Abstract
Approximately 1 in 10 U.S. newborns are born preterm (<37 weeks of gestation), facing risks of low birth weight, respiratory and birth deficits often requiring surgery, mechanical ventilation, and prolonged sedation. Such long-term exposure to sedatives in these babies can potentially pose neurodevelopmental risks and can further impact changes later in life. The present study focused on midazolam (MDZ), a benzodiazepine class drug commonly used as sedative in the neonatal intensive care unit (NICU). Using a robust preclinical rodent model mimicking chronic MDZ exposure, we did a comprehensive characterization on the phenotypic, molecular, biochemical, and behavioral outcomes in these exposed neonates across key developmental milestones. Our findings indicate that long-term MDZ exposure during the neonatal period negatively affects physical attributes in early childhood. While adult bodyweights between control and MDZ-exposed rats remain comparable, the MDZ rats exhibit accelerated and robust weight gain, potentially indicating a predisposition for binge eating behavior. Additionally, dopamine release in MDZ-exposed rats is markedly reduced in adulthood. Elevated levels of pro-inflammatory cytokines and growth factors in the brain during adulthood suggest a shift in development due to early MDZ exposure. Further, trends of heightened anxiety-like behavior and reduced social interaction during early adolescence compared to other stages were observed. Collectively, our study provides a comprehensive assessment of how long-term MDZ exposure during neonatal stages impacts outcomes throughout life, laying the foundation for understanding mechanisms that contribute to neurodevelopmental complications associated with long-term MDZ use in neonates.
Similar content being viewed by others
Introduction
In the early stages of human development, the brain’s vulnerabilities to neurotoxic chemicals become markedly apparent. Such early exposures can elicit numerous adverse outcomes, hindering the proper development and maturation of the brain. Consequently, individuals may experience functional impairments or even the onset of diseases that persist throughout their lifespan, from infancy to advanced age [1]. Premature babies, born before 37 weeks of gestation, face a range of health implications due to their underdeveloped organ systems and limited time for growth in the womb [2, 3]. These neonates are often associated with an increased risk of health problems such as respiratory issues, infections, temperature regulation, neurodevelopmental disabilities, vision or hearing impairments, and chronic health conditions like asthma or heart problems later in life [2]. In recent years, the intensive use of anesthetics and sedatives in premature babies has raised concerns about potential risks and harmful consequences for brain development. Many studies in the past decade conducted in preclinical models, including non-human primates and rodents, have suggested that exposure to general anesthesia at such an early developmental point will likely harm brain development and lead to cognitive dysfunction [4,5,6,7,8]. Human epidemiological data suggested a relationship between anesthesia exposure in early postnatal life and subsequent lasting neurocognitive alteration [9,10,11,12].
Due to the health complications faced by premature babies, extensive medical interventions such as surgery and mechanical ventilation are often necessary for managing the birth deficits. However, these interventions can induce high levels of stress and discomfort. Hence proper sedation for babies undergoing those uncomfortable procedures while receiving intensive care may alleviate stress and avoid complications. Midazolam (MDZ), a benzodiazepine (BDZ) commonly used for pediatric sedation, exerts its effects by crossing the blood-brain barrier and binding allosterically to the GABAA receptor [13,14,15]. Nevertheless, the prolonged stays of neonates in the ICU often involve repeated or continuous administration of sedatives, raising concerns about the potential effects on neurodevelopment.
A previous study from our group revealed long-term use of MDZ in early childhood altered the synaptic proteome and was associated with changes in molecular functions (e.g., actin-binding, cytochrome c oxidase, pyridoxal phosphate binding) and biological processes (e.g., protein depolymerization, tricarboxylic cycle, central nervous system neuron development) [16]. In this study, we further expanded our scope of investigation to examine if chronic neonatal exposure to MDZ can induce adverse outcomes across key stages of the developmental trajectory: early adolescence, late adolescence, and early adulthood. Our study, for the first time, demonstrated that prolonged MDZ exposure during early development induced a broad spectrum of changes in these measurements across the different stages of the developmental trajectory. The comprehensive and systematic approach used in this study allows for thorough research into the longitudinal effects of chronic early MDZ exposure, a critical step in closing the knowledge gap surrounding this commonly used BDZ as a sedative in neonates.
Materials and methods
Animals
Pregnant dams were purchased from Charles River Laboratories Inc., group-housed in a 12-h light-dark cycle, and fed ad libitum. All procedures and protocols were approved by the Institutional Animal Care and Use Committee of the University of Nebraska Medical Center and conducted in accordance with the National Institutes of Health Guide for the Care and Use of Laboratory Animals.
Midazolam treatment
Our animal/treatment paradigm has been established in our recent works [16, 17]. Rats were randomly assigned to either receive saline or MDZ. Briefly, on postnatal (P) day 3, rat pups are given a single subcutaneous injection of 1 mg/kg midazolam and escalated to 10 mg/kg until P21. For the control group, pups will receive an equivalent amount of saline. Pups are carefully watched for signs of distress, including being placed under a heating lamp to reduce thermal loss. For this study, a subset of pups at various time points were sacrificed to collect the brain for evaluating brain phenotypes and perform subsequent molecular studies. Fresh brain weight and pictures were obtained, and ImageJ software was used to measure brain size. The rest of the pups were raised and assessed for behavioral procedures at P28, 45, and 60. A summary of the schematic is provided in Fig. 1A.
A Schematic experiment timeline showing the dose-escalation regimen of midazolam treatment starting on postnatal (P) day 3 with 1 mg/kg to 10 mg/kg on P21, similar to the previous pilot study [16, 17]. Animals were introduced to behavioral assays on P28, P45, and P60. B The growth curve demonstrates that MDZ-exposed animals (orange) gained weight slower than control saline animals (grey) during the exposure period (P3 to P21). Data represented as Mean ± SD. C, D Body weight recorded on early development (C, P7, P14, P21, n = 117–142/group/timepoint), and later development (D, P28, P45, P60, n = 38–78/group/timepoint) significantly reduced body weight in MDZ-exposed animals at P14 to P21. Two-way ANOVA with Sidak correction for multiple comparisons. There was no significant difference between the control and MDZ-exposed animals at later stages, as determined by Two-Way ANOVA with Sidak correction for multiple comparisons. E Overall weight gained a percentage of the post-treatment period (P28 to P60) with a significant difference as determined by Student t-test with Welch’s correction (**p <0.01, n = 39–41/group). F, G MDZ-exposed animals display significantly lower brain weight (F) but higher brain:body weight ratio at P21 (G). In addition, brain:body weight ratio of MDZ animals also displays a higher ratio than saline at P21 (****p < 0.001, n = 8–30/group/time point). Two-Way ANOVA. All data were represented as mean ± SEM, except (B). Data points for all panels and details on sample size and statistical analyses are provided in Source Data and Statistical Supplemental data files.
Plasma collection and analysis
Animals were deeply anesthetized and blood collected by cardiac puncture was collected into EDTA-coated tubes followed by centrifugation at 3000 x g for 20 min to isolate the plasma. Markers associated with lipid and metabolism function (See Supplemental Fig. 2) were analyzed on a Vitros 250 Chemistry Analyzer device (Ortho-Clinical Diagnostics, Johnson and Johnson, Rochester, NY) at the Biomedical and Obesity Research Core at the University of Nebraska–Lincoln.
Western blot
To evaluate the integrity of the blood-brain barrier and associated proteins, we performed immunoblot on brain tissue lysates (10–20 µg) from rat cortices at P21, P28, P45, and P60 animals with corresponding control at each time point. Primary and secondary antibody dilutions were done according to the manufacturer’s suggestion and are shown in Supplemental Table 1.
