Abstract
Hepatocellular carcinoma (HCC) is closely linked to alterations in the gut microbiota. This dysbiosis is characterized by significant changes in the microbial population, which correlate with the progression of HCC. Gut dysbiosis ultimately promotes HCC development in several ways: it damages the integrity of the gut-vascular barrier (GVB), alters the tumor microenvironment (TME), and even affects the intratumoral microbiota. Subsequently, intratumoral microbiota present a characteristic profile and play an essential role in HCC progression mainly by causing DNA damage, mediating tumor-related signaling pathways, altering the TME, promoting HCC metastasis, or through other mechanisms. Both gut microbiota and intratumoral microbiota have dual effects on HCC progression; a comprehensive understanding of their complex biological roles will provide a theoretical foundation for potential clinical applications in HCC treatment.
Similar content being viewed by others
FACTS
-
1.
Gut dysbiosis drives HCC progression through mechanisms such as gut-vascular barrier (GVB) disruption, tumor microenvironment (TME) remodeling, and translocation of microbial metabolites (e.g., LPS, SCFAs) that induce chronic inflammation and immune suppression.
-
2.
TLR4 signaling is a central hub linking gut dysbiosis to HCC progression. LPS-TLR4 interactions drive stemness, angiogenesis, and metastasis through various signaling pathways, metabolites, and immune cells, highlighting its potential as a therapeutic target.
-
3.
Bile acids and SCFAs mediate dual roles in HCC. While hydrophobic bile acids (e.g., DCA) promote HSC senescence and Treg expansion, SCFAs like butyrate suppress tumor growth via CD8+ T cell activation. However, acetate’s role is context-dependent, influenced by dietary factors and microbial sources.
-
4.
Intratumoral microbiota exhibits HCC-specific profiles, with increased Proteobacteria, Firmicutes, and Fusobacterium in tumor tissues. These microbes are closely associated with gut microbiota and contribute to DNA damage, signaling pathway activation (e.g., TLR4/JNK), and immunosuppression.
OPEN QUESTIONS
-
1.
How do HCC etiologies (e.g., viral vs. non-viral) shape gut and intratumoral microbiota heterogeneity? Are microbial biomarkers (e.g., Klebsiella for microvascular invasion) universally applicable across subtypes?
-
2.
What molecular pathways link microbial metabolites to epigenetic reprogramming (e.g., TET2 in B cells, FOXP3 in Tregs) and HCC progression? Can these pathways be reversed through dietary or pharmacological interventions to become therapeutic targets in the clinical treatment of HCC?
-
3.
Since the relationship between the microbiota and the immune system is so intimate, can modulation of specific microbial taxa (e.g., Akkermansia, Bifidobacterium) or metabolites (e.g., butyrate) enhance immunotherapy efficacy (e.g., anti-PD-1) in HCC? What are the optimal strategies for microbiota-targeted adjuvant therapies?
-
4.
What mechanisms govern the translocation and colonization of gut-derived microbes into HCC tissues? How do intratumoral microbiota interact with the TME to influence immune evasion or metastasis?
Introduction
Hepatocellular carcinoma
Hepatocellular carcinoma (HCC) is the most common type of liver malignancy, accounting for approximately 90% of cases, and one of the most common cancers worldwide. It is also one of the most harmful tumors, characterized by high morbidity and mortality rates [1, 2]. According to 2022 GLOBOCAN estimates, there were 865,269 new cases worldwide, accounting for 4.3% of the new cancer cases that year. Moreover, it is the third leading cause of cancer-related death globally, causing 757,948 deaths (7.8%) in 2022 [3].
The pathophysiology of HCC, from oncogenesis to progression, is a complex, multistep process involving dysregulation of cancer driver genes and related signaling pathways [4, 5], abnormal infiltration of immune cells [6, 7], metabolic factors (such as glucose, lipids, and key enzymes) [8,9,10,11,12], and many other factors. Among these factors, the gut microbiota plays a significant role.
Gut microbiota
Gut microbiota composition
The human gastrointestinal tract harbors a complex ecosystem of approximately 2000 genera of bacteria, fungi, archaea, and viruses [13, 14]. The collective genomes of these microorganisms, known as the gut microbiome, encode an estimated five million genes [15, 16]. In this review, we concentrate primarily on the gut bacteria, highlighting the predominance of Bacteroidetes and Firmicutes, which together account for nearly 90% of the bacterial population. Other less dominant bacteria include Proteobacteria (Pseudomonadota), Actinobacteria (Actinomycetota), and Verrucomicrobia [17].
Gut microbiota function
The gut microbiota has important functions for the host. The microbes not only participate in food digestion, molecules decomposition and synthesis, and absorption, providing energy and nutritional support for the host [18, 19], but they also maintain the normal host-physiological functions by regulating metabolism [20,21,22]. By directly or indirectly interacting with the immune system and other aspects of the internal environment, the gut microbiota further protects the host against pathogen invasion and influences disease progression [23,24,25].
Gut dysbiosis in HCC
Gut microbial dysbiosis is the imbalance or other similar alteration in the composition and/or function of the gut microbiota, which may lead to or worsen diseases [26, 27].
The dysbiosis profile
Several studies have found that the gut microbiota in HCC is characterized by a distinctive dysbiosis profile [28]. The structure of the gut microbiota was found to be significantly altered in HCC patients compared to non-HCC patients with or without liver cirrhosis, while no significant difference in gut microbiome composition was found in HCC patients with different etiologies [29]. Across various studies involving different populations, fecal samples, and sample sizes, the trends in the gut dysbiosis profiles in HCC were concordant, though there were subtle differences in the exact results. For example, the phyla Firmicutes and Actinobacteria were significantly increased in the gut of HCC patients [30]. The genus Clostridium increased during HCC progression and may be related to bile acid metabolism [30, 31]. The genus Ruminococcus is greatly increased in patients with HCC compared to other liver diseases [32], yet this genus tends to colonize the intestines of HCC patients without liver microvascular invasion [33], which demonstrates the nuanced differences in gut microbiota distribution across HCC subtypes. The genera Enterococcus also tends to be increased in the gut of HCC patients [34, 35], including the Enterobacter ludwigii, which showed a significant increase of 100 times higher in HCC than other compared groups [36], and the Enterococcaceae which could be a potential marker for HCC diagnosis [37]. The genera Streptococcus and Lactobacillus belong to Firmicutes and enriched in the gut of HCC as well [38,39,40]. Although the genus Bifidobacterium mainly belongs to the phylum Actinobacteria, its abundance tends to be reduced in the gut of HCC patients as the beneficial bacteria [35], and decreases further as the disease progresses [34]. The genera belonging to the phylum Actinobacteria and increased in the gut of HCC patients include Atopobium [41] and Gemmiger [42]. In the phyla Bacteroidetes, fecal samples from HCC patients have higher levels of the genera Desulfovibrio [30], Bacteroides [30, 35], and Parabacteroides [42]. In the phyla Proteobacteria, levels of Escherichia coli [41] and Shigella [33] were increased as well.
Beneficial bacteria, typically reduced in the gut of HCC patients, include Akkermansia, Prevotella_2, Subdoligranulum and Faecalibacterium were decreased [38,39,40].
In a study held by Yang et al. [33] examining fecal microbiota profiles in 364 hepatitis B virus (HBV)-HCC patients and controls, Streptococcus (14.14% v.s. 5.67%) and Escherichia-Shigella (11.5% v.s. 9.55%) were more abundant in HCC than the control group, while Agathobacter was strongly decreased even though it belongs to the phylum Firmicutes. Li et al. [32] examined the gut microbiota in 68 patients with HCC, 33 patients with liver cirrhosis (LC), and 34 normal controls (NC). In their results, 21 genera, including Roseburia, Lachnospira, and Ruminococcus, were increased in HCC compared to LC, and 42 genera including Veillonella, Faecalibacterium, Alistipes, and Phaecolarctobacterium, were strongly decreased in HCC compared to NC. Nevertheless, 35 species, such as Phocaeicola vulgatus, Lachnospira eligens, Bacteroides uniformis, and Ruminococcus bicirculans, differed between HCC and LC. The other significantly increased species in HCC compared to NC included Veillonella parvula, Veillonella sp. T1–7, Veillonella atypica, and Veillonella dispar, and the decreased including Phocaeicola dorei, Bacteroides uniformis, Faecalibacterium prausnitzii, etc.
Selective gut microbiota as potential biomarkers in HCC
Selective gut bacteria have emerged as potential biomarkers for HCC detection, demonstrating high sensitivity and specificity. For instance, Odoribacter splanchnicus and Ruminococcus bicirculans are potential species-level biomarkers of HCC [32], and the combinatorial detection of Coriobacterium, Atopobium and Coprococcus at the genus level was of high diagnostic value in HCC as well [43].
As biomarkers of HCC, the abundance of some gut bacteria closely changed with phenotypes during the tumorigenesis or progression. In a study by Ren et al. [42] analyzing fecal samples from patients, there are 13 genera including Parabacteroides and Gemmiger which were increased in early stage HCC and could serve as microbial markers for the early diagnosis of HCC. In a study by Zhang et al. [34] studying HCC patients as well, higher levels of Enterococcus and Enterobacteriaceae and lower levels of Actinobacteria and Bifidobacterium were statistically related to higher HCC stage and thus worse prognosis. The abovementioned Streptococcus and Escherichia-Shigella were more abundant in HCC and kept ascending during HCC progression thus had the potential of HCC biomarkers as well [33]. There were also significant differences in the gut microbiota between HCC patients with and without microvascular invasion (HCC-MVI or HCC-NVI), HCC-MVI is often accompanied by high invasiveness, high metastasis, and higher malignancy. In HCC-MVI compared to HCC-NVI, Klebsiella, Proteobacteria, Prevotellaceae, and Enterobacteriaceae were significantly enriched, whereas Firmicutes, Ruminococcus, and Monoglobaceae were significantly decreased. Among these gut bacteria, Klebsiella was the key biomarker that distinguished the two subgroups, even predicting clinical outcomes [44]. In 2019, Ni et al. [45] found that pro-inflammatory bacteria significantly increased in HCC patients compared to healthy controls. Furthermore, they introduced an assessment metric, the degree of dysbiosis (D(dys)), and found that it significantly increased in HCC patients compared to healthy controls. In addition, D(dys) increased consistently with HCC stage, although the differences among the stages were not significant.
In 2020, Huang et al. [31] collected fecal samples from 113 HBV-related HCC patients and 100 healthy controls for 16S rRNA sequencing, and selected 32 paired tumor and adjacent non-tumor liver tissues from the HCC group for next-generation RNA sequencing [31]. As a result, they found the increased abundance of Lachnospiracea incertae sedis was accompanied by a decrease in cluster of differentiation (cd) 6 expression, the increased abundance of Bacteroides was accompanied by a decrease in mitogen-activated protein kinase (mapk) 10 expression, and both of the bacteria were in line with sorrower disease-free survival (P = 0.0092 and 0.084, respectively). This result makes sense because CD6 and MAPK10 are tumor suppressors associated with better clinical prognosis. The profiles of gut microbiota and their biomarkers closely related with HCC progression are summarized in Fig. 1.
Breakdown of gut-vascular barrier integrity due to gut dysbiosis
Foremost among all mechanisms, the initial biological event linking gut dysbiosis to tumor progression is the disruption of the gut-vascular barrier (GVB). The gut barrier consists of three layers. The outermost layer is the mucus layer, which mainly exists to shield against pathogens such as certain bacteria [46, 47]. To strongly decrease bacterial migration into the inner section of this mucus layer, antimicrobial peptides (e.g., defensins, lysozyme, and c-lectin Reg3γ) are secreted by intestinal epithelial cells and immune cells (Paneth cells), and immunoglobulin A (IgA) is secreted by plasma cells [48]. The middle layer consists of tightly connected epithelial cells, which ensure selective nutrient transfer while limiting the entry of gut microbes, especially pathogens, from the gut into the host [49]. The innermost layer is the blood vessel endothelium. If pathogens translocate through the intestinal epithelium into the bloodstream, they are mostly blocked by this layer and eliminated by circulating macrophages or engulfed by dendritic cells (DCs) before being transported to mesenteric lymph nodes [50].
In the healthy state, the GVB is characterized by the selective permeability of nutrients, metabolites, water, and bacterial products, the GVB integrity is governed by cellular, neural, immune, and hormonal factors [51]. While in the context of gut microbiota dysbiosis, the integrity of the GVB can be is compromised through a series of interconnected mechanisms. The disruption of the gut barrier, also known as increased intestinal permeability or “leaky gut,” is driven by several factors related with the gut microbiota dysbiosis, briefly including: (1) Inflammation: Chronic low-grade inflammation, often a result of dysbiosis, can lead to the release of pro-inflammatory cytokines and chemokines that damage the tight junctions between intestinal epithelial cells, thereby increasing permeability [51]. For example, HCC patients had a higher level of Proteobacteria, which favors intestinal mucosa inflammation and thus higher gut barrier permeability [52]. Another example, increased harmful microbiota approaching the epithelium can contribute to the local inflammation [53], and dysbiosis-caused increased populations of pathogenic species of bacteria like E. coli, Bacteroides Enterococci and Clostridium histolyticum, which could dismiss higher levels of lipopolysaccharides (LPS) damaging the enterocytes, thus disrupting GVB [54]. (2) Direct Invasion by Pathogens: Some bacteria associated with dysbiosis can invade the gut mucosa, causing damage to the epithelial layer or its function [51, 55]. (3) Metabolic Disruptions: Some products or metabolites which are secreted or regulated by the gut microbiota can affect the balance and function of the intestinal epithelium, leading to barrier dysfunction [56]. Akkermansia, which is decreased in HCC [35], protects the GVB by metabolites like acetate and propionate [57, 58]. This bacteria can also improve GVB by upregulating the expression of some TJ proteins or significantly reduce the LPS level [59].
As a result, gut dysbiosis increases the permeability of the barrier, which allows substances such as short-chain fatty acids (SCFAs), bile acids (BAs), bacterial constituents, choline, and endogenous ethanol to enter the liver, increasing the hepatic metabolic load and inflammatory stimulation, thus increasing the progression of HCC [60]. Due to increased intestinal permeability, factors such as viable pathogenic bacteria, Gram-negative microbial products, and pro-inflammatory luminal metabolites can translocate from the intestinal lumen to the liver via the portal circulation and thereby alter the hepatic microenvironment [49, 61].
Mechanisms by which the gut microbiota influences the HCC-related microenvironment
The gut microbiota can profoundly affect the immune microenvironment of the liver and thereby trigger hepatocarcinogenesis via the following processes: (1) microbial activation of signaling like Toll-like receptor (TLR)-4; (2) microbial stimulation of tumor microenvironment (TME) cells; and (3) influence of gut microbiota-associated metabolites. The typical examples are summarized in Table 1.
PAMP-PRR (TLR4) related signal pathways
Pattern-recognition receptors (PRRs) can sense gut microorganisms based on their pathogen-associated molecular patterns (PAMPs; namely, “microbe-associated molecular patterns”, MAMPs) and subsequently exert biological effects. Among the PRRs, TLR4 is an important PRR that plays an immunosuppressive role and it is a key contributor to hepatocarcinogenesis [62, 63].
