Abstract
We evaluated associations among exposure to prenatal phthalate metabolites, perturbations of the newborn metabolome, and infant neurobehavioral functioning in mother-newborn pairs enrolled in the Atlanta African American Maternal-Child Cohort during 2016–2018. We quantified eight phthalate metabolites in prenatal urine samples collected between 8- and 14-weeks’ (visit 1; n = 216) and 24- and 30-weeks’ gestation (visit 2; n = 145) and metabolite features in newborn dried-blood spot samples collected at delivery. Associations between phthalate metabolite concentrations and metabolic feature intensities at both visits were examined using adjusted generalized linear models (MWAS). Then, an exploratory meet-in-the-middle (MITM) analysis was conducted in a subset with NICU Neonatal Neurobehavioral Scale (NNNS) scores (visit 1 n = 81; visit 2 n = 71). In both the MWAS and MITM, many of the confirmed metabolites are involved in tyrosine and tryptophan metabolism, including tryptophan, tyrosine, thyroxine, and serine. This analysis elucidates how prenatal phthalate exposure disrupts the newborn metabolome and infant neurobehavioral outcomes.
Similar content being viewed by others
Introduction
Phthalates are a group of chemicals invented in 1907 and used to manufacture an extensive range of products, including vinyl flooring, soaps, shampoos, and oil. These additives make products and plastics more durable by improving flexibility or retaining color, scent, or shine, and have become integral to modern human life1. In 2020, the increasing demand for plastic created a $10 billion market for phthalic anhydride, the principal precursor of phthalates, despite growing concern over the health and safety of the product. As these chemicals are ubiquitous, people are routinely exposed as they interact with their environment2,3,4. Exposures occur through eating and drinking products that have come in contact with the chemical and through the use of personal care products, cosmetics, perfumes, and clothing that contain the additive. Exposure also occurs through inhalation of dust or particles contaminated with phthalates1. After entering the body, phthalates are metabolized rapidly and excreted in urine, and therefore, recent exposure can be assessed through measurement of primary and secondary urinary metabolite levels (Table S1)2. Most individuals in the United States (US) population, if not all, have detectable levels of phthalates3. There are differences in exposure level depending on a person’s demographic characteristics, with women more likely to have higher urinary concentrations than men3 and Black individuals having higher urinary concentrations than white individuals3,4. Further, Black women generally had higher cumulative exposures to phthalates compared to white women4,5. This is likely due, at least in part, to differences in the use of personal care products (e.g., hair products), stemming from environmental racism, including the role of discriminatory marketing practices6,7.
Phthalates are considered endocrine-disrupting chemicals (EDCs) and can interrupt or interact with human hormones8. So, although humans are exposed to low levels when interacting with the environment, these chemical compounds, like hormones, can still have an impact on health (non-monotonic toxicity)8,9. The widespread use of the chemicals across a myriad of daily products and the high potential for exposure have raised concerns about the impact on human health. Research has demonstrated that phthalate exposures are associated with different health outcomes10, but most significantly impact reproductive and child health11. It is especially concerning that phthalates can cross the placental barrier and affect normal embryonic and fetal development12. Previous research has shown a link between prenatal urinary phthalate levels and impacts on neurobehavioral development in low-risk infants13,14,15. Specifically, prenatal exposure to phthalates and its interaction with the maternal endocrine system has been associated with Apgar scores 5 min after delivery1,2,3,4,5,6,7,8,9,10,11,12,13,14,15. Further, Yolton et al. found that prenatal di(2-ethylhexyl) phthalate (DEHP) metabolite levels measured at 26 weeks gestation were associated with nonoptimal reflexes, measured using NICU Network Neurobehavioral Scale (NNNS) scores, in 5-week-old male infants in a cohort of 350 mother/infant pairs13. Similarly, Kim, et al. found that DEHP metabolite levels measured in the third trimester were inversely associated with mental and psychomotor indices (Bayley Scales of Infants Development 2nd edition) measured at 6 months old in a cohort of 460 expectant mothers14. Understanding how intermediate biomarkers might underpin these associations could inform causal links or serve as metabolic markers for early intervention.
Despite these potential impacts on maternal and child health, only a handful of studies have focused on phthalate-associated effects on maternal metabolism while pregnant. One study examined the effects of phthalates on the maternal metabolome, analyzing serum samples obtained during the third trimester, as well as the impact of phthalates on the placental metabolome16. This research did not see an association between phthalates and maternal serum samples but did see perturbations in a mixtures analysis between phthalates and the placental metabolome, with reduced concentrations of 2-hydroxybutyrate, carnitine, O-acetylcarnitine, glucitol, and N-acetylneuraminate16. Another study looked at how phthalate levels were associated with the metabolome of pregnant African Americans17. Results indicated perturbations in biological pathways and individual metabolites involved in inflammation, oxidative stress, and endocrine disruption. Although these studies have contributed significantly to our understanding of phthalate-related changes in maternal and placental metabolomes, there is no prior study describing how prenatal urinary phthalate levels relate to the newborn metabolome. Evaluating the biological mechanisms linking prenatal exposure to phthalates with alterations in the newborn metabolome is crucial for elucidating early-life metabolic perturbations associated with these compounds and the corresponding health effects. This is particularly important given the well-documented health impacts of phthalates, especially in underserved and vulnerable populations.
