Abstract
Objective
To evaluate associations between the first trimester SIMPLE nutritional score, early placental markers, and pregnancy outcome.
Methods
This is a longitudinal prospective multicenter observational cohort study recruiting healthy women with no comorbidities and singleton viable pregnancies undergoing first trimester prenatal screening. The SIMPLE nutritional score, biochemical (pregnancy-associated plasma protein A (PAPP-a), free ß-human chorionic gonadotropin (β-HCG)) and ultrasound (placental volume, uterine artery Doppler velocimetry) markers of placental function were collected at enrollment. Birth outcomes were collected at delivery. Main Outcome Measures: Multivariate generalized linear and logistic regression models were performed to investigate associations between SIMPLE score subgroups (<6 versus ≥6) and items, placental markers, and pregnancy outcomes.
Results
Out of 2363 women enrolled, 325 were classified at high nutritional risk based on a first trimester SIMPLE score lower than 6. Multi-adjusted models showed that the SIMPLE score subgroup was significantly associated with first trimester PAPP-a concentrations (SIMPLE score ≥6 versus <6: β = 0.047 (95% CI 0.004;0.089), p < 0.05), as well as with the emergency cesarean section rates (SIMPLE score ≥6 versus <6: aOR = 0.73 (95% CI −1.38;−0.07), p < 0.05). The single item related to the first trimester hemoglobin concentrations higher than 110 g/L was significantly associated with early placental markers, birth (β = −116.2 (95% CI −213.6;18.7), p < 0.05) and placental weights (β = −28.2 (95% CI −50.4;6.0), p < 0.05) in multi-adjusted models.
Conclusions
The observed associations support the introduction of the SIMPLE score in clinical practice as a useful tool for predicting early placental development and pregnancy outcome.
Similar content being viewed by others
Introduction
Maternal nutrition is recognized as a relevant predictor of feto-maternal wellbeing and pregnancy outcome [1,2,3]. In particular, the overwhelming pandemic of female obesity has driven the attention on its adverse short- and long-term effects on human reproduction [4, 5]. In this setting, pregestational body mass index (BMI) and gestational weight gain (GWG) are commonly used as proxy of maternal nutritional, metabolic, and inflammatory status [6, 7]. Nevertheless, several studies showed that maternal adherence to specific dietary patterns is strongly associated with reproductive and pregnancy outcomes, independently of pregestational BMI and GWG [8,9,10]. This might reflect that anthropometric measurements alone may not depict the overall maternal nutritional status. Additionally, due to the need of multi-disciplinary specialists and the time-consuming nature, the validated tools to examine dietary patterns in pregnancy (i.e. food frequency questionnaire) are not feasible in most clinical settings. Therefore, the International Federation of Gynecology and Obstetrics (FIGO) proposed a 10-question checklist investigating the adherence to a healthy diet as a reproducible, time-saving, and accessible tool [11]. Previous studies reported the high acceptability and reproducibility of this tool, further demonstrating a high agreement with the gold-standard food frequency questionnaire in identifying women with suboptimal dietary quality in pregnancy [12,13,14]. In this context, our pilot study on 112 singleton low-risk pregnancies showed that the first trimester nutritional score calculated by using the modified FIGO nutrition checklist (SIMPLE score) was associated with first trimester markers of placental function (serum pregnancy-associated plasma protein-a (PAPP-a) concentrations, uterine artery mean pulsatility index, and placental volume) and gestational age at birth [15]. This study possibly showed the utility of the SIMPLE score as an early screening tool of nutritional risk and predictor of placental function and pregnancy course in clinical practice.
The SIMPLE Study protocol has been previously presented [16]. Briefly, this is a longitudinal prospective multicenter study designed to investigate the associations between maternal first trimester SIMPLE score, early markers of placental function, intrauterine fetal growth, and pregnancy outcome among healthy women with singleton autologous pregnancies in Italy. The aim of the present analysis was to investigate the associations between maternal first trimester SIMPLE score, early markers of placental function, and pregnancy outcome (i.e. gestational age at birth, birth and placental weights, blood loss, and rates of pregnancy complications) in the setting of a nationwide study, to further confirm the results of the pilot study and extend the result general validity.
Materials and methods
This is an ongoing multicenter prospective observational cohort study coordinated by the “V. Buzzi” Children Hospital, Milan (Coordination Unit), involving 24 Italian maternity units (Supplementary Table 1). The present analysis includes all women enrolled from January 2019 to January 2023.