TLR4 is widely expressed in liver cancer stem cells, hepatocytes, Kupffer cells, hematopoietic stem cells, DCs, natural killer (NK) cells, B cells, and T cells. TLR4 predominantly recognizes LPS from Gram-negative bacteria [63,64,65,66] and is downregulated by HCC-suppressing microRNAs (miRNAs) such as miR122 [67]. Gut dysbiosis and TLR4 (and associated signaling) are required not for the initiation of HCC, but for its development [68].
TLR4 is overexpressed in HCC [69] and correlates with microvascular invasion, early recurrence, and poor prognosis in HCC patients [66, 70, 71].
In early HCC patients, LPS-producing gut bacterial genera and LPS were both increased [42]. LPS activated the TLR4-AKT-SOX2 signaling pathway and thereby induced HCC stem cells [72]. Furthermore, LPS/TLR4 signaling promoted HPC fibrotic differentiation and increased interleukin (IL)-6 and tumor necrosis factor (TNF)-α production in rats transplanted with diethylnitrosamine-induced HCC and with exogenous hepatic progenitor cells (HPCs) [73].
In another study, TLR4 recognized LPS and directly activated c-Jun N-terminal kinase (JNK)/MAPK signaling to improve epithelial-mesenchymal transition (EMT), tumor cell invasion, and metastasis [74]. Furthermore, the TLR4-MyD88 (namely Myeloid Differentiation Primary Response 88) axis activated STAT3 (Signal Transducer and Activator of Transcription 3) and SP1 (Specificity Protein 1), which are both transcription factors of the mRNA of the vascular endothelial growth factor (VEGF), so VEGF was overexpressed, which improved HCC angiogenesis and pulmonary metastasis [65].
In addition to directly affecting tumor cells, TLRs modulate other immune cells or stromal cells to affect the HCC TME. Dysbiotic microbiota in Nlrp6(−/−) mice (the mice with mutant NLR family, pyrin domain containing 6) induces a TLR4-dependent expansion of hepatic monocytic myeloid-derived suppressor cells (mMDSCs) and suppresses T-cell abundance. This phenotype is transmissible via fecal microbiota transfer and reversed by antibiotics, pointing to the high plasticity of the TME. While the loss of Akkermansia muciniphila correlates with mMDSC abundance, its reintroduction restores intestinal barrier function and strongly reduces liver inflammation and fibrosis. Furthermore, a study showed that cirrhosis patients have increased bacterial abundance in hepatic tissue, which induces pronounced transcriptional changes, including activation of fibro-inflammatory pathways and cancer immunosuppression processes. This study demonstrated that the gut microbiota closely shapes the hepatic inflammatory microenvironment, offering new approaches for cancer prevention and therapy. TLR4 seemed to indirectly manage the recruitment of regulatory T cells (Tregs) and interacted with macrophages to promote intrahepatic metastasis [75]. TLR4 induced neutrophil extracellular traps (NETs) in the liver and thereby promoted alcoholic steatosis and, eventually, alcoholic HCC [76], it increased HCC metastasis potential mainly bypassing tumorous inflammatory response [77].
Other signaling pathways downstream of the gut microbiota exerted more complicated and even dual effects. For example, certain nonpathogenic E. coli strains stimulated the transcription of genes related to nuclear factor kappa-light-chain-enhancer of activated B cells (NF-κB) mediated inflammatory signaling pathways, while upregulated negative feedback regulators in nucleotide-binding oligomerization domain (NOD)-like signaling pathways, such as tumor necrosis factor alpha-induced protein 3 (TNFAIP3), tempered the inflammatory reaction [78]. Understanding whether and how these factors influence HCC development requires further exploration.
HCC-associated cells and TME
The TME is a complex integrated system mainly composed of tumor cells, surrounding immune and inflammatory cells, tumor-related fibroblasts, nearby interstitial tissues, microvessels, and various cytokines and chemokines [79, 80]. Gut microbes and their metabolites can influence HCC pathogenesis and progression by changing the intestinal microenvironment, altering ligands for specific receptors and modulators of certain protein activities, modulating signaling pathways, and ultimately influencing the expression of various genes in key cells and multiple cytokine levels in the TME [64, 81]. How the gut microbiota influenced HCC progression through the interaction with molecular signaling pathways and various cells were summarized in Fig. 2.
LPS/TLR4 signaling (activated by Gram-negative bacteria) promotes fibrotic differentiation of hepatic progenitor cells (HPCs) and enhances IL-6/TNF-α production, disrupting Ras and p53 pathways to drive malignant proliferation. The TLR4-MyD88 axis activates STAT3 and SP1, upregulating VEGF expression and promoting angiogenesis/metastasis. C. scindens converts primary bile acids into secondary bile acids, decreasing CXCL16 expression and NKT cell recruitment. LTA from Gram-positive bacteria activates IL-33/IL-1β in hepatic stellate cells (HSCs) via TLR2, promoting Treg-mediated HCC progression.
In addition to hepatocytes and HCC cells, the HCC TME involves the following cells: (1) immune cells, such as neutrophils, circulating monocytes/macrophages, resident macrophages (Kupffer cells), DCs, NK cells, natural killer T (NKT) cells, B cells, and T cells such as CD8+ T cells, CD4+ T cells, Tregs, and γδ T cells [82] and (2) other liver-resident cells in the environment or stroma surrounding the HCC cells, such as hepatic stellate cells (HSCs), fibroblasts, and liver sinusoidal endothelial cells [83, 84].
Neutrophils
Tumor-associated neutrophils (TANs) in HCC can be categorized as antitumorigenic (N1) or pro-tumorigenic (N2) [85]. Pro-tumorigenic N2 TANs support HCC by forming decondensed chromatin embedded with granular proteins, namely NETs [85]. Gut microbiota-induced LPS-TLR4 signaling promoted pro-tumorigenic N2 TANs and related NETs in alcoholic HCC [76]. During HCC treatment, TANs were reported to recruit tumor-associated macrophages and Tregs through the secretion of chemokine (C-C motif) Ligand (CCL) 2 and CCL17 to induce drug resistance [86].
Macrophages
Macrophages are classified into two functionally and phenotypically distinct categories: macrophages with an embryonic origin that reside in the liver after specific differentiation (Kupffer cells), and macrophages differentiated from circulating monocytes (circulating monocyte-derived macrophages, called “macrophages” below for short) [87]. When circulating macrophages are recruited to the liver via stimulation by pathological factors in the TME, they polarize into different phenotypes (mainly M1 and M2) [88]. M1 macrophages have an antigen-presenting function, so they can combat pathogenic microorganisms [89] and tumor formation [90], exerting pro-inflammatory effects [91]. M2 macrophages usually support anti-inflammation effects [91], tissue remodeling and angiogenesis [92, 93], while promoting tumors [94]. The gut microbiota can alter macrophage polarization by stimulating certain signaling pathways in the gut microenvironment. In a mouse model of colon inflammation, deoxycholic acid (DCA) was enriched by increased levels of Gram-positive bacteria, which promoted macrophage polarization toward the pro-inflammatory M1 phenotype (partially through TLR2 transactivated by the M2 muscarinic acetylcholine receptor) [95]. However, there was no concrete evidence that bile acids regulated HCC via these mechanisms.
When gut dysbiosis promoted M2 macrophage polarization, HCC pathogenesis was promoted. For example, IL-25, which was secreted by colonic hyperplastic epithelial tuft cells and induced by gut dysbiosis, increased the M2 percentage (CD206/CD68) and Chemokine (C-X-C motif) Ligand (CXCL) 10 secretion of macrophages to promote HCC [96]. Macrophages also contributed to HCC subcomponent phenotypes. A study in 2022 found an increased proportion of M2-type tumor-associated macrophages in HCC patients with microvascular invasion compared to HCC patients without microvascular invasion (P < 0.001). The exact mechanism underlying this phenomenon needs to be further explored [44].
Kupffer cells
Kupffer cells are the key cells that interact with LPS in the liver, and they also play a key role in inducing cytokines such as TNFα and IL-6, which promote the development of HCC associated with microbe-related LPS-TLR signaling [97]. In addition to HCC, Kupffer cells can affect other liver diseases. For example, Kupffer cells ameliorate early alcohol-induced liver injury after endotoxin activation via TLR4 [98]. In an animal model of non-alcoholic steatohepatitis (NASH), various factors such as metabolic disorders, oxidative stress, and translocated bacterial products activated Kupffer cells via TLRs, especially TLR4, leading to increased NF-κB signaling and pro-inflammatory cytokine production [99]. When translocated bacterial DNA bound to TLR9 on Kupffer cells, the cells produced IL-1b, thereby stimulating hepatocytes to accumulate lipids and inducing liver fibrosis [100].
NKT cells
In a mouse model reported in 2018 [101], NKT cell accumulation was regulated by CXCL16 from liver sinusoidal endothelial cells, which was controlled by gut microbiome-mediated primary-to-secondary bile acid conversion. For example, bile acid-modulating commensal bacteria like C. scindens, could convert primary bile acids into secondary bile acids. While antibiotics significantly increased primary bile acids, tauro-β-muricholic acid (T-β-MCA) and β-MCA, and decreased secondary bile acids, T-ω-MCA, taurodeoxycholic acid, ω-MCA, taurolithocholic acid, and tauroursodeoxycholic acid. Secondary bile acid ω-MCA decreased cxcl16 mRNA expression, whereas the primary bile acid T-β-MCA induced Cxcl16 mRNA. As a result, antibiotics indirectly upregulated CXCL16 in liver sinusoidal endothelial cells. Next, the accumulated CXCL16 bound to C-X-C Chemokine Receptor (CXCR) 6 on NKT cells and thereby recruited them, which led to anti-tumor effects against HCC. In contrast, bile acid-modulating bacteria (such as C. scindens) induced HCC progression via the bile acid-CXCL16-CXCR6 axis. In a NASH-associated HCC mouse model, NKT cells were stimulated by the gut microbe A. muciniphila, which thereby prevented HCC progression [102].
B cells
B cells contribute to NASH pathogenesis by activating metabolic T cells and monocyte-derived macrophages (via IgA secretion), thereby promoting fibrosis [103].
In the HCC TME, B cells usually interact with T cells to enhance anti-tumor effects thus improving prognosis [104]. For instance, B cells could be triggered by oxidative stress and then activate Tet methylcytosine dioxygenase 2 (TET2) to promote IL-10 expression [105], and high levels of IL-10 in B cells are usually correlated with HCC progression [106]. Theoretically, gut microbiota could regulate the TET2 level in B cells by modulating oxidative stress [107], and TET2 downregulation supported antitumor immunity to improve anti-programmed death (PD)-1 treatment for HCC [105]. In this way, TET2 inhibition in B cells by the gut microbiota may aid HCC treatment.
T cells
In the pathogenesis of HCC, the gut microbiota and their metabolites often interact with Tregs to establish immunosuppression in the liver [108].
In 2021, nonalcoholic fatty liver disease (NAFLD)-HCC was characterized by expansion of Bacteroides caecimuris (P < 0.0001) and Veillonella parvula (P = 0.002) and dysbiosis of other gut microbes [28]. Accordingly, flow cytometry showed that NAFLD-HCC induced the recruitment of effector IL-10+ Tregs, thus attenuating the expansion of cytotoxic CD8+ T cells [28]. Both Tregs and CD8 + T cells in HCC TME expressed dysfunction markers such as PD-1, Lag-3, and Tim-3 [109].
Many studies have determined the critical role of CD8+T cells in defending against HCC initiation and progression, which improves prognosis [110]. Different CD8 + T cells may predict different HCC incidences. CD8+ resident memory T cells and Tregs were enriched in HBV-related HCC, whereas Tim-3+CD8+ T cells and CD244+ NK cells were enriched in non-viral-related HCC [111]. CD8+T cells were recently found to predict truly recurrent HCC [112]. Single-cell RNA-sequencing of 34 samples from 20 recurrent HCC patients showed that the TME of truly recurrent HCC had more KLRB1 (Killer Cell Lectin Like Receptor B1, namely CD161)+CD8+ T cells with memory phenotype and low cytotoxicity, while the TME of de novo recurrent HCC had more cytotoxic and exhausted CD8+ T cells [112].
CD8+ T cells are generally considered to have anti-tumor effects, while expression of other different markers would present different states and functions of T cells, thus may exert totally different effects on HCC. For example, in the pro-inflammation and pro-tumoral environment formed by the gut microbiota, CD8+CXCR6+PD1+ T cells usually have an auto-aggressive, exhaustive and resident phenotype, which ultimately contribute to HCC pathogenesis [113].
With the effect of inhibiting the proliferation, activation and functions of other cytotoxic T cells, Foxp3+ CD4+ regulatory T cells (Tregs) became the most crucial subset of CD4+ T cells during HCC progression, especially from simple steatosis to HCC for their immunosuppressive effects [108]. Deoxycholic acid (DCA) and lithocholic acid (LCA) were the most abundant metabolites of the gut microbiota, and some gut microbiota may synthesize certain molecules of the bile acids [114]. Certain LCA derivative, isoalloLCA, was found to stimulate mitochondrial reactive oxygen species to upregulate FOXP3, thus exerting an immunosuppressive effect by inducing Treg differentiation [115]. 3β-hydroxydeoxycholic acid (isoDCA) also induced Treg differentiation by acting on DCs to activate FOXP3 [116]. Some subtypes of LCA or DCA synthesized by the gut microbiota may also mediate T cells through certain mechanisms.
HSCs
In a mouse model of HCC induced by a high-fat diet [117], lipoteichoic acid (a cell wall component of Gram-positive gut microbes) triggered IL-33 and IL-1β released from senescent HSCs. IL-33 was IL-1β-dependent and promoted HCC development via Treg activation in the TME. In 2017, a mouse model was used to show that obesity-induced lipoteichoic acid suppressed antitumor immunity and thereby promoted HCC [118]. The lipoteichoic acid enhanced the senescence-associated secretory phenotype and the COX2 level in HSCs in a process involving TLR2. As a result, COX2-mediated prostaglandin E2 (PGE2) boosted Tregs and PD-1+ CD8+ T cells by binding to PTGER4 (Prostaglandin E Receptor 4) on them, thereby contributing to HCC progression. Tregs can upregulate PD-1 on CD8+ T cells, and PD-1 is an inhibitory molecule that impairs the antitumor effect of T cells [119]. COX2 overexpression and excess PGE2 production were detected in HSCs in human NASH-triggered HCC, suggesting that the gut microbiota-driven COX2-PGE2-PTGER4 pathway may function in human NASH-associated HCC [118].
Fibroblasts
In HCC progression, cancer-associated fibroblasts induced neutrophil chemotaxis, protected neutrophils from spontaneous apoptosis, and activated neutrophils via the IL6-STAT3 signaling cascade, and then these neutrophils impaired T cell function via the Prostaglandin E Receptor 41/PD-L1 signaling pathway [120].
