Abstract
Phototherapy offers advantages of non-invasiveness, cost-effectiveness, localized treatment, and potential for home-based care across various medical conditions. However, its adoption is hindered by the large size, limited safety, and professional operation requirements of current phototherapeutic devices. Unlike bulky laser phototherapeutic devices, wearable and implantable LED-based devices overcome these limitations, offering improved safety, portability, and uniform light distribution, making them promising prototypes for next-generation phototherapies. This review explores the home-care potentials of phototherapy from a clinical application perspective and provides a comprehensive overview of its therapeutic mechanisms and diverse applications. By synthesizing the latest advancements and cutting-edge research, we identify key clinical challenges associated with wearable and implantable phototherapy devices and propose fundamental strategies to address these limitations, such as miniaturization, biocompatibility, and energy efficiency. Furthermore, we draw on interdisciplinary cutting-edge research to address the challenges faced by phototherapy devices. We also emphasize the critical value of integrating artificial intelligence (AI) and flexible sensing technologies within phototherapy systems. Specific methods and potential applications are discussed for effectively integrating phototherapy systems with AI algorithms to establish a closed-loop diagnostic and therapeutic system. Grounded in clinical applications, we outline concrete research directions for developing next-generation LED-based phototherapy devices. This review delivers valuable insights for clinicians leveraging phototherapy and offers a roadmap for researchers in material science, flexible electronics, and AI, fostering interdisciplinary innovations to advance future phototherapy applications.

Similar content being viewed by others
Introduction
The application of phototherapy dates back 3500 years, when ancient Egyptians and other civilizations along the Nile River combined medicinal plants with sunlight to treat vitiligo1. In the late 19th century, sunlight was found to have therapeutic effects on anthrax and rickets. In the early 20th century, Niels Ryberg Finsen utilized artificial light sources to treat cutaneous tuberculosis (lupus vulgaris), earning the Nobel Prize in Physiology or Medicine in 19032. In 1960, Dr. Maiman developed the solid-state laser and performed the first retinal tumor surgery using laser technology3. Due to its high brightness, monochromaticity, and directionality, laser therapy has been widely applied in treating pigmented disorders4, tumors5, scars6, infections7, vascular malformations4, and ophthalmic surgeries8. An important development occurred in photomedicine in 1983 when Rox Anderson introduced the concept of selective photothermolysis9. Building on its historical foundation, phototherapy has evolved into a diverse and versatile field, leveraging various light wavelengths for specific therapeutic applications.
Each segment of the electromagnetic spectrum offers distinct biological effects and clinical advantages based on its unique energy, frequency, and wavelength (Fig. 1a). In the gamma-ray range ( < 0.01 nm), high-energy radiation targets tumors in radiotherapy10, while X-rays (0.01 ~ 10 nm) are used for diagnostic imaging11. Ultraviolet (UV) light (10 ~ 400 nm) addresses skin conditions and tumors12. Blue light (450 ~ 490 nm) is used for antibacterial therapy7 and neonatal jaundice treatment13, while green light (495 ~ 570 nm) aids in retinal therapy14 and pain relief15. Yellow light (570 ~ 590 nm) enhances immune function and improves mood16, and red light (620 ~ 750 nm) promotes wound healing17, hair growth18, and deep-tissue phototherapy19. Near-infrared lights (NIR, 700 ~ 2500 nm), particularly 808 and 980 nm, are effective for pain management, and technologies like functional near-infrared spectroscopy are used for tissue imaging20. Mid-infrared lights (2500 ~ 25,000 nm) include CO₂ lasers (10,600 nm) for surgical procedures21, while far-infrared lights ( > 25,000 nm) generate thermal effects for conditions like arthritis22 (Fig. 1a).
Phototherapy and the underlying mechanisms. a Introduction of light. The electromagnetic spectrum illustrates the distribution of electromagnetic waves across various wavelengths. The enlarged section corresponds to the ultraviolet, visible, and infrared regions, which are the primary wavelengths used in phototherapy applications. b Schematic representation of the main mechanisms involved in phototherapy, including optogenetics24, photobiomodulation27, photodynamic therapy30, and blue light therapy13. Optogenetics activates light-sensitive proteins, such as channelrhodopsin-2 (ChR2), allowing significant cation influx, particularly Na+, through ion channels, leading to depolarization and neuronal excitation. Photobiomodulation employs red and near infrared (NIR) light to activate cytochrome C oxidase (CCO) in the mitochondrial electron transport chain, enhancing ATP synthesis and reducing oxidative stress while upregulating signaling molecules such as nitric oxide (NO) and calcium ions (Ca2+). ATP, adenosine triphosphate. Photodynamic therapy uses light of specific wavelengths to activate photosensitizers (PSs), generating reactive oxygen species (•OH, •O2-, and 1O2) to eliminate cancers and pathogens. Blue light phototherapy enhances bilirubin absorption in the skin, converting it into water-soluble lumirubin, which is excreted from the body without hepatic metabolism. c Representative applications of diseases treated with phototherapy and their corresponding research references: encephalopathy25,49,50,51, ophthalmopathy37, anti-cancer58,150,165,166,167, neonatal jaundice13, spinal-cord injury52, peripheral nerve modulation53,54, thrombocytopenia168, hair loss18, cosmetic dermatology31, anti-bacterial7,169,170, heart disease19,41,42, diabetes43,44,45,46,47, bladder pain syndrome48, wound healing17,34, and diabetic foot ulcer35,36. Figure 1, created with BioRender.com, released under a Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International license
The phototherapeutic mechanisms primarily rely on several pathways (Fig. 1b). Optogenetics23 is a technique that allows precise control of neural activity and cellular functions through the activation of specific light-sensitive proteins, including ChR2, enhanced bacteriorhodopsin, natronomonas pharaonis halorhodopsin, and the like24. When exposed to a 473 nm blue light, ChR2 channels open, allowing a significant influx of cations like Na+, leading to depolarization and subsequent neuronal excitation25. This mechanism enables precise regulation of neuronal and cellular functions, making optogenetics a powerful tool widely used in neuroscience and biomedical research (Fig. 1b). Photobiomodulation (PBM)26, previously referred to as low-level laser therapy (LLLT), typically employs red and NIR (600 ~ 980 nm) to activate the rate-limiting enzyme cytochrome C oxidase (CCO) in the mitochondrial electron transport chain. This activation enhances ATP synthesis and reduces oxidative stress while upregulating signaling molecules such as nitric oxide (NO) and calcium ions (Ca2+). Consequently, a cascade of downstream signaling pathways is triggered, resulting in the regulation of cellular physiological functions27 (Fig. 1b). Photodynamic therapy (PDT)28,29 uses light of a specific wavelength to activate photosensitizers (PSs), generating reactive oxygen species (•OH, •O2-, and 1O2) to eliminate cancers and pathogens30. Blue light phototherapy, utilizing the wavelength of 400 ~ 470 nm, facilitates the absorption of light energy by bilirubin molecules in the skin and converts it into water-soluble isomers, such as lumirubin. These isomers can be excreted from the body without requiring hepatic metabolism13 (Fig. 1b). These mechanisms underpin the therapeutic efficacy of phototherapy across diverse medical scenarios.
Current phototherapy has been successfully applied to several major human organs, including skin, nervous, circulatory, urinary, musculoskeletal, and digestive systems (Fig. 1c, Table 1). Due to the limited penetration of light, phototherapy is primarily focused on the body surface, such as hair loss18, dermatological diseases31,32,33, wound healing17,34, chronic wound management35,36, ophthalmopathy37, and neonatal jaundice13,38 (Fig. 1c, Table 1). Such devices are designed to fit the body surface (e.g., skin, mucous membranes) and deliver light energy to superficial tissues, as well as areas that can be penetrated by external light sources, such as subcutaneous capillaries and the cerebral cortex. The therapeutic targets are typically located in the epidermis, dermis, shallow subcutaneous layers, or areas that can be penetrated by near-infrared light, typically up to 3–5 cm beneath the skin39. Since they deliver light to the target area without requiring surgical intervention, these devices are clinically defined as wearable phototherapy devices. For instance, Sahel et al.37 injected an adeno-associated viral vector encoding ChrimsonR into the eye, to facilitate partial vision restoration in a blind patient through the combined use of optogenetics and phototherapy goggles (Fig. 1c). Additionally, the face-fit surface-lighting micro light-emitting diodes (micro-LED) mask developed by Kim et al.31 conforms to complex facial contours, giving rise to significant improvement in facial elasticity, sagging, and wrinkles (Table 1). Analogously, the textile-based blue organic light-emitting diodes (OLEDs) developed by Choi et al.13 balance comfort and therapeutic efficacy, enabling at-home treatment for neonatal jaundice (Fig. 1c). Recently, we fabricated a stretchable red and blue LED (r&bLED) patch36, which potentially offers a convenient antibacterial and wound-healing facilitation for managing chronic infectious wounds at home (Fig. 1c). Furthermore, a randomized controlled trial validated the efficacy of LLLT in the treatment of traumatic brain injury. Among 68 randomly assigned patients, 33 patients received NIR light therapy using a custom LED-helmet within 72 h post-injury, while 35 patients received sham treatment as controls. The results demonstrated statistically significant changes in multiple brain diffusion tensor imaging parameters during the subacute phase39.
To date, researchers are devoting enormous efforts to overcoming the challenges of delivering light to deeper tissues40, with the ultimate goal of expanding the applicability of phototherapy. Among them, fiber-optic and implantable LED devices are being developed to treat heart diseases19,41,42, diabetes43,44,45,46,47, bladder pain syndrome48, encephalopathy25,49,50,51, spinal cord injuries52, and neurological disorders53,54 (Fig. 1c, Table 1). These devices require implantation through natural body cavities (e.g., gastrointestinal tract, oral cavity, nasal cavity), minimally invasive procedures, or open surgery, to make direct contact with or be placed near deeper tissues, enabling precise light energy delivery. From a clinical application perspective, these devices are commonly referred to as implantable phototherapy devices. For example, Ausra et al.42 customized a soft, thin-film micro-LED array that enabled high spatiotemporal precision for optogenetic stimulation delivery, facilitating cardiac pacing and defibrillation when implanted in vivo (Fig. 1c). Additionally, the combination of µLED implants with optogenetically modified neurons expressing channelrhodopsin-2 (ChR2) allows for facile neural modulation within the body25,46,48,52,53 (Table 1). Kim et al.55 developed an implantable multi-LED array that ensures stable contact with the target cortical region and skull for PBM therapy (Table 1). Their studies demonstrated that 630 nm red light effectively reduced infarct volume and neuronal damage following ischemic stroke. Besides, Kathe et al.52 developed a µLED system capable of conforming to the dura mater of the spinal cord. Using an optogenetic model of spinal cord injury in mice, they integrated a physiological signal sensing module with a phototherapy module to achieve closed-loop control of spinal cord neurons. This innovative approach effectively addressed challenges associated with spinal-cord injuries (Fig. 1c, Table 1).
