Abstract
Schlemm’s canal endothelial cells (SECs) serve as the final barrier to aqueous humor (AQH) drainage from the eye. SECs adjust permeability to AQH outflow to modulate intraocular pressure (IOP). The broad identification of IOP-related genes implicates SECs in glaucoma. However, the molecular mechanisms by which SECs sense and respond to pressure changes to regulate fluid permeability and IOP remain largely undefined. We hypothesize that mechano-responsive phosphorylation of the cell adhesion molecule VE-CADHERIN (CDH5) in SECs, by FYN and possibly other SRC family kinases, regulates adherens junction (AJ) permeability to AQH in response to IOP. On experimentally raising IOP in mouse eyes, AJ permeability, CDH5 phosphorylation, and FYN activation at the AJ all increase. FYN null mutant mice display disrupted IOP regulation and reduced AQH outflow. These findings demonstrate an important role of mechanotransducive signaling within SECs in maintaining IOP homeostasis and implicate FYN as a potential target for developing IOP-lowering treatments.
Similar content being viewed by others
Introduction
Schlemm’s canal (SC) has a critical role in aqueous humor (AQH) drainage and intraocular pressure (IOP) homeostasis1,2,3,4 SC is a flattened tube made of endothelial cells encircling the anterior portion of the eye within the tissue of the iridocorneal angle (angle formed by the iris and cornea)2,5,6,7,8. The inner wall of SC is the last barrier to AQH outflow from the eye. The ability of inner wall SECs to rapidly respond to IOP and regulate outflow is expected to be critical in achieving rapid IOP homeostasis. Abnormalities in inner wall biomechanical stiffness are likely to impact homeostatic mechanisms and IOP in glaucoma patients9,10. Despite this importance, the molecular mechanisms controlling AQH outflow through the inner wall SEC barrier are mostly undefined.
The lumen of SC is continuous to the systemic blood circulation. The inner wall of SC must preserve the blood-AQH barrier while being conductive to AQH outflow. The mechanisms underlying these incompatible functions are poorly understood11. Inner wall SECs are morphologically specialized cells that express lymphatic markers like PROX1 and FLT46. These long thin cells experience a basal to apical pressure gradient. These cells and their basement membrane provide the final barrier to AQH drainage from the eye1,2,12. The cellular junctions of SECs are essential for maintaining barrier function.
In addition to maintaining a barrier, the cell junctions also serve as an extracellular outflow route through pores at the cell border (B-pores)3,9,13,14. Flow also occurs through a transcellular route where pressure-modulated intracellular pores (I-pores) in giant vacuoles form in the inner wall SECs to allow AQH outflow9,15. Supporting a role of cell junctions in determining SC permeability and outflow, blockage of intercellular clefts between SC endothelial cells (SECs) by cationic ferritin perfusion reduces outflow16, while knockdown of ZO1 a tight junction-associated protein increases outflow17. However, the effect of ZO1 knockdown on adherens junction was not tested. Inhibiting PTPRB/VEPTP, a junctional receptor tyrosine phosphatase, has been recently shown to increase the outflow of AQH18,19. There is evidence that SC junctions become less complex with the overlap between cells reducing when subjected to increasing pressure20. The molecular mechanisms that generally regulate AQH outflow, specifically through the cell junctions in response to IOP change, remain largely undetermined. Homeostatic mechanotransduction may control the amount of AQH outflow through intracellular and junctional pores.
Details of mechanotransduction in endothelial cells are primarily derived from studies of fluid shear stress responses of blood endothelial cells (BECs). BEC mechanotransducers that elicit flow-dependent responses include the adherens junction complex (AJC), G-protein coupled receptors, caveolae, integrins, the glycocalyx, and the cytoskeleton21. In BECs, the AJC is comprised of the membrane proteins CDH5, PECAM1, and KDR22. CDH5 is the primary junction molecule required to maintain barrier function by promoting homophilic adhesion in vascular endothelium, forming zipper-like AJs at cell contacts. The cytoplasmic CDH5 domain interacts with intracellular proteins (including regulatory protein p120-catenin, β-catenin that links CDH5 with the cytoskeleton), signaling kinases, and receptors.
Mechanical forces on cells activate SRC family kinases (SFKs). Two SFKs, SRC and FYN, are essential activators of mechanoresponses arising from the AJC22,23,24,25,26,27. SFK phosphorylation of CDH5 at key tyrosine residues is required to induce junctional permeability28,29,30,31. Recently, the SFK YES has been shown to regulate the plasticity of AJCs32. SFK-dependent phosphorylation of CDH5 tyrosine 658 and 685 (pY658, pY685-CDH5) in response to shear stress has been demonstrated in vivo in veins30,31. Phosphorylation at Y658 or Y685 induces a dynamic state of the AJ, leading to more permeable junctions in the presence of permeability-inducing agents30,32. CDH5 Y731 is another target of SFKs but is not required for barrier regulation in BECs31. The expression of mutant CDH5s with either Y658F or Y685F phosphorylation-resistant mutations (tyrosine substituted by phenylalanine) prevents the formation of a permeable junction in cell culture and in vivo30,31.
Using mice, extensive whole-mount immunofluorescence imaging, and physiological methods, we show that SFK-mediated site-specific phosphorylation of CDH5 at SEC adherens junctions (AJs) regulates AQH outflow and IOP. SEC AJs were lined with CDH5 and associated cytoplasmic catenin partners. The amount of lectin flow tracer at the cell junctions (marked by CDH5) increased with increasing IOP, indicating increased junctional permeability. The increased junctional permeability correlated with increased pY658-CDH5 and activated SFK at the SEC adherens junction. FYN but not SRC is expressed in SECs, and the absence of FYN resulted in the loss of Y658 and Y685 CDH5 phosphorylation. Dysregulation of AQH drainage and IOP occurs in Fyn KO mice. These results indicate a role for FYN in controlling IOP and AQH outflow by controlling AJ permeability in the SEC.
Results
SECs have continuous cell junctions with CDH5 and CDH5-binding catenin proteins
CDH5 and CDH5-binding proteins play a critical role in maintaining the barrier function of the AJ. These proteins also regulate AJ permeability in BECs29,33. We have previously shown that CDH5 is present at the cell junctions of SC’s inner and outer walls6,34 (see Supplementary Fig. 1 for location of SC in the mouse eye in the context of other CDH5-expressing vessels). The robust almost continuous presence of CDH5 marks the inner wall AJs of the SC in the eyes of a Prox1-GFP mouse (Top panels, Fig. 1, Prox1 is an SC marker that is most robustly expressed in the inner wall, also Supplementary Fig. 1C)6,35,36. We find here that both p120-catenin and β-catenin (middle panels and bottom panels, Fig. 1), which bind specific cytoplasmic domains of CDH5 and regulate CDH5 adhesivity, are co-expressed at the AJ of SECs. These results indicate that SECs have an AJ like that of BECs.
CDH5 and associated cytoplasmic proteins in SC cells. Top, CDH5 decorates cell junctions of the SC. SC labeled with Prox1-GFP (yellow) and CDH5 (magenta). Middle, CDH5 labeled cell junction contains CDH5 associated proteins p120-catenin. Bottom, β-catenin localizes to cell junctions of SC along with CDH5. N = 4 eyes each. Arrows show points that are same in the CDH5 panel and p120-catenin or β-catenin panel. The SC is demarcated by the dashed white line in middle and bottom panels. Scale bar, 10 µm.
The permeability of SEC AJs increases with increasing IOP
Next, we determined if the AJs of SECs became more permeable in response to IOP elevation. We designed a protocol to perfuse Prox1-GFP mouse eyes in vivo with fluorescent GS lectin at set pressures (16 mmHg, 25 mmHg, 45 mmHg) with rapid fixation of intact eyes at the set pressure using acrolein (Fig. 2A). The GS lectin binds terminal, nonreducing α- and β-N-acetyl-D-glucosaminyl (GlcNAc) residues of glycoproteins, thus serving as stable marker for the path of AQH flow. We marked the AJ in anterior segment whole-mounts using CDH5 immunofluorescence. By confocal microscopy, we sampled ~44% of the SC at high resolution (sixteen 246 µm x 246 µm tiles at 63x to cover 4 mm of the diameter of SC in each eye, n = 6 eyes). The images were deconvolved, and the amount of lectin colocalizing with the junctions was calculated (Fig. 2B and C, 2). The colocalization analysis was vital because the bulk of the lectin is found in the trabecular meshwork and complicates analysis without colocalization. Compared to 16 mmHg IOP, we observed a 3.6-fold and 5-fold increase in lectin fluorescence at the AJ at 25 and 45 mmHg, respectively. Thus, AJ permeability in the inner wall of SC increases with increasing IOP.