RNA extraction and RT-qPCR
Brain cortex and liver RNA was extracted from rats aged P21, P28, P45, and P60 using the Direct-Zol RNA kit (Zymo Research) following the manufacturer’s protocol. Subsequently, cDNA synthesis was conducted with 1 ug of RNA using the Superscript IV kit (Invitrogen) per the manufacturer’s instructions. Real-time quantitative polymerase chain reaction (qPCR) was employed to assess the expression of inflammatory cytokines (Il-1b, Il-6, and Tnf-a), with 18S serving as the housekeeping gene. Additionally, custom TaqMan probe plates were purchased from Applied Biosystems and designed for evaluating growth factors, neurotrophic factors, and other immune genes (Applied Biosystems, Ref#: 4413259). Plate layout and reference genes were included in Supplemental Table 2. Relative fold change was calculated based on the 2^-ddCT method.
Neurochemistry quantification by liquid chromatography/mass spectroscopy (LC/MS)
Briefly, the tissue was homogenized in 100–750 µL of 0.1 M TCA, containing 10−2 M sodium acetate, 10−4 M EDTA, and 10.5% methanol (pH 3.8), and the supernatant was subjected to LC/MS analysis after centrifugation. Benzoyl chloride (BZC) was used to derivatize brain supernatants, while internal standards (5 ng/µL stock solutions) were derivatized using isotopically labeled BZC (13C6-BZC) [18]. Liquid chromatography was conducted on a CORTECS Phenyl column (2.1 × 100 mm, 1.6 µm particles) with a Waters Acquity I-Class UPLC system at the Vanderbilt Neurochemistry Core Lab. Mobile phase A comprised 0.1% aqueous formic acid, and mobile phase B consisted of acetonitrile with 0.1% formic acid. MS analysis utilized a Waters Xevo TQ-XS triple quadrupole tandem mass spectrometer with a source temperature of 150 °C and a desolvation temperature of 400 °C.
Mass spectrometry on P60 synaptosomes and bioinformatics analysis
Purified P60 cortical synaptosomes were isolated and processed following a published protocol [16]. TMT-labeled peptides underwent nano-LC-MS/MS analysis, and MS scans used Proteome Discoverer (Thermo Fisher Sci, v 3.0) against the UniProt database (Rat). Differentially expressed proteins (DEPs) were identified (t-test p-value < 0.05, absolute fold change ≥ 1.2) and visualized with a volcano plot using the ggplot2 package in RStudio (version 4.3.1). Gene Ontology (GO) analyses were performed using Cytoscape plug-in ClueGO on DEPs, with criteria set for Rattus norvegicus and pV ≤ 0.05 [19, 20]. Further, Qiagen’s Ingenuity Pathway Analysis (IPA) software was employed to conduct canonical pathway analysis (QIAGEN Inc., https://www.qiagenbioinformatics.com/products/ingenuity-pathway-analysis). This involved comparing DEPs with known canonical pathways related to signaling and metabolism within IPA.
Measurement of mitochondrial bioenergetics
To measure the bioenergetics of brain cortex synaptosomes, the Seahorse XFe96 Extracellular Flux Analyzer was utilized to measure the oxygen consumption rates (OCR) as previously described [21]. For P21, the brain cortex was isolated after a 30-min of MDZ or saline administration. Synaptosomes (6 technical replicated wells and 7 independent biological replicates for each treatment condition) were isolated by Percoll gradients and ultracentrifugation [22] and plated at 15 µg synaptosomes/well in XF assay medium containing 10 mM pyruvate and 15 mM glucose. Baseline OCR measurements were taken before sequentially injecting mitochondrial ATP synthase inhibitor – oligomycin (Oligo, 3.5 μM); mitochondrial oxidative phosphorylation uncoupler – carbonyl cyanide 4-(trifluoromethoxy)phenylhydrazone (FCCP, 1 μM); complex I and III inhibitor – rotenone (R, 14 μM) and antimycin A (A, 14 μM). For OCR measurements and parameters, including basal respiration, maximal respiration, respiration driving proton leak, respiration driving ATP, and spare respiratory capacity were calculated as described [21]. All data collection was performed by Seahorse Wave Controller Software 2.6.
Behavioral studies
Behavioral testing began when the rats reached 28 days old and included tests for obsessive-compulsive-like and anxiety-like behavior (marble burying), and social interaction (sociability and social novelty preference). Whenever subjected to behavioral testing, each rat was tested repeatedly using the same testing order (1. Marble burying; 2. social interaction tests), with a resting phase of 1 day between individual tests. All the behavior tests were carried out at P28, P45, and P60 and the protocols were adapted from established protocols in our labs [23,24,25]. Testing was recorded and manually scored by blinded scorers. Animals that were jumping out of the procedure during testing were excluded from the study.
Statistical analyses
Data were analyzed using GraphPad Prism (version 9.3.1). Significance was determined using appropriate statistical testing outlined within figure legends for specific comparisons followed by Sidak’s multiple comparisons (or Welch’s correction for student-t-test) where appropriate with a minimum criterion for significance of p < 0.05. All data are presented as mean ± SEM with individual data points unless stated elsewhere. The exact n number for each figure panel is provided in Statistical Supplemental Data.
Results
Chronic MDZ exposure in neonates impairs physical attributes in early childhood
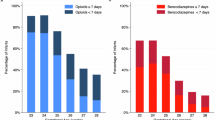
To assess the impact of MDZ exposure on physical development, we measured body and brain weight at multiple development timepoints, including P7, P14, P21, P28, P45, and P60, equivalent to early childhood (P7-P21), early adolescence (P28), adolescent (P45), and young adulthood (P60) in human [26]. MDZ-exposed pups consistently exhibited lower body weight than the control group from P7 to P21 (Fig. 1C). No significant differences were observed in later stages, except for lower body weight in MDZ females at P28 (Fig. 1D and Supplemental Fig. 1A). Importantly, MDZ-exposed animals showed a significantly greater percentage of total weight gain than saline animals (Fig. 1E). Lower brain weight was observed in MDZ animals from P7 to P28, with statistical significance at P21 (Fig. 1F). Examining brain:body weight ratios, P21 MDZ animals had significantly higher ratios than saline animals (Fig. 1G). Further, other brain dimensions, including surface area, width, and length, were consistently lower in MDZ-exposed animals, with statistical significance at P21 and P45 for surface area (Supplemental Fig. 1C–F). These findings indicate that early and chronic MDZ exposure has lasting effects on overall body and brain compositions.
To further assess these physical observations, we measured key plasma metabolites related to glucose and lipid metabolism in P21 and P60 animals. At P21, MDZ-exposed animals exhibited significant increases in direct HDLC, and cholesterol levels compared to controls, which may contribute to the observed reductions in body weight at this developmental stage. However, no significant differences were detected at P60 (Supplemental Fig. 2). These findings highlight a potential link between early metabolic alterations and the physical growth deficits seen in MDZ-treated animals.
Chronic MDZ exposure induces alterations in growth factors, neurotrophic factors, and immune molecule expression
While no observable differences in physical brain characteristics were noted between saline and MDZ groups at other time points, we hypothesized molecular and cellular-level alterations. Consequently, we investigated growth factors, and key signaling molecules regulating cellular processes like proliferation, differentiation, and survival [27, 28]. Compared to their respective saline animals, P21 MDZ animals exhibited a trend towards a reduction in the expression of notable growth factors, Atrn, Bdnf, Cadm1, Fgf2, Igf-1, Ngf, Tgfb-1, and Vegf-a, while in MDZ P60 animals exhibited significantly increased levels of these growth factor expressions (Fig. 2A). For the adolescent timepoints (P28 and P45), no defined trends or significant differences were observed in the expression of growth factors analyzed. Other growth and neurotrophic factors such as Bmp2, Cdh2, Cntf, Fgf1, Fgf9, Fgf17, Gdnf, and Ntf3 also showed no changes (Supplemental Fig. 3).
