Abstract
Patients with severe eosinophilic asthma often require systemic medication, including corticosteroids and anti-type 2 (T2) cytokine biologics, to control the disease. While anti-IL5 and anti-IL4Rα antibodies suppress the effects of IL-4, IL-5 and IL-13, the molecular pathways modified by these biologics that are associated with clinical improvement remain unclear. Therefore, we aimed to describe the effects of T2-targeting biologics on the gene expression of blood immune cells. We conducted single-cell RNA sequencing (scRNA-seq) of peripheral blood mononuclear cells (PBMCs) from eight patients with severe eosinophilic asthma treated with mepolizumab, reslizumab, or dupilumab. PBMCs were obtained before the initiation of biologics and at 1- and 6-month timepoints after the initiation of treatment to elucidate treatment-induced changes. During treatment, the proportions of T cells/natural killer (NK) cells, myeloid cells, and B cells did not change. However, the composition of classical monocytes (CMs) changed: IL1B+ CMs were reduced, and S100A+ CMs were increased. The subsets of T cells also changed, and significant downregulation of the NF-κB pathway was observed. The genes related to the NF-κB pathway were suppressed across T/NK, myeloid, and B cells. The transcriptional landscape did not significantly change after the first month of treatment, but marked changes occurred at six-month intervals. In conclusion, regardless of the type of biologics used, suppression of T2-mediated pathways ultimately reduces the expression of genes related to NF-κB signaling in circulating immune cells. Further studies are warranted to identify potential biomarkers related to treatment response and long-term outcomes.
Clinical trial registration number: NCT05164939
Similar content being viewed by others
Introduction
Severe asthma is a chronic inflammatory disease of the airways characterized by uncontrolled symptoms despite the use of high-dose inhaled corticosteroids1. For patients with severe asthma, systemic medication, including systemic corticosteroids and additional biologics, is often required to control airway inflammation2. Biologics that target type 2 (T2) cytokines such as interleukin (IL)-4, IL-5, and IL-13 have widened the treatment options for patients with severe eosinophilic asthma3. Although the inhibition of key T2 cytokines ultimately alleviates eosinophilic inflammation in the airways and leads to clinical improvement4, the complex interactive molecular networks modulated by biologic therapy remain largely unknown5. In addition, biomarkers that predict treatment response to biologics are lacking, except for the blood eosinophil count, which has satisfactory predictivity6,7 only, as treatment response does not always correlate with blood eosinophil levels8,9.
Recent advances in omics technology have enabled researchers to further elucidate the pathophysiology of asthma and identify its molecular phenotypes10,11. In particular, transcriptomic analysis can provide information on the patterns and dynamics of gene expression related to the severity or the level of control of asthma12. More recently, the application of single-cell RNA sequencing (scRNA-seq) has revealed gene expression at the single-cell level in bronchial biopsies of a small number of patients with mild asthma13. These scRNA-seq studies have enabled the identification of novel cell types and gene networks that may be involved in the pathogenesis of asthma14. To date, no study has investigated the cell-specific transcriptional changes induced by treatment with biologics. Considering that biologic therapies influence circulating blood cells, the identification of alterations in specific pathways involving specific circulating immune cells could provide important insights into the mechanisms of action of these biologic therapies and potential blood biomarkers related to treatment response3.
The prospective observational study precision medicine intervention in severe asthma (PRISM)15, which includes patients with severe asthma, aims to identify molecular pathways related to the progression of severe asthma and the response to biologics by performing multiomics analyses of serially obtained samples. We hypothesized that scRNA-seq analysis of peripheral blood cells from patients within the PRISM study may reveal novel cell-specific pathways modulated by anti-asthma biologics in addition to the expected T2 pathways. Therefore, we performed scRNA-seq analysis on the peripheral blood immune cells of patients with severe asthma who were successfully treated with the anti-IL-5 biologics mepolizumab and reslizumab and the anti-IL4Ra antibody dupilumab.
Methods
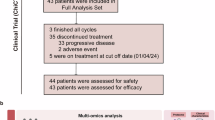
A schematic of the scRNA-seq testing that was performed on peripheral blood mononuclear cells (PBMCs) from eight patients with severe asthma is shown in Fig. 1a. The clinical data and blood samples were obtained consecutively: before initiating treatment with biologics (0 M) and one month (1 M) and six months (6 M) after treatment. The Institutional Review Board of Asan Medical Center approved this study, and all patients provided written informed consent (IRB No. 2019–1676).
a Experimental design illustrating the sample preparation for the study. b UMAP plots of all cells classified into T/NK cells, myeloid cells, B cells, or platelets and separated according to treatment duration. c UMAP plots showing the subtypes of myeloid cells (left panel) and their distributions according to treatment duration (right panel). d Line plots displaying the frequencies of myeloid cell subtypes, where the x-axis represents the treatment duration and the y-axis represents the frequency. Each line type represents a patient, and the colors indicate the biologics with which they were treated: mepolizumab/reslizumab or dupilumab. Asterisks denote significant differences between the two treatment durations with an FDR of 0.01. e Dot plots showing the top 5 highly expressed genes in IL-1B+ CMs (first five) and S100A+ CMs (last five) compared with other myeloid cell subtypes.