A. Experimental scheme, B. Prox1-GFP eyes perfused with lectin at 16, 25 or 45 mmHg. Top panels, SC’s inner wall showing CDH5 and lectin (Lec) labeling, Bottom panels, colocalization of CDH5 and lectin at the AJ. Supplementary Fig. 1 shows all proteins imaged separately. Cyan dashed lines show the direction of flow of tracer into the plane of view (borrowed from organic chemistry depiction of bond direction into paper or screen). C. Quantification of lectin-CDH5 colocalization within the inner wall of SC in eyes perfused at 16 mmHg (mean ± SD, 5.3 ± 2.1 %), 25 mmHg (mean ± SD, 19.1 ± 7%) and 45 mmHg (mean ± SD, 26.9 ± 9.3%). Each of the 96 points represents data for the entire width of a 246 µm lengths of SC from each quadrant (4 tiles per quadrant x 4 quadrants x 6 eyes) at each pressure. One-way ANOVA results, F (2285) = 244.3, p = 1.6 × 10−62. Horizontal line in violin plot is the median and vertical bar the 95%CI. Scale, 25 µm.
Destabilizing phosphorylation of CDH5 Y658 residue with increasing IOP
Phosphorylation of CDH5 at key tyrosine residues destabilizes junctional interactions and is required for induction of junctional permeability28,29,30,31. Phosphorylation of CDH5 tyrosine, pY658 and pY685, in response to shear stress occurs in vivo in veins30,31. Given that SC originates from veins6,37, it is likely that the AJ permeability in SEC results from phosphorylation of Y658 and Y685 in the CDH5 cytoplasmic domain.
To determine if IOP elevation resulted in phosphorylation of pY658 and pY685, we clamped IOP in living mice at 16 mmHg, 25 mmHg, or 45 mmHg for 45 min and then rapidly fixed the eyes in situ under pressure (Fig. 3A). We determined the extent of CDH5 tyrosine phosphorylation at Y658 and Y685 in the SC using phospho-specific antibodies on whole-mounts30. We used an immunofluorescence approach because the limbal tissue has other blood and lymphatic vessels expressing CDH5 (Supplementary Fig. 1C), and due to its small size, we cannot isolate CDH5 exclusively from the SC for Western blots. We analyzed the amount of phospho-CDH5 colocalized with the AJ labeled using a CDH5 antibody and sampling about 44% of SC (as above). Compared to 16 mmHg, AJ CDH5 phosphorylation increased 1.4-fold at Y658 (indicated as pY658) at 25 mmHg and 3.6-fold at 45 mmHg (Fig. 3B, C, Supplementary Fig. 3). In contrast, in the same time frame, pY685 was detected at the AJ at 16 mmHg but was significantly decreased at higher IOP, suggesting dephosphorylation of pY685 at 25 mmHg and 45 mmHg (Fig. 4). These results show that IOP elevation results in the phospho-regulation of AJ resident CDH5 at Y658 and Y685.
A Experimental scheme, B Prox1-GFP eye pressure clamped at 16 mmHg, 25 mmHg, or 45 mmHg. a–c the inner wall of SC with GFP and CDH5 labeling, and a’-c’ colocalization of pY658-CDH5 and CDH5 at cell-cell junctions at the indicated pressure. C. Quantification of pYCDH5-CDH5 colocalization within the inner wall of SC in eyes perfused at 16 mmHg (mean ± SD, 7.8 ± 2.2 %), 25 mmHg (mean ± SD, 14 ± 2.4%) and 45 mmHg (mean ± SD, 28 ± 4.6%). Each of the 96 points represents data from a 246 µm length of SC at each pressure (4 tiles per quadrant x 4 quadrants x 6 eyes. One-way ANOVA results, F (2,285) = 946.71, p = 1.3 × 10−126. Horizontal line in violin plot is the median and vertical bar the 95%CI. Fig S2 shows all proteins visualized as individual channels. Scale, 20 µm.
A Prox1-GFP eye pressure clamped at 16 mmHg, 25 mmHg, and 45 mmHg. a-c, inner wall of SC showing GFP and CDH5 labeling, a’-c’ CDH5 and a”-c” localization of pY658-CDH5 at cell-cell junctions at the indicated pressure. B Quantification of pYCDH5-CDH5 colocalization within the inner wall of SC in eyes perfused at 16 mmHg (mean ± SD. = 40.4 ± 3.4 %), 25 mmHg (mean ± SD. = 9.6 ± 2.6%) and 45 mmHg (mean ± SD = 2.6 ± 0.92%). Each of the 96 points represents data from a 246 µm length of SC from each quadrant (4 tiles per quadrant x 4 quadrants x 6 eyes) at each pressure. One-way ANOVA results, F (2,285) = 6094.9, p = 1.4 × 10−234. Scale, 20 µm.
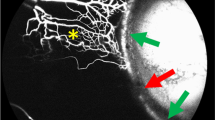
Increasing IOP activates SFKs at SEC inner wall AJs
SFKs phosphorylate tyrosine residues in the CDH5 cytoplasmic domain. SFK-dependent phosphorylation of CDH5 Y658 and Y685) is demonstrated in response to shear stress in vivo in veins30,31. Therefore, SFKs are strong candidates to phosphorylate CDH5 at AJs in the inner wall of Schlemm’s canal. SFKs activation occurs upon phosphorylation at SFK Y41838,39. To assess SFK activation at cell junctions in the inner wall of SC, we determined the levels of activated (phosphorylated) SFK at different pressures by immunostaining with a pan SFK, pY418 specific antibody40,41 (Fig. 5). We elevated IOP in mouse eyes and rapidly fixed eyes under pressure, prepared whole-mounts, and immunostained for pY418-SFK and CDH5 (Fig. 5A). With increasing IOP, the pY418-SFK signal increased at SC inner wall cell junctions (Fig. 5B and C). Compared to 16 mmHg, SFK activation increased 2.9-fold at 25 mmHg and 3.7-fold at 45 mmHg. Thus, an increase in IOP results in an increase in SFK activation.
A Experimental scheme, B Prox1-GFP eye pressure clamped as indicated. a-c, the inner wall of SC showing GFP and CDH5 labeling, and a’-c’ colocalization of pY418-SFK and CDH5 at cell-cell junctions. C Quantification of pYCDH5-CDH5 colocalization within the inner wall of SC in perfused eyes (Pressure, mean ± SD; 16 mmHg,7 ± 2.3%, 25 mmHg, 20.4 ± 2.9%; and 45 mmHg, 26.5 ± 2.8%. Each of the 96 points as in previous figures. One way ANOVA results, F (2285) = 1346.2, p = 6.2 × 10−146. Horizontal line in violin plot is the median and vertical bar the 95%CI. Scale, 20 µm.
FYN is expressed in SECs
Two SFK’s, SRC and FYN, are established to phosphorylate tyrosine residues in the cytoplasmic domain of CDH528,30,42,43. By analyzing our recently generated single-cell sequencing data for limbal tissue, we show that Fyn is expressed in SECs (including inner wall SECs) while Src is not and confirmed this by IHC of anterior segment whole mounts (Fig. 6, Supplementary Fig. 4)44. This agrees with data provided in a recent, single cell sequencing analysis45. Bulk RNA sequencing of isolated SECs also confirms the absence of SRC in SECs45. The SFK YES is also found in SECs but could not be confirmed using an antibody by immunofluorescence (Supplementary Fig. 5). This inability to localize YES in SECs is explained by the fact its expression at RNA level is 24-fold lower than FYN based on bulk RNA sequencing45. Since FYN is the predominantly expressed SFK in SC by both RNA and protein level, we continued to determine the requirement of FYN for normal IOP regulation.
A Feature plot representation of limbal endothelial cells obtained from single cell RNA sequencing shows Fyn but not Src is expressed in the Prox1 expressing SECs. Fyn also localizes to blood endothelial cells in contrast to Src. B XZ confocal sections of Prox1-GFP (yellow) eyes encompassing SC and TM show that FYN localizes (magenta, left) predominantly to the SC while SRC (magenta, right) localizes predominantly to the TM. Inner wall (IW) and outer wall (OW) are labeled. The gray line marks the border between SC IW and TM in first and second panels. XZ optical sections were sliced along the section of XY shown in Fig S4. N = 4 eyes. Scale, 20 µm.
