Abstract
Study design
Nationwide epidemiological open cohort study.
Objectives
To evaluate whether individuals with traumatic spinal cord injury (TSCI) are more prone to develop autoimmune diseases compared to a general non-TSCI population.
Setting
Danish public national registries.
Methods
An open nationwide cohort, including individuals born in Denmark from or alive during 1945-2018 was collected and the study period was 1980-2018. Poissons Log-linear regression estimated the incidence rate ratio (IRR) for developing eight groups of autoimmune diseases. A dose-response relationship based on the cervical/thoracic level of injury was assessed by stratification.
Results
The cohort included 3,272 individuals with TSCI and 4.8 million background individuals, accounting for 50,865 and 140 million person-years respectively. The TSCI population had an overall IRR of 1.81 (95% CI, 1.59 to 2.05) of getting any autoimmune disease. Subgroup analysis found positive associations for; a) Other neurologic IRR 5.19 (95% CI, 2.79 to 9.65), b) multiple sclerosis IRR 3.70 (95% CI, 2.54 to 5.40), c) Dermatologic IRR 2.57 (95% CI, 1.86 to 3.55), d) Type 1 diabetes mellitus IRR 2.01 (95% CI, 1.54 to 2.61), e) Systemic 1.92 (95% CI, 1.44 to 2.55), and f) Gastroenterologic IRR 1.42 (95% CI, 1.05 to 1.92). Cervical levels of TSCI showed an IRR of 1.70 (95% CI, 1.43 to 2.02), while thoracic levels had an IRR 1.98 (95% CI, 1.63 to 2.39).
Conclusions
TSCI may be an individual risk factor of developing an autoimmune disease. There does not appear to exist a dose-response relationship from the level of injury.
Sponsorship
None.
Similar content being viewed by others
Introduction
The worldwide incidence of traumatic spinal cord injury (TSCI) ranges from 5.1 – 150.48 per million person-years [1]. The neurologic injury affects motor-, and sensory functions, bladder, bowel, and sexual function, and TSCI could be seen as a multiorgan disease [2]. Experimental-, clinical-, and observational studies suggest a deteriorating immunological response following TSCI, which may lead to secondary neurologic injury, multiorgan disease and autoimmune disease ultimately increasing morbidity and mortality [2,3,4].
Trauma induces the primary neurological injury. Concomitant cellular damage and the presumably compromised blood spinal cord barrier trigger a deteriorating inflammatory cascade [4, 5]. Myeloid cells’ phagocytosis of myelin turns them into foamy cells resulting in apoptosis/necrosis further fueling the inflammatory process [5]. Eventually, autoreactive T- and B-cells are activated, myelin-specific autoantibodies can be measured, and chronic inflammation is established [4, 6,7,8].
The high inflammatory activity initiates spinal cord injury immunodeficiency syndrome (SCI-IDS), a state of systemic immunosuppression, causing secondary neurologic injury with prolonged self-epitope exposure between antigen-presenting and endemic autoreactive lymphoid cells [4, 9]. The ongoing inflammation and secondary neurologic injury prolong exposure to central nervous system self-epitopes increasing susceptibility to match antigen-presenting cells with autoreactive lymphoid cells; a door that enables autoimmune development [4, 7, 9, 10].
The immunosuppressive state of SCI-IDS may have a protective effect against autoimmune development [11]. However, the same effect also increases susceptibility to infection, which leads to higher rates and severity of hospitalizations for infectious diseases. Post-TSCI infectious diseases are known to affect neurological recovery negatively. Hospitalization for an infectious diseases is a known risk factor of developing any autoimmune disease [9, 11, 12].
Evidence suggest that more cranial injuries amplify both SCI-IDS and autonomic dysreflexia [3, 11, 13]. Autonomic dysreflexia is immunosuppressive due to the high-level releases of norepinephrine and glucocorticoids during attacks [3]. The balance of beneficial and detrimental effects of SCI-IDS and autonomic dysreflexia is likely level-dependent, and the risk of post-TSCI autoimmunity may also be level-dependent [9].