Cortical brain tissue was assessed for mRNA levels of key growth factors and inflammation biomarkers at P21, P28, P45, and P60 using quantitative real-time PCR analysis. Each gene’s relative fold changes were compared to its respective saline per time point. A MDZ-exposed animal at P60 shows a significant increase of growth factors Artn, Bdnf, Cadm1, Fgf2, Igf-1, Ngf, Tgfb1, Vegf-a as well as B increased of inflammatory markers such as Tnf-a, Cd68, and Cd163. Data are displayed as Mean ± SEM; n = 4–6; *p < 0.05, **p < 0.001, ***p < 0.005. Statistical difference was determined by Two-way ANOVA with Sidak’s correction for each gene. Data points for all panels and details on sample size and statistical analyses are provided in Source Data and Statistical Supplemental data files.
Despite MDZ’s ability to cross the blood-brain barrier (BBB), we investigated its impact on BBB integrity during early developmental exposure. Western blot analysis of BBB components and albumin expression revealed no significant differences between experimental groups (Supplemental Fig. 4), indicating no physical disruption. However, non-disruptive factors influenced BBB functioning, including increased cytokine levels [29]. Pro-inflammatory cytokine expression (Il-1β, Il-6, Tnf-α) showed no significant alterations from P21 to P45 but Tnf-α exhibited a notable increase at P60 compared to earlier time points of MDZ. Additionally, immune molecules and cytokines (Cd68, Cd163, Cxcr1, Cxcr4, Gzmb, Mki67, Mr1) displayed varied expression levels, with Cd68 and Cd163 showing significantly increased levels in the cortex of P60 MDZ-exposed animals. While other genes displayed upregulation, these changes did not reach statistical significance (Fig. 2B), suggesting that chronic MDZ exposure during early development may contribute to mild inflammation in early adulthood. To assess potential systemic inflammation, we analyzed pro-inflammatory cytokine expression in the liver at P21 and P60. No significant changes were observed in MDZ-treated animals (Supplemental Fig. 5), indicating that systemic inflammation is unlikely.
Chronic MDZ exposure alters neurochemistry
The brain cortex undergoes evolutionarily conserved development, and neurotransmitters and regulated metabolites play pivotal roles. However, the influence of chronic MDZ exposure on metabolite expression levels is unknown. LCMS analysis on the prefrontal cortex of P21, 28, 45, and 60 in saline and MDZ groups revealed various neurotransmitters and metabolites. Dopamine metabolites such as DOPAC and HVA, along with GABA levels were reduced at P28 in MDZ-treated rats, suggesting a potential link to anxiety-like behaviors. In addition, dopamine levels were notably depleted at P60 (Fig. 3). Alterations in metabolite levels over time suggest potential metabolic stress with long-term MDZ exposure (Supplemental Fig. 6). Taken together with the higher weight gain, lower dopamine release in the brain, and increased growth factors in early adulthood, these findings, as reported in previous studies [30,31,32], suggest that early MDZ exposure may predispose individuals to binge eating and risk-taking behavior.
LC-MS analysis on released neurotransmitters revealed that early chronic MDZ exposure slightly increased dopamine levels in the PFC in P21 rats. Notably, in the early adolescent (P28) timepoint, dopamine metabolites such as DOPAC and HVA were significantly decreased as well as the GABA levels. For adolescent time points (P45), the release of serotonin (5-HT) was significantly increased. For early adulthood (P60), only dopamine is significantly lower in MDZ animals. Significance is determined using Two-Way ANOVA with Sidak’s multiple comparisons. Data represented as mean ± SEM, n = 4–10, n.d. = no data. *p < 0.05 and **p < 0.01. Data points for all panels and details on sample size and statistical analyses are provided in Source Data and Statistical Supplemental data files.
Chronic MDZ exposure in neonates alters synaptic proteome during early adulthood
In our previous study, we observed protein expression alterations in the cortical synaptosome profile at P21 upon MDZ exposure [16]. Subsequently, we investigated molecular-level changes in early adulthood (P60) through proteomics analysis of cortical synaptosomes. Proteomics analysis uncovered only a few proteins whose expression changed in P60 MDZ rats with criteria fulfilling p-value < 0.05 and absolute fold-change ≥ 1.5 (Fig. 4A). Therefore, alterations in the cortex in response to MDZ exposure may be attributable not to prominent changes in the expression of specific proteins but to the cumulative or cooperative effects of small expression changes in proteins that critically regulate cortical activity. We then identified DEPs with a less stringent fold-change, with an absolute fold-change of ≥ 1.2, comprising 135 and 89 significantly up- and down-regulated proteins, respectively (Fig. 4A). Gene Ontology (GO) analysis highlighted associations with biological processes terms, particularly in transmitter-gated ion channel activity (40.0%), regulation of intracellular pH (26.67%), intracellular protein transmembrane transport (13.33%), cellular response to glucose starvation (6.67%), long-term memory (6.67%), and somitogenesis (6.67%) (Fig. 4B). In terms of molecular functions, the majority were linked to inhibitory extracellular ligand-gated ion channel activity (83.33%) and ribosome binding (16.67%) (Fig. 4C). Pathway analysis using Ingenuity Pathways Analysis (IPA) identified potentially activated pathways, including Rho GTPase cycles, mitochondrial translation, Gα12/13 signaling events, and p75NTR receptor-mediated signaling (Fig. 4D). These findings suggest signaling activity and pathway alterations in MDZ-exposed animals during adulthood, despite the initial exposure during the neonatal period. Details of proteins, ClueGO terms, and IPA results were provided in Supplemental Tables 3–5.
A Volcano plot displaying proteomics data for P60 synaptosomes. These points indicate different proteins that display magnitude fold-changes (log2 of fold-change, x-axis) and statistical significance (-log10 of p-values, y-axis). The grey dashed horizontal line shows the cut-off p values, and the two vertical dashed lines indicate down/upregulated proteins. B, C Mapping of biological processes (B) and molecular functions (C) from differentially expressed proteins (DEPs) using ClueGO. D Ingenuity Pathway Analysis (IPA) revealed predicted pathways associated with P60 MDZ rats. The pathways are ranked by the negative log of the FDR-corrected p-value of the enrichment score and color-coded according to the Z score. A significantly activated pathway activity is indicated by a positive Z score, represented by the orange bars, and an overall deactivated pathway activity is represented by a negative Z score, represented by blue bars. The Gray bar represents enriched pathways with no predicted activity change. The asterisks represent the group term p-value representing each category. *p < 0.05 and **p < 0.01, n = 6/group.
MDZ exposure impacts brain bioenergetics
The brain, demanding roughly 20% of the body’s ATP, relies on glycolysis and mitochondria as complex cellular hubs regulating key signaling pathways for neurodevelopmental processes [33, 34]. Our previous study on synaptic proteome profiles at P21 found abundant DEPs impacted mitochondrial function upon MDZ exposure [16]. To explore the impact of chronic MDZ exposure on mitochondrial function, we employed the Seahorse XF analyzer to assess mitochondrial OCR in P21 animals. Results revealed that in response to MDZ, mitochondria in the P21 synaptosomes have significantly increased maximal respiration, suggesting improved mitochondrial function; however, there is no difference in basal respiration, ATP production, proton leak, and non-mitochondrial respiration (Fig. 5A). To further investigate the long-term effects on mitochondrial function, we also performed Seahorse analysis on P60 cortical synaptosomes and found no difference in mitochondrial function between saline and MDZ synaptosomes (Fig. 5B).
A and C Graphical representation of the oxygen consumption rate (OCR) response over time at P21 (A) and P60 (C). Sequential injections are indicated as Oligo (the ATP synthase inhibitor, oligomycin), F (the ATP synthesis uncoupler, FCCP), and R/A (a mixture of the complex I and III inhibitors composed of rotenone and antimycin A, respectively). B and D Calculated mitochondrial respiratory parameters: basal mitochondria, respiration driving proton leak, respiration driving ATP, spare respiratory capacity (SRC), and non-mitochondria respiration from the P21 (B) and P60 (D) OCR is statistically significant in maximal respiration at P21 as determined by two-way ANOVA with Sidak’s correction (n = 7 per group; **p < 0.01). Data represented as mean ± SEM. Data points for all panels and details on sample size, and statistical analyses are provided in Source Data and Statistical Supplemental data files.