FYN phosphorylates CDH5 in the inner wall of SC
To find the functional role of FYN in the SC we determined the effects of loss of FYN in mice at a molecular and physiological level. We started by immunostaining with a CDH5 antibody. The general morphology of SC in FYN mutant (Fyn−/−) mice was indistinguishable from SC in control (WT) mice (Fig. 7A). At a light microscopy level, the iridocorneal angle of the WT and Fyn−/− appear similar (Supplementary Fig. 6). At an ultrastructure level, electron microscopy showed that the SC cell junctions and TM looked similar in WT and FYN mice (Supplementary Fig. 7). Next, we determined if the loss of FYN resulted in changes to the phosphorylation pattern of CDH5. We performed immunoblotting on lysates obtained from limbal strips of wild type and FYN null eyes (Fig. 7B and Supplementary Fig. 8). Our results from two independent experiments show that, FYN, as predicted, was absent in FYN null mice but present in controls with a Western. blot band close to the expected size of 59-kDa (Fig. 7B and Supplementary Fig. 8). CDH5 expression is at similar levels in control and FYN null mice (Fig. 7B and Supplementary Fig. 8). pY658-CDH5- band was <90% of the intensity of the control band after normalization of band intensity to GAPDH levels. pY685-CDH5 was almost wholly absent in mutants ( < 98% reduction). The basal level of SFK activation indicator pY418-SFK was also reduced by <72 % in the FYN null lysate. This indicates that in the limbus CDH5 phosphorylation is predominantly mediated by activated FYN and not activated YES. We are unable to determine the spatial location of the changes in phosphorylation using immunoblotting of limbal strip lysate due to presence of blood and lymphatic vessels in addition to the SC all of which express CDH5 (Supplementary Fig. 1C). Immunofluorescence showed the loss of pY658 and pY685-CDH5 at AJ in SEC. Activation of SFKs, as judged by pY418SRC phosphorylation, was reduced in the Fyn mutant SC. These results show that FYN is the primary SFK responsible for phosphorylating CDH5 in the inner wall of SC.
A Loss FYN does not affect the gross SC morphology, N = 6 eyes. B Comparison of WT and Fyn-/- limbal strip lysates (pool of 6 eyes) by immunoblotting shows the reduction of pY658-CDH5 and pY418-SFK levels with loss of FYN. Antibodies used for immunoblotting are shown to the left of the blots under the heading IB. pY658-CDH5 in control was represented by a single band around the expected 120-KDa size. A faint doublet band was present in the FYN null that was slightly larger and slightly smaller than the pY658-CDH5 band in WT. Two independent immunoblot experiments were performed. C FYN null SC shows loss of phosphorylated CDH5 and activated SRC. pY658-CDH5 (left), pY685-CDH5 (middle), and pY418-SFK (right), Phosphoproteins are shown in cyan and CDH5 in magenta. N = 3 eyes for each genotype and antibody. Scale, A, 50 µm and C, Scale, 20 µm.
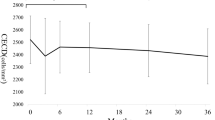
FYN null mice have dysregulated AQH outflow and IOP
To determine the functional role of FYN in AQH drainage and IOP regulation, we measured IOP and determined outflow facility (AQH flow out of the eye nl/min/mmHg), the standard measure of resistance to AQH drainage (Fig. 8). FYN mutants have a dysregulation of IOP with an increased spread of values in each direction. Given this spread, we calculated the variance (VAR) and mean absolute deviation (MAD, see methods). We found that IOP in FYN null eyes showed increased variance (VAR = 7, MAD = 1.86) with a range that was 4.4-fold greater than that of controls (VAR = 1.6, MAD = 1.06) (Fig. 8A). A Levene’s test was performed which showed that the MADs were significantly different (F = 49.8 p = 1.63x10-11). There is a significant elevation of IOP in FYN mutants when comparing the third quartiles (Q3-75th percentile; WT-14.4 ± 0.3 mmHg vs FYN-14.7 ± 0.5 mmHg, p = 0.005) or fourth quartile (Q4->75th percentile; WT-15.5 ± 0.3 mmHg vs FYN-17 ± 1 mmHg, p = 8.2x10−11)) of each genotype. IOP was marginally reduced in the second quartile (Q2-50th percentile; WT-13.3 ± 0.26 mmHg vs FYN-13.2 ± 0.4 mmHg, p = 0.04). Comparing the first quartile to each other, IOP was significantly lower (Q1-25th percentile; WT-12.2 ± 0.3 mmHg vs FYN-10.4 ± 1.5 mmHg, p = 7.4x10−9) (Fig. 8A).The dysregulation of IOP with changes in each direction resembles the spread in IOP values often detected in mice with mutations in various genes that increase IOP and induce glaucoma46,47,48. This spread is not well understood but typically starts at ages when high IOP first becomes elevated and likely reflects abnormalities in diurnal and homeostatic control that result from the IOP elevating effects of increased resistance to aqueous humor outflow48. IOP changes did not correlate with age for WT mice and had a weak correlation for FYN null mice (Supplementary Fig. 9A). These results show that the FYN mutation resulted in a profound dysregulation of IOP consistent with increased resistance to aqueous humor outflow.
Plots show individual data points, colored as indicated on the panels to reflect the quartiles they belong to (25th, 50th, 75th, and > 75th percentile) along with the p-value significance (*) of t-test comparing each quartile means. An overlying notched box plot for overall data shows the median (center line), 1st quartile (25 percentile-bottom bound of box), and 3rd quartile (75th percentile-top bound of the box), the tips of the whiskers represent the minimum and maximum values and the distance between the notches indicate a 95% confidence interval of the median. A IOP is dysregulated in eyes of Fyn-/- mice. The variance of IOP data for FYN null eyes was 4.4-fold that of control (7 vs 1.6) reflecting the dysregulation of IOP, N = 138 eyes. 35 female and 34 male mice of 4-20 months of age. B Fyn-/- mice have reduced aqueous humor outflow facility, C In vivo outflow facility measurements: WT = 4.44 ± 1.7and Fyn-/- = 2.75 ± 1.7, p = 2.2 x 10-6, (mean ± SD) N = 52 eyes, 13 female and 13 male mice of 4-20 months of age. Two-sided t-test was used as the statistical test.
Unlike IOP, the outflow facility is a direct measure of the effect of the mutation on the resistance to AQH drainage at the level of TM/SC. Its measurement is subject to fewer homeostatic mechanisms than IOP as it is not dependent on the rate of AQH humor production and is free from factors that act to regulate IOP at sites away from the drainage structures. AQH outflow facility was significantly lower in FYN null eyes compared to wild type overall (Fig. 8B, quartiles are color coded, WT = 4.4 ± 1.7 and Fyn-/- = 2.75 ± 1.7 nl/min/mmHg, p = 2.2x10-6) and for each quartile comparison (Q1-25th percentile, WT = 2.92 ± 0.5 vs. Fyn-/- 0.8 ± 0.4 nl/min/mmHg, p = 3.8 x 10−12, Q2-50th percentile, 3.7 ± 0.14 vs. 2.2 ± 0.3 nl/min/mmHg, p = 5.8 x 10−10, Q3-75th percentile, 4.4 ± 0.3 vs. 3.1 ± 0.3 nl/min/mmHg, p = 4.6 x 10−11 and, Q4->75th percentile, 6.7 ± 1.6 vs. 5 ± 1.1 nl/min/mmHg, p = 0.005, mean ± SD and p-value shown). Outflow changes only very weakly correlated with age (Supplementary Fig. 9B). These data demonstrate that FYN is a crucial regulator determining the resistance to aqueous humor drainage.
In summary, our data show that the SFK FYN regulates IOP and AQH outflow by impacting the equilibrium between tyrosine phosphorylation and dephosphorylation of CDH5 at AJs in the inner wall of SC. Normal regulation of IOP requires FYN function. We propose a model showing the effect of IOP elevation on the AJC in Fig. 9.
