Abstract
While there is growing evidence of associations between infections and dementia risk, associations with cognitive impairment and potential structural correlates of cognitive decline remain underexplored. Here we aimed to investigate the presence and nature of any associations between common infections, cognitive decline and neuroimaging parameters. The UK Biobank is a large volunteer cohort (over 500,000 participants recruited aged 40–69) with linkage to primary and secondary care records. Using linear mixed effects models, we compared participants with and without a history of infections for changes in cognitive function during follow-up. Linear regression models were used to investigate the association of infections with hippocampal and white matter hyperintensity (WMH) volume. 16,728 participants (median age 56.0 years [IQR 50.0–61.0]; 51.3% women) had baseline and follow-up cognitive measures. We found no evidence of an association between the presence of infection diagnoses and cognitive decline for mean correct response time (slope difference [infections versus no infections] = 0.40 ms, 95% CI: −0.17–0.96 per year), visual memory (slope difference 0.0004 log errors per year, 95% CI: −0.003–0.004, fluid intelligence (slope difference 0.007, 95% CI: −0.010–0.023) and prospective memory (OR 0.88, 95% CI: 0.68–1.14). No evidence of an association was found between infection site, setting or frequency and cognitive decline except for small associations on the visual memory test. We found no association between infections and hippocampal or WMH volume. Limitations of our study include selection bias, potential practice effects and the relatively young age of our cohort. Our findings do not support a major role for common midlife infections in contributing to cognitive decline for this cohort. Further research is warranted in individuals with more severe infections, for infections occurring later in life.
Similar content being viewed by others
Introduction
Growing evidence from longitudinal studies supports the role of common infections such as sepsis [1,2,3,4], pneumonia [4, 5], other lower respiratory tract infections (LRTIs) [4], urinary tract infections (UTIs) [4, 5], and skin and soft tissue infections (SSTIs) [4, 5], in increasing the risk of dementia, though some findings have been conflicting [6].
Dementia has a long preclinical phase which can take decades to develop [7]. Before the clinical expression of dementia, cognitive and neuropathological changes associated with dementia progression can be observed but it is unclear whether infections are relevant during this process [8, 9]. Identifying the point at which infections may act before clinical onset of dementia might allow interventions to be targeted and timed appropriately to prevent or delay the onset of dementia.
Infection-related hospitalisations, particularly for sepsis and pneumonia, have been associated with cognitive decline [10,11,12,13,14]. However, there is limited understanding of the relationship of other sites of common infections diagnosed in different clinical settings such as primary care with changes in cognitive function over time. Other limitations of existing studies include either relatively small study sizes, the use of a single global measure of cognition rather than individual cognitive domains, or inadequate confounder adjustment, given the wide range of potential confounders [15,16,17,18,19,20,21,22,23,24].
A possible link between infections and other subclinical markers of dementia risk such as hippocampal atrophy and white matter hyperintensities (WMH) may exist. However, evidence on the link between common infections and these neuroimaging markers is scarce. Compared to cognitive function measures, neuroimaging measures may be less prone to the effects of sociodemographic influences such as education; investigating both cognitive decline and neuroimaging measures may allow us to triangulate our findings across different outcomes associated with dementia risk.
Therefore, we aimed to explore the association between common infections and subclinical markers of dementia (cognitive decline, hippocampal volume and WMH volume) in a population without pre-existing dementia or evidence of cognitive impairment. We then assessed whether these associations differed by infection site, clinical setting, frequency and timing of infections.
Methods
Study design and population
We used data from the UK Biobank study, an ongoing prospective study which recruited over 500,000 participants aged 40–69 between 2006 and 2010 from 22 assessment centres based in England, Wales and Scotland [25]. Over 9 million individuals registered with the National Health Service (NHS) who lived within 40 km of one of the UK Biobank assessment centres were invited to take part in the study via postal invitations, however, the response rate was low with 5.5% consenting to take part in the study and attending the baseline assessment [25, 26]. The methodology of the UK Biobank has been described previously and is summarised in the Supplementary Information [27].
Linkage to primary care data for ~45% of the cohort has been made available by UK Biobank for non-COVID research [28]. To minimise exposure misclassification, our study population was limited to only participants with linked primary and secondary care records (Fig. 1). We excluded participants who had less than 12 months registration with a GP practice to avoid incorporating historical diagnoses when defining our exposure as previous studies suggest historical diagnoses may be recorded within the first 12 months when a patient registers with a GP practice [29]. We defined baseline as the date participants attended the UK Biobank baseline assessment. A subset of participants was invited to attend the first repeat assessment (2012–13) and the first wave of the neuroimaging assessments (2014 onwards). Cognitive function was assessed at all three assessments.