Microbe-derived metabolites mediate HCC progression
Bile acids
Bile acids are key metabolites related to gut bacteria or the whole gut microbiota [115]. They are synthesized from amphipathic cholesterol in the liver and directly regulated by the farnesoid X receptor (FXR)-fibroblast growth factor 19 (FGF19) axis [121] and G protein-coupled bile acid receptor 1 (GPBAR1/TGR5) [122]. Bile acids are modulated by gut bacteria to generate bioactive molecules [115], with the major effect of solubilizing dietary lipids to help their absorption in the small intestine [123]. After that, about 95% of bile acids are reabsorbed and recycled via the gut–liver axis, and the remaining 5% of bile acids enter the colon to facilitate the production of the major serum bile acids, DCA and LCA, via dihydroxylation; this process is mediated by gut microbes [3, 124, 125].
One of the most important biological effects of bile acids is their crucial role in the differentiation of T cells and macrophage polarization. Distinct derivatives of LCA and DCA (including iso-, 3-oxo-LCA/DCA, allo-, 3-oxoallo-, and isoalloLCA) are involved [126, 127]. 3-oxoLCA inhibited the differentiation of Th17 cells by binding to the small molecule agonist RORγt [115], while isoalloLCA stimulated anti-inflammatory Treg differentiation by upregulating FOXP3 via mitochondrial reactive oxygen species generation and the binding of NR4A1 at the Foxp3 locus [128]. 3β-hydroxydeoxycholic acid (isoDCA) also induced Treg differentiation by acting on DCs to activate FOXP3 [116]. In a mouse model of colonic inflammation, DCA was enriched after Gram-positive bacteria increased, and DCA then promoted macrophage polarization toward the pro-inflammatory M1 phenotype partially via TLR2 transactivated by the M2 muscarinic acetylcholine receptor [95]. As T cells and macrophages both affect the hepatocarcinogenesis-related immune response, bile acids may regulate HCC via these mechanisms.
In recent years, there has been increasing evidence that the gut microbiota influences hepatic metabolic homeostasis by regulating bile acid synthesis and metabolism, leading to HCC development and progression.
DCA, a hydrophobic bile acid, has been reported to be closely related to DNA damage and cell survival [129, 130]. In mice, dietary or genetic obesity increased the DCA level (related to dysbiosis). DCA then induced HSC senescence, thus stimulating the secretion of multiple cytokines that induce hepatocarcinogenesis [131].
Hydrophobic bile acids, under the control of the gut microbiota, may promote HCC. During NASH-HCC formation and development, when bacterial taxa involved in bile acid metabolism (such as the genera Clostridium, Bacteroides, and Desulfovibrio) were significantly increased, the taurochenodeoxycholate (TCDCA) level was strongly increased, while decreasing hydrophobic bile acids reversed NASH-HCC progression [30]. In further in vitro tests, DCA-, LCA-, and TCDCA-treated HepG2 cells all grew faster and had higher oncoprotein levels, illustrating the hepatocarcinogenesis-promoting effects of these hydrophobic bile acids [30]. These findings were further supported by Ma et al. in 2018 [101]. They found that gut microbiota-mediated primary-to-secondary bile acid conversion indirectly disturbed NKT cell accumulation and thereby interfered with HCC-related immune responses via the CXCL16-CXCR6 axis.
In 2020, Huang et al. [31] found that several groups of bile acid-associated gut microbes (Bacteroides, Lachnospiracea incertae sedis, and Clostridium XIVa) were related to transcriptome changes in the TME in HBV-related HCC patients, suggesting that bile acids may be important mediators of the communication between the gut microbiota and HCC, but the mechanisms need further study. Furthermore, in 2023, Li et al. [32] found that taurochenodeoxycholic acid and glycochenodeoxycholate were both tightly associated with HCC in their cohort study, indicating the potential diagnostic value of secondary bile acids in HCC.
The liver not only regulates bile acid production and enterohepatic circulation, but also absorbs nutrients from the portal vein and metabolites from the gut microbiota [132], thus regulating lipid and glucose metabolism [133]. The gut microbiota complements the host with additional metabolic functions including the digestion of complex polysaccharides [134, 135] and the production of fatty acids [136, 137], amino acids [138], and vitamins [139]. The gut bacteria have the genetic potential to perform thousands more chemical reactions than humans [140]. SCFAs are metabolites that are controlled by the gut microbiota and have the greatest impact on HCC.
SCFAs
Several studies have found that the gut microbiota in HCC is characterized by a distinctive dysbiosis profile [28]. During HCC development, the gut microbiota supports SCFA production and elicits a T cell immunosuppressive phenotype. SCFAs, which are produced by the anaerobic fermentation of dietary fiber by the gut microbiota, are characteristically altered during the pathogenesis of HCC, and greatly influence tumor immunity.
For example, in a study in 2021, the gut microbiota of NAFLD-HCC patients compared to patients with other liver diseases was characterized by expansion of Proteobacteria at the phylum level, and expansion of Enterobacteriaceae and reduction of Oscillospiraceae and Erysipelotrichaceae at the family level. At the species level, Bacteroides caecimuris (P < 0.0001) and Veillonella parvula (P = 0.002) were significantly enriched in the NAFLD-HCC patients compared to the NAFLD-cirrhosis patients and non-NAFLD controls [28].
Furthermore, genes related to acetate and butyrate/acetylphosphate synthesis were both overexpressed in the NAFLD-HCC patients compared to the others [28]. Accordingly, Oxaloacetate and acetylphosphate, crucial SCFA intermediates, were significantly elevated in the feces of the NAFLD-HCC patients [28]. The feces of the NAFLD-HCC patients had characteristically higher levels of SCFAs such as acetate, butyrate, and formate (P < 0.0001 for all) compared to the NAFLD-cirrhosis patients and non-NAFLD controls. In the serum, the increased SCFAs were butyrate (P = 0.005) and propionate (P = 0.0002) [28]. Based on statistical analysis of patient data, the gut microbes related to NAFLD-HCC seemed to activate the expansion of effector IL-10+ Tregs and restrain the expansion of cytotoxic CD8+ T cells partially via the effects of SCFAs [28].
HCC development and the associated immune response involves the participation of many T cells, and many studies have identified a potential role of SCFAs in mediating the biological effects of the gut microbiota on T-cell immunity [141,142,143]. Dysbiosis leads to the generation of excessive amounts of SCFAs. SCFAs, especially propionate, reduced IL-17 and IL-22 production by intestinal γδ T cells, and thus had the potential to suppress anti-tumor immunology [142]. On the contrary, Butyrate can be used in the tricarboxylic acid cycle (rather than relying on glycolytic input) in CD8+ T cells, so the cells preferentially exhibit oxidative phosphorylation. This increases CD8+ T cell activity and their long-term survival as memory cells, thus theoretically protect anti-tumor immunology [143]. Some SCFAs (under the control of the gut microbiota) have been reported to promote an immunosuppressive response in an anti-inflammatory environment by strongly regulating Tregs and CD8 + T cells in other diseases [143,144,145], suggesting the complex role of these SCFAs in HCC.
Several studies have reported the anti-HCC role of SCFAs. In an HBx (HBV-encoded oncoprotein) transgenic (HBxTg) mouse model fed SCFAs (consisting of the sodium salts of butyrate, propionate, and acetate), HCC foci were reduced and the altered signaling pathways affected by HBx were rescued, including those involving inflammation, phosphatidylinositol 3-kinase, epidermal growth factor, Ras, and NF-κB signaling. SCFAs also dose-dependently reduced HBx-transfected cell viability, suggesting that SCFAs may delay the progression of HBV-HCC, but the detailed mechanisms remain unclear. One of the mechanisms may involve SCFAs downregulating disabled homolog 2 (DAB2) and thus depressing Ras pathway activity [146].
In a mouse model of HCC, Lactobacillus reuteri was markedly reduced, together with decreased SCFAs levels, especially acetate. Further research found that L. reuteri could increase acetate levels, and acetate then reduced the production of IL-17A in hepatic type 3 innate lymphoid cells (ILC3), thus exerting an anti-tumor effect. Moreover, the combination of acetate with PD-1/PD-L1 blockade significantly enhanced antitumor immunity [147]. This implied that SCFAs such as acetate may not only be regulated by the gut microbiota and affect HCC by influencing T cell-associated immune effects, but may also influence HCC treatment by influencing immune checkpoint inhibitors.
Acetate seems to be a double-edged sword in the HCC process, different sources of acetate may have totally opposite effects. Song et al. recently found that acetate generated by Bifidobacterium pseudolongum suppressed NAFLD-HCC in two mouse models and NAFLD-HCC cell lines [148]. B. pseudolongum was the most depleted bacterium in mice with NAFLD-HCC, and B. pseudolongum supplementation significantly suppressed NAFLD-HCC formation. Acetate was verified as the crucial metabolite generated by B. pseudolongum. It bound to G protein-coupled receptor 43 (GPR43) on hepatocytes in the liver. GPR43 activation suppressed the IL-6/JAK1/STAT3 signaling pathway to restrain NAFLD-HCC formation and progression. However, in the same year in mouse models, Zhou et al. found that gut microbiota-derived acetate induced by high dietary fructose upregulated uridine diphospho-N-acetylglucosamine (UDP-GlcNAc) and enhanced protein O-GlcNAcylation in HCC, thus promoting HCC progression [149]. The mechanism involved acetate produced from fructose by the gut microbiota. The acetate served as a major hepatic acetyl-CoA donor [150], which increased glutamine synthesis, leading to higher O-GlcNAcylation in fructose-rich environments. Hyper-O-GlcNAcylation of eukaryotic elongation factor 1A1 (eEF1A1) then promoted cell proliferation and tumor growth [149].
Butyrate has antitumor properties. In HCC patients, the abundance of butyric acid-producing gut bacterial genera was decreased, butyrate metabolism was activated, and plasma butyrate levels were decreased [42]. Butyrate supplementation can not only inhibit HCC proliferation and metastasis, but also improve the anticancer efficacy of sorafenib by regulating intracellular calcium homeostasis [151] or affecting sorafenib-targeted miRNAs [152]. Butyric acid also plays a crucial role in the synergistic anti-HCC effect of peroxisome proliferator-activated receptor (PPAR)-δ and berberine. Berberine suppressed HCC, which was dependent on the binding of PPARδ to the promoters of apoptotic genes such as caspase 3, B-Cell CLL/Lymphoma 2 (BCL2) associated X protein (BAX), and BCL2. Butyric acid enhanced the efficacy of berberine by reducing PPARδ degradation via inhibiting the ubiquitin–proteasome system [153].
As summarized in Fig. 3, gut microbiota derived metabolites usually have two-sided effects on modulating HCC progression.
SCFAs (butyrate, propionate, acetate) downregulate PI3K/NF-κB signaling in HBV-HCC. L. reuteri-derived acetate suppresses IL-17A in ILC3s, exerting anti-tumor effects. Bifidobacterium pseudolongum-derived acetate binds GPR43, inhibiting IL-6/JAK1/STAT3 in NAFLD-HCC. Butyrate synergizes with berberine to stabilize PPARδ, enhancing apoptosis via caspase 3/BAX.
From microenvironmental imbalance to HCC
As indicated above, gut dysbiosis promotes HCC development through multiple mechanisms: altering PRR expression (e.g., TLRs) and downstream signaling, disrupting immune cell function, and inducing gut-liver metabolic dysregulation. These processes drive chronic inflammation, immune microenvironment remodeling, and immune evasion. For example, during NAFLD-cirrhosis-to-HCC progression, dysbiosis-induced SCFA accumulation expands IL-10+ Tregs and suppresses cytotoxic CD8+ T cells, fostering immunosuppression and hepatocarcinogenesis [28].
Enterobacterial dysbiosis alters the intestinal environment and further exacerbates enterobacterial dysbiosis by changing the immune microenvironment, thus creating a vicious cycle. Enterobacteriaceae, including Klebsiella, E. coli, Aspergillus, and Enterobacteriaceae, are among many potential pathogens. An overabundance of Enterobacteriaceae in the gut releases large amounts of LPS, which is positively correlated with upregulated serum IL-6, IL-1, and TNF-a [154]. These pathological changes may exacerbate enterobacterial dysbiosis by increasing transcellular permeability, thus impairing intestinal barrier function [155]. This ultimately exacerbates Enterobacteriaceae, Haemophilus, and Enterococci overgrowth.
Regarding T cells and intestinal bacteria imbalance, gut dysbiosis and metabolic disorders usually lead to an intensely inflammatory environment in the liver [156], involving immune cells such as CD8+ T cells and NKT cells in HCC pathogenesis [157]. For example, during the progression from NASH to HCC, IL-15 induced FOXO1 (Forkhead Box O1) downregulation and CXCR6 upregulation. This made liver-resident CXCR6+ CD8+ T cells susceptible to stimulatory factors (including acetate and extracellular ATP). As a result, CD8+CXCR6+PD1+ T cells were induced to attack both parenchymal and nonparenchymal cells in an antigen-independent manner, and this auto-aggressive process further aggravated liver injury and caused a pro-tumor environment. Moreover, CD8+CXCR6+PD1+ T cells have an exhaustive, hyperactivated, and resident phenotype, and ultimately contribute to HCC pathogenesis [113].
Accumulation of LPS itself can also promote HCC by triggering tumorigenesis [97] and T cell-related immunosuppression [158].
Thus, gut dysbiosis disrupts the equilibrium between pro-tumorigenic pathobionts (e.g., Enterobacteriaceae) and anti-tumorigenic symbionts (e.g., Akkermansia), offering insights into pathogenesis, therapeutic interventions, and biomarker discovery.
Relationship between gut microbiota and intratumoral microbiota of HCC
In recent years, there have been many studies on the intratumoral microbiota. Intratumoral bacteria are predominantly intracellular, mainly colonizing the cytoplasm of both immune cells and tumor cells [159], and the colonization of intratumoral microbiota was considered due to the hypoxic, immunosuppressed, and nutrient-rich TME [160]. While establishing the relationship between gut and intratumoral microbiota in HCC is complex, emerging evidence suggests a potential correlation.
Some intratumoral microbiota are derived from gut microbiota
In HCC, the intratumoral microbes mainly originate from the hepatic blood system, biliary system, and normal adjacent tissues [161]. As mentioned above, gut microbiota dysbiosis and gut permeability are aggravated at the onset of HCC [52]. In this situation, gut microbiota has the chance to get into the circulation via Blood vessels in the intestines mucosa and mesentery, and can even translocate into the liver via the portal circulation [49, 61]. In a Lewis lung cancer mouse model [162], gut-derived A. muciniphila (which was discussed above, exhibiting several anti-HCC effects) was found migrating into the blood circulation and colonizing local lung cancer tissue. In pancreatic cancer, the gut microbiota is closely related to, and can significantly affect, the intratumoral microbiota [163]. Gut microbes can translocate to and colonize pancreatic tumor tissues, and they control the overall intratumoral microbe composition. They alter immune function, ultimately affecting tumor progression and patient survival [78, 164]. These studies all implied that part of the origin of intratumoral microbiota is the gut microbiota, and the gut microbiota has the potential to mediate tumor progression by influencing the intratumoral microbiota. As the primary organ of HCC, the liver is exposed to the gut microbiota via the portal vein and blood from the gut contributes to nearly 70% of the whole liver blood supply [101, 165]. It is thus natural to consider whether the intratumoral bacteria originated from the gut microbiota and had the potential to influence tumor progression by acting with each other.