Based on the data presented in this paper, we propose a model where the elevation of IOP changes the AJ from a “closed” configuration (closed AJ) to an open configuration (open AJ) to mediate lowering of IOP. This configuration change is hypothesized to result from the loosening of interaction of the AJ adhesion protein CDH5 on adjacent SECs. The loosening of AJ results from phosphorylation of amino acids Y658 and possibly Y685 of its cytoplasmic tail by FYN which is activated by IOP elevation. The open and closed states are in a dynamic equilibrium modulated by changing IOP.
Discussion
This study shows the requirement for the SFK FYN in IOP regulation. FYN responds to IOP elevation by phosphorylating specific residues in CDH5’s cytoplasmic tail, which regulates SC permeability to AQH. Our data demonstrate that FYN is a crucial regulator determining the resistance to AQH drainage within the inner wall of SC. This inner wall function is pertinent as the mechanisms controlling this resistance are not clearly defined and because of the debate regarding where the key site(s) of resistance lie: within either the trabecular meshwork, SC, or possibly distal blood vessels to which SC connects3,49,50. Our data clearly implicate the inner wall of SC as at least partially contributing to this resistance. These findings are important for understanding IOP regulation and have direct clinical relevance for developing IOP-lowering treatments to combat glaucoma, a widespread neurodegenerative disease for which IOP lowering is the standard of care.
The inner wall of SC must function as a blood-AQH barrier and be permeable to AQH outflow in response to pressure. The AJ is vital in maintaining barrier function in veins51, and SC is venous-derived6. SC cells must sense IOP changes and, in a highly regulated manner, become permeable to AQH outflow so as not to lose their barrier function. How this is accomplished is still largely unclear. In addition to a physical barrier, the AJ complex (consisting of CDH5, PECAM1, and KDR) also functions as a mechanosensor in BECs22. SFKs are critical in this mechanosensing function22. Thus, AJs in SC could function as both sensors of pressure-dependent mechano-stimuli and responders that rapidly modulate local permeability. Such a self-contained system would allow for rapid, dynamic, local responses without compromising barrier function. The AJs of SC, thus, are strong candidates for regulating outflow.
Our study is the first to show a functional role for the AJ in SC, particularly the essential AJ adhesion protein (CDH5) in regulating IOP. CDH5 is required for blood vessels and lymphatics to develop correctly52,53,54 and is central in controlling vascular permeability in these tissues53,54. CDH5 is also required for the formation of tight junctions and AJ and TJ components are known to interact55. Thus, disruptive effect of ZO1 knockdown in SC could also be explained by the disruption of AJ for which there is precedence in embryonic vessels56. Our data add SC to this list of vessels, but further experiments are needed to fully understand the roles of CDH5 in SC and its total contribution to outflow resistance (including the specific deletion of CDH5 in SECs)54,57.
For SECs, phosphorylation at Y658 and Y685 was present at “normal IOP” (16 mmHg) with a marked increase of SFK activation and Y658 phosphorylation with increasing IOP. In contrast, phosphorylation at Y685 was detected only at 16 mmHg. This finding agrees with the observation that pY658 and pY685-CDH5 are present at basal levels in the veins and showed altered levels in response to permeability-inducing substances like bradykinin30,58. However, our finding contrasts another study showing increased Y685 phosphorylation upon increasing vascular permeability through VEGF or histamine treatment (with pronounced vascular leakage)31. These differences may be due to differences in a cellular context or other experimental conditions30,31.The kinetics of phosphorylation of Y658 and Y685 seems to vary with the biological system studied and the stimulus that induces phosphorylation30,31,59. In SECs, it is also possible that phosphorylation of one of the tyrosines (e.g., pY658)60 reflects the mechanosensor function of AJ and the phosphorylation of the other (pY685) mediates the response to the IOP mechano-stimulus i.e., to increase junctional permeability. Future studies are needed to further define the role of site-specific CDH5 phosphorylation(s) in regulating SC permeability and aqueous humor outflow, including the generation and use of mice with point mutations that abrogate phosphorylation at key residues31.
Alterations of junctional permeability following phosphorylation of CDH5 at Y658, and Y685 in SECs could result from 1) The loss of p120-catenin binding. Phosphorylation of pY658, which is within the p120-catenin binding site, reduces the binding of p120-catenin and adhesivity of CDH5 junctions60,61,62. However, this loss of binding of p120-catenin to pY658 CDH5 has not been demonstrated in BEC in vivo in mice or in SC by us in this study. To correlate an association or lack therefore of p120 catenin with pY658 CDH5 in SECs with degrees of AJ permeability, real-time determination of p120-catenin binding to CDH5 along with the use a tracer to monitor changes in permeability will be needed. 2) The endocytosis of the phosphorylated CDH5. We could not see a dramatic increase in levels of cytoplasmic CDH5 signal in most cells with the antibodies that we used. However, if sub-micron scale regions showed rapid endocytosis and recycling, we would not have detected the event. These possible mechanisms are currently experimentally inaccessible due to the limitations of technologies. In addition, compared to BECs, SECs could have a different phosphorylation threshold at which the junctions become permeable due to their unique molecular phenotype6.
Regardless of the mechanism of permeability induction at the SEC AJ, an essential requirement is that SC’s barrier function is not compromised. One way to accomplish this is rapidly turning off phosphorylation events by a cognate phosphatase. pY658 and pY685 in CDH5 are targets of PTPRB/VE-PTP30,31. PTPRB is active in SEC18,63). The loss of pY685 could result from PTPRB activation. In a real-world scenario, this is an attractive mechanism as the phosphorylation of CDH5 serves as a rapid on-off switch to control AJ permeability preventing catastrophic loss of barrier function in response to rapid changes in IOP.
The SFKs SRC, FYN, and YES are important activators of mechanoresponses arising from the AJC22,23,24,25,26,32. Based on sc-RNA and bulk-sequencing results44 and our current data, FYN and YES are expressed in SECs but SRC is not. YES, does not rescue the detrimental effects on IOP and AQH outflow caused by the loss of FYN. Together, these results indicate that FYN is essential in controlling AQH physiology. Mechanical forces on cells such as shear stress and strain can activate SFKs22,64,65. AJ mechanoresponses to shear stress can activate SFK downstream of the mechanosensor PECAM122. The biomechanics of the AQH drainage pathway offers some insight when considering our data. SC lumen narrows upon IOP elevation, increasing the shear stress on SECs. In contrast, TM expands with a concomitant reduction of shear stress on TM cells66,67,68. Thus, SFK activation in SC could result from changes in shear stress. SFKs can be activated rapidly ( < 0.3 s) by the mechanical strain as occurs in cultured cells subjected to rapid deformation of the actin and microtubule cytoskeleton24,69. The deformation of the cytoskeleton of the long thin SEC when subjected to mechanical strain, resulting from IOP elevation, could thus result in an SFK activating event. Other possible mechanisms of SFK activation are: 1) Activation of integrins as a result of IOP elevation-related mechanical stimuli70,71, 2) Disruption of caveolae through mechanical stretching of the cell membrane, which can cause the release of SFKs from caveolin resulting in activation of SFKs69,72,73,74. Caveolin modulates IOP, and SNPs within CAV1 are associated with human glaucoma75,76,77. 3) SFKs can be activated by KDR29, which in turn can be activated in SECs by VEGF secreted in response to the mechanical strain experienced by trabecular meshwork (TM) cells78,79. IOP elevation thus could activate SFKs in multiple ways.
One limitation of our study is that the FYN mutant mice had a body-wide knockout. Although we have shown the regulation of SC AJs by FYN and can explain the effects of the FYN mutation on IOP and outflow physiology, we cannot rule out at least a partial role for FYN in the TM (it is expressed in some TM cells, albeit at a lower level) or distal vasculature. Further measurements of IOP and AQH facility after SEC-specific knockout of FYN is needed to confirm a role solely in SECs. The role of SFKs in the TM and their contribution to IOP regulation remains to be determined. In addition, more work needs to be done to understand integration of other mechanisms, such as the NOS3/ NO and TIE2/ANGPT, with the FYN mediated pathway in regulating AQH outflow.
In conclusion, we have found an IOP-stimulus-induced activation of FYN that regulates the permeability of the AJ by phosphorylation of CDH5. These results suggest potential targets for treating elevated IOP, including the SFK(s) and phosphatases (e.g., PTPRB) that regulate the phosphorylation states of CDH5 at the SEC AJ.