Over the past five years, the development of wearable and implantable phototherapy devices has accelerated significantly, with their effectiveness in treating various diseases being well demonstrated. Despite significant advancements, wearable and implantable phototherapy devices still face several challenges. Different diseases require specific parameters (wavelength, power density, and exposure duration) yet current devices often lack the precision and monitoring system to meet diverse clinical needs. Long-term comfort, biocompatibility, and energy supply also require optimization. Furthermore, improving therapeutic efficiency, expanding applications, and reducing costs in complex clinical settings remain pressing issues. Addressing these technical bottlenecks and aligning devices with clinical requirements is essential for advancing this field.
Challenges and unmet clinical needs in phototherapy devices
As previously mentioned, researchers classify LED phototherapy devices into wearable and implantable categories from the perspective of clinical applications. The choice between wearable or implantable phototherapy strategies depends on factors such as the depth of the target tissue40, the nature of the disease, and whether anatomical barriers28 (e.g., bone structures, dense fascia) need to be crossed, as well as the need for precise spatial localization56 (Fig. 2a, b). Wearable devices do not require surgical intervention, providing higher patient compliance; however, they face limitations in addressing the phototherapy of deeper tissues. Implantable phototherapy devices, on the other hand, help overcome the challenge of delivering light to deeper organs and can enable precise phototherapy (e.g., optogenetic control of bladder afferent nerves48) (Fig. 2a, b). However, both types face numerous technical and clinical challenges necessitating efforts to improve therapeutic efficacy and user experience. From the perspective of clinical phototherapy applications, wearable devices require excellent portability, personalized phototherapy capabilities, uniform light distribution, and conformity to the contours of the body surface to enhance therapeutic efficacy (left, Fig. 2). In addition to these requirements, implantable phototherapy devices must meet challenges such as energy supply, device longevity, encapsulation leakage, biocompatibility, and so on (right, Fig. 2).
Challenges in wearable and implantable phototherapy devices. a Wearable phototherapy devices for superficial tissues, emphasizing portability, personalization, and energy supply. b Implantable phototherapy devices for deep tissues, focusing on precise localization, energy supply, and biocompatibility. Challenges of wearable phototherapy devices in clinical applications: c Lack of portability32,33. d Inadequate personalization to meet individual needs57. e Insufficient uniformity of illumination from current light source devices, including traditional light source and LED array17,19 (reprinted with permission32. Copyright 2021, John Wiley & Sons). f Poor conformity of wearable devices31, including issues with joint mobility, sophisticated body surface fit, and lack of comfortability. Challenges of implantable phototherapy devices in clinical settings: g Traditional batteries as power sources raise concerns about implantation and limited functional time48,58. h Device lifespan is constrained by light output attenuation and rupture43.i Encapsulation may fail due to stretching-induced fractures or erosion from acids or enzymes, leading to leakage. j Biocompatibility is limited by heavy metal toxicity from batteries, in vivo corrosivity, and foreign body reactions25. Figure 2, created with BioRender.com, released under a Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International license
Challenges in wearable phototherapy devices
First, insufficient portability of phototherapeutic devices significantly limits their usage scenarios (Fig. 2c). Phototherapy devices for skin diseases are often large and cumbersome, making them unsuitable for home use by patients33. In comparison, Zhang et al.32 developed a compact phototherapy device designed for skin treatment. Its enhanced portability enables patients to undergo treatment conveniently at any time, thereby improving therapeutic outcomes. Secondly, current phototherapy devices lack personalized and precise treatment capabilities (Fig. 2d). For instance, managing symptoms in epilepsy patients often relies on preventive medication or optogenetic-based phototherapy57. If a system could accurately predict epileptic episodes based on the patient’s physiological data and changes in brainwave patterns, timely interventions could significantly improve outcomes. Addressing this challenge is essential for future wearable phototherapy devices to enhance therapeutic efficacy and improve patient compliance. Thirdly, the uniformity of light exposure in phototherapy devices is a critical factor influencing therapeutic outcomes (Fig. 2e). Laser-based point light sources often lead to uneven light intensity, resulting in variable efficacy between central and peripheral regions19. Researchers have explored LED array configurations to enhance light uniformity; however, insufficient illumination persists in the gaps between LEDs17. Moreover, irregular surface geometries in the target illumination area further compromise the effectiveness of phototherapy (Fig. 2f). For instance, the high mobility of human joints makes conventional rigid phototherapy devices incompatible with joint movements, preventing effective therapy during motion. Similarly, the complex anatomical structures of the face and periorbital regions, coupled with significant inter-individual variability, pose challenges to achieving uniform light distribution31. Apparently, improving phototherapy devices to achieve better illumination uniformity, enhanced portability, and greater adaptability to body surface contours is a critical challenge that must be addressed to enhance therapeutic efficacy (Fig. 2c–f).
Challenges in implantable phototherapy devices
Due to the limited penetration depth of light, its delivery directly to internal tissues remains formidable challenges for wearable devices52. On the other hand, implanted phototherapy systems pose unique energy supply challenges, as their batteries not only face implantation difficulties but also present potential biosafety concerns (Fig. 2g). Key considerations include battery size, energy density, and biocompatibility. Mickle et al.48 demonstrated wireless power transfer for optogenetic therapy; however, the required coils were bulky and could only power a limited number of LEDs. In contrast, Yamagishi et al.58 employed a self-powered approach for high-power PDT, but challenges remain in effectively covering large treatment areas. Apparently, engineering a biocompatible, safe, and optimized energy supply tailored to the specific requirements of implantable phototherapy systems is crucial for advancing their functionality and therapeutic potential. Moreover, implantable phototherapy devices must contend with the harsh physicochemical environment. Sim et al.43 demonstrated the use of OLED-based phototherapy devices implanted in the small intestine for diabetes treatment. However, the vulnerability of OLED materials to water and oxygen degradation severely limits the duration of effective phototherapy (Fig. 2h). To address this issue, dense and biocompatible encapsulation techniques are required to ensure device longevity. Nevertheless, overly thick encapsulation materials can compromise light intensity and device flexibility, while excessively thin encapsulation increases the risk of harmful material leakage, raising safety concerns (Fig. 2i). Enhancing the durability of light-emitting materials and improving encapsulation quality are critical challenges for advancing implantable phototherapy devices. Most importantly, as implantable devices, phototherapy systems must ensure robust biocompatibility and safety (Fig. 2j). Materials used in batteries, light-emitting components, encapsulation layers, and conductive elements may contain metals or corrosive materials that can trigger metal toxicity, corrosive reactions, or immune-mediated foreign body responses. Kim et al.25 addressed these challenges by developing a flexible OLED-based phototherapy device using a soft substrate and xylene film encapsulation. This approach minimized mechanical damage to neural tissues while effectively reducing the risk of immune rejection associated with implanted devices. Besides the biocompatibility of materials, heat generated during phototherapy and by the electronic components may cause thermal damage59. Therefore, effective heat dissipation design is also crucial (Fig. 2j).
From the perspective of clinical phototherapy applications, future LED phototherapy devices must achieve comprehensive advancements to address the aforementioned challenges. This will require the development of novel conductive materials, light-emitting materials, encapsulation materials, and batteries, as well as advancements in manufacturing processes. Addressing these issues represents a complex interdisciplinary endeavor. In the following sections, we will propose specific strategies and highlight cutting-edge research aimed at overcoming these challenges. Additionally, we will summarize the design principles and fabrication workflows for next-generation LED phototherapy devices.
Strategies to overcome challenges in phototherapeutic prototypes
As phototherapy technologies continue to advance in the medical field, innovations in material science and fabrication technologies have established a robust foundation for addressing technical challenges and achieving substantial improvements in device performance. Incorporating the latest advancements and clinical needs identified by phototherapy specialists, our research team has reviewed and proposed targeted strategies to tackle the current limitations of phototherapy devices. These strategies focus on enhancing light distribution uniformity, advancing device miniaturization, improving implantability, integrating diagnostic and therapeutic functionalities, and enabling the intelligent modulation of phototherapy parameters.
Strategies to improve illumination uniformity
Zhang et al.60 demonstrated the use of OLED technology to achieve surface light emission, resulting in improved illumination uniformity and enhanced phototherapy efficacy. QLED materials, which are compatible with the same fabrication processes as OLEDs, were utilized by Bian et al.61, who employed spin-coating and thermal evaporation deposition techniques to produce QLED devices capable of uniformly emitting high-intensity green light. Similarly, Kim et al.31 utilized µLED technology, achieving comparable uniformity in light distribution with notable improvements in therapeutic outcomes. Lee et al.62 introduced a diffusion layer, such as SiO₂, and Deng et al.19 employed fiber optic lenses, enabling phototherapy devices with initially uneven illumination to achieve significantly more uniform light distribution (Fig. 3a). This design significantly reduces the risk of localized burns caused by uneven illumination while enhancing the effectiveness of treatment for large lesions, particularly in anatomically complex areas such as the face62, joints63 and curved body surfaces36,64.
