Abstract
Childhood maltreatment is increasingly recognized as a pivotal risk factor for adverse health outcomes. However, comprehensive analyses of its long-term impact are scarce. This study aims to fill this gap by examining the genetic architectures of childhood maltreatment and its influence on adult health and socioeconomic outcomes. Utilizing data from the UK Biobank (N = 129,017), we conducted sex-combined and sex-stratified genome-wide association studies to identify genomic loci associated with five childhood maltreatment subtypes. We then performed genetic correlation and Mendelian randomization (MR) analyses to assess the effects of childhood maltreatment on high-burden diseases, healthcare costs, lifespan, and educational attainment. We identified several novel loci for childhood maltreatment, including one locus for sexual abuse in sex-combined analysis, one novel locus for sexual abuse in males, one locus for emotional neglect in females, and one locus for sexual abuse in females. The pairwise genetic correlations between subtypes of childhood maltreatment were moderate to high, and similar patterns of genetic correlations between childhood maltreatment subtypes were observed in males and females. Childhood maltreatment was genetically correlated with ten out of 16 high-burden diseases significantly after multiple testing correction. Moreover, MR analyses suggest childhood maltreatment may increase the risk of age-related and other hearing loss, low back pain, major depressive disorder, and migraine in adulthood, and reduce the lifespan. Our study elucidates the genetic architecture of specific childhood maltreatment subtypes and the influence of childhood maltreatment on health outcomes in adulthood, highlighting the enduring influence of childhood maltreatment on lifelong health consequences. It is important to develop prevention strategies to lower the incidence of childhood maltreatment and provide support and care for victims of childhood maltreatment for better long-term health outcomes in the population.
Similar content being viewed by others
Introduction
Childhood maltreatment is an important and widespread public health issue across continents [1]. Prevalence of childhood maltreatment varied across sex and maltreatment categories [2] and it is believed that many cases still remained hidden and unreported [1]. For example, in a previous epidemiological study, it was reported that the prevalence of childhood sexual abuse were as high as 20.4% in North America, 9.0% in Asia and 14.3% in Europe among girls, and 14.1% in North America, 6.7% in Asia and 6.2% in Europe among boys [2]. Growing evidence from previous epidemiological studies suggests that childhood maltreatment is an important risk factor for lifelong negative consequences of mental and physical health [3,4,5,6,7], mortality [8, 9], academic performance [10], educational attainment [11], and social life [4, 5]. However, conventional epidemiological studies are often subject to potential confounding despite the effort to control for confounding in statistical analysis. Moreover, to evaluate the impact of childhood maltreatment on health outcome in adulthood, conventional epidemiological studies may require a long follow-up time for data collection.
Latest advances in genome-wide association studies (GWASs) have revealed heritable components in various risk factors, and health outcomes, and identified genetic variants associated with these conditions. As such, Mendelian randomization (MR) - a powerful statistical method to provide evidence of causal effects - has gained popularity due to the fact that readily available GWAS summary statistics can now provide the necessary genetic instruments for MR analysis. By leveraging genetic instruments, MR can be used to estimate the causal effect of an exposure, such as childhood maltreatment in this study, to an outcome in the presence of unobserved confounding [12]. In contrast to conventional epidemiological study, MR analysis does not require data on confounders to yield an unbiased effect estimate of childhood maltreatment, and does not require childhood maltreatment and adulthood health outcome data to be collected in the same sample (in the two-sample MR setting).
Previous GWASs have identified 14 independent genomic loci for childhood maltreatment [13, 14], providing an opportunity to leverage MR analysis to evaluate the impact of childhood maltreatment on adulthood health outcomes. In fact, previous MR analyses showed that overall childhood maltreatment may increase the risk of depression, schizophrenia, and attention deficit hyperactivity disorder but not the risk of coronary artery disease, type 2 diabetes mellitus (T2DM), and C-reactive protein [14]. However, genetic architectures for specific subtypes of childhood maltreatment remain unclear, despite the reported genetic overlap among subtypes of childhood maltreatment (genetic correlations: 0.24–1.00) [14]. In addition, sex differences were observed in the prevalence of childhood maltreatment [2], which suggests that sex-specific effects may be present for childhood maltreatment on health outcomes, which warrants further investigation.
Although previous studies reported childhood maltreatment as an important risk factor for negative health consequences later in life, there has not been a systematic investigation of the impact of childhood maltreatment on disease burden, health economics and outcomes in adulthood. In this study, we aim to investigate the impact of childhood maltreatment on high burden diseases, healthcare costs in adulthood, lifespan, and educational attainment. We first performed genome-wide association analysis to identify genomic loci associated with specific subtypes of childhood maltreatment, including both sex-combined and sex-stratified analysis. Based on the genome-wide analysis results, we then performed genetic correlation and MR analyses to identify causal effects of childhood maltreatment on high burden diseases and healthcare costs in adulthood, lifespan, and educational attainment.
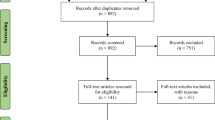
Methods
Subjects
We used data from the UK Biobank (UKB), a prospective cohort study of the UK population with over 500,000 participants aged 40–69 years at recruitment between 2006 and 2010 [15]. Extensive phenotype data were collected, including surveys on baseline characteristics and health outcomes, specific questionnaires and assessments, inpatient hospital records, physical measures and biomarkers [16].
