Abstract
This study compared long-term survival and reintervention rates between Valve-Sparing Root Replacement (VSRR, n = 244) and Aortic Root Replacement (ARR, n = 499) in 743 patients undergoing Type A acute aortic dissection (AAD), given the lack of prospective comparative data. Multivariable analysis is identifying advanced age, high Body Mass Index (BMI), Marfan syndrome, severe aortic regurgitation, bicuspid aortic valve, increased aortic root diameter, and reduced aortic cross-clamp time (ACC) as significant factors associated with ARR. After Propensity Score Matching (PSM), VSRR is showing significantly higher 5-year survival rates than ARR (80.2% vs. 64.1%, P = 0.001), validated by Inverse Probability of Treatment Weighting (IPTW) analysis. Reintervention rates are being found comparable, with endocarditis more prevalent in ARR and aortic regurgitation in VSRR. Subgroup analysis indicated that patients aged less than 60 years and those with a BMI greater than 24 in the VSRR group exhibited significantly improved survival probabilities compared to the ARR group. These findings support the wider utilization of valve-sparing root replacement (VSRR) in appropriately selected patients, highlighting its potential advantages for suitable candidates.
Similar content being viewed by others
Introduction
The surgical management of acute type A aortic dissection remains a formidable challenge1. Despite widespread reporting of perioperative results, there is still no unanimous agreement in the literature on the optimal proximal repair surgical technique, often relying on surgeon discretion or institutional traditions2,3,4,5,6,7,8,9,10,11. ARR surgery, which simultaneously replaces the valve and aortic root, potentially eliminates the need for future valve repairs but poses unique challenges to patients, such as indefinite anticoagulant therapy required for mechanical valves, increasing the risk of blood clots and bleeding12. Conversely, biological valves do not require lifelong anticoagulants but may deteriorate over time, necessitating repeat surgery. In contrast, VSRR surgery, which focuses on replacing the aortic root while preserving the native valve, is a favorable option for patients with functional aortic valves13,14. However, its comparative complexity and demand for high technical proficiency may lead to prolonged extracorporeal circulation, intensified myocardial ischemia, and increased perioperative mortality2,3,7,10,11. While several studies have shown promising mid-term aortic valve function following VSRR surgery, the long-term prognosis remains uncertain2,3,9,10,11,15,16.
The perioperative results data predominantly originate from single institutions, which are inherently prone to selection bias. Furthermore, many of these single-institution studies are relatively small-scale and lack crucial long-term survival data. The necessity of prospective randomized trials in comparing the efficacy of ARR and
VSRR for AAD management is paramount. However, such trials are currently nonexistent, owing to the arduous, expensive, and time-consuming nature of their conduct. In the absence of randomized data, we opted to undertake an observational study in a multicenter database to assess the effectiveness of ARR and VSRR. In this work, we addressed the patient characteristic heterogeneity between the ARR and VSRR groups by utilizing propensity score matching (PSM) to adjust for baseline disparities and minimize confounding effects17,18. Furthermore, the robustness of our findings was reinforced through sensitivity analysis utilizing inverse probability of treatment weighting (IPTW).
Results
Patient characteristics
From 2013 to 2019, a total of 743 patients with acute aortic dissection (AAD) were identified. Of these patients, 499 (67.16%) underwent aortic root replacement (ARR) surgery as their primary treatment, while 244 (32.84%) underwent valve-sparing root replacement (VSRR) surgery. The demographic characteristics of the two groups differed significantly. Specifically, the mean age of patients in the ARR group was 60.09 years, with a male preponderance of 319 individuals (63.93%). In contrast, the VSRR group had a younger mean age of 54.99 years, and a slightly higher proportion of males, accounting for 171 patients (70.08%). Baseline patient characteristics are presented in Table 1. Patients undergoing ARR surgery demonstrated advanced age, elevated body mass index, and a higher prevalence of comorbidities such as Marfan syndrome, aortic regurgitation, chronic kidney disease, peripheral vascular disease, cerebrovascular disease, and bicuspid aortic valve, in comparison to those treated with VSRR. Furthermore, they exhibited a significantly larger aortic root diameter and curtate ACC (aortic cross-clamp) time, as summarized in Table 1.