Sample preparation and sequencing
PBMCs were isolated from whole blood using Ficoll‒Paque™ (Miltenyi Biotec, CA). Single-cell RNA library preparation and sequencing were performed by DNA Link, Inc. (Seoul, Korea), the details of which are described in the Online Supplement.
Data preprocessing
The FASTQ files from all 24 samples from 8 patients were aligned and aggregated using 10x Genomics Cell Ranger 6.0.016. The raw count matrix consisted of 36,601 features and 102,951 cells. Features detected in fewer than 3 cells and cells with fewer than 200 non-zero expressed features were removed. Next, the number of detected features and their counts on a log10 scale and the ratio of mitochondrial genes were calculated for each cell. Cells that did not deviate more than 5 median absolute deviations (MADs) from the medians of the number of detected features and their counts and 10 MADs from the median of the ratio of mitochondrial genes were retained. Among the remaining cells, doublet cells with hybrid scores greater than 0.8 were removed using the scds R package (v1.0.0)17. Finally, 25,242 features of 89,728 cells were used for the analysis. The data were normalized via the NormalizeData function with its default options in Seurat (v4.0.5)18. Throughout the entire process, the Seurat (v4.0.5) and ggplot2 (v3.4.0)19 packages within R (v4.1.1) were used.
Cell type annotation
The cell types were manually annotated using specific markers (Supplementary Fig. 1a). These cell types and CD4+ T cells were clustered into their subtypes according to established markers (Supplementary Fig. 1b–d and Supplementary Fig. 2). CD4+ T cells were further classified into State 0 (S0) and State 1 (S1) groups on the basis of clusters, with State 0 consisting primarily of cells from cluster 0 M and 1 M and State 1 consisting primarily of cells from cluster 6 M. To visualize the cells on a two-dimensional plot, the principal components (PCs) of the gene expression matrix were calculated based on 2,000 highly variable genes via the RunPCA and FindVariableFeatures functions using their default options in Seurat. We selected the optimal number of PCs for clustering the cells based on elbow plots, which represent the standard deviation of each PC. Next, with the optimal number, UMAP scores were calculated via the RunUMAP function in Seurat. For further clustering, the FindNeighbors and FindClusters functions in Seurat were used.
Association test between frequencies of cell types and duration of treatment
The frequencies of cell types were calculated by dividing the number of each cell type by the total number of cells obtained from a single patient. To determine whether the frequencies of the cell types were associated with the duration of treatment, linear mixed effect models were used. Patients were considered random effects in these models. The full model included the status variable, whereas the reduced model only consisted of the intercept term as an explanatory variable. The significance of the status variable was estimated using the difference in likelihoods of the two models, and p values were adjusted via the Benjamini‒Hochberg method.
Differentially expressed gene (DEG) analysis
The FindMarkers function in Seurat was used to compare the gene expression levels between groups. For this test, we used MAST and used the other settings at their default values. Genes whose false discovery rate (FDR) was less than 0.01 and whose log2-fold change was greater than 0.25 compared with the other group(s) were considered differentially expressed genes (DEGs). To test the effects of treatment duration on gene expression levels, T/natural killer (NK), myeloid, and B cells at 0 M and 1 M were combined into one group and compared with their counterparts at 6 M, while CD4+ T cells in the S0 and S1 groups were compared with each other. When comparing subtypes, each subtype was compared with the other subtypes, and when two groups were designated, only those subtypes were compared. Dot plots and heatmaps were drawn using the DotPlot and DoHeatmap functions in Seurat, respectively. The DEGs were further analyzed to identify pathways or transcription factors (TFs) associated with these genes via MSigDB Hallmark 2020 and TRRUST Transcription Factors 2019 implemented in Enrich R (https://maayanlab.cloud/Enrichr/)20. The top 5 most significant terms associated with DEGs at 0 M and 1 M or with S0 were extracted from each analysis, and their p values were compared with those of the association test between the terms and DEGs at 6 M and for S1 cells.