Trauma presumably tears the blood-spinal cord barrier and discontinues the immune-privilege of the central nervous system [14]. This allows unregulated access of the systemic immune system and unphysiological drainage of central nervous system debris to secondary lymphoid tissue [10]. Research into central nervous system drainage pathways and the immune privilege is ongoing, but susceptibility to autoimmunity could be feasible due to the physiological/immunological changes from TSCI, combined with the fact that central nervous system cells have a lower expression of major histocompatibility complex-I and -II receptors [15]. Under normal physiological circumstances, immune cells are presented with fewer central nervous system autoantigens, possibly lowering tolerance to self compared to systemic antigens [5,6,7, 15]. This, along with prolonged self-epitope exposure, could explain why TSCI might lead to posttraumatic immunological dysfunction, resulting in autoimmunity/-inflammation, multiorgan, and autoimmune diseases, and higher posttraumatic morbidity and mortality [5, 7, 8, 13, 16].
The aetiology to autoimmune disease is heavily multifactorial. Some general risk factors have been identified for autoimmune disease including genetics, prior autoimmune disease, and hospitalization for an infection which significantly increase the risk of any autoimmune disease [12, 17,18,19]. However, some studies suggest that specific infections might be protective against some autoimmune diseases [20, 21].
Whether these findings and theories have clinical relevance for the long-term morbidity of TSCI individuals is unknown. There is an important distinction between the evident sensitization to self and the non-investigated symptomatic disease. Based on previous findings, we hypothesized that individuals with TSCIs would be at a higher risk of developing an autoimmune disease following trauma. We aimed to identify if an association exists between TSCI and diagnosed autoimmune disease.
Method
Study design, -population, and -period
A nationwide cohort of individuals born in Denmark between 1st January 1945, and 31st December 2018 was identified. Individuals had to be registered alive and residing in Denmark in the Danish Civil Registration System during the study period from 1st January, 1980–1st December, 2018. The years 1977–1979 were used as a washout to exclude prevalent cases of autoimmune disease and TSCI (see Fig. 1). Individuals (of any age; including pediatric) were longitudinally tracked from birth or 1st January 1980, whichever occurred later, until they reached an endpoint. Endpoints included the diagnose of autoimmune disease, death, emigration from Denmark, diagnosis of a spinal tumor, or the conclusion of the study on 31st December, 2018, whichever came first.
From 1945–1976 (blue period) people born in Denmark, who are still alive are registered. Registration continues until the end of the study. From 1977–31st Dec 1979 (green period) prevalent cases with either TSCI or AD are excluded from the study, leaving the TSCI population empty at the start of the study period. The purple period marks the main study period, where TSCIs are collected and risk time is counted until any endpoint is reached and here from censoring from the study. The yellow period marks the study period for DM-1. CRS Civil Registration System, DNPR Danish National Patient Registry, DM-1 Diabetes Mellitus type 1, DM-2 Diabetes Mellitus type 2, TSCI Traumatic Spinal Cord Injury, AID Autoimmune Disease.
Specifically for Type 1 diabetes mellitus (DM-1), this condition was first possible to distinguish from other types of diabetes in the Danish national patient registry from 1987 and onwards. The design for this outcome was similar, with 1987 serving as the washout period for prevalent cases, and the study period for DM-1 spanning from 1988–2018 (see Fig. 1).
Study variables
TSCI was identified from the Danish national patient registry. We utilized ICD-8 and ICD-10 codes to identify nine diagnoses covering cervical and thoracic types and levels of TSCI (see Supplementary 1 and Section 2.3). Paraplegia/tetraplegia and cord compression (ICD-8: 343.02, 343.03, and ICD-10: G82 and G952) had to be registered within +/- 7 days of a spinal fracture diagnosis and not in relation to a cancer diagnosis -10 year/+7 days timeframe. Conus medullaris TSCI (ICD-8: 958.11, 958.12, 958.13, 958.14, 958.18, 958.19 and ICD-10: S340, S341B, -C, -D, -E) was excluded, as its incidence was deemed inconsistent with clinical reality. ICD-8 diagnosis codes of 805.23, 805.31, 805.33, 805.69, and 805.79 covering different types of spinal fracture were not registered in during the study period and therefore removed from the statistical analysis.
