Abstract
Polymorphonuclear leukocyte (PMN) infiltration is a cardinal feature of peritonitis. CXC chemokine ligands 1 and 8 (CXCL1 and CXCL8), and the cytokine granulocyte colony-stimulating factor (G-CSF) are the key mediators of PMN accumulation. Increasing evidence points to an important role of human peritoneal fibroblasts (HPFB) in the response of the peritoneum to infection. We have examined the synthesis of PMN-targeting cytokines by HPFB exposed to intraperitoneal milieu as represented by peritoneal dialysate effluent (PDE) from patients undergoing peritoneal dialysis. PDE obtained during peritonitis, but not during infection-free periods, significantly increased production of CXCL1, CXCL8, and G-CSF by HPFB. The effect was largely blocked by antibodies to interleukin-1β (IL-1β), whereas neutralization of tumor necrosis factor-α (TNFα) had no major effect. Similar pattern of inhibition was observed when HPFB were exposed to conditioned media from endotoxin-stimulated peritoneal macrophages. Significance of IL-1β stimulation was further shown in experiments with recombinant cytokines. Compared with TNFα, exposure of HPFB to recombinant IL-1β resulted in a much higher release of PMN-targeting cytokines. The assessment of mRNA degradation revealed that the IL-1β-induced transcripts of CXCL1, CXCL8, and G-CSF were more stable compared with those induced by TNFα. These data indicate that HPFB can be a significant source of PMN-targeting cytokines when stimulated with IL-1β in the inflamed peritoneum.
Similar content being viewed by others
Main
Peritonitis occurs frequently in clinical practice. Its acute phase is characterized by a rapid influx of polymorphonuclear leukocytes (PMN) into the peritoneal cavity. PMN play a key role in host defense against infection. It is essential for the effective PMN bactericidal activity to occur that the PMN concentration in the tissue affected reaches a required level.1 The accumulation of PMN in tissues is a result of their recruitment from the blood and mobilization from the bone marrow. The processes are governed by specific PMN-targeting cytokines. They include chemokines of the CXC family (especially those bearing an ELR+ motif, eg CXC chemokine ligands 1 and 8 (CXCL1 and CXCL8)2 and the cytokine granulocyte colony-stimulating factor (G-CSF).3 Increased peritoneal expression of these mediators during acute peritonitis have been well documented in many clinical and experimental studies.4, 5, 6, 7, 8 Importantly, neutralization of CXC chemokines and of G-CSF in experimental models of peritonitis has been shown to reduce PMN accumulation in the inflamed peritoneum7, 9, 10, 11, 12, 13 CXC chemokines have been found to contribute to intraperitoneal PMN accumulation not only by producing chemotactic activity, but also by cooperating with G-CSF in PMN mobilization from the bone marrow.13
The cytokines that control the recruitment of PMN are generated locally at sites of inflammation. In the peritoneum, they are believed to derive largely from the mesothelium.14, 15, 16 Peritoneal mesothelial cells constitute the largest cell population in the peritoneal cavity and display a major biosynthetic potential for generating PMN-targeting cytokines.17, 18, 19 In contrast, the contribution of peritoneal fibroblasts to the inflammatory reaction is less understood.
Fibroblasts are believed to be involved predominantly in the synthesis and remodeling of extracellular matrix in tissues. However, there is a growing body of evidence that fibroblasts may also act as sentinel cells that have a significant impact on the course and resolution of inflammatory responses.20, 21 Fibroblast have been shown to secrete a broad array of inflammatory mediators, including cytokines, chemokines, and prostanoids.22 Moreover, the profile of immunoregulatory cytokines secreted by the fibroblasts has been found to differ significantly according to their tissue origin.23 This diversity is one of the aspects of marked heterogeneity observed among various fibroblasts subpopulations.24
In the normal peritoneum, fibroblasts are only sparsely distributed in the submesothelial stroma.25 However, increasing evidence suggests that their population may significantly increase as a result of peritoneal mesothelial cells undergoing epithelial-to-mesenchymal transition.26 Fibroblast-like cells thus formed have been implicated in the inflammatory response, angiogenesis, and fibrosis seen in the injured peritoneum.27 The injuries may be the result of either peritonitis or hemoperitoneum, and also of prolonged exposure to peritoneal dialysis fluids.28, 25 In severe cases, these situations may be associated with extensive losses of the mesothelium, which may further increase the significance of peritoneal fibroblasts as a source of inflammatory mediators. In this respect, we have shown earlier that human peritoneal fibroblasts (HPFB) are capable of synthesizing large quantities of various chemokines. In this study, we have focused on the synthesis of those HPFB-derived cytokines that specifically target PMN.
MATERIALS AND METHODS
Materials
Unless indicated otherwise, all chemicals were purchased from Sigma-Aldrich. Tissue culture media and fetal calf serum (FCS) were from Invitrogen. All other tissue culture reagents and buffers were from Biochrom AG. Tissue culture plastics were Falcon® from Becton Dickinson. Recombinant cytokines, anti-cytokine antibodies, and cytokine immunoassays were obtained from R&D Systems. All reagents were of tissue culture or molecular biology grade, as required. According to the manufacturers’ data, the endotoxin level in these materials was <0.1 ng/μg protein for cytokines and <0.1 ng/ml for media and buffers.