Genotype data
We obtained imputed genotype data from UKB and filtered out variants and samples with additional quality control (QC) criteria. The imputed genotype data included more than 90 million variants for all participants by using the Haplotype Reference Consortium (HRC) and UK10K plus 1000 Genomes Project (1KG) reference panels [17,18,19]. First, we filtered out variants with imputation quality INFO score <0.8 and variants with minor allele frequency (MAF) < 0.01 by PLINK v2.0 [20]. Second, we filtered out samples with discordant gender in self-reported data and genetic data, samples showing sex chromosome aneuploidies, as well as samples who had withdrawn from the UKB (as of August 24, 2020). Next, we identified UKB samples of European ancestry by using principal component analysis (PCA) with 1KG reference samples [21], in which the PCA were implemented in PLINK v2.0 [20] using the LD-pruned SNPs (at R2 = 0.2 with a 500 kb window). We excluded samples of non-European ancestry to minimize bias from population stratification [22], and we also excluded population outliers in samples of European ancestry by conducting three rounds of in-sample PCA. Samples with any of the top 10 principal components (PCs) that were more than five standard deviations away from the sample average in each round of the in-sample PCA were excluded. We performed a final in-sample PCA to derived PCs for population stratification adjustment in the following genetic analyses.
Childhood maltreatment
Five subtypes of childhood maltreatment, including emotional abuse, emotional neglect, physical abuse, physical neglect, and sexual abuse, were collected from 157,298 UKB samples through self-report with an online questionnaire of five frequency scale questions (data fields 20487, 20488, 20489, 20490, and 20491). We converted the frequency scales, including “never”, “rarely”, “sometimes”, “often”, and “very often”, into binary phenotypes based on the following criteria considering the event described in the questionnaire (Supplementary Table 1): 1) Emotional abuse (felt hated by family member as a child; data field 20487): sometimes or more frequent (≥2) as cases vs. rarely or less frequent (<2) as controls; 2) Emotional neglect (felt loved as a child [inverted scale for traumatic experience]; data field 20489): rarely or less frequent (≤1) as cases vs. some times or more frequent (>1) as controls; 3) Physical abuse (physically abused by family as a child; data field 20488): sometimes or more frequent (≥2) as cases vs. rarely or less frequent (<2) as controls; 4) Physical neglect (someone to take to doctor when needed as a child [inverted scale for traumatic experience]; data field 20491): rarely or less frequent (≤1) as cases vs. some times or more frequent (>1) as controls; 5) Sexual abuse (Sexually molested as a child; data field 20490): rarely or more frequent (≥1) as cases vs. never (<1) as controls [23, 24]. We derived an overall childhood maltreatment score by extracting the first PC in a PCA on the binary phenotypes of the five individual childhood maltreatment subtypes.
Genetic association analysis for childhood maltreatment
To assess the genetic architecture of childhood maltreatment, we performed genetic association analyses on specific childhood maltreatment, including the PCA-derived overall maltreatment, emotional abuse, emotional neglect, physical abuse, physical neglect, and sexual abuse, by using post-QC imputed genotype data from 129,017 samples with complete data for five self-reported childhood maltreatment subtypes. We then performed sex-stratified genetic association analyses to investigate sex differences in childhood maltreatment using the same approaches and criteria in sex-combined analysis (Nmale = 56,977; Nfemale = 72,040). In these GWASs, we used two-step whole-genome regression models implemented in Regenie v1.0.5.4 with adjustment for genotyping batch and the top 20 PCs in sex-combined analysis as well as in sex-stratified analysis. Participants without complete data for five self-reported childhood maltreatment subtypes were excluded from genetic association analyses, and we filtered out variants with imputation INFO < 0.8 and MAF < 1%. We identified the significant loci for childhood maltreatment using FUMA [25] and showed regional plots for these loci using LocusZoom v0.14.0 [26].
Outcomes
We chose leading causes of disease burden, healthcare costs, lifespan, and educational attainment as our primary outcomes for a comprehensive assessment. This strategy helped us examine childhood maltreatment’s wide-ranging effects, encompassing specific major diseases and broader health and socioeconomic impacts in adulthood. Our focus on these areas was intended to deeply understand the influence of early adverse experiences on an individual’s lifelong health risks and burdens across various interconnected domains.
We investigated the impact of childhood maltreatment on our primary outcomes. High burden diseases in adulthood were selected from the top 10 causes of disease burden worldwide reported by Global Burden of Disease in 2019 and the top 10 “level 4” causes of years of life lost and years lived with disability in 2019 [27]. We then excluded two duplicated causes and two causes without suitable GWAS summary statistics, yielding 16 high burden diseases in adulthood in this study. The detailed information of GWAS summary statistics for 16 high burden diseases in adulthood were summarized in Supplementary Table 2, including age-related and other hearing loss, anxiety disorders, breast cancer, chronic obstructive pulmonary disease, colon and rectum cancer, hypertensive heart disease, intracerebral hemorrhage, ischemic heart disease, ischemic stroke, low back pain, major depressive disorder (MDD), migraine, neck pain, any stroke, tracheal, bronchus, and lung cancer, and T2DM. We obtained GWAS summary statistics for healthcare costs from Lee et al. [28], lifespan from Timmers et al. [29], and years of schooling from Okbay et al. [30].
