Abstract
Our previous studies have shown that the maternal hyperinflammatory response in pre-eclampsia lowered the eclampsia-like seizure threshold. Cyclosporin A (CsA), which is an effective immunosuppressant, could attenuate the inflammatory responses in LPS-induced pre-eclampsia rats. Here, we hypothesized that CsA may ameliorate seizure severity through reducing systemic inflammation in pre-eclampsia/eclampsia. In the current study, the effects of CsA on pre-eclampsia manifestation, eclampsia-like seizure activities and systemic inflammation were examined in a pre-eclampsia model. Pregnant rats were given an intraperitoneal injection of the epileptogenic drug pentylenetetrazol (PTZ) following a tail vein injection of lipopolysaccharide to establish the eclampsia-like seizure model. CsA (5 mg/kg) was administered intravenously through the tail after LPS infusion. Mean systolic blood pressure and proteinuria in pre-eclampsia were detected. After PTZ injection, seizure activity was assessed, inflammatory responses were determined and pregnancy outcomes were analyzed. The results showed that CsA treatment significantly decreased blood pressure and proteinuria and increased the fetal and placental weight (P < 0.01). Meanwhile, CsA treatment significantly reduced serum IL-1β, TNF-α, and IL-17 levels (P < 0.01), decreased the seizure scores and prolonged the latency to seizure (P < 0.01). CsA effectively attenuated pre-eclampsia manifestation and eclampsia-like seizure severity. In addition, CsA treatment significantly reduced the inflammatory cytokine levels and improved pregnancy outcomes following eclampsia-like seizures. The decreased inflammatory cytokines in pre-eclampsia are coincident with attenuated pre-eclampsia manifestation after CsA treatment, suggesting that CsA treatment might decrease the eclampsia-like seizure severity through decreasing systemic inflammation in pre-eclasmpsia/eclampsia.
Similar content being viewed by others
Introduction
Eclampsia is characterized by grand mal seizures and elevated neuronal excitability that cannot be attributed to other causes in women with pre-eclampsia, which is an important reason for the adverse perinatal outcomes [1]. Pre-eclampsia/eclampsia, which have been estimated to complicate 2–8% of pregnancies globally, constitute one of the leading causes of perinatal and maternal mortality worldwide [2].
Previous findings have shown that normal pregnancy involves a mild state of inflammation at the maternal-fetal interface [3]. Clinical and experimental evidence suggests that an exaggerated maternal inflammatory response might play a role in the onset of pre-eclampsia [4, 5]. Cipolla et al. showed that pregnant serum induces neuroinflammation and hyperexcitability in hippocampal neurons and seizure activity by TNF-α [6]. In our previous study, we generated and characterized an experimental eclampsia-like model using the epileptogenic drug PTZ (a GABA receptor antagonist) [7]. Our previous studies in animal models of pre-eclampsia and eclampsia revealed that the seizure threshold of eclampsia could be decreased by excessive systemic inflammation in pre-eclampsia. These findings indicated that inhibiting the increased inflammation responses in pre-eclampsia could reverse seizure susceptibility in eclampsia [7,8,9].
Cyclosporin A (CsA) is well known for its immunosuppressive activity [10] and prevents rejection following solid organ and bone marrow transplants as well as in the treatment of immune-related disorders, such as systemic lupus erythematosus (SLE). Furthermore, CsA is used for the treatment of chronic inflammatory diseases [11] and inhibits the production of IL-2 by activating T lymphocytes through a calcineurin-dependent pathway [12]. CsA plays a protective role in pregnancy-related immune inflammatory diseases. Both spontaneous abortion models and in vitro experiments have shown that CsA can inhibit the production of the inflammatory factors TNF-α and IL-4 [13, 14]. Our previous studies showed that CsA could reduce the increased inflammatory responses in LPS-induced pre-eclampsia rats [8]. CsA also has neuroprotective effects by reducing cell death and structural or functional changes following prolonged seizure activity, traumatic brain injury, and stroke [10, 15, 16]. Therefore, in the present study, we investigated whether CsA can ameliorate seizure severity through reducing systemic inflammation in pre-eclampsia/eclampsia.
Materials and methods
Animal model
All experimental procedures were performed within the NIH Guidelines (NIH Publications No. 8023, revised 1978) for the Care and Use of Laboratory Animals and approved by the Committee on the Ethics of Animal Experiments of Guangzhou Medical University (Permit Number: 2013-39). Thirty female Sprague Dawley rats (weighing 240–280 g, obtained from the Medical Experimental Animal Center of Guangdong, China) were used for this study. Rats were fed a common diet by the experimental center at Guangzhou Medical University.