Methods
Mouse strain, breeding, and husbandry
This study was performed per the guidelines in the Guide for the Care and Use of Laboratory Animals of the National Institutes of Health. All the animals were handled according to approved institutional animal care and use committee (IACUC) protocols (#99108, #21016) of The Jackson Laboratory or Columbia University (AABE9554). In addition, all experiments were conducted in accordance with the Association for Research in Vision and Ophthalmology’s statement on the use of animals in ophthalmic research. All mice were housed in a 14-h light to 10-h dark cycle under previously described conditions80. Institutional Animal Care and Use Committee approved all procedures described here. After backcrossing to C57BL/6 J (B6) 10 generation, the following transgenic and knockout mice were used: B6.Prox1-GFP – the mouse line was originally made as a part of GENSAT program-sperm was obtained from MMRC and the mice were rederived at The Jackson Laboratory and backcrossed to C57BL/6 J for >10 generations, B6. Fyn tm1 Sor/JSj (from Jackson Laboratory Stock no. 012468)81, B6. Src tm1 Sor/JSj (from Jackson Laboratory Stock no. 002277)82.
Immunofluorescence on Anterior Eye-Cups
Immunofluorescence on anterior eye segments was done as described in an earlier study6. Briefly, anterior eye-cups from 4–6 month old mice were dissected and four centripetal cuts were made to relax the eye-cup and dividing the eye into inferior, superior and nasal quadrants. The eye cups were incubated with 3% bovine serum albumin and 1% Triton X-100 in 1×phosphate buffered saline (PBS, blocking buffer) at room temperature for one h in 2 ml glass vials to block nonspecific binding of antibody and to permeabilize the tissue. The anterior cups were then incubated with primary antibodies of choice in 200 µl blocking buffer for 2 d, with rocking, at 4 °C. The anterior cups were washed three times over a 3-h period with 1× PBS containing 0.1% Tween-20. The primary antibodies were detected with the appropriate species-specific secondary antibody (all Alexa 488, 594, or 647 at 1:1,000 dilution, Thermo Fisher Sci, Waltham, MA) diluted in blocking buffer also had DAPI to label nuclei. The immunostained eyecups were washed four times over a 3-h period in 1× PBS. Eye cups were then whole mounted on slides in Prolong Diamond (Thermo Fisher Sci, Waltham, MA). The following primary antibodies were used in this study: Goat IgG against CDH5 (1:100, AF1002, R&D Systems, Minneapolis, MN), pY658 and pY685-CDH5 (1:40, gift of F. Orsenoigo and E.Dejana), pY658 CDH5 (1:50, 44-1144 G, Thermo Fisher Sci, Waltham, MA), SRC (1:50, ab109381, Abcam, Cambridge, MA), FYN (1:50, ab125016, Abcam, Cambridge, MA), FYN (1:50, HPA023887, SIGMA-ALDRICH, Burlington, MA), pY418SRC (1:50, ab4816, Abcam, Cambridge, MA). Immunostaining with the phospho-specific antibodies requires great care as they proved extremely sensitive to fixation and pH. Eyes were fixed for 1 hour at 4°C in 4% PFA at pH around 7 (6.9-7.2). Over-fixation ( > 2 H) and improper pH of fix (outside the range stated) will result in the failure of immunostaining with the phosphor-specific antibodies.
Confocal microscopy and post-processing
Confocal
Microscopy was performed using an LSM SP8 confocal microscope (Leica) using either a 20× 0.7 NA multi-immersion objective or a 63× 1.3 NA glycerol immersion objective. The Mark and Find mode was used to automate the collection of images encompassing the entire limbus and generated a folder full of Z stacks at various individual overlapping positions along the limbus. For collections that were intended for colocalization, imaging was done after automatically optimizing the XYs format to set the optimal number of pixels to meet the Nyquist criterion for best lateral resolution for NA of objective and emission wavelength.
Deconvolution
Deconvolution was performed using Huygens Deconvolution software (Scientific Volume Imaging, Netherlands). Point spread function (PSF) was calculated automatically based on microscopic parameters and model of microscope. Classical maximum likelihood estimation method was used to perform deconvolution.
3D rendering
Individual confocal Z stacks (.lsm files) were processed directly using Imaris 9.3 (BitPlane AG, Zurich, Switzerland). Either the maximum intensity projection setting or the blend setting in Surpass mode of Imaris was used for 3D rendering. Images were oriented so that structures of interest were visible. Multiposition Z stacks generated using the Mark and Find setting on the confocal microscope were imported into Imaris and converted into Imaris files (.ims files). The resulting Imaris files were then stitched to generate a comprehensive Z stack encompassing the limbus using XuvTools83. Deconvolution was performed using Huygens Deconvolution software using the Classic Maximum Likelihood Estimation algorithm. Colocalization of channels was performed using the colocalization function of Imaris on deconvolved images. Thresholding was performed to remove the background signal prior to performing colocalization. Thresholding varied slightly between different primary antibodies. The colocalization percentages were recorded and graphed, and statistics were obtained from using PlotsOfData84. This procedure was performed in a blinded fashion in that the perfusion pressures were masked until calculating statistics. The colocalized channel was created in Imaris. Images were captured after rendering using the snapshot feature of Imaris and adjusted for levels (experimental group treated identically), and assembled in Adobe Photoshop CS6 (Adobe, San Jose, CA). Controls and experimental image sets were treated identically for all the above computational processes.
Electron microscopy
Mice were euthanized and eyes immediately were enucleated and fixed with 0.8% paraformaldehyde and 1.2% glutaraldehyde in 0.1 M phosphate buffer pH 7.2 at 4 °C. The eyes were fixed for 1 h and the anterior segment removed and cut into 1 × 2 mm blocks that included cornea, iris, TM and ciliary body. Fixation was continued at 4 °C for 12 h and the tissues were washed in phosphate buffer and then post-fixed with 1% osmium tetroxide, dehydrated and embedded in Embed-812 resin. Sections of 1 µm were cut and stained with Toluidine Blue O for orientation and determining if open SC was present and morphology of the limbus was intact. Ultrathin sections of 80–100 nm were cut and collected on TEM grids and stained with uranyl acetate and lead citrate. We evaluated 3 eyes and 10 sections per eye. Images were collected on a JOEL JEM-1230 electron microscope operating at an accelerating voltage of 80 kV and captured on a NAOSPRT15 camera at an exposure time of 2000 msec.
Immunoblotting
Protein lysate was prepared from pools of 6 limbal strips from B6 and B6. Fyn-/- eyes (2 replicates). Briefly, limbal strips were dissected from eyes on ice and placed in liquid nitrogen. The frozen limbal strips were crushed into powder using a pestle. The resulting powder was extracted with 200 µl ice cold RIPA buffer (MILLIPORE SIGMA, Burlington, MA) with Halt™ Protease and Phosphatase Inhibitor Cocktail (1:100,78440, Thermo Fisher Sci, Waltham, MA) for 30 min at room temperature and then a further 30 min on ice. The lysates were sonicated briefly and spun down at 14,000 × g for 30 min. The supernatant was diluted 1:1 with Laemmli Sample Buffer (1610737, BIO-RAD, Hercules, CA) and heated to 80˚C for 30 min.
A total of 30 µl of the B6 and B6. Fyn-/- lysate was loaded (4 sets per gel) on 4-20% TGX precast Mini-PROTEAN gels (4561103, BIO-RAD, Hercules, CA) and run at 100 V. The gel was transferred to PVDF membrane using an iBLOT dry transfer system (Thermo Fisher Sci, Waltham, MA). The blots were cut into strips to give B6 and B6. Fyn-/- lysate paired lanes. The membrane was blocked using 5% bovine serum albumin in Tris-buffered saline plus 0.1% Tween 20 (TBST) for 1 h at RT. The following antibodies were used for immunoblotting: Goat IgG against CDH5 (1:500, AF1002, R&D Systems, Minneapolis, MN), pY658-CDH5 (1:250, 44-1144 G, Thermo Fisher Sci, Waltham, MA).
FYN (1:500, HPA023887, SIGMA-ALDRICH, Burlington, MA), pY418SRC (1:500, ab4816, Abcam, Cambridge, MA) and GAPDH (1:500,). Appropriate horse radish peroxidase-conjugated antibodies were used at a dilution of 1:2500. The blots were developed using SuperSignal™ West Pico PLUS Chemiluminescent Substrate (34580, Thermo Fisher Sci, Waltham, MA). The blots were imaged on the Azure c600 Ultimate Western system. For quantification, band intensities were determined using the Gels feature of the Analyze function in Fiji/ImageJ. To calculate normalized expression of proteins in WT and FYN null lysates, the ratio of band intensity of CDH5, pY658-CDH5, pY685-CDH5, pY418-SFK respectively and GAPDH band intensity in matched paired lanes was calculated. The % decrease for normalized band intensity for each antibody was calculated for FYN null sample. Images were further processed (levels) and assembled in Adobe Photoshop.