The protocol was approved by the Medical Ethical and Institutional Review Board at the ‘V. Buzzi’ Children Hospital, Milan (promoting center, reference number 46091/2018, 7/11/2018), and followed at all recruiting centers. All participants signed a written informed consent form before participation.
Eligible patients were subsequently enrolled during the ultrasound scan of the first trimester combined screening test for aneuploidies (11+0-13+6 weeks), according to the following inclusion criteria: singleton viable pregnancy, maternal age of at least 18 years, gestational age between 11+0 and 13+6 weeks of pregnancy confirmed by a crown-rump length (CRL) measurement of 45–84 mm, and signed written informed consent. Exclusion criteria were: no comprehension of the Italian language, any known maternal chronic disease, ongoing pharmacological treatment at the time of enrollment, oocyte donation pregnancy, fetal congenital anomalies and aneuploidies further confirmed by invasive prenatal testing or diagnosed at birth.
At enrollment, all women filled a general questionnaire detailing age, pregestational BMI, ethnicity, conception mode, lifestyle habits (i.e. smoking and alcohol consumption), and medical history. A modified version of the FIGO nutrition checklist (SIMPLE checklist) was used at recruitment to provide a 0–10 nutritional score measuring the adherence to the national recommendations for a healthy diet in pregnancy (SIMPLE score). In detail, the FIGO nutrition checklist consists of four sections covering information on diet quality and specific micronutrients deficiencies. Additional adaptations of the checklist were based on the Italian guidelines on maternal nutrition during pregnancy, including one additional question on the consumption of iodized salt and the modified recommended intake of fruit and vegetables to five portions per day (SIMPLE checklist). A one-point score was calculated in case of positive answer for: consumption of meat 2–3 times per week, fruit and vegetables at least 5 times per day, fish 1–2 times per week, dairy products daily, whole cereals at least once per day, sweet and snacks less than 5 times per weeks, first trimester hemoglobin concentrations higher than 110 g/L, folic acid supplement use, use of iodized salt, and sun exposure at least 10–15 min per day.
Biochemical parameters, including serum PAPP-a and free β-human chorionic gonadotropin (free β-HCG), were obtained from one venous blood sample collected at enrollment, by using a solid-phase two-site sequential chemiluminescent immunometric assay (BRAHMS Kryptor, Hennigsdorf, Germany). Besides their use as markers of fetal aneuploidies, PAPP-a and HCG are glycoproteins mainly produced by the syncytiotrophoblast which may regulate the placental development through the modulations of the insulin-like growth factor pathways and vasculogenesis, finally playing a key role in trophoblastic invasion and fetal growth regulation [17, 18]. All ultrasound measurements were performed at enrollment by a Fetal Medicine Foundation certified sonographer according to the International Society of Ultrasound in Obstetrics and Gynecology (ISUOG) guidelines. In addition to CRL and biparietal diameter (BPD), the transabdominal measurements of Doppler velocimetry of uterine arteries (UA) and two-dimensional placental volume were performed. Transabdominal UA Doppler velocimetry was measured by identifying the artery along the uterine body from a midsagittal section and moving laterally to the paracervical vascular plexus [19]. The two-dimensional estimated placental volume (EPV) measurement was performed according to the formula proposed by Sonek et al., by acquiring the placental width (measuring the distance among placental edges, perpendicular to surface of placenta), height (as distance from uteroplacental interface to line used to measure width) and thickness (as distance from uteroplacental interface to fetal surface of placenta) [20].
Data on delivery outcomes were recorded from medical registry or phone interview. Maternal baseline characteristics, biochemical and ultrasound markers of placental function, and birth outcomes were described as medians and ranges for quantitative variables, and absolute and relative frequencies for categorical variables. Subgroups based on the SIMPLE score were defined based on the 25th percentile of the score distribution: high nutritional risk for SIMPLE scores <6 and low nutritional risk for SIMPLE score ≥6. Chi-square and Kruskall–Wallis or t-tests as appropriate were used to compare baseline characteristics, first trimester biochemical and ultrasound markers of placental function, and birth outcomes between these two subgroups.
