Abstract
This study aimed to investigate the relationship between cerebral small vessel disease (CSVD) and orthostatic hypotension (OH) using self-measured blood pressure at home in community-dwelling older subjects. Between May 2016 and October 2018, 663 community-dwelling adults aged ≥60 years were enrolled in Shandong, China. CSVD, including white matter hyperintensities (WMHs), lacunes, enlarged Virchow–Robin spaces (EVRS) and microbleeds, was assessed using brain magnetic resonance imaging. After receiving appropriate training, the subjects participated in “home-measured (H)OH” by themselves for three consecutive days. Participants were classified into no-HOH, 1 HOH, and ≥2 HOH episode groups according to the presence of HOH episodes. The WMH volume, WMH-to-total intracranial volume (TIV) ratio, total numbers of lacunes and EVRS, and prevalence of Fazekas scale score ≥2, lacunes, and EVRS were elevated in the 1 and ≥2 HOH episode groups compared with the no-HOH episode group (P < 0.05). The prevalence and total number of microbleeds were significantly higher in the ≥2 HOH episodes group than in the no-HOH and 1 HOH episode groups (P < 0.05). HOH episodes were significantly associated with WMH volume, WMH-to-TIV ratio, and the total numbers of lacunes, EVRS, and microbleeds after adjustment for confounders (P < 0.05). The risks of Fazekas scale score ≥2, lacunes, EVRS, and microbleeds were 2.123-, 1.893-, 2.162-, and 1.656-fold higher in the 1 HOH episode group and 4.910-, 5.359-, 3.048-, and 2.418-fold higher in the ≥2 HOH episodes group, respectively, than those in the no-HOH group. The presence of HOH episodes was an independent risk factor for CSVD in the community-based older population.
Similar content being viewed by others
Introduction
Cerebral small vessel disease (CSVD) is an important age-related pathologic process and manifests as white matter hyperintensities (WMHs), lacunes, enlarged Virchow–Robin spaces (EVRS), and microbleeds on conventional brain magnetic resonance imaging (MRI) [1,2,3]. The prevalence of CSVD has been variably reported, ranging from 5% in subjects aged 50 years to almost 100% in those aged 90 years and older [3,4,5]. There are no significant racial–ethnic, sex, or geographical differences in the prevalence of CSVD [3, 6]. CSVD is responsible for 25–30% of all strokes and ~45% of dementia and global functional decline [3, 7, 8]. Moreover, it will continue to impose higher personal and societal healthcare burdens with the steadily increasing life expectancy worldwide [9].
Although the exact pathogenesis of CSVD is not yet completely elucidated, CSVD is commonly associated with cardiovascular risk factors, such as high blood pressure (BP), diabetes mellitus, dyslipidemia, and aging [3]. High arterial BP (>140/90 mm Hg) has been demonstrated to be the most important modifiable risk factor for CSVD [6]. High average BP levels, as well as excessive BP variability, have been demonstrated to be associated with an increased risk of CSVD [10,11,12]. However, previous studies have shown conflicting results regarding whether CSVD is associated with the variability of the BP response to orthostatism [13,14,15,16].
Orthostatic hypotension (OH) is one of the impaired BP responses to postural change and is defined as sustained reduction ≥20 mmHg in systolic (S)BP or ≥ 10 mm Hg in diastolic (D)BP within 3 min of standing from the supine position [17,18,19,20,21]. Its prevalence has been variably reported as ranging from 5 to 30% in unselected community-dwelling subjects depending on age [21,22,23]. Growing evidence shows that OH is an independent risk factor for cardio- and cerebrovascular events, including heart failure, atrial fibrillation, ischemic stroke, unexplained falls, frailty, syncope, and all-cause mortality [20, 21, 24, 25].
Given the low reproducibility of OH measurement [26,27,28], we used self-measured BP at home (also known as home blood pressure measurement, HBPM) to determine the OH in this study. HBPM has been recommended by varying guidelines as a method for confirming the diagnosis of hypertension and monitoring BP and is expected to become a new model of BP management in the future [29,30,31,32]. This technique eliminates white-coat hypertension and masked hypertension, accurately reflects an individual’s BP level in relatively well-controlled conditions outside the clinical setting and avoids observer and regression dilution biases [29,30,31]. The feasibility and accuracy of home measured OH (HOH) have previously been demonstrated [26, 27].
For the first time, in this study, our main goal was to explore the association of self-measured HOH with CSVD in community-dwelling older subjects.