MDZ neonates display disrupted social behavior during adolescence
Early exposure to anesthesiology and sedative agents, associated with learning deficits in both human and preclinical studies, raises concerns about broader neurobehavioral impacts. We comprehensively assessed complex behavioral deficits at multiple developmental stages to address the research gap on the long-term effects of early-life exposure to MDZ.
In sociability testing at P28, the MDZ group exhibited lower sociability, interacting less with naïve and inanimate objects and displaying increased touches per entry in the toy chamber. At P45 and P60, no significant differences were observed (Fig. 6A). On the other hand, MDZ animals displayed no significant difference in time spent, number of entries, and contacts in both naïve and cagemate chambers but there was a significantly higher in number of touches per entry in the cagemate chamber at early adolescent (Fig. 6B). These findings suggest social anxiety-like patterns at P28, with less impact at P45 and P60.
A Sociability test revealed reductions of P28 MDZ animals in the total number of entries and contacts to the Naïve chamber but not at other time points. In addition, P28 MDZ also showed an overall reduction in entering the Toy chamber but did not differ in the number of contacts. Interestingly, P28 MDZ displayed a significantly lower number of touches per entry in the toy chamber (*p < 0.05, n = 37–39/group/timepoint), not the Naïve chamber. B The Social Novelty Preference test displayed no significant difference in time spent, number of entries, and contacts in Naïve and cagemate chambers in each condition and time point. However, P28 MDZ displayed a significant increase in the touches per entry to the cagemate chamber (*p < 0.05, n = 37–39/group/timepoint). C Marble burying assay analysis revealed no significant difference between MDZ and Saline at all time points (n = 32–34/group/timepoint). Repeated measures Two-way ANOVA with Sidak’s correction was used to determine the significant difference as data were represented as mean ± SEM. Data points for all panels and details on sample size, and statistical analyses are provided in Source Data and Statistical Supplemental data files.
To understand anxiety-like behavior, we conducted a marble-burying assessment at P28, P45, and P60. While no statistically significant differences were found, trends indicated that MDZ-exposed animals at P28 and P60 tended to bury more marbles, suggesting slightly higher anxiety levels than at P45 (Fig. 6C).
Discussion
The current study performed a comprehensive examination of molecular and cellular changes in the brain cortex in response to repeated exposure to MDZ, a common sedative used in the NICU. Our findings reveal, for the first time, that chronic early MDZ exposure induces vulnerability in the cortex. This vulnerability is characterized by significant abnormal patterns in growth factors, inflammatory expressions, and metabolic dysregulation, accompanied by longitudinal metabolic dysfunction and behavioral perturbations in the cortical synaptic microenvironment. Our results demonstrate that cumulative early-life exposure to MDZ over an extended period can lead to molecular and behavioral alterations with mild lasting effects.
Anthropometric measurements in infants and children are pivotal in identifying growth abnormalities, malnutrition, obesity, and developmental issues. Assessments of height, length, weight, and head circumference are indispensable for evaluating overall health, nutritional status, and the impact of diseases [35, 36]. Previous studies mentioned no substantial difference in weight gain or loss in rodent models that received 3 to 5 days of MDZ treatment during early age [8, 37]. Lower weight gain during exposure can be due to the repetitive dosage received, which accumulates in the body system and suppresses the nutrition intake. Importantly, we did not observe any difference in body weight until P14, which is nearly 11 days of exposure to MDZ. A previous study reported that BDZ exposure could result in a small loss in body weight from a study on human adults [38]. We also observed that MDZ animals at P21 have a relatively larger brain:body mass ratio, along with smaller body weight at P21, which implies that MDZ might be causing a reduction in overall body weight, which could be due to decreased appetite, altered metabolism, or other systemic effects. Interestingly, our plasma analysis found a high level of HDLC, (Supplemental Fig. 2). High HDL is often associated with lower body weight [39, 40], and the brain is also the organ that contains the highest proportion of lipids in the body [41]. The brain contains the highest proportion of lipids in the body, and during early development, particularly in the first few years, it undergoes significant myelination, the process of forming the myelin sheath, a lipid-rich layer that insulates nerve fibers and facilitates rapid signal transmission between neurons [26, 42, 43]. Repeated MDZ exposure during early neonatal development might impact this crucial phase of brain growth. The lower body weight observed could be a compensatory mechanism, wherein the body allocates more resources to support brain development and myelination at the expense of overall body growth. This prioritization ensures that essential neurological processes are not compromised, even if it means reduced physical growth. Accordingly, we examined if long-term exposure to MDZ in neonates induces alterations at the molecular and cellular levels.
We sought to identify molecular markers contributing to the variable response to early MDZ exposure by examining gene expression changes in growth factors (GFs) and inflammation markers across developmental stages. Neural development involves intricate processes such as neurogenesis, gliogenesis, and synapse formation, with GFs playing a crucial role in influencing cognitive and motor functions [44]. Our study indicated a decrease in GF gene expressions post-MDZ exposure at P21, followed by significant upregulation at early adulthood (P60) (Fig. 2A). While limited information exists on GF behavior post-chronic MDZ exposure during early development, studies suggest MDZ can suppress neural stem cell proliferation in neonatal mice [45]. Additionally, a study on human adults reported a decrease in the growth hormone response during BDZ administration, significantly increased after BDZ treatment discontinuation [46]. Moreover, acute BDZ exposure was found to decrease brain-derived neurotrophic factor (BDNF) expressions in the hippocampus [47]. Although not statistically significant at P21, our findings suggest potential MDZ-induced suppression of normal brain growth, offering insights into negative cognitive outcomes. Importantly, a study on general anesthesia (GA) exposure at P7 rats demonstrated an increase in BDNF levels in the cortex via activating Trk-independent p75NTR -dependent pathways, ultimately stimulating the Akt pathway and activating caspase-3 apoptosis [48]. In our study, we observed a potential activation of p75NTR (Fig. 4D) in P60 animals rather than post-MDZ exposure at P21. The contrasting patterns in GF expression at P60 in young adult rats raise questions about whether this corresponds to when the brains of animals exposed to MDZ began to catch up with regular growth. These observations shed light on the intricate molecular landscape underlying MDZ effects during early development.
We also observed a trend in increasing gene expressions responsible for inflammatory signaling, including Tnf-a, Cd68, and Cd163 in the cortex of MDZ P60 (Fig. 2B). Our IPA also showed that the Rho-GTPase pathway is highly activated (Fig. 4D). The Rho GTPases play a critical role in neuronal morphology, migration, and central nervous system plasticity [49,50,51]. Previous studies have reported that Rho GTPases also function downstream of TNFα, resulting in NFκB activation [52, 53]. The activation of Rho GTPases is predicted, possibly explaining the observed increase in Tnf-a gene expression in our P60 MDZ samples. Notably, growth factors such as NGF, BDNF, and NTF3 are known for their ability to stimulate and promote neurite outgrowth [54,55,56]. Combining the evidence of increased GFs, inflammatory marker expressions, and activation of the Rho-GTPase pathway, it is plausible that a delay in neurodevelopment occurred. This delay is supported by low learning outcomes seen in other preclinical models with repetitive MDZ exposure during early development.