Each rat used in all the pregnancy groups was separately mated overnight. Day 1 of pregnancy was defined as the day when spermatozoa were found in a vaginal smear. Animals were randomly assigned to three groups: the pregnant group (P group, n = 10), the pre-eclampsia group (PE group, n = 10), and the pre-eclampsia group treated with CsA (PE + CsA group, n = 10). PE group: based on the method of Fass et al., rats were intraperitoneally anesthetized with 10% chloral hydrate (3.5 mL/kg). Then, the tail intravenous injection of LPS (1.0 mg/kg body weight in 2 mL of pyrogen-free saline solution) was conducted at a speed of 2 mL/h on gestational day 14 (GD14) [17]. PE + CsA group: after LPS infusion, rats were treated with 5 mg/kg of CsA through tail intravenous injection from GD16 to GD18. P group: on GD14, the rats received 0.9% saline according to the method of LPS infusion. On GD20, seizures were induced by intraperitoneal injection of PTZ (40 mg/kg) in all animals.
Drugs and solutions
LPS (strain Escherichia coli 055:B5, Sigma-Aldrich, St. Louis, MO), PTZ, and CsA (Sandimmun Neoral, Novartis, Switzerland) were dissolved in 0.9% saline. A stock solution of 1 mg/mL LPS was prepared and kept at −20 °C. A 1% (g/100 mL) PTZ solution was freshly prepared each day. A 50 mg/mL CsA solution was freshly prepared and diluted to 5 mg/mL when used. ELISA kits, which were obtained from eBioscience (San Diego, USA), were used to analyze the levels of tumor necrosis factor (TNF-α), interleukin-1β (IL-1β), and interleukin-17 (IL-17).
Measurement of systolic blood pressure and 24 h urinary albumin excretion
SBP measurements were carried out three times a day from 9:00 a.m. to 12:00 a.m. on GDs 14 (before LPS infusion), 16 and 19 by a noninvasive blood pressure system (BP100-A, Chengdu Taimeng Technologies). SBP measurements were performed three times on each occasion for each rat, and the mean values were recorded. At the same time points, rats were individually placed in metabolic cages to collect urine for 24 h urinary albumin excretion (from the previous day at 6 p.m. to the recorded day at 6 p.m.) measurements using an automatic analyzer (HIACHI 7600-020, Japan).
Latency to seizure and behavioral seizure score measurements
On GD20, immediately after the PTZ injection, each animal was placed in the center of a cage (30 × 30 × 50 cm), and its behavior was monitored for 60 min. According to methods in Racine et al., seizure severity was classified into five stages: stage 1, immobility, eyes closed, and facial clonus; stage 2, head nodding and more severe facial clonus; stage 3, clonus of one forelimb; stage 4, rearing with bilateral forelimb clonus; and stage 5, generalized tonic-clonic seizure [18]. The scoring for the seizures was carried out by an observer who was unaware of the animal’s group. The latency to develop seizures was measured; the time began from the PTZ injection and ended at the occurrence of stage 1 seizures.
Cytokine analysis
On GD20 after behavioral assessment, rats were anesthetized nonfatally by intraperitoneal administration of chloral hydrate; 2 mL blood specimens were taken from the inferior cava vena of each rat. A highly sensitive enzyme-linked immunosorbent assay (eBioscience, USA) was used to detect the serum levels of cytokines (IL-1β, TNF-α, IL-17, and IL-10).
Measurement of pregnancy outcomes
On GD20, the blood samples were collected, and then, the rats were sacrificed. The pups and placentas were removed by caesarean section, counted, and weighed. Pup viability, resorption, and gross morphology were also assessed.
The graphical timeline

Statistical analysis
All values are expressed as the mean ± SEM. One-way analysis of variance was used to compare the mean values between different groups; if the homogeneity test of variance was met, further data analysis was followed by an appropriate least significant difference post hoc test; if not, Dunnett’s test was applied. The Wilcoxon sign rank test was used to compare median scores. SPSS 13.0 software (SPSS, Chicago, IL, USA) was used to perform all statistical analyses. Statistical significance was defined as p < 0.05.