Cell‒cell communication analysis
Cell-cell communication analyses were conducted via the CellChat R package (v1.5.0)21 for CD4+ T-cell subtypes (excluding T-cell receptor (TCR)-stimulated subtypes), IL1B+ and S100A+ classical monocytes, and naïve and memory B cells. Ligand‒receptor interaction data were obtained from CellChatDB.human, which was provided by the package mentioned above. Signaling pathways in the inferred cellular communication networks were identified on the basis of biologics and treatment duration. Chord diagrams of signaling pathway networks were drawn via the netVisual_aggregate function in the package with its default options. The difference in the number of interactions between S1 and S0 is shown in raster plots.
Results
Characteristics of the study participants
A total of eight patients with severe eosinophilic asthma were included in the analysis. The baseline data and changes in clinical variables, including inflammatory markers, lung function, asthma control test score, number of acute exacerbations, and use of maintenance oral corticosteroids (OCS) over time, are described in Table 1 and Supplementary Table 1. Two patients were treated with mepolizumab (100 mg IV every 4 weeks), two patients were treated with reslizumab (3 mg/kg IV every 4 weeks), and four patients were treated with dupilumab (600 mg loading dose followed by 300 mg IV every 2 weeks) for up to six months. Four participants treated with anti-IL-5 antibodies had a significantly improved FEV1 (% predicted) (53.00 ± 6.48 vs. 72.75 ± 10.21, p = 0.008) (Table 1) along with a reduced blood eosinophil count (1244 ± 1088.4 vs. 36.5 ± 13.99, p = 0.030) after 6 months of biologic therapy (Supplementary Table 1). Two of the four patients treated with dupilumab succeeded in the withdrawal of maintenance OCS (Table 1). In all the molecular analyses, the results of the patients on mepolizumab and reslizumab were combined and compared with the results of the patients on dupilumab.
Transcriptional profiles of blood immune cells after biologic treatment
From the 24 samples from 8 patients analyzed over 3 timepoints, we identified 25,242 features and 89,728 cells. Marker genes were used to call immune cell types (Supplementary Fig. 1a), including the subtypes of T/NK cells (Supplementary Fig. 1b), myeloid cells (Supplementary Fig. 1c), and B cells (Supplementary Fig. 1d). A UMAP projection of T/NK cells, myeloid cells, B cells, and platelets from the combined data plotted according to the treatment duration revealed that the distribution of cells at 6 M was different from that at 0 M and 1 M (Fig. 1b). However, the overall proportions of T/NK, myeloid, and B cells remained similar during treatment with biologics (Supplementary Fig. 1e). Several clusters belonging to these cell types were differentially distributed at 6 M compared with 0 M and 1 M (Fig. 1c and Supplementary Fig. 1f). These findings suggest that the states of cell subtypes are altered by treatment with biologics. A subanalysis of myeloid cells revealed the presence of classical monocytes (CMs), intermediate monocytes (IMs), nonclassical monocytes (NMs), unclassified monocytes, conventional dendritic cells (cDCs), and plasmacytoid dendritic cells (pDCs). CMs were further divided into S100A+ and IL1B+ CMs (Fig. 1c). The predominant changes in myeloid cells at 6 M occurred mainly among CMs (Fig. 1d), while the IL1B+ CMs that were dominant at 0 M and 1 M were supplanted by S100A+ CMs at 6 M irrespective of the type of biologic therapy. The most highly expressed DEGs in IL1B+ CMs were IL1B, CXCL8, and CCL3, whereas S100A+ CMs were characterized by high expression of S100 protein family genes, including S100A8, S100A9, and S100A12 (Fig. 1e).
The transcriptional profiles of T/NK cells were well separated between the 1 M and 6 M treatment groups within each subtype of T/NK cells (Supplementary Fig. 1f); however, the proportion of each subtype did not change significantly over time (Supplementary Fig. 1g). In contrast, biologic therapy failed to induce any significant changes in B-cell clusters or in the proportions of subtypes present in the blood (Supplementary Fig. 1h and 1i).
Transcriptomic profile of blood CD4+ T cells after biologic treatment
We expected the profile of CD4+ T cells, which drive type 2 inflammation in asthma, to be modified with anti-T2 biologics. As indicated above (Supplementary Fig. 1f), the transcription profile of CD4+ T cells at 6 M was considerably different from that at 0 M and 1 M. Therefore, we classified these T cells not only into classical subtypes but also into State 0 (S0) and State 1 (S1) groups, which represent different types or states of these cells. Thus, the cells were annotated as one of the following: naïve S0 and S1, T central memory (TCM) S0 and S1, effector memory (EM) S0 and S1, and terminally differentiated effector memory cells (EM/EMRA) S0 and S1. Different states or cell types were not observed for regulatory T cells (Tregs) or TCR-stimulated naïve or memory cells after 6 M; thus, these cells did not transition into different states (Fig. 2a). Naïve S0, TCM S1, Treg, TCR-stimulated naïve, and TCR-stimulated memory cells did not significantly change after 6 months. In contrast, the enrichment of naïve S1, EM S1, and EM/EMRA S1 cells was significantly increased at 6 M, irrespective of the treatment received. The enrichment of TCM S0, EM S0, and EM/EMRA S0 cells was significantly decreased at 6 M across all treatments (Fig. 2b).