Culture of Peritoneal Fibroblasts
HPFB were isolated from omentum by trypsin digestion as described by Jörres et al29 and Beavis et al30 The specimens of apparently normal omentum were obtained from consenting patients undergoing elective abdominal surgery. The donors did not suffer from peritoneal pathologies such as peritoneal inflammation and/or malignant spreading. Cells were characterized and propagated as described in detail elsewhere.31 In addition, HPFB were stained with the TE-7 antibody, which has recently been postulated to specifically recognize fibroblasts.32 Before the experiments, cells were rendered quiescent by incubation in medium (Hams’ F12) with reduced FCS concentration (0.1%) for 48 h.29 Cells were treated as specified in the figure legends. After the exposure, the supernatants were collected, centrifuged to remove cellular debris, and stored at −80°C until assayed. The cells were detached and counted using the Neubauer chamber.
Immunocytochemistry
HPFB were seeded into the Lab-Tek™ Chamber Slides (Nunc), cultured in standard medium until ∼70% confluent, and then fixed with 3.7% buffered formaldehyde for 10 min. The specimens were washed with PBS, permeabilized with 1% Triton X-100 for 30 min, and blocked with 1% bovine serum albumin and 0.1% Tween 20 in PBS for 1 h. The mouse monoclonal TE-7 antibody (Chemicon/Millipore) that identifies fibroblasts32 was then applied at a concentration of 1.3 μg/ml for 30 min at room temperature. Isotype IgG1 (Chemicon/Millipore) at the same concentration was used as a negative control. After the specimens were washed with PBS, cells were treated with 0.3% H2O2 to quench endogenous peroxidase activity. Bound antibodies were detected by immunoperoxidase staining using the EnVision+ System (Dako) as per manufacturer's instructions.
Spent Peritoneal Dialysate
Peritoneal dialysate effluent (PDE) was obtained from consenting patients undergoing continuous ambulatory peritoneal dialysis (CAPD) for renal failure. PDE was collected from patients with and without peritonitis (Table 1). Peritonitis was diagnosed by the presence of at least two of the three following criteria: abdominal pain, cloudy dialysate effluent (which typically corresponds to the presence of more than 100 white blood cells/μl with the fraction of PMN >50%), and the isolation of microorganisms from the dialysate.33 PDE was collected on the day of presentation with peritonitis. The effluent was drained on ice, centrifuged, filtered through a 0.2 μm pore size filter, and stored in aliquots at −80°C, as described earlier.34 PDE was also obtained from patients (n=9) with no record of peritonitis and/or catheter exit site infection during 4 weeks before effluent collection.35 Equal volumes of PDE from these patients were pooled and processed as above.
Culture and Conditioned Medium from Peritoneal Macrophages
Human peritoneal macrophages (PM) were harvested from infection-free CAPD patients (n=4), as described earlier.36 Isolated cells were incubated in Hams's F12 medium (with 0.2% FCS) and stimulated with or without lipopolysaccharide (LPS, from E. coli O26:B5, 1 μg/ml) for 2 h at 37°C. After the exposure, PM were washed twice with medium and incubated in the absence of stimulation for the next 24 h. Conditioned media (PM-CM) were then collected, filtered, and stored in aliquots at −80°C.
Blocking Experiments
The ability of PDE and PM-CM to induce cytokine synthesis in HPFB was assessed in the presence of antibodies (R&D Systems) against IL-1β (AF-201-NA) and tumor necrosis factor-α (TNFα; AF-210-NA). PDE or PM-CM were pre-incubated with the antibodies (either alone or in combination) for 30 min at 37°C and then applied to HPFB cultures. Unspecific IgG of the same class (AB-108-C) was used as a control. Optimal neutralizing concentrations of the antibodies were determined by measuring their capacity to reduce IL-1β- and TNFα-driven IL-6 release from HPFB as described in the Results section.
Cytokine Measurements
Concentrations of cytokines and soluble cytokine receptors were measured using DuoSet Immunoassays (R&D Systems), according to manufacturer's instructions. Specific release of cytokines by HPFB exposed to PDE and PM-CM was calculated after subtracting background levels detected in these media from those recorded in post-culture supernatants.34 The results obtained were normalized per number of corresponding cells.
RNA Isolation and Analysis
Total RNA from HPFB cultures was extracted with the RNA Bee (Tel-Test) and purified according to the manufacturer's protocol. RNA (1μg) was reverse transcribed into cDNA with random hexamer primers, as described.37 Expression of target mRNAs was assessed by semi-quantitative PCR as summarized in Table 2. Primer sequences for human G-CSF mRNA were kindly provided by Stratagene. PCR products were separated by electrophoresis in ethidium bromide-stained 3% agarose gels and visualized under UV illumination.
The stability of target mRNAs was assessed by measuring the rate of mRNA degradation in the presence of the transcription inhibitor actinomycin D. Briefly, HPFB were stimulated with either IL-1β or TNFα (at 1 ng/ml) for 6 h at 37°C, then washed, and pulsed with actinomycin D (5 μg/ml). At defined times, after the addition of actinomycin D, the total RNA was extracted, reverse transcribed, and PCR amplified as described above.
Statistical Analysis
Data are presented as means±s.e.m. of the results obtained in independent experiments with cells from different donors. Statistical analyses were carried out using GraphPad Prism 4.00 software (GraphPad Software Inc.). The data were compared with repeated measures analysis of variance with Newman-Keuls modification. A P-value of <0.05 was considered significant.
