Abstract
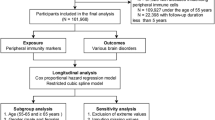
The innate immune system plays an integral role in the progression of many neurodegenerative diseases. In addition to central innate immune cells (e.g., microglia), peripheral innate immune cells (e.g., blood monocytes, natural killer cells, and dendritic cells) may also differ in these conditions. However, the characterization of peripheral innate immune cell types across different neurodegenerative diseases remains incomplete. This study aimed to characterize peripheral innate immune profiles using flow cytometry for immunophenotyping of peripheral blood mononuclear cells in n = 148 people with Alzheimer’s disease (AD), frontotemporal dementia (FTD), corticobasal syndrome (CBS), progressive supranuclear palsy (PSP), Lewy body dementia (LBD) as compared to n = 37 healthy controls. To compare groups, we used multivariate dissimilarity analysis and principal component analysis across 19 innate immune cell types. We identified pro-inflammatory profiles that significantly differ between patients with all-cause dementia and healthy controls, with some significant differences between patient groups. Regression analysis confirmed that time to death following the blood test correlated with the individuals’ immune profile weighting, positively to TREM2+ and non-classical monocytes and negatively to classical monocytes. Taken together, these results describe transdiagnostic peripheral immune profiles and highlight the link between prognosis and the monocyte cellular subdivision and function (as measured by surface protein expression). The results suggest that blood-derived innate immune profiles can inform sub-populations of cells relevant for specific neurodegenerative diseases that are significantly linked to accelerated disease progression and worse survival outcomes across diagnoses. Blood-based innate immune profiles may contribute to enhanced precision medicine approaches in dementia, helping to identify and monitor therapeutic targets and stratify patients for candidate immunotherapies.
Similar content being viewed by others
Introduction
Despite the clinical and pathological heterogeneity characterizing the main dementias, dysregulation of the innate immune system is identified as a common feature in all neurodegenerative diseases [1]. Centrally, activation of cerebral microglia is reported for Alzheimer’s disease (AD) and its prodromal mild cognitive impairment (MCI), Lewy body dementia (LBD) including Parkinson’s disease dementia (PDD) and dementia with Lewy bodies (DLB), and the syndromes associated with frontotemporal lobar degeneration (FTLD). The latter includes the behavioural variant of frontotemporal dementia (bvFTD), non-fluent (nfPPA) and semantic (svPPA) variants of primary progressive aphasia, corticobasal syndrome (CBS), and progressive supranuclear palsy (PSP). Moreover, genome-wide association studies link mutations in genes coding for proteins related to the immune system to the development of multiple neurodegenerative conditions [2,3,4,5,6,7]. For example, mutations in the gene for triggering receptor expressed on myeloid cells 2 (TREM2, encoding a receptor on monocytes and microglia) may cause FTLD-syndromes and AD, with an effect size comparable to the immune-related APOE4 variant [2, 8]. Such genomic associations are complemented by evidence of abnormalities in central and peripheral innate immune systems in neurodegenerative diseases [9].
Most evidence describing abnormal innate immunity in dementia to date concerns cerebral cells. Specifically, microglial activation in the central nervous system is implicated in many forms of dementia [10,11,12,13,14,15,16]. For example, human post mortem studies report activated microglia in association with the severity of amyloid and tau pathology in AD, FTLD-syndromes and LBD [11, 12, 17, 18]. However, post mortem studies are not well suited to characterize microglial changes in early disease stages. Instead, overexpression of the translocator protein 18 kDa (TSPO), overexpressed in activated microglia, can be detected by positron emission tomography (PET). Microglial activation presents early in people living with many types of dementia and predicts the rate of cognitive decline [13,14,15,16, 19]. While TSPO PET is a powerful, informative tool to visualize cerebral innate immune activation, it is expensive and not readily scalable. Alternatively, peripheral blood-based markers of immune dysregulation are to be potentially scalable and repeatable over time.
Cells of the innate immune system— including monocytes, dendritic cells, and natural killer (NK) cells – rapidly and non-specifically initiate an immune response upon detection of pathogens or cellular damage [20]. While this process is beneficial in the short-term to eliminate harmful stimuli, chronic or dysregulated activation can lead to disease. The peripheral immune system may interact with the central nervous system indirectly via chemokine and cytokine signalling or directly via infiltration into and meningeal surveillance of the parenchyma [21,22,23,24,25,26,27]. Elevated pro-inflammatory cytokine concentrations are reported in post mortem brain tissue and cerebrospinal fluid (CSF) in people with AD, LBD, and FTLD-syndromes [28,29,30,31]; while peripheral infections can exacerbate the neuroinflammatory environment and accelerate cognitive decline [26, 32]. Taken together, evidence implicates primary effector cells of the peripheral innate immune system in the pathogenesis of neurodegenerative diseases.
Monocytes, NK cells, and dendritic cells are each implicated in the pathogenesis of dementias. For example, TREM2 is expressed on the surface of peripheral monocytes [33] and may be a marker of monocyte recruitment in AD [27]. Elevated concentration of CSF soluble TREM2 (sTREM2), cleaved from the membranes of microglia or monocytes, is linked to disease progress cognitive decline in AD [34] and FTLD [11]. Beyond TREM2, CSF concentrations of chemokine motif ligand 2 (CCL2), mediating the chemotaxis of monocytes, are also predictive of cognitive decline in AD [35]. Similarly, abnormal activation patterns of NK cells occur with AD [36] and Parkinson’s disease (closely related to DLB and PDD) [37]. Finally, myeloid dendritic cell frequency is reduced in people with AD and Parkinson’s disease [38,39,40]. Overall, evidence involving monocytes, NK cells, and dendritic cells supports a more integrative neurodegenerative disease processes than initially appreciated.
While the mechanisms of action of peripheral immune cells remain unclear, they are nonetheless more readily accessible to quantify, compared to central innate immune cells, via phlebotomy. The identification of innate cell types in the periphery of people with dementia may clarify links between innate immunity and neurodegenerative disease, and yield clinically relevant, blood-based biomarkers to support target identification and patient stratification for immune-targeting therapies. However, current immunophenotyping data is limited to few diagnoses of dementia and remains incomplete in cellular subtype characterization [38, 39, 41,42,43]. To meet the needs for diagnostic, prognostic and trialist use, there is a pressing need for improved profiling of peripheral innate immunity in multiple neurodegenerative disorders.
This study therefore aims to characterize innate immune profiles in blood of people with diverse neurodegenerative dementias, including AD, FTLD-syndromes and LBD using Flow Cytometry- a well-established method of identifying cells via their unique expression of activation and lineage markers on the cell surface. We test the hypothesis that innate immune cell profiles are abnormal in people with any of these disorders, with at least partial commonality in the immune profile for the neurodegenerative disorders investigated here (i.e. a transdiagnostic abnormality). Given the multivariate nature of immune activation, we use data driven approaches to reduce dimensionality (complexity) and test for (dis)-similarity between the clinical diagnostic groups. We then highlight clinical relevance by the correlation or multivariate immune profiles with time to death.
Materials and methods
Participants
Patients (n = 148) were recruited from clinics for cognitive and movement disorders at the Cambridge University Hospitals NHS Trust as well as collaborating regional psychiatry and neurology services.