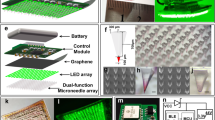
Advanced strategies to address challenges in clinical applications of phototherapy. a Enhance the uniform illumination of phototherapy via OLED60, micro-LED31, diffuser layer62, and optical lens19 technologies. b Achieving miniaturization of the overall device through effective integrated circuits52, flexible materials34, and modular design. c By selecting biocompatible materials, employing appropriate encapsulation strategies, ensuring the mechanical compatibility of flexible phototherapy devices with tissues, and optimizing energy supply solutions, the implantability of phototherapy devices can be enhanced (the image for structural design is reprinted with permission75. Copyright 2023, Nonferrous Metals Society of China. The image for active refrigeration is reprinted with permission76 under Creative Common CC BY license. Copyright 2022, John Wiley & Sons). d Realizing theranostic integration by monitoring relevant electrochemical79, spectroscopic67,140,163, and bioelectric signals80. e Employing AI to intelligently integrate detection information and output suitable phototherapy parameters57. Figure 3, created with BioRender.com, released under a Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International license
Strategies for miniaturization of phototherapy devices
Miniaturization technologies are key to realizing wearable and implantable phototherapy devices (Fig. 3b). Through efficient integrated circuit designs and modular structures, the size and weight of devices have been substantially reduced. In this regard, Li et al.36 designed a phototherapy patch comprising a phototherapy module, sensing module, power supply module, and Bluetooth/Wi-Fi module, significantly enhancing the portability and usability (Fig. 3b). The use of soft materials further enables the device to closely conform to the human body, ensuring effective illumination in complex curved areas such as joints, thereby enhancing both comfort and therapeutic results65. Additionally, soft materials allow for further miniaturization of the device66, making it more suitable for wearable or implantable phototherapy applications.
Strategies to enhance implantability of phototherapy devices
For implantability55, optimizing material selection and encapsulation technologies are crucial to ensuring both performance and biosafety. Additionally, the mechanical properties of the implantable phototherapy device and their compatibility with the target organ41,67, along with the choice of energy supply method41, are equally crucial to the design of implantable phototherapy devices (Fig. 3c). The use of biocompatible materials, such as hydrogels, flexible polymers, and biocompatible metals, significantly reduces the risks of inflammation and immune rejection68. Multilayer encapsulation technologies (including both inorganic and organic layers) preserve device stability under extreme in vivo conditions, such as high humidity, acidity, and oxygen levels, while preventing leakage of harmful substances69. Furthermore, by adjusting the Young’s modulus and tensile strength of device materials to align with the mechanical properties of human tissues, potential biosafety issues post-implantation can be minimized. Ideally, the device’s overall Young’s modulus should be lower than that of the target tissue, while its tensile strength should exceed that of the tissue70. Additionally, depending on the device’s expected in vivo residence time, solutions such as soft batteries70, micro-batteries71, wireless power48, or energy harvesting methods58 can be employed to address energy supply challenges (Fig. 3c). Thermal management is critical for implantable phototherapy devices. For low level light power therapies, such as PBM43 or optogenetics52, passive heat transfer via body tissues suffices to maintain safe temperatures. However, high level light power applications like PDT require effective thermal management. Pulsed light therapy72,73 can control heat generation while maintaining efficacy. Flexible thermal conductive materials74, optimized heat dissipation structures75,76, and micro cooling plates77 enable passive and active cooling, ensuring the device stays within safe temperature ranges, thus enhancing performance and biosafety (Fig. 3c).
Strategies for integrating monitoring, AI and phototherapy
The integration of therapeutic and diagnostic capabilities represents a critical advancement in phototherapy devices (Fig. 3d). By incorporating electrochemical sensors78 and spectroscopic analysis modules79, these devices can monitor biochemical indicators such as glucose, urea, and pH levels, alongside hemodynamic parameters like blood oxygen saturation and tumor markers. Additionally, integrating bioelectric signal monitoring80, including electrocardiograms (ECG), electroencephalograms (EEG), and electromyograms (EMG), provides comprehensive physiological data to support personalized diagnosis and treatment (Fig. 3d). Leveraging intelligent adjustment technologies, phototherapy devices can now dynamically optimize treatment parameters based on patients’ real-time conditions (Fig. 3e). Using multimodal deep learning algorithms57, these devices analyze physiological indicators, biochemical markers, and behavioral data to intelligently adjust parameters such as wavelength, light intensity, and exposure duration. This closed-loop system enhances phototherapy efficiency, reduces reliance on medical professionals, and facilitates home-based applications, paving the way for improved therapeutic outcomes and broader usability.
Based on cutting-edge research, we propose the aforementioned strategies from a clinical perspective to address these challenges in phototherapy. In the following sections, we will elaborate on the implementation of these strategies through advancements in multidisciplinary research and discuss their specific impact on enhancing the phototherapy application.
Cutting-edge technologies and future processes
1. Advances in the development of LED phototherapy devices
To address the challenges of performance and applicability in LED phototherapy devices, researchers have introduced a variety of innovative strategies through material selection and process optimization. Significant progress has been made in areas such as soft substrates, soft active materials, soft emissive layers, soft encapsulations, and power supplies.
Soft substrate
The soft substrate is critical for determining the mechanical properties of phototherapy devices and ensuring compatibility with target tissues (Fig. 4a). An ideal substrate, as summarized in the table shown in Fig. 4a, should have a lower Young’s modulus than the target tissue while providing sufficient tensile strength, high-temperature resistance, chemical stability, and stretchability. Polyimide (PI) is well-suited for wearable and implantable devices due to its thermal and mechanical properties17, while softer, biocompatible materials like Polydimethylsiloxane (PDMS)32, Thermoplastic Polyurethane (TPU)36, Styrene-Ethylene-Butylene-Styrene81 (SEBS), and Ecoflex82 are preferable for dynamic areas. Tailoring substrate selection to specific applications enables optimal adaptation to target regions. For example, wrapping the spinal cord for optogenetic therapies in paralysis treatment52, conforming to the body surface for blue-light therapy in jaundice management13, or adhering to the intestinal lining for red-light therapy applications43 (Fig. 4a).
Key progresses and innovations in processes and materials. a The ideal properties required for soft substrates and representative applications in nervous system (reprinted with permission52. Copyright 2022, Springer Nature)52, body surface13, and gastrointestinal tract (reprinted with permission43 under Creative Common CC BY license. Copyright 2023, American Association for the Advancement of Science)43. b Soft active materials, including metal thin films (the left image is reprinted with permission57. Copyright 2023, Springer Nature. The right image is reprinted with permission85. Copyright 2021, John Wiley & Sons)57,85, liquid metals (reprinted with permission86. Copyright 2023, American Association for the Advancement of Science)86,87,171, and conductive polymer materials (reprinted with permission89. Copyright 2023, Springer Nature)89, along with their associated fabrication processes such as spin coating, 3D printing, screen printing, inkjet printing, dispensing, and photolithography. c Soft emissive component including Micro-LED31 and OLED (reprinted with permission60. Copyright 2022, Springer Nature)60 (reprinted with permission105. Copyright 2020, Springer Nature). d Soft encapsulation: hybrid organic/inorganic multilayer69. e Heat dissipation design: flexible thermal materials, external control module72,73, boron nitride nanoseed structure74, and microchannels77 for enhanced heat management. (reprinted with permission74 under Creative Common CC BY license. Copyright 2020, Springer Nature) f Power supply including soft battery (the middle image is reprinted with permission122 under Creative Common CC BY license. Copyright 2024, Springer Nature. The right image is reprinted with permission148. Copyright 2022, Springer Nature)120,121,122 wireless power supply123,124,125,126 (the image for RF antenna is reprinted with permission77. Copyright 2020, Springer Nature. The image for Infrared light is reprinted with permission125. Copyright 2018, National Academy of Sciences). Figure 4, created with BioRender.com, released under a Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International license
Soft active materials
In the fabrication of wearable or implantable phototherapy devices, soft active materials (Fig. 4b) should exhibit essential characteristics such as high electrical conductivity, stretchability, low cost, compatibility with diverse fabrication processes, biocompatibility, and durability. These requirements are designed to ensure that phototherapy devices maintain efficient optical power output to meet therapeutic needs while preserving stretchability.
Metal thin films are commonly used in device circuits due to their high conductivity and cost-effectiveness. They have been applied in optogenetic modulation for epilepsy57, phototherapeutic repair of cerebral infarction55, antimicrobial treatments for implant infections83, and red-light therapy for hair loss18. Structural optimization ensures their flexibility and mechanical stability. Current research mainly focuses on techniques such as serpentine patterns57, island-bridge structures84, or metal cracks85 to enhance their tensile strength. However, these approaches often significantly increase the device’s volume, which hinders miniaturization. Therefore, intrinsically stretchable materials such as liquid metals and polymers are better suited for future phototherapy devices. For instance, liquid metal materials, celebrated for their self-healing properties and exceptional ductility, are especially well-suited for dynamic applications86, such as treating arthritis, adapting to the beating surface of the heart19,41, and addressing urinary dysfunction through optogenetic modulation in response to bladder pressure changes48. Encapsulating liquid metals in elastomers can further improve their stretchability87,88. Furthermore, the liquid metal’s inherent chemical stability and the hermetic sealing design effectively address the challenges of oxidation, ensuring long-term performance and reliability in stretchable systems86. Conductive polymers, which offer good stretchability and low cost, are another promising option. Although they are susceptible to water and oxygen degradation, surface molecular modifications can significantly enhance their durability89, while maintaining good electrical conductivity (Fig. 4b). Many novel soft active materials can meet these requirements but are limited by their thermal tolerance, making them unsuitable for high-temperature processing. Consequently, the development of low-temperature fabrication techniques offers a pathway to expand the applications of these advanced materials. Cutting-edge processing methods currently include spin coating90, 3D printing91, screen printing92, inkjet printing93, dispensing printing, and photolithography94 (Fig. 4b).
Soft emissive components
The light sources used in flexible LED-based phototherapy devices can be classified into three main types: µLEDs, OLED, and QLEDs. µLEDs31,52,95 offer high light intensity ( ~ 1,000,000 nits), long lifespan ( ~ 100,000 h), and a narrow FWHM (15–20 nm), but have limitations in heat dissipation, flexibility, and light uniformity compared to OLED13,25,43 and QLED61,96,97. OLED-based devices require further enhancement in brightness and resistance to oxygen and moisture98,99, while QLEDs need to improve stability, ensuring no heavy metal incorporation61,100 (Table 2). To address these challenges, researchers have proposed various strategies.