Methods
Study population
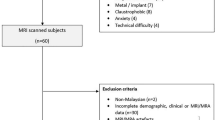
This study used a cross-sectional design and was conducted in compliance with the ethical standards established in the “Declaration of Helsinki”. The data were collected at eight community centers in the Shandong area, China. Between May 2016 and October 2018, 854 older adults aged 60 years and older were screened. Among them, 748 were eligible and willing to take part in this study. The exclusion criteria included symptomatic stroke or transient ischemic attack, Alzheimer disease, Mini-Mental State Examination score ≤ 23 points, Parkinson disease, schizophrenia, seizures, bipolar disorder, claustrophobia, chronic heart failure, chronic renal failure and dialysis treatment, hyper- or hypothyroidism, liver disease, and drug history. Older adults with an inability to stand in an upright position, contraindications to MRI, and an inability to provide informed consent were also excluded.
This study was approved by the Research Ethics Committee of the Institute of Basic Medicine, Shandong Academy of Medical Sciences. Written informed consent was obtained from each individual participant.
Procedure for self-measured blood pressure at home
First, participants and at least one of their relatives were systematically instructed on how to measure their own BP at home by physicians and trained public health nurses. After their HBPM ability was verified, an automatic device [BP3MX1-1, Microlife WatchBP Home; CX Electronic (Shenzhen) Co. Ltd, Shenzhen, Guangdong, China] was loaned out to every participant as a home sphygmomanometer. The device, which incorporates an integrated circuit memory and a clock to store BP readings and measurement times, was validated and fulfilled the criteria of the International Protocol of the European Society of Hypertension [33]. Each step in the HBPM procedure complies with the following protocol: BP was measured three times with a 2-min interval in a sitting position after at least 5 min of sitting rest and followed by one time in a standing position. The measurements were performed for three consecutive days: each morning just after waking and before taking any medication and each evening after dinner.
Determining home orthostatic hypotension
Changes in orthostatic BP were calculated by the differences between the mean of the three BP measurements in the sitting position and the BP measurement in the standing position. HOH was defined by a reduction of ≥20 mmHg in SBP and/or a reduction of ≥10 mmHg in DBP according to the same international guidelines used for clinic OH as described elsewhere [17,18,19,20,21]. The number of OH episodes within the 3 days was recorded and used for analyzes.
Determining brain magnetic resonance imaging markers of cerebral small vessel disease
As previously described [11, 34, 35], MRI markers of CSVD, including WMH, lacunes, EVRS, and microbleeds, were determined using a 3.0-T GE Signa Horizon scanner (Signa Horizon LX; General Electric Medical Systems, Milwaukee, WI) or 3.0-T Siemens Allegra scanner (Siemens Medical, Erlangen, Germany) with uniform MRI protocols. The MRI protocols consisted of T1-weighted 3D magnetization-prepared rapid gradient echo [repetition time (TR) = 1900 ms, echo time (TE) = 3 ms, 1-mm slice thickness with no gap], T2-weighted 3D fast spin-echo (TR = 3000 ms, RE = 98 ms, 3-mm slice thickness with no gap), T2*-weighted gradient-echo type echoplanar (TR = 600 ms, TE = 16 ms, 3-mm slice thickness with no gap), and fluid-attenuated inversion recovery (FLAIR; TR = 5000 ms, TE = 355 ms, 2-mm slice thickness with no gap) sequences.
All scan images were transferred to an offline workstation. The processing and analyzes of scans were rated by experienced neuroradiologists who were blinded to the clinical data of participants. WMH volume was computed automatically from periventricular and subcortical segmentation routines with T2-weighted and FLAIR scans using FreeSurfer. The total WMH volume was the sum of the volume of periventricular and subcortical WMHs. Correction of total WMH was calculated as: WMH-to-TIV (total intracranial volume) ratio (%) = [total WMH (mL)/TIV (mL)] × 100%. Volumetric analysis was performed using the brain extraction tool and FMFIB’s automated segmentation tools from the FSL (FMRIB Software Library; Oxford Center for Functional MR Imaging of the Brain, Oxford, England, www.fmrib.ox.ac.uk/fsl, version 4.19) software package. Moreover, according to the Fazekas rating scale, WMH was visually rated on FLAIR images as none, punctuate caps, early confluent, and confluent (score: 0, 1, 2, and 3, respectively). According to the diagnostic criteria defined in STRIVE v1 [2], lacunes were determined as 3–15 mm cavities in the deep gray or white matter with cerebrospinal fluid-like signals on T1- and T2-weighted and FLAIR images. EVRS was determined as visible fluid-filled spaces adjacent to cerebral vessels and discriminated from the small lacunes of presumed vascular origin on T2-weighted and FLAIR images. Microbleeds were determined as 2–10 mm ovals or round, hypointense, and homogeneous foci in the brain parenchyma and systematically distinguished from mimics of microbleeds, including signal averaging from bone, sulcal vessels, and calcifications on T2*-weighted images. The numbers of lacunes, EVRS, and microbleeds were recorded for each participant. For further analysis, the Fazekas scale was dichotomized as <2 (none and punctuate caps) versus ≥2 (early confluent and confluent) depending on the score. Lacunes, EVRS, and microbleeds were dichotomized as 0 versus ≥1 depending on the numbers, respectively.