We included participants with a clinical diagnosis that met the standardised criteria of MCI/AD [44, 45] (n = 24; 5 MCI and 19 AD), probable or possible PSP (n = 54, predominantly Richardson’s syndrome) [46], CBS [47] (n = 23), FTD [48, 49] (n = 18; 12 bvFTD and 6 PPA), PDD (n = 3), or DLB (n = 26) [50]. In a sub-group of participants (n = 34), PET and/or CSF markers for amyloid were obtained to confirm the presence or absence of β-amyloid (interpreted as AD pathology) in conditions with weak clinicopathological correlations and either high likelihood of a significant fraction with AD as main or co-pathology (CBS and DLB) or a high likelihood of clinical diagnostic false positives (amnestic MCI). Of the CBS patients, n = 12 underwent amyloid PET, which confirmed amyloid positivity in n = 4. Of the MCI patients, all were confirmed amyloid-positive with PET imaging with the Pittsburgh compound B (PiB tracer at a cut-off of 19 centiloids [51]) and/or CSF Alzheimer’s biomarkers at lumbar puncture (Amyloid-beta 1-42/40 ratio < 0.065 as recommended laboratory threshold from University College London Hospitals reference Laboratory [52]). Of the DLB cohort, n = 6 out of 17 patients resulted amyloid-positive at PiB PET. We also included n = 37 healthy controls given MMSE > 26/30, absence of memory symptoms, no signs of dementia, or any other significant medical illnesses [53]. Exclusion criteria for both patient and healthy control cohorts included recent or current acute infection, major concurrent psychiatric illness, other severe physical illness, or a history of other significant neurological illness and/or autoimmune conditions.
All participants underwent baseline clinical and neuropsychological assessment, including the revised Addenbrooke’s Cognitive Examination (ACE-R, 0-100 points) and mini-mental state examination (MMSE). The ACE-R is subdivided into five domains: Attention and Orientation (18/100), Memory (26/100), Fluency (14/100), Language (26/100), and Visuospatial abilities (16/100). In a subset of participants, an informant completed the 8 Item Clinical Dementia Rating (CDR) FTLD NACC (Table 1.) Survival data were collected for all up to and including the 17th of October 2023 (the census date).
Ethics approval and consent to participate
Participants with mental capacity gave their written informed consent to take part in the study according to the Declaration of Helsinki. For those who lacked capacity, their participation followed the consultee process in accordance with the UK law. The research protocols were approved by the National Research Ethics Service’s East of England Cambridge Central Committee.
Blood collection and flow cytometry analyses
At baseline, 18 ml of blood was drawn in EDTA and analysed at the NIHR Cambridge Cell Immunophenotyping Hub. Wherever possible, samples were processed within 2 h (over 98% of samples). Blood was layered onto sterile Ficoll (Cytiva, Cat#: 17144003) for peripheral blood mononuclear cell (PBMC) isolation by a technician blind to group status. Two aliquots containing ~1 × 106 PBMCs were stained using the antibody cocktail shown in Supplementary Table S1, using either TREM2 or a matched isotype control. At the end of staining, cells were washed, and the data were acquired on live (i.e., non-fixed) cells with a BD LSR Fortessa instrument.
Cell classifications were determined via manual gating in FlowJo (BD) by individuals blind to participant group according to standards recommended for the Human Immunology Project [54]. Briefly, monocytes were identified as HLA-DR+/CD14+; populations were further stratified based on CD16 and CD14 positivity where CD16-/CD14hi monocytes were labelled as classical, CD16+/CD14+ monocytes labelled as intermediate, and CD16+/CD14lo monocytes labelled as nonclassical. Each monocyte subpopulation was then gated to discern CCR5+, CCR2+, and TREM2+ staining. Dendritic cells (DCs) were identified as HLA-DR+/CD14- and further stratified based on CD123 and CD11c staining: CD123+/CD11c+ cells were double positive (DC+/+), CD123+/CD11c- were plasmacytoid DCs, CD123-/CD11c+ were myeloid DCs, and CD123-/CD11c- were double negative (DC-/-). NK cells were identified as CD56+ and further subdivided into two groups as either CD16+ (which were CD56lo) or CD16- (which were CD56hi). The full gating strategy is found in Supplementary Fig. S2. Interrater validation studies showed excellent concordance between different evaluators (Supplementary Fig. S3; Supplementary Table S2).
Plasma dementia-related biomarkers
In a sub-cohort of 122 participants (Control = 27, AD = 17, CBS = 16, FTD = 12, LBD = 22, PSP = 28), plasma samples were stored at −70 °C for further analyses at the Clinical Neurochemistry Laboratory in Mölndal (Sweden). Plasma samples were thawed on wet ice, centrifuged at 500× g for 5 min at 4 °C. Calibrators (neat) and samples (plasma: 1:4 dilution) were measured in duplicates. The plasma assays performed were the Quanterix Simoa Human Neurology 4-Plex E assay (measuring Aβ40, Aβ42, GFAP and NfL, Quanterix, Billerica, MA) and the p-tau217 ALZpath assay measuring p-tau217 of the human tau protein associated with AD, as previously described [55]. Plasma samples were analysed at the same time using the same batch of reagents. A four-parameter logistic curve fit data reduction method was used to generate a calibration curve. Two control samples of known concentration of the protein of interest (high-control and low-control) were included as quality control. Intra-assay coefficients of variation were below 10%.
Statistical analysis
Analyses were performed using R (Version 2023.03.0 + 386). Non-parametric tests were used for all pairwise comparisons given non-normal data distributions. For inference, p-values were corrected for multiple comparisons using the Benjamini-Hochberg procedure to control the false discovery rate (FDR) and considered significant with threshold p-FDR < 0.05. For transparency and explorative analyses, uncorrected p-values are also reported. Statistical analysis was carried out in three steps.
First, to understand similarity of innate immune cell profiles between diagnoses and controls, absolute cell numbers from FlowJo were normalized to standardize across minimum and maximum absolute cell count ranges. These normalized cell counts were averaged within each diagnosis to yield an average, normalized 19-cell vector per diagnosis. To evaluate dissimilarity between diagnoses, Euclidean distance was calculated on the normalized data based on a 19-cell vector for all diagnoses followed by single linkage hierarchical clustering.
Second, a Principal Component Analysis (PCA) was applied on the 19 innate immune cell classes. This reduced the dimensionality of our dataset to minimize multiple comparisons, identifying a limited number of components that best explain the data variance. The PCA was computed using cell counts calculated as a proportion of their parent population across all cell types (Supplementary Fig. S1). Local Outlier Factor (LOF) analysis with a hyperparameter of k = 10 identified 2 participants as outliers following PCA computation (LOF = 3) [56]. These outliers were excluded before re-computing the PCA. We retained 3 components based on eigenvalues > 1, explained variance > 10%, and application of the visual “elbow method” from the scree plot for further analyses [57, 58] (Supplementary Fig. S4). Individual participant loadings in each of the 3 selected components were included in group-comparison analyses using Mann–Whitney U tests to compare median values between patients and controls, and Kruskal–Wallace tests to compare across patient groups followed by Dunn’s post hoc analysis, where applicable.