In a well-established prospective cohort of pregnant African American people and their infants, we first sought to investigate the relationship between prenatal urinary phthalate levels and perturbations in the newborn metabolome. Based on these initial metabolomics results and previous epidemiological research13,14,15, we also hypothesized that urinary phthalate levels may interfere with infant neurodevelopment (evaluated by NNNS scores) through perturbations in the newborn metabolome. To test this hypothesis, we conduct an exploratory metabolomics analysis to further examine the potential mechanisms behind prenatal exposure to phthalates and neurobehavioral outcomes by identifying potential intermediate biomarkers between phthalate exposure and NNNS scores within a subset of the same population using a meet-in-the-middle (MITM) approach.
Results
Study population and exposure levels
In the main metabolomic-wide association study (MWAS), we evaluated a total of 216 participants with urinary phthalate data from prenatal visit 1(8-14 weeks gestation) and 145 participants with urinary phthalate data from prenatal visit 2 (24–30 weeks gestation). In the subset used for the MITM analysis (which required newborn metabolome and NNNS data), there were 81 participants with phthalate exposure data from prenatal visit 1 and 71 with phthalate exposure data from prenatal visit 2. Characteristics of participants with data from across the different visits and between the full sample MWAS and the subset were similar (Table 1). Characteristics from both subsets did not differ from the larger Atlanta African American Maternal-Child Cohort (Table S2). Participants were in their mid-20s, and most had a high school education or higher. For most of the participants (57%), the pregnancy captured in this study was not their first. Participants did report substance use during pregnancy, with ~10% reporting alcohol use, ~15% reporting tobacco use, and ~40% reporting marijuana use.
The phthalate metabolite levels were summarized for each visit in the full sample (Table 2) and in the subset (Table S3). All phthalate metabolites were found in 100% of samples. In the full sample, urinary phthalate levels were compared to the geometric mean levels reported by the National Health and Nutrition Examination Survey (NHANES) during the same study period (2015-2016) in both the general US population aged 20 years or older and in non-Hispanic Blacks18. For MEP, the geometric mean levels at both clinical visits were higher than the levels of people aged 20+ and non-Hispanic Blacks. The geometric mean level of MEHP at both clinical visits was higher than the levels reported among non-Hispanic Blacks in the NHANES data. The other phthalate levels were comparable to the NHANES levels. Correlations of phthalate metabolites within and across visit are summarized for the full sample (Figure S3). Within visits, only phthalate metabolites that are related to DEHP (MEHP, MEOHP, MEHHP, and MECPP) were highly correlated. Across visits, phthalate metabolites were not highly correlated.
High-resolution metabolomic profiling
After data quality filtering, 13,680 peaks were filtered out, and 7191 total metabolic features remained. In the MWAS with visit 1 at p < 0.05, there were 224, 687, 282, 349, 501, 289, 292, 394, and 365 features associated with MEP, MBP, MiBP, MBzP, MEHP, MEOHP, MEHHP, MECPP, and \(\Sigma\)DEHP, respectively (Table S4). In the MWAS with visit 2 at p < 0.05, there were 260, 354, 634, 304, 349, 426, 304, 488, and 393 features associated with MEP, MBP, MiBP, MBzP, MEHP, MEOHP, MEHHP, MECPP, and \(\Sigma\)DEHP, respectively (Table S4). These significant features were used for the pathway analysis. There were fewer features associated with urinary phthalate levels after correcting for multiple testing (q < 0.2; Table S4). These features were used in chemical annotation.
The metabolites associated with each phthalate exposure and either attention or arousal are summarized in Table S5. Generally, <50 metabolomic features met the threshold (p < 0.05), and visit 2 had more significant overlapping features than visit 1. These features were used in the MITM analysis chemical annotation.
Pathway analysis
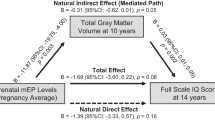
Using mummichog19, we investigated the enrichment of endogenous metabolic pathways with features significantly associated with each phthalate metabolite (p < 0.05). There were 28 perturbed metabolic pathways associated with phthalate measured in visit 1 and 12 in visit 2. Eleven pathways were identified in both visits (Fig. 1). Many of the pathways identified were involved in oxidative stress, acute inflammatory response, and low-grade inflammation, such as vitamin metabolism (vitamin K, H, B6, B5, E, and B3), tyrosine metabolism, tryptophan metabolism, the urea cycle, and pyruvate metabolism (Figs. 1 and S4).