In a secondary analysis, we categorized TSCI as either cervical or thoracic level of injury to evaluate a possible dose-response relationship based on the region of injury. The categorization is detailed in Supplementary 1.
As primary outcome was 31 autoimmune/-inflammatory diseases, categorized into eight groups as listed in Supplementary 2. Grouping was done to maintain confidentiality. The time of diagnosis was set to the first hospital contact for medical elucidation of autoimmune/-inflammatory disease ending with a diagnosis of such. For the TSCI group, an autoimmune disease diagnosis was further restricted as follows: a diagnosis of TSCI and autoimmune disease during the same hospital stay resulted in the exclusion of both TSCI and autoimmune disease and the individual was censored from the study. Supplementary 2 lists the autoimmune diseases and their grouping and Fig. 1 displays the study period for the various outcomes.
Registries
Statistics Denmark maintains the public Danish registries including The Civil registration system and Danish national patient registry. Since 1968, the Civil registration system has recorded information on people residing in Denmark. From here we have recorded; birthday, birth country, sex, migration status, death, and the person-specific and unique Civil registration system number [22]. Sex is identifiable from the Civil registration system number [22]. The Danish national patient registry contains information on all in- and outpatients visits, including diagnosis and temporal context. These variables were included in the study. Registration began in 1977 using the ICD-8 system, and the Danish national patient registry transitioned to the ICD-10 in 1994. Discrimination between type 1 and type 2 diabetes started in 1987 (see Fig. 1) [23, 24].
Co-variates
Charlson Comorbidity index was included in the analysis as a mediator to adjust for comorbidities and highlight the burden among individuals with TSCIs. The validated 2011 version from Christensen et. al. was used [25]. Charlson comorbidity index was evaluated as a time-dependent variable and modified as described in Supplementary 3, with the exclusion of connective tissue disease (an outcome), viral liver disease (included in hospitalization for an infection variable), primary biliary cirrhosis (an outcome), diabetes type 1 and 2, para- and tetraplegia (exposure), and AIDS. Diabetes type 1 was excluded as it is an outcome. Diabetes type 2 was excluded because most cases are managed by general practitioners who do not report diagnosis to the included registries. Therefore, diabetes type 2 was only adjusted based on diabetes complications that are managed in-hospital and reported to the included registries. AIDS was excluded as it was not considered a confounder. Age, sex, and calendar year were considered confounders. Hospitalization for infection was stratified in bacterial, viral, and other infections, evaluated as mediators with categorical variables as either 0 = no, 1 ≤ 5 years since hospitalization for infection, or 2 ≥ 5 years since hospitalization for infection, according to the study by Nielsen P.R. et al. [12] (see Table 1). Interpretation of the causal diagram is shown in Fig. 2.
Six mediated paths going; 1: TSCI → Detection bias → AID. 2: TSCI → Co-morbidity → AID. 3: TSCI → Co-morbidity → Infection → AID. 4: TSCI → Co-morbidity → infection → Detection bias → AID. 5: TSCI → Infection → AID6: TSCI → Infection → Detection bias → AID. In red is marked confounding paths. Genetics and lifestyle factors (marked with white) are unobserved and cannot be adjusted or restricted in the analysis. TSCI Traumatic spinal cord injury, AID Autoimmune disease.