Finally, we tested for associations between the individual participant loadings and clinical outcome. Individual component loadings were individually evaluated as a predictor of NfL, p-tau217, Aβ40/Aβ42, GFAP, and ACE-R total scores using a linear regression, controlling for age and sex. Similarly, we investigated each principal component loading in relationship to years of survival following blood draw using a linear model, including age, sex, and biomarkers as covariates.
Results
Participant summary clinical characteristics are in Table 1. There were 76 female and 109 male participants. Most groups, apart from CBS, had more males than females. As expected, control participants scored significantly higher on the ACE-R examination than each patient group (p < 0.001 for all comparisons); while people with AD had significantly lower ACE-R total scores than people with PSP (p = 0.002).
Dissimilarity analysis
Figure 1 shows dissimilarity values of the 19-cell vector measured by Euclidean distance between groups (See Supplementary Figs S5 and S6, and Supplementary Tables S7 and S8, for individual cell pairwise comparisons). Hierarchical clustering via single linkage represented in the dendrogram summarizes the group-wise differences in the pattern (rather than magnitude) of immune profiles. Maximal relative distance was found between controls and all patient groups as evidenced by the distinct cluster or branch from the dendrogram. The smallest distance (i.e. most similarity) was identified within PSP and FTD groups, while PSP, CBS and FTD groups were more similar to each other than to AD/LBD. Importantly, the distance value between CBS and AD (2.14) and LBD (2.18) are smaller than the distance between AD, LBD, and other FTLD conditions.
Colours and values represent the Euclidean distance calculated from a 19-cell vector averaged across each group. The value for the Euclidean distance is relative to the dataset, thus the number displayed represents the length of the line segment between groups relative to the total group distance. Darker colours and larger Euclidean distance values indicate greater dissimilarity between 19-cell immune profiles across diagnostic groups, while lighter colours indicate relative similarity. The dendrogram represents single linkage hierarchical clustering. Note that all patients separate from controls initially and that the group of syndromes associated with frontotemporal lobar degeneration are similar to each other (PSP, FTD, and CBS), in contrast to Alzheimer’s disease (AD) and Lewy Body dementia (LBD). These relative similarities are highlighted in yellow.
Principal Component Analysis
From the PCA on the 19 cell populations, three components were selected for further analyses. Together, these components accounted for half of the total variance in the data. Supplementary Table S3 shows the contribution of each cell type to the selected components. The first principal component (PC1) accounted for 17.97% of the variance and was strongly positively weighted by TREM2+ monocytes and nonclassical monocytes (excluding CCR5+ nonclassical monocytes). PC1 was most negatively loaded onto classical monocytes, including CCR2+ classical monocytes, as well as NK cells high in CD16 expression (CD16+ NK cells) (Fig. 2C). The second principal component (PC2) accounted for 16.02% of the total variance. PC2 was strongly, negatively weighted by intermediate monocytes and CCR5+ monocytes, and strongly positively weighted by dendritic cells negative for CD11c and CD123 (Fig. 3C). The third principal component (PC3) accounted for 12.98% of the total variance and was most strongly positively weighted by CD16- NK Cells, and most strongly, negatively weighted in CD16+ NK cells and TREM2+ monocytes (Fig. 4C). PC relationships to sex and age are found in Supplementary Table S4. Regression analysis revealed that there was no significant relationship between individual loadings in PC1, PC2, or PC3 and age (p >0.05). There was no significant relationship between individual loadings in PC1, PC2, or PC3 and sex (p >0.05). We identified 3 patients (2 FTD and 1 CBS) with hsCRP > 10 mg/L. Similar components and individual component loadings were obtained when excluding these participants, which may be indicative of either central or peripheral inflammatory conditions (see Supplementary Fig. S7, Table S5).
A Median individual loading onto PC1 between controls and all-cause dementia patients (W = 3351, p = 0.02). B Median individual loading onto PC1 for each diagnostic group. Note the absence of significant differences between patient groups. C Correlations of each cell type with PC1. Darker colours indicate stronger positive and negative correlations to PC1. Mann–Whitney U and Kruskal–Wallace tests were used to compare medians. Results were considered significant at p <0.05 indicated with *.
A Median individual loading onto PC2 between controls and all-cause dementia patients. B Median individual loading onto PC2 for each group. C Correlations of each cell type with PC2. Darker colours indicate stronger positive and negative correlations to PC3. Mann–Whitney U and Kruskal–Wallace tests were used to compare medians. Results were considered significant at p < 0.05.
A Median individual loading onto PC3 between controls and all-cause dementia patients, W = 2025, p = 0.015. B Median individual loading onto PC3 for each group. Post hoc comparisons indicate LBD differs individually from controls, (H = 3.38, p = 0.015). C Cellular correlations to PC3 extracted following PCA. Darker colours indicate stronger positive and negative correlations to PC3. Mann–Whitney U and Kruskal–Wallace tests were used to compare medians followed by Dunn’s Post hoc analysis with FDR correction for multiple comparison. A dashed line indicates a result of statistical significance prior to FDR correction that did not maintain significance following correction.
All-cause dementia patients showed significantly lower median loading values in PC1 (U = 3351, p = 0.035) as compared to controls (Fig. 2A). Multi-group comparison did not identify a significant difference in PC1 loading between controls and each patient group (H = 10.4, p = 0.065) (Fig. 2B). There was no statistically significant difference in individual PC2 loading between all-cause dementia and controls (U = 2844, p = 0.767) or between controls and each patient group (H = 3.88, p = 0.567) (Fig. 3A, B). All-cause dementia patients had significantly reduced PC3 loading as compared to controls (U = 2025, p = 0.0145) (Fig. 4A). Multi-group comparison identified a significant difference in PC3 loading across groups (H = 15.9, p = 0.007), and post hoc analysis revealed that patients with LBD showed significantly lower median loading values in PC3 than controls (p-FDR = 0.01) (Fig. 4B). See Supplementary Table S6 for statistics from post hoc analysis group comparisons.
Clinical outcomes
Individual patient loadings of PC1, PC2, and PC3 were each evaluated as a predictor of ACE-R scores including the interaction of diagnostic group as an independent variable. Regression analysis did not reveal significant predictive value of PC1, PC2, or PC3 for ACE-R total scores. There was no interaction between diagnostic group, age, or sex, with any principal component in terms of ACE-R score.
In the subset with biomarker data, patient loadings of PC1, PC2, and PC3 were each evaluated as a predictor of plasma-based biomarker values (mg/L) including the interaction of diagnostic group as an independent variable. Regression analysis did not reveal significant predictive value of PC1, PC2, or PC3 for p-tau217, NfL, Aβ40/Aβ42, or GFAP (p < 0.05). There was no interaction between diagnostic group, age, or sex, with any principal component in terms of these biomarkers.
We used our data to evaluate the sample size required for traditional Cox proportional hazards regression. We completed a power calculation (power = 0.8, alpha = 0.05). To detect a hazard ratio <0.8 or >1.2 as seen in previous studies using this regression in immune data in dementia, we would require 234 patients with confirmed death, or 835 total participants given our current distribution of deceased to living patients (28%).