IOP measurements
IOP was measured using the microneedle method as previously described in detail85,86. Briefly, mice were acclimatized to the procedure room and anesthetized via an intraperitoneal injection of a mixture of ketamine (99 mg/kg; Ketathesia, Henry Schein, Dublin, OH, USA) and xylazine (9 mg/kg; Anased, Akorn Inc, Gurnee, IL, USA) immediately prior to IOP assessment, a procedure that does not alter IOP in the experimental window86.
Pressure perfusion of mouse eyes
Mice were anesthetized using isoflurane (5% for induction, 2% for maintenance) and kept warm using a 37˚C heated mount. PBS was placed on the eye to prevent drying. The eye was cannulated using a beveled 60 µm pulled glass microneedle connected to a pressure sensor and a gravity-driven hydrostatic column filled with PBS. Following cannulation, the column was adjusted to induce the raised pressure (16 mm Hg, 25 mmHg, or 45 mmHg) in the eye for 45 minutes. These pressures were picked based on an earlier work showing effects of pressure on effects on SC junctions20.
To label the path of AQH outflow, 0.5 mg/ml of Alexa 594 conjugated GSII lectin (L21416, Thermo Fisher Sci, Waltham, MA) in PBS was perfused at the desired pressure.
Rapid fixation of eyes under pressure
After clamping eyes at the desired pressure for 45 min, the eyes were numbed with proparacaine for one minute under pressure with the microneedle still inserted in the eye. We numb the eye after perfusion period to prevent any pain reaction from the application of acrolein in the following step. This would also prevent the animal from twitching or blinking which could cause the microneedle to break or be removed from the eye. Then to fix the eyes under pressure, 10 µl of a solution of 1.1% acrolein and 2% paraformaldehyde (PFA) in PBS was applied topically to the eye. After 5 min, the eye was washed with PBS. The mouse was euthanized, and the eye was enucleated and placed in 4% PFA for one hour at 4 °C. The eye was then subjected to several room-temperature washes. First were two five-minute washes in PBS, followed by a 20-minute wash in 1% sodium borohydride in PBS, and finally, six more five-minute washes in PBS before immunofluorescence.
In vivo AQH outflow measurement in mice
Outflow facility was measured by a two-step pressure method and calculated based on the Goldman equation F = (IOP-EVP) x C + Fu, where C = conventional outflow facility, F = total outflow rate, IOP = is intraocular pressure, EVP = Episcleral venous pressure, and Fu = unconventional outflow87. The facility of the mouse eye was calculated by measuring flow rates of fluid in a specified time at two different pressures. Mice were anesthetized with isoflurane (5% for induction, 2% for maintenance) and secured on a heated mount (37˚C) with a nose cone for isoflurane delivery. After placing a drop of PBS, on the cornea, an eye was cannulated using a beveled 60 µm glass microneedle mounted on a capillary holder attached to a pressure transducer (DTXPlus TNF-R; Argon Medical Systems, Plano, TX, USA; a range of -30 mmHg to 300 mmHg and hysteresis and sensitivity variations is no more than 2% of the reading or ±1 mmHg, whichever is greater, over the operating range). The pressure transducer, in turn, was connected by a stopcock and a short length of pressure-resistant tubing to a gravity-driven pressure (hydrostatic) column with an in-line flow sensor (SLG-0150; Sensirion AG, Switzerland)88. The pressure transducer is connected to a computer via an amplifier and analog-to-digital converter. The pressure measurements were made with custom-built software76. The flow sensor is connected to the computer through a USB cable and software provided by Sensirion was used to measure flow.
The hydrostatic column, pressure and flow sensors, stopcock, and needle were all filled with PBS. The stopcock was kept closed prior to cannulation. It was opened following cannulation to induce a pressure of 20 mmHg in the eye. Following five minutes of equilibration, the total volume of liquid that flowed from the column over 10 minutes was measured. The pressure was then raised to 30 mmHg, and the five minutes of equilibration and 10 minutes of measurement were repeated. C, the outflow facility was calculated by dividing the difference between two flow rates by the difference between the corresponding pressures and time elapsed to give a value in nl/min/mmHg. The AQH outflow data had a normal distribution based on Shapiro-Francia (p = 0, W’ = 0.0511) and Anderson-Darling (p = 0, W = 0.3683). The data was graphed using R studio and ggplot2.
Statistical analysis
Throughout the text, reported P values were obtained using a two-tailed Student’s t-test, and one-way ANOVA followed by Tukey HSD test. P values of <0.05 were considered significant and are indicated. Statistical analysis of data t-test, was done using Microsoft Excel and R. One-way ANOVA was done using Data analysis tool in Excel to obtain exact p-value and also a tool available at the website- https://www.socscistatistics.com/tests/anova/default2.aspx. The mean absolute deviation (MAD) is a robust measure of the variability of quantitative data and was used to judge the dysregulation of IOP and AQH outflow facility. Variance and quartiles were determined by Microsoft Excel formula. Some summary statistics were also obtained from PlotsOfData84. Levene’s test to check if the difference between the variability of two or more groups is significant was performed using a web-based calculator (https://statskingdom.com/230var_levenes.html). The Levene’s test compares the Mean Absolute Deviations (MAD), which is another way to check the data variability. On the other hand, if the MADs are not the same it is very likely that the variances are not the same. Pearson’s correlation graphing, correlation coefficient and p values were obtained using R.
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Data availability
Source data are provided with this paper.
References
Tamm, E. R. The trabecular meshwork outflow pathways: structural and functional aspects. Exp. eye Res. 88, 648–655 (2009).
Overby, D. R., Stamer, W. D. & Johnson, M. The changing paradigm of outflow resistance generation: towards synergistic models of the JCT and inner wall endothelium. Exp. eye Res. 88, 656–670 (2009).
Johnson, M. ‘What controls aqueous humour outflow resistance?’. Exp. eye Res. 82, 545–557 (2006).
Ramos, R. F., Hoying, J. B., Witte, M. H. & Daniel Stamer, W. Schlemm’s canal endothelia, lymphatic, or blood vasculature? J. glaucoma 16, 391–405 (2007).
Dvorak-Theobald, G. Schlemm’s canal: its anastomoses and anatomic relations. Trans. Am. Ophthalmol. Soc. 32, 574–595 (1934).
Kizhatil, K., Ryan, M., Marchant, J. K., Henrich, S. & John, S. W. Schlemm’s canal is a unique vessel with a combination of blood vascular and lymphatic phenotypes that forms by a novel developmental process. PLoS Biol. 12, e1001912 (2014).
Narayanaswamy A, et al. Aqueous outflow channels and its lymphatic association: a review. Surv. Ophthalmol. (2021).
Lewczuk K, Jablonska J, Konopinska J, Mariak Z, Rekas M. Schlemm’s canal: the outflow ‘vessel’. Acta Ophthalmol, (2021).
Stamer, W. D. et al. Biomechanics of Schlemm’s canal endothelium and intraocular pressure reduction. Prog. retinal eye Res. 44, 86–98 (2015).
Overby, D. R. et al. Altered mechanobiology of Schlemm’s canal endothelial cells in glaucoma. Proc. Natl Acad. Sci. USA 111, 13876–13881 (2014).
Braakman, S. T., Moore, J. E. Jr., Ethier, C. R. & Overby, D. R. Transport across Schlemm’s canal endothelium and the blood-aqueous barrier. Exp. eye Res. 146, 17–21 (2016).
Niederkorn, J. Y. Immune privilege in the anterior chamber of the eye. Crit. Rev. Immunol. 22, 13–46 (2002).
Braakman, S. T., Read, A. T., Chan, D. W., Ethier, C. R. & Overby, D. R. Colocalization of outflow segmentation and pores along the inner wall of Schlemm’s canal. Exp. eye Res. 130, 87–96 (2015).
Epstein, D. L. & Rohen, J. W. Morphology of the trabecular meshwork and inner-wall endothelium after cationized ferritin perfusion in the monkey eye. Invest Ophthalmol. Vis. Sci. 32, 160–171 (1991).