In the field of soft emission components, µLEDs/Micro-LED have become a focal point due to their high brightness, dense emission, and exceptional precision, making them the ideal selection for phototherapy device101 (Fig. 4c, Table 2). The challenge of transferring µLEDs onto flexible substrates102 has been effectively resolved with advanced laser transfer technologies31. With decreasing costs, flexible µLEDs show great promise as phototherapy light sources, particularly for complex surfaces like the face18,31,34, intestines43, brain52,55, heart19, and lungs103.
At the same time, OLED materials, conferring flexibility, low-temperature fabrication, and uniform light emission (Table 2), are already being applied in areas such as diabetic management43, hyperbilirubinemia treatment13,38, hemodynamic monitoring60, and neuroregulation25. However, their limited lifespan under high-intensity illumination constrains their broader use in phototherapy devices. While photobiomodulation and metronomic photodynamic therapy (PDT) can achieve therapeutic effects at lower light intensities, simultaneous improvements in brightness and durability are essential to extend OLED applications to a wider range of therapies, including photodynamic and photothermal treatments. Encouragingly, advances in thin-film packaging technologies are now effectively addressing these issues104. In parallel, new OLED optimization strategies, such as incorporating special solvents to dilute and reduce defects in the regions where electrons are captured within the OLED structure, along with the use of the double-sided polariton-enhanced Purcell effect to improve OLED stability, are further enhancing the light emission efficiency and lifespan of OLEDs60,98,99,105,106,107,108 (Fig. 4c). As detailed in Table 2, Red/Green (Phosphorescent) OLEDs exhibit lifespans exceeding ~100,000 h, while Blue OLEDs, especially the phosphorescent type, are showing ongoing improvements108,109. Remarkably, researchers have also achieved major breakthroughs in the fabrication of intrinsically stretchable OLEDs60,105,110, which currently represent the most stretchable light-emitting components developed to date.
QLEDs offer excellent flexibility, uniform surface emission, high light intensity ( > 300,000 nits), and narrow FWHM (20–30 nm)111,112 (Table 2). Current research focuses on developing biocompatible, heavy-metal-free (e.g., Cd-free) flexible QLEDs61,100. However, their limited stability and short lifespan remain significant challenges for phototherapy, with only a few studies addressing these issues112,113,114,115. New methods, such as electrically excited transient absorption (EETA)61, can effectively quantify the issues present in heavy-metal-free QLEDs. By optimizing the core-shell structure100 and surface passivation strategies116, it is possible to further enhance the luminous efficiency and stability, ensuring the biological safety of QLEDs (Fig. 4c).
Soft encapsulation
Encapsulation technologies also play a vital role in ensuring device stability. The ideal encapsulation should maintain the device’s stretchability, lightweight nature, and durability (Fig. 4d). Hybrid organic/inorganic multilayer encapsulation104,117 combines the gas-barrier properties of inorganic layers with the flexibility of organic layers, providing stability for phototherapy devices in extreme environments such as fluid-filled cavities like the abdominal and thoracic cavities, intracranial regions, and even the gastrointestinal tract, while minimizing the risk of toxic substance leakage—an essential consideration for implantable devices (Fig. 4d).
Heat dissipation design
LED phototherapy devices must address the potential side effects of heat generation during use. The skin’s outer layers, including the epidermis, dermis, and subcutaneous tissue, have low thermal conductivity (κ ≈ 0.3 W m−1 K−1)118, posing challenges for heat management. An ideal design integrates flexible thermal materials, efficient heat dissipation structures, and effective heat transfer mechanisms (Fig. 4e). In phototherapy, an effective strategy for preventing thermal damage is to transmit the LED light source via optical fibers while keeping the heat-generating control units external119. Metronomic PDT72,73, using low-dose, extended-duration, high-frequency light, reduces local thermal load accumulation and provides an effective heat management solution. This approach offers a viable strategy for addressing heat dissipation in PBM, optogenetics, and blue light therapy. However, further studies are needed to assess its applicability across other phototherapy strategies. Additionally, advanced thermal management designs, such as polymer/boron nitride nanosheets74 and miniaturized microchannel heat sinks77, offer potential solutions for enhancing heat dissipation in LED phototherapy devices (Fig. 4e).
Power supply
The power supply for phototherapy devices (Fig. 4f) plays a pivotal role in determining their functionality and application potential. An ideal power source should combine high energy density, soft, biocompatibility, and durability to meet the diverse demands of wearable and implantable phototherapy systems. Recent innovations in power systems have been driven by soft batteries and wireless power transfer technologies, enabling both device miniaturization and extended operational lifespans. Soft batteries have progressed significantly, making it possible to integrate them into textiles for wearable phototherapy devices, such as LED therapy patches designed to treat skin conditions like acne, wounds, and psoriasis120. Alternatively, they can be incorporated as miniaturized droplet121 or thin-film batteries122 in micro-sized phototherapy devices, allowing precise energy delivery for localized treatments. For implantable phototherapy devices, the choice of power source is dictated by the application. Solid-state batteries, with their ability to prevent toxic substance leakage, are better suited for long-term implantable systems. Wireless power transfer technologies, such as magnetic induction and triboelectric nanogenerators123 (TENGs), can harness kinetic energy from the human body to power implantable devices. These technologies expand the usability of phototherapy systems in scenarios requiring portability and frequent use. Additional methods, such as ultrasonic power124, infrared functionality125, and far-field communication (RF)126, present promising wireless energy options for implantable applications. These approaches are particularly advantageous for treatments requiring minimal device maintenance and long-term functionality. Despite these advances, phototherapy devices often demand substantial power for high-intensity light output, particularly in applications such as deep tissue treatment58 or PDT127. In these cases, wireless power solutions alone are insufficient to sustain real-time energy needs and they must be paired with integrated batteries to provide reliable energy storage. The careful selection and integration of power systems, tailored to the specific clinical context, ensures that phototherapy devices achieve optimal performance across a wide range of medical applications.
2. Future manufacturing processes for LED phototherapy devices
In response to the challenges currently faced by LED-based phototherapy devices in clinical applications, as well as recent advancements in the field, we present a universal fabrication process for future wearable/implantable LED phototherapy devices.
Selection of soft substrates
Selecting the appropriate soft substrate based on the intended application is a key step toward achieving device flexibility and stretchability (Fig. 5a). Textile-based substrates, with their breathability and softness, are particularly suitable for large-area treatment scenarios13, such as phototherapy garments for jaundice treatment, phototherapy knee braces for arthritis management, and phototherapy caps for promoting hair growth. Hydrogel substrates, known for their high biocompatibility and transparency, are preferred for devices in direct contact with the skin or organs70. Polymer substrates, which balance mechanical strength and flexibility, are better suited for highly deformable regions and implantable phototherapy devices. Current soft substrates face significant challenges in conforming to complex biological surfaces (e.g., brain gyri or joint folds). As shown in Fig. 4a (left), the elastic modulus of brain and lung tissues is an order of magnitude lower than that of common polymer substrates (PI, PET, PDMS, SEBS), and the grooves in regions like the brain and skin hinder full adhesion of flexible phototherapy devices, affecting treatment uniformity128. Flexibility is influenced by device thickness, Young’s modulus, and width66, with studies showing that a thickness of 10–100 μm ensures effective brain tissue adaptation129. Ultra-flexible nanoelectronics (<10 μm feature size, 1 μm thickness) can further reduce chronic inflammation130. Currently, phototherapy devices are often fabricated on polymer substrates, and researchers have employed various methods to optimize the interface compatibility with tissues. OLED and QLED devices have achieved thicknesses around 10 μm25,43,100, offering excellent flexibility, while micro-LEDs can enhance tissue and organ compatibility and phototherapy efficacy through substrate design (octopus’ structure)95.
Technical roadmap for integrating monitoring and treatment in future phototherapy devices. a Selecting appropriate soft substrates based on specific clinical applications (e.g., textile13,34, hydrogel70, polymer36). b Fabrication of the conductive layer utilizing low-temperature processing techniques90,93,172. c Fabrication methods for soft emissive component: laser-induced transfer for micro-LED31,62,133, spin coating60 or thermal evaporation173 for OLED. d Soft thin-film encapsulation using atomic layer deposition135. e Novel power supply methods: microbatteries71, flexible batteries120, wireless power supply174, and triboelectric nanogenerator123. f Feasible strategies for integrating phototherapy devices with sensors79,140. g Overall operational logic of future phototherapy devices. Figure 5, created with BioRender.com, released under a Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International license
Fabrication processes for electrodes
To address the temperature tolerance of new materials, low-temperature fabrication techniques are better suited for future LED phototherapy devices131 (Fig. 5b). Methods like inkjet and 3D printing enable precise fabrication of complex structures93 while optimizing conductive ink properties for multilayer flexible circuits. Spin-coating132 further improves the uniformity and optical performance of emissive layers with precise film thickness control (Fig. 5b).
Preparation of soft emissive components
The manufacturing processes for soft emission components are continuously optimized to improve efficiency and reduce costs (Fig. 5c). Laser-induced transfer technology enables high-precision and large-scale production of µLEDs133, making them one of the most promising solutions for future phototherapy applications. Meanwhile, thermal evaporation132 techniques and advanced spin-coating90 methods significantly enhance the luminous efficiency and lifespan of OLED and QLED devices by improving the fabrication of the emissive layer. When combined with elastomers, OLED60 and QLED134 devices exhibit enhanced stretchability and flexibility. Both of these light-emitting components can achieve ultra-uniform surface emission and meet the optical power requirements of phototherapy. Additionally, Surface-Mount Device LEDs can be directly integrated into phototherapy devices through soldering36 (Fig. 5c).
Soft thin-film encapsulation
To preserve the softness and thinness of future LED phototherapy devices, atomic layer deposition135 (ALD) (Fig. 5d) can sequentially deposit organic and inorganic layers, providing effective water and oxygen barriers. ALD’s self-limiting growth mechanism ensures smooth atomic surfaces and uniform nanoscale films, making it a promising approach for thin-film encapsulation69.