Statistical analysis
The statistical analysis was conducted as a survival analysis using data recorded from 1st January, 1980–31st December, 2018, employing Poisson Regression with person years at risk as an offset variable. This model is equivalent to a Cox regression model [26, 27]. We used the Genmod procedure in the statistical software SAS version 9.4 (SAS Institute Inc., USA). Risk time was calculated from entry to the study until the individual reached the first endpoint, at which point they were censored from the study. An individual’s risk time was included in all outcomes, but only an individual’s first diagnosed autoimmune disease counted if that was the first temporal endpoint. We constructed three adjusted analyses, incorporating covariates from the previous model; (1) Basic adjustment: Included sex, age (in one‐year groups), and calendar year (in one‐year groups). (2) Charlson comorbidity index adjustment; Further adjusted for Charlson comorbidity index as time-dependent covariate. (3) Fully adjusted; Further adjusted for hospitalization for bacterial, viral, and other) infections (see Supplementary 4).
Results
The study included 4,874,564 individuals, accounting for 138,046,152 risk years. Of these 3272 was diagnosed with TSCI, accumulating 50,865 risk-years. The median annual TSCI incidence was 72 (IQR 64.5; 80.0). The annual incidence of TSCI is displayed in Supplementary 5.
Basic demographics of the TSCI and non-TSCI populations are displayed in Table 1.
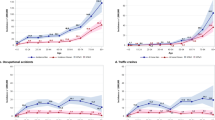
In total, 236 individuals with TSCI and 274,314 without TSCI had an autoimmune disease diagnosis (see Fig. 3). The incidence rate ratios (IRR) of being diagnosed with an autoimmune disease given a pre-existing TSCI are shown in Table 2 with three models displayed: From basic adjusted to fully adjusted model. TSCI showed either an increased IRR of being diagnosed with an autoimmune disease or no association across all outcomes. The overall incident association was IRR 1.81 (95% CI, 1.59 to 2.05) and IRR 1.32 (95% CI, 1.16 to 1.50) in the basic- and fully adjusted models, respectively. Among the eight groups of autoimmune diseases, the strongest association in the basic adjusted model were (a) Other neurologic IRR 5.19 (95% CI, 2.79 to 9.65), including myasthenia gravis and idiopathic polyneuropathy, (b) Multiple sclerosis IRR 3.70 (95% CI, 2.54 to 5.40), (c) Dermatologic IRR 2.57 (95% CI, 1.86 to 3.55), (d) DM-1 IRR 2.01 (95% CI, 1.54 to 2.61), (e) Systemic IRR 1.92 (95% CI, 1.44 to 2.55), and Gastroenterologic IRR 1.42 (95% CI, 1.05 to 1.92). Endocrine & haematologic and Iridocyclitis autoimmune diseases showed no association in the basic adjusted model. All associations were uniformly mitigated through adjustment. The significant associations for Gastroenterologic and DM-1 were eliminated in the Charlson comorbidity index- and fully adjusted models, respectively. The All-incident analysis is in supplementary 6 grouped in TSCI diagnosis before or from 1995 and forward as means of sensitivity analysis of TSCI diagnosis from ICD-8 and ICD-10 respectively. There was no significant difference.
Displaying a selection of study participants and accumulated person-years and the main outcome of the study; an overall increased IRR of 1.81 of being diagnosed with an autoimmune disease given a preexisting TSCI compared to the Danish background population.N counts, PY Person years, IR Incidence rate, IRR Incidence rate ratio AID Autoimmune Disease.
Table 3 shows the result for all-incident, Gastroenterologic, DM-1, multiple sclerosis, Dermatologic, and Systemic autoimmune diseases when TSCI was categorized as either cervical or thoracic. There were 130 cases of cervical TSCI and 106 cases of thoracic TSCI based on 29,512 and 21,192 person-years at risk, respectively. The all-incident types analysis suggests a tendency towards higher risk with thoracic TSCI for most outcomes, except for Dermatologic and Systemic types.
Discussion
In this nationwide cohort study, we found that TSCI is associated with a higher IRR of autoimmune diseases, particularly those affecting the nervous system. Additionally, we provide an overview of the associations for various autoimmune diseases, grouped primarily by the affected organ.
Although the biological pathway is not fully understood, a possible biological sequence from TSCI to chronic neuroinflammation, leading to secondary neurologic injury, the activation of neuro-autoreactive lymphoid cells, and ultimately autoimmunity might explain our findings [4, 5, 7, 10, 13]. The strong association of neurologic autoimmune diseases with TSCI aligns with the biological effects observed in previous experimental and observational studies.