Our study explored two subsets of the UK Biobank population, a cognition subset, and a separate neuroimaging subset. For the cognition subset, we included participants with valid measures of cognitive function completed at baseline and at least one follow-up measure on the same test. For our neuroimaging cohort, we included only participants with data on hippocampal or WMH volume who attended the first neuroimaging visit. We excluded participants with dementia or cognitive impairment at baseline in both cohorts using self-report data and linked primary and secondary care records. We excluded participants with a history of dementia or cognitive impairment because the aim of our study was to investigate whether infections were associated with earlier or subclinical markers of dementia risk thus we were specifically interested in the stage before clinical expression of dementia.
Exposures
Our exposures were one or more of the following common infections: sepsis, pneumonia, other LRTIs, UTIs and SSTIs. We examined these as exposures in combination and separately. Sepsis is defined as a serious, life-threatening condition caused by a dysregulated host response following a range of infections [30]. Infections were identified in the 5 years up to UK Biobank participants’ baseline assessment visit. This time period of 5 years was chosen due to issues with the completeness of historical linked primary care data. Infections were defined using Read codes in linked primary care records and International Classification of Diseases (ICD)-10 codes in hospital records. To increase the specificity of our infection definition, participants were defined as having UTIs or SSTIs if they were also prescribed antibiotics on the same date as infection diagnosis.
Outcomes
Cognitive function
Participants completed a 15 min battery of computerised cognitive function tests including measurement of reaction time which is referred to in this study as the mean correct response time test, visual memory (pairs matching test), fluid intelligence (verbal-numerical reasoning) and prospective memory. Details of these tests and their association with age have been reported elsewhere [31, 32]. Our outcome measures for these tests were: (1) mean correct response time (milliseconds) taken for a participant to correctly identify matching pairs of cards (Data-field 404), (2) total number of incorrect matches in participants who completed the visual memory test (Data-field 399), (3) total number of incorrect answers on the fluid intelligence test (Data-field 20016) and (4) participants were scored 0 for the correct answer and 1 for an incorrect answer at the first attempt for the prospective memory test (one minus Data-field 20018). Lower scores in all cognitive tests indicated better performance. We dealt with outliers for mean correct response time using an approach consistent with the method outlined by the UK Biobank. We therefore excluded response times under 50 milliseconds due to anticipation and response times over 2000 milliseconds were excluded as the UK Biobank indicates that the cards used for this web-based test had disappeared by then.
Neuroimaging measures
We used measures of hippocampal volume (Data-fields 25019 and 25020) with lower volumes being indicative of Alzheimer’s disease pathology and WMH volume (Data-field 25781) with higher volumes indicative of cerebral small vessel disease pathology measures from the first imaging visit (Supplementary Information). We assessed the total volume of WMH volume using postprocessed measures from T1 and T2 weighted fluid attenuation inversion recovery (FLAIR) imaging technique derived by the UK Biobank study [33, 34].
Covariates
Data from baseline assessment questionnaires, verbal interview and linked primary and secondary care data were used to define covariates. Demographic variables included age (years), sex, ethnicity (White European, South Asian, African or Caribbean, Mixed or Other) and years in full-time education based on the International Standard Classification of Education (ISCED) 1997 (Supplementary Table 1) [35, 36]. Socioeconomic status was measured using the Townsend Deprivation scores [37]. Potential lifestyle factors included body mass index (BMI, kg/m2), smoking, alcohol intake frequency and physical activity. Diabetes was ascertained using HbA1c and all data sources mentioned above. Other comorbidities included anxiety and depression, asthma, chronic kidney disease, chronic liver disease, chronic obstructive pulmonary disease, heart failure, hypertension, inflammatory bowel disease, multiple sclerosis, obstructive sleep apnoea, rheumatoid arthritis, psoriasis, severe mental illness, stroke and traumatic brain injury (Supplementary Information). Code lists for covariates ascertained in electronic health records can be accessed at: https://doi.org/10.17037/DATA.00002573.
Missing data on covariates was minimal (≤3.6% in total) in both cohorts and not all of these covariates were adjusted for in each analysis thus we used a complete case analysis for all analyses (Supplementary Information).
Approval for the UK Biobank study was obtained from the North West Multi-Centre Research Ethics Committee and the present research was conducted under application number 7661. All participants of the study provided written informed consent. Ethical approval was also obtained from the London School of Hygiene and Tropical Medicine research ethics committee (reference number 22721).