Confounding factors
We conducted a comprehensive analysis using both univariate and multivariable logistic regression models to identify confounders pertaining to aortic valve replacement (ARR). As summarized in Table 2, the univariate analysis highlighted significant predictors, such as age at initial diagnosis (P < 0.001), BMI (P < 0.001), chronic kidney disease (P = 0.008), peripheral vascular disease (P = 0.032), cerebrovascular disease (P < 0.001), Marfan syndrome (P < 0.001), aortic regurgitation (P < 0.001), bicuspid aortic valve (P < 0.001), enlarged aortic root diameter (P < 0.001), and decreased aortic cross-clamp time (ACC, min).
Upon multivariable analysis, we confirmed that advanced age at diagnosis (P < 0.001), increased BMI (P < 0.001), Marfan syndrome (P < 0.001), severe aortic regurgitation (P < 0.001), bicuspid aortic valve (P < 0.001), and a marked increase in aortic root diameter (P < 0.001), along with reduced ACC (min), were independently and significantly associated with a heightened relevance for ARR. Notably, chronic kidney disease, peripheral vascular disease, and cerebrovascular disease did nottabfigdemonstrate independent associations with ARR and were thus excluded from the propensity score matching (PSM) analysis.
Outcomes
The standardized mean differences analysis revealed that all covariate imbalances were under 10%, indicating an acceptable matching process. Further examination of the propensity score distributions before and after matching showed a more uniform distribution post-matching, suggesting enhanced comparability between groups (Fig. 1 and Supplementary Table 1). After mitigating potential biases through PSM analysis, patients undergoing VSRR exhibited a higher incidence of low cardiac output syndrome, hepatic dysfunction, root aneurysm requiring reintervention, spontaneous hemorrhage, and moderate to severe aortic stenosis compared to ARR patients. Additionally, VSRR patients had higher in-hospital and overall mortality rates than ARR patients (Table 3).
This figure presents the standardized mean differences (SMD) for various covariates related to the study, both before and after propensity score matching (PSM). Each panel represents a different variable: distance, no or mild aortic regurgitation, ACC time, moderate, Marfan syndrome, aortic root diameter, bicuspid aortic valve, BMI, AGE, and severe AR (both unadjusted and adjusted). The SMD values indicate the degree of imbalance between the groups. Covariate balance was evaluated by analyzing the standardized difference of means, with an absolute value of the mean difference <0.1 considered indicative of successful matching. No_or_Mild no or mild aortic regurgitation, AR aortic regurgitation.
Survival analysis
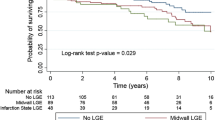
Initially, survival analyses conducted on the unmatched cohorts of patients undergoing valve-sparing root replacement (VSRR) and aortic root replacement (ARR) did not yield statistically significant differences in survival outcomes (Fig. 2). However, upon application of propensity score matching, a distinct advantage in survival emerged for the VSRR group compared to the ARR group, with a P-value of 0.001 indicating statistical significance (Fig. 3). More precisely, the 5-year overall survival (OS) rate for patients in the VSRR group stood at 80.2%, which was notably and significantly higher than the 64.1% observed in the ARR group, as evident from the data presented in Table 4. This disparity in survival rates was further corroborated by the inverse probability of treatment weighting (IPTW) analysis, which robustly demonstrated an association between VSRR and increased survival, as depicted in Fig. 4.
This figure illustrates the survival probability over time for patients undergoing valve-sparing root replacement (VSRR) and aortic root replacement (ARR). The horizontal axis represents the time in months since diagnosis until death or last contact, while the vertical axis indicates the survival probability. The color coding distinguishes between the two patient groups: blue represents the “No” group (ARR), and red represents the “Yes” group (VSRR). Additionally, the chart displays the number of patients at risk at various time points. However, survival analyses conducted on the unmatched cohorts of these patients did not yield statistically significant differences in survival outcomes, with a p value of 0.062, which is greater than the commonly accepted significance level of 0.05.