Thus, to carry out a primary survival analysis, we tested whether PC1, PC2 or PC3 were predictive of years of time to death in the subset of 42 patients who died prior to our census date (2 AD, 2 CBS, 10 LBD, 8 FTD, and 20 PSP). Higher individual loadings in PC1 predicted longer time intervals from the research visit to death (y = 0.4463x + 2.0915, F = 10.24, p = 0.0027, r2 = 0.184) (Fig. 5). This correlation remained significant after controlling for age, sex, and diagnosis (F = 3.48, p = 0.00507, βAge= −0.025, βMale=0.13). Importantly, PC1 predicted survival over and above all biomarkers when including NfL, Aβ40/Aβ42, p-tau217, and GFAP as covariates in our model (F = 1.443, p = 0.035, βNfL= −0.012, βp-tau217 = 1.23, βAB42/AB40 = − 0.09, βGFAP = 0.001). There was no association between PC2 (F = 0.1043, p = 0.75) or PC3 (F = 2.983, p = 0.09) and years of survival following blood draw.
A linear regression was used to establish how years of survival following blood draw was predicted by individual PC1 loading across all patient groups (β = 0.450, F = 10.098, p = 0.0026, r2 = 0.184), in a subset of 42 patients who had died by the census date. Outcomes were considered significant at p < 0.05.
Discussion
The main outcome of this study is confirmation that peripheral blood-based innate immunophenotypes are abnormal in people with AD, LBD, FTD, PSP, and CBS. The principal components of the 19-cell class immunophenotype were similarly abnormal in each type of neurodegenerative disease, and one component (or immune profile) predicted time to death. We identified transdiagnostic similarly in the magnitude of this abnormality in PC1, and diagnostic specificity in the magnitude and composition of this abnormality for LBD patients in PC3. Importantly, the multivariate pattern of cell-types was dissimilar between controls and all-cause dementia participants in this study. Taken together, these results indicate that even peripheral immune profiles have diagnostic specificity and identify a cellular profile represented by a redistribution of monocyte subtypes as being linked to survival across neurodegenerative dementias.
In the introduction, we proposed that peripheral innate immune cells are directly related to the pathogenesis of neurodegenerative diseases, based on genomics data and the physiological integration between central and peripheral immune compartments [2,3,4,5,6,7, 38,39,40,41,42,43, 59, 60]. Rather than a cell-by-cell account, we adopted a multivariate approach and identified three principal components of interest. The first (PC1) was weighted positively to TREM2+ and nonclassical monocytes and negatively to classical monocytes. The second (PC2) was weighted positively to CCR5+ monocytes and intermediate subtypes, and negatively to DC-/- cells. The third component (PC3) was positively weighted by CD16- NK cells and negatively weighted by CD16+ NK cells. These multivariate (multi-cell type) patterns help to contextualize the results of more selective prior studies.
For example, previous work demonstrated altered monocyte subpopulations in AD that varied with disease stage [41], albeit without natural killer cell or dendritic cell data. While we do not present data on disease severity, our data corroborate these findings by suggesting aberrant levels of monocyte subtypes in neurodegenerative disease. In addition, monocyte subtype redistribution may explain why total monocytes have not been found to be different in the MCI stage as compared to controls [42]. Similarly, our identification of greater CD16+ NK cell overexpression in disease adds to existing literature identifying NK cell alterations in AD versus controls, however, this study did not compare CD16+ and CD16- NK cell subtypes [43]. Peripheral myeloid DCs have previously been found to be altered in AD and Parkinson’s disease versus controls [38, 39]. While results from PC2 suggest AD may indeed be characterized by a trend of reduced myeloid DCs (Fig. 3B), these cells did not strongly correlate to PC1 or PC3, thus underscoring the potential relative importance of monocytes and NK cells in all-cause neurodegenerative dementia. In all, our work builds upon extant immunophenotyping literature and confirms monocyte and NK cell population changes with multiple neurodegenerative diseases.
Monocytes are a heterogeneous population of innate immune cells [61]. They have diverse functions: cytokine release, migration to damaged tissues, and differentiation into phagocytic cells. Based on surface markers, monocytes can be divided into classical, nonclassical, and intermediate subtypes. Classical monocytes are pro-inflammatory, potentially neurotoxic, and are recruited to damaged tissue during inflammation [62]. Nonclassical monocytes are anti-inflammatory and may be neuroprotective [63, 64]. In addition, monocytes may express functional receptors such as CCR2, a chemotaxis receptor controlling the recruitment of the cell, or TREM2, a receptor controlling phagocytic and inflammatory function [65, 66]. In contrast, NK cells in other diseases facilitate the death of infected cells, regulate the adaptive immune response through cytokine production, and mediate autoimmunity. NK cells can be subdivided based on their relative presentation of surface markers into CD16-, regulating cytokine production, or CD16+, indicating cytotoxicity [67]. NK cells have been implicated in many disorders of the central nervous system, including neurodegenerative dementia [43, 68, 69]. Finally, dendritic cells are monocyte-derived antigen presenting immune cells that have been linked to Parkinson’s disease and AD [38, 39].
Although previous evidence suggested monocyte, NK, and dendritic cells are each involved in neurodegenerative diseases, prior evidence was mainly gleaned from investigation in Alzheimer’s disease. Our results identify abnormal features of the peripheral innate immune system that are common across AD, LBD, FTD, CBS and PSP. By using data-driven analytic methods, we explore multivariate peripheral features that may not be revealed by evaluating one cellular type at a time. Innate immune patterns across the 19 cells investigated in this study identify patient groups to be dissimilar from controls and exhibit a cluster of innate immune patterns in FTLD as compared to LBD and AD. Interestingly, we confirmed cases of amyloid pathology in CBS, AD, and LBD patients. A relatively smaller distance between CBS and AD/LBD as compared to PSP and FTD suggests a shared innate immune pattern, at least in part, may reflect amyloid pathology (Fig. 1). Through the application of dimensionality reduction techniques, our results imply neurodegenerative disease to be characterized by pro-inflammatory and cytotoxic peripheral immune dynamics atypical to healthy aging.
We observed reduced PC1 loading in all-cause dementia patients versus controls (Fig. 2A). This suggests that reduced relative expression of TREM2+ on peripheral monocytes and increased relative prevalence of classical monocytes may be a characteristic pro-inflammatory and cytotoxic immune signature linked to neurodegenerative dementia. TREM2 is involved in modulating inflammation, mediating phagocytosis, and promoting myeloid cell survival [65, 70]. While the current study did not evaluate CSF levels of sTREM or CCL2, looking at TREM2 and CCR2 expressed on peripheral monocytes enables the investigation of functional dynamics of active peripheral cells accessible from blood. In the context of neurodegenerative diseases, TREM2 expressed on microglia is linked to prevention or downregulation of tau hyperphosphorylation and cited to harbour a protective effect in neurodegenerative disease [71, 72]. However, this interaction has been investigated primarily in microglia of murine models of AD rather than peripheral monocytes and human studies across the dementia spectrum. Our results support claims of TREM2 as an important receptor acting from the periphery in neurodegenerative disease [27]. While TREM2 is often reported in relation to microglia, transcriptional analyses in the human brain suggest the infiltration of TREM2 expressing monocyte-derived immune cells in patients with AD [73]. In addition, elevated levels of TREM2 transcript in peripheral blood cells is found to be protective in the clinical progression of AD [74]. Although the current study is correlational without evidence of causality, we build upon the clinical relevance of peripheral TREM2 by analysing peripheral monocyte dynamics, rather than TREM2 expressing cells alone.