Following TSCI, the initial immunological response involves polymorph nuclear myeloid infiltration of the lesion site, followed by M1 and M2 macrophages within the first hours to days [5]. Subsequently T-cells, especially CD8+ T-cells, are present, peaking early and persisting at about 10% of the peak concentration [5, 10]. B-cell expansion, maturation, and ectopic lymphoid follicle formation occur in the injured spinal cord, producing autoreactive antibodies such as anti-myelin basic protein (anti-MBP) [6, 7]. This process resembles the pathology seen in multiple sclerosis[16]. Recent human TSCI studies quantify the immunological response aligning with earlier experimental data, particularly the non-resolving aspects of the inflammatory cascade that may lead to central nervous system autoimmunity [13, 14]. Our study underscores the role of anti-MBP in secondary morbidity among TSCI patients, highlights its association with multiple sclerosis and Idiopathic polyneuropathy, both characterized by a pathological demyelination [5, 6, 8, 14, 16].
The development of Systemic and Dermatologic autoimmune diseases might be supported by the findings of systemic anti-nuclear antibodies (ANA) and anti-DNA (dsDNA) antibodies following TSCI, similar to those seen in rheumatism, systemic lupus erythematosus and autoimmune dermatologic diseases [7, 8]. These studies, along with our findings, suggest a true biological pathway where the combined innate and adaptive immune response to TSCI can lead to the maturation and clonal expansion of autoreactive T- and B-cells, ultimately leading to autoimmune disease.
That the initial increased risk of Gastroenterologic and DM-1 conditions, nullified in the Charlson comorbidity index and fully adjusted models, may indicate the influence of other factors on those associations. The impact of Charlson comorbidity index and hospitalization for infections, possibly arising from SCI-IDS and autonomic dysreflexia, emphasize their implications for multiorgan disease beyond autoimmune diseases.
SCI-IDS and inherited infectious susceptibility could mediate the pathway from TSCI to autoimmune disease [12]. Due to the small number of individuals with TSCI and an autoimmune disease, stratified analysis for formal mediation-analysis was not feasible [28]. Instead, we adjusted for hospitalization for infection to highlight its importance and the implicit risk, potentially modifiable pharmacologically. Interpretations should be cautious; we believe that only the direction, not the effect size, can be evaluated. The consistent direction of effect estimates suggests validity but does not rule out a potential collider bias.
We aimed to minimize misclassification of co-variates, suspecting that autoimmune diseases in the TSCI group could introduce detection bias or reversed causality, leading to differential misclassification. To mitigate this risk, we censored individuals diagnosed with TSCI and autoimmune disease during the same hospitalization, counting their risk time as non-TSCI, but excluding them as autoimmune disease cases. To avoid the confounding effects of multiple autoimmune diseases, we evaluated only an individual’s first autoimmune disease [19]. Despite these efforts, the multimorbidity and frequent hospitalizations of TSCI patients could lead to residual detection bias.
Table 3 suggests that thoracic TSCI predominantly increases the risk of autoimmune disease compared to a cervical TSCI. Initially, we hypothesized that cervical TSCI would be associated with a higher risk of autoimmune disease based on findings that higher injury levels amplify SCI-IDS and autonomic dysreflexia [3, 11]. Experimental studies have shown lesions above T9 reduce preganglionic inhibitory activity of postganglionic sympathetic nerves to the spleen, causing leukopenia and enhancing SCI-IDS [3, 11]. Similar findings apply to autonomic dysreflexia [3].
Our results indicate that non-penetrating thoracic TSCI might require more energy, leading to greater neurologic trauma and collateral damage, potentially explaining the higher risk of autoimmune disease despite less SCI-IDS and autonomic dysreflexia. Additionally, thoracic TSCI might result in more significant blood-spinal cord barrier disruption due to a higher probability of American Spinal Injury Association Impairment Scale (AIS) A injuries than cervical TSCI. Breakage of the blood-spinal cord barrier seems to be more prevalent and more pronounced in thoracic TSCI too [14]. Therefore, our findings could be more influenced by the magnitude of trauma than the level of TSCI.