Results
CsA administration reduced SBP and mean 24 h proteinuria levels in pre-eclampsia rats
To detect the effects of CsA on PE-like manifestations, SBP and mean 24 h proteinuria levels were analyzed. Before LPS administration on GD14, the SBP values were comparable between the groups with no statistically significant differences (Fig. 1, P > 0.05). SBP increased obviously in the PE group on days 16 and 19 of gestation (125 ± 1.25 mmHg, 128 ± 0.88 mmHg) compared with the P group on 16 (102 ± 1.13 mmHg) and 19 (102 ± 1.26 mmHg) days after gestation (*P < 0.01); within the PE group, SBP also increased on days 16 and 19 of gestation after LPS administration compared with values on GD14 (105 ± 1.15 mmHg) (*P < 0.01). After LPS infusion, SBP was also increased in the PE + CsA group on GD16 (125 ± 1.27 mmHg) compared with the P group (102 ± 1.13 mmHg) (#*P < 0.01); it was lower on GD19 (106 ± 1.26 mmHg) compared with the PE group (128 ± 0.88 mmHg) (#P < 0.01); within the PE + CsA group, SBP was higher on day 16 of gestation (125 ± 1.27 mmHg) compared with values on GD14 (103 ± 1.62 mmHg) (#*P < 0.01), but it decreased significantly on day 19 of gestation compared with the value on GD16 (#P < 0.01).
Changes in mean systolic blood pressure (SBP) in all three groups at 14, 16, and 19 days after gestation. Values are presented as the mean ± SEM. SBP increased significantly in the PE group compared with the P group on 16 and 19 days after gestation (*P < 0.01); within the PE group, SBP was also higher on days 17 and 19 of gestation after LPS administration compared with values on GD14 (*P < 0.01). Following LPS administration, SBP was also increased in the PE + CsA group on GD16 compared with the P group (#*P < 0.01) and was lower on GD19 compared with the PE group (#P < 0.01); within the PE + CsA group, SBP was higher on day 16 of gestation compared with values on GD14 (#*P < 0.01), but it decreased significantly on day 19 of gestation compared with the value on GD16 (#P < 0.01)
Quantitative analysis (Fig. 2) showed that proteinuria increased significantly in the PE group at GDs 16 (5150 ± 154 µg/24 h) and 19 (4820 ± 132 µg/24 h) compared with the P group on 16 (2110 ± 204 µg/24 h) and 19 (1900 ± 176 µg/24 h) days after gestation (*P < 0.01); within the PE group, proteinuria was also higher on days 16 and 19 of gestation after LPS administration compared with values on GD14 (2215 ± 175 µg/24 h) (*P < 0.01). Following LPS administration, proteinuria was also increased in the PE + CsA group on GD16 (4775 ± 172 µg/24 h) compared with the P group (#*P < 0.01), and it was lower on GD19 (2400 ± 216 µg/24 h) compared with the PE group (#P < 0.01); within the PE + CsA group, proteinuria was higher on GD16 compared with values on GD14 (2240 ± 194 µg/24 h) (#*P < 0.01), but it decreased significantly on GD19 compared with the value on GD16 (#P < 0.01).
Changes in the mean 24 h proteinuria level in all three groups at 14, 16, and 19 days after gestation. Values are presented as the mean ± SEM. Proteinuria increased significantly in the PE group compared with the P group on 16 and 19 days after gestation (*P < 0.01); within the PE group, proteinuria was also higher on days 17 and 19 of gestation after LPS administration compared with values on GD14 (*P < 0.01). Following LPS administration, proteinuria was also increased in the PE + CsA group on GD16 compared with the P group (#*P < 0.01), and it was lower on GD19 compared with the PE group (#P < 0.01); within the PE + CsA group, proteinuria was higher on day 16 of gestation compared with values on GD14 (#*P < 0.01), but it decreased significantly on day 19 of gestation compared with the value on GD16 (#P < 0.01)
CsA administration reduced seizure severity in pre-eclampsia rats with PTZ treatment
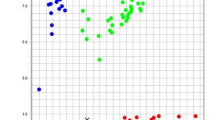
According to methods reported in our previous study, PTZ injection in a rat pre-eclampsia model can be used to establish a rat eclampsia-like model. For the PE group, PTZ injection can quickly induce different stages of seizures. Compared with those in the P + PTZ group, seizure scores significantly increased in the PE + PTZ group (Fig. 3a, *p < 0.01) but were lower in the PE + CsA + PTZ group than the PE + PTZ group (Fig. 3a, #p < 0.01). Compared with the P (119.5 ± 9.34 s) group, the latency to develop stage 1 seizures was significantly higher in the PE + PTZ (12.62 ± 3.77 s) group (Fig. 3b, *p < 0.01). However, CsA treatment increased the latency in the PE + CsA + PTZ (62.8 ± 7.86 s) group compared with the PE + PTZ group (Fig. 3b, #p < 0.01).