This figure illustrates the survival probability over time in months since diagnosis until death or last contact. The horizontal axis depicts the time period, while the vertical axis indicates the survival probability. The chart employs color coding to differentiate between two variables: blue represents the “No” group (ARR), and red represents the “Yes” group (VSRR). Additionally, the chart displays the number of patients at risk at various time points. After applying propensity score matching, a significant survival advantage emerged for the VSRR group compared to the ARR group, with a p value of 0.001, indicating statistical significance (p value < 0.05).
This figure depicts the survival probability over time for two groups, distinguished by color coding. The horizontal axis represents the time in months since diagnosis until death or last contact, while the vertical axis indicates the survival probability. Blue represents the “No” group (ARR), and red represents the “Yes” group (VSRR). The chart also displays the number of patients at risk at various time points. Upon application of the inverse probability of treatment weighting (IPTW) analysis, a statistically significant advantage in survival emerged for the VSRR group compared to the ARR group, with a p value of < 0.001 (p< 0.001), indicating a clear distinction between the two groups.
Subgroup analysis of the impact of potential confounding variables on treatment outcomes
Subgroup analysis revealed that, within the subgroup of patients aged <60 years and those with a BMI exceeding 24, the VSRR group demonstrated a significant improvement in survival probability compared to the ARR group. Specifically, for patients under 60 years old, the hazard ratio was 0.638 (95% CI: 0.413 to 0.987) with a p-value of 0.042. For individuals with a BMI between 23.9 and 28, the hazard ratio was 0.494 (95% CI: 0.267 to 0.913), yielding a p-value of 0.024. Furthermore, in patients with a BMI g>28, the hazard ratio was 0.454 (95% CI: 0.213 to 0.969), with a p-value of 0.041. Additionally, an examination of heterogeneity across subgroups was conducted. The results indicated that the survival probability improvement in the VSRR group compared to the ARR group was statistically significant across subgroups with varying degrees of aortic regurgitation (P for interaction = 0.031), as depicted in Supplementary Table 2.
Discussion
The current study uniquely aims to bridge the knowledge gap regarding the clinical merits of VSRR compared to ARR. By integrating cohorts from three prominent aortic centers, our findings offer three significant insights. Firstly, after adjusting for baseline differences through propensity score matching (PSM), VSRR exhibited a superior survival rate compared to ARR. Further analysis revealed that, within specific subgroups, VSRR demonstrated significantly improved survival probabilities compared to ARR. Specifically, patients aged <60 years and those with a BMI >24 in the VSRR group showed higher survival rates. Secondly, it is noteworthy that the rate of re-intervention following VSRR remains relatively high. Finally, as a large retrospective study conducted in an Asian region, we believe that our findings provide crucial new data to support the field.
Despite ARR’s position as the primary treatment for AAD, the utilization of VSRR has been steadily increasing1,2,19. Nonetheless, to date, no randomized controlled trials comparing survival rates between these two procedures have been reported. Although observational studies are not a perfect substitute for randomized clinical trials, they serve as a valuable complement to address knowledge gaps and inquiries that may not be feasible or addressed in randomized trials. However, direct comparisons between VSRR and ARR are hampered by significant selection bias, as VSRR tends to be performed in younger, healthier patients, whereas ARR is more widely applicable, encompassing older and sicker patients. These limitations are evident in the significant differences in baseline characteristics observed in unmatched comparisons. To address these limitations, propensity-matched analyses were conducted on a multicenter database comprising 743 patients who underwent either ARR or VSRR surgery. Prior to matching, no statistical difference in 5-year survival was observed between the two groups. However, following propensity score matching, the VSRR group exhibited better survival outcomes. The results indicated that patients treated with VSRR exhibited an 80.2% greater OS benefit compared to those receiving ARR. This survival benefit remained consistentfollowing the application of inverse probability of treatment weighting (IPTW) analysis.