Our definition of TSCI and the incidence (see Supplementary 5) aligns with Bjornshave Noe et al., report from the Spinal Cord Injury Centre of Western Denmark from 1990–2012 [29]. Our annual incidence data from 1981–2012 show realistic and relevant variation, but the increase from 2013-2018 might reflect misclassification. Table 1 shows the accumulated person years by calendar period. The TSCI population´s flattening curve and the steady state of the non-TSCI population in the study´s later period suggest possible bias from incidence issues in 2014–2018. Misclassified TSCIs may not have a higher autoimmune disease risk, potentially increasing type 2 error risk, but such bias cannot fully explain the association.
Our register-based study has limitations including small sample sizes in groups of TSCI patients with outcomes, and the inability to adjust for lifestyle factors like smoking, alcohol, body mass index, and familiar co-occurrence of autoimmune disorders. The positive predictive value of included variables is partially known and we cannot rule out misclassification from non-validated variables, though Danish registries are generally high quality [23]. The DM1 diagnosis has a high positive predictive value but unknown sensitivity, though a high sensitivity is expected given the clinical course [30].
The study population included all Danes born in Denmark, with complete public registration in the Danish Civil registration system, minimizing selection bias [22].
Several trauma-related factors including immediate treatment, pre-hospital vital parameters, pre-hospital transport time, initial AIS, decompressive surgery, and primary spinal cord tissue vitality could not be evaluated. These factors could illuminate the effect of secondary neurologic injury and inflammatory activity on autoimmune risk. The Danish TSCI demographics as described by Noe et al. [29] indicate that sharp and penetrating TSCI is rare, limiting our findings to blunt trauma TSCI populations.
Studying rare diseases risks large association deviations from small count variations. We advise the reader to consider raw counts, rates, and the full spectrum of estimated confidence intervals and associations. Based on our results, clinicians should monitor for potential late sequelae of TSCI. Prevention and medical optimization might reduce the Charlson comorbidity index´s impact and infection-related hospitalizations until further controlled studies are available.
Conclusions
TSCI is associated with an increased risk of developing autoimmune diseases, particularly those affecting the nervous system, in an open nationwide cohort with long follow-up. Infections following TSCI may explain some of the risk of developing autoimmune diseases.
Data availability
The data that support the findings of this study are available from Statistics Denmark but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are however available from the authors upon reasonable request and with permission of Danish Data Protection Agency, Statistics Denmark, and the Danish Health Data Authority.
References
Jazayeri SB, Maroufi SF, Mohammadi E, Dabbagh Ohadi MA, Hagen EM, Chalangari M, et al. Incidence of traumatic spinal cord injury worldwide: A systematic review, data integration, and update. World Neurosurg X. 2023;18:100171.
Sun X, Jones ZB, Chen XM, Zhou L, So KF, Ren Y. Multiple organ dysfunction and systemic inflammation after spinal cord injury: a complex relationship. J Neuroinflammation. 2016;13:260.
Zhang Y, Guan Z, Reader B, Shawler T, Mandrekar-Colucci S, Huang K, et al. Autonomic dysreflexia causes chronic immune suppression after spinal cord injury. J Neurosci. 2013;33:12970–81.
Kwiecien JM, Dabrowski W, Dabrowska-Bouta B, Sulkowski G, Oakden W, Kwiecien-Delaney CJ, et al. Prolonged inflammation leads to ongoing damage after spinal cord injury. PLoS One. 2020;15:e0226584.
Pruss H, Kopp MA, Brommer B, Gatzemeier N, Laginha I, Dirnagl U, et al. Non-resolving aspects of acute inflammation after spinal cord injury (SCI): indices and resolution plateau. Brain Pathol. 2011;21:652–60.