a UMAP plots showing the subtypes of CD4+ T cells (left panel) and their distributions according to treatment duration (right panel). b Line plots displaying the subtypes, where the x-axis and y-axis represent the treatment duration and frequency, respectively. The line types and colors correspond to the conditions, and asterisks indicate significant changes between the treatment durations with an FDR of 0.01. S0 and S1 represent States 0 and 1, respectively.
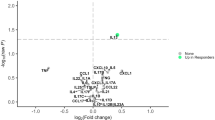
Genes involved in the NF-κB pathway are downregulated across cell types
When we compared the gene expression levels between S0 and S1 CD4+ T cells, activator protein 1 (AP-1) genes such as FOS, FOSB, JUN, and JUNB were significantly downregulated, whereas GIMAP family genes (GIMAP1, GIMAP4, GIMAP5, and GIMAP7) were significantly upregulated in the S1 group (Fig. 3a). Pathway and TF analyses of the DEGs between the two groups revealed that the downregulated DEGs in the S1 group were associated with TNF-α signaling via NF-κB, followed by hypoxia, interferon (IFN)-γ responses, the p53 pathway, and apoptosis (Fig. 3b). Among the top 20 downregulated DEGs, 14 genes, including AP-1 genes, DUSP1/2, CD69, TNFAIP3, NFKBIA, ZFP36, PPP1R15A, SLC2A4, SOCS3, and BTG2, were involved in the NF-κB pathway. In the TF analysis, the two main subunits of NF-κB, RELA and NFKB1, were significantly associated with the downregulated DEGs in the S1 group (Fig. 3c). In addition, STAT3, a target of IL-4/5/13, was significantly associated with these DEGs, with an FDR of 0.05.
a Heatmap displaying the expression levels of DEGs that were significantly different between S0 and S1 CD4+ T cells and categorized by treatment duration and biologic conditions. The top 20 downregulated and upregulated DEGs in CD4+ T S1 cells compared with S0 cells are shown on the y-axis. b Top 5 MSigDB hallmark 2020 pathways and their p values associated with upregulated DEGs in State 0. The y-axis represents the names of the pathways, and the x-axis represents the −log10 of their p values. Each pathway has two bars representing p values calculated for upregulated DEGs in S0 (red) and S1 (turquoise). c The top 5 TRRUST transcription factors and their p values associated with upregulated DEGs in S0 (red). The turquoise bars represent p values of the corresponding pathways associated with upregulated DEGs in State 1.
When the gene expression levels in individual T/NK, myeloid, and B-cell subsets were investigated, a similar pattern was observed. Among the top 20 downregulated DEGs, NF-κB pathway-related genes, such as FOS, FOSB, JUN, DUSP1, NFKBIA, ZFP36, and PPP1R15A, were shared among the three main cell types, namely, T/NK cells, myeloid cells, and B cells (Supplementary Fig. 3a). TNF-α signaling via NF-κB was the most significant pathway of the cell types, followed by the hypoxia and apoptosis pathways (Supplementary Fig. 3b). In contrast to the reduction in the IFN-γ response and UV response pathways observed in T/NK cells and B cells, myeloid cells exhibited a loss in gene expression related to the inflammatory and p53 pathways. In the TF analyses, RELA and NFKB1 were also commonly found in T/NK, myeloid, and B cells and were among the top 5 associated transcription factors with downregulated DEGs at 6 months (Supplementary Fig. 3c).
Different effects of biologics on CD4+ T cells according to the mechanism of action
Since different compositional changes in CD4+ T cells were noted according to the mechanism of action of biologics by 6 M (Fig. 2b), we extracted and separately analyzed S1 CD4+ T cells (Fig. 4a). The proportions of the naïve S1 subtype were 37.7% and 4.7% in the mepolizumab/reslizumab and dupilumab groups, respectively, whereas those of the TCM S1 subtype were 13.6% and 43.1% in the mepolizumab/reslizumab and dupilumab groups, respectively (Fig. 4b). Although patients treated with dupilumab had different OCS maintenance statuses (Table 1), the frequencies of naïve and TCM S1 subtypes were not different between patients who underwent withdrawal during treatment (patients 6 and 8) and patients who did not (patient 7) (Fig. 2b and Supplementary Table 2). The downregulated DEGs in the naïve S1 CD4+ T-cell subtype compared with those in the TCM S1 CD4+ T-cell subtype were significantly associated with TNF-α signaling via NF-κB, hypoxia, the IFN-γ response, the p53 pathway, and apoptosis (Fig. 4c). Moreover, the downregulated DEGs in the TCM S1 CD4+ T-cell subtype compared with those of the naïve S1 CD4+ T-cell subtype were significantly associated with the complement pathway (Fig. 4c).