The present study indicates a potential survival benefit of VSRR over ARR in certain cases, a finding that has not been robustly supported in the current literature. A meta-analysis conducted by Elbatarny et al.15 revealed that, in comparison to composite valve transplantation, retaining the aortic valve is not only safe but also reduces the risk of late mortality, thromboembolism/stroke, and bleeding. This suggests that aortic valve preservation should be considered for patients with well-preserved valve morphology. Similarly, Levine et al.3 reported that VSRR is associated with improved survival and a reduced need for subsequent reinterventions compared to bioprosthetic composite valve grafts (CVG).
Conversely, Mario Gaudino10, Sergey Leontyev9, and Eilon Ram2 failed to detect significant variations in long-term survival between VSRR and aortic root replacement (ARR). Gaudino et al.10 reported that surgical type does not affect early or late survival, with mechanical CVG still being the durability benchmark. However, biocomposite valve grafts and valve-preserving reconstructions offer viable options for patients unsuitable for long-term anticoagulation. Leontyev et al.9 found the David operation resulted in reduced blood loss compared to the Bentall procedure, without increasing reoperation risk. This operation is preferred in patients with suitable anatomical features due to its avoidance of bleeding and other long-term artificial valve complications. Eilon Ram et al.2 subsequently reported favorable early and medium-term outcomes for both VSRR and CVG in carefully selected patients, with no significant survival differences between the two approaches. Despite valve retention’s higher risk of aortic insufficiency, no differences in reoperation rates were observed.
In our comprehensive analysis, we found no evidence to support the previously reported concerns of increased reoperation rates and decreased durability associated with David’s surgery20, as our study did not observe any notable difference in the overall reoperation rates between Aortic Root Replacement (ARR) and Valve-Sparing Root Replacement (VSRR) during the follow-up period, following propensity score matching. However, a subtle yet significant distinction emerged when we delved into the subgroup analysis of the causes of re-surgery. Specifically, endocarditis emerged as the primary reason for reintervention in the ARR group, whereas moderate to severe aortic regurgitation was the predominant factor in the VSRR cohort. Regarding other long-term outcomes, our study failed to detect any statistically significant differences in the incidence of complications such as stroke between the two surgical procedures. Nevertheless, in the immediate postoperative phase, patients undergoing VSRR exhibited a heightened susceptibility to low cardiac output syndrome and liver insufficiency. Notably, these VSRR patients were typically younger, had pre-existing moderate to severe aortic regurgitation, and frequently experienced cardiac insufficiency or even heart failure during postoperative surveillance. Furthermore, a subset of these VSRR patients engaged in high-risk behaviors, including alcoholism and inadequate sleep, during the postoperative follow-up period, which could potentially exacerbate liver damage. Our further investigation uncovered a robust correlation between these early postoperative complications and elevated early mortality rates. Additionally, our findings are consistent with previous studies conducted by other researchers, which have reported a higher prevalence of endocarditis among Bentall patients21,22. This underscores the importance of maintaining a heightened level of vigilance in this patient population to mitigate potential adverse outcomes.
This study has some limitations. As a retrospective, three-center study conducted in high-volume aortic centers, the associations described here cannot be interpreted as causal. Additionally, the generalizability of the presented results may be limited. However, given the challenges of conducting randomized clinical trials to compare these procedures, we believe our study provides an important addition to the literature. We also acknowledge that preoperative and intraoperative decision-making as well as postoperative care may vary among surgeons and institutions, potentially influencing outcomes. Thus, the influence of unmeasured confounders remains a possibility. Furthermore, the approach to ARR was based on surgeon preferences, although the techniques used for each type of surgery were consistent across the entire cohort. Nonetheless, we consider the comparison between ARR and VSRR to be highly relevant in contemporary practice.
Conclusion
Upon comprehensive analysis utilizing propensity score matching, Valve-Sparing Root Replacement (VSRR) has emerged as the superior surgical option, exhibiting improved 5-year survival outcomes in comparison to Aortic Root Replacement (ARR). This conclusion is fortified by the additional validation achieved through the application of inverse probability of treatment weighting (IPTW) analysis. Additional subgroup analysis revealed significantly higher survival probabilities for VSRR compared to ARR, specifically in patients aged <60 years and those with a BMI >24. Collectively, our findings present persuasive arguments in favor of a more widespread adoption of VSRR for appropriate patient cohorts. This strategic shift in surgical approach has the potential to elevate patient outcomes and augment OS rates in the context of aortic root disease management.