Chemical identification
Newborn metabolomic signals were identified by comparing them to North Carolina’s Human Health Exposure Analysis Resource (HHEAR) Hub’s in-house experimental standards library (IESL). After correcting for multiple testing (q < 0.2), 24 confirmed metabolites of the newborn metabolome associated with prenatal visit 1 phthalate metabolites and six confirmed newborn metabolites associated with prenatal visit 2 phthalate metabolites. In visit 1 analyses, the majority (21 metabolites) were associated with MBP, and the remaining were associated with MEHP. In visit 2 analyses, one newborn metabolite was associated with MBP, three with MECPP, and two with both MECPP and MEOHP (Table 3). Annotated endogenous metabolites seemed to be generally involved in neurological health through perturbations in metabolites and pathways involved in tryptophan metabolism, linoleic acid metabolism, and tyrosine metabolism (Table 3; Fig. 2).
Items in circles denote pathways and items in rectangle boxes denote metabolites. Blue pathways and metabolites were found in visit 1 (V1). Orange pathways and metabolites were found in visit 2 (V2). Black pathways and metabolites were found in both visits. Gray pathways and metabolites are provided for biological context but were not explicitly identified in this research. Solid arrows represent metabolites directly upstream/downstream of each other. Dashed lines represent a biochemical pathway linking metabolites not shown for clarity. Up arrows represent a positive association and down arrows a negative association. Twenty metabolites were not included, as no clear biological link was identified (see Table 3). Those marked with the maternal metabolome symbol were identified in a paper looking at the metabolic perturbations from phthalates in the maternal metabolome in this same cohort17. Source data are provided as a Source Data file.
In the MITM analysis, no significant signals were associated with both exposure and outcome after correcting for multiple testing (q < 0.2). At a p < 0.05 threshold, there were 12 confirmed newborn metabolites for visit 1 and 21 identified newborn metabolites for a visit 2 that were associated with at least one phthalate metabolite and one of the NNNS outcomes. Annotated endogenous metabolites, including tyrosine, 5-hydrotyptophan, serotonin, serine, and phenylalanine, were involved in neurological health and inflammation through perturbations in tryptophan metabolism, glycine, serine, and threonine metabolism, and fatty acids (Table 4, Fig. 3).
Sankey plots in a are from visit 1 (n = 81), and b are from visit 2 (n = 71). The first node is the phthalate exposures, leading to the associated metabolites in the second node, and ending at the NNNS outcomes, attention and arousal, in the last node. The yellow/blue colors on the left-hand side indicate different phthalate metabolites. The red colors on the right-hand side differentiate attention (dark red) and arousal (light red) or both (orange) outcomes. Only significant, annotated findings are displayed in this figure; for details on the significance level and beta values, please see Table 4. Source data are provided as a Source Data file. MEP Monoethyl phthalate, MBP Mono-n-butyl phthalate, MiBP Monoisobutyl phthalate, MBzP Monobenzyl phthalate, MEHP Mono-2-ethylhexyl phthalate, MEOHP Mono-2-ethyl-5-oxohexyl phthalate, MEHHP Mono-2-ethyl-5-hydroxyhexyl phthalate, MECPP Mono-2-ethly-5-carboxypentyl phthalate, \(\Sigma\)DEHP Sum of Di-2-ethylhexyl phthalate metabolites.
Discussion
Using cutting-edge, targeted exposure assessment and untargeted metabolomics methodologies, this study identified and characterized associations among in utero exposure to phthalates, perturbations of the newborn metabolome, and measures of infant neurodevelopment. To our knowledge, this is the first study to use newborn DBS metabolomics to understand how prenatal exposure to phthalates perturb the newborn metabolome and how these perturbations could provide a molecular mechanism for impacts on NNNS scores.
Compared to NHANES, the geometric mean levels of MEP and MEHP at both clinical visits were higher in our study population than the levels of US adults (20 and older) as well as US non-Hispanic Blacks. Of note, MEP is the more abundant phthalate metabolite generally found in populations18. Taken together, these results support the existence of environmental disparities in phthalates exposures and suggest that we need further regulation on phthalates targeted at pregnant people generally and especially pregnant African American people.
Many of the pathways identified in the full study sample were involved in oxidative stress and acute and systemic inflammatory response, including vitamin K, H, B6, B5, E, and B3 metabolism, tyrosine metabolism, and tryptophan metabolism (Figs. 1 and S4). Further, there were more unique pathways associated with prenatal visit 1 than prenatal visit 2, suggesting that the timing of the exposure in gestation might have differential biological impacts (Fig. 1). For example, pathways associated with visit 1 only include leukotriene and arachidonic metabolism, which are highly inflammatory20.
These findings, along with the observed variances in metabolite perturbations across visits 1 and 2 and the differential associations of various phthalate metabolites with distinct gestational stages, suggest potential implications for fetal development. In early pregnancy (visit 1), major development of the central nervous system, eyes, teeth, genitalia, and refinement of the limbs and heart are taking place. Whereas later pregnancy (visit 2) primarily entails refinement processes within these systems, particularly focusing on central nervous system maturation and refinement within the eyes and genitalia21. The absence of significant impacts on later gestational periods does not preclude potential effects during the critical phases of early embryogenesis. These findings underscore the necessity for targeted investigations spanning the entirety of gestation and advocate for nuanced consideration of pregnancy timing when evaluating environmental exposures.