In contrast to the diagnostic generalizability of PC1, patients with LBD displayed lower median individual loadings in PC3 versus controls (Fig. 4B). This third component was weighted positively by CD16- NK cells and negatively by NK Cells and CD16+ NK cells. Given CD16+ NK cells contributed to the negative arm of both PC1 and PC3, this cell type is of interest in all-cause dementia. However, LBD was particularly characterized by an increased number in NK cells and a functional shift in NK cell subtypes. Indeed, human postmortem studies show redistribution of NK cellular subtypes in patients with alpha-synuclein pathology, suggesting a potentially strong effect in this disease group [37, 75]. Beyond this, reduced average PC3 loading in LBD suggests this cohort may harbour TREM2 dynamics that are dissimilar to other dementias as these cells comprise the negative end of PC3 (opposite to PC1 composition). The present findings distinguishing LBD are in line with previous observed differences in microglial activation and TREM2 genetic relationships in LBD as compared to other diseases [18, 29, 76]. However, because we did not identify relationships between PC3 and clinical or cognitive outcomes, the relevance of NK cells in therapeutic target and monitoring of LBD patients must be further investigated.
The results presented in this study are relevant to therapeutic development and application in neurodegenerative disease. We identify inflammatory profiles that are transdiagnostic and prognostic, pointing toward the application of successful inflammatory therapeutics across neurodegenerative diseases. As there are an increasing number of immunomodulatory drugs under evaluation in dementia [77, 78], there is an increasing need to understand immune changes in neurodegeneration so that these therapies may be accurately targeted and monitored with appropriate biomarkers of response in clinical trials. This is particularly pertinent for our understanding of the functional outcomes associated with TREM2, where animal models show conflicting results [33]. Further studies are needed to clarify the functional role of TREM2 as expressed by different cells of the immune system in humans [73]. Specifically, our results probe further investigation into common features of immune profiles for the effective adaptation of treatment and disease monitoring.
The clinical relevance of shifting peripheral monocyte patterns toward a protective, anti-inflammatory phenotype is highlighted by the associations of PC1 individual loading with survival across patient groups (Fig. 5). Increased peripheral TREM2+ expression and nonclassical monocytes combined with reductions in classical monocytes and CD16+ NK cells may represent a protective effect in neurodegenerative disease, while the opposite patterns may contribute to accelerated clinical decline. Our survival analysis revealed PC1 as a strong predictor of survival over and above plasma dementia-relevant markers. This result suggests that the cell types dominating PC1 may harbour important prognostic monitoring information to be applied to clinical practice and clinical trials.
While further investigation is certainly required to establish effective PBMC biomarkers for clinical use, akin to ongoing investigations in lymphocyte/monocyte ratios [79], dynamic changes in monocyte composition (TREM2+ and classical/nonclassical monocytes) may serve as an accessible, transdiagnostic node for dementia monitoring and prediction. Moreover, the present link between increased TREM2+ monocytes and prognosis is especially relevant in light of ongoing clinical trials targeting TREM2 in people with AD [80]. Given the transdiagnostic loading of PC1, TREM2 mediated treatments may be effective in other neurodegenerative conditions. Because we did not identify any relationships between immune profiles and biomarkers of cerebral pathology measured in a subset of our participants, our results do not suggest monocyte redistribution to be a strong diagnostic or pathological biomarker for dementia, but rather may enable transdiagnostic enrichment of clinical trials and practice.
Our study has several limitations. First, patient recruitment and cohort definition are based on clinical criteria rather than pathology-confirmed cases, although clinic-pathological correlations are high for PSP, FTD, LBD and AD. Next, the heterogeneity within cohorts (e.g., grouping bvFTD with PPA) and co-pathologies (e.g., CBS underpinned by CBD and/or AD) may complicate the interpretation of the results and reduce sensitivity to between-group differences. In addition, group sizes are unbalanced, although the non-parametric tests used are relatively robust to moderate variation in group size. Although the present cohort is representative of patients who are referred in dementia clinics, future studies with larger sample sizes with more pathology-specific markers and genotyping (including APOE) may be able to clarify the interaction between innate immune system and co-pathologies across all syndromes. In addition, our cohort was predominantly white/caucasian reflecting the ethnicity distribution of the over 65-year-old population in the UK. Further studies are needed in ethnically diverse populations, to test the generalisation of our results. Importantly, ACE-R was used as the primary assessment to capture cognitive decline as this exam is widely implemented in memory clinics. However, this screening-test varies in sensitivity to the domain-specific cognitive changes associated with different diagnoses, and this may have reduced power to detect correlations with cognitive deficits. Additionally, presently investigated peripheral cell types are not dementia-specific and may capture comorbidities that are not directly linked to dementia. We have attempted to mitigate the potential confound of co-occurring inflammatory conditions, or the use of specific anti-inflammatory medication in several ways. First, the source study excluded patients with co-morbid pro-inflammatory conditions, such as rheumatoid arthritis, inflammatory bowel disease, psoriasis or other autoimmune disorders, and cancer; and all contributory cohorts excluded recent systemic infections and current acute medical illness. Moreover, we demonstrate that exclusion of the small number of patients with elevated hsCRP, indicative of systemic inflammation, does not alter the main results of the study (Supplementary Fig. S7). In this this study, we were unable to include correlations with central measures of inflammation, as imaging was not a requirement for recruitment and participant inclusion. However, recent studies have shown strong associations between blood-based inflammatory markers (i.e. cytokines) and central inflammation in dementia, as measured by TSPO PET [81]. Linking innate immune blood-based profiles with central inflammation will be a key step for future research. Finally, data collection spanned several years, which may have led to batch variation in our immunophenotyping analysis. To help control sample variability, sample gating was conducted by a single person, and validated against the gating of two other experts on a sub-sample.
In conclusion, the present study provides a comprehensive characterization of the peripheral innate immune system in multiple neurodegenerative dementias. We suggest dysfunctional patterns of the innate immune system are characteristic of neurodegenerative diseases. Blood-derived innate immune profiles can distinguish sub-populations of cells relevant to diverse clinical cohorts and their prognosis. Further studies are needed to clarify interactions between the peripheral innate immunity profiles and dementia-related events in the cerebrum, including neuroinflammation. We hope that the identification of blood-based innate immune profiles can contribute to enhanced precision medicine approaches dementia, to identify new therapeutic targets and improve clinical trial design for immunotherapies.
Data availability
Anonymized processed data can be shared upon request to the corresponding author. Raw data may also be requested but are likely to be subject to a data transfer agreement with restrictions required to comply with participant consent and data protection regulations.
References
Mason HD, McGavern DB. How the immune system shapes neurodegenerative diseases. Trends Neurosci. 2022;45(Oct):733–48.
Guerreiro R, Wojtas A, Bras J, Carrasquillo M, Rogaeva E, Majounie E, et al. TREM2 variants in Alzheimer’s disease. N Engl J Med. 2013;368(Jan):117–27.
Beecham GW, Hamilton K, Naj AC, Martin ER, Huentelman M, Myers AJ, et al. Genome-wide association meta-analysis of neuropathologic features of Alzheimer’s disease and related dementias. PLOS Genet. 2014;10(Sep):e1004606.