Heritability, phenotypic, and genetic correlation analyses
We performed Linkage Disequilibrium Score Regression (LDSC) v1.0.1 with the GWAS summary data to estimate the observed scale SNP-based heritability of childhood maltreatment and high burden diseases using pre-calculated LD scores for Europeans based on the 1KG Project phase 3 data from the LDSC website (https://github.com/bulik/ldsc) [31]. For five binary childhood maltreatment subtypes, we also performed LDSC to estimate the liability scale SNP-based heritability, in which we used median prevalence reported in Moody et al. 2018 as the population prevalence [2]. For 16 high burden diseases, we used the population prevalence reported in the original paper or population prevalence estimated in FinnGen to estimate the liability scale SNP-based heritability using LDSC (Supplementary Table 2). We applied Spearman rank correlation analysis to estimate the pairwise phenotypic correlations between subtypes of childhood maltreatment. For genetic correlations, we performed LDSC to estimate the genetic correlations between subtypes of childhood maltreatment and between specific childhood maltreatment and high burden diseases [32]. For variant QC, we excluded strand ambiguous SNPs and variants with imputation INFO < 0.8 and MAF < 1% in LDSC analyses.
Mendelian randomization
To investigate the causal relationships between childhood maltreatment and health-related outcomes, we applied a two-sample MR by using genetic variants as instrumental variables [33,34,35]. First, we performed LD clumping with a r2 threshold of 0.01 on SNPs with an association P-value < 1.0 × 10−5 to retain only approximately independent SNPs as genetic instruments. Following previous MR studies, we used a relaxed threshold to improve the power of MR by including more genetic instruments for childhood maltreatment [36,37,38]. Next, we harmonized childhood maltreatment and outcome data by aligning the effect alleles between the two studies/datasets. We removed palindromic SNPs with a MAF > 0.42 and aligned the strands for palindromic SNP with MAF ≤ 0.42 by matching MAF across childhood maltreatment and outcome data. When the SNPs were not available in the outcome summary data, we included proxy SNPs with the highest LD (r2 ≥ 0.8). Proxy SNPs were weighted by the effect size of the variant for which they are a proxy. Subsequently, we estimated the causal effects of childhood maltreatment on each outcome, including 16 high burden diseases, healthcare costs, lifespan, and educational attainment, by using the inverse-variance weighted (IVW) method as the main MR analysis and the weighted median approach as sensitivity analysis. We also performed the exploratory MR analysis to estimate the sex-specific causal effect of childhood maltreatment on outcomes. Sex-stratified GWASs for most of the outcomes in this study were not available; therefore, we used sex-combined GWASs for 15 high burden diseases (i.e., with the exclusion of breast cancer), healthcare costs, lifespan, and educational attainment in sex-stratified MR analysis. To check for horizontal pleiotropy, we performed a MR-PRESSO [39] test to detect pleiotropic outliers and to correct for horizontal pleiotropy via outlier removal. We also performed the test for the intercept in the MR-Egger regression as well as the MR-Egger test [40] and Cochran’s Q test for heterogeneity.
Results
Genome-wide associations for childhood maltreatment
We performed GWASs for the PC-derived overall maltreatment (Supplementary Figure 1) and five subtypes of childhood maltreatment, including emotional abuse (Supplementary Figure 2), emotional neglect (Supplementary Figure 3), physical abuse (Supplementary Figure 4), physical neglect (Supplementary Figure 5), and sexual abuse (Fig. 1), with stringent QC and imputed genotypic data from 129,017 samples. The λGC ranged from 1.032–1.140 and LDSC intercepts ranged from 1.007–1.019 for childhood maltreatment, which suggested minimal bias due to population stratification (Fig. 1b, Supplementary Figure 6a–e, and Supplementary Table 3). We identified two genome-wide significant loci (P-value < 5.0 × 10−8) from the GWAS for the overall maltreatment (Supplementary Figure 1 & 7 and Supplementary Table 4, 5). Both loci were previously reported in Warrier et al. 2021 [14]. For subtypes of childhood maltreatment, we identified one genome-wide significant locus with leading associated variants rs1387776 (nearest gene: RP11-644C3.1) from the GWAS for sexual abuse (Fig. 1c and Supplementary Table 4, 5), which was reported for the first time (defined by not located within ± 500 kb of the previously reported lead SNPs [13, 14]). No significant loci were identified for the remaining four childhood maltreatment subtypes.
a Manhattan plot. The x axis represents chromosomal position, and the y axis represents the –log10(P-value) for association of variants with sexual abuse. The horizontal red dashed line marks the threshold for genome-wide significance (P-value = 5 × 10−8). b Quantile-Quantile (Q-Q) plot. The x axis and y axis represent the expected value and the observed value of –log10(P-value) for association of variants with sexual abuse, respectively. The red dashed line marks the diagonal line. c Regional association plot in a genome-wide significant locus rs1387776. The x axis represents the chromosomal position, and the y axis represents the –log10(P-value) for association of variants with sexual abuse. LD estimates of surrounding SNPs with the index SNP are indicated by color. Note that LINC01208 is the alternative name for RP11-644C3.1 (Supplementary Table 5).
Next, we performed sex-stratified GWAS for childhood maltreatment (Supplementary Figure 8–19 and Supplementary Table 3). In males, rs12879558 (nearest gene: TMEM260) showed genome-wide significant association (P-value < 5.0 × 10−8) with sexual abuse (Supplementary Figure 13 & 20 and Supplementary Table 4, 5). This is the first time that TMEM260 was reported to be associated with childhood maltreatment. In females, we identified a genome-wide significant variant rs6974757 (nearest gene: FOXP2) for the overall maltreatment (Supplementary Figure 14 & 21 and Supplementary Table 4, 5); a genome-wide significant variant rs4727799 (nearest gene: FOXP2) for emotional abuse (Supplementary Figure 15 & 22 and Supplementary Table 4, 5); two genome-wide significant variants rs4326125 (nearest gene: RP11-32D16.1) and rs6974757 (nearest gene: FOXP2) for emotional neglect (Supplementary Figure 16 & 23 and Supplementary Table 4, 5); and a genome-wide significant variant rs1901175 (nearest gene: KCNV1) for sexual abuse (Supplementary Figure 19 & 24 and Supplementary Table 4, 5). The loci with leading SNPs rs12879558, rs4326125, and rs1901175 were novel findings that were not reported in previous GWASs.