Based on the annotated metabolites in the full sample, we hypothesized three potential underlying mechanisms (Table 3, Fig. 2). In line with the pathway results, many of the annotated metabolites centered around tyrosine and tryptophan metabolism and are involved in abnormal neurodevelopment and brain maturation. Among the annotated metabolites, tyrosine stands out as a crucial neurotransmitter and, in this study, was associated with downregulation after exposure to phthalates22. Serine plays a key role as a neurotransmitter precursor, and tryptophan is essential to brain development23,24. Both were associated with an upregulation in response to MBP exposure, potentially as a protective response. Additionally, the presence of thyroxine, a thyroid hormone, is noteworthy, as low levels of this hormone have been associated with increased susceptibility to illness and neurodevelopmental issues in newborns25. This was downregulated in response to MBP exposure. Finally, the metabolite dihomo-gamma-linoleate within linoleic acid metabolism was associated with a downregulation by MBP exposure. This polyunsaturated fatty acid is a component of neural membranes26. Its significance for newborn health is emphasized by its abundance in breastmilk27. The interplay of metabolites within these pathways emphasizes the potential impact of phthalates, specifically MBP, on abnormal neurodevelopment, underlining the need for closer examination of this exposure and its intricate biochemical influences on brain maturation during this critical developmental period.
We observed similar and consistent findings in the same cohort when examining disruptions to the maternal metabolome in response to urinary phthalate levels previously17. Specifically, we observed biological perturbations in the maternal metabolome centering around tyrosine metabolism and also identified perturbations to tyrosine and thyroxine17. These robust and consistent observations underscore the potential interconnectedness of maternal and fetal metabolic responses to environmental exposures, emphasizing the need for a comprehensive understanding of these perturbations for both maternal and infant health.
As many of the endogenous annotated metabolites were involved with neurological function, an exploratory MITM analysis was conducted in a smaller subset of the participants with infant NNNS scores available. Many of the annotated endogenous metabolites from the MITM analysis were also part of tryptophan and tyrosine metabolism (Table 4, Fig. 3). Within tyrosine metabolism, phthalate metabolites were associated with a downregulation of tyrosine and a subsequent negative association with attention scores. This connection is especially pertinent considering that attention and arousal, key symptoms associated with clinical tyrosine deficiency and deficits in amino acids within the tyrosine metabolic pathway, play a crucial role in neurological function. Phthalate metabolites were associated with a downregulation of 5-hydrotryptophan, a precursor of the neurotransmitter serotonin, as well as serotonin itself28,29, both of which are also part of tryptophan metabolism. Both 5-hydroxytryptophan and serotonin were associated with a decrease in arousal scores. Serine and phenylalanine, both neurotransmitter precursors23,30, were associated with a downregulation in response to urinary phthalate levels and then subsequently related to a negative association with attention scores. The observed associations between phthalate metabolites and downregulation of key neurotransmitter precursors, coupled with negative impacts on attention and arousal scores, suggest that phthalates may have long-term developmental consequences for these infants. This study highlights the importance of further targeted research into tryptophan and tyrosine metabolism in both infants and children to understand their role in development.
We also identified and confirmed exogenous environmental metabolites from both the MWAS and the MITM analysis (Table 4). This underscores the capability of metabolomics to identify novel environmental exposures simultaneously, highlighting its utility in uncovering novel factors that may impact maternal and newborn health. For example, a fungicide (oxadixyl) was identified in the MWAS, and pesticides (propham and flonicamid) were identified in the MITM analysis. The interaction of these exposures with phthalates could be considered in future analyses. Further, biomarkers commonly associated with cigarette smoking were identified in both the MWAS (trans-3’-hydroxycotinine and (R)-N-Acetyl-S-(1-(hydroxymethyl)-2-propen-1-yl)-L-cysteine) and the MITM (cotinine, N-Acetyl-S-(3-hydroxypropyl-1-methyl)-L-cysteine, and (R)-N-Acetyl-S-(1-(hydroxymethyl)-2-propen-1-yl)-L-cysteine) analysis31,32,33,34. In a separate MITM study within the same cohort that investigated the effects of maternal cotinine on the maternal metabolome, serine emerged as a perturbed metabolite35. This finding aligns with the present study, as serine was identified in both the MWAS and MITM analysis. It is important to consider the interpretation of these findings within the context of exposure to complex mixtures. When conducting our statistical modeling, we considered each phthalate independently as a surrogate of exposure. Thus, an observed metabolic perturbation associated with a particular phthalate may not necessarily indicate a causal association between the metabolic feature and that specific modeled indicator. Instead, such change may be more likely associated with multiple, correlated pollutants within a complex exposure mixture. This consistency in perturbed metabolites across different studies with varied single exposures suggests that future research should consider the cumulative impact of multiple exposures, integrating the analysis of a mixture approach36,37,38. By doing so, we can enhance our comprehension of how multiple components of the exposome collectively influence health outcomes.