RESULTS
PDE Concentrations of Inflammatory Cytokines
PDE from infection-free patients contained no or barely detectable amounts of CXCL1, CXCL8, and G-CSF (Table 1). In contrast, all these cytokines were significantly elevated in PDE from patients with CAPD-associated peritonitis. Although the absolute cytokine concentrations varied considerably, the magnitude of their increases was similar for individual patients. The highest levels of CXCL1, CXCL8, and G-CSF were detected in those effluents that also contained increased concentrations of potent proinflammatory cytokines, TNFα and IL-1β (Table 1).
HPFB Response to PDE
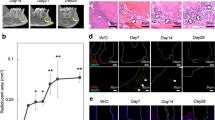
To determine whether HPFB could have contributed to the intraperitoneal presence of CXCL1, CXCL8, and G-CSF, HPFB were established in culture, exposed to PDE (50% v/v in medium), and the specific secretion of cytokines was measured. Identity of HPFB isolated was confirmed by staining with the TE-7 antibody (Figure 1). As illustrated in Figure 2a, the release of cytokines by these cells was maximum in response to those peritonitis effluents that themselves contained the highest concentrations of CXCL1, CXCL8, and G-CSF, and also the highest levels of TNFα and IL-1β. In addition, the exposure of HPFB to these effluents resulted in a clear induction of mRNAs for CXCL1, CXCL8, and G-CSF (Figure 2b). In contrast, HPFB exposed to effluents containing little or no TNFα and IL-1β secreted markedly less CXCL1, CXCL8, and G-CSF.
(a) Effect of peritoneal effluent on cytokine secretion by HPFB. PDE was drained from CAPD patients with peritonitis (Patient nos. 1–4, see Table 1 for details). In addition, PDE was obtained and pooled from nine infection-free patients (Stable). PDE was mixed (1:1) with culture medium and applied to HPFB for 48 h. The data were obtained from three experiments with HPFB isolated from different donors. (b) Effect of effluent from inflamed peritoneum on cytokine mRNA expression in HPFB. PDE was drained from patient no. 1 and 2 during acute phase of peritonitis. PDE was mixed (1:1 v/v) with culture medium and applied to HPFB cultures for 6 h. Expression of selected cytokines was assessed by RT-PCR. Results are representative of two separate experiments.
To test whether TNFα and IL-1β were responsible for the effects of PDE observed, blocking experiments were performed. First, to determine the neutralizing potential of the antibodies chosen, HPFB were stimulated with a fixed dose of recombinant IL-1β or TNFα in the presence of increasing concentrations of the antibodies. After 48 h, the supernatants were assayed for IL-6 that had earlier been shown to be readily stimulated by IL-1β and TNFα.29 These experiments showed that both antibodies at 1 μg/ml effectively blocked IL-1β and TNFα activity (Figure 3a). To determine precisely how much IL-1β and TNFα can be neutralized by that dose of antibodies, it was mixed with increasing doses of recombinant IL-1β and TNFα and added to HPFB cultures. Under such conditions, the antibodies could neutralize up to 3000 pg/ml of IL-1β and up to 10 000 pg/ml of TNFα (Figure 3b and c). These concentrations were well above those found in PDE; therefore, in subsequent blocking experiments both antibodies were used at 1 μg/ml.
Neutralizing capacity of the antibodies against IL-1β and TNFα. (a) HPFB were stimulated with either 50 pg/ml of IL-1β or 250 pg/ml of TNFα in the presence of increasing concentrations of antibodies, as indicated. (b and c) HPFB were treated with increasing doses of either IL-1β or TNFα administered in the presence or absence of 1 μg/ml of the relevant antibody. After 48 h cell supernatants were assessed for IL-6. Results of a representative experiment out of the two performed.
The addition of anti-IL-1β antibody to infected PDE significantly reduced its ability to stimulate the production of CXCL1, CXCL8, and G-CSF in HPFB (Figure 4). The degree of inhibition was 64±9%, 46±17%, and 80±10%, for CXCL1, CXCL8, and G-CSF, respectively. In contrast, antibodies to TNFα had no significant effect on the secretion of these cytokines and did not modulate the inhibitory effects of the IL-1β blockade further.
Effect of IL-1β and TNFα blockade on the ability of peritoneal effluent to induce cytokine secretion by HPFB. PDE was obtained during acute phase of peritonitis, mixed with an equal volume of control medium, and supplemented either with antibodies against IL-1β and TNFα or with control IgG (all at 1 μg/ml). Quiescent HPFB were then exposed to these fluids for 48 h and the specific release of cytokines was measured. The data were derived from six experiments performed with HPFB from three different donors and PDE was obtained from two patients (Patient nos. 1 and 2 from Table 1). The results were expressed as percentages of initial control values recorded in the absence of antibodies, which were 3512±388, 1428±314, and 425±152 pg/104 cells for CXCL1, CXCL8, and G-CSF, respectively. Asterisks represent significant differences compared with these control values.