After performing a Log10 transformation of non-normally distributed variables to approximate Gaussian distributions, generalized linear models adjusted for confounding factors (gestational age and GWG at enrollment, maternal age, parity, pregestational BMI, smoking habit, alcohol consumption, conception mode, fetal sex) were estimated to investigate associations between the SIMPLE score subgroup (≥6 versus <6, independent variable), first trimester biochemical (PAPP-a, free ß-HCG), and ultrasound (mean UtA PI, placental volume) markers of placental function, and pregnancy outcomes (gestational age at birth, birth weight, blood loss) (dependent variables). Multi-adjusted regression models including the previously defined confounding factors were designed to evaluate the associations between the SIMPLE score subgroup (≥6 versus <6, independent variable) and rates of adverse pregnancy outcomes (preterm delivery, gestational diabetes mellitus (GDM), hypertensive disorders of pregnancy, fetal growth restriction (FGR), and cesarean section). When pregnancy outcome data were considered as dependent variables, the additional adjustment for gestational age and GWG at term was performed. Finally, the same multivariate models were estimated to evaluate the associations between the single 10 items of the SIMPLE score and first trimester and pregnancy outcome data.
P-values < 0.05 were considered statistically significant. All analyses were performed using SAS 9.4 and SPSS Statistics for Windows, Version 21.0 (IBM Corp. Armonk, New York, NY, USA) and R version 3.2.1 (The R Foundation for Statistical Computing).
Results
A total of 2363 pregnant women with a singleton pregnancy were enrolled in the present study based on the inclusion criteria.
The SIMPLE nutrition checklist was fully filled out by 2259 women out of 2363, whilst at least one missing response was detected in 104 self-filled questionnaires. Supplementary Fig. 1 shows the flowchart of the study population. 2139 women (94.7% of the total study population) showed at least one nutritional risk as defined by at least one negative answer at the SIMPLE nutrition checklist and 325 women (14.4%) were classified at high nutritional risk due to a calculated SIMPLE score lower than 6. Table 1 presents the baseline characteristics of the total study population and SIMPLE score subgroups at enrollment. The high nutritional risk subgroup (SIMPLE score <6) showed lower maternal age and educational level, as well as higher non-caucasian ethnicity and smoking habit compared to the low nutritional risk subgroup (SIMPLE score ≥6). The major areas of nutritional deficiencies as detected by the SIMPLE nutrition checklist were related to daily whole grain consumption, sun exposure, and reported first trimester hemoglobin concentrations higher than 110 g/L (Supplemental Table 2). The first trimester ultrasound and biochemical data were compared between the two SIMPLE score subgroups, showing significantly higher free beta-HCG concentrations in the low nutritional risk subgroup (Supplementary Table 3).
Data on pregnancy outcome were available for 1872 women (387 missing data, Supplementary Fig. 1). Table 2 shows the pregnancy outcome data in the total study population and SIMPLE score subgroups. The subgroup at low nutritional risk showed a significantly higher gestational age at birth (278 versus 276 days) and lower cesarean section rate (23.3% versus 33.5%) compared to the subgroup at high nutritional risk. No differences were detected with regard to the rates of pregnancy complications, birth and placental weights. No stillbirths were detected in the study population. Pregnancy outcome stratified based on the SIMPLE score are shown in Supplemental Table 4.
The results from generalized linear and logistic regression models are shown in Table 3 and Table 4, respectively. After adjustment for the previously defined confounding factors, the SIMPLE score subgroup showed significant associations with first trimester PAPP-a concentrations in the total study population, meaning lower PAPP-a concentrations in the subgroup at low nutritional risk (Table 3). The logistic regression models confirmed a significant association between the SIMPLE score subgroup and the rate of cesarean section (OR 0.65 (95% CI: 0.47;0.90), p < 0.05), meaning a lower cesarean section rate by 35% in the subgroup at low nutritional risk. No associations were detected with other adverse outcomes including hypertensive disorders of pregnancy, GDM, prematurity, and FGR rates (Table 4). When only emergency cesarean sections during labor were selected (n = 156, 32.8% of the total cesarean section number), the association remained significant (SIMPLE score ≥6 versus <6: β = −0.73 (95% IC −1.38; −0.07), p < 0.05).