We also identified metabolites in the MWAS, including 3-hydroxyhippuric acid and hydroxyphenylacetic acid, which are related to the microbiome39,40. Metabolomics has the potential to highlight areas for further exploration within the microbiome, offering insights into how microbial composition and activity may influence metabolic pathways. Although investigating the microbiome is beyond the scope of this research, it is crucial to consider factors such as the type of birth (vaginal or cesarean) when studying newborn populations. These factors can significantly impact the microbiome and subsequent metabolic profiles. Therefore, future studies should ensure sample sizes are sufficiently large to allow for stratification based on these variables.
This study had several notable strengths. First, this is a well-established, socioeconomically diverse African American prospective birth cohort with validated processes for exposure measurements and metabolic data collection from newborn DBS samples. As this is a prospective cohort design, we also had well-established temporality between the exposure and outcome. Next, this study leveraged both an untargeted MWAS and MITM framework to identify and measure links between phthalate exposures, metabolomics signatures, and infant health outcomes. Finally, this research is among an all-African-American population, a group that is currently underrepresented in this existing literature with a higher risk of exposure to environmental contaminants such as phthalates, compared to their white counterparts6. The study also had several limitations to note. This study was limited to US-born participants without active chronic medical conditions or chronic medication use, limiting the generalizability of these results to populations with these characteristics. There were also limitations to consider with the covariate set. First, there was also no information on diet available, which would be an important covariate with phthalates, as much of the human exposure is from food and drink packaging1. Future studies looking at phthalate exposure should collect this information. Next, there was no information available from the substance use variables on frequency, intensity, and duration of use, information future studies could collect to prevent residual confounding. Further, as this is a pregnancy cohort, women may have underreported their use due to social desirability bias, introducing the potential for misclassification bias. However, reported use of alcohol and tobacco in this population is only slightly lower than national estimates and use of marijuana are higher than national estimates41, so we hypothesize any effect from this bias would be minimal. Beyond covariates, the phthalate measurement was a one-time snapshot of an exposure level that is dynamic and can change over time, which could misrepresent an individual’s overall exposure experience, although research indicates a one-time sample can be representative42. Additionally, this research only focused on exposures to individual phthalate metabolites, and as demonstrated in this study, there could be other co-exposures that may contribute to the true effect of this environmental contaminant on health. Further, a study in this cohort demonstrated the observed negative association between environmental contaminants and adverse pregnancy outcomes can strengthen when including psychosocial stressors as an additional exposure43. Although beyond the scope of the current work, future studies could utilize mixture methods to consider additional contaminants and psychosocial stressors, especially as this population experiences discrimination on the basis of both race and gender38. Additionally, this research considered each timepoint cross-sectionally. Future studies should consider more sophisticated approaches to independently assess the effects of multiple exposure time points on the metabolomic profile. However, our current approach serves as a foundational step in understanding the temporal dynamics of phthalate exposure and its impact on the newborn metabolome. Next, due to the highly multidimensional analysis, there is an increased risk for type I errors. This was addressed by imposing stringent criteria whenever possible throughout the analysis, including applying the Benjamini-Hochberg FDR. Unfortunately, for the MWAS pathway analysis and the entirety of the MITM analysis, we could not use FDR-corrected significance thresholds due to the limited statistical power resulting from the sample size, as the more stringent threshold would not include a sufficient number of metabolic features to conduct a meaningful pathway analysis or have MITM results. Therefore, these results should be carefully interpreted and confirmed using additional studies with larger sample sizes. The use of less invasive techniques for metabolomics studies, such as newborn DBS, could facilitate larger cohorts. Regarding newborn DBS samples obtained through heel-sticks, issues have been pointed out, such as uneven cell distribution, cell lysis, hematocrit variation, and pre-analytical clotting when employing untargeted metabolomics analysis on this biomatrix44,45,46. Despite the normalization of untargeted DBS metabolomics analysis based on the size and weight of the DBS, limitations in sample volume prevented the application of additional, potentially more optimal normalization methods, such as adjustments for hemoglobin, specific gravity, protein, or potassium47. Further, as this investigation used a single, 15-mm punch, this sample may not represent larger portions of blood because of potential variation in signals dependent on spotting and drying time. Using NNNS scores as an outcome presents certain considerations. The design of NNNS is intended to encompass a broad spectrum of neurobehavioral domains, including attention and arousal. While this lack of specificity might limit its precision in pinpointing specific clinical phenomena, it enables the test to capture general trends in infants. This broader scope facilitates comparability across infants within a study population48. Although NNNS scores may not provide clinical recognition of a specific condition, their ability to highlight general trends offers valuable insights into both present and future neurobehavioral function49,50,51. Finally, there are fewer assumptions required for using the MITM framework compared to formal mediation analysis, and the results are suggestive of future hypothesis testing in other samples and should be interpreted with caution.
Taken together, this research supports the current mechanistic understanding of how prenatal phthalate exposure influences the newborn metabolome and how these biological perturbations might impact neurobehavioral outcomes. Additional research is needed to evaluate the generalizability of these findings, test for differences between African Americans and other populations, incorporate additional co-exposures, and investigate the potential of these metabolic responses for detection, treatment, and prevention strategies in public health and clinical settings.