Our neurochemical panel (Fig. 3) revealed interesting observations in neurochemical alterations post-chronic MDZ exposure. Dopamine is the neurotransmitter that regulates motivational behavior, including feeding behaviors [32, 57]. Importantly, previous research has found that MDZ or other BDZ (e.g., diazepam) can disinhibit the dopamine neurons in the ventral tegmental area (VTA) via positive modulation of the GABAARs, which subsequently leads to increased dopamine release [30,31,32]. Although our P21 MDZ brain cortex results do not reveal a statistically significant upregulated dopamine in the prefrontal cortex, interestingly, dopamine depletion is observed in young adult P60 MDZ animals. Moreover, our synaptic proteome analysis in P60 animals also highlighted that DEPs potentially play a role in responding to cellular starvations (Fig. 4B). Considering dopamine’s role in feeding and risk-taking behaviors, it’s plausible that these rats experienced adverse effects, prompting increased food intake to compensate for the sudden dopamine depletion. Notably, serotonin (5-HT) levels detected in P45 rats were significantly elevated. In addition, it is important to note that the MDZ started to gain weight the most between P28 and P45 (Fig. 1B and Supplemental Fig. 1B). These heightened serotonin levels and significant weight gain in P45 MDZ rats may be linked to increased food intake, as elevated serotonin is appetite suppressive [58]. This mechanism could potentially contribute to restoring body and brain homeostasis by signaling a state of satiety. At present, the understanding of the mechanisms that alter neurotransmitters such as dopamine and serotonin after a prolonged period of chronic BDZ use is very limited. Future studies should explore these alterations and associated mechanisms, considering the integration of imaging studies to capture the dynamic fluctuations in neurochemical balance. This approach will facilitate a better comprehension of the long-term impacts following the cessation of chronic BDZ use.
During development, processes like neurogenesis, synaptogenesis, synaptic pruning, and gliogenesis demand substantial energy exchange. Several in vitro and in vivo studies consistently demonstrate that exposure to general anesthetics or sedatives leads to imbalances in mitochondrial energy production in the developing brain [59,60,61,62,63]. Given neurons’ exceptionally high energy demand, comprising 75–80% of brain energy consumption which makes them highly vulnerable to any disruptions in oxygen metabolism and mitochondrial function. Dysregulation of mitochondrial biogenesis, dynamics, and bioenergetics is linked to neurodevelopmental disorders, given neurons’ reliance on oxidative phosphorylation for ATP, crucial for synaptic function [64]. In our investigation into the impact of chronic early developmental exposure to MDZ on brain bioenergetics, we observed a significant increase in maximal respiration in synaptic mitochondria post-MDZ exposure at P21 compared to saline-treated animals. Maximal respiration, indicative of the maximum oxygen consumption rate under mitochondrial uncoupling, suggests heightened energy demand. The observed elevation in maximal respiration in cortical mitochondria under MDZ influence implies increased energy demand during sedation (Fig. 5A). Recent research by van der Kooij MA et al. proposes a hypothesis on BDZ influencing mitochondrial function by binding to GABAA receptors of GABAergic interneurons, disinhibiting dopaminergic neurons, and enhancing dopamine release [32]. Although their focus is on the VTA and nucleus accumbens neurons, our findings align, revealing slightly increased dopamine release in the PFC and maximal respiration in the cortex. This supports the notion that BDZ stimulates dopamine release, elevating metabolic demand across brain regions. While our study doesn’t directly link decreased body weight gain to increased brain energy demand, it prompts consideration for future investigations.
The cortex, a pivotal brain region governing decision-making, social interaction, and emotional regulation, plays a crucial role in various behaviors. While existing studies on the long-term impacts of MDZ exposure have focused on memory and learning [65], aspects such as social interaction remain relatively understudied. Social behavior, essential for social network maintenance in higher mammals, may be at risk due to early exposure to environmental toxicants, including anesthetics [7, 66]. Human studies on GA associate childhood exposure with enduring behavioral and emotional issues, including heightened susceptibility to anxiety, depression, attention deficit disorder, and social interaction challenges [11, 67,68,69]. Previous research by Sprung and colleagues (2012), suggests an increased incidence of attention deficit and hyperactivity disorder diagnoses in children exposed multiple times to GA [69]. Bakri et al. found a higher risk of anxiety, depression, and attention deficit disorder in children exposed to GA before age 5 [70]. Non-human primate studies align with these findings, revealing behaviors indicative of heightened emotional reactivity and fear after multiple exposures to anesthesia during infancy [71]. Rodent studies on GA, such as those conducted by Satomoto et al. on mice exposed to sevoflurane [72], indicate impaired cognitive development and abnormal social behaviors. Conversely, Diana et al. found that P7 rats exposed to GA (consisting of 9 mg/kg MDZ, 70% N2O, and 0.75% isoflurane) for 6 h showed a tendency toward reduced social fear during young adulthood, suggestive of increased risk-taking behavior [7]. Despite variations in observed impairments, neonatal exposure to GA or sedative agents significantly modifies social and emotional development across species. Our study contributes to this body of research, focusing on a specific agent with a unique duration of exposure. Notably, we observed a significant decrease in social interaction in adolescents but not later in adolescence or early adulthood (Fig. 6A, B). At P28, MDZ-exposed rats interacted less with a stranger/naïve animal, as evident in their lower entries and contacts. Additionally, in the presence of their cagemate, P28 MDZ animals tended to touch the chamber containing their cagemate. These findings strongly suggest social anxious-like behavior with chronic MDZ exposure during early development.
Also, our current study, revealed significant changes in dopamine levels, growth factors, heightened inflammation markers, and decreased social interaction—symptoms indicative of schizophrenia [73,74,75,76,77,78,79,80]. Schizophrenia which manifests typically during late adolescence or early adulthood is often marked by cognitive and functional deficits that disrupt social engagement. While the exact etiology of schizophrenia remains elusive, it is widely recognized as a complex neurodevelopmental disorder influenced by both genetic and environmental factors. Interestingly, few studies showed that sub-anesthetic doses of NMDA antagonists in rodents produce a range of behaviors comparable to schizophrenic symptoms, including hyperlocomotion, cognitive deficits, and impaired social behaviors [81, 82]. The association between sedation exposure during childhood and schizophrenia or other psychiatric neuro-disorders and the associated mechanisms remained elusive in the literature. While BDZs are sometimes used to manage schizophrenia in adults [83,84,85], the impact of early-life exposure to anesthetics and sedatives on later schizophrenia risk remains poorly understood. Our current findings whilst still in early stages now offer a possible association that prolonged exposure to anesthetics during early development could potentially contribute to the early onset of schizophrenia. However, more mechanistic research is warranted on these lines for affirmation.
To our knowledge, this study provides an elaborate understanding on how early life chronic exposure to MDZ impacts neurodevelopment across the different stages. Despite certain limitations, our study captures a unique snapshot on outcomes associated with molecular, morphological, synaptic, and behavioral aspects of neural development, shedding new light on the role of MDZ impacting the nervous system at different developmental stages. This study serves as a significant reference for future research exploring the downstream mechanisms and offers further insights into developing an appropriate approach to address neurodevelopmental alterations associated with prolonged MDZ use in neonates.
Data availability
The mass spectrometry proteomics data have been deposited to the ProteomeXchange Consortium via the PRIDE partner repository with the dataset identifier PXD062940. All other relevant data supporting the key findings of this study are available within the article and its supplemental information files (supplemental information is available at MP’s website) or from the corresponding authors upon request.
References
Wallois F, Routier L, Bourel-Ponchel E Chapter 25 - Impact of prematurity on neurodevelopment. In: Gallagher A, Bulteau C, Cohen D, Michaud JL, editors. Handbook of Clinical Neurology. Elsevier; 2020. p. 341-75.
Ward RM, Beachy JC. Neonatal complications following preterm birth. BJOG: An Int J Obstet Gynaecol. 2003;110:8–16.
Morniroli D, Tiraferri V, Maiocco G, De Rose DU, Cresi F, Coscia A, et al. Beyond survival: the lasting effects of premature birth. Front Pediatr. 2023;11:1213243. https://doi.org/10.3389/fped.2023.1213243.
Jevtovic-Todorovic V, Hartman RE, Izumi Y, Benshoff ND, Dikranian K, Zorumski CF, et al. Early exposure to common anesthetic agents causes widespread neurodegeneration in the developing rat brain and persistent learning deficits. J Neurosci. 2003;23:876–82. https://doi.org/10.1523/JNEUROSCI.23-03-00876.2003.
Maloney SE, Creeley CE, Hartman RE, Yuede CM, Zorumski CF, Jevtovic-Todorovic V, et al. Using animal models to evaluate the functional consequences of anesthesia during early neurodevelopment. Neurobiol Learn Mem. 2019;165:106834 https://doi.org/10.1016/j.nlm.2018.03.014.