We randomly analyzed 65 MRI scans to assess the limited intrarater reliability of the WMH volume and the discernment of the Fazekas scale, lacunes, EVRS, and microbleeds. The intrarater coefficients of variation for WMH volume was 0.93, and the weighted Cohen’s kappa was 0.87 for Fazekas scale lesions, 0.82 for lacunes, 0.80 for EVRS, and 0.81 for microbleeds, indicating good reliability.
Covariates
A clinical visit was conducted to assess covariates for each participant. The data, including age; sex; education; alcohol consumption; smoking; the presence of hypertension, diabetes mellitus, and dyslipidemia; antihypertension, antidiabetic, antidyslipidemic, antiplatelet, and anticoagulant medication (including direct oral anticoagulant and warfarin); weight and height (used to calculate body mass index); clinic SBP and DBP; plasma lipids including total cholesterol, low-density lipoprotein cholesterol (LDL-c), high-density lipoprotein cholesterol (HDL-c), and triglycerides; and fasting plasma glucose (FPG), were collected.
Statistical analysis
Depending on the number of HOH episodes, participants were classified into no-HOH episode, 1 HOH episode, and ≥2 HOH episode groups. Characteristics of the groups were described using the mean ± standard deviation (SD) or the median with interquartile range (IQR) for continuous variables depending on the normality of the data and frequency with percentages for categorical data. The numbers of lacunes, EVRS, and microbleeds are presented as total counts with percentages. The normality of continuous data was determined using the Kolmogorov–Smirnov test. The characteristics of participants among groups were compared using one-way analysis of variance with Bonferroni post hoc test for continuous data with normal distribution, the Kruskal–Wallis H test with Wilcoxon rank-sum test for continuous data with a skewed distribution, and the Chi-square test for categorical data. We performed multiple linear backward stepwise regression analyses to assess the association between the presence of HOH (no-HOH = 0, 1 HOH episode = 1, and ≥2 HOH episodes = 2) and WMH volume and WMH-to-TIV ratio. A model of generalized estimating equations was used to determine the association between the presence of HOH and the numbers of lacunes, EVRS, and microbleeds. The risks of Fazekas scale score ≥2, lacunes, EVRS, and microbleeds (odds ratio) were compared using models of logistic regression among the three groups. The adjustments for covariates in each model were included as described above, such as age, sex, education, alcohol consumption, smoking, disease and medical treatment history, body mass index, clinic SBP and DBP, plasma lipids, FPG, and the changes in home supine-to-orthostatic SBP and DBP. SPSS for Windows (version 24.0; SPSS Inc., Chicago, IL, USA) was used to conduct all statistical analyses. A two-sided P value of <0.05 was considered statistically significant.
Results
Demographic and clinical characteristics of participants
Among 748 eligible participants, 85 were excluded from this study, including 27 due to incomplete assessment of brain MRI and 58 due to unqualified/incomplete data for HBPM. Ultimately, 663 fulfilled the study criteria, and their data were used for analysis. The mean age of the participants was 68.57 ± 5.67 years, and 375 (56.6%) were females. There were 214 (32.3%) participants with 1 HOH episode and 97 (14.6%) with ≥2 HOH episodes. Among them, 96 person-times were symptomatic OH. The main OH symptoms were dizziness and palpitation. The median WMH volume was 2.75 (IQR, 1.93–3.66) mL, and the WMH-to-TIV ratio was 0.21% (IQR, 0.16–0.28%). The prevalence of Fazekas scale score ≥2 was 16.0%, lacunes was 14.6%, EVRS was 13.7%, and microbleeds was 9.5%. The total number of lacunes was 312, EVRS was 407, and microbleeds were 191. There were no significant differences in the demographic and clinical characteristics among the three groups, which were stratified according to the number of HOH episodes (Table 1).