CsA administration reduced seizure severity in pre-eclampsia rats with PTZ stimulation. CsA administration decreased seizure severity in eclampsia-like rats. Whisker boxes represent the interquartile distributions. a Compared with those in the P + PTZ group, seizure scores were significantly increased in the PE + PTZ group (*p < 0.01), but they were lower in the PE + CsA + PTZ group than the PE + PTZ group (#p < 0.01). b Compared with the P group, the latency to develop stage 1 seizures was significantly higher in the PE + PTZ group (*p < 0.01). However, CsA pre treatment increased the latency in the PE + CsA + PTZ group compared with the PE + PTZ group (#p < 0.01)
CsA administration inhibited the enhancement of inflammatory cytokine levels in eclampsia-like rats
To detect the effects of CsA on systemic inflammation following eclampsia-like seizures, the concentrations of IL-1β, TNF-α, IL-17, and IL-10 were measured. Compared with those in the P + PTZ (63.50 ± 4.57 pg/mL) group, the IL-1β levels were significantly higher in the PE + PTZ (109.42 ± 3.29 pg/mL) group (*p < 0.01) but were lower in the PE + CsA + PTZ (73.55 ± 3.17 pg/mL) group compared with the PE + PTZ group (Fig. 4a, #p < 0.01). After PTZ stimulation, the TNF-α levels increased significantly in the PE + PTZ (160.22 ± 4.92 pg/mL) group compared with that in the P + PTZ (142.54 ± 3.20 pg/mL) group; after CsA administration, the levels were lower in the PE + CsA + PTZ (135.52 ± 4.14 pg/mL) group than the PE + PTZ group (Fig. 4b, #p < 0.01). The changing tendency of IL-17 levels was similar to that of IL-1β and TNF-α (Fig. 4c). There was also no significant difference in IL-10 levels within each group after PTZ stimulation (Fig. 4d).
CsA administration inhibited the enhancement of inflammatory cytokine levels in eclampsia-like rats. The concentrations of TNF-α and IL-1β were significantly reduced in the PE + PTZ group treated with CsA. a Compared with those in the P + PTZ group, the IL-1β levels were significantly higher in the PE + PTZ group (*p < 0.01) but were lower in the PE + CsA + PTZ group compared with the PE + PTZ group (#p < 0.01). b After PTZ stimulation, the TNF-α levels increased significantly in the PE group compared with that in the P group; following CsA administration (*p < 0.01), the levels were lower in the PE + CsA + PTZ group than the PE + PTZ group (#p < 0.01). c The changing tendency of IL-17 levels was similar to that of TNF-α and IL-1β. d There was also no significant difference in IL-10 levels within each group after PTZ stimulation
CsA administration improved pregnancy outcome in eclampsia-like rats
The numbers of live fetuses and resorptions were not significantly different among the groups. After PTZ stimulation in the PE rats, the fetal weight and placental weight decreased significantly in the PE group compared with the P group (3.7 ± 0.06 g vs. 4.3 ± 0.07 g; 0.44 ± 0.007 g vs. 0.52 ± 0.011 g; *p < 0.05, Table 1). CsA pre treatment significantly increased the fetal weight and placental weight in the PE + CsA group compared with the PE group (3.7 ± 0.06 g vs. 3.9 ± 0.06 g; 0.44 ± 0.007 g vs. 0.49 ± 0.011 g; *p < 0.05, Table 1).
Discussion
In this study, we found that CsA administration significantly alleviated the clinical characteristics of pre-eclampsia, such as SBP and 24 h proteinuria, as our previous research showed. Seizure severity and inflammatory responses were significantly enhanced in the pre-eclampsia group, while these changes were significantly attenuated after CsA administration. Improved pregnancy outcomes occurred in pre-eclampsia rats with PTZ stimulation. Our previous study showed that inflammation increased the susceptibility to seizure activity, while magnesium sulfate decreased proinflammatory mediators and significantly attenuated latency, duration and rate of the PTZ-induced seizure pattern. These studies further support the notion that inflammation modulates the seizure threshold. CsA has been used in the clinic since 1983 and was recently found to have a protective role in pregnancy-related immune inflammatory diseases. We hypothesized that the mechanisms underlying the protective effects of CsA in pre-eclampsia and eclampsia might be mediated through inhibiting systemic inflammation.