Young C, Jevtovic-Todorovic V, Qin YQ, Tenkova T, Wang H, Labruyere J, et al. Potential of ketamine and midazolam, individually or in combination, to induce apoptotic neurodegeneration in the infant mouse brain. Br J Pharmacol. 2005;146:189–97. https://doi.org/10.1038/sj.bjp.0706301.
Diana P, Joksimovic SM, Faisant A, Jevtovic-Todorovic V. Early exposure to general anesthesia impairs social and emotional development in rats. Mol Neurobiol. 2020;57:41–50. https://doi.org/10.1007/s12035-019-01755-x.
Xu J, Mathena RP, Singh S, Kim J, Long JJ, Li Q, et al. Early developmental exposure to repetitive long duration of midazolam sedation causes behavioral and synaptic alterations in a rodent model of neurodevelopment. J Neurosurg Anesthesiol. 2019;31:151–62. https://doi.org/10.1097/ana.0000000000000541.
Puia-Dumitrescu M, Comstock BA, Li S, Heagerty PJ, Perez KM, Law JB, et al. Assessment of 2-Year neurodevelopmental outcomes in extremely preterm infants receiving opioids and benzodiazepines. JAMA Netw Open. 2021;4:e2115998 https://doi.org/10.1001/jamanetworkopen.2021.15998.
Duerden EG, Guo T, Dodbiba L, Chakravarty MM, Chau V, Poskitt KJ, et al. Midazolam dose correlates with abnormal hippocampal growth and neurodevelopmental outcome in preterm infants. Ann Neurol. 2016;79:548–59. https://doi.org/10.1002/ana.24601.
Wilder RT, Flick RP, Sprung J, Katusic SK, Barbaresi WJ, Mickelson C, et al. Early exposure to anesthesia and learning disabilities in a population-based birth cohort. Anesthesiology. 2009;110:796–804. https://doi.org/10.1097/01.anes.0000344728.34332.5d.
Colon E, Bittner EA, Kussman B, McCann ME, Soriano S, Borsook D. Anesthesia, brain changes, and behavior: Insights from neural systems biology. Prog Neurobiol. 2017;153:121–60. https://doi.org/10.1016/j.pneurobio.2017.01.005.
Pacifici GM. Clinical pharmacology of midazolam in neonates and children: effect of disease—a review. Int J Pediatrics. 2014;2014:309342 https://doi.org/10.1155/2014/309342.
Ng E, Taddio A, Ohlsson A. Intravenous midazolam infusion for sedation of infants in the neonatal intensive care unit. Cochrane Database Syst Rev. 2017;1:CD002052-CD https://doi.org/10.1002/14651858.CD002052.pub3.
Stark A, Smith PB, Hornik CP, Zimmerman KO, Hornik CD, Pradeep S, et al. Medication use in the neonatal intensive care unit and changes from 2010 to 2018. J Pediatrics. 2022;240:66–71.e4. https://doi.org/10.1016/j.jpeds.2021.08.075.
Nguyen NM, Vellichirammal NN, Guda C, Pendyala G. Decoding the synaptic proteome with long-term exposure to midazolam during early development. Int J Mol Sci. 2022;23:4137 https://doi.org/10.3390/ijms23084137.
Nguyen NM, Meyer D, Meyer L, Chand S, Jagadesan S, Miravite M, et al. Identification of YWHAH as a novel brain-derived extracellular vesicle marker post long-term midazolam exposure during early development. Cells. 2023;12:966 https://doi.org/10.3390/cells12060966.
Wong J-MT, Malec PA, Mabrouk OS, Ro J, Dus M, Kennedy RT. Benzoyl chloride derivatization with liquid chromatography–mass spectrometry for targeted metabolomics of neurochemicals in biological samples. J Chromatogr A. 2016;1446:78–90. https://doi.org/10.1016/j.chroma.2016.04.006.
Shannon P, Markiel A, Ozier O, Baliga NS, Wang JT, Ramage D, et al. Cytoscape: a software environment for integrated models of biomolecular interaction networks. Genome Res. 2003;13:2498–504. https://doi.org/10.1101/gr.1239303.
Bindea G, Mlecnik B, Hackl H, Charoentong P, Tosolini M, Kirilovsky A, et al. ClueGO: a Cytoscape plug-in to decipher functionally grouped gene ontology and pathway annotation networks. Bioinformatics. 2009;25:1091–3. https://doi.org/10.1093/bioinformatics/btp101.
Lamberty BG, Estrella LD, Mattingly JE, Emanuel K, Trease A, Totusek S, et al. Parkinson’s disease relevant pathological features are manifested in male Pink1/Parkin deficient rats. Brain, Behavior, Immun - Health. 2023;31:100656 https://doi.org/10.1016/j.bbih.2023.100656.
Stauch KL, Purnell PR, Fox HS. Aging synaptic mitochondria exhibit dynamic proteomic changes while maintaining bioenergetic function. Aging (Albany NY). 2014;6:320–34. https://doi.org/10.18632/aging.100657.
Odegaard KE, Schaal VL, Clark AR, Koul S, Gowen A, Sankarasubramani J, et al. Characterization of the intergenerational impact of in utero and postnatal oxycodone exposure. Transl Psychiatry. 2020;10:329 https://doi.org/10.1038/s41398-020-01012-z.
Gowen AM, Yi J, Stauch K, Miles L, Srinivasan S, Odegaard K, et al. In utero and post-natal opioid exposure followed by mild traumatic brain injury contributes to cortical neuroinflammation, mitochondrial dysfunction, and behavioral deficits in juvenile rats. Brain, Behavior, Immun - Health. 2023;32:100669 https://doi.org/10.1016/j.bbih.2023.100669.
Flores A, Nguyen NM, Devanaboyina M, Sanketh S, Athota P, Jagadesan S, et al. Neurobehavioral characterization of perinatal oxycodone-exposed offspring in early adolescence. J Neuroimmune Pharmacol. 2024;19:29 https://doi.org/10.1007/s11481-024-10129-7.
Semple BD, Blomgren K, Gimlin K, Ferriero DM, Noble-Haeusslein LJ. Brain development in rodents and humans: identifying benchmarks of maturation and vulnerability to injury across species. Prog Neurobiol. 2013;106-107:1–16. https://doi.org/10.1016/j.pneurobio.2013.04.001.
Crutcher KA. The role of growth factors in neuronal development and plasticity. CRC Crit Rev Clin Neurobiol. 1986;2:297–333.
Landreth G, Siegel G, Agranoff B, Albers R, Perry B Classes of growth factors acting in the nervous system. Basic Neurochemistry: Molecular, Cellular and Medical Aspects, GJ Siegel, BW Agranoff, RW Albers, SK Fisher, and MD Uhler, Eds. 1999:473-83.
Varatharaj A, Galea I. The blood-brain barrier in systemic inflammation. Brain, Behavior, Immun. 2017;60:1–12. https://doi.org/10.1016/j.bbi.2016.03.010.
Xi ZX, Stein EA. Nucleus accumbens dopamine release modulation by mesolimbic GABAA receptors-an in vivo electrochemical study. Brain Res. 1998;798:156–65. https://doi.org/10.1016/s0006-8993(98)00406-5.
Riegel AC, Kalivas PW. Neuroscience: Lack of inhibition leads to abuse. Nature. 2010;463:743–4. https://doi.org/10.1038/463743a
van der Kooij MA, Hollis F, Lozano L, Zalachoras I, Abad S, Zanoletti O, et al. Diazepam actions in the VTA enhance social dominance and mitochondrial function in the nucleus accumbens by activation of dopamine D1 receptors. Mol Psychiatry. 2018;23:569–78. https://doi.org/10.1038/mp.2017.135.
Rossi A, Pizzo P. Mitochondrial bioenergetics and neurodegeneration: a: paso doble. Neural Regen Res. 2021;16:686–7. https://doi.org/10.4103/1673-5374.295331.