a Dimension plots of CD4+ T S1 cells plotted according to subtype (left panel) and biologics type (right panel). On the right panel, the cells associated with mepolizumab/reslizumab and dupilumab are colored red and turquoise, respectively. b Pie charts show the frequencies of the subtypes according to the biologics type. c Dot plots of DEGs included in the MSigDB hallmark 2020 pathways were significantly associated with upregulated DEGs in TCM S1 cells compared with naïve S1 cells (the first five), and vice versa (the last). The colored bars and circles represent the average expression and percent expression of the corresponding genes according to subtype, respectively. d Chord plots of the MHC-II signaling pathway network of the 0/1 M and 6 M groups of the mepolizumab/reslizumab and dupilumab groups. e Chord plots of the CD40 signaling pathway network of the 0/1 M and 6 M groups in patients in the mepolizumab/reslizumab and dupilumab groups. S0 and S1 represent States 0 and 1, respectively.
After treatment, the number of cell‒cell interactions generally decreased; specifically, the number of interactions between CMs or B cells and naïve S0 CD4+ T cells decreased the most across all treatments (Supplementary Fig. 4a). However, distinct differences were observed between the results after mepolizumab/reslizumab and those after dupilumab treatment, as the former resulted in enhanced connections in TCM S1 cells and the latter resulted in enhanced connectivity within naïve S1 T cells (Supplementary Fig. 4a). Connectivity maps of all the studied cell types revealed differences in S0 and S1 with respect to the MHC-II signaling pathway network (Supplementary Fig. 4b) but not in the CD40 signaling pathway network across all treatments (Supplementary Fig. 4c). Separation of the two treatment groups revealed a greater impact of dupilumab than of mepolizumab/reslizumab on both the MHC-II signaling pathway network (Fig. 4d) and the CD40 signaling pathway (Fig. 4e). The interactions between CD4+ T and B cells considerably decreased only in patients treated with dupilumab (Fig. 4d, e).
Discussion
In the present study, we delineated the alterations in the cellular transcriptomic profiles of specific PBMC subsets from patients with severe eosinophilic asthma treated with mepolizumab, reslizumab, or dupilumab for six months. T2-targeting biologics reduced IL1B+ CMs and increased S100A+ CMs. These biologics also altered the composition of subsets of CD4+ T cells, which indicates significant downregulation of the NF-κB pathway across immune cells. Key regulatory pathways, including MHC-II and CD40 signaling and links to B-cell activation, were differentially affected in the dupilumab- and mepolizumab/reslizumab-treated patient groups. Transcriptional changes in PBMCs occurred at least one month after the initiation of treatment with biologics, which reflects altered systemic conditions induced by biologics.
Previous studies utilizing scRNA-seq analyses of immune and structural cells in humans and mice have contributed to our understanding of the pathophysiology of asthma14. In terms of human studies, Chen and colleagues compared the transcriptional characteristics of PBMCs from patients with severe asthma and those from healthy controls22. Although the composition of the cell subsets was similar between the groups, increased expression of JAK1, the long noncoding RNA NEAT1, and IL32 was noted in specific cell types of patients with severe asthma. Li and colleagues reported the results of single-cell transcriptomics of immune cells in bronchoalveolar lavage fluid during asthma exacerbation, which highlighted an increase in CD8+ T cells, monocytes, and macrophages and the distinct expression of proinflammatory cytokine genes and transcription factors associated with asthma exacerbation23. However, longitudinal serial data from scRNA-seq of immune cells from patients with asthma over time and following therapy are lacking14.