Differences in the characteristics of blood pressure and MRI findings
Table 2 provides detailed characteristics of clinically obtained BP, home BP and markers of CSVD. The differences between clinical SBP and home supine SBP were not significant among the three groups (P > 0.05), even though they were higher in the ≥2 HOH episode group than in the no-HOH episode group. As expected, the home orthostatic SBP and the changes in home supine-to-orthostatic SBP and DBP in the ≥2 HOH episode group were significantly higher than those in the no-HOH and 1 HOH episode groups (P < 0.05). The home orthostatic DBP was significantly higher in the 1 HOH episode and ≥2 HOH episode groups than in the no-HOH episode group (P < 0.05).
From the no-HOH episode group to the ≥2 HOH episode group, the WMH volume (P < 0.001), WMH-to-TIV ratio (P < 0.001), and the total numbers of lacunes (P < 0.001) and EVRS (P < 0.001) were increased, and there were significant differences among the three groups (P < 0.05). Correspondingly, the prevalence of Fazekas scale score ≥2, lacunes, and EVRS increased from the no-HOH episode group to the ≥2 HOH episode group, and there were significant differences between any two groups (P < 0.05). Compared with the no-HOH and 1 HOH episode groups, the prevalence and total number of microbleeds were significantly higher in the ≥2 HOH episode group (P < 0.05).
Factors possibly related to cerebral small vessel disease
First, we performed a multiple linear regression analysis to assess the factors possibly related to WMH volume and WMH-to-TIV ratio (Table 3). The results showed that HOH episodes, age, home SBP, smoking, LDL-c, FPG, and antihypertensive medication were significantly associated with the volume of WMHs (all P < 0.05). HOH episodes, age, home SBP, smoking, FPG, antihypertensive medication, and antidiabetic medication were significantly associated with the volume of WMH (all P < 0.05).
Then, we developed a model of generalized estimating equations to determine the factors that were possibly related to the numbers of lacunes, EVRS, and microbleeds (Table 4). For the number of lacunes, there were statistically significant results for HOH episodes, home SBP, age, and LDL-c. For the number of EVRS, there were significant results for HOH episodes, home SBP, age, FPG, alcohol consumption, and antihypertensive medication. For the number of microbleeds, there were significant results for ≥2 episodes of HOH, age, FPG, heart rate, and antidiabetic medication.
Finally, we used logistic regression analyses to evaluate the contributions of the presence of HOH episodes to the risks of Fazekas scale score ≥2, lacunes, EVRS, and microbleeds. Figure 1 summarizes the results after adjustment for covariates. Compared with the no-HOH episode group, the risks of Fazekas scale score ≥2, lacunes, EVRS, and microbleeds were 2.123-, 1.893-, 2.162-, and 1.656-fold higher in the 1 HOH episode group and 4.910-, 5.359-, 3.048-, and 2.418-fold higher in the ≥2 HOH episode group, respectively.
Discussion
The main findings of this study were that (1) the WMH and total numbers of lacunes, EVRS, and microbleeds were increased with the higher presence of HOH episodes, and (2) a higher presence of HOH episodes occurred with higher prevalences of Fazekas scale score ≥2, lacunes, EVRS, and microbleeds after adjustment for covariates, including the changes in home supine-to-orthostatic SBP and DBP.
The core mechanism underlying CSVD is commonly assumed to be ischemia caused by impaired autoregulation, vasospasm, hypotension, and falling cerebral blood flow [1]. OH is regarded to be strongly associated with autonomic nervous disturbances and results in reduced cerebral blood flow [14, 15, 36]. A study demonstrated that asymptomatic community-dwelling elderly individuals with postural hypotension had more periventricular WMH burden than those without postural hypotension [37]. In older patients with sustained hypertension, Kario et al. reported that OH is related to a higher risk of silent cerebral infarcts [15]. In a prospective cohort of patients with Lewy body disorders, the severity of OH has been suggested to be associated with WMH burden and reduced cerebral blood flow [36].
In this study, we assessed the association of CSVD and the presence of HOH episodes. Consistent with previous studies [13,14,15, 36], we found that the WMH burden and numbers of lacunes, EVRS, and microbleeds were significantly higher in the participants with ≥2 HOH episodes than in those with <2 HOH episodes. Moreover, we found that the risk was up to fivefold higher for Fazekas scale score ≥2 and lacunes, more than threefold higher for EVRS, and twofold higher for microbleeds in the participants with ≥2 HOH episodes compared with those with no HOH episodes. The most important finding was that the presence of HOH episodes was always an independent contributor to the markers of CSVD, even after adjustment for confounders, including the changes in supine-to-orthostatic SBP and DBP.