Materials and methods
Ethics approval and Informed consent to participate
The authors bear full responsibility for the accuracy and integrity of this work, ensuring that any inquiries related to it are thoroughly investigated and resolved. The patient data used in the study was not anonymized. Prior to the publication of this study, informed consent was obtained from all participants for the inclusion of their data and any accompanying images. The research adhered strictly to the principles outlined in the Declaration of Helsinki (2013 revision). The study and its database were reviewed and approved by ethics boards, with the following reference numbers: [2024] Scientific Research No. 112, 2024LWB265, and [2024] Ethics Review No. (172). Regarding patient consent for data use, it was obtained during the patients’ treatment process. Furthermore, to maintain adherence to ethical standards, we took the additional step of re-contacting the patients or their authorized representatives to obtain specific consent for the utilization of their data in this particular study.
Data source
The data pertaining to patients with acute aortic dissection (AAD) who underwent surgical treatment at three tertiary Grade A hospitals (Fujian Medical University Union Hospital, Zhangzhou Affiliated Hospital of Fujian Medical University and the First Affiliated Hospital of Xiamen University) between February 1, 2013, and February 1, 2019, was retrieved from various databases, encompassing case management systems, imaging systems, and surgical records. The clinical information, demographic characteristics, and baseline data were extracted from electronic medical records, and the operative notes were rigorously reviewed. All imaging modalities, specifically transesophageal echocardiography (TEE) and computed tomography, were analyzed to validate the anatomical diagnosis. The study encompasses all eligible individuals within the designated study period, adhering to specific inclusion criteria: age over 18, clinical diagnosis of AAD confirmed by CT angiography (CTA) or ultrasound, emergency surgery within 48 h of admission, and informed consent from patients. The exclusion criteria for the study encompassed infective endocarditis, prior AV surgery, and the utilization of non-David V or Bentall root replacements, as depicted in Fig. 5. Notably, the presence of moderate or severe aortic regurgitation did not constitute an absolute contraindication for valve-sparing root replacement (VSRR), thus allowing for its consideration in select cases.
A total of 864 surgeries were performed during February 2013 to February 2019. Of these, 121 surgeries were excluded for various reasons: 47 due to infective endocarditis, 62 due to prior AV surgery, 11 due to non-David V (DV) or Bentall surgery, and 1 due to being a second surgery in the database. The final cohort for analysis, by either ARR or valve-sparing root replacement (VSRR), included 743 surgeries. Among these, 499 surgeries involved aortic root replacement (ARR) with valve replacement, while 244 surgeries involved valve-sparing root replacement (VSRR). The symbols used in the flowchart are as follows: ● represents excluded cases. AV aortic valve.
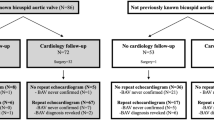
In this study, we have comprehensively documented the key variables pertaining to patient characteristics, intraoperative specifics, and in-hospital outcomes. The following aspects are noteworthy: During the data collection process, “race” information is often self-reported by participants/respondents, which helps ensure the accuracy and authenticity of the data. The “education level” assessment may combine multiple data sources, including self-reports of participants, census data, and administrative records. In categorizing people into different categories, we follow standardized classification criteria and use objective, quantifiable indicators whenever possible. However, there are some exceptions where data is missing, specifically for EF (18 missing, 2.3%), CPB time (11 missing, 1.4%), and cross-clamp time (4 missing, 0.5%). The median follow-up duration for the entire cohort was 5.6 years, with a slight variation of 5.2 years for patients undergoing VSRR and 5.8 years for those undergoing ARR. When updated follow-up information was unavailable, patients were censored at the date of their last contact. The primary endpoint of this study was to assess all-cause mortality. Additionally, we considered any reintervention necessitated due to aortic valve-related issues as a secondary endpoint. The study design, results, and implications are summarized in Fig. 6.