Heritability
We estimated the SNP-based heritability for overall maltreatment and five subtypes of childhood maltreatment using LDSC. The observed scale SNP-based heritability of the childhood maltreatment ranged from 0.9–6.3% in all samples, from 0.8–5.6% in males, and from 1.9–7.7% in females (Fig. 2a and Supplementary Table 3), and the liability scale SNP-based heritability of the childhood maltreatment subtypes ranged from 10.2–20.6% in all samples, from 8.6–19.6% in males, and from 10.8–24.6% in females (Supplementary Figure 25 and Supplementary Table 3). The overall maltreatment has the highest heritability among six childhood maltreatment traits. Most of these heritability were statistically significant (P-value < 0.05) except for physical neglect in males. For completeness, we still included all subtypes of childhood maltreatment in the following genetic correlation and MR analysis.
a Observed scale SNP-based heritability. We performed the linkage disequilibrium score regression (LDSC) to estimate the observed scale SNP-based heritability of childhood maltreatment. The x axis represents the childhood maltreatment, and the y axis represents the SNP-based heritability. Error bars (black line) are 95% confidence intervals. b Pairwise genetic correlation for childhood maltreatment in combined sexes. c Pairwise genetic correlation for childhood maltreatment in males. d Pairwise genetic correlation for childhood maltreatment in females. In panel b–d, * indicates the P-value < 0.0033 (Bonferroni corrected significance level = 0.05/15 = 0.0033), and lines show the dendrogram of the hierarchical clustering based on average linkage and Euclidean distance.
Phenotypic and genetic architecture of childhood maltreatment
We observed low to moderate positive phenotypic correlations between childhood maltreatment phenotypes, ranging from 0.05 to 0.65 (Supplementary Figure 26a and Supplementary Table 6). Phenotypically, overall maltreatment showed moderate correlations with emotional abuse, physical abuse, emotional neglect, and sexual abuse (r = 0.514–0.647) and a relatively lower correlation with physical neglect (r = 0.310), while the childhood maltreatment subtypes are also showing high phenotypic correlation except physical neglect (Supplementary Table 6). In sex-stratified analysis, we showed similar patterns of pairwise phenotypic correlations between childhood maltreatment phenotypes (Supplementary Figure 26b–c).
Genetically, we observed moderate to high positive genetic correlations between childhood maltreatment subtypes, ranging from 0.31–0.99 (Fig. 2b and Supplementary Table 7). We showed significant pairwise genetic correlations among overall maltreatment, emotional abuse, emotional neglect, physical abuse, and sexual abuse after Bonferroni correction (Bonferroni corrected significance level = 0.05/15 = 0.0033); in contrast, physical neglect only showed significant genetic correlation with overall maltreatment and emotional neglect. Similar patterns of pairwise genetic correlations between childhood maltreatment were found in sex-stratified analysis. In males, the pairwise genetic correlations among overall maltreatment, emotional abuse, emotional neglect, physical abuse, and sexual abuse (except between emotional neglect and sexual abuse) remain significant after Bonferroni correction (Bonferroni corrected significance level = 0.05/15 = 0.0033; Fig. 2c and Supplementary Table 7). Whereas in females, we found significant pairwise correlations among overall maltreatment, emotional abuse, emotional neglect, physical abuse, and sexual abuse as well as between overall maltreatment and physical neglect and between emotional neglect and physical neglect after Bonferroni correction (Bonferroni corrected significance level = 0.05/15 = 0.0033; Fig. 2d and Supplementary Table 7). Moreover, the genetic correlations between males and females were highly positive for each childhood maltreatment subtype except physical neglect (rg ranged from 0.737–0.890 excluding physical neglect; rg for physical neglect = 0.399; Supplementary Figure 27 and Supplementary Table 8).
The impact of childhood maltreatment on high burden diseases in adulthood
Childhood maltreatment were genetically correlated with multiple leading causes of disease burden, including anxiety disorders, heart failure, intracerebral hemorrhage, ischemic heart disease, low back pain, MDD, migraine, neck pain, lung cancer, and T2DM after Bonferroni correction (Bonferroni corrected significance level = 0.05/16 = 0.0031; Fig. 3 and Supplementary Table 9).
There are six panels for six types of childhood maltreatment in which a panel shows a type of childhood maltreatment. The x axis is the genetic correlation between childhood maltreatment and disease, and the y axis represents the disease. Bars in different color were used to distinguish the results for different types of childhood maltreatment. Error bars (black line) are 95% confidence intervals, which are clipped to arrows when they exceed the limit of x-axis. * indicates the P-value < 0.05, and ** indicates the P-value < 0.0031 (Bonferroni corrected significance level = 0.05/16 = 0.0031).
The exploratory analyses of two-sample MR showed evidence that physical abuse increases the risk of MDD after Bonferroni correction (Bonferroni corrected significance level = 0.05/19 = 0.0026; Fig. 4 and Supplementary Table 10) from IVW MR estimators. We also observed some suggestive results that showed nominal significance in both IVW and weighted median MR analyses, including the effect of overall maltreatment on the risk of MDD, the effect of emotional neglect on the risk of MDD and migraine, and the effect of sexual abuse on the risk of age-related and other hearing loss (Fig. 4, Supplementary Figure 28 and Supplementary Table 10). We detected two outliers in the MR effect of overall maltreatment on the risk of MDD and one outlier in the MR effect of emotional neglect on the risk of MDD using MR-PRESSO (Supplementary Table 11). As we corrected for horizontal pleiotropy via outlier removal, the effect estimates remained similar. In sex-stratified MR analysis, we observed sex-specific effects, including the effect of emotional abuse on the risk of MDD in males, the effect of overall maltreatment on the risk of anxiety disorders in females, and the effect of sexual abuse on the risk of stroke in females (Supplementary Table 12).