HPFB Response to PM-Derived Products
As PM are thought to be a main source of IL-1β and TNFα in the inflamed peritoneum, we assessed the response of HPFB to media conditioned in the presence of PM. IL-1β and TNFα levels were 2±1 and 66±23 pg/ml in supernatants from unstimulated PM, and 435±200 and 9822±2839 pg/ml in supernatants from LPS-stimulated PM (n=4), respectively. Exposure of HPFB to CM from unstimulated PM increased the release of CXCL1 and CXCL8 only slightly, and did not induce G-CSF secretion (Figure 5a). In contrast, the exposure of HPFB to medium from LPS-stimulated PM led to massive induction of all cytokines investigated. The effect was clearly dose-dependent as it was reduced after serial dilutions of PM-CM. Furthermore, the capacity of CM from LPS-stimulated PM (diluted 1:20) to induce cytokines was significantly inhibited by antibodies to IL-1β and, to lesser extent, also to TNFα. (Figure 5b).
(a) Effect of peritoneal macrophage-conditioned medium on cytokine secretion by HPFB. The release of cytokines was measured after a 48-h exposure of HPFB to CM from either unstimulated peritoneal macrophages (PM) or from macrophages stimulated with LPS (LPS-PM). CM from the latter was serially diluted with control medium, as indicated. Data were derived from four experiments performed with cells from different donors. (b) Effect of IL-1β and TNFα blockade on the ability of PM-CM to induce cytokine secretion by HPFB. CM from LPS-stimulated PM was diluted 20-fold with control medium and supplemented either with antibodies against IL-1β and TNFα or with control IgG (all at 1 μg/ml). HPFB were exposed to the PM-CM for 48 h and the specific release of cytokines was measured. The data were derived from three experiments performed with HPFB from separate donors. The results were expressed as percentages of the control values recorded in the absence of antibodies, which were 10290±204, 4798±1229, and 1698±218 pg/104 cells for CXCL1, CXCL8, and G-CSF, respectively. Asterisk represents a significant difference compared with values detected in the absence of antibodies. Hash represents a significant difference compared with values detected in the presence of anti-IL-1β antibodies.
HPFB Response to Recombinant Cytokines
To further characterize the role of IL-1β and TNFα in HPFB responses to PDE and PM-CM, cells were treated with recombinant IL-1β and TNFα at doses up to 10 000 pg/ml. The experiments showed that both IL-1β and TNFα stimulated a dose- and time-dependent release of CXCL1, CXL8 and G-CSF from HPFB (Figure 6). Similar dose- and time effects were seen at the mRNA level (Figure 7). Interestingly, the effects induced by IL-1β were significantly more potent than those induced by TNFα. This pattern was observed only for PMN-targeting cytokines, as TNFα was capable of inducing other chemokines (eg CCL2 and CCL5) with the strength similar to or greater than that of IL-1β (data not shown).
Time- and dose-effect of recombinant IL-1β and TNFα on cytokine secretion by HPFB. (a–c) Cells were treated with increasing doses of either IL-1β (black bars) or TNFα (white bars) for 48 h. (d–f) Cells were treated with either control medium (black squares), IL-1β (1000 pg/ml, black circles), or TNFα (1000 pg/ml, white circles) for the times indicated. The post-culture supernatants were assayed for CXCL1 (a and d), CXCL8 (b and e), and G-CSF (c and f). Data were derived from 6–10 experiments with cells from different donors. Asterisks represent significant differences compared with the control at the same time point.
Time- and dose-effect of recombinant IL-1β and TNFα on cytokine mRNA expression by HPFB. (a) HPFB were treated with 1000 pg/ml of either IL-1β or TNFα for the times indicated. (b) HPFB were treated with either IL-1β or TNFα (at 1, 50, and 1000 pg/ml) for 3 h. Cytokine mRNA expression was analyzed by RT-PCR. Results are representative of three separate experiments.
Combining IL-1β with TNFα further increased secretion of cytokines investigated. The increases were additive for CXCL1 and CXCL8, and synergistic for G-CSF (Figure 8). When HPFB were exposed to 100 pg/ml of IL-1β together with 500 pg/ml of TNFα, the induction of G-CSF was more than twofold above the expected additive values.
Effect of a combination of IL-1β and TNFα on cytokine release by HPFB. Cells were exposed to control medium or IL-1β (at 1, 10, and 100 pg/ml) in the presence or absence of TNFα (at either 25 or 500 pg/ml). After a 48-h incubation, the supernatants were assayed for CXCL1 (panel a), CXCL8 (panel b), and G-CSF (panel c) by ELISA. Data were derived from four experiments with cells from different donors. Asterisks represent statistically significant differences compared with the calculated additive values.
Assessment of the Role of Soluble TNF Receptors
PDE from patients with peritonitis contained significant quantities of soluble TNF receptors (sTNF-RI/p55 and sTNF-RII/p75). As binding to these receptors might potentially inactivate bioactive TNFα, we treated HPFB with TNFα (at 1000 pg/ml) in the presence of recombinant soluble TNF receptors and assessed the release of CXCL8 (as a chemokine being relatively strongly induced by TNFα; see Figure 6b). These experiments revealed that soluble TNF receptors at doses as high as 200 ng/ml (ie >30–100-fold higher than concentrations found in PDE) did not diminish the effect of TNFα (Figure 9a). Next we tested whether TNF receptors could be shed from HBFB in response to IL-1β and TNFα. HPFB released very low levels of sTNF-RI constitutively, and IL-1β slightly enhanced the release in a dose-dependent manner (Figure 9b). In contrast, TNFα did not significantly affect the release of sTNF-RI from HPFB. The levels of sTNF-RII in HPFB cultures were barely detectable and were neither modified by IL-1β nor by TNFα (data not shown).