Zajarias-Fainsod D, Carrillo-Ruiz J, Mestre H, Grijalva I, Madrazo I, Ibarra A. Autoreactivity against myelin basic protein in patients with chronic paraplegia. Eur Spine J. 2012;21:964–70.
Ankeny DP, Lucin KM, Sanders VM, McGaughy VM, Popovich PG. Spinal cord injury triggers systemic autoimmunity: evidence for chronic B lymphocyte activation and lupus-like autoantibody synthesis. J Neurochem. 2006;99:1073–87.
Palmers I, Ydens E, Put E, Depreitere B, Bongers-Janssen H, Pickkers P, et al. Antibody profiling identifies novel antigenic targets in spinal cord injury patients. J Neuroinflammation. 2016;13:243.
Kopp MA, Meisel C, Liebscher T, Watzlawick R, Cinelli P, Schweizerhof O, et al. The spinal cord injury-induced immune deficiency syndrome: results of the SCIentinel study. Brain. 2023;146:3500–12.
Zrzavy T, Schwaiger C, Wimmer I, Berger T, Bauer J, Butovsky O, et al. Acute and non-resolving inflammation associate with oxidative injury after human spinal cord injury. Brain. 2021;144:144–61.
Brommer B, Engel O, Kopp MA, Watzlawick R, Muller S, Pruss H, et al. Spinal cord injury-induced immune deficiency syndrome enhances infection susceptibility dependent on lesion level. Brain. 2016;139:692–707.
Nielsen PR, Kragstrup TW, Deleuran BW, Benros ME. Infections as risk factor for autoimmune diseases - A nationwide study. J Autoimmun. 2016;74:176–81.
Schwab JM, Haider C, Kopp MA, Zrzavy T, Endmayr V, Ricken G, et al. Lesional Antibody Synthesis and Complement Deposition Associate With De Novo Antineuronal Antibody Synthesis After Spinal Cord Injury. Neurol Neuroimmunol Neuroinflamm. 2023;10:e200099.
Wichmann TO, Kasch H, Dyrskog S, Hoy K, Moller BK, Krog J, et al. The inflammatory response and blood-spinal cord barrier integrity in traumatic spinal cord injury: a prospective pilot study. Acta Neurochir (Wien). 2022:3143–53.
Louveau A, Harris TH, Kipnis J. Revisiting the mechanisms of CNS immune privilege. Trends Immunol. 2015;36:569–77.
Magliozzi R, Howell O, Vora A, Serafini B, Nicholas R, Puopolo M, et al. Meningeal B-cell follicles in secondary progressive multiple sclerosis associate with early onset of disease and severe cortical pathology. Brain. 2007;130:1089–104.
Olson JK, Croxford JL, Miller SD. Virus-induced autoimmunity: potential role of viruses in initiation, perpetuation, and progression of T-cell-mediated autoimmune disease. Viral Immunol. 2001;14:227–50.
Getts DR, Chastain EM, Terry RL, Miller SD. Virus infection, antiviral immunity, and autoimmunity. Immunol Rev. 2013;255:197–209.
Anaya JM, Corena R, Castiblanco J, Rojas-Villarraga A, Shoenfeld Y. The kaleidoscope of autoimmunity: multiple autoimmune syndromes and familial autoimmunity. Expert Rev Clin Immunol. 2007;3:623–35.
Christen U, Benke D, Wolfe T, Rodrigo E, Rhode A, Hughes AC, et al. Cure of prediabetic mice by viral infections involves lymphocyte recruitment along an IP-10 gradient. J Clin Invest. 2004;113:74–84.
Zaccone P, Fehervari Z, Phillips JM, Dunne DW, Cooke A. Parasitic worms and inflammatory diseases. Parasite Immunol. 2006;28:515–23.
Schmidt M, Pedersen L, Sorensen HT. The Danish Civil Registration System as a tool in epidemiology. Eur J Epidemiol. 2014;29:541–9.