There are six panels for six types of childhood maltreatment in which a panel shows a type of childhood maltreatment. The x axis is the Mendelian randomization effect size of childhood maltreatment on disease by using the inverse-variance weighted approach, and the y axis represents the diseases. The squares are point estimates for Mendelian randomization effect size (βIVW), and error bars are 95% confidence intervals, which are clipped to arrows when they exceed the limit of x-axis. Different colors were used to distinguish the results for different types of childhood maltreatment. *: indicates the P-value < 0.05. **: indicates the P-value < 0.0026 (Bonferroni corrected significance level = 0.05/19 = 0.0026).
The impact of childhood maltreatment on healthcare costs, lifespan, and educational attainment
Exploratory MR analyses showed that overall maltreatment decreases the lifespan after Bonferroni correction (Bonferroni corrected significance level = 0.05/19 = 0.0026; Table 1) in both IVW and weighted median MR analyses. We also observed a suggestive result that emotional neglect decreases the lifespan with nominal significance in both IVW and weighted median MR analyses. Next, we performed MR-PRESSO global test to detect the horizontal pleiotropy, and we then removed two outliers in the MR effect of overall maltreatment on lifespan to correct the horizontal pleiotropy (Supplementary Table 11). The effect estimate remained similar after correcting for horizontal pleiotropy via outlier removal. We also observed nominally significant effects of childhood maltreatment on healthcare costs in the IVW MR analyses (the effect of overall maltreatment on healthcare costs with the smallest P-value = 0.0138; Table 1); however, we did not obtain consistent results in weighted median MR analysis. In sex-stratified MR analysis, we observed a female-specific effect that physical abuse leads to lower educational attainment in IVW as well as weighted median MR analyses with nominal significance (Supplementary Table 12).
Discussion
We reported sex-combined and sex-stratified GWAS for overall and specific subtypes of childhood maltreatment in European population, and identified one novel locus for childhood sexual abuse (for sex-combined analysis), one novel locus for sexual abuse in males, one novel locus for emotional neglect in females, and one novel locus for sexual abuse in females. The pairwise genetic correlations between childhood maltreatment were high, and similar patterns of genetic correlations between childhood maltreatment were observed in males and females. Childhood maltreatment was genetically correlated with 10 out of 16 high-burden diseases examined here. Moreover, we observed that childhood maltreatment may increase the risk of age-related and other hearing loss, low back pain, MDD, and migraine and decrease the lifespan from exploratory MR analyses.
Compared with previous two GWASs for childhood maltreatment [13, 14], our study adds new results and insights into the genetic architecture of childhood maltreatment (Supplementary Table 13). First, the current study focuses on more detailed phenotyping and is the first to report association findings for sex-specific and subtype-specific of childhood maltreatment [1]. Various forms of childhood maltreatment might have distinct genetic underpinnings. Our GWASs for specific childhood maltreatment subtypes identified one novel locus with leading variant rs1387776 (nearest gene: RP11-644C3.1) for sexual abuse in combined sexes. Moreover, we identified sex-specific genetic loci for childhood maltreatment, including rs12879558 (nearest gene: TMEM260) for sexual abuse in males, rs4326125 (nearest gene: RP11-32D16.1) for emotional neglect in females, and rs1901175 (nearest gene: KCNV1) for sexual abuse in females. TMEM260, RP11-32D16.1, and KCNV1 were reported to be associated with childhood maltreatment for the first time. Importantly, previous within-family analyses provided supporting evidence for the hypothesis that the heritable component of childhood maltreatment may be a consequence of active or reactive gene–environment correlation (without direct underlying biological mechanism for childhood maltreatment) [14]. That is, the genes/loci identified in the current GWAS might be associated with childhood maltreatment through other behavioral traits, such as risk taking or personality eliciting responses from care providers. Second, we performed extensive genetic correlations analyses, unveiling a shared genetic basis between different subtypes of childhood maltreatment and their associations with health outcomes in adulthood. The genetic correlations between childhood maltreatment subtypes are overall significant, (except between physical neglect and emotional abuse, physical abuse and sexual abuse.), displaying similar patterns in sex-combined and sex-stratified analysis. Specifically, we observed high genetic correlations between males and females for overall maltreatment (rg = 0.828), emotional abuse (rg = 0.890), emotional neglect (rg = 0.737), physical abuse (rg = 0.888), and sexual abuse (rg = 0.824). As in the previous study [14], we observed genetic correlations between childhood maltreatment and the risk of MDD, ischemic heart disease, and lung cancer. In addition, childhood maltreatment was genetically correlated with multiple leading causes of disease burden, including anxiety disorders, heart failure, intracerebral hemorrhage, ischemic heart disease, low back pain, MDD, migraine, neck pain, lung cancer, and T2DM after Bonferroni correction. Third, we reported detailed sex-specific SNP-based heritability for different subtypes of childhood maltreatment, showing a slightly higher estimate in females than in males (7.7% vs 5.6% for overall maltreatment; 4.5% vs 3.1% for emotional abuse; 4.7% vs 2.1% for emotional neglect; 4.3% vs 3.8% for physical abuse; 1.9% vs 0.8% for physical neglect; 3.4% vs 2.0% for sexual abuse).