Clinical and experimental studies have suggested that successful pregnancy is a Th1-Th2 cooperative phenomenon with a predominantly Th2-type lymphocyte response. The imbalance of Th1 and Th2 cells and the alterations of the prevalence of Th17 with excessive inflammation might be one important cause of pre-eclampsia [19]. The administration of LPS as a model for PE is a classical and typical method that was initially established by Fass et al. PE is a complex disease involving multiple factors, so different methods have been applied to explore the pathogenesis of PE [7,8,9, 20]. The study of abnormal inflammatory responses in PE is important for understanding the immunoregulatory mechanisms of pregnancy, PE, and other diseases related to pregnancy. In fact, in addition to using LPS to induce inflammation in pregnant animals to establish the PE model, researchers used inflammatory factors such as TNF-α and IL-6 to induce models of pre-eclampsia [21, 22]. Moreover, inflammatory Th1-like cells were transferred into pregnant mice and resulted in hypertension and proteinuria [23]. IL-10, originally known as cytokine synthesis inhibitory factor, might inhibit the synthesis of Th1 cytokines. Sharma et al. showed that IL-10 content decreased in cytoplasmic trophoblast villi in PE compared with placenta from normal pregnancy. IL-10 has been identified as an important cytokine in pregnancy and maintenance of pregnancy by corpus-luteum maturation and progesterone production [24]. These studies suggest that inflammation plays an important role in the pathogenesis of pre-eclampsia. CsA can enhance Th2 bias at the maternal-fetal interface in early human pregnancy [14]. In our studies, we demonstrated that CsA can improve pre-eclampsia/eclampsia by decreasing excessive systemic inflammation. CsA might be a new treatment choice for pre-eclampsia/eclampsia. In addition, several studies demonstrated that inhibition of the inflammatory response improved the clinical signs of pre-eclampsia. In the rat model of pregnancy-induced hypertension syndrome, blood pressure was improved by pharmacologically immunosuppressing lymphocytes [25, 26]. However, IL-10 did not significantly change in our study, possibly because of the different models and sample sizes. Our studies showed that CsA significantly decreased both TNF-α, IL-1β, and IL-17 concentrations in LPS-treated pregnant rats, while it also reduced the increased blood pressure and proteinuria level. These results indicated that CsA might be used to manage pre-eclampsia by inhibiting systemic inflammation.
Studies have found that CsA can show neuroprotective effects following prolonged seizure activity, traumatic brain injury, and stroke [16, 27, 28]. In this study, CsA administration reduced the seizure score and prolonged the seizure latency, which resulted in an increasing seizure threshold in this model and manifested as neuroprotective effects. Acute seizure severity and neurocyte death could be ameliorated through treatment with CsA during or after epilepsy [28, 29]. A low dose of CsA treatment also reduced the eclampsia-like seizure severity in the present study. These results implied that CsA might affect the central nervous system and neuronal excitability. Because blood–brain barrier breakdown was observed widely in brain regions during PTZ-induced seizures [30, 31], CsA may directly penetrate into the brain, or CsA could modulate the peripheral cytokines in the BBB, leading to the effects on seizures induced by PTZ. A systemic inflammatory response may affect mitochondrial function. The mitochondrial permeability transition pore (mPTP) is a complex channel of the inner membrane, the opening of which leads to mitochondrial swelling and dissipation of mitochondrial membrane potential. As a result, energy metabolic disorder and insufficient ATP supply reduce neuronal membrane potential and increase neuronal excitability, decreasing the seizure threshold [32]. CsA has been proposed to block mPTP by specific binding to cyclophilin D (CypD). CsA acts by inhibiting the PPIase activity of CypD, resulting in the dissociation of CypD from the adenine nucleotide translocator, which is localized in the inner membrane and acts as a structural component of the mPTP [33]. CsA may play a neuroprotective role by protecting mitochondrial function from the energy metabolic pathway. In further experiments, we will investigate the pathophysiology of how CsA ameliorates eclampsia.
Clinical and neuropathological evidence suggests that inflammation could also play a central role in seizure disorders. Several studies demonstrated the increased levels of inflammatory mediators in the serum of epilepsy patients [34]. Inflammation induced by a low dose of LPS reduced the electrical induction after the discharge threshold in the hippocampus and increased the rate of acquisition of kindling-induced seizures [35]. Vezzani et al. showed that proinflammatory cytokines such as IL-1β and TNF-α can enhance neuronal excitability, initiate spontaneous seizures and were correlated with seizure frequency [36]. A systemic inflammatory response may be involved in the pathogenesis of PE and eclampsia. Eclampsia is seizures caused by elevated neuronal excitability on the basis of pre-eclampsia. In our previous studies, the same methods used in the present study were used to establish the rat pre-eclampsia and eclampsia model. The results revealed that the levels of inflammatory cytokines (TNF-α and IL-1β) were significantly higher in the PE group than in the P group; after PTZ injection, the PE group was more likely to develop seizures [9]. These findings suggest that the inflammatory mechanism may contribute to the susceptibility to seizure activity in pre-eclampsia. Therefore, anti-inflammatory cytokines may ameliorate seizures and modify the underlying pathophysiology of seizures. Our previous study indicated that systemic inflammation had transient or long-term effects on seizure susceptibility by inducing a mirror inflammatory response in the nervous system through microglial activation. Magnesium sulfate and nicotine provide neuroprotection in the eclampsia-like model by ameliorating neuroinflammation [37, 38]. Researchers found that CsA could be used for the treatment of chronic inflammatory diseases, and the mechanism was related to its inhibition of proinflammatory cytokine production [12, 39]. We found that CsA significantly decreased both TNF-α and IL-1β concentrations in pre-eclampsia [8], and the inflammatory cytokine levels increased significantly following eclampsia-like seizure. CsA treatment decreased the severity of eclampsia-like seizure along with the decreasing systemic inflammation in pre-eclampsia and decreased systemic inflammation induced by seizure.