This figure illustrates a multicenter, propensity-matched study comparing survival rates between valve-sparing aortic root replacement (VSRR) and aortic root replacement (ARR) for the treatment of type A aortic dissection (AAD). The study enrolled a total of 743 patients, with 499 in the VSRR group and 244 in the ARR group. Due to the lack of randomized controlled trials comparing these two surgical approaches, observational studies have been hindered by selection bias. To address this, the core methodology employed a propensity score-matched analysis (PSM), resulting in 249 patients in the VSRR group and 147 patients in the ARR group after matching. Sensitivity analysis was conducted using inverse probability of treatment weighting (IPTW) to further validate the results. A, B highlight the key clinical implications of the study, which demonstrate that VSRR demonstrated improved long-term survival over ARR, albeit without significant differences in re-intervention rates. Our data advocate for a more extensive adoption of VSRR among suitable candidates, highlighting its potential benefits in the treatment of type A aortic dissection.
Surgical technique
Although the surgical indication was individually determined by the attending surgeon, it generally adhered to the contemporary guidelines published at the time of surgery23,24. All surgical interventions were performed using a median sternotomy approach, central cannulation, moderately hypothermic cardiopulmonary bypass (32°C), aortic cross-clamping, and myocardial protection achieved through cold antegrade blood cardioplegia. Specifically, the David I technique14 was utilized for VSARR, while the modified Bentall technique25 was adopted for ARR. In cases requiring concomitant hemiarch/transverse aortic procedures, the selection of the arterial cannulation site and the cerebral protection method was left to the discretion of the operating surgeon.
Statistical analysis
The relationships between treatment modality and patient demographic and clinical characteristics were examined using the Pearson χ2 or Fisher’s exact test for categorical data and the Wilcoxon rank sum test for ordinal and continuous data. Regarding the primary outcome, two analytical models were formulated: a propensity score-matched model and an unmatched univariable analysis utilizing the Kaplan-Meier estimator of inverse probability of treatment weight (IPTW). Additionally, a propensity score model for the receipt of ARR was established via stepwise variable selection within a multivariable logistic regression framework. This model incorporated candidate variables that demonstrated significant associations with treatment modality through univariable analysis, with a threshold of P < 0.05 required for initial inclusion and subsequent retention in the final model. Based on these propensity scores, a stabilized inverse probability of treatment weight was calculated. It is noteworthy that in the context of weighted analysis utilizing IPTW (Inverse Probability of Treatment Weighting), the efficiency and accuracy of statistical analysis are enhanced through the adjustment of weights. This process leads to an apparent increase in the effective sample size or information content within each group under the weighted analysis. It is crucial to emphasize that this augmentation represents a statistical increase, rather than a physical one, underscoring the refined precision and sensitivity gained through the application of IPTW26,27.
To establish the propensity-score–matched model for OS, a greedy, nearest neighbor matching algorithm was employed to match patients treated with valve-sparing root replacement (VSRR) to patients treated with aortic root replacement (ARR), with a 1:2 ratio, based on their propensity scores. The maximum permissible difference in propensity scores was set at 2%. Covariate balance was evaluated by analyzing the standardized difference of means, with an absolute value of the mean difference <0.1 considered indicative of successful matching. Subsequently, Kaplan-Meier estimators were calculated for both groups and were compared using the log-rank test. In the final OS model, IPTW-adjusted Kaplan-Meier estimators were calculated for the entire patient cohort and were contrasted between treatment groups via the log-rank test. Participants were further stratified into subgroups according to specific criteria: age, BMI, degree of aortic regurgitation, presence or absence of Marfan syndrome, and bicuspid aortic valve. Cox regression analysis was subsequently conducted on the data pertaining to each subgroup. To ascertain whether there was an interaction effect between the grouping variables and the treatment factors, heterogeneity among the subgroups was assessed using a test for interaction (P for interaction).