We performed exploratory MR analyses to investigate the causal impact of childhood maltreatment on high burden diseases, healthcare costs, lifespan, and educational attainment. We showed moderate evidence that childhood maltreatment may increase the risk of MDD from IVW MR estimators and decrease the lifespan from both IVW and weighted median MR estimators after Bonferroni correction. We also showed suggestive results with nominal significance in both IVW and weighted median MR analyses, including the effect of childhood maltreatment on the risk of age-related and other hearing loss, low back pain, and migraine, which may result in a higher lifetime cost and create a substantial economic burden [3, 41]. Based on the regional economic value of disability-adjusted life years lost for each risk factor, the projected total annual costs attributable to adverse childhood experiences were US$581 billion in Europe [3]. For victims of nonfatal childhood maltreatment, short-term and long-term healthcare costs per-victim were estimated to be US$35,162 and US$11,341, respectively, and the lifetime costs of childhood maltreatment was estimated to be US$830,928 [41]. A previous study observed significantly higher annual health care use and costs for women with a child abuse history, including physical and sexual abuse, compared to women without a child abuse history [42]. The causal influence of each subtype of childhood maltreatment on healthcare costs was unclear, we therefore investigated the causal relationships between specific childhood maltreatment and healthcare costs by using a MR study design. However, we only observed nominally significant effects of childhood maltreatment on healthcare costs in the IVW MR analysis, while the weighted median MR analysis did not show consistent results.
This study has several limitations. We used retrospective data of childhood maltreatment which might introduce recall bias. A systematic review and meta-analysis study showed poor agreement between prospective and retrospective measures of childhood maltreatment [43]; however, a previous GWAS showed a high genetic correlation between prospectively measured childhood maltreatment and retrospectively reported childhood maltreatment [14]. Warrier et al. proposed that the potential reasons for low overlap between prospective and retrospective data collections were either through non-genetic mechanisms or genetic effects not tagged by the SNPs tested [14]. Second, the 28-item short form of the Childhood Trauma Questionnaire was well-designed [44] and widely used to assess the childhood maltreatment, but in UK Biobank, childhood maltreatments were collected using five frequency scale questions, one question for one subtype of childhood maltreatment, with a 5-point Likert-type scale, which may not be optimal for childhood maltreatment data collection. Next, a sex-stratified analysis in a larger sample would potentially show more findings especially for association analysis. Future studies with larger sample size and power to facilitate sex-stratified analysis are warranted [14]. Furthermore, due to a limited number of genome-wide significant SNPs identified in childhood maltreatment GWAS, we opted for a more lenient threshold of association P-values < 1.0 × 10−5 when selecting genetic instruments [36,37,38], which may lead to insufficient power in our exploratory MR analysis. Additionally, the GWAS for lifespan includes around 68.3% of samples from UKB, which overlap with our childhood maltreatment GWAS, potentially also leading to a weak instrument bias [45]. As such, our results should be interpreted with caution and further investigations are warranted to validate our exploratory MR findings. Moreover, we performed sex-stratified MR analysis to investigate the sex-specific effect of childhood maltreatment on the outcomes. Due to the fact that sex-stratified GWASs for most of the outcomes in this study were not available, we performed exploratory analysis in sex-stratified MR analysis by using sex-specific GWASs for childhood maltreatment and sex-combined GWASs for outcomes based on the assumption of no sex-specific genetic effects on outcomes. Further research is required to evaluate the sex-specific effects of childhood maltreatment on outcomes when the sex-specific GWASs for outcomes become available. Finally, as we only included individuals of European ancestry in the present study, the results may have limited generalizability to other populations.
In conclusion, our study elucidates the genetic architecture of specific childhood maltreatment and specific sex as well as the causal influence of childhood maltreatment on health outcomes in adulthood. Our exploratory MR analyses identified causal effects of childhood maltreatment on adult health outcomes, highlighting the enduring influence of childhood maltreatment on lifelong health consequences. As the heritable component of childhood maltreatment may be a proxy of gene–environment correlation [13, 14], it is important to develop prevention strategies to lower the incidence of childhood maltreatment and provide support and care for victims of childhood maltreatment.
Data availability
We collected publicly available GWAS summary statistics for high burden diseases from each GWAS which were listed in Supplementary Table 2. The full summary statistics of GWAS for specific childhood maltreatment, including both sex-combined and sex-stratified analysis, are available at the NHGRI-EBI GWAS Catalog (https://www.ebi.ac.uk/gwas/downloads) with accession numbers from GCST90551832 to GCST90551849.
Code availability
Previously developed pipelines were used to produce the results of the current study. No custom code was developed. Please see the list of URLs for details on the codes. PLINK v2.0, https://www.cog-genomics.org/plink/2.0/; LocusZoom v0.14.0, https://my.locuszoom.org/; LDSC v1.0.1, https://github.com/bulik/ldsc; TwoSampleMR v0.5.6, https://github.com/MRCIEU/TwoSampleMR.
References
Responding to child maltreatment: a clinical handbook for health professionals. Geneva: World Health Organization; 2022.
Moody G, Cannings-John R, Hood K, Kemp A, Robling M. Establishing the international prevalence of self-reported child maltreatment: a systematic review by maltreatment type and gender. BMC Public Health. 2018;18:1164.
Bellis MA, Hughes K, Ford K, Ramos Rodriguez G, Sethi D, Passmore J. Life course health consequences and associated annual costs of adverse childhood experiences across Europe and North America: a systematic review and meta-analysis. Lancet Public Health. 2019;4:e517–28.