CsA is a commonly used immunosuppressant drug. This drug has been widely used in solid organ and bone marrow transplants to prevent rejection, as well as in the treatment of immune-related disorders such as SLE. Other studies have shown that therapeutic doses of CsA can also be safely applied during pregnancy. More than 70% of women who were treated by CsA after organ transplantation had successful pregnancies and had healthy offspring [40, 41]. The curative effect of CsA on pregnancy associated with SLE and rheumatoid arthritis was positive, and CsA treatment had no significant effect on fetal growth and development [42]. Clinical data suggested that a suitable dose of CsA had satisfactory curative effects and pregnancy outcomes in treating patients. The pregnancy outcomes in matings treated with CsA were improved [43]. The above studies suggested that CsA might provide a new treatment for diseases related to pregnancy. Our previous and present studies revealed that the fetal weight and placental weight decreased following pre-eclampsia and eclampsia, and CsA pre treatment significantly increased these values. All these findings indicated that therapeutic doses of CsA may be used as a new treatment in pre-eclampsia and eclampsia.
Our previous and present studies showed that systemic inflammation increased in pre-eclampsia, and excessive systemic inflammation in pre-eclampsia decreased the seizure threshold in an eclampsia-like model [7]. In addition, systemic inflammation increased significantly following eclampsia-like seizure compared with that in the pre-eclampsia group [7]. CsA administration significantly decreased the severity of eclampsia-like seizure along with the decrease in excessive systemic inflammation. CsA treatment also decreased systemic inflammation induced by eclampsia-like seizures to exert a protective effect. Similar to the clinically relevant anticonvulsant drug magnesium sulfate, CsA can prevent seizure and seizure recurrence. CsA treatment can also reduce the damage caused by seizures. We speculate that CsA might be used not only to prevent but also to treat eclampsia-like seizures. However, future studies are needed to solidify our present results.
Limitations of the study
First, PTZ is a GABA receptor antagonist, and whether GABA receptor dysfunction is implicated in the pathogenesis of eclampsia is unknown; thus, this may be a limitation of a PTZ-induced eclampsia-like model. Second, inflammatory models are classical, and other models will be applied in future research to clarify our present results.
References
Podjarny E, Losonczy G, Baylis C. Animal models of preeclampsia. Semin Nephrol. 2004;24:596–606.
Steegers EA, von Dadelszen P, Duvekot JJ, Pijnenborg R. Pre-eclampsia. Lancet. 2010;376:631–44.
Sargent IL, Germain SJ, Sacks GP, Kumar S, Redman CW. Trophoblast deportation and the maternal inflammatory response in pre-eclampsia. J Reprod Immunol. 2003;59:153–60.
Mihu D, Razvan C, Malutan A, Mihaela C. Evaluation of maternal systemic inflammatory response in preeclampsia. Taiwan J Obstet Gynecol. 2015;54:160–6.
Cotechini T, Graham CH. Aberrant maternal inflammation as a cause of pregnancy complications: A potential therapeutic target? Placenta. 2015;36:960–6.
Cipolla MJ, Pusic AD, Grinberg YY, Chapman AC, Poynter ME, Kraig RP. Pregnant serum induces neuroinflammation and seizure activity via TNFα. Exp Neurol. 2012;234:398–404.
Huang Q, Liu L, Hu B, Di X, Brennecke SP, Liu H. Decreased seizure threshold in an eclampsia-like model induced in pregnant rats with lipopolysaccharide and pentylenetetrazol treatments. PLoS ONE. 2014;9:e89333.
Hu B, Yang J, Huang Q, Bao J, Brennecke SP, Liu H. Cyclosporin A significantly improves preeclampsia signs and suppresses inflammation in a rat model. Cytokine. 2016;81:77–81.