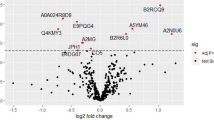
Finally, the single items of the SIMPLE score were considered in multi-adjusted models including the same confounding factors (Fig. 1). Fish consumption and folic acid supplementation were significantly associated with first trimester BPD measurements (β = 0.23 (95% CI 0.03; 0.44), p < 0.05, and β = −0.53 (95% CI −0.97; −0.09), p < 0.01, respectively), dairy consumption and sun exposure with free β-HCG concentrations (β = 4.54 (95% CI 0.19; 8.89), p < 0.05, and β = 4.32 (95% CI 0.37; 8.27), p < 0.01, respectively), sweets and snacks consumption and sun exposure with PAPP-a concentrations (β = -0.25 (95% CI −0.45; −0.05), p < 0.01, and β = −0.21 (95% CI −0.38; −0.04), p < 0.05, respectively), and hemoglobin concentrations higher than 110 g/L with CRL (β = −0.52 (95% CI −0.95; −0.09), p < 0.05), BPD (β = −0.31 (95% CI −0.49; −0.12), p = 0.01), placental volume (β = 29.2 (95% CI 18.5; 39.9), p < 0.001), free β-HCG (β = 7.42 (95% CI 3.42; 11.42), p < 0.001) and PAPP-a (β = −0.47 (95% CI −0.64; −0.29), p < 0.001) concentrations. Concerning the association between the single items of the SIMPLE score and pregnancy outcomes, only first trimester hemoglobin concentrations reported higher than 110 g/L were significantly associated with birth (β = -116.2 (95% CI −213.6; 18.7), p < 0.05) and placental weights (β = −28.2 (95% CI −50.4; 6.0), p < 0.05), with no association with fetal-placental weight ratio.
Generalized linear models were performed after a log-10 transformation of non-normally distributed variables to approximate Gaussian distributions. All models are adjusted for maternal age (continuous), BMI (continuous), smoking habit (current versus ex/never), alcohol consumption (yes/no), conception mode (spontaneous versus ART), parity (nulliparous versus multiparous), fetal sex (male versus female), first trimester gestational age (continuous), first trimester gestational weight gain (continuous). PAPP-a pregnancy-associated plasma protein-A, free β-HCG free β-human chorionic gonadotropin, BPD biparietal diameter.
Discussion
The present multicenter prospective cohort study firstly described the adherence to a healthy diet based on the national recommendations on nutrition in pregnancy in a large sample of healthy women with singleton first trimester viable pregnancies in Italy. Alarming rates of nutritional risk were reported in a sample of apparently low-risk pregnancies, with 94.7% of the total study population showing at least one nutritional risk (as defined by one negative answer to the SIMPLE nutrition checklist) and 14.4% of the total study population reporting five or more negative answers. Our results are in line with recent data from a smaller Greek study where 99% of the included pregnancies exhibited at least one nutritional risk factor based on the FIGO nutrition checklist [21].
The detected areas of major deficiencies were reported in whole grain consumption, sun exposure and reported hemoglobin levels higher than 110 g/L, with about one half of the total study population providing negative answers. As expected, the subgroup at high nutritional risk included younger, less educated, and more frequently non-caucasian and smoker women compared to the group with low nutritional risk.
Secondly, our results showed significant associations between the first trimester maternal SIMPLE score and early biochemical markers of placental development, whilst no associations were detected with placental ultrasound markers, in contrast to the SIMPLE pilot study [15]. This may be probably explained by the multicentric design of the present study and the related difficulties in technical measurements, as demonstrated by the very high variability of the placental volume measurements in the total study population. The univariate analysis showed significantly lower free β-HCG concentrations in the subgroup of women at high nutritional risk, but this result lost statistical significance in the multivariate model, thus meaning a difference mainly mediated by confounding factors. Conversely, when adjustment for confounding factors notoriously related to placental development and function was included, significant associations were confirmed between the SIMPLE score subgroup and first trimester PAPP-a concentrations. Previous studies showed the strong dependence of first trimester PAPP-a concentrations on gestational age and both pregnancy and maternal characteristics. In particular, lower PAPP-a concentrations were reported in case of singleton versus multiple pregnancy, ART versus spontaneous conception, male fetuses, maternal caucasian ethnicity, pregestational diabetes, lower pregestational weight, smoking and multiparous mothers [22,23,24,25,26,27]. These results explain the current inclusion of all these variables in the algorithm of the first trimester combined screening test for aneuploidies. Nevertheless, our results highlight that first trimester maternal nutritional habits may further impact on first trimester biomarker concentrations, possibly affecting the screening results. Unexpectedly, the detected association between the SIMPLE score and PAPP-a concentrations was negative in both univariate and multivariate models, but this might be mediated by differences in the mass of the trophoblastic tissues, as shown by the smaller ultrasound-determined placental volume in case of higher SIMPLE scores, in agreement with previous studies [28]. Both the underlying mechanisms and relevance of this association is still unknown and needs further research to be elucidated. Additionally, the single items of the SIMPLE score were individually evaluated in order to define the ones mostly impacting on first trimester biochemical and ultrasound markers of feto-placental development. Folic acid supplementation, hemoglobin concentrations higher than 110 g/L, sun exposure, and consumption of fish, dairy and sweets were found significantly associated with both ultrasound (CRL, BPD, placental volume) and biochemical (PAPP-a, free β-HCG) markers in multivariate models including adjustment for gestational age, maternal and pregnancy characteristics. These results are in line with growing literature showing significant effects of periconceptional maternal nutritional habits and lifestyle on early parameters of embryonic growth and placental development [29, 30].