Strope TA, Birky CJ, Wilkins HM. The role of bioenergetics in neurodegeneration. Int J Mol Sci. 2022;23:9212 https://doi.org/10.3390/ijms23169212.
Andrews ET, Beattie RM, Johnson MJ. Measuring body composition in the preterm infant: Evidence base and practicalities. Clin Nutr. 2019;38:2521–30. https://doi.org/10.1016/j.clnu.2018.12.033.
Casadei K, Kiel J. Anthropometric Measurement. StatPearls. Treasure Island (FL): StatPearls Publishing; 2023.
Iqbal O’Meara AM, Miller Ferguson N, Zven SE, Karam OL, Meyer LC, Bigbee JW, et al. Potential neurodevelopmental effects of pediatric intensive care sedation and analgesia: repetitive benzodiazepine and opioid exposure alters expression of glial and synaptic proteins in juvenile rats. Crit Care Explor. 2020;2:e0105 https://doi.org/10.1097/cce.0000000000000105.
Oswald I, Adam K. Benzodiazepines cause small loss of body weight. Br Med J. 1980;281:1039–40. https://doi.org/10.1136/bmj.281.6247.1039-a.
Dansinger M, Williams PT, Superko HR, Asztalos BF, Schaefer EJ. Effects of weight change on HDL-cholesterol and its subfractions in over 28,000 men and women. J Clin Lipidol. 2019;13:308–16. https://doi.org/10.1016/j.jacl.2018.12.001.
Park KH, Yadav D, Kim SJ, Kim JR, Cho KH. Slim body weight is highly associated with enhanced lipoprotein functionality, higher HDL-C, and large HDL particle size in young women. Front Endocrinol. 2018;9:406 https://doi.org/10.3389/fendo.2018.00406.
Katz R, Hamilton JA, Pownall HJ, Deckelbaum RJ, Hillard CJ, Leboeuf RC, et al. Brain uptake and utilization of fatty acids, lipids & lipoproteins: recommendations for future research. J Mol Neurosci. 2007;33:146–50. https://doi.org/10.1007/s12031-007-0059-7.
Herschkowitz N, Kagan J, Zilles K. Neurobiological bases of behavioral development in the first year. Neuropediatrics. 1997;28:296–306. https://doi.org/10.1055/s-2007-973720.
Huttenlocher PR. Synaptic density in human frontal cortex - developmental changes and effects of aging. Brain Res. 1979;163:195–205. https://doi.org/10.1016/0006-8993(79)90349-4.
Galvez-Contreras AY, Campos-Ordonez T, Lopez-Virgen V, Gomez-Plascencia J, Ramos-Zuniga R, Gonzalez-Perez O. Growth factors as clinical biomarkers of prognosis and diagnosis in psychiatric disorders. Cytokine Growth Factor Rev. 2016;32:85–96. https://doi.org/10.1016/j.cytogfr.2016.08.004.
Doi H, Matsuda T, Sakai A, Matsubara S, Hoka S, Yamaura K, et al. Early-life midazolam exposure persistently changes chromatin accessibility to impair adult hippocampal neurogenesis and cognition. Proc Natl Acad Sci USA. 2021;118:e2107596118 https://doi.org/10.1073/pnas.2107596118.
Shur E, Petursson H, Checkley S, Lader M. Long-term benzodiazepine administration blunts growth hormone response to diazepam. Arch Gen Psychiatry. 1983;40:1105–8. https://doi.org/10.1001/archpsyc.1983.01790090067010.
Licata SC, Shinday NM, Huizenga MN, Darnell SB, Sangrey GR, Rudolph U, et al. Alterations in brain-derived neurotrophic factor in the mouse hippocampus following acute but not repeated benzodiazepine treatment. PLoS One. 2013;8:e84806 https://doi.org/10.1371/journal.pone.0084806.
Lu LX, Yon J-H, Carter LB, Jevtovic-Todorovic V. General anesthesia activates BDNF-dependent neuroapoptosis in the developing rat brain. Apoptosis. 2006;11:1603–15. https://doi.org/10.1007/s10495-006-8762-3.
Kozma R, Sarner S, Ahmed S, Lim L. Rho family GTPases and neuronal growth cone remodelling: relationship between increased complexity induced by Cdc42Hs, Rac1, and acetylcholine and collapse induced by RhoA and lysophosphatidic acid. Mol Cell Biol. 1997;17:1201–11. https://doi.org/10.1128/mcb.17.3.1201.
Sugihara K, Nakatsuji N, Nakamura K, Nakao K, Hashimoto R, Otani H, et al. Rac1 is required for the formation of three germ layers during gastrulation. Oncogene. 1998;17:3427–33. https://doi.org/10.1038/sj.onc.1202595.
Govek EE, Hatten ME, Van Aelst L. The role of Rho GTPase proteins in CNS neuronal migration. Dev Neurobiol. 2011;71:528–53. https://doi.org/10.1002/dneu.20850.
Perona R, Montaner S, Saniger L, Sánchez-Pérez I, Bravo R, Lacal JC. Activation of the nuclear factor-kappaB by Rho, CDC42, and Rac-1 proteins. Genes Dev. 1997;11:463–75. https://doi.org/10.1101/gad.11.4.463.
Tong L, Tergaonkar V. Rho protein GTPases and their interactions with NFκB: crossroads of inflammation and matrix biology. Biosci Rep. 2014;34:e00115 https://doi.org/10.1042/bsr20140021.
Ito K, Enomoto H. Retrograde transport of neurotrophic factor signaling: implications in neuronal development and pathogenesis. J Biochem. 2016;160:77–85. https://doi.org/10.1093/jb/mvw037.
Bahlakeh G, Rahbarghazi R, Mohammadnejad D, Abedelahi A, Karimipour M. Current knowledge and challenges associated with targeted delivery of neurotrophic factors into the central nervous system: focus on available approaches. Cell Biosci. 2021;11:181 https://doi.org/10.1186/s13578-021-00694-2.
Miranda M, Morici JF, Zanoni MB, Bekinschtein P. Brain-Derived neurotrophic factor: a key molecule for memory in the healthy and the pathological brain. Front Cell Neurosci. 2019;13:363 https://doi.org/10.3389/fncel.2019.00363.
Baik JH. Dopaminergic control of the feeding circuit. Endocrinol Metab. 2021;36:229–39. https://doi.org/10.3803/EnM.2021.979.
Voigt JP, Fink H. Serotonin controlling feeding and satiety. Behav Brain Res. 2015;277:14–31. https://doi.org/10.1016/j.bbr.2014.08.065.
Sanchez V, Feinstein SD, Lunardi N, Joksovic PM, Boscolo A, Todorovic SM, et al. General anesthesia causes long-term impairment of mitochondrial morphogenesis and synaptic transmission in developing rat brain. Anesthesiology. 2011;115:992–1002. https://doi.org/10.1097/ALN.0b013e3182303a63.
Wu J, Yang JJ, Cao Y, Li H, Zhao H, Yang S, et al. Iron overload contributes to general anaesthesia-induced neurotoxicity and cognitive deficits. J Neuroinflammation. 2020;17:110 https://doi.org/10.1186/s12974-020-01777-6.
Xu F, Armstrong R, Urrego D, Qazzaz M, Pehar M, Armstrong JN, et al. The mitochondrial division inhibitor Mdivi-1 rescues mammalian neurons from anesthetic-induced cytotoxicity. Mol Brain. 2016;9:35 https://doi.org/10.1186/s13041-016-0210-x.
Bai X, Yan Y, Canfield S, Muravyeva MY, Kikuchi C, Zaja I, et al. Ketamine enhances human neural stem cell proliferation and induces neuronal apoptosis via reactive oxygen species-mediated mitochondrial pathway. Anesth Analg. 2013;116:869–80. https://doi.org/10.1213/ANE.0b013e3182860fc9.