Liu L, Han X, Huang Q, Zhu X, Yang J, Liu H. Increased neuronal seizure activity correlates with excessive systemic inflammation in a rat model of severe preeclampsia. Hypertens Res. 2016;39:701–8.
Domañska-Janik K, Buzañska L, Dłuzniewska J, Kozłowska H, Sarnowska A, Zabłocka B. Neuroprotection by cyclosporin A following transient brain ischemia correlates with the inhibition of the early efflux of cytochrome C to cytoplasm. Brain Res Mol Brain Res. 2004;121:50–59.
Kountouras J, Zavos C, Chatzopoulos D. Immunomodulatory benefits of cyclosporine A in inflammatory bowel disease. J Cell Mol Med. 2004;8:317–28.
Pino-Lagos K, Michea P, Sauma D, Alba A, Morales J, Bono MR, et al. Cyclosporin A-treated dendritic cells may affect the outcome of organ transplantation by decreasing CD4+CD25+ regulatory T cell proliferation. Biol Res. 2010;43:333–7.
Tang C, Chen L, Gu W, Du M, Li M, Chen Q, et al. Cyclosporin A enhances the ability of trophoblasts to displace the activated human umbilical vein endothelial cell monolayers. Int J Clin Exp Pathol. 2013;6:2441–50.
Piao HL, Wang SC, Tao Y, Zhu R, Sun C, Fu Q, et al. Cyclosporine A enhances Th2 bias at the maternal-fetal interface in early human pregnancy with aid of the interaction between maternal and fetal cells. PloS ONE. 2012;7:e45275.
Jung S, Yang H, Kim BS, Chu K, Lee SK, Jeon D. The immunosuppressant cyclosporin A inhibits recurrent seizures in an experimental model of temporal lobe epilepsy. Neurosci Lett. 2012;529:133–8.
Albensi BC, Sullivan PG, Thompson MB, Scheff SW, Mattson MP. Cyclosporin ameliorates traumatic brain-injury-induced alterations of hippocampal synaptic plasticity. Exp Neurol. 2000;162:385–9.
Faas MM, Schuiling GA, Baller JF, Visscher CA, Bakker WW. A new animal model for human preeclampsia: ultra-low-dose endotoxin infusion in pregnant rats. Am J Obstet Gynecol. 1994;171:158–64.
Racine RJ. Modification of seizure activity by electrical stimulation. II. Motor seizure. Electroencephalogr Clin Neurophysiol. 1972;32:281–94.
Ramma W, Ahmed A. Is inflammation the cause of pre-eclampsia? Biochem Soc Trans. 2011;39:1619–27.
Neroli S, Annemarie H, Angela M. Animal models of pre-eclampsia. Am J Reprod Immunol. 2010;65:533–41.
Gadonski G, LaMarca BB, Sullivan E, Bennett W, Chandler D, Granger JP. Hypertension produced by reductions in uterine perfusion in the pregnant rat: role of interleukin 6. Hypertension. 2006;48:711–6.
LaMarca BB, Cockrell K, Sullivan E, Bennett W, Granger JP. Role of endothelin in mediating tumor necrosis factor-induced hypertension in pregnant rats. Hypertension. 2005;46:82–6.
Zenclussen AC, Fest S, Joachim R, Klapp BF, Arck PC. Introducing a mouse model for pre-eclampsia: adoptive transfer of activated Th1 cells leads to pre-eclampsia-like symptoms exclusively in pregnant mice. Eur J Immunol. 2004;34:377–87.
Sharma A, Satyam A, Sharma JB. Leptin, IL-10 and inflammatory markers (TNF-alpha, IL-6 and IL-8) in pre-eclamptic, normotensive pregnant and healthy non-pregnant women. Am J Reprod Immunol. 2007;58:21–30.
Tinsley JH, Chiasson VL, South S, Mahajan A, Mitchell BM. Immunosuppression improves blood pressure and endothelial function in a rat model of pregnancy-induced hypertension. Am J Hypertens. 2009;22:1107–14.
Guzik TJ, Hoch NE, Brown KA, McCann LA, Rahman A, Dikalov S, et al. Role of the T cell in the genesis of angiotensin II induced hypertension and vascular dysfunction. J Exp Med. 2007;204:2449–60.
Borlongan CV, Yu G, Matsukawa N, Xu L, Hess DC, Sanberg PR, et al. Acute functional effects of cyclosporine-A and methylprednisolone treatment in adult rats exposed to transient ischemic stroke. Life Sci. 2005;76:1503–12.
Santos JB, Schauwecker PE. Protection provided by cyclosporin A against excitotoxic neuronal death is genotype dependent. Epilepsia. 2003;44:995–1002.