Microbiota profiles in gut and in HCC tumor tissues seem to be consistent
Unlike in the gut microbiota, Proteobacteria, Actinobacteria, Bacteroidetes, and Firmicutes were the four dominant bacterial phyla (accounting for up to 90% of the bacteria) in both HCC and matched adjacent nontumor tissues, on the basis of different spatial location and microenvironment [166, 167]. Each type of tumor has a distinct intratumoral microbiome compositive feature [159]. HCC presents characteristic intratumoral microbiota profile that differs from other tumors as well [161, 168].
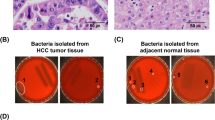
In a study by Sun et al. involving 28 patients with primary liver cancer (including 11 patients with HCC), Pseudomonas was significantly decreased at the genus level (probably due to its antitumor effects) in the tumor tissues compared to the adjacent normal tissues, and Rhizobiaceae at the family level and Agrobacterium at the genus level were significantly increased in the tumor tissues compared to the adjacent normal tissues [167]. In a study by Huang et al. [161] involving 28 normal liver tissues, 64 peritumoral, and 64 HCC tissues. At the phylum level, the HCC tissues had higher levels of Proteobacteria, Firmicutes, and Actinobacteriota, and lower levels of Patescibacteria and Acidobacteriota compared to the normal tissues. At the class level, the HCC tissues were enriched in Gammaproteobacteria, Bacilli, and Actinobacteria compared to the normal tissues. In particular, the abundance of Gammaproteobacteria in HCC tissues was significantly increased compared to the normal tissues. In the study by He et al. [168] involving 99 HCC and adjacent normal tissues. Enterobacteriaceae, Fusobacterium and Neisseria were significantly increased in the HCC tissues compared to the adjacent normal tissues, Pseudomonas was decreased in HCC tissue compared to the norma. Specifically, the proportion of Proteobacteria in HCC was slightly higher and the abundance of Actinobacteriota was significantly lower at the phylum level. As for the genus level, the abundances of the genera Dietzia, Faecalibacterium, Megamonas, Hydrogenophaga, Agathobacter, Chryseobacterium, and Ruminococcaceae were significantly lower, while the abundances of Neisseria, Clostridia_UCG-014, Fusobacterium, and Lactobacillus were significantly higher in the HCC tissues compared to the adjacent normal tissues.
The trends of the same microbiota in gut and in HCC tumor tissues seem to be consistent. In a study by Sun et al. involving 91 HCC patients undergoing hepatectomy, Actinobacteria, which was increased in the gut of HCC patients [30] (related to increased stage and worse prognosis [34]), was notably enriched in HCC tissues [166]. At the phylum level, Proteobacteria [33], Firmicutes [30], Which were significantly increased in the gut of HCC patients, were found to have a higher level in HCC tissue constantly [161]. Enterobacteriaceae, the expansion of which in gut was supposed to belong to a distinctive gut dysbiosis profile of HCC [28], was found increased in the HCC tissues, too [168]. At the genus level, Faecalibacterium [32], Agathobacter [33], and Ruminococcaceae [35], which were significantly decreased in the gut of HCC patients, were found to have significantly lower levels in HCC tissue compared to the adjacent normal tissues [168]. Lactobacillus was significantly increased in both the gut [41] and the HCC tissues [168] compared to the normal controls.
In summary, though HCC presents characteristic microbiota profiles in both gut and HCC tissues which differ from other tumors, the composition and trend of gut and microbiota had much in common (Fig. 1).
Gut microbiota and intratumoral microbiota share the same risk-predicters
Furthermore, there was significant microbial heterogeneity in the intratumoral microbiota between different HCC patients and between multiple tumor foci in the same patient [166]. HCC with different risk factors (with or without HBV, cirrhosis, and so on) or different prognoses also had different intratumoral microbiota [161] (Fig. 4).
For example, Gammaproteobacteria was increased and could secrete cytolethal distending toxin (CDT) and thus cause significant dose-dependent DNA damage which may cause original HCC. Intratumoral microbiota has the potential to intervene in HCC progression by influencing the function of immune cells such as macrophages, T cells and MDSCs. Some downregulated intratumoral microbes might be protective microbes and were significantly positively correlated with some metabolites also decreased in HCC tissues. In lung cancer, gut-derived Akkermansia muciniphila migrated into the blood circulation and colonized local lung cancer tissue and then inhibited tumorigenesis mainly by modulating other intratumoral microbiota and activating lung-resident γδ T cells. In CRC, the intratumoral microbiota pks+ Escherichia and Bacteroides fragilis increased metastasis by destroying the gut–vascular barrier by the stimulation of IL-17 and DNA damage. Increased Fusobacterium nucleatum in CRC cells activated YAP signaling and downregulated the transcription factor forkhead box D3 (FOXD3), which reduced METTL3 transcription. This subsequently reduced the m6A levels of kinesin family member 26B (KIF26B) mRNA and thereby upregulated its expression and inhibited its degradation, which together contributed to CRC metastasis. Improved intratumor microbiota diversity in pancreatic cancer was modulated by the gut microbiota and increased survival due to increased cytotoxic T cells and decreased MDSCs.
For example, Methylobacterium in HCC tissue was associated with poor long-term survival in postoperative HCC patients [166]. At either family or genus level in HCC tissue, intratumoral Pseudomonadaceae exhibited an anti-tumor effect and was linearly associated with prognosis [167]. A high abundance of Fusobacterium in HCC tissue was positively associated with HCC progression [168].
A high level of Proteobacteria in the gut is associated with HCC-MVI [44], gut inflammation and dysbiosis [52], basically pathologic status and poor prognosis. Correspondingly, high level of Proteobacteria in HCC tissues is associated with the elevation of aspartate aminotransferase (AST), alanine aminotransferase (ALT) and TBA levels, which might also indicate a pathophysiological hepatic condition [166]. Loss of Akkermansia in the gut correlates with cellular immunity disorder, liver inflammation and intrahepatic metastasis in HCC, thus poor prognosis [102], lately loss of Akkermansia in HCC tissue was found associated with poor long-term survival in postoperative HCC patients as well [166]. A higher abundance of Enterobacteriaceae in the gut statistically correlates with HCC-MVI [44], higher HCC stage and worse prognosis [34], higher abundance of Enterobacteriaceae in HCC tissue was found related with HCC progression and thus prognosis as well [168]. Although little is known about the crosstalk between the gut microbiota and the intratumoral microbiota, several studies have reported some gut microbiota as HCC risk factors, may play roles in HCC tissue and related to HCC progression and prognosis as well.
Mechanisms by which the gut microbiota affects the intratumoral microbiota in HCC
The influence of the gut microbiota on the intratumoral microbiome is a multifaceted and intricate process involving various mechanisms.
Firstly, as discussed above, the gut-derived A. muciniphila could migrate from the gut and colonize local lung cancer tissue through blood circulation [162], and the gut microbiota can translocate to and colonize pancreatic tumor tissues to control the intratumoral microbiota composition, these facts imply that the gut microbiota has the potential directly colonize the HCC tissue to become and modulate the intratumoral microbiota. Secondly, the gut microbiota contributes to the maintenance of intestinal barrier integrity. Imbalances in the gut microbiota may lead to compromised barrier function, allowing the translocation of bacteria and bacterial products to affect the liver and tumor via the portal venous system [169]. The gut microbiota significantly affects the abundance, distribution and biological role of the intratumoral microbiota by this way. Finally, we have detailed how gut microbiota affects the TME through immune cells [170, 171], metabolites [28, 147], etc., all of which can influence the intratumoral microbiota. The gut microbiota is closely related to the microvascular infiltration [44] and inflammatory microenvironment [45, 49, 61] in tumors, which all play an important role in the growth and reproduction of bacteria in tumor tissues.
Mechanisms by which the intratumoral microbiota affects HCC progression
Regarding the mechanisms by which the intratumoral microbiota affects HCC progression, although the exact mechanisms are not yet fully known, we summarized three possible ways by which the intratumoral microbiota may affect HCC progression, based on existing studies on HCC and other tumors (Fig. 4).
Causing DNA damage
The intratumoral microbiota can cause chronic persistent inflammation by disrupting the mucosal barrier via mechanical stimulation, or by secreting toxins that lead to genetic material damage or mutations, upregulating tumor-associated signaling pathways and thus leading to genotoxicity and inducing malignant transformation of cells. For example, HCC tissue had significantly increased Proteobacteria at the phylum level and significantly increased Gammaproteobacteria at the class level, and the most representative product secreted by Gammaproteobacteria is cytolethal distending toxin (CDT) [172], which is a multimeric protein composed of three subunits, CdtA, CdtB, and CdtC. CdtB causes significant dose-dependent DNA damage [173], and may cause original HCC by this way.
Mediating tumor-related signaling pathways
The abovementioned Streptococcus and Veillonella were high in HCC and increased with HCC progression [28, 33], and they were also involved in the development of lung cancer related signaling pathways [174]. Intratumoral Fusobacterium was increased in HCC [168], and Fusobacterium nucleatum in CRC cells activated YAP signaling and downregulated the transcription factor forkhead box D3 (FOXD3), which reduced methyltransferase like protein (METTL) 3 transcription. This subsequently reduced the m6A levels of kinesin family member 26B (KIF26B) mRNA and thereby upregulated its expression and inhibited its degradation, which together contributed to CRC metastasis [175]. Although there are no studies on their intratumoral effects in HCC, they (or other functionally similar microbes) have the potential to induce HCC progression by mediating signaling pathways.
Directly altering the TME
Intratumoral microbes may infiltrate the TME after being stimulated by oxygen and chemotactic gradients [176], The intratumoral microbiota is not only a key component of the TME, but it can also reprogram tumor metabolism to affect tumor invasion and metastasis.
In particular, the intratumoral microbiota affects the immune cells in the TME to influence tumorigenesis and cancer treatment. Intratumor microbes affected the immune checkpoint proteins: in several tumors, fatty acid synthase 2 (fap2) expressed by Fusobacterium nucleatum could directly bind to the checkpoint protein TIGIT and thereby inhibit the anti-tumor activity of human NK and T cells [170]. In CRC, enterotoxigenic Bacteroides fragilis triggered colon tumorigenesis based on the generation of pro-tumoral MDSCs [177]. In pancreatic tumors, anaerobic bacteria such as Bacteroides, Lactobacillus, and Peptoniphilus may shorten survival time by decreasing the number of tumor-infiltrating T cells [171].
Intratumoral microbiota has the potential to intervene in HCC progression by influencing the function of immune cells such as macrophages, T cells and MDSCs. In 2023, Li et al. [178] analyzed 70 samples, including 29 paired tumor and nontumor tissues from patients with HBV-HCC and 12 liver tissues from patients with chronic hepatitis B (CHB). They established two HCC subtypes based on different intra-tissue microbiota phenotypes and heterogeneity features, namely bacteria- and virus-dominant subtypes, which exhibited distinct clinical manifestations. Patients with bacteria-dominant HCC had larger and more invasive tumors, and worse survival, compared to those with virus-dominant HCC. There was increased M2-type macrophage infiltration in bacteria-dominant HCC compared to virus-dominant tumor HCC. Some risk factors like HBV may result in a unique microenvironment that favors the distinct microbiota colonization, which increases the recruitment and infiltration of CD8 + T cells, monocytic MDSCs (mMDSCs) and polymorphonuclear MDSCs (pmnMDSCs) in HBV-HCC, and finally accelerated the disease progression via inhibiting host antitumor immunity [165].
The close association has been found between different intratumoral microbiota and metabolites in HCC, although the exact mechanism is unclear. In a study analyzing HCC tissues in mice [179], the Kyoto Encyclopedia of Genes and Genomes analysis found that the intratumoral microbial gene’s functions were markedly enriched in the lysosome, glycosaminoglycan degradation, favone and favonol biosynthesis and autophagy yeast than in normal tissues. The Clusters of Orthologous Groups of proteins (COG) functional analysis found that the intratumoral microbial gene’s functions were markedly enriched in glycerol-3-phosphate transport, Fe3+-siderophore transport, Sugar (pentulose or hexulose) kinase and Fermentation-respiration switch esterase (FrsA) than in normal tissues. In HCC tissue compared to the normal, the most upregulated metabolites include docosatrienoic acid, FAHFA, L-palmitoylcarnitine, androsterone, citrulline, adrenic acid, myristic acid and so on, the most downregulated metabolites include lactobionic acid, feruloyl putrescine, 6-phosphogluconic acid, S-(methyl) glutathione, thromboxane B1, cholic acid, stercobilin and so on. Furthermore, in the analysis investigating the association between the top 20 diferrential metabolites and the top 10 diferrential intratumoral bacteria, top abundant intratumoral bacteria Allobacillus sp SKP4 8 and Ralstonia sp UNC404CL21Col showed significant positive correlations with most metabolites, including citrulline, cytidine 5′-monophosphate (hydrate), indole-3-lactic acid, 2′-O-methylguanosine, cytidine5′-monophosphate, L-(+)-Citrulline, cis-4-HydroxyD-proline, and myristic Acid, while showed significant negative correlations with a-Lactose and N-acetyl-Dglucosamine. However, the top abundant normal-tissue bacteria Pseudomonas koreensis and Pseudomonas psychrotolerans were in negative correlation with most metabolites, and the trend was opposite to the Allobacillus sp SKP4 8 and Ralstonia sp UNC404CL21Col. Some downregulated intratumoral microbes might be protective microbes and were significantly positively correlated with some metabolites also decreased in HCC tissues, and they may be involved in the synthetic and metabolic processes of some protective compound metabolites [180].
Modulating HCC metastasis
The intratumoral microbiota plays an important role in metastasis. Intravenous antibiotics selectively inhibit the intratumoral (not gut) bacteria, while oral antibiotics deplete both types of bacteria. In a mouse breast cancer model, intravenous antibiotics decreased metastasis while not affecting the primary lesion, while oral antibiotics decreased both metastasis and primary lesion formation, hinting at the key role of the intratumoral microbiota in metastasis [181]. In HCC, the situation is more complicated. The liver is exposed to gut microbiota metabolites and products carried by the blood, as 70% of the whole liver blood supply is from the gut [101]. In many mouse models, oral antibiotics had liver-selective antitumor effects by restraining the gut microbiota that specifically influenced intrahepatic tumors. These mouse models included the spontaneous HCC transgenic model, the subcutaneous implantation model (liver metastases were reduced but not the primary foci), and the intrasplenic tumor injection model (liver metastases were reduced, while lung metastases were increased by tumor cell tail vein injection in a different model). The liver-selective antitumor effects may partly be the result of the gut microbiota using bile acids to control NKT cell infiltration in the liver [101].
Additionally, tumor-derived exosomes can transfer miRNAs and proteins and promote tumor metastasis through multiple mechanisms, such as remodeling TME, promoting EMT and inhibiting the antitumor immune response [182,183,184]. Tumor cells infected by bacteria may secrete more exosomes, thus accelerating the metastasis of the tumor [185, 186].