Naj AC, Jun G, Beecham GW, Wang LS, Vardarajan BN, Buros J, et al. Common variants at MS4A4/MS4A6E, CD2AP, CD33 and EPHA1 are associated with late-onset Alzheimer’s disease. Nat Genet. 2011;43(May):436–41.
Fernández-Santiago R, Sharma M. What have we learned from genome-wide association studies (GWAS) in Parkinson’s disease? Ageing Res Rev. 2022;79(Aug):101648.
Ferrari R, Hernandez DG, Nalls MA, Rohrer JD, Ramasamy A, Kwok JBJ, et al. Frontotemporal dementia and its subtypes: a genome-wide association study. Lancet Neurol. 2014;13(Jul):686–99.
Jabbari E, Koga S, Valentino RR, Reynolds RH, Ferrari R, Tan MMX, et al. Genetic determinants of survival in progressive supranuclear palsy: a genome-wide association study. Lancet Neurol. 2021;20(Feb):107–16.
Jonsson T, Stefansson H, Steinberg S, Jonsdottir I, Jonsson PV, Snaedal J, et al. Variant of TREM2 associated with the risk of Alzheimer’s disease. N Engl J Med. 2013;368(Jan):107–16.
Bettcher BM, Tansey MG, Dorothée G, Heneka MT. Peripheral and central immune system crosstalk in Alzheimer disease — a research prospectus. Nat Rev Neurol. 2021;17(Nov):689–701.
Alliot F, Godin I, Pessac B. Microglia derive from progenitors, originating from the yolk sac, and which proliferate in the brain. Dev Brain Res. 1999;117(Nov):145–52.
Woollacott IOC, Toomey CE, Strand C, Courtney R, Benson BC, Rohrer JD, et al. Microglial burden, activation and dystrophy patterns in frontotemporal lobar degeneration. J Neuroinflammation. 2020;17(Aug):234.
Mackenzie IRA. Activated microglia in dementia with Lewy bodies. Neurology. 2000;55(Jul):132–4.
Malpetti M, Rittman T, Jones PS, Cope TE, Passamonti L, Bevan-Jones WR, et al. In vivo PET imaging of neuroinflammation in familial frontotemporal dementia. J Neurol Neurosurg Psychiatry. 2021;92(Mar):319–22.
Malpetti M, Passamonti L, Rittman T, Jones PS, Vázquez Rodríguez P, Bevan-Jones WR, et al. Neuroinflammation and Tau colocalize in vivo in progressive supranuclear palsy. Ann Neurol. 2020;88:1194–204.
Malpetti M, Kievit RA, Passamonti L, Jones PS, Tsvetanov KA, Rittman T, et al. Microglial activation and tau burden predict cognitive decline in Alzheimer’s disease. Brain. 2020;143(May):1588–602.
Malpetti M, Cope TE, Street D, Jones PS, Hezemans FH, Mak E, et al. Microglial activation in the frontal cortex predicts cognitive decline in frontotemporal dementia. Brain. 2023 Mar:awad078.
Hopperton KE, Mohammad D, Trépanier MO, Giuliano V, Bazinet RP. Markers of microglia in post-mortem brain samples from patients with Alzheimer’s disease: a systematic review. Mol Psychiatry. 2018;23(Feb):177–98.
Amin J, Holmes C, Dorey RB, Tommasino E, Casal YR, Williams DM, et al. Neuroinflammation in dementia with Lewy bodies: a human post-mortem study. Transl Psychiatry. 2020;10(Aug):1–11.
Finze A, Biechele G, Rauchmann BS, Franzmeier N, Palleis C, Katzdobler S, et al. Individual regional associations between Aβ-, tau- and neurodegeneration (ATN) with microglial activation in patients with primary and secondary tauopathies. Mol Psychiatry. 2023 Jul;1–13.
Roh JS, Sohn DH. Damage-associated molecular patterns in inflammatory diseases. Immune Netw. 2018;18(Aug):e27.
Møllgård K, Beinlich FRM, Kusk P, Miyakoshi LM, Delle C, Plá V, et al. A mesothelium divides the subarachnoid space into functional compartments. Science. 2023;379(Jan):84–8.
Louveau A, Harris TH, Kipnis J. Revisiting the mechanisms of CNS immune privilege. Trends Immunol. 2015;36(Oct):569–77.
Ferro A, Auguste YSS, Cheadle L Microglia, Cytokines, and Neural Activity: Unexpected Interactions in Brain Development and Function. Front Immunol [Internet]. 2021 [cited 2023 Jan 29];12. Available from: https://www.frontiersin.org/articles/10.3389/fimmu.2021.703527
Litvin DG, Denstaedt SJ, Borkowski LF, Nichols NL, Dick TE, Smith CB, et al. Peripheral-to-central immune communication at the area postrema glial-barrier following bleomycin-induced sterile lung injury in adult rats. Brain Behav Immun. 2020;87(Jul):610–33.
Riazi K, Galic MA, Kuzmiski JB, Ho W, Sharkey KA, Pittman QJ. Microglial activation and TNFα production mediate altered CNS excitability following peripheral inflammation. Proc Natl Acad Sci. 2008;105(Nov):17151–6.
Wohleb ES, Fenn AM, Pacenta AM, Powell ND, Sheridan JF, Godbout JP. Peripheral innate immune challenge exaggerated microglia activation, increased the number of inflammatory CNS macrophages, and prolonged social withdrawal in socially defeated mice. Psychoneuroendocrinology. 2012;37(Sep):1491–505.
Fahrenhold M, Rakic S, Classey J, Brayne C, Ince PG, Nicoll JAR, et al. TREM2 expression in the human brain: a marker of monocyte recruitment? Brain Pathol. 2017;28(Oct):595–602.
Amin J, Boche D, Clough Z, Teeling J, Williams A, Gao Y, et al. Peripheral immunophenotype in dementia with Lewy bodies and Alzheimer’s disease: an observational clinical study. J Neurol Neurosurg Psychiatry. 2020;91(Nov):1219–26.
Surendranathan A, Su L, Mak E, Passamonti L, Hong YT, Arnold R, et al. Early microglial activation and peripheral inflammation in dementia with Lewy bodies. Brain. 2018;141(Dec):3415–27.
Rentzos M, Zoga M, Paraskevas GP, Kapaki E, Rombos A, Nikolaou C, et al. IL-15 Is elevated in cerebrospinal fluid of patients with Alzheimer’s disease and frontotemporal dementia. J Geriatr Psychiatry Neurol. 2006;19(Jun):114–7.
Fernández-Botrán R, Ahmed Z, Crespo FA, Gatenbee C, Gonzalez J, Dickson DW, et al. Cytokine expression and microglial activation in progressive supranuclear palsy. Parkinsonism Relat Disord. 2011;17(Nov):683–8.
Perry VH, Cunningham C, Holmes C. Systemic infections and inflammation affect chronic neurodegeneration. Nat Rev Immunol. 2007;7(Feb):161–7.
Jay TR, von Saucken VE, Landreth GE. TREM2 in Neurodegenerative Diseases. Mol Neurodegener. 2017;12(Aug):56.
Ewers M, Franzmeier N, Suárez-Calvet M, Morenas-Rodriguez E, Caballero MAA, Kleinberger G, et al. Increased soluble TREM2 in cerebrospinal fluid is associated with reduced cognitive and clinical decline in Alzheimer’s disease. Sci Transl Med. 2019;11(Aug):eaav6221.