Setkowicz Z, Ciarach M. Neuroprotectants FK-506 and cyclosporin A ameliorate the course of pilocarpine-induced seizures. Epilepsy Res. 2007;73:151–5.
Ziylan YZ, Ates N. Age-related changes in regional patterns of blood-brain barrier breakdown during epileptiform seizures induced by pentylenetetrazol. Neurosci Lett. 1989;96:179–84.
Asanuma M, Nishibayashi S, Kondo Y, Iwata E, Tsuda M, Ogawa N. Effects of single cyclosporin A pretreatment on pentylenetetrazol-induced convulsion and on TRE-binding activity in the rat brain. Brain Res Mol Brain Res. 1995;33:29–36.
Hardie DG, Ross FA, Hawley SA. Ampk: a nutrient and energy sensor that maintains energy homeostasis. Nat Rev Mol cell Biol. 2012;13:251–62.
Fakharnia F, Khodagholi F, Dargahi L, Ahmadiani A. Prevention of cyclophilin D-mediated mPTP opening using cyclosporine-A alleviates the elevation of necroptosis, autophagy and apoptosis-related markers following global cerebral ischemia-reperfusion. J Mol Neurosci. 2017;61:52–60.
Aronica E, Crino PB. Inflammation in epilepsy: clinical observations. Epilepsia. 2011;52:26–32.
Auvin S, Shin D, Mazarati A, Sankar R. Inflammation induced by LPS enhances epileptogenesis in immature rat and may be partially reversed by IL1RA. Epilepsia. 2010;51:34–38.
Vezzani A, Ravizza T, Balosso S, Aronica E. Glia as a source of cytokines: implications for neuronal excitability and survival. Epilepsia. 2008;49:24–32.
Li X, Han X, Yang J, Bao J, Di X, Zhang G, et al. Magnesium sulfate provides neuroprotection in eclampsia-like seizure model by ameliorating neuroinflammation and brain edema. Mol Neurobiol. 2017;54:7938–48.
Li X, Han X, Bao J, Liu Y, Ye A, Thakur M, et al. Nicotine increases eclampsia-like seizure threshold and attenuates microglial activity in rat hippocampus through the α7 nicotinic acetylcholine receptor. Brain Res. 2016;1642:487–96.
Steiner S, Daniel C, Fischer A, Atreya I, Hirschmann S, Waldner M, et al. Cyclosporine A regulates pro-inflammatory cytokine production in ulcerative colitis. Arch Immunol Ther Exp. 2015;63:53–63.
Coscia LA, Constantinescu S, Moritz MJ, Frank AM, Ramirez CB, Maley WR, et al. Report from the National Transplantation Pregnancy Registry (NTPR): outcomes of pregnancy after transplantation. Clin Transpl. 2010:65–85.
Miniero R, Tardivo I, Curtoni ES, Segoloni GP, La Rocca E, Nino A, et al. Pregnancy after renal transplantation in Italian patients: focus on fetal outcome. J Nephrol. 2002;15:626–32.
Bar OzB, Hackman R, Einarson T, Koren G. Pregnancy outcome after cyclosporine therapy during pregnancy: a meta-analysis. Transplantation. 2001;71:1051–5.
Zhou WH, Dong L, Du MR, Zhu XY, Li DJ. Cyclosporin A improves murine pregnancy outcome in abortion-prone matings: involvement of CD80/86 and CD28/CTLA-4. Reproduction. 2008;135:385–95.
Acknowledgements
The authors thank Lijun Dai and Chengjie Liang from Guangzhou Medical University for their help with the animal experiments. This study was supported by the National Natural Sciences Foundation of China (81871181), the Guangzhou Science and Technology Project (201607010222), and the Guangzhou Institute of Pediatrics/Guangzhou Women and Children’s Medical Center/(YIP-2019-029).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Huang, Q., Hu, B., Han, X. et al. Cyclosporin A ameliorates eclampsia seizure through reducing systemic inflammation in an eclampsia-like rat model. Hypertens Res 43, 263–270 (2020). https://doi.org/10.1038/s41440-019-0387-3
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41440-019-0387-3
This article is cited by
-
Preeclampsia up to date—What’s going on?
Hypertension Research (2023)
-
The preventive effects of aspirin on preeclampsia based on network pharmacology and bioinformatics
Journal of Human Hypertension (2022)
-
The bioflavonoid troxerutin prevents gestational hypertension in mice by inhibiting STAT3 signaling
Hypertension Research (2021)
-
Neurology of Preeclampsia and Related Disorders: an Update in Neuro-obstetrics
Current Pain and Headache Reports (2021)