Energy supply methods
The power supply for future LED phototherapy devices should be tailored to specific application requirements (Fig. 5e). For wearable devices, rechargeable micro-batteries are ideal, offering extended use36 for applications such as acne, wounds, and psoriasis. Implantable devices for short-term applications may utilize high-energy-density micro-batteries or soft batteries, particularly for treating heart diseases, cancer, and deep tissue disorders. Long-term implantable devices require wireless power transfer systems to provide sustained energy supply. While wireless coils are commonly used, their size constraints limit achievable power levels and application scenarios. Alternative methods, including RF communication126, ultrasound124, infrared125, and energy harvesting technologies like piezoelectric nanogenerators136 or self-powered systems137, show potential but are insufficient for high-power phototherapy applications. However, their real-time power output often falls short of the demands of high-intensity phototherapy applications, necessitating battery storage to ensure a reliable and continuous energy supply.
Integration of sensing modules
The integration of sensors is pivotal for enhancing the intelligence of phototherapy devices (Fig. 5f). Electrodes for electrochemical and electrophysiological sensors are typically patterned using laser engraving138, with functional materials deposited to enable targeted data collection139. Photoelectric detectors, based on spectroscopic principles, are fabricated similarly to LED emissive materials68, while pre-packaged detectors can be soldered directly onto flexible circuits140. As shown in Fig. 5g, the design of future phototherapy devices incorporates micro-processing chips that collect sensor data and use built-in algorithms to dynamically adjust treatment parameters in real time. Sensors monitoring parameters such as tissue oxygen levels, skin temperature, and light absorption enable real-time feedback and optimization of therapy, ensuring maximum efficacy tailored to specific clinical conditions.
Integrating sensors that monitor physiological parameters marks a significant advancement in phototherapy device technology. These sensors enable real-time feedback and dynamic optimization of treatment parameters, ensuring maximum therapeutic efficacy by adapting to specific clinical conditions. Seamless integration of sensors during device fabrication enhances functionality, streamlines design, and creates compact, efficient systems that reduce manual adjustments and improve adaptability across diverse clinical scenarios. Future devices, leveraging advanced Internet of Things technologies, will better meet clinical needs and address the growing demand for professional phototherapy services in home settings, further broadening the scope and impact of phototherapy technology.
Future directions: towards intelligent and integrated phototherapy systems
The rapid development of soft wearable and implantable sensors drives phototherapy devices toward enhanced intelligence and integration. A range of wearable and implantable sensor devices (Fig. 6a), including smart glasses141, smart contact lenses142,143,144, monitoring headphones80, implantable EMG, EEG and ECG devices57, smartwatches141, microneedle patches79, tendon sensors63, and wound monitoring patches138, have been developed to continuously monitor a wide variety of physiological, biochemical, and behavioral indicators (Fig. 6b).
Wearable monitoring devices and potential algorithms. a Existing wearable monitoring devices: smart glasses141, contact lenses142,143, earbuds80, implantable electrodes57, microneedle patch79, smartwatch152, sweat monitoring devices164, wearable motion tracking devices63, diabetic wound monitoring138. b Monitoring indicators of wearable devices, including physiological indicators, biochemical indicators and behavioral indicators. c Workflow for processing monitoring data and potential algorithms, including acquiring monitoring information from sensors, data fusion, training models to predict patient physiological conditions, and outputting personalized phototherapy parameters. d Applications combining wearable monitoring devices with phototherapy devices13,17,18,31,36,41,46,48,52,175. Figure 6, created with BioRender.com, released under a Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International license
In the treatment of chronically infected wounds (Fig. 6c), phototherapy devices integrated with sensors collect key physiological and biochemical data, such as pH, temperature, lactate, uric acid, and oxygen saturation, providing real-time insights into wound infection and healing progress138 (Fig. 6b). These data are wirelessly transmitted to cloud platforms, where deep learning models, trained on large datasets, analyze the wound state, and recommend optimized phototherapy parameters (Fig. 6c). Models are embedded into phototherapy devices, using algorithms like CNNs for image data, LSTMs for time-series data, and Transformers for multimodal spatiotemporal inputs. Reinforcement learning methods, including Deep Q-Learning, Policy Gradient methods, and supervised control, refine the settings by learning from therapeutic outcomes. Model feedback and online learning further enhance adaptability, ensuring continuous optimization based on real-world data. This intelligent system dynamically adjusts phototherapy parameters—such as wavelength, intensity, and duration—creating a closed-loop framework for precise, efficient, and personalized wound management (Fig. 6c).
Based on the integration strategy of phototherapy devices with AI, Table 3 summarizes representative sensors that could be integrated with phototherapy systems in the future. Possible application scenarios are illustrated in Fig. 6d, with their integration approaches described as follows:
For the head, phototherapy devices based on optogenetics have been developed for the treatment of epilepsy57, Alzheimer’s disease145,146, and depression147 (Figs. 1a, 6d). These devices can integrate with wearable sensors, such as earbuds80 and smart contact lenses142,143, to monitor brainwaves, neural signals, and tissue oxygenation levels (Table 3), enabling personalized optical therapies tailored to the patient’s disease progression. Additionally, facial sweat sensors148 and electrochemical biosensors79 (Table 3) have the potential to be combined with phototherapy masks31 and soft light-emitting patch17 for applications in acne treatment149, pigmentation disorders150, and facial rejuvenation62 (Figs. 1a, 6d).
In the torso region, wearable microneedle sensors79, electrochemical sweat sensors151, and smartwatches152 are capable of monitoring blood glucose levels, blood oxygen saturation, heart rate, pulse, ECG signals, and physical activity acceleration, providing valuable insights into both cardiac and behavioral functions (Table 3). These advancements support applications such as light-based modulation of glucose metabolism43, Parkinson49 and optogenetic cardiac pacemakers41(Figs. 1a, 6d). Moreover, integrating transcutaneous bilirubin sensors153,154,155 with phototherapy garments13 enhances the treatment of hyperbilirubinemia (Table 3), while implantable sensors combined with phototherapy devices hold promise for simultaneously monitoring gastrointestinal microbiota and modulating gut flora43 (Fig. 6d).
For the limbs, sensors that measure deep tissue oxygen concentration67 and peripheral metabolites79 (Table 3), when integrated with phototherapy devices, enable closed-loop management of chronic infectious wounds, offering new solutions for addressing diabetes-related complications(Fig. 6d). Furthermore, optogenetic peripheral nerve modulation is becoming increasingly sophisticated. For example, integrating implantable pressure sensors with phototherapy devices allows precise regulation of bladder pressure, providing a solution for urinary dysfunction48. Lastly, incorporating sensors capable of detecting visual evoked potentials and electroretinography signals into phototherapy glasses allows real-time monitoring of visual function and supports vision restoration through targeted phototherapy37(Fig. 6d).
The future of intelligent phototherapy systems extends beyond parameter adjustment to deep integration with treatment feedback mechanisms. Through real-time data analysis, these systems can detect subtle changes in disease states and automatically update AI models, further enhancing treatment precision. The high level of integration between phototherapy devices and sensors enables lightweight and non-invasive designs, making them highly suitable for daily use in home settings.
In conclusion, the advancements in soft wearable and implantable sensors, combined with the powerful data processing capabilities of AI algorithms, provide a solid foundation for the widespread application of intelligent phototherapy devices. This direction not only enhances treatment efficiency and safety but also advances the field of precision medicine, offering personalized solutions for a range of complex diseases.
Conclusions and future perspective
This review adopts the perspective of clinical phototherapy practitioners, addresses specific clinical needs, and summarizes the extensive applications of phototherapy devices in the medical field. It highlights the major challenges encountered during the implementation of wearable and implantable phototherapy devices. Drawing on advancements in photomedicine, materials science, and soft electronics, the review proposes targeted strategies to address these challenges, summarizes interdisciplinary research contributing to the future development of phototherapy devices, and outlines a potential fabrication roadmap for future devices. Furthermore, it explores the integration of emerging AI technologies and soft sensing modules to design closed-loop phototherapy-monitoring systems for enhanced therapeutic outcomes.
Building on the outlined challenges and strategies for advancing phototherapy devices, it is essential to recognize the transformative role of photomedicine in clinical practice. Photomedicine has emerged as a cornerstone in disease diagnosis and treatment, transitioning from its historical role as an adjunct therapy to serving as a first-line treatment for various conditions. It has demonstrated remarkable efficacy in managing neonatal jaundice, wound healing, pigmentary disorders, and vascular anomalies. This transition underscores its value as a low-cost, highly precisive physical therapy. The increasing clinical relevance of photomedicine necessitates its broader adoption, particularly as advancements in technology continue to improve its therapeutic precision and accessibility. Despite its promise, significant challenges remain in the design and engineering of wearable and implantable phototherapy devices. Wearable devices often face issues related to portability, personalization, illumination uniformity, and compatibility with the mechanical and optical properties of target tissues. We highlight the potential of OLED and µLED technologies, combined with optical lenses and diffusion layers, to improve illumination uniformity and facilitate miniaturization through modular designs. On the other hand, implantable devices, while offering more targeted treatment, encounter limitations such as insufficient energy supply, reduced durability, encapsulation leakage, and biosafety concerns. Novel biomaterials, multilayer thin-film encapsulation, and soft or micro-batteries can be incorporated to enhance durability and biosafety. Additionally, integrating sensors such as electrochemical, spectroscopic, and electrophysiological systems enable closed-loop diagnostic and therapeutic capabilities, further advancing the precision and effectiveness of phototherapy applications.
Advances in light-emitting and conductive materials are also shaping the future of phototherapy devices. µLEDs and OLEDs are identified as the most suitable light-emitting materials due to their high efficiency, flexibility, and biocompatibility. Similarly, liquid metals and stretchable conductive polymers are emerging as promising candidates for soft active materials, enabling devices to better conform to complex anatomical surfaces. To realize the potential of these technologies, low-temperature fabrication techniques are essential, particularly for new soft active materials that are sensitive to high-temperature environments. Additionally, hybrid organic-inorganic thin-film encapsulation and advanced wearable/implantable power solutions further accelerate the development of future phototherapy devices. To support the development of next-generation phototherapy devices, we outline a comprehensive design framework that incorporates the selection of soft substrates, active material deposition, and device schematics. This framework provides a roadmap for researchers and engineers to create devices that meet the stringent requirements of medical applications, including safety, durability, and user-friendliness.