The primary objective of this study was to compare the OS of patients with acute type A aortic dissection (AAD) treated conservatively with ARR versus those surgically treated with VSRR.OS was measured from the date of diagnosis to the date of death as a result of any cause. A significance level of P < 0.05 indicated statistically significant differences, with all P-values being two-sided. All necessary calculations were executed utilizing R software, version 4.4.0, as well as SPSS version 26.
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Data availability
Data supporting the findings of this study are available in the article and its Supplementary information. The data underlying this article is under restricted access due to the inclusion of confidential patient information. For any questions, please contact the corresponding author.
References
Wallen, T. et al. Elective aortic root replacement in North America: analysis of STS adult cardiac surgery database. Ann. Thorac. Surg. 107, 1307–1312 (2019).
Ram, E. et al. Valve sparing vs composite valve graft root replacement: propensity score-matched analysis. Ann. Thorac. Surg. 117, 69–76 (2023).
Levine, D. et al. Valve-sparing root replacement versus composite valve graft root replacement: analysis of more than 1500 patients from 2 aortic centers. J. Thorac. Cardiovasc. Surg. 168, 770–780.e6 (2023).
Bethancourt, C. N. et al. Valve-sparing root replacement versus bio-Bentall: inverse propensity weighting of 796 patients. Ann. Thorac. Surg. 113, 1529–1535 (2022).
Yamabe, T. et al. Incidence, cause, and outcome of reinterventions after aortic root replacement. Ann. Thorac. Surg. 113, 25–32 (2022).
Kalra, K. et al. Regurgitant bicuspid aortopathy: is valve-sparing root replacement equivalent to Bentall procedure? Ann. Thorac. Surg. 112, 737–745 (2021).
Nguyen, S. N. et al. Bicuspid-associated aortic root aneurysm: mid to long-term outcomes of David V versus the bio-Bentall procedure. Semin. Thorac. Cardiovasc. Surg. 33, 933–943 (2021).
Yamabe, T. et al. Assessment of long-term outcomes: aortic valve reimplantation versus aortic valve and root replacement with biological valved conduit in aortic root aneurysm with tricuspid valve. Eur. J. Cardiothorac. Surg. 59, 658–665 (2021).
Leontyev, S. et al. Early and late results after David vs Bentall procedure: a propensity matched analysis. Ann. Thorac. Surg. 110, 120–126 (2020).
Gaudino, M. et al. Biological solutions to aortic root replacement: valve-sparing versus bioprosthetic conduit. Interact. Cardiovasc. Thorac. Surg. 24, 855–861 (2017).
Gaudino, M., Lau, C., Munjal, M., Avgerinos, D. & Girardi, L. N. Contemporary outcomes of surgery for aortic root aneurysms: a propensity-matched comparison of valve-sparing and composite valve graft replacement. J. Thorac. Cardiovasc. Surg. 150, 1120–1129.e1 (2015).
Bentall, H. & De Bono, A. A technique for complete replacement of the ascending aorta. Thorax 23, 338–339 (1968).
Brown, J. M., O’Brien, S. M., Wu, C., Sikora, J. A., Griffith, B. P. & Gammie, J. S. Isolated aortic valve replacement in North America comprising 108,687 patients in 10 years: changes in risks, valve types, and outcomes in the Society of Thoracic Surgeons National database. J. Thorac. Cardiovasc Surg. 137, 82–90 (2009).
David, T. E. & Feindel, C. M. An aortic valve-sparing operation for patients with aortic incompetence and aneurysm of the ascending aorta. J. Thorac. Cardiovasc Surg. 103, 617–621 (1992).
Elbatarny, M. et al. Valve-sparing root replacement versus composite valve grafting in aortic root dilation: a meta-analysis. Ann. Thorac. Surg. 110, 296–306 (2020).
Pantaleo, A. et al. Biological versus mechanical Bentall procedure for aortic root replacement: a propensity score analysis of a consecutive series of 1112 patients. Eur. J. Cardiothorac. Surg. 52, 143–149 (2017).
Ho, D. E., Imak, K., King, G. & Stuart, E. A. Matching as non parametric preprocessing for reducing model dependence in parametric causal inference. Political Anal. 15, 199–236 (2007).