Statistical analysis
We developed a statistical analysis plan before conducting our analyses as shown in the Supplementary Material pages 33–47. We descriptively explored the potential for selection bias in our study by comparing the baseline characteristics of participants included and excluded from our study.
Association between common infections and cognitive decline
For each continuous cognitive measure (mean correct response time, visual memory and fluid intelligence), we fitted linear mixed models with random intercept and slope effects using an unstructured covariance matrix to estimate the rates of cognitive decline over follow-up in participants with and without a history of infections. Interaction terms were fitted between infections and time since baseline to assess the difference in cognitive decline over follow-up. Due to skewed distribution and zero value inflation of the visual memory error scores, a value of one was added to the scores which were then logn-transformed. For the dichotomous test (prospective memory), we used logistic regression models for participants with correct recall at baseline to examine the association between infections and cognitive decline with a binary variable (coded as 0 for correct recall and 1 for incorrect recall at follow-up).
For linear mixed models, minimally adjusted models included age, sex and an interaction term between time and infection. For all other analyses, minimally adjusted models included age and sex. For each analysis, we considered adjustment for all potential confounders described above and adjusted for covariates that changed the main association estimates by an important amount (9% or greater change in association magnitude) in the fully adjusted model.
In our secondary analyses, we investigated the association between site, clinical setting (GP-recorded or hospital-recorded), frequency (with the number of infections modelled as a continuous variable) and timing of infections expressed as year(s) since infection diagnosis in the 5 years up to baseline (0 to <1 year, 1 to <2 years, 2 to <3 years, 3 to <4 years and 4 to 5 years). Given the potential interaction between inflammatory comorbidities, such as diabetes, and dementia pathogenesis, we explored whether the associations of infections on cognition differ by diabetes category (using a binary variable for diabetes) and tested for the presence of effect modification by fitting an interaction term [38]. We performed additional analyses to compare the associations between infections and cognitive decline by age group (40–49, 50–59 and 60+) and sex. This is because increasing age is associated with greater trajectories of cognitive decline and some studies have reported sex differences in cognitive decline [39, 40].
Association of common infections with hippocampal and WMH volume
We log-transformed WMH volume due to a positively skewed distribution. We used linear regression models to estimate the association between infections and each structural neuroimaging measure. We used the same strategy for confounder adjustment as the approach described for our cognitive decline analyses. To aid interpretation, log-transformed WMH volume was reported using exponentiated betas and was interpreted as percentages. For example, exponentiated beta 1.01 refers to a 1% increase in WMH volume.
Sensitivity analyses
We conducted a range of sensitivity analyses to test the robustness of our findings. First, we found evidence of non-normal distribution for mean correct response time. However, when we inverse or log transformed this variable, we were unable to fit the models due to unstable standard errors and models failing to converge. Thus, we used raw scores in our main analyses and in a sensitivity analysis we specified an independent covariance structure which allowed us to re-run our models using the inverse transformed variable which showed evidence of a normal distribution (Supplementary Information). Second, we repeated our main analyses excluding participants diagnosed with infections during follow-up to reduce misclassification of our exposure. Third, we repeated our main analyses excluding participants whose current registration date with a GP practice was <5 years. Given that infections were defined within 5 years prior to baseline, this analysis ensured that all participants had at least 5 years of follow-up in which to capture infection diagnoses. Fourth, previous studies suggest infections may have differing associations with the left and right hippocampus thus we repeated our main analyses on hippocampal volume separately for the left and right hippocampus [41].
Statistical analyses were performed in Stata MP (version 16.0) and RStudio (version 4.1.0).
Results
Of the 176,207 participants with linked primary and secondary care records and no history of cognitive impairment or dementia at baseline, 16,728 (9.5%) had baseline and at least one follow-up cognitive measure on the same test, and of whom 2,004 (12.0%) had two follow-up cognitive measures. 14,712 participants completed neuroimaging measurements at the first imaging visit (Fig. 1). The mean time interval between baseline and the first or second repeat cognitive function assessment was 4.0 years (sd 0.78) and 8.27 years (sd 1.6), respectively. Compared to participants without follow-up cognitive measures, participants included in our study were slightly younger, less likely to be female, had more years in education, fewer infections and performed better on baseline cognitive tests (Table 1). Further descriptive information on infections in participants included and excluded from the study is presented in Supplementary Table 2. 323 (1.0%) participants excluded from the study had infection-related mortality compared to 5 (0.2%) participants included in the study.