There may also be a synergistic effect of gut flora and intratumor flora in promoting tumor metastasis, because bacteria of the same genus tend to act accordingly in tumor metastatic progress whether in the gut or in tumor cells. Fusobacterium nucleatum in gut inhibited the anti-tumor activity of human NK cells and T cells [170], in tumour cells it increased the mobility of these cells mobility, rendered them more resistant to stress in the circulation, and finally promoted tumour metastasis [187].
Other anti-tumor effects
Intratumoral microbiota could protect tumor cells from fluid shear stress during cell migration [188]. In the research of intratumoral microbiota in a murine spontaneous breast cancer model, intratumor bacteria colonized in circulating tumor cells were found to defending the fluid shear stress by reorganizing actin cytoskeleton resulted in metastasis process [181]. S. xylosus, L. animalis, and S. cuniculi could increase the survival of breast cancer cells in the lung from 3.4 to 6.4 fold [181], none of them were reported in HCC to take a significant role in tumor cells. This field is still relatively new and needs to be explored how specific bacteria affect what specific tumour type metastates to specific organs.
It is clear that intratumoral microbiota are not exclusively pro-tumor, they can activate a bacterial antigen-specific response, which can be used not only to amplify the immune response to tumor antigens, thus increase the killing power of the tumor [188]. Briefly, bacteria could destroy tumor cells after targeting and localizing them and then release tumor-associated antigen and damage-associated molecular pattern to recruit or activate immune cells [189]. For example, in melanoma, researchers found that some microbial antigens were homologous to tumor antigens and thus they share similar antigenic epitopes [190]. Subsequently, the tail length tape measure protein of the bacteriophage Enterococcus hirae, and SVYRYYGL (SVY) epitope on the Bifidobacterium breve was similar to the tumor antigen and might cross-react, promoting T-cell responses [191]. It is of great potential in tumor therapy if we improve the tumor microenvironment by inhibiting pro-tumor intratumoral microbiota and stimulating tumor immune response by increasing some special intratumoral bacterial epitopes.
In summary, this review discussed the role of gut microbiota in the HCC progression, the relationship between gut microbiota and intratumoral microbiota and their interaction in HCC. Both the gut and intratumoral microbiota have a two-sided role in HCC progression, and it is of great potential in tumor therapy if we inhibit pro-tumor microbiota and stimulate tumor immune response by increasing anti-tumor microbiota.
Discussion
The mechanisms by which gut dysbiosis leads to the progression and metastasis of many tumors, including HCC, have been studied for many years. The liver absorbs nutrients from the portal vein, and the liver also receives metabolites from the gut microbiota via the gut–liver axis [132]. The gut–liver axis is the main pathway through which the gut microbiota influences the development of liver disease [132]. The main components of this axis are (1) a mucus layer containing commensal microorganisms, secreted IgA, and antimicrobial peptides; (2) a layer of intestinal epithelial cells with tight junctions between neighboring cells; and (3) a lamina propria with a resident population of innate and adaptive immune cells [192]. The gut microbiota influences HCC mainly by modulating bile acid metabolism, affecting nutrient metabolism, and altering levels of metabolic products.
Importantly, most of the gut microbiota are nonharmful. In a balanced state or under external conditions, the gut microbiota, and various biomolecules in the internal environment often interact with each other and exert synergistic anti-tumor effects. For example, PPARs are a family of transcription factors that govern essential metabolic activities. One of the members, PPARδ, plays a critical role in the antitumor effect of butyrate and berberine. Berberine increased BAX, cleaved caspase 3, and decreased BCL2 expression to suppress HCC development dependent on PPARδ. On the other hand, berberine activated the PPARδ transcriptional function to facilitate the binding of PPARδ to the promoters of apoptotic genes such as caspase 3, BAX, and BCL2. Moreover, berberine restored the dysregulated gut microbiota induced by the liver tumor burden, rescuing the level of the gut microbial metabolite butyric acid. Butyric acid in return enhanced the efficacy of berberine by reducing PPARδ degradation via inhibiting the ubiquitin–proteasome system [153]. As the important link in the middle, the balance of the gut microbiota is crucial to disease progression, and disruption of the balanced gut microbiota can strongly destroy the overall anti-tumor effect, and even produce a tumor-promoting microenvironment.
Metabolites, such as SCFAs, are double-edged in HCC as well. For example, in NAFLD-HCC, the gut microbiota induced high levels of SCFAs such as butyrate, which was correlated with increased IL-10+ Tregs but decreased CD8+ cells [28], seemingly not consistent with its anti-HCC effect. In another example, acetate induced by various factors exerted different effects on HCC, which has been mentioned above [148, 149]. The paradox of the tumor-promoting or tumor-suppressing functions of SCFAs suggests that to accurately elucidate the functions of microbial metabolites, it is important not to lose sight of the environments in which the metabolites function, as well as the different types and concentrations of the metabolites. For example, when concentrations of SCFAs are within their normal physiologic ranges, they significantly inhibit the development of colon cancer. Increasing the dose of SCFAs beyond the tolerance threshold promotes tumor progression, and the same mechanism and principle may exist in HCC, waiting to be explored and investigated [193, 194].
Although little is known about the crosstalk between the gut microbiota and the intratumoral microbiota, several studies have reported on the biological functions of the gut microbiota, via effects on the intratumoral microbiota, in various cancers.
In a Lewis lung cancer mouse model [162], gut-derived A. muciniphila (which was discussed above, exhibiting several anti-HCC effects) migrated into the blood circulation and colonized local lung cancer tissue. A. muciniphila then inhibited tumorigenesis partly by modulating the tumoral symbiotic microbiota. A higher level of gut A. muciniphila (due to gavage) increased the abundance of intratumoral Akkermansia, Lactobacillus, Bifidobacterium, Staphylococcus, and Bacteroides, and these symbiotic bacteria likely played an inhibitory role in glutamine (Gln) and adenosine metabolism, thus helping to block local tumor progression in the lungs. Alterations in the lung intratumoral microbiota can influence lung cancer progression via many routes. The lung cancer microbiota may activate lung-resident γδ T cells to increase inflammation associated with lung adenocarcinoma. In detail, the microbes may stimulate MyD88-dependent myeloid cells to produce IL-1β and IL-23, activating Vγ6+ Vδ1+ γδT cells to produce factors such as IL-17, leading to inflammation and tumor cell proliferation [195]. Some intratumoral microbes in squamous cell carcinoma caused epithelial TP53 mutations [196]. Thus, the gut microbiota significantly alters the intratumoral microbiota in lung cancer, and the intratumoral microbiota influences lung cancer progression Through a variety of means including glutamine (Gln) and adenosine metabolism, γδ T cells, interleukin and TP53. Furthermore, the roles of the intratumoral microbiota are more complicated than “pro-tumor” v.s. “anti-tumor”. In the Lewis lung cancer mouse model, Staphylococcus and Lactobacillus, which may block local tumor progression at the primary tumor site [162], were reported to colonize tumor cells that migrated from the primary site to metastatic foci and thereby significantly increased the number of metastatic foci in a spontaneous breast tumor model, and they did not influence the primary site [181].
As for colorectal cancer (CRC), there were significant differences in the intratumoral microbiota between tissues with and without KRAS mutation or microsatellite instability (two key factors underlying CRC progression and prognosis). This indicates the close associations of intratumoral microbial heterogeneity with genetic alteration and CRC development [197]. When CRC cells began to metastasize, the intratumoral microbiota increased metastasis by destroying the gut–vascular barrier and building a bacterial premetastatic niche in the liver [198]. The mechanism involves increased genotoxic pks+ E. coli-encoded colibactin-synthesizing enzyme levels that promote CRC metastasis [199]. This may be driven by Bacteroides fragilis, as colibactin lead to increased IL-17 and DNA damage in colonic tissue and worsens prognosis [200]. E. coli in CRC disrupted the gut–vascular barrier reached the liver via the blood and then facilitated liver metastasis [201].
Improved intratumor microbiota diversity in pancreatic cancer was modulated by the gut microbiota and increased survival due to increased cytotoxic T cells and decreased MDSCs [163]. Increased Pseudoxanthomonas, Streptomyces, Saccharopolyspora, and Bacillus clausii in pancreatic tumor tissue predicted better survival [163], while anaerobic bacteria (such as Bacteroides, Lactobacillus, and Peptoniphilus) were significantly positively associated with shorter survival time [171]. Regarding the potential mechanism in pancreatic cancer, increases in the genera Acinetobacter, Pseudomonas, and Sphingopyxis, were positively correlated with DNA replication and oncogenic factors including K-ras signaling, EMT, and MAPK signaling, while being negatively correlated with bile acid metabolism, pancreatic beta cells, and pancreatic secretion [202].
These studies may provide us with ideas to explore how gut microbiota interacts with intratumor microbiota and together affects tumor progression. This can help us understand more deeply the correlation between intratumoral microbiota and gut microbiota, as well as help us to further explore the possible mechanisms of the intratumoral microbiota modulating other types of tumors like HCC. Many of the possible mechanisms that how intratumoral microbiota improve HCC progression that we summarized in the previous section are based on these studies.
Intratumoral microbiota also has two sides on tumors, some of the intratumoral microbiota can inhibit tumor progression as well. Some microbial antigens were homologous to tumor antigens [190], thus can stimulate anti-tumor immune reactions [191]. It is of great potential in tumor therapy if we improve the tumor microenvironment by inhibiting pro-tumor intratumoral microbiota and stimulating tumor immune response by increasing some special intratumoral bacterial epitopes.
Both the gut and intratumoral microbiota have a two-sided role in HCC progression, fully understanding and mastering the complex biological roles of these microbiota will provide a theoretical foundation for the potential clinical application of gut and intratumoral microbiota in the treatment of HCC.
The gut microbiota plays a significant role not only in the initiation and progression of HCC but also exerts a substantial influence on its treatment through these biological mechanisms. For example, the treatment options for HCC patients including liver surgical resection, percutaneous ablation, liver transplantation, radiation, as well as trans-arterial and systemic therapies, the clinical decision making based on the patient’s tumor stage, liver function, and performance status. Above these therapies, nowadays trials aim to address the efficacy of immunotherapy plus targeted therapy or not as adjuvant or neo-adjuvant treatment, with initial promising results from phase 2 trials [203,204,205] and phase 3 trials [206]. To the advanced unresectable HCC, immunotherapy and targeted therapy are supposed to be the main treatment [207, 208]. The role of gut microbiota and its metabolites in modulating local and systemic immune responses, thereby impacting the cancer-immune axis and influencing the efficacy of immunotherapy for HCC, is emerging as a topic of significant interest in the field [209, 210]. Based on these facts, the significant therapeutic role of the gut microbiota in HCC warrants further in-depth investigation and exploration.
References
Llovet JM, Kelley RK, Villanueva A, Singal AG, Pikarsky E, Roayaie S, et al. Hepatocellular carcinoma. Nat Rev Dis Prim. 2021;7:6.
Vogel A, Meyer T, Sapisochin G, Salem R, Saborowski A. Hepatocellular carcinoma. Lancet. 2022;400:1345–62.
Hofmann AF. Chemistry and enterohepatic circulation of bile acids. Hepatology. 1984;4:4S–14S.
Guichard C, Amaddeo G, Imbeaud S, Ladeiro Y, Pelletier L, Maad IB, et al. Integrated analysis of somatic mutations and focal copy-number changes identifies key genes and pathways in hepatocellular carcinoma. Nat Genet. 2012;44:694–8.
Totoki Y, Tatsuno K, Covington KR, Ueda H, Creighton CJ, Kato M, et al. Trans-ancestry mutational landscape of hepatocellular carcinoma genomes. Nat Genet. 2014;46:1267–73.
Donne R, Lujambio A. The liver cancer immune microenvironment: therapeutic implications for hepatocellular carcinoma. Hepatology. 2023;77:1773–96.
Liu X, Li J, Wang Q, Bai L, Xing J, Hu X, et al. Analysis on heterogeneity of hepatocellular carcinoma immune cells and a molecular risk model by integration of scRNA-seq and bulk RNA-seq. Front Immunol. 2022;13:1012303.
Cai LY, Chen SJ, Xiao SH, Sun QJ, Ding CH, Zheng BN, et al. Targeting p300/CBP attenuates hepatocellular carcinoma progression through epigenetic regulation of metabolism. Cancer Res. 2021;81:860–72.
Hu B, Yu M, Ma X, Sun J, Liu C, Wang C, et al. IFNα potentiates Anti-PD-1 efficacy by remodeling glucose metabolism in the hepatocellular carcinoma microenvironment. Cancer Discov. 2022;12:1718–41.
Cai J, Chen T, Jiang Z, Yan J, Ye Z, Ruan Y, et al. Bulk and single-cell transcriptome profiling reveal extracellular matrix mechanical regulation of lipid metabolism reprograming through YAP/TEAD4/ACADL axis in hepatocellular carcinoma. Int J Biol Sci. 2023;19:2114–31.
Sun J, Ding J, Shen Q, Wang X, Wang M, Huang Y, et al. Decreased propionyl-CoA metabolism facilitates metabolic reprogramming and promotes hepatocellular carcinoma. J Hepatol. 2023;78:627–42.
Xia P, Zhang H, Lu H, Xu K, Jiang X, Jiang Y, et al. METTL5 stabilizes c-Myc by facilitating USP5 translation to reprogram glucose metabolism and promote hepatocellular carcinoma progression. Cancer Commun. 2023;43:338–64.
Consortium HMP. Structure, function and diversity of the healthy human microbiome. Nature. 2012;486:207–14.
Leviatan S, Shoer S, Rothschild D, Gorodetski M, Segal E. An expanded reference map of the human gut microbiome reveals hundreds of previously unknown species. Nat Commun. 2022;13:3863.
Sommer F, Bäckhed F. The gut microbiota–masters of host development and physiology. Nat Rev Microbiol. 2013;11:227–38.
Quan Y, Zhang KX, Zhang HY. The gut microbiota links disease to human genome evolution. Trends Genet. 2023;39:451–61.
Eckburg PB, Bik EM, Bernstein CN, Purdom E, Dethlefsen L, Sargent M, et al. Diversity of the human intestinal microbial flora. Science. 2005;308:1635–8.
Li M, Wang S, Li Y, Zhao M, Kuang J, Liang D, et al. Gut microbiota-bile acid crosstalk contributes to the rebound weight gain after calorie restriction in mice. Nat Commun. 2022;13:2060.
Van Hul M, Cani PD. The gut microbiota in obesity and weight management: microbes as friends or foe? Nat Rev Endocrinol. 2023;19:258–71.
Tremaroli V, Bäckhed F. Functional interactions between the gut microbiota and host metabolism. Nature. 2012;489:242–9.
Cani PD. Metabolism in 2013: the gut microbiota manages host metabolism. Nat Rev Endocrinol. 2014;10:74–76.
Geach T. Gut microbiota: mucin-munching bacteria modulate glucose metabolism. Nat Rev Endocrinol. 2017;13:66.
Altay O, Nielsen J, Uhlen M, Boren J, Mardinoglu A. Systems biology perspective for studying the gut microbiota in human physiology and liver diseases. EBioMedicine. 2019;49:364–73.
White LS, Van den Bogaerde J, Kamm M. The gut microbiota: cause and cure of gut diseases. Med J Aust. 2018;209:312–7.