Pedrigi, R. M., Simon, D., Reed, A., Stamer, W. D. & Overby, D. R. A model of giant vacuole dynamics in human Schlemm’s canal endothelial cells. Exp. eye Res. 92, 57–66 (2011).
Ethier, C. R. & Chan, D. W. Cationic ferritin changes outflow facility in human eyes whereas anionic ferritin does not. Invest Ophthalmol. Vis. Sci. 42, 1795–1802 (2001).
Tam, L. C. et al. Enhancement of outflow facility in the murine eye by targeting selected tight-junctions of schlemm’s canal endothelia. Sci. Rep. 7, 40717 (2017).
Li, G. et al. A small molecule inhibitor of ve-ptp activates tie2 in schlemm’s canal increasing outflow facility and reducing intraocular pressure. Investigative Ophthalmol. Vis. Sci. 61, 12 (2020).
Winderlich, M. et al. VE-PTP controls blood vessel development by balancing Tie-2 activity. J. Cell Biol. 185, 657–671 (2009).
Ye, W., Gong, H., Sit, A., Johnson, M. & Freddo, T. F. Interendothelial junctions in normal human Schlemm’s canal respond to changes in pressure. Invest Ophthalmol. Vis. Sci. 38, 2460–2468 (1997).
Chen LJ, Wang WL, Chiu JJ. Vascular Endothelial Mechanosensors in Response to Fluid Shear Stress. In: Molecular and Cellular Mechanobiology (eds Chien S, Engler AJ, Wang PY). Springer (2016).
Tzima, E. et al. A mechanosensory complex that mediates the endothelial cell response to fluid shear stress. Nature 437, 426–431 (2005).
Jalali, S. et al. Shear stress activates p60src-Ras-MAPK signaling pathways in vascular endothelial cells. Arterioscler Thromb. Vasc. Biol. 18, 227–234 (1998).
Na, S. et al. Rapid signal transduction in living cells is a unique feature of mechanotransduction. Proc. Natl Acad. Sci. USA 105, 6626–6631 (2008).
Okuda, M. et al. Shear stress stimulation of p130(cas) tyrosine phosphorylation requires calcium-dependent c-Src activation. J. Biol. Chem. 274, 26803–26809 (1999).
Chiu, Y. J., McBeath, E. & Fujiwara, K. Mechanotransduction in an extracted cell model: Fyn drives stretch- and flow-elicited PECAM-1 phosphorylation. J. Cell Biol. 182, 753–763 (2008).
Fleming, I., Fisslthaler, B., Dixit, M. & Busse, R. Role of PECAM-1 in the shear-stress-induced activation of Akt and the endothelial nitric oxide synthase (eNOS) in endothelial cells. J. cell Sci. 118, 4103–4111 (2005).
Angelini, D. J. et al. TNF-alpha increases tyrosine phosphorylation of vascular endothelial cadherin and opens the paracellular pathway through fyn activation in human lung endothelia. Am. J. Physiol. Lung Cell Mol. Physiol. 291, L1232–L1245 (2006).
Dejana, E., Orsenigo, F. & Lampugnani, M. G. The role of adherens junctions and VE-cadherin in the control of vascular permeability. J. cell Sci. 121, 2115–2122 (2008).
Orsenigo, F. et al. Phosphorylation of VE-cadherin is modulated by haemodynamic forces and contributes to the regulation of vascular permeability in vivo. Nat. Commun. 3, 1208 (2012).
Wessel, F. et al. Leukocyte extravasation and vascular permeability are each controlled in vivo by different tyrosine residues of VE-cadherin. Nat. Immunol. 15, 223–230 (2014).
Jin, Y. et al. Tyrosine-protein kinase Yes controls endothelial junctional plasticity and barrier integrity by regulating VE-cadherin phosphorylation and endocytosis. Nat. Cardiovascular Res. 1, 1156–1173 (2022).
Vestweber, D. VE-cadherin: the major endothelial adhesion molecule controlling cellular junctions and blood vessel formation. Arterioscler Thromb. Vasc. Biol. 28, 223–232 (2008).
Heimark, R. L., Kaochar, S. & Stamer, W. D. Human Schlemm’s canal cells express the endothelial adherens proteins, VE-cadherin and PECAM-1. Curr. eye Res. 25, 299–308 (2002).
Gong, S. et al. A gene expression atlas of the central nervous system based on bacterial artificial chromosomes. Nature 425, 917–925 (2003).
Truong, T. N., Li, H., Hong, Y. K. & Chen, L. Novel characterization and live imaging of Schlemm’s canal expressing Prox-1. PloS one 9, e98245 (2014).
Hamanaka, T., Bill, A., Ichinohasama, R. & Ishida, T. Aspects of the development of Schlemm’s canal. Exp. Eye Res. 55, 479–488 (1992).
Thomas, S. M. & Brugge, J. S. Cellular functions regulated by Src family kinases. Annu Rev. Cell Dev. Biol. 13, 513–609 (1997).
Piwnica-Worms, H., Saunders, K. B., Roberts, T. M., Smith, A. E. & Cheng, S. H. Tyrosine phosphorylation regulates the biochemical and biological properties of pp60c-src. Cell 49, 75–82 (1987).
Chiang, G. G. & Sefton, B. M. Phosphorylation of a Src kinase at the autophosphorylation site in the absence of Src kinase activity. J. Biol. Chem. 275, 6055–6058 (2000).
Stover, D. R., Furet, P. & Lydon, N. B. Modulation of the SH2 binding specificity and kinase activity of Src by tyrosine phosphorylation within its SH2 domain. J. Biol. Chem. 271, 12481–12487 (1996).
Dejana, E. & Orsenigo, F. Endothelial adherens junctions at a glance. J. cell Sci. 126, 2545–2549 (2013).
Komarova, Y. A., Kruse, K., Mehta, D. & Malik, A. B. Protein interactions at endothelial junctions and signaling mechanisms regulating endothelial permeability. Circulation Res. 120, 179–206 (2017).
Balasubramanian R, et al. Transcriptomic profiling of Schlemm’s canal cells reveals a lymphatic-biased identity and three major cell states. bioRxiv, 2023.2008.2031.555823 (2023).
van Zyl, T. et al. Cell atlas of aqueous humor outflow pathways in eyes of humans and four model species provides insight into glaucoma pathogenesis. Proc. Natl Acad. Sci. USA 117, 10339–10349 (2020).
Chang, B. et al. Haploinsufficient Bmp4 ocular phenotypes include anterior segment dysgenesis with elevated intraocular pressure. BMC Genet 2, 18 http://www.biomedcentral.com/1471-2156/1472/1418 (2001).
John, S. W. M. et al. Essential iris atrophy, pigment dispersion, and glaucoma in DBA/2 J mice. Invest Ophthalmol. Vis. Sci. 39, 951–962 (1998).
Tolman NG, et al. Genetic background modifies vulnerability to glaucoma-related phenotypes in Lmx1b mutant mice. Dis. Model Mech. 14, (2021).
Acott, T. S., Vranka, J. A., Keller, K. E., Raghunathan, V. & Kelley, M. J. Normal and glaucomatous outflow regulation. Prog. retinal eye Res. 82, 100897 (2021).
Reina-Torres, E. et al. The vital role for nitric oxide in intraocular pressure homeostasis. Prog. retinal eye Res. 83, 100922 (2021).
Simionescu, M., Simionescu, N. & Palade, G. E. Segmental differentiations of cell junctions in the vascular endothelium. microvasculature. J. Cell Biol. 67, 863–885 (1975).
Carmeliet, P. et al. Targeted deficiency or cytosolic truncation of the VE-cadherin gene in mice impairs VEGF-mediated endothelial survival and angiogenesis. Cell 98, 147–157 (1999).
Dejana, E. & Vestweber, D. The role of VE-cadherin in vascular morphogenesis and permeability control. Prog. Mol. Biol. Transl. Sci. 116, 119–144 (2013).
Hagerling R, et al. Distinct roles of VE-cadherin for development and maintenance of specific lymph vessel beds. Embo J. 37, (2018).
Dejana, E., Orsenigo, F., Molendini, C., Baluk, P. & McDonald, D. M. Organization and signaling of endothelial cell-to-cell junctions in various regions of the blood and lymphatic vascular trees. Cell Tissue Res 335, 17–25 (2009).