Characteristics of participants included in the two subsets of our study, one with follow-up cognitive measures and the other who attended the first imaging visit, are presented in Table 2 and Supplementary Fig. 1. 11, 455 participants were included in both cohorts. In our cognition cohort, the median age was 56.0 (IQR, 50.0–61.0) and 51.3% were female. 2,971 (17.8%) participants were diagnosed with a previous infection at least 5 years prior to baseline. These infections included 23 (0.1%) sepsis, 45 (0.3%) pneumonia, 1,681 (10.1%) other LRTIs, 674 (4.0%) UTIs and 532 (3.2%) SSTIs. 6 participants (0.0%) had multiple infection diagnoses on the same date from different infection sites. 2,770 participants (93.2%) had GP-recorded infections and 201 (6.8%) had hospital-recorded infections.
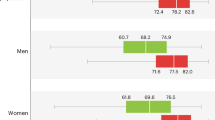
Figure 2 and Table 3 show no evidence for differences in cognitive performance change over follow-up in participants with a history of any infections compared to those without infections for the mean correct response time (estimated difference in slope [infections versus no infections] = 0.40 ms, 95% CI: −0.17–0.96 per year), visual memory (estimated difference in slope 0.0004 log errors per year, 95% CI: (−0.003–0.004), fluid intelligence (estimated difference in slope 0.007, 95% CI: −0.010–0.023) and prospective memory tests (OR 0.88, 95% CI: 0.68–1.14). The results for all covariates for these models are shown in Supplementary Table 3. No evidence of an association was found between the site and clinical setting of infections with cognitive decline for any of the tests, apart from visual memory. The log of the visual memory errors increased by 0.011 (95% CI: 0.004–0.018) per year in participants with a history of UTIs compared to those with no prior infection.
Linear mixed models with random intercept and slope used to illustrate fitted changes in cognitive function over time for the mean correct response time, visual memory (log transformed) and fluid intelligence test. A Mean correct response time models adjusted for age (years), sex, time, baseline test score, interaction term with time × infection status, ethnicity, BMI, years in full-time education, physical activity, alcohol consumption, diabetes, anxiety and depression, COPD, multiple sclerosis, hypertension and heart failure. B Visual memory models adjusted for age (years), sex, time, baseline test score, interaction term with time × infection status, ethnicity, BMI, smoking status, socioeconomic deprivation, physical activity, alcohol frequency, years in full-time education, diabetes, anxiety and depression, COPD, hypertension, inflammatory bowel disease, rheumatoid arthritis, obstructive sleep apnoea, and multiple sclerosis. C Fluid intelligence models adjusted for age (years), sex, time, baseline test score, interaction term with time × infection status and years in full-time education.
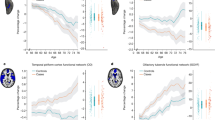
Association between infections and neuroimaging outcomes
Figure 3 shows that a history of any infections and LRTIs excluding pneumonia was associated with a 5% higher WMH volume compared to no prior infection in minimally adjusted models. In fully adjusted analyses, the difference reduced to a 2% higher WMH volume for those with infections and included the null. No evidence of an association was found between the presence or site of infections with hippocampal volume in minimally or fully adjusted models.
WMH; White matter hyperintensities. A represents the association between common infections and hippocampal volume. Minimally adjusted models for adjusted for age (years) and sex. Fully adjusted models additionally adjusted for ethnicity, BMI, smoking, physical activity, alcohol consumption, years in full-time education, diabetes, chronic obstructive pulmonary disease, asthma and hypertension (n = 14,239). B represents the association of common infections with WMH volume. Minimally adjusted models for (B) adjusted for age (years) and sex and fully adjusted models additionally adjusted for BMI, smoking and hypertension (14,357).
Additional secondary analyses and sensitivity analyses
Secondary analyses on the association between numbers of infections and cognitive decline show that the increase over time in the log of visual memory errors was slightly steeper by 0.006 (95% CI: 0.002 to 0.011) per year, for every additional infection (Supplementary Table 4). No evidence of an association was found between the number of infections beyond the first and cognitive decline in all other tests. Supplementary Fig. 2 depicts the association between the timing of infections in the 5 years prior to baseline and cognitive decline in fully adjusted models. We found no evidence of an association between common infections in each year prior to baseline and cognitive decline according to any of the tests. In further additional secondary analyses, we found evidence of an interaction by diabetes for mean correct response time (p for interaction = 0.015). Participants with diabetes and infections performed better on mean correct response time compared to participants with diabetes and no infection. In stratified results, there was no evidence of an association between common infections and cognitive decline in any of the cognitive tests in people with and without diabetes (Supplementary Table 5). We found no difference by sex and age in the association between infections and cognitive decline for any of the cognitive measures (Supplementary Tables 6, 7). Our sensitivity analyses did not materially change our conclusions (Supplementary Tables 8–12).