However, our results were in disagreement with the study conducted by Foster-Dingley et al. [16]. In older patients with discontinuation of antihypertensive treatment, Foster-Dingley et al. [16] found no association between the presence of OH and cerebral vascular damage, including WMH, lacunar infarcts, and microbleeds. The discrepancy between the two studies might result from the differences in the participants and the methods of determining OH. In this study, we used HBPM to determine OH, and the presence of HOH episodes was assessed within 3 continuous days. The participants in our study were older subjects with normal cognitive function in a community-based dwelling, and in Foster-Dingley’s study, they were older patients with mild cognitive deficits using antihypertensive medication. It was demonstrated that hypertension and antihypertensive therapies were significantly associated with the progression of CSVD [1, 38,39,40,41].
Furthermore, we found that the association of the presence of HOH episodes was weaker with microbleeds than with WMH, lacunes, and EVRS. There was no significant difference in the risk of microbleeds between the no and 1 HOH episode groups (odds ratio was 1.656, and 95% confidence interval was 0.891–3.077). These results may be explained by the discrepancies in the specific underlying mechanism among CSVD subtypes, although ischemia is commonly regarded as the core mechanism underlying CSVD, and strong correlations are exhibited among CSVD subtypes [1]. Despite the ischemic mechanism, the hemorrhagic mechanism, including red blood cell leakage from capillaries, amyloid angiopathy, and bleeding vessels, is considered to play an important role in microbleeds [1, 42,43,44]. Cerebral hypoperfusion and hypoxia resulting from OH might induce the dysfunction of cerebral microvasculature, including capillaries, and ultimately, red blood cell leakage from capillaries occurs.
Antihypertensive agents have different characteristics depending on the type. Studies have reported that OH is associated with specific classes of antihypertensive agents, such as alpha blockers, diuretics, and beta blockers [45, 46]. As a result, CSVD may be significantly impacted by these specific classes of antihypertensive agents. In this study, however, we did not find significant differences in participants using these agents among the three groups. Moreover, we included these specific antihypertensive agents as confounders in the models to diminish their impacts on CSVD.
Bleeding is a common side effect of antiplatelet agents and anticoagulants. Cerebral microbleeds are demonstrated to be increased not only by antiplatelet agents but also by anticoagulants [47, 48], although there are reports that direct oral anticoagulants do not increase the risk of cerebral microbleeds [49, 50]. Considering the side effects of bleeding, we analyzed antiplatelet medication and anticoagulants among the three groups. We found that the differences in the antiplatelet medication and anticoagulant use were not significant among the three groups, and their effects on cerebral bleeds were not significant. The causes may be that there were fewer participants using antiplatelet medication and anticoagulants in this study. Only ~3% of participants took anticoagulants, and <15% of participants used antiplatelet medication.
The major strength of this study is that HBPM was used to assess the episodes of OH. It more accurately reflects an individual’s BP level under relatively well-controlled conditions than office BP measurement. The presence of HOH episodes within 3 continuous days was used to group the participants.
However, several limitations in this study should be considered. First, we did not clarify the causal relationship between CSVD and HOH episodes due to the cross-sectional design of this study. Second, the measurement of BP at home by patients themselves, at least to some extent, is not as standardized as measurements done at the office by physicians, even if the feasibility and accuracy of HBPM have previously been demonstrated and the participants were trained to conduct HBPM. Third, we did not consider the time and type of antihypertensive medications, which would influence the occurrence of OH episodes. In addition, we did not consider the differences between morning and evening HOH episodes. The presence of OH episodes may vary during differing times within the day.
In conclusion, our investigation indicated that the presence of HOH episodes was an independent risk factor for CSVD in the community-based older population. HOH monitoring deserves more attention in association with the management of patients with chronic cardio- and cerebrovascular diseases. However, large and longitudinal prospective multiethnic, multinational, and multicenter studies are needed to validate the results and illuminate the causal relationship between CSVD and HOH episodes.
References
Wardlaw JM, Smith C, Dichans M. Mechanisms of sporadic cerebral small vessel disease: insights from neuroimaging. Lancet Neurol. 2013;12:483–97.
Wardlaw JM, Smith EE, Biessels GJ, Cordonnier C, Fazekas F, Frayne R.Standards for ReportIng Vascular changes on nEuroimaging (STRIVE v1). et al. Neuroimaging standards for research into small vessel disease and its contribution to ageing and neurodegeneration. Lancet Neurol.2013;12:822–38.