By alleviating eosinophilic inflammation, biologics that target key T2 cytokines have shown therapeutic benefits in severe eosinophilic asthma3. Several studies have evaluated the impact of biologics on circulating immune cells other than granulocytes in patients with asthma. In 2003, Buttner and colleagues reported that treatment with mepolizumab did not alter the distributions of T-cell subsets, B cells, natural killer cells, memory cells, naïve cells, or γδT cells24. Another study revealed that mepolizumab reduced the proportions of CD45+, CD8+ and NKT-like cells in the blood and increased the Treg population25. Lommatzsch and colleagues reported an increase in immature B cells after six months of treatment with dupilumab but not with benralizumab26. However, the clinical relevance of changes in the proportions of specific cell types remains uncertain. Our analysis revealed that treatment with biologics induced changes in subsets of CMs and CD4+ T cells, which suggests the importance of these cell types in the pathogenesis of severe asthma. A greater proportion of blood CMs has been reported in patients with severe asthma than in those with nonsevere asthma27, and CD4+ T cells are known to play an essential role in the development and progression of asthma28. Among CMs, the proportion of the IL1B+ subgroup was reduced, whereas that of the S100A+ subgroup was increased. The finding of decreased IL1B transcripts is consistent with suppression of the NF-κB and AP-1 pathways since IL-1 is associated with innate cytokines that activate the inflammatory process29. IL-1β is involved in chronic inflammatory diseases, and an association between IL1Bhi monocytes derived from PBMCs and active inflammatory arthritis has been reported30. However, the clinical relevance of increased S100A+ transcripts in CMs is uncertain. S100A proteins act as damage-associated molecular patterns, and elevated gene expression of some isoforms has been suggested as a prognostic marker in various pathologic conditions31. Considering that S100A8/9 induces neutrophil activation and has been reported as a marker of several inflammatory diseases, upregulation of S100A genes may indicate a shift toward the recovery of T2-skewed inflammation, as reflected by a relative increase in T1 inflammation32. The interpretation of increased S100A+ CMs in severe asthma requires further study with a longer observation period and a larger number of patients.
We further revealed that treatment with biologics induced downregulation of the key proinflammatory NF-κB and AP-1 pathways regardless of the biologic used. NF-κB and AP-1 are key players in severe relative steroid-refractory chronic airway inflammation33, and persistent NF-κB activation has been observed in patients with severe uncontrolled asthma34. In addition, external stimuli, including allergens, endotoxins, and microbial infections, stimulate activation of the NF-κB pathway. A reduction in NF-κB activity in lung tissue has been observed in patients treated with inhaled corticosteroids35,36. Considering that glucocorticoids are potent inhibitors of NF-κB activation, these findings explain the steroid-sparing effect of biologics, including dupilumab, which exerts anti-inflammatory effects despite transient elevation of blood eosinophils9,37. The observed downregulation of the NF-κB pathway across multiple PBMC types following treatment with biologics suggests the suppression of overactive immune responses and a potential reduction in immune-mediated tissue damage33. The downregulation of STAT3, which is involved in the activation of Th2 and Th17 cells, was also noted in the analysis38. In asthma, STAT3 participates in airway remodeling via the activation of M2 macrophages and fibroblasts39. The reduction in the main inflammatory signaling pathways, including the NF-κB and JAK/STAT signaling pathways, in PBMCs suggests the resolution of systemic inflammation after treatment with biologics.
Despite their similar efficacy in terms of clinical outcomes, mepolizumab and reslizumab bind to IL-5, whereas dupilumab blocks IL-4Rα3. When the composition of CD4+ T cells was compared according to the mechanisms of action of these biologics, downregulated DEGs in the TCM CD4+ T-cell S1 subtype were found to be related to the complement pathway, which was observed in patients who were treated with anti-IL5 biologics. Components of complement are known to regulate the adaptive immune response by binding to their receptors expressed on T cells40, which suggests that treatment with mepolizumab or reslizumab might also inhibit the complement pathway. An increase in sputum C3c, a marker of complement activation, has been reported to be a predictor of a suboptimal response to mepolizumab and reslizumab8. Network analysis also revealed different cell‒cell interactions in both the MHC-II and CD40 signaling pathways between biologics that target IL-5 and those that target IL-4/13. These findings indicate heterogeneity in the interplay between immune cells during the overall anti-inflammatory process according to the type of biologic used.
In contrast to changes in the clinical variables that started within four weeks after the initiation of biologics, the transcriptional profiles of immune cells markedly differed between one and six months. This aligns with the rapid change in eosinophils seen with T2-targeted therapies, followed by a slower, systemic anti-inflammatory response involving other immune cells. These findings highlight eosinophils as key effector cells and support the concept of severe asthma as a systemic disease with evolving immune involvement. Although the changes in asthma-related outcomes varied among the participants, they exhibited similar changes in circulating immune cell activation states following biologic therapy. The differences in lung function and asthma control suggest that the presence of additional factors contributes to respiratory symptoms, including immune reactions with structural cells in the airways3. Future studies should investigate whether changes in NF-κB, AP-1, and S100A pathway activation in blood cells reflect similar changes in the airways of patients with severe eosinophilic asthma following successful biologic treatment.