(a) Effect of soluble TNF receptors on TNFα-induced CXCL8 production by HPFB. Cells were stimulated with TNFα (1000 pg/ml) in the presence of increasing doses of either sTNF-RI or sTNF-RII. The release of CXCL8 was assessed after 48 h. (b) Effect of IL-1β and TNFα on TNF-RI release by HPFB. Cells were treated with increasing doses of either IL-1β or TNFα for 48 h and the supernatants were assayed for sTNF-RI. Data were derived from six to seven experiments with cells from different donors. An asterisk represents a significant difference compared with the untreated control.
The Role of Transcript Stability in Cytokine-Induced HPFB Responses
To assess whether the differences in the magnitude of IL-1β- and TNFα-elicited responses could be related to differences in the stability of mRNA transcripts induced, the rate of their degradation was measured in the presence of the transcription inhibitor actinomycin D. These experiments showed that the degradation of IL-1β-induced transcripts of CXCL1, CXCL8, and G-CSF was delayed compared with those induced by TNFα (Figure 10).
Stability of IL-1β- and TNFα-induced cytokine mRNAs in HPFB. Quiescent HPFB were stimulated with 1 ng/ml of either IL-1β or TNFα for 6 h, then washed and treated with actinomycin D (5 μg/ml). Total RNA was extracted at the time points indicated and analyzed by RT-PCR in panel a. The expression of mRNAs for CXCL1 (panel b), CXCL8 (panel c), and G-CSF (panel d), as measured as cytokine/β-actin ratios, was presented as a percentage of the value representing time zero; IL-1β (black circles), TNFα (white circles).
DISCUSSION
Although the peritoneal mesothelium is a potent source of PMN-targeting cytokines, its integrity may easily be jeopardized by infection, surgical trauma, and/or exposure to dialysis fluids.25, 28, 38, 39 Such events would increase the significance of cytokines produced by other cell types. This study shows that HPFB may be an important source of cytokines mediating PMN recruitment into the peritoneum.
First, we established apparently normal HPFB in culture. Fibroblast may be difficult to positively identify, therefore in addition to standard criteria (spindle cell morphology and the absence of markers of other cell types), we stained the cells with the TE-7 antibody. This antibody was initially raised against human thymic stroma,40 but it was recently adopted for identifying fibroblasts and shown to stain 50–100% fibroblast with moderate intensity and high specificity.32 Indeed, we found that HPFB stained extensively with the TE-7 antibody, but not with the control antibody.
Having confirmed HPFB identity, we showed that the exposure of HPFB to a milieu present in the inflamed peritoneum triggered the secretion of PMN-targeting cytokines. The most potent reaction was induced by those samples of peritoneal fluid that contained the highest concentrations of proinflammatory cytokines, IL-1β and TNFα. These effluents also contained high levels of CXCL8 and CXCL1, with CXCL8 slightly predominating in absolute values. In contrast, HPFB treated with these effluents under controlled in vitro conditions seemed to produce more CXCL1 than CXCL8. These data do not have to be contradictory, as chemokine levels in vivo are also related to the production by other sources such as peritoneal macrophages and/or mesothelial cells. They are also affected by the time that elapsed from the onset of infection and the volume of dialysis fluid drained.5, 4
To determine the contribution of IL-1β and TNFα to the effects observed, the impact of PDE was assessed in the presence of potent blocking antibodies. These experiments showed that IL-1β was a key stimulus, as the neutralization of IL-1β, but not of TNFα, significantly reduced the production of all PMN-targeting cytokines by HPFB.
During peritonitis IL-1β and TNFα are thought to be generated primarily by peritoneal macrophages.41 The exposure of HPFB to IL-1β- and TNFα-containing media from cultures of endotoxin-stimulated PM resulted in a huge release of PMN-targeting cytokines. The pattern of inhibition with neutralizing antibodies pointed again to IL-1β as a chief inducer of the cytokines investigated.
As the samples of both peritoneal dialysate and PM-CM could potentially contain other mediators that modulated proinflammatory activities of IL-1β and TNFα, we examined the pattern of CXCL1, CXCL8, and G-CSF release by HPFB treated with pure recombinant IL-1β and TNFα. The experiments revealed that in this setting also IL-1β was a much more potent stimulus of PMN-targeting cytokines than TNFα. The difference was particularly pronounced with respect to CXCL1 and G-CSF. Interestingly, IL-1β at a concentration as low as 1 pg/ml was capable of triggering a substantial release of all PMN-specific cytokines by HPFB. That may explain the presence of these cytokines in the PDE from patient 4, which contained only very little IL-1β.
On the other hand, as the anti-IL-1β neutralizing antibody did not totally abolish the stimulatory effect of PDE, other factors present in PDE might have contributed to the cytokine release. For example, it has been shown that peritoneal inflammation may be associated with a rapid and transient production of IL-17,42 which is a powerful inducer of CXCL143 and G-CSF44 production in mesothelial cells. One may speculate that some effects could also be related to the massive presence of protein in the hyperpermeable-inflamed peritoneum. It has been shown that overexposure of renal tubular cells to plasma proteins may upregulate inflammatory mediators, including CXCL8.45 Furthermore, it has been suggested that an increase in CXCL8 release by mesothelial cells may occur as a result of exposure to glucose degradation products present in dialysis solutions46 or may be related to peritoneal dialysis fluid-induced heat shock response.47 These factors might partly explain the presence of CXCL8 in PDE of patient 3, despite the absence of detectable IL-1β and TNFα.