Cannistraro RJ, Badi M, Eidelman BH, Dickson DW, Middlebrooks EH, Meschia JF. CNS small vessel disease: a clinical review. Neurology. 2019;92:1146–56.
de Leeuw FE, de Groot JC, Achten E, Oudkerk M, Ramos LM, Heijboer R, et al. Prevalence of cerebral white matter lesions in elderly people: a population based magnetic resonance imaging study. The Rotterdam scan study. J Neurol Neurosurg Psychiatry. 2011;70:9–14.
Poels MM, Vernooij MW, Ikram MA, Hofman A, Krestin GP, van der Lugt A, et al. Prevalence and risk factors of cerebral microbleeds: an update of the Rotterdam scan study. Stroke. 2010;41:S103–6.
Hilal S, Mok V, Youn YC, Wong A, Ikram MK, Chen CL. Prevalence, risk factors and consequences of cerebral small vessel disease: data from three Asian countries. J Neurol Neurosurg Psychiatry. 2017;88:669–74.
Hilal S, Baaij LGA, de Groot M, Niessen WJ, Ikram MK, Ikram MA, et al. Prevalence and clinical relevance of diffusion-weighted imaging lesions: the Rotterdam study. Neurology. 2019;93:e1058–67.
Inzitari D, Pracucci G, Poggesi A, Carlucci G, Barkhof F, Chabriat H.LADIS Study Group et al. Changes in white matter as determinant of global functional decline in older independent outpatients: three year follow-up of LADIS (Leukoaraiosis and disability) study cohort. BMJ. 2009;339:b2477.
Goldstein ED, Badi MK, Hasan TF, Lesser ER, Hodge DO, Lin MP, et al. Cerebral small vessel disease burden and all-cause mortality: Mayo clinic florida familial cerebrovascular diseases registry. J Stroke Cerebroavasc Dis. 2019;28:104285.
Havlik RJ, Foley DJ, Sayer B, Masaki K, White L, Launer LJ. Variability in midlife systolic blood pressure is related to late-life white matter lesions: the Honolulu-Asia Aging study. Stroke. 2002;33:26–30.
Zhang H, Cui Y, Zhao Y, Dong Y, Wang J, Duan D, et al. Association of circadian rhythm of blood pressure and cerebral small vessel disease in community-based elderly population. J Gerontol A Biol Sci Med Sci. 2019;74:1322–30.
Liu Z, Zhao Y, Zhang H, Chai Q, Cui Y, Diao Y, et al. Excessive variability in systolic blood pressure that is self-measured at home exacerbates the progression of brain white matter lesions and cognitive impairment in the oldest old. Hypertens Res. 2016;39:245–53.
Matsubayashi K, Okumiya K, Wada T, Osaki Y, Fujisawa M, Doi Y, et al. Postural dysregulation in systolic blood pressure is associated with worsened scoring on neurobehavioral function tests and leukoaraiosis in the older elderly living in a community. Stroke. 1997;28:2169–73.
Soennesyn H, Nilsen DW, Oppedal K, Greve OJ, Beyer MK, Aarsland D. Relationship between orthostatic hypotension and white matter hyperintensity load in older patients with mild dementia. PLoS ONE. 2012;7:e52196.
Kario K, Eguchi K, Hoshide S, Hoshide Y, Umeda Y, Mitsuhashi T, et al. U-curve relationship between orthostatic blood pressure change and silent cerebrovascular disease in elderly hypertensives: orthostatic hypertension as a new cardiovascular risk factor. J Am Coll Cardiol. 2002;40:133–41.
Foster-Dingley JC, Moonen JEF, de Ruijter W, van der Mast RC, van der Grond J. Orthostatic hypotension in older persons is not associated with cognitive functioning, features of cerebral damage or cerebral blood flow. J Hypertens. 2018;36:1201–6.
Consensus statement on the definition of orthostatic hypotension, pure autonomic failure, and multiple system atrophy. The Consensus Committee of the American Autonomic Society and the American Academy of Neurology. Neurololgy. 1996;46:1470.
McNicholas T, Tobin K, Carey D, O’Callaghan S, Kenny RA. Is baseline orthostatic hypotension associated with a decline in global cognitive performance at 4-year follow-up? Data from TILDA (The Irish Longitudinal Study on Ageing). J Am Heart Assoc. 2018;7:e008976.
Suemoto CK, Baena CP, Mill JG, Santos IS, Lotufo PA, Benseñor I. Orthostatic hypotension and cognitive function: cross-results from the ELSA-Brasil study. J Gerontol A Biol Sci Med Sci. 2019;74:358–65.