This study has several limitations. First, the number of included participants was small. However, longitudinal changes were analyzed for each participant, which minimized the potential nuisance effect caused by heterogeneity among all participants. Second, the participants exhibited good responses to treatment with biologics. Therefore, we could not identify a predictive signature or potential biomarker for treatment response to biologics. To address this, a follow-up study including patients with a broader range of treatment responses is needed. Third, the analyzed blood samples did not include granulocytes, including eosinophils and neutrophils, which could also play an important role in severe asthma. Granulocytes, particularly neutrophils and eosinophils, are highly fragile and prone to lysis during isolation and processing, which can result in the loss of cellular content and poor-quality RNA. Additionally, abundant RNases in these cells lead to rapid RNA degradation, which increases the difficulty of the 10x Genomics analysis41. Due to these technical limitations, we prioritized the analysis of PBMCs, which are more stable and provide high-quality RNA for scRNA-seq. Nevertheless, the deconvolution of bulk RNA-seq data from these patients may indicate alterations in the blood granulocyte status with different biologic therapies. Finally, we did not investigate the changes in the structural cells of the airway, which is a target organ in asthma. However, our study revealed alterations in the transcriptomic profiles of circulating immune cells of patients with severe asthma induced by treatment with biologics. The transcriptomic changes evident six months after treatment with biologics highlighted the downregulation of the NF-κB, AP-1, and STAT signaling pathways. Further studies with larger populations and longer treatment durations are warranted to identify potential biomarkers related to treatment response and long-term outcomes.
References
Song, W. J., Lee, J. H., Kang, Y., Joung, W. J. & Chung, K. F. Future risks in patients with severe asthma. Allergy Asthma Immunol. Res. 11, 763–778 (2019).
Lee, J. H. et al. Clinical characteristics and disease burden of severe asthma according to oral corticosteroid dependence: real-world assessment from the Korean Severe Asthma Registry (KoSAR). Allergy Asthma Immunol. Res. 14, 412–423 (2022).
McGregor, M. C., Krings, J. G., Nair, P. & Castro, M. Role of biologics in asthma. Am. J. Respir. Crit. Care Med. 199, 433–445 (2019).
Maglio, A. et al. Severe asthma remissions induced by biologics targeting IL5/IL5r: results from a multicenter real-life study. Int. J. Mol. Sci. 24, 2455 (2023).
Salter, B., Lacy, P. & Mukherjee, M. Biologics in asthma: a molecular perspective to precision medicine. Front. Pharm. 12, 793409 (2021).
Ortega, H. G. et al. Severe eosinophilic asthma treated with mepolizumab stratified by baseline eosinophil thresholds: a secondary analysis of the DREAM and MENSA studies. Lancet Respir. Med. 4, 549–556 (2016).
Pavlidis, S. et al. “T2-high” in severe asthma related to blood eosinophil, exhaled nitric oxide and serum periostin. Eur. Respir. J. 53, 1800938 (2019).
Mukherjee, M. et al. Suboptimal treatment response to anti-IL-5 monoclonal antibodies in severe eosinophilic asthmatics with airway autoimmune phenomena. Eur. Respir. J. 56, 2000117 (2020).
Wechsler, M. E. et al. Effect of dupilumab on blood eosinophil counts in patients with asthma, chronic rhinosinusitis with nasal polyps, atopic dermatitis, or eosinophilic esophagitis. J. Allergy Clin. Immunol. Pr. 10, 2695–2709 (2022).
Radzikowska, U. et al. Omics technologies in allergy and asthma research: an EAACI position paper. Allergy 77, 2888–2908 (2022).
Kuo, C. S. et al. T-helper cell type 2 (Th2) and non-Th2 molecular phenotypes of asthma using sputum transcriptomics in U-BIOPRED. Eur. Respir. J. 49, 1602135 (2017).
Park, H. W. & Weiss, S. T. Understanding the molecular mechanisms of asthma through transcriptomics. Allergy Asthma Immunol. Res. 12, 399–411 (2020).
Vieira Braga, F. A. et al. A cellular census of human lungs identifies novel cell states in health and in asthma. Nat. Med. 25, 1153–1163 (2019).
Tang, W. et al. Single-cell RNA-sequencing in asthma research. Front. Immunol. 13, 988573 (2022).
Lee, J. H. et al. Precision Medicine Intervention in Severe Asthma (PRISM) study: molecular phenotyping of patients with severe asthma and response to biologics. ERJ Open Res. 9, 00485–02022 (2023).
Zheng, G. X. et al. Massively parallel digital transcriptional profiling of single cells. Nat. Commun. 8, 1–12 (2017).
Bais, A. S. & Kostka, D. scds: computational annotation of doublets in single-cell RNA sequencing data. Bioinformatics 36, 1150–1158 (2020).
Hao, Y. et al. Integrated analysis of multimodal single-cell data. Cell 184, 3573–87. e29 (2021).
Wickham, H., Chang, W. & Wickham, M. H. Package ‘ggplot2’. Create elegant data visualisations using the grammar of graphics. Version 2, 1–189 (2016).