The early appearance of soluble TNF receptors during peritonitis has been well documented.48 As their levels may be several hundred times higher than those of TNFα, they may limit TNFα activity by competing for the ligand with the cell surface receptors.49 To test whether this mechanism could underlie a weak effect of TNFα on HPFB chemokine synthesis, we assessed its activity in the presence of exogenous soluble TNF receptors. We found no significant effect of these receptors, at clinically relevant doses, on TNFα stimulatory activity. Moreover, we tested whether HPFB shed TNF receptors in response to proinflammatory cytokines, as this might result in a decrease in the number of receptors on the cell surface and diminished cell responsiveness to TNFα. We found a slight increase in sTNF-RI shedding by HPFB treated with IL-1β, but not with TNFα. Taken together, these results did not indicate that the poor induction of PMN-targeting cytokines by TNFα was related to the inhibition by soluble TNF receptors.
Interestingly, we observed that the magnitude of differences between IL-1β- and TNFα-induced effects seemed to be less at the mRNA level than at the protein level. We hypothesized that a different pattern of HPFB response to IL-1β and TNFα could be regulated at the post-transcriptional level. Indeed, we found that IL-1β-induced transcripts of CXCL1, CXCL8, and G-CSF were more stable than those induced by TNFα. Stabilization of mRNA is an effective means for increasing the pool of translatable mRNA and ultimately the amount of protein synthesized.50 In this respect Cubitt et al51 showed that increased mRNA stability was responsible for much higher CXCL1 release by keratinocytes in response to IL-1α compared with TNFα. It is thought that IL-1 stabilizes mRNAs of several inflammatory genes, including CXCL1 and CXCL8,52 partly by inhibiting deadenylation and decay mediated by AU-rich elements of the transcript.
Although IL-1β and TNFα display several overlapping properties, the evident predominance of IL-1β has already been observed in the context of peritonitis. Yung et al53 have shown that IL-1β, by acting on mesothelial cells, is a key stimulator of hyaluronan synthesis during peritonitis. On the other hand, IL-1β and TNFα are known to exhibit synergistic activities, as exemplified by their impact on fibroblast prostaglandin production.54 We have earlier shown an amplifying effect of TNFα on CCL2 and CXCL8 release by HPFB.55 In this study we found that TNFα increased the IL-1β-induced releases of CXCL1 and CXCL8 in an additive manner. In addition, TNFα increased synergistically the IL-1β-stimulated G-CSF secretion, which is interesting, given that TNFα alone had a rather modest effect on G-CSF release. In keeping with these observations, we found that neutralization of TNFα activity, in addition to IL-1β blockade, further decreased the capacity of PM-CM to induce all the cytokines studied. Similar effect was reported earlier by Betjes et al,56 who examined the ability of PM-CM to induce CXCL8 in peritoneal mesothelial cells. Surprisingly, we did not detect such an effect when anti-TNFα antibodies were added to TNFα-containing peritoneal effluents from patients with peritonitis. It could be attributed to the limited neutralizing capacity of the antibody working in a complex environment of the peritoneal effluent.
In conclusion, our observations indicate that peritoneal fibroblasts may be an important source of cytokines that ensure neutrophil accumulation in the peritoneum during peritonitis. Our data also point to IL-1β as a key mediator that elicits such a response in peritoneal fibroblasts.
References
Li Y, Karlin A, Loike JD, et al. Determination of the critical concentration of neutrophils required to block bacterial growth in tissues. J Exp Med 2004;200:613–622.
Kobayashi Y . Neutrophil infiltration and chemokines. Crit Rev Immunol 2006;26:307–316.
Metcalf D, Robb L, Dunn AR, et al. Role of granulocyte-macrophage colony-stimulating factor and granulocyte colony-stimulating factor in the development of an acute neutrophil inflammatory response in mice. Blood 1996;88:3755–3764.
Brauner A, Hylander B, Wretlind B . Interleukin-6 and interleukin-8 in dialysate and serum from patients on continuous ambulatory peritoneal dialysis. Am J Kidney Dis 1993;22:430–435.
Brauner A, Hylander B, Lu Y . Granulocyte stimulating factor in patients on peritoneal dialysis and LPS stimulated peripheral blood mononuclear cells. Inflammation 1998;22:393–401.
Betjes MG, Visser CE, Zemel D, et al. Intraperitoneal interleukin-8 and neutrophil influx in the initial phase of a CAPD peritonitis. Perit Dial Int 1996;16:385–392.
Mercer-Jones MA, Shrotri MS, Heinzelmann M, et al. Regulation of early peritoneal neutrophil migration by macrophage inflammatory protein-2 and mast cells in experimental peritonitis. J Leukoc Biol 1999;65:249–255.
Ko YC, Mukaida N, Kasahara T, et al. Specific increase in interleukin-8 concentrations in dialysis fluid of patients with peritonitis receiving continuous ambulatory peritoneal dialysis. J Clin Pathol 1995;48:115–119.