Peters R, Anstey KJ, Booth A, Beckett N, Warwick J, Antikainen R, et al. Orthostatic hypotension and symptomatic subclinical orthostatic hypotension increase risk of cognitive impairment: an integrated evidence review and analysis of a large older adult hypertensive cohort. Eur Heart J. 2018;39:3135–43.
Ricci F, De Caterina R, Fedorowski A. Orthostatic hypotension: epidemiology, prognosis, and treatment. J Am Coll Cardiol. 2015;66:848–60.
Finucane C, O’Connell MD, Fan CW, Savva GM, Soraghan CJ, Nolan H, et al. Age-related normative changes in phasic orthostatic blood pressure in a large population study: findings from the Irish Longitudinal Study on Ageing (TILDA). Circulation. 2014;130:1780–9.
Xin W, Lin Z, Mi S. Orthostatic hypotension and mortality risk: a meta-analysis of cohort studies. Heart. 2014;100:406–13.
Angelousi A, Girerd N, Benetos A, Frimat L, Gautier S, Weryha G, et al. Association between orthostatic hypotension and cardiovascular risk, cerebrovascular risk, cognitive decline and falls as well as overall mortality: a systematic review and meta-analysis. J Hypertens. 2014;32:1562–71.
Ko D, Preis SR, Lubitz SA, McManus DD, Vasan RS, hamburg NM, et al. Relation of orthostatic hypotension with new-onset atrial fibrillation (from the Framingham Heart Study). Am J Cardiol. 2018;121:596–601.
Cremer A, Rousseau AL, Boulestreau R, Kuntz S, Tzourio C, Gosse P. Screening for orthostatic hypotension using home blood pressure measurements. J Hypertens. 2019;37:923–7.
Cohen A, Vidal JS, Roca F, Rananja H, hernandorena I, Coude du Foresto L, et al. Feasibility and determinants of orthostatic hypotension self-measurement at home in an elderly community-dwelling population. Am J Hypertens. 2019;32:824–32.
Belmin J, Abderrhamane M, Medjahed S, Sibony-Prat J, Bruhat A, Bojic N, et al. Variability of blood pressure response to orthostatism and reproducibility of the diagnosis of orthostatic hypotension in elderly subjects. J Gerontol A Biol Sci Med Sci. 2000;55:M667–71.
Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, et al. List of authors/Task Force members:. 2018 practice guidelines for the management of arterial hypertension of the European Society of Hypertension and the European Society of Cardiology: ESH/ESC Task Force for the Management of Arterial Hypertension. J Hypertens. 2018;36:2284–309.
Whelton PK, Carey RM, Aronow WS, Casey DE Jr, Collins KJ, Dennison Himmelfarb C, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2018;138:e484–594.
Joint Committee for Guideline Revision. 2018 Chinese guidelines for prevention and treatment of hypertension—a report of the revision committee of Chinese Guidelines for Prevention and Treatment of Hypertension. J Geriatr Cardiol. 2019;16:182–241.
Blacher J, Halimi JM, Hanon O, Mourad JJ, Pathak A, Schnebert B.French Society of Hypertension et al. Management of arterial hypetension in adults: 2013 guidelines of the French Society of Arterial Hypertension. Fundam Clin Pharm.2014;28:1–9.
Stergiou GS, Giovas PP, Gkinos CP, Patouras JD. Validation of the Microlife WatchBP Home device for self home blood pressure measurement according to the International Protocol. Blood Press Monit. 2007;12:185–8.
Ji T, Zhao Y, Wang J, Cui Y, Duan D, Chai Q, et al. Effect of low-dose statins and Apolipoprotein E genotype on cerebral small vessel disease in older hypertensive patients: a subgroup analysis of a randomized clinical trial. J Am Med Dir Assoc. 2018;19:995–1002.
Chen Y, Yu H, Zhu J, Zhang H, Zhao Y, Dong Y, et al. Low carotid endothelial shear stress associated with cerebral small vessel disease in an older population: a subgroup analysis of a population-based prospective cohort study. Atherosclerosis. 2019;288:42–50.
Robertson AD, Messner MA, Shirzadi Z, Kleiner-Fisman G, Lee J, Hopyan J, et al. Orthostatic hypotension, cerebral hypoperfusion, and visuospatial deficits in Lewy body disorders. Parkinsonism Relat Disord. 2016;22:80–86.
Longstreth WT Jr, Manolio TA, Arnold A, Burke GL, Bryan N, Jungreis CA, et al. Clinical correlates of white matter findings on cranial magnetic resonance imaging of 3301 elderly people. The Cardiovascular Health Study. Stroke. 1996;27:1274–82.