Westin K, Buchhave P, Nielsen H, Minthon L, Janciauskiene S, Hansson O. CCL2 is associated with a faster rate of cognitive decline during early stages of Alzheimer’s disease. PLOS ONE. 2012;7(Jan):e30525.
Jadidi-Niaragh F, Shegarfi H, Naddafi F, Mirshafiey A. The role of natural killer cells in Alzheimer’s disease. Scand J Immunol. 2012;76:451–6.
Earls RH, Lee JK. The role of natural killer cells in Parkinson’s disease. Exp Mol Med. 2020;52(Sep):1517–25.
Ciaramella A, Salani F, Bizzoni F, Orfei MD, Caltagirone C, Spalletta G, et al. Myeloid dendritic cells are decreased in peripheral blood of Alzheimer’s disease patients in association with disease progression and severity of depressive symptoms. J Neuroinflammation. 2016;13(Jan):18.
Ciaramella A, Salani F, Bizzoni F, Pontieri FE, Stefani A, Pierantozzi M, et al. Blood dendritic cell frequency declines in idiopathic Parkinson’s disease and is associated with motor symptom severity. PLOS ONE. 2013;8(Jun):e65352.
Ciaramella A, Sanarico N, Bizzoni F, Moro ML, Salani F, Scapigliati G, et al. Amyloid β peptide promotes differentiation of pro-inflammatory human myeloid dendritic cells. Neurobiol Aging. 2009;30(Feb):210–21.
Thome AD, Faridar A, Beers DR, Thonhoff JR, Zhao W, Wen S, et al. Functional alterations of myeloid cells during the course of Alzheimer’s disease. Mol Neurodegener. 2018;13(Nov):61.
Magaki S, Yellon SM, Mueller C, Kirsch WM. Immunophenotypes in the circulation of patients with mild cognitive impairment. J Psychiatr Res. 2008;42(Feb):240–6.
Martins LCA, Rocha NP, Torres KCL, dos Santos RR, França GS, de Moraes EN, et al. Disease-specific expression of the serotonin-receptor 5-HT2C in natural killer cells in Alzheimer’s dementia. J Neuroimmunol. 2012;251(Oct):73–9.
McKhann GM, Knopman DS, Chertkow H, Hyman BT, Jack CR Jr, Kawas CH, et al. The diagnosis of dementia due to Alzheimer’s disease: Recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement. 2011;7:263–9.
Albert MS, DeKosky ST, Dickson D, Dubois B, Feldman HH, Fox NC, et al. The diagnosis of mild cognitive impairment due to Alzheimer’s disease: Recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement. 2011;7:270–9.
Höglinger GU, Respondek G, Stamelou M, Kurz C, Josephs K a., Lang AE, et al. Clinical diagnosis of progressive supranuclear palsy: The movement disordersociety criteria. Movement Disorders. 2017;32:853–64.
Armstrong MJ, Litvan I, Lang AE, Bak TH, Bhatia KP, Borroni B, et al. Criteria for thediagnosis of corticobasal degeneration. Neurology. 2013;80:496–503.
Rascovsky K, Hodges JR, Knopman D, Mendez MF, Kramer JH, Neuhaus J, et al. Sensitivity of revised diagnostic criteria for the behavioural variant of frontotemporal dementia. Brain. 2011;134:2456–77.
Gorno-Tempini, Maria Luisa, et al. Classification of primary progressive aphasia and its variants. Neurology 2011;76.11:1006–14.
McKeith IG, Boeve BF, Dickson DW, Halliday G, Taylor JP, Weintraub D, et al. Diagnosis and management of dementia with Lewy bodies. Neurology. 2017;89:88–100.
Jack Jr CR, Wiste HJ, Weigand SD, Therneau TM, Lowe VJ, Knopman DS, et al.. Defining imaging biomarker cut points for brain aging and Alzheimer’s disease. Alzheimer’s & Dementia. 20171;13:205–16.
Keshavan A, O’Shea F, Chapman MD, Hart MS, Lunn MP, Paterson RW, et al. CSF biomarkers for dementia. Pract Neurol. 2022;22(Aug):285.
Bevan-Jones WR, Surendranathan A, Passamonti L, Rodríguez PV, Arnold R, Mak E, et al. Neuroimaging of Inflammation in Memory and Related Other Disorders (NIMROD) study protocol: a deep phenotyping cohort study of the role of brain inflammation in dementia, depression and other neurological illnesses. BMJ Open. 2017;7(Jan):e013187.
Maecker HT, McCoy JP, Nussenblatt R. Standardizing immunophenotyping for the Human Immunology Project. Nat Rev Immunol. 2012;12(Mar):191–200.
Ashton NJ, Brum WS, Di Molfetta G, Benedet AL, Arslan B, Jonaitis E, et al. Diagnostic Accuracy of a Plasma Phosphorylated Tau 217 Immunoassay for Alzheimer Disease Pathology. JAMA Neurol [Internet]. 2024 Jan [cited 2024 Jan 24]; Available from: https://jamanetwork.com/journals/jamaneurology/fullarticle/2813751
Breunig MM, Kriegel HP, Ng RT, Sander J. LOF: identifying density-based local outliers. ACM. SIGMOD Rec. 2000;29(Jun):93–104.
Thorndike RL. Who belongs in the family? Psychometrika. 1953;18(Dec):267–76.
Syakur MA, Khotimah BK, Rochman EMS, Satoto BD. Integration K-means clustering method and elbow method for identification of the best customer profile cluster. IOP Conf Ser Mater Sci Eng. 2018;336(Apr):012017.
Zhang YR, Wang JJ, Chen SF, Wang HF, Li YZ, Ou YN, et al. Peripheral immunity is associated with the risk of incident dementia. Mol Psychiatry. 2022;27(Apr):1956–62.
Prinz M, Priller J, Sisodia SS, Ransohoff RM. Heterogeneity of CNS myeloid cells and their roles in neurodegeneration. Nat Neurosci. 2011;14(Oct):1227–35.
Sprangers S, Vries TJde, Everts V. Monocyte heterogeneity: consequences for monocyte-derived immune cells. J Immunol Res. 2016;2016:1475435.
Russo MV, Latour LL, McGavern DB. Distinct myeloid cell subsets promote meningeal remodeling and vascular repair after mild traumatic brain injury. Nat Immunol. 2018;19(May):442–52.
Ziegler-Heitbrock L Blood Monocytes and Their Subsets: Established Features and Open Questions. Front Immunol [Internet]. 2015 [cited 2023 Jun 12];6. Available from: https://www.frontiersin.org/articles/10.3389/fimmu.2015.00423.
Berriat F, Lobsiger CS, Boillée S. The contribution of the peripheral immune system to neurodegeneration. Nat Neurosci. 2023;26(Jun):942–54.
Colonna M The biology of TREM receptors. Nat Rev Immunol. 2023 Feb;1–15.
Serbina NV, Pamer EG. Monocyte emigration from bone marrow during bacterial infection requires signals mediated by chemokine receptor CCR2. Nat Immunol. 2006;7(Mar):311–7.
Cooper MA, Fehniger TA, Caligiuri MA. The biology of human natural killer-cell subsets. Trends Immunol. 2001;22(Nov):633–40.