Hogarth K, Tarazi D, Maynes JT. The effects of general anesthetics on mitochondrial structure and function in the developing brain. Front Neurol. 2023;14:1179823 https://doi.org/10.3389/fneur.2023.1179823.
Hyder F, Rothman DL, Bennett MR. Cortical energy demands of signaling and nonsignaling components in brain are conserved across mammalian species and activity levels. Proc Natl Acad Sci USA. 2013;110:3549–54. https://doi.org/10.1073/pnas.1214912110.
Nguyen NM, Pendyala G Sedation with midazolam in the NICU: implications on neurodevelopment. NeuroImmune Pharmacology Therapeutics. 2024. https://doi.org/10.1515/nipt-2024-0009.
Jin X, Ji L, Chen Q, Sheng R, Ji F, Yang J. Anesthesia plus surgery in neonatal period impairs preference for social novelty in mice at the juvenile age. Biochemical Biophys Res Commun. 2020;530:603–8. https://doi.org/10.1016/j.bbrc.2020.07.108.
DiMaggio C, Sun LS, Kakavouli A, Byrne MW, Li G. A retrospective cohort study of the association of anesthesia and hernia repair surgery with behavioral and developmental disorders in young children. J Neurosurg Anesthesiol. 2009;21:286–91. https://doi.org/10.1097/ANA.0b013e3181a71f11.
Chemaly M, El-Rajab MA, Ziade FM, Naja ZM. Effect of one anesthetic exposure on long-term behavioral changes in children. J Clin Anesth. 2014;26:551–6. https://doi.org/10.1016/j.jclinane.2014.03.013.
Sprung J, Flick RP, Katusic SK, Colligan RC, Barbaresi WJ, Bojanić K, et al. Attention-deficit/hyperactivity disorder after early exposure to procedures requiring general anesthesia. Mayo Clin Proc. 2012;87:120–9. https://doi.org/10.1016/j.mayocp.2011.11.008.
Bakri MH, Ismail EA, Ali MS, Elsedfy GO, Sayed TA, Ibrahim A. Behavioral and emotional effects of repeated general anesthesia in young children. Saudi J Anaesth. 2015;9:161–6. https://doi.org/10.4103/1658-354x.152843.
Raper J, Alvarado MC, Murphy KL, Baxter MG. Multiple anesthetic exposure in infant monkeys alters emotional reactivity to an acute stressor. Anesthesiology. 2015;123:1084–92. https://doi.org/10.1097/aln.0000000000000851.
Satomoto M, Satoh Y, Terui K, Miyao H, Takishima K, Ito M, et al. Neonatal exposure to sevoflurane induces abnormal social behaviors and deficits in fear conditioning in mice. Anesthesiology. 2009;110:628–37. https://doi.org/10.1097/ALN.0b013e3181974fa2.
Durany N, Michel T, Zöchling R, Boissl KW, Cruz-Sánchez FF, Riederer P, et al. Brain-derived neurotrophic factor and neurotrophin 3 in schizophrenic psychoses. Schizophrenia Res. 2001;52:79–86. https://doi.org/10.1016/S0920-9964(00)00084-0.
Takahashi M, Shirakawa O, Toyooka K, Kitamura N, Hashimoto T, Maeda K, et al. Abnormal expression of brain-derived neurotrophic factor and its receptor in the corticolimbic system of schizophrenic patients. Mol Psychiatry. 2000;5:293–300. https://doi.org/10.1038/sj.mp.4000718.
Zhu Y, Webster MJ, Walker AK, Massa P, Middleton FA, Weickert CS. Increased prefrontal cortical cells positive for macrophage/microglial marker CD163 along blood vessels characterizes a neuropathology of neuroinflammatory schizophrenia. Brain, Behavior, Immun. 2023;111:46–60. https://doi.org/10.1016/j.bbi.2023.03.018.
Turkmen BA, Yazici E, Erdogan DG, Suda MA, Yazici AB. BDNF, GDNF, NGF and Klotho levels and neurocognitive functions in acute term of schizophrenia. BMC Psychiatry. 2021;21:562 https://doi.org/10.1186/s12888-021-03578-4.
Weickert CS, Lee CH, Lenroot RK, Bruggemann J, Galletly C, Liu D, et al. Increased plasma Brain-Derived Neurotrophic Factor (BDNF) levels in females with schizophrenia. Schizophrenia Res. 2019;209:212–7. https://doi.org/10.1016/j.schres.2019.04.015.
Gören JL. Brain-derived neurotrophic factor and schizophrenia. Ment Health Clin. 2016;6:285–8. https://doi.org/10.9740/mhc.2016.11.285.
Brisch R, Saniotis A, Wolf R, Bielau H, Bernstein HG, Steiner J, et al. The role of dopamine in schizophrenia from a neurobiological and evolutionary perspective: old fashioned, but still in vogue. Front Psychiatry. 2014;5:47 https://doi.org/10.3389/fpsyt.2014.00047.
Powell SB, Swerdlow NR. The relevance of animal models of social isolation and social motivation for understanding schizophrenia: review and future directions. Schizophrenia Bull. 2023;49:1112–26. https://doi.org/10.1093/schbul/sbad098.
Rogers R, Wise RG, Painter DJ, Longe SE, Tracey I. An investigation to dissociate the analgesic and anesthetic properties of ketamine using functional magnetic resonance imaging. J Am Soc Anesthesiologists. 2004;100:292–301.
Verma A, Moghaddam B. NMDA receptor antagonists impair prefrontal cortex function as assessed via spatial delayed alternation performance in rats: modulation by dopamine. J Neurosci. 1996;16:373–9.
Baandrup L. Polypharmacy in schizophrenia. Basic Clin Pharmacol Toxicol. 2020;126:183–92. https://doi.org/10.1111/bcpt.13384.
Ballon J, Stroup TS. Polypharmacy for schizophrenia. Curr Opin Psychiatry. 2013;26:208–13. https://doi.org/10.1097/YCO.0b013e32835d9efb.
Miron AA, Petric PS, Teodorescu A, Ifteni P, Chele G, Szalontay AS. Benzodiazepines and mood stabilizers in schizophrenia patients treated with oral versus long-acting injectable antipsychotics—an observational study. Brain Sci. 2023;13:173.
Acknowledgements
This work was supported by Lieberman Endowment (G.P); start-up funds provided by Department of Anesthesiology, UNMC (S.V.Y and G.P) and pilot grant from the Child Health Research Institute, UNMC (G.P. and K.S.). We sincerely acknowledge Vanderbilt University Neurochemistry Core for their invaluable assistance in liquid chromatography/mass spectrometry analysis of neurochemistry. The views presented are solely those of the author(s) and do not represent the perspectives of Vanderbilt University. We also thank the Mass Spectrometry and Proteomics Core Facility at UNMC and the Biomedical and Obesity Research Core at the University of Nebraska–Lincoln for their help in performing the proteomics and plasma metabolites analysis.
Author information
Authors and Affiliations
Contributions
N.M.N.: conceptualization, formal analysis, investigation, visualization, project administration, and writing – original draft. P.A., A.F., C.K., and A.T.: investigation and analysis. D.M., V.K.S, V.L.S, R.B: investigation. K.Sualy, K.Stauch, S.K.N, and S.V.Y.: resources and funding acquisition; G.P.: conceptualization, supervision, resources, project administration, funding acquisition.
Corresponding author
Ethics declarations
Competing interests
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Ethics declarations
Institutional Review Board Statement. All animal procedures were approved by the Institutional Animal Care and Use Committee of University of Nebraska Medical Center (Animal Use Protocol 19-130-01-EP) and conducted in accordance with the NIH Guide for the Care and Use of Laboratory Animals.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Source data
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Nguyen, N.M., Athota, P., Flores, A. et al. Comprehensive characterization of chronic midazolam exposure on neonates and long-term neurodevelopment. Mol Psychiatry 30, 5203–5214 (2025). https://doi.org/10.1038/s41380-025-03104-y
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41380-025-03104-y