Finally, when pregnancy outcomes were considered as dependent variables, the first trimester maternal SIMPLE score was significantly associated with gestational age at birth only in the univariate model with a 2-days difference between subgroups, whilst multi-adjusted regression models demonstrated significant associations with higher rates of cesarean section in the subgroup at high nutritional risk. No associations were observed with birth weight and rates of GDM, FGR and hypertensive disorders of pregnancy. In particular, the first trimester SIMPLE score was negatively associated with both rates of total and emergency cesarean sections, meaning a lower cesarean section rates at increasing values of the first trimester SIMPLE score. This result is of interest as the cesarean section unequivocally represents an adverse pregnancy outcome, leading to increased maternal and perinatal morbidity and mortality [31]. It can be hypothesized that a fetus of a healthy mother, with optimal nutritional and lifestyle habits as early as the first trimester of pregnancy, might have more adequate nutritional and oxygen reserves for withstanding the stress linked to labor evolution, compared to a mother with nutritional deficiencies. Additionally, when the single items of the SIMPLE score were investigated in associations with term pregnancy outcomes, only first trimester hemoglobin concentrations higher than 110 g/L showed negative associations with both birth and placental weight at delivery. This result is in line with previous reports of a U-shaped relationship between maternal hemoglobin levels and placental and birth weight, indicating a potential negative effect of both iron depletion and overload on intrauterine development and growth [32, 33]. In particular, despite the association between maternal anemia and adverse pregnancy outcome (i.e. low birth weight, preterm birth, stillbirth, postpartum hemorrhage, perinatal and maternal mortality) is well-known, both the timing of diagnosis and the severity should be considered to stratify the risk of adverse outcome. As an example, a 2012 meta-analysis of 12 studies indicated that moderate to severe, but not mild maternal anemia was associated with an increased risk of small-for- gestational-age babies [34]. In line with these data, a large retrospective study on 173,031 pregnant women revealed an odds ratio (OR) of 1.68 (95% CI: 1.29; 2. 21) for preterm birth only for first trimester moderate-to-severe anemia (defined as less than 95 g/L at 12 weeks’ gestation), additionally showing significant associations between high first trimester hemoglobin level (greater than 149 g/L at 12 weeks’ gestation) and small for gestational age newborns (OR 1.27 (95% CI 1.02, 1.58)) [35]. These results highlight that an optimal range of maternal hemoglobin during the first trimester should be defined, based on the evidence that both extremes are associated with adverse obstetric outcome.
The present study shows several strengths and limitations. Firstly, the multicentric design of the study surely limited the interpretation of results on first trimester ultrasound markers, particularly for placental volume. Although an initial training was mandatory provided by the promoting center on the acquisition of the placental volume measurements, the detected high variability and the lack of internal validation of the measurement reduced the validity of this result. The same can be partially stated with regard to biochemical markers, whose collection was not centralized and was conversely delegated to each recruiting center, thus leading to potential differences in laboratory testing and results. The SIMPLE score was additionally calculated only in late first trimester, when modifications of nutritional behaviors could not be excluded due to nausea or hyperemesis. Therefore, subsequent changes in nutritional habits and exposures could not be excluded and may impact on the observed pregnancy outcomes. Furthermore, maternal complex dietary patterns and nutritional biomarkers (e.g. ferritin) were not available as a useful tool for internal validation of the SIMPLE score. Lastly, information on physical activity, as a crucial component of nutritional habits and lifestyle, as well as neonatal data after delivery were not collected.