Walley KR, Lukacs NW, Standiford TJ, et al. Elevated levels of macrophage inflammatory protein 2 in severe murine peritonitis increase neutrophil recruitment and mortality. Infect Immun 1997;65:3847–3851.
Call DR, Nemzek JA, Ebong SJ, et al. Ratio of local to systemic chemokine concentrations regulates neutrophil recruitment. Am J Pathol 2001;158:715–721.
Ness TL, Hogaboam CM, Strieter RM, et al. Immunomodulatory role of CXCR2 during experimental septic peritonitis. J Immunol 2003;171:3775–3784.
Tanimoto N, Terasawa M, Nakamura M, et al. Involvement of KC, MIP-2, and MCP-1 in leukocyte infiltration following injection of necrotic cells into the peritoneal cavity. Biochem Biophys Res Commun 2007;361:533–536.
Wengner AM, Pitchford SC, Furze RC, et al. The coordinated action of G-CSF and ELR+ CXC chemokines in neutrophil mobilization during acute inflammation. Blood 2008;111:42–49.
Topley N, Liberek T, Davenport A, et al. Activation of inflammation and leukocyte recruitment into the peritoneal cavity. Kidney Int Suppl 1996;56:S17–S21.
Yao V, Platell C, Hall JC . Role of peritoneal mesothelial cells in peritonitis. Br J Surg 2003;90:1187–1194.
McLoughlin R . Resolving peritoneal inflammation: flicking the right ‘switches’. Perit Dial Int 2005;25:223–229.
Topley N, Brown Z, Jörres A, et al. Human peritoneal mesothelial cells synthesize interleukin-8. Synergistic induction by interleukin-1 beta and tumor necrosis factor-alpha. Am J Pathol 1993;142:1876–1886.
Visser CE, Tekstra J, Brouwer-Steenbergen JJ, et al. Chemokines produced by mesothelial cells: huGRO-alpha, IP-10, MCP-1 and RANTES. Clin Exp Immunol 1998;112:270–275.
Lanfrancone L, Boraschi D, Ghiara P, et al. Human peritoneal mesothelial cells produce many cytokines (granulocyte colony-stimulating factor [CSF], granulocyte-monocyte-CSF, macrophage-CSF, interleukin-1 [IL-1], and IL-6) and are activated and stimulated to grow by IL-1. Blood 1992;80:2835–2842.
Flavell SJ, Hou TZ, Lax S, et al. Fibroblasts as novel therapeutic targets in chronic inflammation. Br J Pharmacol 2008;153:S241–S246.
Buckley CD, Pilling D, Lord JM, et al. Fibroblasts regulate the switch from acute resolving to chronic persistent inflammation. Trends Immunol 2001;22:199–204.
Smith RS, Smith TJ, Blieden TM, et al. Fibroblasts as sentinel cells. Synthesis of chemokines and regulation of inflammation. Am J Pathol 1997;151:317–322.
Parsonage G, Falciani F, Burman A, et al. Global gene expression profiles in fibroblasts from synovial, skin and lymphoid tissue reveals distinct cytokine and chemokine expression patterns. Thromb Haemost 2003;90:688–697.
Rinn JL, Bondre C, Gladstone HB, et al. Anatomic demarcation by positional variation in fibroblast gene expression programs. PLoS Genet 2006;2:e119.
Dobbie JW, Lloyd JK, Gall CA . Categorization of ultrastructural changes in peritoneal mesothelium, stroma and blood vessels in uremia and CAPD patients. Adv Perit Dial 1990;6:3–12.
Jimenez-Heffernan JA, Aguilera A, Aroeira LS, et al. Immunohistochemical characterization of fibroblast subpopulations in normal peritoneal tissue and in peritoneal dialysis-induced fibrosis. Virchows Arch 2004;444:247–256.
Aroeira LS, Aguilera A, Sanchez-Tomero JA, et al. Epithelial to mesenchymal transition and peritoneal membrane failure in peritoneal dialysis patients: pathologic significance and potential therapeutic interventions. J Am Soc Nephrol 2007;18:2004–2013.
Ryan GB, Grobety J, Majno G . Mesothelial injury and recovery. Am J Pathol 1973;71:93–112.
Jörres A, Ludat K, Lang J, et al. Establishment and functional characterization of human peritoneal fibroblasts in culture: regulation of interleukin-6 production by proinflammatory cytokines. J Am Soc Nephrol 1996;7:2192–2201.
Beavis MJ, Williams JD, Hoppe J, et al. Human peritoneal fibroblast proliferation in 3-dimensional culture: modulation by cytokines, growth factors and peritoneal dialysis effluent. Kidney Int 1997;51:205–215.
Witowski J, Jorres A . Peritoneal cell culture: fibroblasts. Perit Dial Int 2006;26:292–299.
Goodpaster T, Legesse-Miller A, Hameed MR, et al. An immunohistochemical method for identifying fibroblasts in formalin-fixed, paraffin-embedded tissue. J Histochem Cytochem 2008;56:347–358.
Troidle L, Gorban-Brennan N, Kliger A, et al. Continuous peritoneal dialysis-associated peritonitis: a review and current concepts. Semin Dial 2003;16:428–437.
Witowski J, Jörres A, Coles GA, et al. Superinduction of IL-6 synthesis in human peritoneal mesothelial cells is related to the induction and stabilization of IL-6 mRNA. Kidney Int 1996;50:1212–1223.