Schmidt M, Schmidt SA, Sandegaard JL, Ehrenstein V, Pedersen L, Sorensen HT. The Danish National Patient Registry: a review of content, data quality, and research potential. Clin Epidemiol. 2015;7:449–90.
Denmark S Registry- and variable list, Statistics Denmark https://www.dst.dk/extranet/forskningvariabellister/Oversigt%20over%20registre.html: Denmarks Statistics; 2022 [updated 31st December 2021. Available from: https://www.dst.dk/extranet/forskningvariabellister/Oversigt%20over%20registre.html.
Christensen S, Johansen MB, Christiansen CF, Jensen R, Lemeshow S. Comparison of Charlson comorbidity index with SAPS and APACHE scores for prediction of mortality following intensive care. Clin Epidemiol. 2011;3:203–11.
Efron B. Logistic regression, survival analysis, and the Kaplan-Meier curve. J Am Stat Assoc. 1988;83:414–25.
Iacobelli S, Carstensen B. Multiple time scales in multi-state models. Stat Med. 2013;32:5315–27.
Rijnhart JJM, Lamp SJ, Valente MJ, MacKinnon DP, Twisk JWR, Heymans MW. Mediation analysis methods used in observational research: a scoping review and recommendations. BMC Med Res Methodol. 2021;21:226.
Bjornshave Noe B, Mikkelsen EM, Hansen RM, Thygesen M, Hagen EM. Incidence of traumatic spinal cord injury in Denmark, 1990-2012: a hospital-based study. Spinal Cord. 2015;53:436–40.
Thygesen SK, Christiansen CF, Christensen S, Lash TL, Sorensen HT. The predictive value of ICD-10 diagnostic coding used to assess Charlson comorbidity index conditions in the population-based Danish National Registry of Patients. BMC Med Res Methodol. 2011;11:83.
Funding
The funders of the study were not involved in any part of the research process. Open access funding provided by Aarhus University Hospital.
Author information
Authors and Affiliations
Contributions
Authors ordered with most influential first: Conceptualization: Mikkel Mylius Rasmussen Data Curation: Thomas Munk Laursen & Tim Damgaard Nielsen Formal analysis: Thomas Munk Laursen Funding acquisition: Tim Damgaard Nielsen & Mikkel Mylius Rasmussen Investigation: Equal Methodology: Bodil Hammer Bech, Tim Damgaard Nielsen, Mikkel Mylius Rasmussen, Thomas Munk Laursen Project administration: Tim Damgaard Nielsen & Mikkel Mylius Rasmussen Resources: Thomas Munk Laursen Software: Thomas Munk Laursen Supervision: Mikkel Mylius Rasmussen, Bodil Hammer Bech, Thomas Munk Laursen Validation: Mikkel Mylius Rasmussen, Tim Damgaard Nielsen, Bodil Hammer Bech Visualization: Tim Damgaard Nielsen, Thomas Munk Laursen Writing - original draft: Tim Damgaard Nielsen Review and editing: Mikkel Mylius Rasmussen, Bodil Hammer Bech, Thomas Munk Laursen.
Corresponding author
Ethics declarations
Competing interests
The study was funded by the victims fund (‘Offerfonden’) administratively placed under the Danish Ministry of Justice. All authors declare no actual or potential conflicts of interest with the funding source or other potential financial, professional, or personal relationships that may conflict with the study aims.
Ethics approval and consent to participate
The study was approved by the Danish Data Protection Agency, and data access was granted by Statistics Denmark and the Danish Health Data Authority. According to Act no. 1338 of 1 September 2020, section 10 on research ethics for the administration of health scientific research projects and health data scientific research projects, approval by the Ethics Committee and written informed consent were not required for register-based projects. All data were de-identified and not recognizable at an individual level.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Nielsen, T.D., Laursen, T.M., Bech, B.H. et al. Traumatic spinal cord injury and its correlation to risk of autoimmune/-inflammatory disease. Spinal Cord 62, 642–650 (2024). https://doi.org/10.1038/s41393-024-01026-0
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41393-024-01026-0