Chen, E. Y. et al. Enrichr: interactive and collaborative HTML5 gene list enrichment analysis tool. BMC Bioinform. 14, 1–14 (2013).
Jin, S. et al. Inference and analysis of cell‒cell communication using CellChat. Nat. Commun. 12, 1–20 (2021).
Chen, A. et al. Single-cell characterization of a model of poly I:C-stimulated peripheral blood mononuclear cells in severe asthma. Respir. Res. 22, 122 (2021).
Li, H. et al. Single-cell transcriptomic analysis reveals key immune cell phenotypes in the lungs of patients with asthma exacerbation. J. Allergy Clin. Immunol. 147, 941–954 (2021).
Büttner, C., Lun, A., Splettstoesser, T., Kunkel, G. & Renz, H. Monoclonal anti-interleukin-5 treatment suppresses eosinophil but not T-cell functions. Eur. Respir. J. 21, 799–803 (2003).
Bergantini, L. et al. Regulatory T cell monitoring in severe eosinophilic asthma patients treated with mepolizumab. Scand. J. Immunol. 94, e13031 (2021).
Lommatzsch, M. et al. Dupilumab treatment increases transitional B cells in severe asthma. Allergy 78, 2055–2057 (2023).
Niessen, N. M. et al. Neutrophilic asthma features increased airway classical monocytes. Clin. Exp. Allergy 51, 305–317 (2021).
Muehling, L. M., Lawrence, M. G. & Woodfolk, J. A. Pathogenic CD4(+) T cells in patients with asthma. J. Allergy Clin. Immunol. 140, 1523–1540 (2017).
Borthwick, L. A. The IL-1 cytokine family and its role in inflammation and fibrosis in the lung. Semin. Immunopathol. 38, 517–534 (2016).
Zhou, Z. et al. Single-cell profiling identifies IL1B(hi) macrophages associated with inflammation in PD-1 inhibitor-induced inflammatory arthritis. Nat. Commun. 15, 2107 (2024).
Singh, P. & Ali, S. A. Multifunctional role of S100 protein family in the immune system: an update. Cells 11, 2274 (2022).
Sprenkeler, E. G. G. et al. S100A8/A9 is a marker for the release of neutrophil extracellular traps and induces neutrophil activation. Cells 11, 236 (2022).
Schuliga, M. NF-kappaB signaling in chronic inflammatory airway disease. Biomolecules 5, 1266–1283 (2015).
Gagliardo, R. et al. Persistent activation of nuclear factor-kappaB signaling pathway in severe uncontrolled asthma. Am. J. Respir. Crit. Care Med. 168, 1190–1198 (2003).
Wilson, S. J., Wallin, A., Della-Cioppa, G., Sandström, T. & Holgate, S. T. Effects of budesonide and formoterol on NF-kappaB, adhesion molecules, and cytokines in asthma. Am. J. Respir. Crit. Care Med. 164, 1047–1052 (2001).
Hancox, R. J., Stevens, D. A., Adcock, I. M., Barnes, P. J. & Taylor, D. R. Effects of inhaled beta agonist and corticosteroid treatment on nuclear transcription factors in bronchial mucosa in asthma. Thorax 54, 488–492 (1999).
Auphan, N., DiDonato, J. A., Rosette, C., Helmberg, A. & Karin, M. Immunosuppression by glucocorticoids: inhibition of NF-kappa B activity through induction of I kappa B synthesis. Science 270, 286–290 (1995).
Nikolskii, A. A. et al. Role of STAT3 transcription factor in pathogenesis of bronchial asthma. Biochemistry 86, 1489–1501 (2021).
Zhang, Y. et al. IL33/ST2 contributes to airway remodeling via p-JNK MAPK/STAT3 signaling pathway in OVA-induced allergic airway inflammation in mice. Exp. Lung Res. 45, 65–75 (2019).
Zhang, X. & Köhl, J. A complex role for complement in allergic asthma. Expert Rev. Clin. Immunol. 6, 269–277 (2010).
Borrelli, C., Gurtner, A., Arnold, I. C. & Moor, A. E. Stress-free single-cell transcriptomic profiling and functional genomics of murine eosinophils. Nat. Protoc. 19, 1679–1709 (2024).
Acknowledgements
This research was supported by the Bio & Medical Technology Development Program of the National Research Foundation (NRF) funded by the Korean government (MSIT) (2019M3E5D3073365).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Park, K., Lee, JH., Shin, E. et al. Single-cell RNA sequencing reveals transcriptional changes in circulating immune cells from patients with severe asthma induced by biologics. Exp Mol Med 56, 2755–2762 (2024). https://doi.org/10.1038/s12276-024-01368-y
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s12276-024-01368-y