Witowski J, Korybalska K, Ksiazek K, et al. Peritoneal dialysis with solutions low in glucose degradation products is associated with improved biocompatibility profile towards peritoneal mesothelial cells. Nephrol Dial Transplant 2004;19:917–924.
Mackenzie RK, Coles GA, Williams JD . Eicosanoid synthesis in human peritoneal macrophages stimulated with S. epidermidis. Kidney Int 1990;37:1316–1324.
Jörres A, Dinter H, Topley N, et al. Inhibition of tumour necrosis factor production in endotoxin-stimulated human mononuclear leukocytes by the prostacyclin analogue iloprost: cellular mechanisms. Cytokine 1997;9:119–125.
von Ruhland CJ, Newman GR, Topley N, et al. Can artifact mimic the pathology of the peritoneal mesothelium? Perit Dial Int 2003;23:428–433.
Polubinska A, Winckiewicz M, Staniszewski R, et al. Time to reconsider saline as the ideal rinsing solution during abdominal surgery. Am J Surg 2006;192:281–285.
Haynes BF, Scearce RM, Lobach DF, et al. Phenotypic characterization and ontogeny of mesodermal-derived and endocrine epithelial components of the human thymic microenvironment. J Exp Med 1984;159:1149–1168.
Topley N, Mackenzie RK, Williams JD . Macrophages and mesothelial cells in bacterial peritonitis. Immunobiology 1996;195:563–573.
Shibata K, Yamada H, Hara H, et al. Resident Vdelta1+ gammadelta T cells control early infiltration of neutrophils after Escherichia coli infection via IL-17 production. J Immunol 2007;178:4466–4472.
Witowski J, Pawlaczyk K, Breborowicz A, et al. IL-17 stimulates intraperitoneal neutrophil infiltration through the release of GRO alpha chemokine from mesothelial cells. J Immunol 2000;165:5814–5821.
Witowski J, Ksiazek K, Warnecke C, et al. Role of mesothelial cell-derived granulocyte colony-stimulating factor in interleukin-17-induced neutrophil accumulation in the peritoneum. Kidney Int 2007;71:514–525.
Tang S, Leung JC, Abe K, et al. Albumin stimulates interleukin-8 expression in proximal tubular epithelial cells in vitro and in vivo. J Clin Invest 2003;111:515–527.
Welten AG, Schalkwijk CG, ter Wee PM, et al. Single exposure of mesothelial cells to glucose degradation products (GDPs) yields early advanced glycation end-products (AGEs) and a proinflammatory response. Perit Dial Int 2003;23:213–221.
Bender TO, Riesenhuber A, Endemann M, et al. Correlation between HSP-72 expression and IL-8 secretion in human mesothelial cells. Int J Artif Organs 2007;30:199–203.
Zemel D, Imholz AL, de Waart DR, et al. Appearance of tumor necrosis factor-alpha and soluble TNF-receptors I and II in peritoneal effluent of CAPD. Kidney Int 1994;46:1422–1430.
Garton KJ, Gough PJ, Raines EW . Emerging roles for ectodomain shedding in the regulation of inflammatory responses. J Leukoc Biol 2006;79:1105–1116.
Hollams EM, Giles KM, Thomson AM, et al. mRNA stability and the control of gene expression: implications for human disease. Neurochem Res 2002;27:957–980.
Cubitt CL, Lausch RN, Oakes JE . Differential induction of GRO alpha gene expression in human corneal epithelial cells and keratocytes exposed to proinflammatory cytokines. Invest Ophthalmol Vis Sci 1997;38:1149–1158.
Stoeckle MY . Post-transcriptional regulation of gro alpha, beta, gamma, and IL-8 mRNAs by IL-1 beta. Nucleic Acids Res 1991;19:917–920.
Yung S, Coles GA, Davies M . IL-1 beta, a major stimulator of hyaluronan synthesis in vitro of human peritoneal mesothelial cells: relevance to peritonitis in CAPD. Kidney Int 1996;50:1337–1343.
Elias JA, Gustilo K, Baeder W, et al. Synergistic stimulation of fibroblast prostaglandin production by recombinant interleukin 1 and tumor necrosis factor. J Immunol 1987;138:3812–3816.
Witowski J, Thiel A, Dechend R, et al. Synthesis of C-X-C and C-C chemokines by human peritoneal fibroblasts: induction by macrophage-derived cytokines. Am J Pathol 2001;158:1441–1450.
Betjes MG, Tuk CW, Struijk DG, et al. Interleukin-8 production by human peritoneal mesothelial cells in response to tumor necrosis factor-alpha, interleukin-1, and medium conditioned by macrophages cocultured with Staphylococcus epidermidis. J Infect Dis 1993;168:1202–1210.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Witowski, J., Tayama, H., Książek, K. et al. Human peritoneal fibroblasts are a potent source of neutrophil-targeting cytokines: a key role of IL-1β stimulation. Lab Invest 89, 414–424 (2009). https://doi.org/10.1038/labinvest.2009.1
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/labinvest.2009.1
Keywords
This article is cited by
-
The peritoneal “soil” for a cancerous “seed”: a comprehensive review of the pathogenesis of intraperitoneal cancer metastases
Cellular and Molecular Life Sciences (2018)
-
The proto-oncogene c-Fos transcriptionally regulates VEGF production during peritoneal inflammation
Kidney International (2013)