Forbes JD, Chen CY, Knox NC, Marrie RA, El-Gabalawy H, de Kievit T, et al. A comparative study of the gut microbiota in immune-mediated inflammatory diseases-does a common dysbiosis exist? Microbiome. 2018;6:221.
Wei S, Bahl MI, Baunwall SMD, Hvas CL, Licht TR. Determining gut microbial dysbiosis: a review of applied indexes for assessment of intestinal microbiota imbalances. Appl Environ Microbiol. 2021;87:e00395–21.
Srivastava S, Singh A, Sandeep K, Yadav D. Epigenetic regulation of gut microbial dysbiosis. Indian J Microbiol. 2021;61:125–9.
Behary J, Amorim N, Jiang XT, Raposo A, Gong L, McGovern E, et al. Gut microbiota impact on the peripheral immune response in non-alcoholic fatty liver disease related hepatocellular carcinoma. Nat Commun. 2021;12:187.
Zheng R, Wang G, Pang Z, Ran N, Gu Y, Guan X, et al. Liver cirrhosis contributes to the disorder of gut microbiota in patients with hepatocellular carcinoma. Cancer Med. 2020;9:4232–50.
Xie G, Wang X, Huang F, Zhao A, Chen W, Yan J, et al. Dysregulated hepatic bile acids collaboratively promote liver carcinogenesis. Int J Cancer. 2016;139:1764–75.
Huang H, Ren Z, Gao X, Hu X, Zhou Y, Jiang J, et al. Integrated analysis of microbiome and host transcriptome reveals correlations between gut microbiota and clinical outcomes in HBV-related hepatocellular carcinoma. Genome Med. 2020;12:102.
Li X, Yi Y, Wu T, Chen N, Gu X, Xiang L, et al. Integrated microbiome and metabolome analysis reveals the interaction between intestinal flora and serum metabolites as potential biomarkers in hepatocellular carcinoma patients. Front Cell Infect Microbiol. 2023;13:1170748.
Yang J, He Q, Lu F, Chen K, Ni Z, Wang H, et al. A distinct microbiota signature precedes the clinical diagnosis of hepatocellular carcinoma. Gut Microbes. 2023;15:2201159.
Zhang N, Gou Y, Liang S, Chen N, Liu Y, He Q, et al. Dysbiosis of gut microbiota promotes hepatocellular carcinoma progression by regulating the immune response. J Immunol Res. 2021;2021:4973589.
Ponziani FR, Bhoori S, Castelli C, Putignani L, Rivoltini L, Del Chierico F, et al. Hepatocellular carcinoma is associated with gut microbiota profile and inflammation in nonalcoholic fatty liver disease. Hepatology. 2019;69:107–20.
Zhang L, Wu YN, Chen T, Ren CH, Li X, Liu GX. Relationship between intestinal microbial dysbiosis and primary liver cancer. Hepatobiliary Pancreat Dis Int. 2019;18:149–57.
Kang Y, Cai Y, Yang Y. The gut microbiome and hepatocellular carcinoma: implications for early diagnostic biomarkers and novel therapies. Liver Cancer. 2022;11:113–25.
Aymeric L, Donnadieu F, Mulet C, du Merle L, Nigro G, Saffarian A, et al. Colorectal cancer specific conditions promote Streptococcus gallolyticus gut colonization. Proc Natl Acad Sci USA. 2018;115:E283–E291.
Yang N, Xu J, Wang X, Chen N, Su L, Liu Y. The spatial landscape of the bacterial community and bile acids in the digestive tract of patients with bile reflux. Front Microbiol. 2022;13:835310.
Yan H, Wei W, Hu L, Zhang Y, Zhang H, Liu J. Reduced feeding frequency improves feed efficiency associated with altered fecal microbiota and bile acid composition in pigs. Front Microbiol. 2021;12:761210.
Zhang HL, Yu LX, Yang W, Tang L, Lin Y, Wu H, et al. Profound impact of gut homeostasis on chemically-induced pro-tumorigenic inflammation and hepatocarcinogenesis in rats. J Hepatol. 2012;57:803–12.
Ren Z, Li A, Jiang J, Zhou L, Yu Z, Lu H, et al. Gut microbiome analysis as a tool towards targeted non-invasive biomarkers for early hepatocellular carcinoma. Gut. 2019;68:1014–23.
Xu W, Jiang Y, Tao J, Liu Y, Xia Y, Chen C, et al. Correlation analysis for alterations of intestinal flora in hepatocellular carcinoma patients: combinatorial detection of Coriobacterium, Atopobium, Coprococcus and Veillonella dispar may be a new method for HCC diagnosis. J Med Microbiol. 2023;72. https://doi.org/10.1099/jmm.0.001713
Zhang N, Wang Z, Lv J, Zhang S, Liu Y, Liu T, et al. Characterization of gut microbiota and exploration of potential predictive model for hepatocellular carcinoma microvascular invasion. Front Med. 2022;9:836369.
Ni J, Huang R, Zhou H, Xu X, Li Y, Cao P, et al. Analysis of the relationship between the degree of dysbiosis in gut microbiota and prognosis at different stages of primary hepatocellular carcinoma. Front Microbiol. 2019;10:1458.
Spadoni I, Zagato E, Bertocchi A, Paolinelli R, Hot E, Di Sabatino A, et al. A gut-vascular barrier controls the systemic dissemination of bacteria. Science. 2015;350:830–4.
Johansson ME, Phillipson M, Petersson J, Velcich A, Holm L, Hansson GC. The inner of the two Muc2 mucin-dependent mucus layers in colon is devoid of bacteria. Proc Natl Acad Sci USA. 2008;105:15064–9.
Wang L, Fouts DE, Stärkel P, Hartmann P, Chen P, Llorente C, et al. Intestinal REG3 lectins protect against alcoholic steatohepatitis by reducing mucosa-associated microbiota and preventing bacterial translocation. Cell Host Microbe. 2016;19:227–39.
Anand S, Mande SS. Host-microbiome interactions: gut-liver axis and its connection with other organs. NPJ Biofilms Microbiomes. 2022;8:89.
Meroni M, Longo M, Dongiovanni P. Alcohol or gut microbiota: who is the guilty? Int J Mol Sci. 2019;20:4568.
Portincasa P, Bonfrate L, Khalil M, Angelis M, Calabrese FM, D’Amato M, et al. Intestinal barrier and permeability in health, obesity and NAFLD. Biomedicines. 2021;10:83.
Zhao C, Hu X, Bao L, Wu K, Zhao Y, Xiang K, et al. Gut dysbiosis induces the development of mastitis through a reduction in host anti-inflammatory enzyme activity by endotoxemia. Microbiome. 2022;10:205.
Johansson ME. Fast renewal of the distal colonic mucus layers by the surface goblet cells as measured by in vivo labeling of mucin glycoproteins. PLoS ONE. 2012;7:e41009.
Salguero MV, Al-Obaide MAI, Singh R, Siepmann T, Vasylyeva TL. Dysbiosis of Gram-negative gut microbiota and the associated serum lipopolysaccharide exacerbates inflammation in type 2 diabetic patients with chronic kidney disease. Exp Ther Med. 2019;18:3461–9.
Kiouptsi K, Pontarollo G, Reinhardt C. Gut Microbiota and the microvasculature. Cold Spring Harb Perspect Med. 2023;13:a041179.
Jadhav K, Cohen TS. Can you trust your gut? implicating a disrupted intestinal microbiome in the progression of NAFLD/NASH. Front Endocrinol. 2020;11:592157.
Liu MJ, Yang JY, Yan ZH, Hu S, Li JQ, Xu ZX, et al. Recent findings in Akkermansia muciniphila-regulated metabolism and its role in intestinal diseases. Clin Nutr. 2022;41:2333–44.
Liu Q, Yu Z, Tian F, Zhao J, Zhang H, Zhai Q, et al. Surface components and metabolites of probiotics for regulation of intestinal epithelial barrier. Microb Cell Fact. 2020;19:23.
Plovier H, Everard A, Druart C, Depommier C, Van Hul M, Geurts L, et al. A purified membrane protein from Akkermansia muciniphila or the pasteurized bacterium improves metabolism in obese and diabetic mice. Nat Med. 2017;23:107–13.
Lange NF, Radu P, Dufour JF. Prevention of NAFLD-associated HCC: role of lifestyle and chemoprevention. J Hepatol. 2021;75:1217–27.
Miele L, Valenza V, La Torre G, Montalto M, Cammarota G, Ricci R. et al. Increased intestinal permeability and tight junction alterations in nonalcoholic fatty liver disease. Hepatology. 2009;49:1877–87.
Ciesielska A, Matyjek M, Kwiatkowska K. TLR4 and CD14 trafficking and its influence on LPS-induced pro-inflammatory signaling. Cell Mol Life Sci. 2021;78:1233–61.
Heine H, Zamyatina A. Therapeutic targeting of TLR4 for inflammation, infection, and cancer: a perspective for disaccharide lipid A mimetics. Pharmaceuticals. 2022;16:23
Chen C, Wang Z, Ding Y, Qin Y. Tumor microenvironment-mediated immune evasion in hepatocellular carcinoma. Front Immunol. 2023;14:1133308.
Zhang C, Wang N, Tan HY, Guo W, Chen F, Zhong Z, et al. Direct inhibition of the TLR4/MyD88 pathway by geniposide suppresses HIF-1α-independent VEGF expression and angiogenesis in hepatocellular carcinoma. Br J Pharmacol. 2020;177:3240–57.
Liu WT, Jing YY, Yu GF, Han ZP, Yu DD, Fan QM, et al. Toll like receptor 4 facilitates invasion and migration as a cancer stem cell marker in hepatocellular carcinoma. Cancer Lett. 2015;358:136–43.
Wei X, Liu H, Li X, Liu X. Over-expression of MiR-122 promotes apoptosis of hepatocellular carcinoma via targeting TLR4. Ann Hepatol. 2019;18:869–78.
Dapito DH, Mencin A, Gwak GY, Pradere JP, Jang MK, Mederacke I, et al. Promotion of hepatocellular carcinoma by the intestinal microbiota and TLR4. Cancer cell. 2012;21:504–16.
Chen T, Li Q, Wu J, Wu Y, Peng W, Li H, et al. Fusobacterium nucleatum promotes M2 polarization of macrophages in the microenvironment of colorectal tumours via a TLR4-dependent mechanism. Cancer Immunol Immunother. 2018;67:1635–46.
Shi G, Wang C, Zhang P, Ji L, Xu S, Tan X, et al. Donor polymorphisms of toll-like receptor 4 rs1927914 associated with the risk of hepatocellular carcinoma recurrence following liver transplantation. Arch Med Res. 2017;48:553–60.
Eiró N, Altadill A, Juárez LM, Rodríguez M, González LO, Atienza S, et al. Toll-like receptors 3, 4 and 9 in hepatocellular carcinoma: Relationship with clinicopathological characteristics and prognosis. Hepatol Res. 2014;44:769–78.
Zhou S, Du R, Wang Z, Shen W, Gao R, Jiang S, et al. TLR4 increases the stemness and is highly expressed in relapsed human hepatocellular carcinoma. Cancer Med. 2019;8:2325–37.
Liu WT, Jing YY, Gao L, Li R, Yang X, Pan XR, et al. Lipopolysaccharide induces the differentiation of hepatic progenitor cells into myofibroblasts constitutes the hepatocarcinogenesis-associated microenvironment. Cell Death Differ. 2020;27:85–101.
Li H, Li Y, Liu D, Liu J. LPS promotes epithelial-mesenchymal transition and activation of TLR4/JNK signaling. Tumour Biol. 2014;35:10429–35.
Yang J, Zhang JX, Wang H, Wang GL, Hu QG, Zheng QC. Hepatocellular carcinoma and macrophage interaction induced tumor immunosuppression via Treg requires TLR4 signaling. World J Gastroenterol. 2012;18:2938–47.
Liu Y, Zhang X, Chen S, Wang J, Yu S, Li Y, et al. Gut-derived lipopolysaccharide promotes alcoholic hepatosteatosis and subsequent hepatocellular carcinoma by stimulating neutrophil extracellular traps through toll-like receptor 4. Clin Mol Hepatol. 2022;28:522–39.
Yang LY, Luo Q, Lu L, Zhu WW, Sun HT, Wei R, et al. Increased neutrophil extracellular traps promote metastasis potential of hepatocellular carcinoma via provoking tumorous inflammatory response. J Hematol Oncol. 2020;13:3.
Shen R, Ke L, Li Q, Dang X, Shen S, Shen J, et al. Abnormal bile acid-microbiota crosstalk promotes the development of hepatocellular carcinoma. Hepatol Int. 2022;16:396–411.
Quail DF, Joyce JA. Microenvironmental regulation of tumor progression and metastasis. Nat Med. 2013;19:1423–37.
Yang JD, Nakamura I, Roberts LR. The tumor microenvironment in hepatocellular carcinoma: current status and therapeutic targets. Semin Cancer Biol. 2011;21:35–43.
Llovet JM, Willoughby CE, Singal AG, Greten TF, Heikenwälder M, El-Serag HB, et al. Nonalcoholic steatohepatitis-related hepatocellular carcinoma: pathogenesis and treatment. Nat Rev Gastroenterol Hepatol. 2023;20:487–503.
Ringelhan M, Pfister D, O’Connor T, Pikarsky E, Heikenwalder M. The immunology of hepatocellular carcinoma. Nat Immunol. 2018;19:222–32.
Ezhilarasan D, Najimi M. Deciphering the possible reciprocal loop between hepatic stellate cells and cancer cells in the tumor microenvironment of the liver. Crit Rev Oncol Hematol. 2023;182:103902.
Dhar D, Baglieri J, Kisseleva T, Brenner DA. Mechanisms of liver fibrosis and its role in liver cancer. Exp Biol Med. 2020;245:96–108.
Arvanitakis K, Mitroulis I, Germanidis G. Tumor-associated neutrophils in hepatocellular carcinoma pathogenesis, prognosis, and therapy. Cancers. 2021;13:2899.
Zhou SL, Zhou ZJ, Hu ZQ, Huang XW, Wang Z, Chen EB, et al. Tumor-associated neutrophils recruit macrophages and T-regulatory cells to promote progression of hepatocellular carcinoma and resistance to sorafenib. Gastroenterology. 2016;150:1646–58.e1617.
Tacke F. Targeting hepatic macrophages to treat liver diseases. J Hepatol. 2017;66:1300–12.
Wang C, Ma C, Gong L, Guo Y, Fu K, Zhang Y, et al. Macrophage polarization and its role in liver disease. Front Immunol. 2021;12:803037.
Jiao Y, Zhang T, Zhang C, Ji H, Tong X, Xia R, et al. Exosomal miR-30d-5p of neutrophils induces M1 macrophage polarization and primes macrophage pyroptosis in sepsis-related acute lung injury. Crit Care. 2021;25:356.
Gunassekaran GR, Poongkavithai Vadevoo SM, Baek MC, Lee B. M1 macrophage exosomes engineered to foster M1 polarization and target the IL-4 receptor inhibit tumor growth by reprogramming tumor-associated macrophages into M1-like macrophages. Biomaterials. 2021;278:121137.