On the other hand, this study presents several strengths. Firstly, the multicentric nationwide design allowed us to reach a large sample size, further representative of the whole Italian population. Additionally, the included population represents a well-defined sample of healthy women with low-risk pregnancies. The inclusion of maternal pregestational extreme BMI values, despite being synonymous of chronic comorbidity, contributed to increase the external validity of our findings, being representative of the national prevalence of abnormal BMI among fertile women. Although residual confounding could not be completely excluded, full adjustment for all known factors associated with intrauterine growth and development were considered in the final models.
In conclusion, the present study described the associations between first trimester maternal nutritional habits measured by the SIMPLE score, early biochemical and ultrasound markers of feto-placental growth, and pregnancy outcome in a large sample of singleton pregnancies in Italy. This study lays the foundation for the use of the SIMPLE score in clinical settings, as a useful, reproducible and time-saving predictor of early placental development and pregnancy outcome. In particular, the identification of areas of deficiencies through the SIMPLE score should lead to an individualized counseling aimed at modifying inadequate nutritional behaviors, with possible referral to dedicated specialists in case of a high nutritional risk. Future research should focus on the high-risk population and develop intervention strategies aiming at reducing the related risk.
Data availability
Data described in the manuscript will be made available upon request to the corresponding author.
References
Miele MJ, Souza RT, Calderon IM, Feitosa FE, Leite DF, Rocha Filho EA, et al. Maternal Nutrition Status Associated with Pregnancy-Related Adverse Outcomes. Nutrients. 2021;13:2398. https://doi.org/10.3390/nu13072398. Published 2021 Jul 13.
Merchant T, Soyemi E, Roytman MV, DiTosto JD, Beestrum M, Niznik CM, et al. Healthcare-based interventions to address food insecurity during pregnancy: a systematic review. Am J Obstet Gynecol MFM. 2023;5:100884. https://doi.org/10.1016/j.ajogmf.2023.100884.
Practice Committee of the American Society for Reproductive Medicine. Electronic address: asrm@asrm.org; Practice Committee of the American Society for Reproductive Medicine. Obesity and reproduction: a committee opinion. Fertil Steril. 2021;116:1266–85. https://doi.org/10.1016/j.fertnstert.2021.08.018.
Leddy MA, Power ML, Schulkin J. The impact of maternal obesity on maternal and fetal health. Rev Obstet Gynecol. 2008;1:170–8.
Fleming TP, Watkins AJ, Velazquez MA, Mathers JC, Prentice AM, Stephenson J, et al. Origins of lifetime health around the time of conception: causes and consequences. Lancet. 2018;391:1842–52. https://doi.org/10.1016/S0140-6736(18)30312-X.
Hrolfsdottir L, Schalkwijk CG, Birgisdottir BE, Gunnarsdottir I, Maslova E, Granström C, et al. Maternal diet, gestational weight gain, and inflammatory markers during pregnancy. Obesity (Silver Spring). 2016;24:2133–9. https://doi.org/10.1002/oby.21617.
Bjørke-Monsen AL, Ulvik A, Nilsen RM, Midttun Ø, Roth C, Magnus P, et al. Impact of Pre-Pregnancy BMI on B Vitamin and Inflammatory Status in Early Pregnancy: An Observational Cohort Study. Nutrients. 2016;8:776. https://doi.org/10.3390/nu8120776.
Anelli GM, Parisi F, Sarno L, Fornaciari O, Carlea A, Coco C, et al. Associations between Maternal Dietary Patterns, Biomarkers and Delivery Outcomes in Healthy Singleton Pregnancies: Multicenter Italian GIFt Study. Nutrients. 2022;14:3631. https://doi.org/10.3390/nu14173631.
Parisi F, Rousian M, Huijgen NA, Koning AHJ, Willemsen SP, de Vries JHM, et al. Periconceptional maternal ‘high fish and olive oil, low meat’ dietary pattern is associated with increased embryonic growth: The Rotterdam Periconceptional Cohort (Predict) Study. Ultrasound Obstet Gynecol. 2017;50:709–16. https://doi.org/10.1002/uog.17408.
Sanderman EA, Willis SK, Wise LA. Female dietary patterns and outcomes of in vitro fertilization (IVF): a systematic literature review. Nutr J. 2022;21:5. https://doi.org/10.1186/s12937-021-00757-7.
International Federation of gynecology and obstetrics (FIGO) nutrition checklist. 2015. Available: https://www.figo.org/sites/default/files/uploads/wgpublications/FIGO_Nutrition_Checklit.pdf. [Accessed 29 Apr 2020].