Petruccelli K, Davis J, Berman T. Adverse childhood experiences and associated health outcomes: a systematic review and meta-analysis. Child Abuse Negl. 2019;97:104127.
Nelson CA, Bhutta ScottRD, Harris ZA, Danese NB, Samara A. M. Adversity in childhood is linked to mental and physical health throughout life. Bmj. 2020;371:m3048.
McKay MT, Cannon M, Chambers D, Conroy RM, Coughlan H, Dodd P, et al. Childhood trauma and adult mental disorder: a systematic review and meta-analysis of longitudinal cohort studies. Acta Psychiatr Scand. 2021;143:189–205.
Daníelsdóttir HB, Aspelund T, Shen Q, Halldorsdottir T, Jakobsdóttir J, Song H, et al. Adverse Childhood Experiences and Adult Mental Health Outcomes. JAMA Psychiatry. 2024;81:586–94.
Segal L, Armfield JM, Gnanamanickam ES, Preen DB, Brown DS, Doidge J, et al. Child maltreatment and mortality in young adults. Pediatrics. 2021;147:e2020023416.
D’Arcy-Bewick S, Terracciano A, Turiano N, Sutin AR, Long R, O’Súilleabháin PS. Childhood abuse and neglect, and mortality risk in adulthood: a systematic review and meta-analysis. Child Abuse Negl. 2022;134:105922.
Ryan JP, Jacob BA, Gross M, Perron BE, Moore A, Ferguson S. Early exposure to child maltreatment and academic outcomes. Child Maltreat. 2018;23:365–75.
Houtepen LC, Heron J, Suderman MJ, Fraser A, Chittleborough CR, Howe LD. Associations of adverse childhood experiences with educational attainment and adolescent health and the role of family and socioeconomic factors: A prospective cohort study in the UK. PLoS Med. 2020;17:e1003031.
Sanderson E, Glymour MM, Holmes MV, Kang H, Morrison J, Munafò MR, et al. Mendelian randomization. Nat Rev Methods Primers. 2022;2:6.
Dalvie S, Maihofer AX, Coleman JRI, Bradley B, Breen G, Brick LA, et al. Genomic influences on self-reported childhood maltreatment. Transl Psychiatry. 2020;10:38.
Warrier V, Kwong ASF, Luo M, Dalvie S, Croft J, Sallis HM, et al. Gene-environment correlations and causal effects of childhood maltreatment on physical and mental health: a genetically informed approach. Lancet Psychiatry. 2021;8:373–86.
Sudlow C, Gallacher J, Allen N, Beral V, Burton P, Danesh J, et al. UK biobank: an open access resource for identifying the causes of a wide range of complex diseases of middle and old age. PLoS Med. 2015;12:e1001779.
Bycroft C, Freeman C, Petkova D, Band G, Elliott LT, Sharp K, et al. The UK Biobank resource with deep phenotyping and genomic data. Nature. 2018;562:203–9.
Auton A, Brooks LD, Durbin RM, Garrison EP, Kang HM, Korbel JO, et al. A global reference for human genetic variation. Nature. 2015;526:68–74.
Walter K, Min JL, Huang J, Crooks L, Memari Y, McCarthy S, et al. The UK10K project identifies rare variants in health and disease. Nature. 2015;526:82–90.
McCarthy S, Das S, Kretzschmar W, Delaneau O, Wood AR, Teumer A, et al. A reference panel of 64,976 haplotypes for genotype imputation. Nat Genet. 2016;48:1279–83.
Chang CC, Chow CC, Tellier LC, Vattikuti S, Purcell SM, Lee JJ. Second-generation PLINK: rising to the challenge of larger and richer datasets. Gigascience. 2015;4:7.
Chen CY, Tian R, Ge T, Lam M, Sanchez-Andrade G, Singh T, et al. The impact of rare protein coding genetic variation on adult cognitive function. Nat Genet. 2023;55:927–38.
Peterson RE, Kuchenbaecker K, Walters RK, Chen CY, Popejoy AB, Periyasamy S, et al. Genome-wide association studies in ancestrally diverse populations: opportunities, methods, pitfalls, and recommendations. Cell. 2019;179:589–603.
Walker EA, Gelfand A, Katon WJ, Koss MP, Von Korff M, Bernstein D, et al. Adult health status of women with histories of childhood abuse and neglect. Am J Med. 1999;107:332–9.
Glaesmer H, Schulz A, Häuser W, Freyberger HJ, Brähler E, Grabe HJ. [The childhood trauma screener (CTS) - development and validation of cut-off-scores for classificatory diagnostics]. Psychiatr Prax. 2013;40:220–6.
Watanabe K, Taskesen E, van Bochoven A, Posthuma D. Functional mapping and annotation of genetic associations with FUMA. Nat Commun. 2017;8:1826.
Boughton AP, Welch RP, Flickinger M, VandeHaar P, Taliun D, Abecasis GR, et al. LocusZoom.js: interactive and embeddable visualization of genetic association study results. Bioinformatics. 2021;37:3017–8.
GBD 2019 Diseases and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396:1204–22.
Lee J, Jukarainen S, Karvanen A, Dixon P, Davies NM, Smith GD, et al. Quantifying the causal impact of biological risk factors on healthcare costs. Nature Communications. 2023;14:5672.
Timmers PR, Mounier N, Lall K, Fischer K, Ning Z, Feng X, et al. Genomics of 1 million parent lifespans implicates novel pathways and common diseases and distinguishes survival chances. Elife. 2019;8:e39856.