Finally, integrating AI with phototherapy devices represents a significant opportunity to advance the field. Leveraging wearable and implantable sensing technologies, AI has the potential to enable closed-loop systems that combine diagnostic and therapeutic capabilities, allowing for real-time adjustments to various clinical applications. Such intelligent systems hold transformative potential, as evidenced by proposed application scenarios that demonstrate their ability to improve outcomes across a range of medical conditions. These advancements highlight the exciting future of photomedicine and its growing role in precision healthcare.
References
Li, X. S. et al. Clinical development and potential of photothermal and photodynamic therapies for cancer. Nat. Rev. Clin. Oncol. 17, 657–674 (2020).
Finsen, N. R. Phototherapy (Edward Arnold Publishers Ltd., 1901).
Maiman, T. H. Stimulated optical radiation in ruby. Nature 187, 493–494 (1960).
Batta, K. et al. Randomised controlled study of early pulsed dye laser treatment of uncomplicated childhood haemangiomas: results of a 1-year analysis. Lancet 360, 521–527 (2002).
Dolmans, D. E. J. G. J., Fukumura, D. & Jain, R. K. Photodynamic therapy for cancer. Nat. Rev. Cancer 3, 380–387 (2003).
Seaton, E. D. et al. Pulsed-dye laser treatment for inflammatory acne vulgaris: randomised controlled trial. Lancet 362, 1347–1352 (2003).
Lu, M. et al. Bacteria-specific phototoxic reactions triggered by blue light and phytochemical carvacrol. Sci. Transl. Med. 13, eaba3571 (2021).
Kim, T. I. et al. Refractive surgery. Lancet 393, 2085–2098 (2019).
Anderson, R. R. & Parrish, J. A. Selective photothermolysis: precise microsurgery by selective absorption of pulsed radiation. Science 220, 524–527 (1983).
Parker, T. et al. Gamma knife radiosurgery for uveal melanomas and metastases: a systematic review and meta-analysis. Lancet Oncol. 21, 1526–1536 (2020).
Ho, P. W. L., Szeto, C. C. & Chow, K. M. Continuous glucose monitoring device causes consternation on chest x-ray. Lancet 399, 2412 (2022).
An, L. Y. et al. Sexual dimorphism in melanocyte stem cell behavior reveals combinational therapeutic strategies for cutaneous repigmentation. Nat. Commun. 15, 796 (2024).
Choi, S. et al. Wearable photomedicine for neonatal jaundice treatment using blue organic light-emitting diodes (OLEDs): toward textile-based wearable phototherapeutics. Adv. Sci. 9, 2204622 (2022).
Stitt, A. W. et al. The progress in understanding and treatment of diabetic retinopathy. Prog. Retinal Eye Res. 51, 156–186 (2016).
Tang, Y. L. et al. Green light analgesia in mice is mediated by visual activation of enkephalinergic neurons in the ventrolateral geniculate nucleus. Sci. Transl. Med. 14, eabq6474 (2022).
Oh, P. S. & Jeong, H. J. Therapeutic application of light emitting diode: Photo-oncomic approach. J. Photochem. Photobiol. B: Biol. 192, 1–7 (2019).
Lee, S. Y. et al. Combinatorial wound healing therapy using adhesive nanofibrous membrane equipped with wearable LED patches for photobiomodulation. Sci. Adv. 8, eabn1646 (2022).
Lee, H. E. et al. Trichogenic photostimulation using monolithic flexible vertical AlGaInP light-emitting diodes. ACS Nano 12, 9587–9595 (2018).
Deng, K. C. et al. A biodegradable, flexible photonic patch for in vivo phototherapy. Nat. Commun. 14, 3069 (2023).
Sakai, J. Functional near-infrared spectroscopy reveals brain activity on the move. Proc. Natl. Acad. Sci. USA 119, e2208729119 (2022).
Tomassetti, C. et al. Estimation of the endometriosis fertility index prior to operative laparoscopy. Hum. Reprod. 36, 636–646 (2021).
Chen, X. et al. Far infrared irradiation suppresses experimental arthritis in rats by down-regulation of genes involved inflammatory response and autoimmunity. J. Adv. Res. 38, 107–118 (2022).
Lee, H. E. et al. Optogenetic brain neuromodulation by stray magnetic field via flash-enhanced magneto-mechano-triboelectric nanogenerator. Nano Energy 75, 104951 (2020).
Rajalingham, R. et al. Chronically implantable LED arrays for behavioral optogenetics in primates. Nat. Methods 18, 1112–1116 (2021).
Kim, D. et al. Ultraflexible organic light-emitting diodes for optogenetic nerve stimulation. Proc. Natl. Acad. Sci. USA 117, 21138–21146 (2020).
Van Tran, V. et al. Light emitting diodes technology-based photobiomodulation therapy (PBMT) for dermatology and aesthetics: recent applications, challenges, and perspectives. Opt. Laser Technol. 135, 106698 (2021).
Yang, L. D. et al. Mitochondria as a target for neuroprotection: role of methylene blue and photobiomodulation. Transl. Neurodegeneration 9, 19 (2020).
Kim, W. S. et al. AI-enabled, implantable, multichannel wireless telemetry for photodynamic therapy. Nat. Commun. 13, 2178 (2022).
Piksa, M. et al. The role of the light source in antimicrobial photodynamic therapy. Chem. Soc. Rev. 52, 1697–1722 (2023).
Pham, T. C. et al. Recent strategies to develop innovative photosensitizers for enhanced photodynamic therapy. Chem. Rev. 121, 13454–13619 (2021).
Kim, M. S. et al. Clinical validation of face-fit surface-lighting micro light-emitting diode mask for skin anti-aging treatment. Adv. Mater. 36, 2411651 (2024).
Zhang, H. et al. Biocompatible light guide-assisted wearable devices for enhanced UV light delivery in deep skin. Adv. Funct. Mater. 31, 2100576 (2021).
Bachelez, H. et al. Tofacitinib versus etanercept or placebo in moderate-to-severe chronic plaque psoriasis: a phase 3 randomised non-inferiority trial. Lancet 386, 552–561 (2015).
Jeon, Y. et al. Sandwich-structure transferable free-form OLEDs for wearable and disposable skin wound photomedicine. Light Sci. Appl. 8, 114 (2019).
Yang, L. et al. Biofilm microenvironment triggered self-enhancing photodynamic immunomodulatory microneedle for diabetic wound therapy. Nat. Commun. 14, 7658 (2023).
Li, M. et al. A wearable and stretchable dual-wavelength LED device for home care of chronic infected wounds. Nat. Commun. 15, 9380 (2024).
Sahel, J. A. et al. Partial recovery of visual function in a blind patient after optogenetic therapy. Nat. Med. 27, 1223–1229 (2021).
McDonagh, A. F. Letter: phototherapy and hyperbilirubinaemia. Lancet 1, 339 (1975).
Figueiro Longo, M. G. et al. Effect of transcranial low-level light therapy vs sham therapy among patients with moderate traumatic brain injury: a randomized clinical trial. JAMA Netw. Open 3, e2017337 (2020).
Kim, J. et al. Implantable MicroLED-mediated chemo-photodynamic combination therapy for glioma treatment. Adv. Funct. Mater. 34, 2316386 (2024).
Hsueh, B. et al. Cardiogenic control of affective behavioural state. Nature 615, 292–299 (2023).
Ausra, J. et al. Wireless, fully implantable cardiac stimulation and recording with on-device computation for closed-loop pacing and defibrillation. Sci. Adv. 8, eabq7469 (2022).
Sim, J. H. et al. OLED catheters for inner-body phototherapy: a case of type 2 diabetes mellitus improved via duodenal photobiomodulation. Sci. Adv. 9, eadh8619 (2023).
Qiao, L. L. et al. A sensitive red/far-red photoswitch for controllable gene therapy in mouse models of metabolic diseases. Nat. Commun. 15, 10310 (2024).
Shao, J. W. et al. Smartphone-controlled optogenetically engineered cells enable semiautomatic glucose homeostasis in diabetic mice. Sci. Transl. Med. 9, eaal2298 (2017).
Kawana, Y. et al. Optogenetic stimulation of vagal nerves for enhanced glucose-stimulated insulin secretion and β cell proliferation. Nat. Biomed. Eng. 8, 808–822 (2024).
Mansouri, M. et al. Smart-watch-programmed green-light-operated percutaneous control of therapeutic transgenes. Nat. Commun. 12, 3388 (2021).
Mickle, A. D. et al. A wireless closed-loop system for optogenetic peripheral neuromodulation. Nature 565, 361–365 (2019).
Sinha, G. Trials begin for a new weapon against Parkinson’s: light. Science 369, 1415–1416 (2020).
Li, D. Y. et al. Photostimulation of brain lymphatics in male newborn and adult rodents for therapy of intraventricular hemorrhage. Nat. Commun. 14, 6104 (2023).
Tao, L. C. et al. Microglia modulation with 1070-nm light attenuates Aβ burden and cognitive impairment in Alzheimer’s disease mouse model. Light Sci. Appl. 10, 179 (2021).
Kathe, C. et al. Wireless closed-loop optogenetics across the entire dorsoventral spinal cord in mice. Nat. Biotechnol. 40, 198–208 (2022).
Zhang, Y. et al. Battery-free, fully implantable optofluidic cuff system for wireless optogenetic and pharmacological neuromodulation of peripheral nerves. Sci. Adv. 5, eaaw5296 (2019).
Liu, X. Y. et al. Fatigue-resistant hydrogel optical fibers enable peripheral nerve optogenetics during locomotion. Nat. Methods 20, 1802–1809 (2023).
Kim, H. et al. Benefits of a skull-interfaced flexible and implantable multilight emitting diode array for photobiomodulation in ischemic stroke. Adv. Sci. 9, e2104629 (2022).
Hee Lee, J. et al. Implantable micro-light-emitting diode (µLED)-based optogenetic interfaces toward human applications. Adv. Drug Deliv. Rev. 187, 114399 (2022).
Ouyang, W. et al. A wireless and battery-less implant for multimodal closed-loop neuromodulation in small animals. Nat. Biomed. Eng. 7, 1252–1269 (2023).
Yamagishi, K. et al. Tissue-adhesive wirelessly powered optoelectronic device for metronomic photodynamic cancer therapy. Nat. Biomed. Eng. 3, 27–36 (2019).
Chai, R. Z. & Zhang, Y. Adaptive thermal management of implantable device. IEEE Sens. J. 19, 1176–1185 (2019).