Jacob CM, Inskip HM, Lawrence W, McGrath C, McAuliffe FM, Killeen SL, et al. Acceptability of the FIGO Nutrition Checklist in Preconception and Early Pregnancy to Assess Nutritional Status and Prevent Excess Gestational Weight Gain: A Study of Women and Healthcare Practitioners in the UK. Nutrients. 2022;14:3623. https://doi.org/10.3390/nu14173623. Published 2022 Sep 1.
Killeen SL, Callaghan SL, Jacob CM, Hanson MA, McAuliffe FM. Examining the use of the FIGO Nutrition Checklist in routine antenatal practice: multistakeholder feedback to implementation. Int J Gynaecol Obstet. 2020;151:51–56. https://doi.org/10.1002/ijgo.13323.
Tsoi, Chan KY, Li RSM, McAuliffe LS, Hanson MA FM, Tam WH, et al. Evaluation of dietary pattern in early pregnancy using the FIGO Nutrition Checklist compared to a food frequency questionnaire. Int J Gynaecol Obstet. 2020;151:37–44. https://doi.org/10.1002/ijgo.13324.
Parisi F, Savasi VM, di Bartolo I, Mandia L, Cetin I. Associations between First Trimester Maternal Nutritional Score, Early Markers of Placental Function, and Pregnancy Outcome. Nutrients. 2020;12:1799. https://doi.org/10.3390/nu12061799.
Parisi F, Coco C, Cetin I. SIMPLE study group. Prospective multicentre Italian pregnancy cohort study (SIMPLE) on the associations of maternal first trimester SIMPLE nutritional score with early placental function markers and pregnancy outcomes. BMJ Open. 2022;12:e062940. https://doi.org/10.1136/bmjopen-2022-062940.
Spencer K, Cowans NJ, Avgidou K, Molina F, Nicolaides KH. First-trimester biochemical markers of aneuploidy and the prediction of small-for-gestational age fetuses. Ultrasound Obstet Gynecol. 2008;31:15–9.
Goetzinger KR, Singla A, Gerkowicz S, Dicke JM, Gray DL, Odibo AO. The efficiency of first-trimester serum analytes and maternal characteristics in predicting fetal growth disorders. Am J Obstet Gynecol. 2009;201:412.e1–6. https://doi.org/10.1016/j.ajog.2009.07.016.
Bhide A, Acharya G, Bilardo CM, Brezinka C, Cafici D, Hernandez-Andrade E, et al. ISUOG practice guidelines: use of Doppler ultrasonography in obstetrics. Ultrasound Obstet Gynecol. 2013;41:233–9. https://doi.org/10.1002/uog.12371.
Sonek J, Krantz D, Carmichael J, Downing C, Jessup K, Haidar Z, et al. First-trimester screening for early and late preeclampsia using maternal characteristics, biomarkers, and estimated placental volume. Am J Obstet Gynecol. 2018;218:126.e1–126.e13. https://doi.org/10.1016/j.ajog.2017.10.024.
Grammatikopoulou MG, Nigdelis MP, Haidich A-B, Kyrezi M, Ntine H, Papaioannou M, et al. Diet Quality and Nutritional Risk Based on the FIGO Nutrition Checklist among Greek Pregnant Women: A Cross-Sectional Routine Antenatal Care Study. Nutrients. 2023;15:2019. https://doi.org/10.3390/nu15092019.
Cowans NJ, Stamatopoulou A, Maiz N, Spencer K, Nicolaides KH. The impact of fetal gender on first trimester nuchal translucency and maternal serum free beta-hCG and PAPP-A MoM in normal and trisomy 21 pregnancies. Prenat Diagn. 2009;29:578–81. https://doi.org/10.1002/pd.2246.
Gjerris AC, Loft A, Pinborg A, Christiansen M, Tabor A. First-trimester screening markers are altered in pregnancies conceived after IVF/ICSI. Ultrasound Obstet Gynecol. 2009;33:8–17. https://doi.org/10.1002/uog.6254.
Krantz DA, Hallahan TW, Macri VJ, Macri JN. Maternal weight and ethnic adjustment within a first-trimester Down syndrome and trisomy 18 screening program. Prenat Diagn. 2005;25:635–40. https://doi.org/10.1002/pd.1188.
Spencer K, Ong CY, Liao AW, Nicolaides KH. The influence of parity and gravidity on first trimester markers of chromosomal abnormality. Prenat Diagn. 2000;20:792–4.