Poli A, Kmiecik J, Domingues O, Hentges F, Bléry M, Chekenya M, et al. NK cells in central nervous system disorders. J Immunol. 2013;190(Jun):5355–62.
Poli A, Michel T, Thérésine M, Andrès E, Hentges F, Zimmer J. CD56bright natural killer (NK) cells: an important NK cell subset. Immunology. 2009;126:458–65.
Deczkowska A, Weiner A, Amit I. The physiology, pathology, and potential therapeutic applications of the TREM2 signaling pathway. Cell. 2020;181(Jun):1207–17.
Peng X, Guo H, Zhang X, Yang Z, Ruganzu JB, Yang Z, et al. TREM2 inhibits tau hyperphosphorylation and neuronal apoptosis via the PI3K/Akt/GSK-3β signaling pathway in vivo and in vitro. Mol Neurobiol. 2023;60(May):2470–85.
Gratuze M, Leyns CEG, Holtzman DM. New insights into the role of TREM2 in Alzheimer’s disease. Mol Neurodegener. 2018;13(Dec):66.
Silvin A, Uderhardt S, Piot C, Da Mesquita S, Yang K, Geirsdottir L, et al. Dual ontogeny of disease-associated microglia and disease inflammatory macrophages in aging and neurodegeneration. Immunity. 2022;55(Aug):1448–1465.e6.
Casati M, Ferri E, Gussago C, Mazzola P, Abbate C, Bellelli G, et al. Increased expression of TREM2 in peripheral cells from mild cognitive impairment patients who progress into Alzheimer’s disease. Eur J Neurol. 2018;25:805–10.
Earls RH, Menees KB, Chung J, Gutekunst CA, Lee HJ, Hazim MG, et al. NK cells clear α-synuclein and the depletion of NK cells exacerbates synuclein pathology in a mouse model of α-synucleinopathy. Proc Natl Acad Sci USA. 2020;117(Jan):1762–71.
Walton RL, Soto-Ortolaza AI, Murray ME, Lorenzo-Betancor O, Ogaki K, Heckman MG, et al. TREM2 p.R47H substitution is not associated with dementia with Lewy bodies. Neurol Genet. 2016;2(Jul):e85.
Albertini C, Petralla S, Massenzio F, Monti B, Rizzardi N, Bergamini C. et al. Targeting Lewy body dementia with neflamapimod-rasagiline hybrids. Arch Pharm (Weinheim). 2024;357(Jun):e2300525
Cummings J, Zhou Y, Lee G, Zhong K, Fonseca J, Cheng F. Alzheimer’s disease drug development pipeline: 2024. Alzheimers Dement Transl Res Clin Interv. 2024;10(Apr):e12465.
Mehta NH, Zhou L, Li Y, McIntire LB, Nordvig A, Butler T, et al. Peripheral immune cell imbalance is associated with cortical beta-amyloid deposition and longitudinal cognitive decline. Sci Rep. 2023;13(May):8847.
George J. TREM2 as an evolving therapeutic target in Alzheimer’s disease. Neural Regen Res. 2023;18(Apr):2680–1.
Malpetti M, Swann P, Tsvetanov KA, Chouliaras L, Strauss A, Chikaura T, et al. Blood inflammation relates to neuroinflammation and survival in frontotemporal lobar degeneration. Brain. 2024 Aug;awae269.
Acknowledgements
This study was co-funded by the Dementias Platform UK and Medical Research Council (MC_UU_00030/14; MR/T033371/1); Race Against Dementia Alzheimer’s Research UK (ARUK-RADF2021A-010); the Wellcome trust (103838; 220258); the Cambridge University Centre for Parkinson-Plus (RG95450); the National Institute for Health Research (NIHR) Cambridge Biomedical Research Centre (BRC-1215-20014; NIHR203312: the views expressed are those of the authors and not necessarily those of the NIHR or the Department of Health and Social Care); the Progressive Supranuclear Palsy Association (PSPA2022/SMALL GRANTS002); the Addenbrookes Charitable Trust (Ref: 900380). HZ is a Wallenberg Scholar and a Distinguished Professor at the Swedish Research Council supported by grants from the Swedish Research Council (#2023-00356; #2022-01018 and #2019-02397), the European Union’s Horizon Europe research and innovation programme under grant agreement No 101053962, and Swedish State Support for Clinical Research (#ALFGBG-71320). For the purpose of open access, the authors have applied a Creative Commons Attribution (CC BY) license to any Author Accepted Manuscript version arising from this submission. This work is licensed under a Creative Commons Attribution 4.0 International License. We thank our participant volunteers for their participation in this study, thank the National Institute for Health Research (NIHR) Cambridge BioResource centre staff, and the research nurses for their contribution, the staff at the NIHR Cambridge Cell Phenotyping Hub at the university of Cambridge and the East Anglia Dementias and Neurodegenerative Diseases Research Network (DeNDRoN) for help with subject recruitment.
Author information
Authors and Affiliations
Contributions
AS, PS, SLK, RC, NS, LT, AGM, LC, NS, NJA, GS, WRBJ, AS, JBR, JOB and MM contributed to study execution, data collection and/or analysis. AS and MM drafted the first version of the manuscript. KB, HZ, MM oversaw the sample and data analysis. MM conceptualised the study, JBR and JOB contributed to the study design. All authors reviewed the manuscript and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors have no conflicts of interest to report related to this work. Unrelated to this work, JTO has received honoraria for work as DSMB chair or member for TauRx, Axon, Eisai and Novo Nordisk, and has acted as a consultant for Biogen and Roche, and has received research support from Alliance Medical and Merck. JBR is a non-remunerated trustee of the Guarantors of Brain, Darwin College and the PSP Association (UK). He provides consultancy unrelated to the current work to Asceneuron, Alector, Astronautx, Astex, Curasen, ClinicalInk, CumulusNeuro, Wave, SVHealth, and has research grants from AZ-Medimmune, Janssen, and Lilly as industry partners in the Dementias Platform UK. M.M. has acted as a consultant for Astex Pharmaceuticals. H.Z. has served at scientific advisory boards and/or as a consultant for Abbvie, Acumen, Alector, Alzinova, ALZPath, Amylyx, Annexon, Apellis, Artery Therapeutics, AZTherapies, Cognito Therapeutics, CogRx, Denali, Eisai, LabCorp, Merry Life, Nervgen, Novo Nordisk, Optoceutics, Passage Bio, Pinteon Therapeutics, Prothena, Red Abbey Labs, reMYND, Roche, Samumed, Siemens Healthineers, Triplet Therapeutics, and Wave, has given lectures in symposia sponsored by Alzecure, Biogen, Cellectricon, Fujirebio, Lilly, Novo Nordisk, and Roche, and is a co-founder of Brain Biomarker Solutions in Gothenburg AB (BBS), which is a part of the GU Ventures Incubator Program (outside submitted work).
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Strauss, A., Swann, P., Kigar, S.L. et al. Peripheral innate immunophenotype in neurodegenerative disease: blood-based profiles and links to survival. Mol Psychiatry 30, 1985–1994 (2025). https://doi.org/10.1038/s41380-024-02809-w
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41380-024-02809-w
This article is cited by
-
Spilling the T: T cells in tauopathy mechanisms, disease progression, and therapeutic horizons
Molecular Neurodegeneration Advances (2026)