Zhang, Z. et al. High-brightness all-polymer stretchable LED with charge-trapping dilution. Nature 603, 624–630 (2022).
Bian, Y. Y. et al. Efficient green InP-based QD-LED by controlling electron injection and leakage. Nature 635, 854–859 (2024).
Lee, J. H. et al. Wearable surface-lighting micro-light-emitting diode patch for melanogenesis inhibition. Adv. Healthc. Mater. 12, 2201796 (2023).
Lee, J. et al. Stretchable and suturable fibre sensors for wireless monitoring of connective tissue strain. Nat. Electron. 4, 291–301 (2021).
Negri, L. B. et al. An antimicrobial blue light prototype device controls infected wounds in a preclinical porcine model. J. Infect. Dis. 231, e545–e552 (2024).
Jung, Y. H. et al. A wireless haptic interface for programmable patterns of touch across large areas of the skin. Nat. Electron. 5, 374–385 (2022).
Tang, X. et al. Flexible brain-computer interfaces. Nat. Electron. 6, 109–118 (2023).
Cai, X. et al. A wireless optoelectronic probe to monitor oxygenation in deep brain tissue. Nat. Photonics 18, 492–500 (2024).
Lee, G. H. et al. Multifunctional materials for implantable and wearable photonic healthcare devices. Nat. Rev. Mater. 5, 149–165 (2020).
Mariello, M. et al. Recent advances in encapsulation of flexible bioelectronic implants: materials, technologies, and characterization methods. Adv. Mater. 34, 2201129 (2022).
He, J. Q. et al. Scalable production of high-performing woven lithium-ion fibre batteries. Nature 597, 57–63 (2021).
Zhu, G. Z. et al. Rechargeable Na/Cl2 and Li/Cl2 batteries. Nature 596, 525–530 (2021).
Davies, N. & Wilson, B. C. Interstitial in vivo ALA-PpIX mediated metronomic photodynamic therapy (mPDT) using the CNS-1 astrocytoma with bioluminescence monitoring. Photodiagn. Photodyn. Ther. 4, 202–212 (2007).
Davies, N. & Wilson, B. C. Tetherless fiber-coupled optical sources for extended metronomic photodynamic therapy. Photodiagn. Photodyn. Ther. 4, 184–189 (2007).
Tan, C. X. et al. A high performance wearable strain sensor with advanced thermal management for motion monitoring. Nat. Commun. 11, 3530 (2020).
Tao, P. D. et al. Enhancement of in-plane thermal conductivity of flexible boron nitride heat spreaders by micro/nanovoid filling using deformable liquid metal nanoparticles. Rare Met. 42, 3662–3672 (2023).
Xu, S. D. et al. Realizing a 10 °C cooling effect in a flexible thermoelectric cooler using a vortex generator. Adv. Mater. 34, 2204508 (2022).
van Erp, R. et al. Co-designing electronics with microfluidics for more sustainable cooling. Nature 585, 211–216 (2020).
Min, J. H. et al. An autonomous wearable biosensor powered by a perovskite solar cell. Nat. Electron. 6, 630–641 (2023).
Tehrani, F. et al. An integrated wearable microneedle array for the continuous monitoring of multiple biomarkers in interstitial fluid. Nat. Biomed. Eng. 6, 1214–1224 (2022).
Xu, Y. C. et al. In-ear integrated sensor array for the continuous monitoring of brain activity and of lactate in sweat. Nat. Biomed. Eng. 7, 1307–1320 (2023).
Zhang, S. P. et al. On-skin ultrathin and stretchable multifunctional sensor for smart healthcare wearables. npj Flex. Electron. 6, 11 (2022).
Zhou, J. et al. Multiscale and hierarchical wrinkle enhanced graphene/Ecoflex sensors integrated with human-machine interfaces and cloud-platform. npj Flex. Electron. 6, 55 (2022).
Zhang, L. D. et al. Advanced and readily-available wireless-powered blue-light-implant for non-invasive peri-implant disinfection. Adv. Sci. 10, 2203472 (2023).
Bo, R. H. et al. Mechanically-guided 3D assembly for architected flexible electronics. Chem. Rev. 123, 11137–11189 (2023).
Kong, M. et al. Transparent omni-directional stretchable circuit lines made by a junction-free grid of expandable Au lines. Adv. Mater. 33, 2100299 (2021).
Shen, Q. C. et al. Liquid metal-based soft, hermetic, and wireless-communicable seals for stretchable systems. Science 379, 488–493 (2023).
Lee, W. et al. Universal assembly of liquid metal particles in polymers enables elastic printed circuit board. Science 378, 637–641 (2022).
Liu, S. L. Z., Shah, D. S. & Kramer-Bottiglio, R. Highly stretchable multilayer electronic circuits using biphasic gallium-indium. Nat. Mater. 20, 851–858 (2021).
Zheng, Y. et al. Environmentally stable and stretchable polymer electronics enabled by surface-tethered nanostructured molecular-level protection. Nat. Nanotechnol. 18, 1175–1184 (2023).
Min, H. et al. Additive treatment yields high-performance lead-free perovskite light-emitting diodes. Nat. Photonics 17, 755–760 (2023).
Su, R. T. et al. 3D-printed flexible organic light-emitting diode displays. Sci. Adv. 8, eabl8798 (2022).
Chen, C. S. et al. Perovskite solar cells based on screen-printed thin films. Nature 612, 266–271 (2022).
Wang, S. C. et al. Inkjet-printed xerogel scaffolds enabled room-temperature fabrication of high-quality metal electrodes for flexible electronics. Adv. Funct. Mater. 32, 2203730 (2022).
Liu, G. Q. et al. Evolution of dip-pen nanolithography (DPN): from molecular patterning to materials discovery. Chem. Rev. 120, 6009–6047 (2020).
Lee, J. H. et al. Deeply implantable, shape-morphing, 3D MicroLEDs for pancreatic cancer therapy. Adv. Mater. https://doi.org/10.1002/adma.202411494 (2024).
Lin, Q. H. et al. Flexible quantum dot light-emitting device for emerging multifunctional and smart applications. Adv. Mater. 35, 2210385 (2023).
Jang, E. & Jang, H. Review: quantum dot light-emitting diodes. Chem. Rev. 123, 4663–4692 (2023).
Zhao, H. N. et al. Stable blue phosphorescent organic LEDs that use polariton-enhanced Purcell effects. Nature 626, 300–305 (2024).
Cho, H. H. et al. Suppression of Dexter transfer by covalent encapsulation for efficient matrix-free narrowband deep blue hyperfluorescent OLEDs. Nat. Mater. 23, 519–526 (2024).
Kim, T. et al. Efficient and stable blue quantum dot light-emitting diode. Nature 586, 385–389 (2020).
Ryu, J. E. et al. Technological breakthroughs in chip fabrication, transfer, and color conversion for high-performance micro-LED displays. Adv. Mater. 35, 2204947 (2023).
Chang, W. et al. Concurrent self-assembly of RGB microLEDs for next-generation displays. Nature 617, 287–291 (2023).
Huang, J. S. et al. Near-infrared photodynamic chemiluminescent probes for cancer therapy and metastasis detection. Angew. Chem. Int. Ed. 62, e202303982 (2023).
Keum, C. et al. A substrateless, flexible, and water-resistant organic light-emitting diode. Nat. Commun. 11, 6250 (2020).
Kim, J. H. & Park, J. W. Intrinsically stretchable organic light-emitting diodes. Sci. Adv. 7, eabd9715 (2021).
Huang, T. Y. et al. Delocalizing electron distribution in thermally activated delayed fluorophors for high-efficiency and long-lifetime blue electroluminescence. Nat. Mater. 23, 1523–1530 (2024).
Hua, T. et al. Deep-blue organic light-emitting diodes for ultrahigh-definition displays. Nat. Photonics 18, 1161–1169 (2024).
Zhao, H. N., Arneson, C. E. & Forrest, S. R. Stable, deep blue tandem phosphorescent organic light-emitting diode enabled by the double-sided polariton-enhanced Purcell effect. Nat. Photonics 19, 607–614 (2025).
Tankelevičiūtė, E., Samuel, I. D. W. & Zysman-Colman, E. The blue problem: OLED stability and degradation mechanisms. J. Phys. Chem. Lett. 15, 1034–1047 (2024).
Choi, D. K. et al. Highly efficient, heat dissipating, stretchable organic light-emitting diodes based on a MoO3/Au/MoO3 electrode with encapsulation. Nat. Commun. 12, 2864 (2021).
Cha, G. D., Kim, D. H. & Kim, D. C. Wearable and implantable light-emitting diodes and their biomedical applications. Korean J. Chem. Eng. 41, 1–24 (2024).
Chen, H. et al. Flexible quantum dot light-emitting devices for targeted photomedical applications. J. Soc. Inf. Disp. 26, 296–303 (2018).
Chen, H. et al. Quantum dot light emitting devices for photomedical applications. J. Soc. Inf. Disp. 25, 177–184 (2017).
Kim, Y. W. et al. Wearable quantum dots organic light-emitting diodes patch for high-power near infra-red photomedicene with real-time wavelength control. Chem. Eng. J. 499, 156121 (2024).
Tri, T. T. et al. Maximization of cytochrome C oxidase enzyme activity by optimizing color conversion from red organic light-emitting diodes. Appl. Mater. Today 38, 102223 (2024).
Wang, Y. K. et al. Long-range order enabled stability in quantum dot light-emitting diodes. Nature 629, 586–591 (2024).
Kang, K. S. et al. Reliable high temperature, high humidity flexible thin film encapsulation using Al2O3/MgO nanolaminates for flexible OLEDs. Nano Res. 13, 2716–2725 (2020).
Kishore, R. A. et al. Ultra-high performance wearable thermoelectric coolers with less materials. Nat. Commun. 10, 1765 (2019).
Liu, H. et al. Development and evaluation of a low-cost, portable, LED-based device for PDT treatment of early-stage oral cancer in resource-limited settings. Lasers Surg. Med. 51, 345–351 (2019).
Lu, C. H. et al. High-performance fibre battery with polymer gel electrolyte. Nature 629, 86–91 (2024).