Spencer K, Bindra R, Cacho AM, Nicolaides KH. The impact of correcting for smoking status when screening for chromosomal anomalies using maternal serum biochemistry and fetal nuchal translucency thickness in the first trimester of pregnancy. Prenat Diagn. 2004;24:169–73. https://doi.org/10.1002/pd.819.
Spencer K, Cicero S, Atzei A, Otigbah C, Nicolaides KH. The influence of maternal insulin-dependent diabetes on fetal nuchal translucency thickness and first-trimester maternal serum biochemical markers of aneuploidy. Prenat Diagn. 2005;25:927–9. https://doi.org/10.1002/pd.1229.
Metzenbauer M, Hafner E, Hoefinger D, Schuchter K, Stangl G, Ogris E, et al. Three-dimensional ultrasound measurement of the placental volume in early pregnancy: method and correlation with biochemical placenta parameters. Placenta. 2001;22:602–5. https://doi.org/10.1053/plac.2001.0684.
Parisi F, Rousian M, Steegers-Theunissen RPM, Koning AHJ, Willemsen SP, de Vries JHM, et al. Early first trimester maternal ‘high fish and olive oil and low meat’ dietary pattern is associated with accelerated human embryonic development. Eur J Clin Nutr. 2018;72:1655–62. https://doi.org/10.1038/s41430-018-0161-7.
Smit AJP, Hojeij B, Rousian M, Schoenmakers S, Willemsen SP, Steegers-Theunissen RPM, et al. A high periconceptional maternal ultra-processed food consumption impairs embryonic growth: The Rotterdam periconceptional cohort. Clin Nutr. 2022;41:1667–75. https://doi.org/10.1016/j.clnu.2022.06.006.
WHO Statement on Caesarean Section Rates, 2015. Available at: https://iris.who.int/bitstream/handle/10665/161442/WHO_RHR_15.02_eng.pdf?sequence=1
Evanchuk JL, Kozyrskyj A, Vaghef-Mehrabani E, Lamers Y, Giesbrecht GF, Letourneau N, et al. Maternal Iron and Vitamin D Status during the Second Trimester Is Associated with Third Trimester Depression Symptoms among Pregnant Participants in the APrON Cohort. J Nutr. 2023. https://doi.org/10.1016/j.tjnut.2023.10.029.
Rooney DJ, Conway M, O’Keeffe LM, McDonnell CM, Bartels HC, Yelverton C, et al. Dietary intakes of iron, folate, and vitamin B12 during pregnancy and correlation with maternal hemoglobin and fetal growth: findings from the ROLO longitudinal birth cohort study. Arch Gynecol Obstet. 2023. https://doi.org/10.1007/s00404-023-06916-x.
Kozuki N, Lee AC, Katz J. Child Health Epidemiology Reference Group. Moderate to severe, but not mild, maternal anemia is associated with increased risk of small-for-gestational-age outcomes. J Nutr. 2012;142:358–62. https://doi.org/10.3945/jn.111.149237.
Scanlon KS, Yip R, Schieve LA, Cogswell ME. High and low hemoglobin levels during pregnancy: differential risks for preterm birth and small for gestational age. Obstet Gynecol. 2000;96:741–8. https://doi.org/10.1016/s0029-7844(00)00982-0.
Funding
The research project findings discussed here were supported by funding from Bayer Consumer Care AG. The funds were used to create the public database of the study. Bayer Consumer Care AG, as a co-founder of the study, will have single access to the published results for internal use as part of its institutional activities in full compliance with legal requirements. This work was partially supported by the Italian Ministry of Health.
Author information
Authors and Affiliations
Consortia
Contributions
FP and IC designed the study. FP, CC, SG, VS, LM, FP, AS, MG, GC, NDS, MM, RDA, LN conducted the study and abstracted study data. FP and GE conducted all analyses. FP and IC interpreted study findings and wrote the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics
The protocol was approved by the Medical Ethical and Institutional Review Board at the ‘V. Buzzi’ Children Hospital, Milan (promoting center, reference number 46091/2018, 7/11/2018), and followed at all recruiting centers. All methods were performed in accordance with the relevant guidelines and regulations.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Parisi, F., Coco, C., Esposito, G. et al. Maternal first trimester SIMPLE nutritional score, early markers of placental function and pregnancy outcome: a prospective multicenter Italian study (SIMPLE study). Eur J Clin Nutr 79, 855–862 (2025). https://doi.org/10.1038/s41430-025-01619-9
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41430-025-01619-9