Methods
Study population
The project utilizes data from the Atlanta African American Maternal-Child Cohort, a prospective cohort that recruited pregnant African American individuals from Grady Memorial Hospital and Emory University Hospital Midtown since 201452. The study was approved by the Emory University Institutional Review Board, and all participants provided written informed consent prior to enrollment.
Participants were eligible for the study if they self-reported non-Hispanic African American or Black race, were US-born, 18–40 years old, and were pregnant with a singleton fetus between 8 and 14 weeks gestation. As the primary goal of this cohort was to identify what may be contributing to adverse birth outcomes in African Americans in otherwise healthy women, participants were excluded if there was any active diagnosis of chronic medical conditions or chronic use of prescription medications (verified through the prenatal medical record). The study participants included in the metabolome-wide association study (MWAS) were further restricted to mother-newborn pairs with mothers who had urine samples available for the determination of urinary phthalate levels and newborns with metabolomics profiles from dried blood spot (DBS) samples (visit 1 n = 216; visit 2 n = 145; Fig. S1). Participants could be in visit 1 only (n = 76), visit 2 only (n = 5), or represented in both visits (n = 140). The MITM analysis was further subset to those mother-newborn pairs for whom NNNS data was available (visit 1 n = 81; visit 2 n = 71). For the cohort, prenatal data was collected during two clinical visits: the first collection was targeted to occur during the 8–14 week gestational period and the second during the 24–30 week gestational period. During the first visit in early pregnancy, sociodemographic data such as maternal age and education were collected from self-reported surveys and from prenatal administrative records review. Health information was completed by self-report, including prior pregnancies (if any) and substance use. For substance use, medical records were reviewed for reported use prior to pregnancy, and use during pregnancy was self-reported. During the first and second visits, prenatal urine samples were collected (and assayed as described below), and clinical data (such as height and weight, from which maternal body mass index and weight gain were calculated) were collected. Additionally, after delivery, medical record abstraction was used to ascertain the infant’s gestational age at birth, weight, and sex. Covariate information used in this analysis was pulled from these data sources.
Exposure collection
Previous research has demonstrated that a one-time urine sample can capture a representative picture of recent phthalate exposure, even with the relatively short half-life (around 12 h)42 of these compounds. Metabolites of eight phthalates were measured in urine collected during the two prenatal clinical visits (Table S1). These phthalate metabolites were: monoethyl phthalate (MEP), mono-n-butyl phthalate (MBP), monoisobutyl phthalate (MiBP), monobenzyl phthalate (MBzP), mono-2-ethylhexyl phthalate (MEHP), mono-2-ethyl-5-oxohexyl phthalate (MEOHP), mono-2-ethyl-5-hydroxyhexyl phthalate (MEHHP), and mono-2-ethyl-5-carboxypentyl phthalate (MECPP). Briefly, urine samples (0.5 ml) were mixed with stable isotopically labeled analogs of the phthalate metabolites and 2000 units of β-glucuronidase in 1 mM ammonium acetate (pH 5) buffer and incubated overnight at 37 °C13. Then, enzyme activity was terminated by adding 0.15 M sodium phosphate buffer to the sample. Phthalate metabolites were extracted using the Bond Elut solid phase extraction cartridge (Agilent Technologies, Inc., Santa Clara, CA). These samples were reconstituted with Milli-Q water, and the target compounds were separated using high-performance liquid chromatography on a Betasil Phenyl (3μ,150 × 2.1 mm) (Thermo Scientific, San Jose, CA) analytical column and finally were analyzed by tandem mass spectrometry on an Agilent 6460 triple quadrupole mass spectrometer (Agilent Technologies, Inc). Concentrations were derived from a regression analysis of the peak area of the analyte ion divided by the peak area of the internal standard ion and the calibrant concentrations. Quality assurance and control procedures were also incorporated into the analyses (i.e., analyses of NIST reference materials and quality control samples). The analytical method was certified by successful participation in the German External Quality Assessment Scheme.
As MEHP, MEHHP, MEOHP, and MECPP are metabolites of the same phthalate exposure, DEHP, these exposures were considered together as the molar sum of these analytes (\(\Sigma\)DEHP). The molar sum of DEHP metabolites was calculated using the following formula17,53:
As previously described, the limits of quantification (ng/mL) for these phthalates metabolites were: 1.0 (MEP), 4.0 (MBP), 2.0 (MiBP), 0.2 (MBzP), 0.2 (MEHP), 0.4 (MEOHP), 0.4 (MEHHP), and 5.25 (MECPP)17. The linear range was 0.01–50 ng/mL for all phthalate metabolites except for MEP, which was 5–500 ng/mL. Samples that fell above those concentrations were diluted and repeated. Accuracy based upon the National Institute of Standards and Technology (NIST) was 91–105%. The percent relative standard deviations were all below 12%. Any values that fell below the LOD were assigned the LOD divided by the square root of 2 (\({LOD}/\sqrt{2}\))54,55. To account for the variability of urine dilution, all exposure variables were creatinine adjusted by adding it as an independent covariate in the final model56,57.