Okbay A, Beauchamp JP, Fontana MA, Lee JJ, Pers TH, Rietveld CA, et al. Genome-wide association study identifies 74 loci associated with educational attainment. Nature. 2016;533:539–42.
Bulik-Sullivan BK, Loh PR, Finucane HK, Ripke S, Yang J, Patterson N, et al. LD Score regression distinguishes confounding from polygenicity in genome-wide association studies. Nat Genet. 2015;47:291–5.
Bulik-Sullivan B, Finucane HK, Anttila V, Gusev A, Day FR, Loh PR, et al. An atlas of genetic correlations across human diseases and traits. Nat Genet. 2015;47:1236–41.
Smith GD, Ebrahim S. ‘Mendelian randomization’: can genetic epidemiology contribute to understanding environmental determinants of disease? Int J Epidemiol. 2003;32:1–22.
Burgess S, Scott RA, Timpson NJ, Davey Smith G, Thompson SG. Using published data in Mendelian randomization: a blueprint for efficient identification of causal risk factors. Eur J Epidemiol. 2015;30:543–52.
Evans DM, Davey Smith G. Mendelian randomization: new applications in the coming age of hypothesis-free causality. Annu Rev Genomics Hum Genet. 2015;16:327–50.
Gage SH, Jones HJ, Burgess S, Bowden J, Davey Smith G, Zammit S, et al. Assessing causality in associations between cannabis use and schizophrenia risk: a two-sample Mendelian randomization study. Psychol Med. 2017;47:971–80.
Hartwig FP, Borges MC, Horta BL, Bowden J, Davey Smith G. Inflammatory biomarkers and risk of schizophrenia: a 2-sample mendelian randomization study. JAMA Psychiatry. 2017;74:1226–33.
Choi KW, Chen CY, Stein MB, Klimentidis YC, Wang MJ, Koenen KC, et al. Assessment of bidirectional relationships between physical activity and depression among adults: a 2-sample mendelian randomization study. JAMA Psychiatry. 2019;76:399–408.
Verbanck M, Chen CY, Neale B, Do R. Detection of widespread horizontal pleiotropy in causal relationships inferred from Mendelian randomization between complex traits and diseases. Nat Genet. 2018;50:693–8.
Burgess S, Thompson SG. Interpreting findings from Mendelian randomization using the MR-Egger method. Eur J Epidemiol. 2017;32:377–89.
Peterson C, Florence C, Klevens J. The economic burden of child maltreatment in the United States, 2015. Child Abuse Negl. 2018;86:178–83.
Bonomi AE, Anderson ML, Rivara FP, Cannon EA, Fishman PA, Carrell D, et al. Health care utilization and costs associated with childhood abuse. J Gen Intern Med. 2008;23:294–9.
Baldwin JR, Reuben A, Newbury JB, Danese A. Agreement between prospective and retrospective measures of childhood maltreatment: a systematic review and meta-analysis. JAMA Psychiatry. 2019;76:584–93.
Bernstein DP, Fink L Childhood Trauma Questionnaire: A Retrospective Self-report: Manual. Psychological Corporation; 1998.
Burgess S, Davies NM, Thompson SG. Bias due to participant overlap in two-sample Mendelian randomization. Genet Epidemiol. 2016;40:597–608.
Acknowledgements
We thank all the participants and researchers of the UK Biobank. We thank dbGaP (accession phs000179.v5.p2 & phs000765.v2.p2) and FinnGen for providing resources and releasing the genome-wide association summary statistics that made this study possible. We would like to thank the National Core Facility for Biopharmaceuticals (NCFB, 111-2740-B-492-001) and National Center for High-performance Computing (NCHC) of National Applied Research Laboratories (NARLabs) of Taiwan for providing computational and storage resources. This study was supported by the National Health Research Institutes in Taiwan (NP-111, 112, 113-PP-09 to Y.F.L.), the Ministry of Science and Technology in Taiwan (MOST 109-2314-B-400-017 and 110-2314-B-400-028-MY3 to Y.F.L.), National Science and Technology Council in Taiwan (NSCT 112-2314-B-002-200-MY3 to Y.A.F. and 113-2628-B-400-002 to Y.F.L.), the National Taiwan University (NTU-112L7404 to Y.A.F.), the Yushan Young Fellow Program by the Ministry of Education (MOE; NTU-112V1020-2 to Y.A.F.), and the Population Health Research Center from Featured Areas Research Center Program within the framework of the Higher Education Sprout Project by the MOE in Taiwan (NTU-112L9004 to Y.A.F.).
Author information
Authors and Affiliations
Contributions
YAF and YFL take responsibility for the integrity of the data and accuracy of the data analysis. TTC, CYC, and YFL conceived and designed the study. TTC and CYC performed the statistical analyses. TTC and CYC drafted the manuscript. CYC, YAF, and YFL supervised the entire study. JL and AG provide health cost GWAS summary statistics. TTC, CYC, CYL, JL, AG, YAF, and YFL critically revised the paper. All authors contributed to interpretation of the data, writing the manuscript, and have read and approved the final draft for submission.
Corresponding author
Ethics declarations
Ethics
The use of UK Biobank data in the current study has been approved by UK Biobank under application number 54423.
Competing interests
CYC is an employee of Biogen. Biogen has no conflict of interest with the current work. The remaining authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Chen, TT., Chen, CY., Liu, CY. et al. Genetic architectures of childhood maltreatment and causal influence of childhood maltreatment on health outcomes in adulthood. Mol Psychiatry 30, 3404–3412 (2025). https://doi.org/10.1038/s41380-025-02928-y
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41380-025-02928-y