Zhang, Y. J. et al. A microscale soft lithium-ion battery for tissue stimulation. Nat. Chem. Eng. 1, 691–701 (2024).
Hong, Y. et al. Energetic and durable all-polymer aqueous battery for sustainable, flexible power. Nat. Commun. 15, 9539 (2024).
Zhang, C. et al. Conjunction of triboelectric nanogenerator with induction coils as wireless power sources and self-powered wireless sensors. Nat. Commun. 11, 58 (2020).
Seo, D. et al. Wireless recording in the peripheral nervous system with ultrasonic neural dust. Neuron 91, 529–539 (2016).
Ding, H. et al. Microscale optoelectronic infrared-to-visible upconversion devices and their use as injectable light sources. Proc. Natl Acad. Sci. USA 115, 6632–6637 (2018).
Park, S. I. et al. Soft, stretchable, fully implantable miniaturized optoelectronic systems for wireless optogenetics. Nat. Biotechnol. 33, 1280–1286 (2015).
Liu, Z. et al. Human motion driven self-powered photodynamic system for long-term autonomous cancer therapy. ACS Nano 14, 8074–8083 (2020).
Jeong, Y. C. et al. Progress in brain-compatible interfaces with soft nanomaterials. Adv. Mater. 32, 1907522 (2020).
Kim, T. I. et al. Injectable, cellular-scale optoelectronics with applications for wireless optogenetics. Science 340, 211–216 (2013).
Yang, X. et al. Bioinspired neuron-like electronics. Nat. Mater. 18, 510–517 (2019).
Zhang, Z. T. Light-emitting materials for wearable electronics. Nat. Rev. Mater. 7, 839–840 (2022).
Ma, D. X. et al. Distribution control enables efficient reduced-dimensional perovskite LEDs. Nature 599, 594–598 (2021).
Shin, J. et al. Vertical full-colour micro-LEDs via 2D materials-based layer transfer. Nature 614, 81–87 (2023).
Kim, D. C. et al. Intrinsically stretchable quantum dot light-emitting diodes. Nat. Electron. 7, 365–374 (2024).
Si, M. W. et al. Scaled indium oxide transistors fabricated using atomic layer deposition. Nat. Electron. 5, 164–170 (2022).
Chorsi, M. T. et al. Highly piezoelectric, biodegradable, and flexible amino acid nanofibers for medical applications. Sci. Adv. 9, eadg6075 (2023).
Zhang, Y. P. et al. Flexible self-powered integrated sensing system with 3D periodic ordered black phosphorus@MXene thin-films. Adv. Mater. 33, 2007890 (2021).
Sani, E. S. et al. A stretchable wireless wearable bioelectronic system for multiplexed monitoring and combination treatment of infected chronic wounds. Sci. Adv. 9, eadf7388 (2023).
Bidinger, S. L. et al. Pulsed transistor operation enables miniaturization of electrochemical aptamer-based sensors. Sci. Adv. 8, eadd4111 (2022).
Wu, H. et al. On-skin biosensors for noninvasive monitoring of postoperative free flaps and replanted digits. Sci. Transl. Med. 15, eabq1634 (2023).
Lee, J. H. et al. 3D printed, customizable, and multifunctional smart electronic eyeglasses for wearable healthcare systems and human-machine interfaces. Acs Appl. Mater. Interfaces 12, 21424–21432 (2020).
Kim, S. K. et al. Bimetallic nanocatalysts immobilized in nanoporous hydrogels for long-term robust continuous glucose monitoring of smart contact lens. Adv. Mater. 34, 2110536 (2022).
Kim, J. et al. A soft and transparent contact lens for the wireless quantitative monitoring of intraocular pressure. Nat. Biomed. Eng. 5, 772–782 (2021).
Liu, W. J. et al. Neuroprosthetic contact lens enabled sensorimotor system for point-of-care monitoring and feedback of intraocular pressure. Nat. Commun. 15, 5635 (2024).
Cardoso, F. D. S., Gonzalez-Lima, F. & Gomes da Silva, S. Photobiomodulation for the aging brain. Ageing Res. Rev. 70, 101415 (2021).
Cunnane, S. C. et al. Brain energy rescue: an emerging therapeutic concept for neurodegenerative disorders of ageing. Nat. Rev. Drug Discov. 19, 609–633 (2020).
Aini, N. et al. The effects of light therapy on sleep, depression, neuropsychiatric behaviors, and cognition among people living with dementia: a meta-analysis of randomized controlled trials. Am. J. Geriatr. Psychiatry 32, 681–706 (2024).
Yin, L. et al. A stretchable epidermal sweat sensing platform with an integrated printed battery and electrochromic display. Nat. Electron. 5, 694–705 (2022).
Wainwright, M. et al. Photoantimicrobials-are we afraid of the light? Lancet Infect. Dis. 17, E49–E55 (2017).
Ju, X. K. et al. A wearable electrostimulation-augmented ionic-gel photothermal patch doped with MXene for skin tumor treatment. Nat. Commun. 15, 762 (2024).
Sempionatto, J. R. et al. An epidermal patch for the simultaneous monitoring of haemodynamic and metabolic biomarkers. Nat. Biomed. Eng. 5, 737–748 (2021).
Schalkamp, A. K. et al. Wearable movement-tracking data identify Parkinson’s disease years before clinical diagnosis. Nat. Med. 29, 2048–2056 (2023).
Chung, H. U. et al. Skin-interfaced biosensors for advanced wireless physiological monitoring in neonatal and pediatric intensive-care units. Nat. Med. 26, 418–429 (2020).
Chung, H. U. et al. Binodal, wireless epidermal electronic systems with in-sensor analytics for neonatal intensive care. Science 363, eaau0780 (2019).
Inamori, G. et al. Neonatal wearable device for colorimetry-based real-time detection of jaundice with simultaneous sensing of vitals. Sci. Adv. 7, eabe3793 (2021).
Hillebrandt, S. et al. High brightness, highly directional organic light-emitting diodes as light sources for future light-amplifying prosthetics in the optogenetic management of vision loss. Adv. Opt. Mater. 11, 2200877 (2022).
Lee, G. H. et al. Smart wireless near-infrared light emitting contact lens for the treatment of diabetic retinopathy. Adv. Sci. 9, 2106254 (2022).
Sun, S. Q. et al. Red organic light-emitting diodes based photobiomodulation therapy enabling prominent hair growth. Nano Res. 16, 7164–7170 (2023).
Jeon, Y. et al. Parallel-stacked flexible organic light-emitting diodes for wearable photodynamic therapeutics and color-tunable optoelectronics. ACS Nano 14, 15688–15699 (2020).
Lian, C. et al. Flexible organic light-emitting diodes for antimicrobial photodynamic therapy. npj Flex. Electron. 3, 18 (2019).
Song, J. et al. Organic light-emitting diodes: pushing toward the limits and beyond. Adv. Mater. 32, 1907539 (2020).
Kang, S. K. et al. Bioresorbable silicon electronic sensors for the brain. Nature 530, 71–76 (2016).
Wang, C. H. et al. Monitoring of the central blood pressure waveform via a conformal ultrasonic device. Nat. Biomed. Eng. 2, 687–695 (2018).
Xu, C. H. et al. A physicochemical-sensing electronic skin for stress response monitoring. Nat. Electron. 7, 168–179 (2024).
Juengpanich, S. et al. Pre-activated nanoparticles with persistent luminescence for deep tumor photodynamic therapy in gallbladder cancer. Nat. Commun. 14, 5699 (2023).
Tang, Y. F. et al. Oxygen-independent organic photosensitizer with ultralow-power NIR photoexcitation for tumor-specific photodynamic therapy. Nat. Commun. 15, 2530 (2024).
Chen, J. et al. Atomically precise photothermal nanomachines. Nat. Mater. 23, 271–280 (2024).
Zhang, Q. et al. Noninvasive low-level laser therapy for thrombocytopenia. Sci. Transl. Med. 8, 349ra101 (2016).
Wang, Z. H. et al. Adoptive macrophage directed photodynamic therapy of multidrug-resistant bacterial infection. Nat. Commun. 14, 7251 (2023).
Xiu, W. et al. Potentiating hypoxic microenvironment for antibiotic activation by photodynamic therapy to combat bacterial biofilm infections. Nat. Commun. 13, 3875 (2022).
Li, G. Q. et al. Three-dimensional flexible electronics using solidified liquid metal with regulated plasticity. Nat. Electron. 6, 154–163 (2023).
Verboven, I. & Deferme, W. Printing of flexible light emitting devices: a review on different technologies and devices, printing technologies and state-of-the-art applications and future prospects. Prog. Mater. Sci. 118, 100760 (2021).
Koo, J. H. et al. A vacuum-deposited polymer dielectric for wafer-scale stretchable electronics. Nat. Electron. 6, 137–145 (2023).
Won, S. M. et al. Wireless and battery-free technologies for neuroengineering. Nat. Biomed. Eng. 7, 405–423 (2023).
Yang, S. L. X. et al. GSH/pH dual activatable cross-linked and fluorinated PEI for cancer gene therapy through endogenous iron De-hijacking and in situ ROS amplification. Adv. Mater. 36, 2304098 (2024).
Acknowledgements
We would like to thank all authors for their significant contributions to this review. Chenxi Wang and Qiang Yu conducted the writing, literature search, figure preparation, and summarization of key findings. Ming Li, Haoyi Chen, Huizhen Fan, and Yingying Ma assisted with literature retrieval, reference verification, table preparation, and manuscript proofreading. Zhitao Zhang provided expert guidance on OLED and Micro-LED processes and materials, helping refine the manuscript framework. Mei X. Wu offered professional insights on phototherapy development and clinical applications and reviewed the manuscript. Min Lu conceptualized the overall framework and supervised the writing and revisions. We would like to extend our special thanks to the Wellman Center for Photomedicine and Dermatology Department, Harvard Medical School and Harvard University, for their invaluable support and guidance, which greatly facilitated the successful completion of this review. Their expertise and resources provided critical insights into the development and clinical translation of phototherapy devices.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wang, C., Yu, Q., Li, M. et al. Challenges and opportunities in next-generation LED therapeutic devices. Light Sci Appl 14, 319 (2025). https://doi.org/10.1038/s41377-025-01990-z
Received:
Revised:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41377-025-01990-z