Discussion
To our knowledge, this is the largest longitudinal study to date examining the association of common infections occurring in midlife with subclinical markers of dementia risk (cognitive decline, hippocampal volume and WMH volume). We did not find evidence for an association between common infections and cognitive decline for any of the cognitive measures, except for visual memory. We found evidence of small associations between UTIs and an increasing number of infections with worsening of performance on the visual memory test over follow-up. Infections were not associated with lower hippocampal or higher WMH volume after adjustments for potential confounding.
Previous studies
Previous studies have yielded mixed findings for the association between infections and cognitive impairment. In a US case-control study of intensive care unit survivors (ICU) with a mean age of 65.9 years, no association was found between sepsis and cognitive decline [42]. However, given that ICU stay and sepsis are associated with mortality risk, the competing risk of mortality in ICU survivors with sepsis may have weakened the associations found in this study [43, 44]. Two prospective US studies with a mean and median age, respectively, of 77 years found an association between pneumonia or severe sepsis hospitalisation and cognitive impairment [10, 12].
Differences in our findings compared to previous studies may be due to heterogeneity in populations studied including their ages, clinical setting, site of infection, cognitive measures and domains assessed, and study design. Participants in our study were younger (mean/median both 56 years) than those in previous studies. Age is an important risk factor for cognitive decline and dementia, with the risk of dementia doubling every 5 years after the age of 65 [45]. We found no evidence of an association between hospitalised infections with cognitive decline, however, we had a reduced power to detect an association as only a small subset of 201 (6.8%) participants with infections had hospitalised infections while those with hospital infections in previous studies ranged from 827 to 1,529 participants [10, 12, 42]. These studies only assessed sepsis or pneumonia as individual exposures; however, our study had insufficient statistical power to study the association of these infections with cognitive decline individually. Given that exposed participants in our study were predominantly diagnosed with more mild infections (GP-recorded infections and other LRTIs), this may explain the lack of association observed as it is hypothesised that more severe systemic infections may be more likely to trigger the release of pro-inflammatory cytokines and induce systemic inflammation (or other pathways) which may lead to cognitive decline or dementia [46]. Alternatively, it is also possible that hospitalised infections do not play a role in cognitive decline and the association shown by previous studies may be driven by factors related to hospitalisation and cognition.
Two case-control studies found lower hippocampal volume in hospitalised individuals with sepsis compared to healthy controls [41, 47]. These studies were limited by their small sample size (<45 participants each) and one study had inadequately matched controls. Differences in study design and statistical method limited comparability of these studies with our findings. White matter lesions have been identified in septic shock patients who developed acute brain dysfunction, however, there is a lack of studies examining the association of common, predominantly bacterial infections, other than sepsis with WMH or hippocampal volume [48].
An explanation for our lack of evidence of an association between infections, cognitive decline, hippocampal or WMH volume could be that these neuroimaging or cognitive measures may have lacked sufficient sensitivity to detect subtle brain changes following infection in the prodromal phases. Alternatively, it could be that our finding of small associations between infections and cognitive decline on the visual memory test should be interpreted with caution. Given the number of analyses on multiple cognitive tests conducted in this study, it is possible that these findings may have occurred by chance.
Strengths and limitations
Strengths of this study include the large size of the study population and the use of repeated assessments over follow-up assessing four individual domains of cognition. The extensive information on sociodemographic and lifestyle factors and comorbidities linked to primary and secondary care electronic health records allowed for the adjustment of multiple confounding variables. Furthermore, we explored medically recorded common infections by infection site, severity, timing and dose response as well as conducting extensive secondary and sensitivity analyses.