Locati M, Curtale G, Mantovani A. Diversity, mechanisms, and significance of macrophage plasticity. Annu Rev Pathol. 2020;15:123–47.
Mantovani A, Biswas SK, Galdiero MR, Sica A, Locati M. Macrophage plasticity and polarization in tissue repair and remodelling. J Pathol. 2013;229:176–85.
Zuo W, Sun R, Ji Z, Ma G. Macrophage-driven cardiac inflammation and healing: insights from homeostasis and myocardial infarction. Cell Mol Biol Lett. 2023;28:81.
Mantovani A, Sozzani S, Locati M, Allavena P, Sica A. Macrophage polarization: tumor-associated macrophages as a paradigm for polarized M2 mononuclear phagocytes. Trends Immunol. 2002;23:549–55.
Wang L, Gong Z, Zhang X, Zhu F, Liu Y, Jin C, et al. Gut microbial bile acid metabolite skews macrophage polarization and contributes to high-fat diet-induced colonic inflammation. Gut Microbes. 2020;12:1–20.
Li Q, Ma L, Shen S, Guo Y, Cao Q, Cai X, et al. Intestinal dysbacteriosis-induced IL-25 promotes development of HCC via alternative activation of macrophages in tumor microenvironment. J Exp Clin Cancer Res. 2019;38:303.
Yu LX, Yan HX, Liu Q, Yang W, Wu HP, Dong W. et al. Endotoxin accumulation prevents carcinogen-induced apoptosis and promotes liver tumorigenesis in rodents. Hepatology. 2010;52:1322–33.
Uesugi T, Froh M, Arteel GE, Bradford BU, Thurman RG. Toll-like receptor 4 is involved in the mechanism of early alcohol-induced liver injury in mice. Hepatology. 2001;34:101–8.
Roh YS, Seki E. Toll-like receptors in alcoholic liver disease, non-alcoholic steatohepatitis and carcinogenesis. J Gastroenterol Hepatol. 2013;28:38–42.
Miura K, Kodama Y, Inokuchi S, Schnabl B, Aoyama T, Ohnishi H, et al. Toll-like receptor 9 promotes steatohepatitis by induction of interleukin-1beta in mice. Gastroenterology. 2010;139:323–34.e327.
Ma C, Han M, Heinrich B, Fu Q, Zhang Q, Sandhu M, et al. Gut microbiome-mediated bile acid metabolism regulates liver cancer via NKT cells. Science. 2018;360:eaan5931.
Li T, Lin X, Shen B, Zhang W, Liu Y, Liu H, et al. Akkermansia muciniphila suppressing nonalcoholic steatohepatitis associated tumorigenesis through CXCR6(+) natural killer T cells. Front Immunol. 2022;13:1047570.
Kotsiliti E, Leone V, Schuehle S, Govaere O, Li H, Wolf MJ, et al. Intestinal B cells license metabolic T-cell activation in NASH microbiota/antigen-independently and contribute to fibrosis by IgA-FcR signalling. J Hepatol. 2023;79:296–313.
Garnelo M, Tan A, Her Z, Yeong J, Lim CJ, Chen J, et al. Interaction between tumour-infiltrating B cells and T cells controls the progression of hepatocellular carcinoma. Gut. 2017;66:342–351.
Lu Z, Liu R, Wang Y, Jiao M, Li Z, Wang Z, et al. Ten-eleven translocation-2 inactivation restrains IL-10-producing regulatory B cells to enable antitumor immunity in hepatocellular carcinoma. Hepatology. 2023;77:745–59.
Xue H, Lin F, Tan H, Zhu ZQ, Zhang ZY, Zhao L. Overrepresentation of IL-10-Expressing B cells suppresses cytotoxic CD4+ T cell activity in HBV-induced hepatocellular carcinoma. PLoS ONE. 2016;11:e0154815.
Weng MT, Chiu YT, Wei PY, Chiang CW, Fang HL, Wei SC. Microbiota and gastrointestinal cancer. J Formos Med Assoc Taiwan. 2019;118:S32–S41.
Riaz F, Wei P, Pan F. Fine-tuning of regulatory T cells is indispensable for the metabolic steatosis-related hepatocellular carcinoma: a review. Front Cell Dev Biol. 2022;10:949603.
Chew V, Lai L, Pan L, Lim CJ, Li J, Ong R, et al. Delineation of an immunosuppressive gradient in hepatocellular carcinoma using high-dimensional proteomic and transcriptomic analyses. Proc Natl Acad Sci USA. 2017;114:E5900–E5909.
Liu T, Tan J, Wu M, Fan W, Wei J, Zhu B, et al. High-affinity neoantigens correlate with better prognosis and trigger potent antihepatocellular carcinoma (HCC) activity by activating CD39(+)CD8(+) T cells. Gut. 2021;70:1965–77.
Lim CJ, Lee YH, Pan L, Lai L, Chua C, Wasser M, et al. Multidimensional analyses reveal distinct immune microenvironment in hepatitis B virus-related hepatocellular carcinoma. Gut. 2019;68:916–27.
Chen S, Huang C, Liao G, Sun H, Xie Y, Liao C, et al. Distinct single-cell immune ecosystems distinguish true and de novo HBV-related hepatocellular carcinoma recurrences. Gut. 2023;72:1196–210.
Dudek M, Pfister D, Donakonda S, Filpe P, Schneider A, Laschinger M, et al. Auto-aggressive CXCR6(+) CD8 T cells cause liver immune pathology in NASH. Nature. 2021;592:444–9.
Funabashi M, Grove TL, Wang M, Varma Y, McFadden ME, Brown LC, et al. A metabolic pathway for bile acid dehydroxylation by the gut microbiome. Nature. 2020;582:566–70.
Hang S, Paik D, Yao L, Kim E, Trinath J, Lu J, et al. Bile acid metabolites control T(H)17 and T(reg) cell differentiation. Nature. 2019;576:143–8.
Campbell C, McKenney PT, Konstantinovsky D, Isaeva OI, Schizas M, Verter J, et al. Bacterial metabolism of bile acids promotes generation of peripheral regulatory T cells. Nature. 2020;581:475–9.
Yamagishi R, Kamachi F, Nakamura M, Yamazaki S, Kamiya T, Takasugi M, et al. Gasdermin D-mediated release of IL-33 from senescent hepatic stellate cells promotes obesity-associated hepatocellular carcinoma. Sci Immunol. 2022;7:eabl7209.
Loo TM, Kamachi F, Watanabe Y, Yoshimoto S, Kanda H, Arai Y, et al. Gut microbiota promotes obesity-associated liver cancer through PGE(2)-mediated suppression of antitumor immunity. Cancer Discov. 2017;7:522–38.
Bauer CA, Kim EY, Marangoni F, Carrizosa E, Claudio NM, Mempel TR. Dynamic Treg interactions with intratumoral APCs promote local CTL dysfunction. J Clin Investig. 2014;124:2425–40.
Cheng Y, Li H, Deng Y, Tai Y, Zeng K, Zhang Y, et al. Cancer-associated fibroblasts induce PDL1+ neutrophils through the IL6-STAT3 pathway that foster immune suppression in hepatocellular carcinoma. Cell Death Dis. 2018;9:422.
Bajaj JS, Hylemon PB. Gut-liver axis alterations in alcoholic liver disease: are bile acids the answer?. Hepatology. 2018;67:2074–5.
Vallianou N, Christodoulatos GS, Karampela I, Tsilingiris D, Magkos F, Stratigou T, et al. Understanding the role of the gut microbiome and microbial metabolites in non-alcoholic fatty liver disease: current evidence and perspectives. Biomolecules. 2021;12:56.
Collins SL, Stine JG, Bisanz JE, Okafor CD, Patterson AD. Bile acids and the gut microbiota: metabolic interactions and impacts on disease. Nat Rev Microbiol. 2023;21:236–47.
Hofmann AF. The enterohepatic circulation of bile acids in mammals: form and functions. Front Biosci. 2009;14:2584–98.
Ticho AL, Malhotra P, Dudeja PK, Gill RK, Alrefai WA. Intestinal absorption of bile acids in health and disease. Compr Physiol. 2019;10:21–56.
Sato Y, Atarashi K, Plichta DR, Arai Y, Sasajima S, Kearney SM, et al. Novel bile acid biosynthetic pathways are enriched in the microbiome of centenarians. Nature. 2021;599:458–64.
Cai J, Sun L, Gonzalez FJ. Gut microbiota-derived bile acids in intestinal immunity, inflammation, and tumorigenesis. Cell Host Microbe. 2022;30:289–300.
Li W, Hang S, Fang Y, Bae S, Zhang Y, Zhang M, et al. A bacterial bile acid metabolite modulates T(reg) activity through the nuclear hormone receptor NR4A1. Cell Host Microbe. 2021;29:1366–77.e1369.
Ahmad F, Saha P, Singh V, Wahid M, Mandal RK, Nath Mishra B, et al. Diet as a modifiable factor in tumorigenesis: focus on microbiome-derived bile acid metabolites and short-chain fatty acids. Food Chem. 2023;410:135320.
Fu T, Coulter S, Yoshihara E, Oh TG, Fang S, Cayabyab F, et al. FXR regulates intestinal cancer stem cell proliferation. Cell. 2019;176:1098–112.e1018.
Yoshimoto S, Loo TM, Atarashi K, Kanda H, Sato S, Oyadomari S, et al. Obesity-induced gut microbial metabolite promotes liver cancer through senescence secretome. Nature. 2013;499:97–101.
Bajaj JS. Alcohol, liver disease and the gut microbiota. Nat Rev Gastroenterol Hepatol. 2019;16:235–46.
Fuchs CD, Trauner M. Role of bile acids and their receptors in gastrointestinal and hepatic pathophysiology. Nat Rev Gastroenterol Hepatol. 2022;19:432–50.
Wei X, Li N, Wu X, Cao G, Qiao H, Wang J, et al. The preventive effect of Glycyrrhiza polysaccharide on lipopolysaccharide-induced acute colitis in mice by modulating gut microbial communities. Int J Biol Macromol. 2023;239:124199.
Hu W, Di Q, Liang T, Zhou N, Chen H, Zeng Z, et al. Effects of in vitro simulated digestion and fecal fermentation of polysaccharides from straw mushroom (Volvariella volvacea) on its physicochemical properties and human gut microbiota. Int J Biol Macromol. 2023;239:124188.
Satheesh Babu AK, Srinivasan H, Anandh Babu PV. Breaking bugs: gut microbes metabolize dietary components and modulate vascular health. Crit Rev Food Sci Nutr. 2023;64:1–9.
Cheng H, Zhang D, Wu J, Liu J, Zhou Y, Tan Y, et al. Interactions between gut microbiota and polyphenols: a mechanistic and metabolomic review. Phytomedicine. 2023;119:154979.
Dodd D, Spitzer MH, Van Treuren W, Merrill BD, Hryckowian AJ, Higginbottom SK, et al. A gut bacterial pathway metabolizes aromatic amino acids into nine circulating metabolites. Nature. 2017;551:648–52.
Degnan PH, Taga ME, Goodman AL. Vitamin B12 as a modulator of gut microbial ecology. Cell Metab. 2014;20:769–78.
Turnbaugh PJ, Ley RE, Hamady M, Fraser-Liggett CM, Knight R, Gordon JI. The human microbiome project. Nature. 2007;449:804–10.
Tan JK, Macia L, Mackay CR. Dietary fiber and SCFAs in the regulation of mucosal immunity. J Allergy Clin Immunol. 2023;151:361–70.
Dupraz L, Magniez A, Rolhion N, Richard ML, Da Costa G, Touch S, et al. Gut microbiota-derived short-chain fatty acids regulate IL-17 production by mouse and human intestinal γδ T cells. Cell Rep. 2021;36:109332.
Bachem A, Makhlouf C, Binger KJ, de Souza DP, Tull D, Hochheiser K, et al. Microbiota-derived short-chain fatty acids promote the memory potential of antigen-activated CD8(+) T cells. Immunity. 2019;51:285–97.e285.
Smith PM, Howitt MR, Panikov N, Michaud M, Gallini CA, Bohlooly YM, et al. The microbial metabolites, short-chain fatty acids, regulate colonic Treg cell homeostasis. Science. 2013;341:569–73.
Alrafas HR, Busbee PB, Nagarkatti M, Nagarkatti PS. Resveratrol modulates the gut microbiota to prevent murine colitis development through induction of Tregs and suppression of Th17 cells. J Leukoc Biol. 2019;106:467–80.
McBrearty N, Arzumanyan A, Bichenkov E, Merali S, Merali C, Feitelson M. Short chain fatty acids delay the development of hepatocellular carcinoma in HBx transgenic mice. Neoplasia. 2021;23:529–38.
Hu C, Xu B, Wang X, Wan WH, Lu J, Kong D, et al. Gut microbiota-derived short-chain fatty acids regulate group 3 innate lymphoid cells in HCC. Hepatology. 2023;77:48–64.
Song Q, Zhang X, Liu W, Wei H, Liang W, Zhou Y, et al. Bifidobacterium pseudolongum-generated acetate suppresses non-alcoholic fatty liver disease-associated hepatocellular carcinoma. J Hepatol. 2023;79:1352–65.
Zhou P, Chang WY, Gong DA, Xia J, Chen W, Huang LY, et al. High dietary fructose promotes hepatocellular carcinoma progression by enhancing O-GlcNAcylation via microbiota-derived acetate. Cell Metab. 2023;35:1961–75.e1966.
Zhao S, Jang C, Liu J, Uehara K, Gilbert M, Izzo L, et al. Dietary fructose feeds hepatic lipogenesis via microbiota-derived acetate. Nature. 2020;579:586–91.
Che Y, Chen G, Guo Q, Duan Y, Feng H, Xia Q. Gut microbial metabolite butyrate improves anticancer therapy by regulating intracellular calcium homeostasis. Hepatology. 2023;78:88–102.
Kumar M, Kaur R, Kanthaje S, Dhiman RK, Chakraborti A. Bacterial metabolite butyrate in modulating sorafenib-targeted microRNAs to curtail its resistance in hepatocellular carcinoma. J Cancer Res Clin Oncol. 2023;149:5823–39.
Shou JW, Shaw PC. Berberine activates PPARδ and promotes gut microbiota-derived butyric acid to suppress hepatocellular carcinoma. Phytomedicine. 2023;115:154842.
Zhu L, Baker SS, Gill C, Liu W, Alkhouri R, Baker RD, et al. Characterization of gut microbiomes in nonalcoholic steatohepatitis (NASH) patients: a connection between endogenous alcohol and NASH. Hepatology. 2013;57:601–9.
Barreau F, Hugot JP. Intestinal barrier dysfunction triggered by invasive bacteria. Curr Opin Microbiol. 2014;17:91–98.
Yahoo N, Dudek M, Knolle P, Heikenwälder M. Role of immune responses in the development of NAFLD-associated liver cancer and prospects for therapeutic modulation. J Hepatol. 2023;79:538–51.
Wolf MJ, Adili A, Piotrowitz K, Abdullah Z, Boege Y, Stemmer K, et al. Metabolic activation of intrahepatic CD8+ T cells and NKT cells causes nonalcoholic steatohepatitis and liver cancer via cross-talk with hepatocytes. Cancer Cell. 2014;26:549–64.