Metabolomic data collection
This study used newborn DBS samples, which are routinely collected shortly after delivery for medical screening and public health surveillance58,59,60,61. Previous research has demonstrated that DBS samples are representative biospecimens of the human metabolome and are comparable to whole blood samples containing serum and plasma while having the added advantage of being less invasive and allowing for insights into the early metabolomic response to prenatal exposures, which are largely understudied61. DBS samples were collected via heel stick within 24–48 h of birth. This procedure followed a standardized protocol, including the disinfection of the skin, sample collection using a 2.5 mm lancet, and obtaining ~75 μL of blood on a Guthrie card62. Samples were stored in a walk-in refrigerator (2–8 °C) for up to three months until they were transferred to Emory University and stored within gas-impermeable bags with dessicant in a freezer (−80 °C) until further processing. The site used consistency in the collection, storage, and shipment of biospecimens, and any signals that quickly degrade or would have variability in degradation due to sample storage time would not be expected to arise as significantly associated with the studied phenotype. In this cohort, single 15-mm punches (~50\(\mu\)L of whole blood) were received from the Guthrie cards between 2016 and 202059.
Untargeted high-resolution metabolomics profiling was performed in a single run at the North Carolina HHEAR Hub, located at the UNC Nutrition Research Institute within the North Carolina Research Campus (Kannapolis, NC), using established methodologies58,63,64. Briefly, DBS samples underwent extraction with 1 mL ice-cold methanol, including 500 ng/mL L-tryptophan-d5. The samples were vortexed at 5000 rpm for 10 min and sonicated for an additional 20 min. After centrifugation at 16,000 × g for 10 min at 4 °C, 600 µL of the extracted supernatant was transferred into a 2.0 mL LoBind microfuge tube. A combined 70 µL of the extracted supernatant from all study samples was pooled and then redistributed into new tubes, each containing 600 µL, to generate the total study pool samples. Empty blood spot cards (without blood), matching the size and material of study samples, were used as blanks and processed using identical procedures. The supernatant (70 µL) from each of the blanks was mixed together and then distributed into multiple low-bind 2.0 mL tubes, each containing 600 µL. All supernatant aliquots (600 µL), including study samples, study pools, and blanks, were dried by vacuum concentrator overnight and reconstituted with 100 µL water-methanol (95:5, v/v) for ultra-high performance (UHP) LC-HR-MS analysis. External quality control samples consisted of 50 µL aliquots of NIST reference plasma (SRM 1950) and were prepared using a similar procedure. After study sample randomization, quality control study pools, NIST plasma references, and blanks were interspersed at a rate of 10% among the study samples during the analysis sequence, which was divided into three batches.
The untargeted data was obtained using a Vanquish UHPLC system coupled with a Q Exactive™ HF-X Hybrid Quadrupole-Orbitrap Mass Spectrometer (Thermo Fisher Scientific, San Jose, CA). For analysis, a 5 µL volume was injected. The HSS T3 C18 column (2.1 × 100 mm, 1.7 µm, Waters Corporation) was used to separate metabolites at 50 °C with water and methanol as mobile phases, each containing 0.1% formic acid (v/v). The UHPLC linear gradient was initiated with 2% methanol and then reached 100% methanol in 16 min and was held at this level for 4 min, with a flow rate of 400 µL/minute. The untargeted metabolomics data was acquired in the 70–1050 m/z range using the data-dependent acquisition mode for the MS/MS spectra data. Subsequently, the UHPLC-HR-MS data underwent processing using Progenesis QI (version 2.1, Waters Corporation) for peak identification and alignment. Background signals were excluded if their mean intensity across blanks exceeded that of the quality control study pools based on the unnormalized data. The remaining peaks were normalized using the “normalize to all” feature in Progenesis QI. Signals exhibiting significant differences across the three running batches (with false discovery rate (FDR) correction q < 0.05) were excluded from further analysis. Finally, the metabolomics data was filtered to include only those detected in 95% of serum samples and subsequently log10-transformed to normalize data.
NNNS scores
We evaluated infant neurodevelopmental functioning using the NNNS65. Initially developed for the National Institutes of Health (NIH) to evaluate drug-exposed and at-risk infant, the NNNS is a validated measure of early neurodevelopment in very young infants65. The measure has demonstrated validity across multiple studies, including those with US, and Black participants50,66. The complete assessment was designed to provide comprehensive, theoretically driven, and psychometrically sound measures in 12 subdomains, including attention (i.e., information processing) and arousal (i.e., state control and excitability). Although originally developed for infants prenatally exposed to drugs of abuse, previous research has demonstrated that the scores can be applied to low-risk infants with no known drug exposure49. Further, research has indicated that NNNS scores are associated with differences in behavior in early childhood49,50,51. In this study, the NNNS was administered when infants were on average 2–4 weeks old (corrected for gestational age a birth) by trained and certified research specialists among those whose families agreed to participate in the infant follow-up. The NNNS administration did not vary across the 2–4-week age range. The NNNS was administered in a quiet location in the participant’s home or the lab setting, according to standardized procedures. The measure was administered by one research specialist, with a second research specialist present at the visit, filming the administration for reliability checks. Both examiners were blind to the newborn’s exposure group. All examiners completed a 5-day training program and established adequate inter-rater reliability with a NNNS trainer. Caregivers were present in the home or the lab setting but did not participate in the administration of the NNNS.