Our study had several limitations. First, there was evidence of a ‘healthy volunteer’ bias in the cohort studied and in the overall UK Biobank population [25]. In this study, this selection bias was likely given that participants with poorer cognitive ability and fewer years in education were more likely to have no follow-up cognitive measures. This selective attrition would likely underestimate any associations of common infections with cognitive decline thus biasing our estimates towards the null. Selection bias may have also occurred if individuals with more severe infections did not attend the baseline assessment, biasing associations towards the null. Second, our findings may also have been influenced by a potential practice effect in which participants’ performance on the same cognitive tests improved during follow-up due to familiarity with the test [49]. Although both infected and uninfected groups would have been expected to have a similar benefit of practice, these practice effects may dilute any differences between the two groups therefore potentially masking any association of infections on cognitive decline [31, 49]. Third, cognitive tests were non-standardised and visual memory test results have poor correlation between the baseline and the first repeat assessment (r = 0.16) which will likely have led to non-differential measurement error, biasing effect estimates towards the null [31]. Fourth, although we assessed a wide range of potential confounders, we cannot rule out the possibility of residual confounding through unmeasured confounders e.g. frailty and other forms of physical activity such as light intensity physical activity or social activities. Fifth, we restricted our analyses to only infections diagnosed within 5 years prior to baseline, therefore, infections occurring prior to this period were not included in our primary analyses which may underestimate our associations. Sixth, neuroimaging measures were assessed at one time point in our study thus we were unable to investigate longitudinal changes in hippocampal and WMH volume over time. Seventh, our study focused on a population without dementia or cognitive impairment at baseline as such our findings cannot be generalised to individuals with existing cognitive impairment/dementia. Eighth, participants in our study had a mean age of ~55 years old which may limit the generalisability of our findings to older adults, who are at a greater risk of cognitive decline and dementia. Lastly, our study population was healthier than the general population and had more years in education compared to those excluded during follow-up. This may have delayed cognitive decline thus reducing the ability to detect a significant association between common infections and cognitive decline.
Conclusion
In summary, our findings extend the scarce literature on infections, cognitive decline and neuroimaging measures into a younger age group than the majority of previous studies. We found no evidence of accelerated cognitive decline in people across the age groups of 40–69 (at UK Biobank recruitment) with a history of common infections occurring in midlife compared to those without infections in all cognitive tests except for visual memory. Further studies are needed to assess the potential effects of common infections on cognition at different life stages and in more representative populations, including ethnic and other diversity with sufficient sample sizes to test different types of infection. These studies need careful attention to loss to follow-up as well as incorporating the impacts of mortality. Future studies should also explore trajectories of cognitive decline in people with pre-existing cognitive impairment or dementia following infection and investigate longitudinal changes in hippocampal volume, WMH volume and other subclinical neuropathologies over time in individuals with and without infections.
Code availability
Analysis codes used in this study can be accessed at https://github.com/RutendoMuzambi/InfectionsCognitionNeuroimaging.
Data availability
Data are available to researchers through an application via https://www.ukbiobank.ac.uk/enable-your-research/register.
References
Shah FA, Pike F, Alvarez K, Angus D, Newman AB, Lopez O, et al. Bidirectional relationship between cognitive function and pneumonia. Am J Respir Crit Care Med. 2013;188:586–92.
Tate JA, Snitz BE, Alvarez KA, Nahin RL, Weissfeld LA, Lopez O, et al. Infection hospitalization increases risk of dementia in the elderly. Crit Care Med. 2014;42:1037–46.
Mawanda F, Wallace RB, McCoy K, Abrams TE. Systemic and localized extra-central nervous system bacterial infections and the risk of dementia among US veterans: a retrospective cohort study. Alzheimers Dement. 2016;4:109–17.
Muzambi R, Bhaskaran K, Smeeth L, Brayne C, Chaturvedi N, Warren-Gash C. Assessment of common infections and incident dementia using UK primary and secondary care data: a historical cohort study. Lancet Healthy Longev. 2021;2:e426–35.
Morton CEFH, Pearce N, Smeeth L, Warren-Gash C. Association between common infections and incident post-stroke dementia: a cohort study using the clinical practice research datalink. Clin Epidemiol. 2020;12:907–16.
Ahlström B, Larsson I-M, Strandberg G, Lipcsey M. A nationwide study of the long-term prevalence of dementia and its risk factors in the Swedish intensive care cohort. Crit Care. 2020;24:548.
Bäckman L, Jones S, Berger AK, Laukka EJ, Small BJ. Cognitive impairment in preclinical Alzheimer’s disease: a meta-analysis. Neuropsychology. 2005;19:520–31.
Bäckman L, Jones S, Berger AK, Laukka EJ, Small BJ. Multiple cognitive deficits during the transition to Alzheimer’s disease. J Intern Med. 2004;256:195–204.
Brayne C, Richardson K, Matthews FE, Fleming J, Hunter S, Xuereb JH, et al. Neuropathological correlates of dementia in over-80-year-old brain donors from the population-based Cambridge city over-75s cohort (CC75C) study. J Alzheimers Dis. 2009;18:645–58.
Iwashyna TJ, Ely EW, Smith DM, Langa KM. Long-term cognitive impairment and functional disability among survivors of severe sepsis. JAMA. 2010;304:1787–94.