Telesford KM, Yan W, Ochoa-Reparaz J, Pant A, Kircher C, Christy MA, et al. A commensal symbiotic factor derived from Bacteroides fragilis promotes human CD39(+)Foxp3(+) T cells and Treg function. Gut Microbes. 2015;6:234–42.
Nejman D, Livyatan I, Fuks G, Gavert N, Zwang Y, Geller LT, et al. The human tumor microbiome is composed of tumor type-specific intracellular bacteria. Science. 2020;368:973–80.
Walker SP, Tangney M, Claesson MJ. Sequence-based characterization of intratumoral bacteria-A guide to best practice. Front Oncol. 2020;10:179.
Huang JH, Wang J, Chai XQ, Li ZC, Jiang YH, Li J, et al. The intratumoral bacterial metataxonomic signature of hepatocellular carcinoma. Microbiol Spectr. 2022;10:e0098322.
Zhu Z, Cai J, Hou W, Xu K, Wu X, Song Y, et al. Microbiome and spatially resolved metabolomics analysis reveal the anticancer role of gut Akkermansia muciniphila by crosstalk with intratumoral microbiota and reprogramming tumoral metabolism in mice. Gut Microbes. 2023;15:2166700.
Riquelme E, Zhang Y, Zhang L, Montiel M, Zoltan M, Dong W, et al. Tumor microbiome diversity and composition influence pancreatic cancer outcomes. Cell. 2019;178:795–806.e712.
Chen Y, Liu B, Wei Y, Kuang DM. Influence of gut and intratumoral microbiota on the immune microenvironment and anti-cancer therapy. Pharmacol Res. 2021;174:105966.
Liu Y, Kim ES, Guo H. Hepatitis B virus-related hepatocellular carcinoma exhibits distinct intratumoral microbiota and immune microenvironment signatures. J Med Virol. 2024;96:e29485.
Sun L, Ke X, Guan A, Jin B, Qu J, Wang Y, et al. Intratumoural microbiome can predict the prognosis of hepatocellular carcinoma after surgery. Clin Transl Med. 2023;13:e1331.
Qu D, Wang Y, Xia Q, Chang J, Jiang X, Zhang H. Intratumoral microbiome of human primary liver cancer. Hepatol Commun. 2022;6:1741–52.
He Y, Zhang Q, Yu X, Zhang S, Guo W. Overview of microbial profiles in human hepatocellular carcinoma and adjacent nontumor tissues. J Transl Med. 2023;21:68.
Park EM, Chelvanambi M, Bhutiani N, Kroemer G, Zitvogel L, Wargo JA. Targeting the gut and tumor microbiota in cancer. Nat Med. 2022;28:690–703.
Gur C, Ibrahim Y, Isaacson B, Yamin R, Abed J, Gamliel M, et al. Binding of the Fap2 protein of Fusobacterium nucleatum to human inhibitory receptor TIGIT protects tumors from immune cell attack. Immunity. 2015;42:344–55.
Abe S, Masuda A, Matsumoto T, Inoue J, Toyama H, Sakai A, et al. Impact of intratumoral microbiome on tumor immunity and prognosis in human pancreatic ductal adenocarcinoma. J Gastroenterol. 2024;59:250–62.
Jinadasa RN, Bloom SE, Weiss RS, Duhamel GE. Cytolethal distending toxin: a conserved bacterial genotoxin that blocks cell cycle progression, leading to apoptosis of a broad range of mammalian cell lineages. Microbiology. 2011;157:1851–75.
Elwell CA, Dreyfus LA. DNase I homologous residues in CdtB are critical for cytolethal distending toxin-mediated cell cycle arrest. Mol Microbiol. 2000;37:952–63.
Tsay JJ, Wu BG, Badri MH, Clemente JC, Shen N, Meyn P, et al. Airway microbiota is associated with upregulation of the PI3K pathway in lung cancer. Am J Respir Crit Care Med. 2018;198:1188–98.
Chen S, Zhang L, Li M, Zhang Y, Sun M, Wang L, et al. Fusobacterium nucleatum reduces METTL3-mediated m(6)A modification and contributes to colorectal cancer metastasis. Nat Commun. 2022;13:1248.
Xie Y, Xie F, Zhou X, Zhang L, Yang B, Huang J, et al. Microbiota in tumors: from understanding to application. Adv Sci. 2022;9:e2200470.
Thiele Orberg E, Fan H, Tam AJ, Dejea CM, Destefano Shields CE, Wu S, et al. The myeloid immune signature of enterotoxigenic Bacteroides fragilis-induced murine colon tumorigenesis. Mucosal Immunol. 2017;10:421–33.
Li S, Xia H, Wang Z, Zhang X, Song T, Li J, et al. Intratumoral microbial heterogeneity affected tumor immune microenvironment and determined clinical outcome of HBV-related HCC. Hepatology. 2023;78:1079–91.
Xue C, Gu X, Shi Q, Ma X, Jia J, Su Y, et al. The interaction between intratumoral bacteria and metabolic distortion in hepatocellular carcinoma. J Transl Med. 2024;22:237.
Eren CY, Gurer HG, Gursoy OO, Sezer CV. Antitumor effects of L-citrulline on hela cervical cancer cell lines. Anti-Cancer Agents Med Chem. 2022;22:3157–62.
Fu A, Yao B, Dong T, Chen Y, Yao J, Liu Y, et al. Tumor-resident intracellular microbiota promotes metastatic colonization in breast cancer. Cell. 2022;185:1356–72.e1326.
Zhang N, Nan A, Chen L, Li X, Jia Y, Qiu M, et al. Circular RNA circSATB2 promotes progression of non-small cell lung cancer cells. Mol Cancer. 2020;19:101.
Zhao X, Wu X, Qian M, Song Y, Wu D, Zhang W. Knockdown of TGF-β1 expression in human umbilical cord mesenchymal stem cells reverts their exosome-mediated EMT promoting effect on lung cancer cells. Cancer Lett. 2018;428:34–44.
Kim DH, Kim H, Choi YJ, Kim SY, Lee JE, Sung KJ, et al. Exosomal PD-L1 promotes tumor growth through immune escape in non-small cell lung cancer. Exp Mol Med. 2019;51:1–13.
Guo S, Chen J, Chen F, Zeng Q, Liu WL, Zhang G. Exosomes derived from Fusobacterium nucleatum-infected colorectal cancer cells facilitate tumour metastasis by selectively carrying miR-1246/92b-3p/27a-3p and CXCL16. Gut. 2020. https://doi.org/10.1136/gutjnl-2020-321187.
Cao Y, Wang Z, Yan Y, Ji L, He J, Xuan B, et al. Enterotoxigenic bacteroidesfragilis promotes intestinal inflammation and malignancy by inhibiting exosome-packaged miR-149-3p. Gastroenterology. 2021;161:1552–66.e1512.
Galeano Niño JL, Wu H, LaCourse KD, Kempchinsky AG, Baryiames A, Barber B, et al. Effect of the intratumoral microbiota on spatial and cellular heterogeneity in cancer. Nature. 2022;611:810–7.
Ferrari V, Rescigno M. The intratumoral microbiota: friend or foe? Trends Cancer. 2023;9:472–9.
Ramírez-Labrada AG, Isla D, Artal A, Arias M, Rezusta A, Pardo J, et al. The influence of lung microbiota on lung carcinogenesis, immunity, and immunotherapy. Trends Cancer. 2020;6:86–97.
Snyder A, Makarov V, Merghoub T, Yuan J, Zaretsky JM, Desrichard A, et al. Genetic basis for clinical response to CTLA-4 blockade in melanoma. N Engl J Med. 2014;371:2189–99.
Fluckiger A, Daillère R, Sassi M, Sixt BS, Liu P, Loos F, et al. Cross-reactivity between tumor MHC class I-restricted antigens and an enterococcal bacteriophage. Science. 2020;369:936–42.
Vancamelbeke M, Vermeire S. The intestinal barrier: a fundamental role in health and disease. Expert Rev Gastroenterol Hepatol. 2017;11:821–34.
Hou H, Chen D, Zhang K, Zhang W, Liu T, Wang S, et al. Gut microbiota-derived short-chain fatty acids and colorectal cancer: Ready for clinical translation? Cancer Lett. 2022;526:225–35.
Duizer C, de Zoete MR. The role of microbiota-derived metabolites in colorectal cancer. Int J Mol Sci. 2023;24:8024.
Jin C, Lagoudas GK, Zhao C, Bullman S, Bhutkar A, Hu B, et al. Commensal microbiota promote lung cancer development via γδ T cells. Cell. 2019;176:998–1013.e1016.
Greathouse KL, White JR, Vargas AJ, Bliskovsky VV, Beck JA, von Muhlinen N, et al. Interaction between the microbiome and TP53 in human lung cancer. Genome Biol. 2018;19:123.
Liu W, Zhang X, Xu H, Li S, Lau HC, Chen Q, et al. Microbial community heterogeneity within colorectal neoplasia and its correlation with colorectal carcinogenesis. Gastroenterology. 2021;160:2395–408.
Murota Y, Jobin C. Bacteria break barrier to promote metastasis. Cancer Cell. 2021;39:598–600.
Pleguezuelos-Manzano C, Puschhof J, Rosendahl Huber A, van Hoeck A, Wood HM, Nomburg J, et al. Mutational signature in colorectal cancer caused by genotoxic pks(+) E. coli. Nature. 2020;580:269–73.
Dejea CM, Fathi P, Craig JM, Boleij A, Taddese R, Geis AL, et al. Patients with familial adenomatous polyposis harbor colonic biofilms containing tumorigenic bacteria. Science. 2018;359:592–7.
Bertocchi A, Carloni S, Ravenda PS, Bertalot G, Spadoni I, Lo Cascio A, et al. Gut vascular barrier impairment leads to intestinal bacteria dissemination and colorectal cancer metastasis to liver. Cancer Cell. 2021;39:708–24.e711.
Guo W, Zhang Y, Guo S, Mei Z, Liao H, Dong H, et al. Tumor microbiome contributes to an aggressive phenotype in the basal-like subtype of pancreatic cancer. Commun Biol. 2021;4:1019.
Ho WJ, Zhu Q, Durham J, Popovic A, Xavier S, Leatherman J, et al. Neoadjuvant cabozantinib and nivolumab converts locally advanced HCC into resectable disease with enhanced antitumor immunity. Nat Cancer. 2021;2:891–903.
Kaseb AO, Hasanov E, Cao HST, Xiao L, Vauthey JN, Lee SS, et al. Perioperative nivolumab monotherapy versus nivolumab plus ipilimumab in resectable hepatocellular carcinoma: a randomised, open-label, phase 2 trial. Lancet Gastroenterol Hepatol. 2022;7:208–18.
Marron TU, Fiel MI, Hamon P, Fiaschi N, Kim E, Ward SC, et al. Neoadjuvant cemiplimab for resectable hepatocellular carcinoma: a single-arm, open-label, phase 2 trial. Lancet Gastroenterol Hepatol. 2022;7:219–29.
Qin S, Chen M, Cheng AL, Kaseb AO, Kudo M, Lee HC, et al. Atezolizumab plus bevacizumab versus active surveillance in patients with resected or ablated high-risk hepatocellular carcinoma (IMbrave050): a randomised, open-label, multicentre, phase 3 trial. Lancet. 2023;402:1835–47.
Yau T, Park JW, Finn RS, Cheng AL, Mathurin P, Edeline J, et al. Nivolumab versus sorafenib in advanced hepatocellular carcinoma (CheckMate 459): a randomised, multicentre, open-label, phase 3 trial. Lancet Oncol. 2022;23:77–90.
Llovet JM, Kudo M, Merle P, Meyer T, Qin S, Ikeda M, et al. Lenvatinib plus pembrolizumab versus lenvatinib plus placebo for advanced hepatocellular carcinoma (LEAP-002): a randomised, double-blind, phase 3 trial. Lancet Oncol. 2023;24:1399–410.
Liu X, Li S, Wang L, Ma K. Microecological regulation in HCC therapy: gut microbiome enhances ICI treatment. Biochim Biophys Acta Mol Basis Dis. 2024;1870:167230.
Zhu C, Zhang C, Wang S, Xun Z, Zhang D, Lan Z, et al. Characterizations of multi-kingdom gut microbiota in immune checkpoint inhibitor-treated hepatocellular carcinoma. J Immunother Cancer. 2024;12:e008686.
Li J, Sung CY, Lee N, Ni Y, Pihlajamäki J, Panagiotou G, et al. Probiotics modulated gut microbiota suppresses hepatocellular carcinoma growth in mice. Proc Natl Acad Sci USA. 2016;113:E1306–1315.
Chen S, Han P, Zhang Q, Liu P, Liu J, Zhao L, et al. Lactobacillus brevis alleviates the progress of hepatocellular carcinoma and type 2 diabetes in mice model via interplay of gut microflora, bile acid and NOTCH 1 signaling. Front Immunol. 2023;14:1179014.
Acknowledgements
We would like to thank all the members of the Department of Gastroenterology in our hospitals for their careful review of the manuscript and valuable comments.
Funding
This work was supported by the National Natural Science Foundation of China (NSFC) Young Scientists Fund Project (No. NSFC 82100124), Guangdong Province Science and Technology Department’s Guangdong-Hong Kong-Macao Joint Innovation Program (2023A0505010007), and Guangzhou Science and Technology Program - Municipal-University Joint Key Project (2023A03J0955).
Author information
Authors and Affiliations
Contributions
Yiqin Wang, Yongqiang Li, and Yong Lin are involved in the designing and drafting of the manuscript. Chuangyu Cao, Dongcheng Chen, Xianguang Huang and Canhua Li are responsible for searching and screening papers, and manuscript revision. Haoming Xu and Huasheng Lai are responsible for the manuscript revising, Huiting Chen and Yongjian Zhou are responsible for the concept and design of the study and the interpretation of the data. All authors contributed to the paper and approved the submitted version.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wang, Y., Li, Y., Lin, Y. et al. Roles of the gut microbiota in hepatocellular carcinoma: from the gut dysbiosis to the intratumoral microbiota. Cell Death Discov. 11, 140 (2025). https://doi.org/10.1038/s41420-025-02413-z
Received:
Revised:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41420-025-02413-z
This article is cited by
-
Dietary intervention reshapes gut microbiota and lipid metabolism to enhance anti-tumor immunity and prognosis in hepatocellular carcinoma: a randomized controlled trial
BMC Cancer (2026)
-
Engineering microbial metabolites to modulate tumor immunity and advance cancer immunotherapy
Discover Immunity (2026)
-
A Microbial Odyssey: Reshaping Probiotic Destinies through Advanced Delivery Technologies
Probiotics and Antimicrobial Proteins (2026)
-
HBV reprograms the tumor microenvironment in hepatocellular carcinoma: mechanisms and therapeutic implications
Clinical and Experimental Medicine (2026)
-
Gut microbiome dysbiosis in hepatocellular carcinoma patients with persistent HCV viremia versus viral clearance: a cross-sectional study
Gut Pathogens (2025)