, Tatsumoto N, Hiyama K, Imamura Y, Murakami Y, et al. Telomerase activity in gastric cancer. Cancer Res 1995; 55: 3258–3262.
Chadeneau C, Hay K, Hirte HW, Gallinger S, Bacchetti S . Telomerase activity associated with acquisition of malignancy in human colorectal cancer. Cancer Res 1995; 55: 2533–2536.
Okayasu I, Mitomi H, Yamashita K, Mikami T, Fujiwara M, Kato M, et al. Telomerase activity significantly correlates with cell differentiation, proliferation and lymph node metastasis in colorectal carcinomas. J Cancer Res Clin Oncol 1998; 124: 444–449.
Tahara H, Nakanishi T, Kitamoto M, Nakashio R, Shay JW, Tahara E, et al. Telomerase activity in human liver tissue: comparison with chronic liver disease and hepatocellular carcinomas. Cancer Res 1995; 55: 2734–2736.
Hiyama E, Kodama T, Shinbara K, Iwao T, Itoh M, Hiyama K, et al. Telomerase activity is detected in pancreatic cancer but not in benign tumors. Cancer Res 1997; 57: 326–331.
Langford LA, Piatyszek MA, Xu R, Schold SC Jr, Shay JW . Telomerase activity in human brain tumours. Lancet 1995; 346: 1267–1268.
Langford LA, Piatyszek MA, Xu R, Schold SC, Wright WE, Shay JW . Telomerase activity in ordinary meningiomas predicts poor outcome. Hum Pathol 1997; 228: 416–420.
Hiyama E, Gollahon L, Kataoka T, Kuroi K, Yokoyama T, Gazdar AF, et al. Telomerase activity in human breast tumors. J Natl Cancer Inst 1996; 88: 116–122.
Landberg G, Nielsen NH, Nilsson P, Emdin SO, Cajander J, Roos G . Telomerase activity is associated with cell cycle deregulation in human breast cancer. Cancer Res 1997; 57: 549–554.
Counter CM, Gupta J, Harley CB, Leber B, Bacchetti S . Telomerase activity in normal leukocytes and in haematology malignancies. Blood 1995; 85: 2315–2320.
Umbricht CB, Saji M, Westra WH, Udelsman R, Zeiger MA, Sukumar S . Telomerase activity: a marker to distinguish follicular thyroid adenoma from carcinoma. Cancer Res 1997; 57: 2144–2147.
Okayasu I, Osakabe T, Fujiwara M, Fukuda H, Kato M, Oshimura M . Significant correlation of telomerase activity in thyroid papillary carcinomas with cell differentiation, proliferation and extrathyroidal extension. Jpn J Cancer Res 1997; 88: 965–970.
Kobayashi Y . Histology classification. In: The Japan Lung Cancer Association, editor. General rule for clinical and pathological record of lung cancer. 5th ed. Tokyo, Japan: Kanehara Shuppan Co; 1999. p. 92–106.
Taccagni G, Dell’Antonio G, Terreni MR, Cantaboni A . Heterogeneous subcellular morphology of lung adenocarcinoma cells: identification of different cytotypes on cytological material. Ultrastruct Pathol 1990; 14: 65–80.
Sinicrope FA, Ruan SB, Cleary KR, Stephens LC, Lee JJ, Levin B . bcl-2 and p53 oncoprotein expression during colorectal tumorigenesis. Cancer Res 1995; 55: 237–241.
Saegusa M, Takano Y, Kamata Y, Okayasu I . Bcl-2 expression and allelic loss of the p53 gene in gastric carcinomas. J Cancer Res Clin Oncol 1996; 122: 427–432.
Wright WE, Shay JW, Piatyszek MA . Modifications of a telomoric repeat amplification protocol (TRAP) result in increased reliability, linearity and sensitivity. Nucleic Acids Res 1995; 23: 3794–3795.
Miura I, Siegfried JM, Resau J, Keller SM, Zhou JY, Testa JR . Chromosome alterations in 21 non-small cell lung carcinomas. Genes Chromosomes Cancer 1990; 2: 328–338.
Hamden DG, Klinger HP, editors. ISCN, an international system for human cytogenetic nomenclature. Basel: S. Karger Co; 1985.
Rhyu MS . Telomeres, telomerase, and immortality. J Natl Cancer Inst 1995; 87: 884–894.
Albanell J, Lonardo F, Rusch V, Engelhardt M, Langenfeld J, Han W, et al. High telomerase activity in primary lung cancers: association with increased cell proliferation rates and advanced pathologic stage. J Natl Cancer Inst 1997; 89: 1609–1615.
Gerdes J, Lemke H, Baisch H, Wacke HH, Schwabb U, Stein H . Cell cycle analysis of a cell proliferation-associated human nuclear antigen defined by the monoclonal antibody Ki-67. J Immunol 1984; 133: 1710–1715.
Broccoli D, Young JW, DeLange T . Telomerase activity in normal and malignant hematopoietic cells. Proc Natl Acad Sci U S A 1995; 92: 9082–9086.
Hiyama K, Hirai Y, Kyoizumi S, Akiyama M, Hiyama E, Piatyszek MA, et al. Activation of telomerase in human lymphocytes and hematopoietic progenitor cells. J Immunol 1995; 155: 3711–3715.
Kyo S, Takakura M, Kohama T, Inoue M . Telomerase activity in human endometrium. Cancer Res 1997; 57: 610–614.
Endo C, Sagawa M, Sato M, Chen Y, Sakurada A, Aikawa H, et al. Sequential loss of heterozygosity in the progression of squamous cell carcinoma of the lung. Br J Cancer 1998; 78: 612–615.
Al-Mulla F, Keith WN, Pickford IR, Going JJ, Birnie GD . Comparative genomic hybridization analysis of primary colorectal carcinomas and their synchronous metastases. Genes Chromosomes Cancer 1999; 24: 306–314.
Ried T, Heselmeyer-Haddad K, Blegen H, Schrock E, Auer G . Genomic changes defining the genesis, progression, and malignancy potential in solid human tumors: a phenotype/genotype correlation. Genes Chromosomes Cancer 1999; 25: 195–204.
Acknowledgements
We thank Ms. Y. Numata and K. Hana for their expert technical assistance, Ms. T. Hiraide for her support in the preparation of the manuscript, and Dr. M. Sada for her assistance with the statistical analysis.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Fujiwara, M., Okayasu, I., Takemura, T. et al. Telomerase Activity Significantly Correlates with Chromosome Alterations, Cell Differentiation, and Proliferation in Lung Adenocarcinomas. Mod Pathol 13, 723–729 (2000). https://doi.org/10.1038/modpathol.3880125
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/modpathol.3880125
Keywords
This article is cited by
-
Differential expression of telomerase reverse transcriptase (hTERT) in lung tumours
British Journal of Cancer (2004)