Ehlenbach WJ, Hough CL, Crane PK, Haneuse SJ, Carson SS, Curtis JR, et al. Association between acute care and critical illness hospitalization and cognitive function in older adults. Jama. 2010;303:763–70.
Davydow DS, Hough CL, Levine DA, Langa KM, Iwashyna TJ. Functional disability, cognitive impairment, and depression following hospitalization for pneumonia. AM J Med. 2013;126:615–24.e5.
Pandharipande PP, Girard TD, Jackson JC, Morandi A, Thompson JL, Pun BT, et al. Long-term cognitive impairment after critical illness. N Engl J Med. 2013;369:1306–16.
Gracner T, Agarwal M, Murali KP, Stone PW, Larson EL, Furuya EY, et al. Association of infection-related hospitalization with cognitive impairment among nursing home residents. JAMA Netw Open. 2021;4:e217528.
Irving PM, de Lusignan S, Tang D, Nijher M, Barrett K. Risk of common infections in people with inflammatory bowel disease in primary care: a population-based cohort study. BMJ Open Gastroenterol. 2021;8:e000573.
Listing J, Gerhold K, Zink A. The risk of infections associated with rheumatoid arthritis, with its comorbidity and treatment. Rheumatology. 2012;52:53–61.
Seminog OO, Goldacre MJ. Risk of pneumonia and pneumococcal disease in people with severe mental illness: English record linkage studies. Thorax. 2013;68:171–6.
Kourbeti IS, Vakis AF, Papadakis JA, Karabetsos DA, Bertsias G, Filippou M, et al. Infections in traumatic brain injury patients. Clin Microbiol Infect. 2012;18:359–64.
Chiner E, Llombart M, Valls J, Pastor E, Sancho-Chust JN, Andreu AL, et al. Association between obstructive sleep apnea and community-acquired pneumonia. PloS ONE. 2016;11:e0152749.
Livingston G, Huntley J, Sommerlad A, Ames D, Ballard C, Banerjee S, et al. Dementia prevention, intervention, and care: 2020 report of the Lancet Commission. Lancet. 2020;396:413–46.
Zilkens RR, Bruce DG, Duke J, Spilsbury K, Semmens JB. Severe psychiatric disorders in mid-life and risk of dementia in late- life (age 65-84 years): a population based case-control study. Curr Alzheimer Res. 2014;11:681–93.
Sangha PS, Thakur M, Akhtar Z, Ramani S, Gyamfi RS. The link between rheumatoid arthritis and dementia: a review. Cureus. 2020;12:e7855.
Zhang B, Wang HE, Bai Y-M, Tsai S-J, Su T-P, Chen T-J, et al. Inflammatory bowel disease is associated with higher dementia risk: a nationwide longitudinal study. Gut. 2021;70:85–91.
Andrade AG, Bubu OM, Varga AW, Osorio RS. The relationship between obstructive sleep apnea and Alzheimer’s disease. J Alzheimers Dis. 2018;64:S255–70.
Fry A, Littlejohns TJ, Sudlow C, Doherty N, Adamska L, Sprosen T, et al. Comparison of sociodemographic and health-related characteristics of UK biobank participants with those of the general population. Am J Epidemiol. 2017;186:1026–34.
Swanson JM. The UK Biobank and selection bias. Lancet. 2012;380:110.
Sudlow C, Gallacher J, Allen N, Beral V, Burton P, Danesh J, et al. UK biobank: an open access resource for identifying the causes of a wide range of complex diseases of middle and old age. PLoS Med. 2015;12:e1001779.
U.K. Biobank. UK Biobank Primary care linked data version 1.0. 2019. https://biobank.ndph.ox.ac.uk/showcase/showcase/docs/primary_care_data.pdf. Accessed 17 January 2022
Lewis JD, Bilker WB, Weinstein RB, Strom BL. The relationship between time since registration and measured incidence rates in the General Practice Research Database. Pharmacoepidemiol Drug Saf. 2005;14:443–51.
Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, et al. The third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA. 2016;315:801–10.
Lyall DM, Cullen B, Allerhand M, Smith DJ, Mackay D, Evans J, et al. Cognitive test scores in UK biobank: data reduction in 480,416 participants and longitudinal stability in 20,346 participants. PLOS ONE. 2016;11:e0154222.
Cornelis MC, Wang Y, Holland T, Agarwal P, Weintraub S, Morris MC. Age and cognitive decline in the UK Biobank. PLOS ONE. 2019;14:e0213948.