SPRINT MIND Investgators for the SPRINT Research Group, Nasrallah IM, Pajewski NM, Auchus AP, Chelune G, Cheung AK, et al. Association of intensive vs standard blood pressure control with cerebral white matter lesions. JAMA. 2019;322:524–34.
Zhang H, Cui Y, Zhao Y, Dong Y, Duan D, Wang J, et al. Effects of sartans and low-dose statins on cerebral white matter hyperintensities and cognitive function in older patients with hypertension: a randomized, double-blind and placebo-controlled clinical trial. Hypertens Res. 2019;42:717–29.
Godin O, Tzourio C, Mailard P, Mazoyer B, Dufouil C. Antihypertnsive treatment and change in blood pressure are associated with the progression of white matter lesion volumes: the Three-City (3C)-Dijon Magnetic Resonance Imaging Study. Circulation. 2011;123:266–73.
White WB, Wakefield DB, Moscufo N, Guttmann CRG, Kaplan RF, Bohannon RW, et al. Effects of intensive versus standard ambulatory blood pressure control on cerebrovascular outcomes in older people (INFINITY). Circulation. 2019;140:1626–35.
Kester MI, Goos JD, Teunissen CE, Benedictus MR, Bouwman FH, Wattjes MP, et al. Associations between cerebral small-vessel disease and Alzheimer disease pathology as measured by cerebrospinal fluid biomarkers. JAMA. Neurol 2014;71:855–62.
Greenberg SM, Vernooij MW, Cordonnier C, Viswanathan A, Al-Shahi Salman R, Warach S, et al. Microbleeds Study Group. Cerebral microbleeds: a guide to detection and interpretation. Lancet Neurol. 2009;8:165–74.
Moran C, Phan TG, Srikanth VK. Cerebral small vessel disease: a review of clinical, radiological, and histopathological phenotypes. Int J Stroke. 2012;7:36–46.
Juraschek SP, Appel LJ, Miller ER III, Mukamal KJ, Lipsitz L. Hypertension treatment effects on orthostatic hypotension and its relationship with cardiovascular disease: results from the AASK trial. Hypertension. 2018;72:986–93.
Freeman R, Wieling W, Axelrod FB, Benditt DG, Benarroch E, Biaggioni I, et al. Consensus statement on the definition of orthostatic hypotension, neutrally mediated syncope and the postural tachycardia syndrome. Auto Neurosci. 2011;161:46–48.
Wilson D, Werring DJ. Antithrombotic therapy in patients with cerebral microbleeds. Curr Opin Neurol. 2017;30:38–47.
Cheng Y, Liu J, Zhang S, Li J, Wei C, Wang D, et al. Prior antithrombotic therapy is associated with cerebral microbleeds in ischemic stroke patients with atrial fibrillation and/or rheumatic heart disease. Front Neurol. 2018;9:1184.
Badi MK, Vilanilam GK, Gupta V, Barrett KM, Lesser ER, Cochuyt JJ, et al. Pharmacotherapy for patients with atrial fibrillation and cerebral microbleeds. J Stroke Cerebrovasc Dis. 2019;28:2159–67.
Pan KL, Singer DE, Ovbiagele B, Wu YL, Ahmed MA, Lee M. Effects of non-vitamin K antagonist oral anticoagulants versus warfarin in patients with atrial fibrillation and valvular heart disease: a systematic review and meta-analysis. J Am Heart Assoc. 2017;6:e005835.
Acknowledgements
The authors thank all participants and individuals who offered their assistance to this study.
Funding
This work was supported by the National Natural Science Foundation of China (grant numbers 81670432 and 81973139); Key Technology Research and Development Project of Shandong Province (grant numbers 2018GSF118044, 2017GSF218060, and 2019GSF108079); and The Innovation Project of Shandong Academy of Medical Sciences and Academic Promotion Program of Shandong First Medical University.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Cui, Y., Zhang, H., Zhao, Y. et al. Home-measured orthostatic hypotension associated with cerebral small vessel disease in a community-based older population. Hypertens Res 43, 798–807 (2020). https://doi.org/10.1038/s41440-020-0429-x
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41440-020-0429-x
Keywords
This article is cited by
-
Excessive salt intake accelerates the progression of cerebral small vessel disease in older adults
BMC Geriatrics (2023)
-
Efficacy and safety of Dengyinnaotong Capsule in patients with Cognitive impairment caused by cerebral Small Vessel Disease: study protocol of a multicenter, randomized, open-label, controlled trial (De-CSVD trial)
Trials (2022)
-
Hypertension management to prevent dementia
Hypertension Research (2022)