Katsuno, T. et al. Deficiency of zonula occludens-1 causes embryonic lethal phenotype associated with defected yolk sac angiogenesis and apoptosis of embryonic cells. Mol. Biol. cell 19, 2465–2475 (2008).
Frye, M. et al. Interfering with VE-PTP stabilizes endothelial junctions in vivo via Tie-2 in the absence of VE-cadherin. J. Exp. Med. 212, 2267–2287 (2015).
Adam, A. P., Sharenko, A. L., Pumiglia, K. & Vincent, P. A. Src-induced tyrosine phosphorylation of VE-cadherin is not sufficient to decrease barrier function of endothelial monolayers. J. Biol. Chem. 285, 7045–7055 (2010).
Klomp, J. E. et al. Time-variant SRC kinase activation determines endothelial permeability response. Cell Chem. Biol. 26, 1081–1094 e1086 (2019).
Conway, D. E. et al. VE-cadherin phosphorylation regulates endothelial fluid shear stress responses through the polarity protein LGN. Curr. Biol. 27, 2219–2225.e2215 (2017).
Garrett, J. P., Lowery, A. M., Adam, A. P., Kowalczyk, A. P. & Vincent, P. A. Regulation of endothelial barrier function by p120-cateninVE-cadherin interaction. Mol. Biol. cell 28, 85–97 (2017).
Potter, M. D., Barbero, S. & Cheresh, D. A. Tyrosine phosphorylation of VE-cadherin prevents binding of p120- and beta-catenin and maintains the cellular mesenchymal state. J. Biol. Chem. 280, 31906–31912 (2005).
Thomson BR, et al. Targeting the vascular-specific phosphatase PTPRB protects against retinal ganglion cell loss in a pre-clinical model of glaucoma. Elife 8, (2019).
Wan, Q. et al. Subcellular domain-dependent molecular hierarchy of SFK and FAK in mechanotransduction and cytokine signaling. Sci. Rep. 7, 9033 (2017).
Bershadsky, A. D., Balaban, N. Q. & Geiger, B. Adhesion-dependent cell mechanosensitivity. Annu Rev. Cell Dev. Biol. 19, 677–695 (2003).
Johnstone, M. A. & Grant, W. G. Pressure-dependent changes in structures of the aqueous outflow system of human and monkey eyes. Am. J. Ophthalmol. 75, 365–383 (1973).
McDonnell, F. et al. Shear stress in schlemm’s canal as a sensor of intraocular pressure. Sci. Rep. 10, 5804 (2020).
Sherwood, J. M., Stamer, W. D. & Overby, D. R. A model of the oscillatory mechanical forces in the conventional outflow pathway. J. R. Soc., Interface / R. Soc. 16, 20180652 (2019).
Han, B. et al. Conversion of mechanical force into biochemical signaling. J. Biol. Chem. 279, 54793–54801 (2004).
Gagen, D., Faralli, J. A., Filla, M. S. & Peters, D. M. The role of integrins in the trabecular meshwork. J. Ocul. Pharmacol. Therapeutics: Off. J. Assoc. Ocul. Pharmacol. Therapeutics 30, 110–120 (2014).
Harburger, D. S. & Calderwood, D. A. Integrin signalling at a glance. J. cell Sci. 122, 159–163 (2009).
Sinha, B. et al. Cells respond to mechanical stress by rapid disassembly of caveolae. Cell 144, 402–413 (2011).
Gervasio, O. L., Phillips, W. D., Cole, L. & Allen, D. G. Caveolae respond to cell stretch and contribute to stretch-induced signaling. J. cell Sci. 124, 3581–3590 (2011).
Osawa, M., Masuda, M., Harada, N., Lopes, R. B. & Fujiwara, K. Tyrosine phosphorylation of platelet endothelial cell adhesion molecule-1 (PECAM-1, CD31) in mechanically stimulated vascular endothelial cells. Eur. J. Cell Biol. 72, 229–237 (1997).
Elliott, M. H. et al. Caveolin-1 modulates intraocular pressure: implications for caveolae mechanoprotection in glaucoma. Sci. Rep. 6, 37127 (2016).
Kizhatil, K. et al. An in vitro perfusion system to enhance outflow studies in mouse eyes. Investigative Ophthalmol. Vis. Sci. 57, 5207–5215 (2016).
Thorleifsson, G. et al. Common variants near CAV1 and CAV2 are associated with primary open-angle glaucoma. Nat. Genet. 42, 906–909 (2010).
Reina-Torres, E. et al. VEGF as a paracrine regulator of conventional outflow facility. Investigative Ophthalmol. Vis. Sci. 58, 1899–1908 (2017).
Wen, J. C. et al. Intravitreal anti-VEGF injections reduce aqueous outflow facility in patients with neovascular age-related macular degeneration. Investigative Ophthalmol. Vis. Sci. 58, 1893–1898 (2017).
Smith, R. S. et al. Haploinsufficiency of the transcription factors FOXC1 and FOXC2 results in aberrant ocular development. Hum. Mol. Genet. 9, 1021–1032 (2000).
Stein, P. L., Lee, H. M., Rich, S. & Soriano, P. pp59fyn mutant mice display differential signaling in thymocytes and peripheral T cells. Cell 70, 741–750 (1992).
Soriano, P., Montgomery, C., Geske, R. & Bradley, A. Targeted disruption of the c-src proto-oncogene leads to osteopetrosis in mice. Cell 64, 693–702 (1991).
Emmenlauer, M. et al. XuvTools: free, fast and reliable stitching of large 3D datasets. J. Microsc 233, 42–60 (2009).
Postma, M. & Goedhart, J. PlotsOfData-A web app for visualizing data together with their summaries. PLoS Biol. 17, e3000202 (2019).
John, S. W. M., Hagaman, J. R., MacTaggart, T. E., Peng, L. & Smithes, O. Intraocular pressure in inbred mouse strains. Invest Ophthalmol. Vis. Sci. 38, 249–253 (1997).
Savinova, O. V. et al. Intraocular pressure in genetically distinct mice: an update and strain survey. BMC Genet 2, 12 http://www.biomedcentral.com/1471-2156/1472/1412 (2001).
Aihara, M., Lindsey, J. D. & Weinreb, R. N. Aqueous humor dynamics in mouse. Invest Ophthalmol. Vis. Sci. 44, 3423 (2003).
Sherwood, J. M., Reina-Torres, E., Bertrand, J. A., Rowe, B. & Overby, D. R. Measurement of outflow facility using iperfusion. PloS one 11, e0150694 (2016).
Acknowledgements
We are grateful to Dr. Elisabetta Dejana (Uppsala University) and Fabrizio Orsenigo (FIRC Institute of Molecular Oncology: Milan) for their generous gift of the phosphor-CDH5 antibodies. Dr. Dan Stamer (Duke University) for critically reading the manuscript. We thank Dr. David Reed (OSU) for his help with statistical analysis. The project was funded by National Eye Institute (NEI) grant R01EY032062 (KK and SWMJ), with partial contributions from R01EY028175 (KK), R01EY032507, and R01EY018606 and New York Fund for Innovation in Research and Scientific Talent (NYFIRST; EMPIRE CU19-2660) award (SWMJ). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. Additional support was provided by Bright Focus Foundation grant BFOCUS CG2020004 (KK and SWMJ) and startup funds at Columbia University, including the Precision Medicine Initiative. Initial funding was provided by HHMI (SWMJ). The project was also supported by a Vison Core grant P30 EY019007 and an unrestricted departmental award from RPB.
Author information
Authors and Affiliations
Contributions
K.K. – conceived and designed experiments, analyzed data, wrote the manuscript, sought and obtained funding. G.C. – performed experiments and analyzed data. D.S., A.B., and L.H. – performed experiments. R.B. – designed and performed experiments, analyzed data, edited manuscript. S.J. – conceived and designed experiments, analyzed data, edited manuscript, sought and obtained funding.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Communications thanks Aftab Taiyab and the other, anonymous, reviewer(s) for their contribution to the peer review of this work. A peer review file is available.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Source data
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Kizhatil, K., Clark, G.M., Sunderland, D.K. et al. FYN regulates aqueous humor outflow and IOP through the phosphorylation of VE-CADHERIN. Nat Commun 16, 51 (2025). https://doi.org/10.1038/s41467-024-55232-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41467-024-55232-8
This article is cited by
-
Geometric determinants of sinterless, low-temperature-processed 3D-nanoprinted glass
Microsystems & Nanoengineering (2025)