U.K. Biobank. UK Biobank Brain Imaging Documentation version 1.8. https://biobank.ctsu.ox.ac.uk/crystal/crystal/docs/brain_mri.pdf.2020. Accessed 17 January 2022
Littlejohns TJ, Holliday J, Gibson LM, Garratt S, Oesingmann N, Alfaro-Almagro F, et al. The UK Biobank imaging enhancement of 100,000 participants: rationale, data collection, management and future directions. Nat Commun. 2020;11:2624.
ISCED. International Standard Classification of Education. http://uis.unesco.org/sites/default/files/documents/internationalstandard-classification-of-education-1997-en_0.pdf.1997. Accessed 17 January 2022
Schneider SL. The International Standard Classification of Education (ISCED-97): an evaluation of content and criterion validity for 15 European countries. Mannheim: Mannheimer Zentrum für Europäische Sozialforschung (MZES). 2008.
Townsend P, Phillimore P, Beattie A. Health and deprivation: inequality and the North. Croom Helm. 1988
Sandu RE, Buga AM, Uzoni A, Petcu EB, Popa-Wagner A. Neuroinflammation and comorbidities are frequently ignored factors in CNS pathology. Neural Regen Res. 2015;10:1349–55.
McCarrey AC, An Y, Kitner-Triolo MH, Ferrucci L, Resnick SM. Sex differences in cognitive trajectories in clinically normal older adults. Psychol Aging. 2016;31:166–75.
Levine DA, Gross AL, Briceño EM, Tilton N, Giordani BJ, Sussman JB, et al. Sex differences in cognitive decline among US adults. JAMA Netw Open. 2021;4:e210169.
Semmler A, Widmann CN, Okulla T, Urbach H, Kaiser M, Widman G, et al. Persistent cognitive impairment, hippocampal atrophy and EEG changes in sepsis survivors. J Neurol Neurosurg Psychiatry. 2013;84:62–9.
Sakusic A, Gajic O, Singh TD, O’Horo JC, Jenkins G, Wilson GA, et al. Risk factors for persistent cognitive impairment after critical illness, nested case-control study. Crit Care Med. 2018;46:1977–84.
Moitra VK, Guerra C, Linde-Zwirble WT, Wunsch H. Relationship between ICU length of stay and long-term mortality for elderly ICU survivors. Crit Care Med. 2016;44:655–62.
Rhee C, Jones TM, Hamad Y, Pande A, Varon J, O’Brien C, et al. Prevalence, underlying causes, and preventability of sepsis-associated mortality in US acute care hospitals. JAMA Netw Open. 2019;2:e187571.
Hugo J, Ganguli M. Dementia and cognitive impairment: epidemiology, diagnosis, and treatment. Clin Geriatr Med. 2014;30:421–42.
Perry VH, Cunningham C, Holmes C. Systemic infections and inflammation affect chronic neurodegeneration. Nat Rev Immunol. 2007;7:161.
Yuan M, Yan D-Y, Xu F-S, Zhao Y-D, Zhou Y, Pan L-F. Effects of sepsis on hippocampal volume and memory function. World J Emerg Med. 2020;11:223–30.
Polito A, Eischwald F, Maho A-L, Polito A, Azabou E, Annane D, et al. Pattern of brain injury in the acute setting of human septic shock. Crit Care. 2013;17:R204.
Calamia M, Markon K, Tranel D. Scoring higher the second time around: meta-analyses of practice effects in neuropsychological assessment. Clin Neuropsychol. 2012;26:543–70.
Funding
RM is supported by an Alzheimer’s Society Ph.D. studentship 379 (AS-PhD-17-013). CWG is supported by a Wellcome Intermediate Clinical Fellowship, Wellcome Trust (201440/Z/16/Z). KB holds a Wellcome Senior Research Fellowship (220283/Z/20/Z) and also held a Sir Henry Dale Fellowship jointly funded by the Wellcome Trust and the Royal Society during this work. VG is jointly funded by a grant from Diabetes UK and the British Heart Foundation (grant 15/0005250).
Author information
Authors and Affiliations
Contributions
CWG, KB, LS, CB, RM, NC, CTR, VG, and DMW contributed to the conception and/or design of the study. RM analysed the data and wrote the first draft of the paper. All authors were involved in the data interpretation and revision of the paper.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Muzambi, R., Bhaskaran, K., Rentsch, C.T. et al. Are infections associated with cognitive decline and neuroimaging outcomes? A historical cohort study using data from the UK Biobank study linked to electronic health records. Transl Psychiatry 12, 385 (2022). https://doi.org/10.1038/s41398-022-02145-z
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41398-022-02145-z