Thoemmes F. Propensity Score Matching in SPSS, 2012. https:// arxiv.org/abs/1201.6385 (2014).
Williams, J. B. et al. Contemporary results for proximal aortic replacement in North America. J. Am. Coll. Cardiol. 60, 1156–1162 (2012).
Kari, F. A. et al. Residual and progressive aortic regurgitation after valve-sparing root replacement: a propensity-matched multi-institutional analysis in 764 patients. Ann. Thorac. Surg. 101, 1500–1506 (2016).
Esaki, J. et al. Clinical outcomes of the David V valve-sparing root replacement compared with bioprosthetic valve-conduits for aortic root aneurysms. Ann. Thorac. Surg. 103, 1824–1832 (2017).
Esaki, J. et al. The David V calve-sparing root replacement provides improved survival compared with mechanical valve-conduits in the treatment of young patients with aortic root pathology. n Thorac. Surg. 102, 1522–1530 (2016).
Erbel, R. et al. 2014 ESC Guidelines on the diagnosis and treatment of aortic diseases: document covering acute and chronic aortic diseases of the thoracic and abdominal aorta of the adult. The Task Force for the Diagnosis and Treatment of Aortic Diseases of the European Society of Cardiology (ESC). Eur. Heart J. 35, 2873–2926 (2014).
Hiratzka, L. F. et al. 2010 ACCF/AHA/AATS/ACR/ASA/SCA/SCAI/SIR/STS/SVM guidelines for the diagnosis and management of patients with thoracic aortic disease: executive summary: a report of the ACCF/AHA/AATS/ACR/ASA/SCA/SCAI/SIR/STS/SVM. Circulation 121, 1544–1579 (2010).
Kouchoukos, N. T., Wareing, T. H., Murphy, S. F. & Perrillo, J. B. Sixteen-year experi ence with aortic root replacement. Results 172 Oper. Ann. Surg. 214, 308–318 (1991).
Bruxvoort, K. et al. Association between 2-dose vs 3-dose Hepatitis B vaccine and acute myocardial infarction. JAMA 327, 0 (2022).
Iacoboni, G. et al. Recent bendamustine treatment before apheresis has a negative impact on outcomes in patients with large B-cell lymphoma receiving chimeric antigen receptor T-cell therapy. J. Clin. Oncol. 42, 0 (2023).
Acknowledgements
This work was supported by the National Natural Science Foundation of China (grant numbers 82241209, 82241210); Joint Funds for the Innovation of Science and Technology, Fujian Province (grant number 2020Y9067); Fujian Provincial Special Reserve Talents Fund (grant number 2021-25); Key Laboratory of Cardio-Thoracic Surgery (Fujian Medical University); Fujian Province University Construction Project (grant number 2019-67); Startup Fund for Scientific Research, Fujian Medical University (grant numbers 2020QH2026, 2023QH1031, and 2023QH1038); and Fujian Provincial Centre for Cardiovascular Medicine Construction Project (grant number 2021-76).
Author information
Authors and Affiliations
Contributions
L. Chen (First Author): Conceptualization, Methodology, Software, Investigation, Resources, Supervision, Formal Analysis, Validation Writing—Original Draft. Y.C Pan, H.J Zhang and Chunsheng Wang: Data Curation, Visualization, Investigation, Writing—Original Draft. Y Chen, Z.H Qiu and H Lu: Visualization, Writing—Review and Editing. L.W Chen (Corresponding Author): Conceptualization, Funding Acquisition, Resources, Supervision, Writing—Review and Editing.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Communications thanks Anoop Shah, and the other, anonymous, reviewer(s) for their contribution to the peer review of this work. A peer review file is available.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Chen, L., Pan, Y., Zhang, H. et al. Propensity score matching analysis of valve-sparing versus aortic root replacement in type A aortic dissection patients. Nat Commun 16, 1238 (2025). https://doi.org/10.1038/s41467-025-56509-2
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41467-025-56509-2
This article is cited by
-
Management strategies for acute type A aortic dissection during pregnancy: a single-center retrospective experience
BMC Pregnancy and Childbirth (2026)