NNNS standardized arousal and attention summary scores were created on the basis of confirmatory principal components analyses and were used in the statistical analyses. The first composite score assesses newborn arousal by combining summary scores related to excitability, arousal, the number of calming strategies required by the examiner, physiological signs of stress (e.g., tremors, startles), and the newborn’s self-regulation capacity (reverse scored). Higher scores on this composite indicate increased levels of newborn arousal. The second composite score measures the newborn’s attention, reflecting their ability to respond to, focus on, and track external stimuli. This score is summarized by components related to attention and lethargy (reverse scored), with higher scores indicating more mature levels of newborn attention. In this study, standardized scores were created from the averages of each component. Previously published research has detailed the correlations between NNNS summary scores for this sample and demonstrated that the summary scores in each composite were moderate to highly correlated, supporting the creation of two overarching scores67.
Statistical analyses
We analyzed phthalate metabolite data from the two study prenatal visits cross-sectionally. The use of two separate regression models allows us to examine the potential differential impacts of phthalate exposure during early and late pregnancy, thereby offering preliminary indications of critical periods without the added complexity of a longitudinal analysis that might compromise the integrity of our analysis. A descriptive analysis of selected covariates was conducted with a summary of continuous variables presented using the median and interquartile range (IQR) and categorical variables presented as the count (n) and frequency (%).
For the untargeted MWAS, generalized linear models were applied to examine the association between phthalate metabolite concentrations in early pregnancy (visit 1) and in late pregnancy (visit 2) and newborn metabolic feature intensities. All models controlled for mother’s age, education, parity, alcohol consumption, tobacco use, marijuana use, pre-pregnancy BMI, urine creatinine levels, as well as the baby’s sex and gestational age (GA) in weeks at the time of the study visit. The model took the following form:
Where \({\log }_{10} ({Y}_{{ij}} )\) refers to the normalized (log base 10) intensity of the newborn metabolic feature j for participant i, \(\alpha\) is the intercept, and \({\beta }_{1j}\left({{{{\rm{Phthalate}}}}}_{{{{\rm{i}}}}}\right)\) is one of the nine different phthalate metabolite exposures measured in this study (MEP, MBP, MiBP, MBzP, MEHP, MEOHP, MEHHP, MECPP, and \(\Sigma\)DEHP). \({\epsilon }_{{ij}}\) represents random error. Other covariates were selected through a thorough review of the literature and a directed acyclic graph (Figure S2) to identify covariates that could potentially introduce confounding bias68. The p values obtained from the MWAS were corrected for FDR using the Benjamini-Hochberg procedure since multiple comparisons were made69.
Pathway enrichment analysis
A metabolic pathways enrichment analysis was conducted in the full MWAS to predict the functional biological activity of uncharacterized metabolic features that were associated with at least one urinary phthalate level. Due to a limited number of significant features at the FDR-corrected q < 0.2 threshold (Table S4), the less stringent cutoff of p < 0.05 was used for pathway analyses. All pathway analyses were conducted in Python (version 3.9) using mummichog (version 2.3)19, a bioinformatics tool that is able to utilize the mass spectrometry data from unidentified metabolic features to infer biological pathways. The program further provides an adjusted p value for each pathway by resampling the reference input file, assuming a gamma distribution. To minimize the chance of false positive discoveries, only pathways that had an adjusted p < 0.05 after 1000 permutations were performed, and pathways enriched with \(\ge 10\%\) overlapping signals relative to the pathway size were retained.
Chemical identification and annotation
To avoid false positive matches, only metabolites that met the FDR-corrected q < 0.2 threshold were annotated. Metabolomic signals were identified by comparing them to the NC HHEAR Hub’s IESL, encompassing over 2400 compounds. This library contains both endogenous and exogenous metabolites. The endogenous metabolites are linked to an individual’s metabolism. In contrast, exogenous metabolites are associated with lifetime exposures, such as environmental contaminants, dietary compounds, pharmaceuticals, and secondary metabolites formed after exposure. All standard reference compounds in the IESL were analyzed under identical conditions as the study samples. The same signals were cross-referenced with publicly available databases, including NIST and METLIN, for further verification58.
The matching process involved assigning ontology levels (OL) to signals, indicating the strength of evidence supporting their identification or annotation. These levels considered various factors, including retention time (RT), exact mass (MS), MS/MS fragmentation pattern, and isotopic ion pattern. Metabolites that closely matched the IESL by RT (within ±0.5 min), MS (within <5 ppm), and displayed a high degree of similarity in MS/MS fragmentation patterns (similarity score >30) received an OL1 label. For metabolites matching by RT and MS, they were labeled OL2a. Metabolites that earned an OL1 or OL2a label were considered confidently identified in this study. An OL2b label was assigned to signals that matched the IESL by MS and MS/MS but fell outside the RT window (±0.5 min). These metabolites were often conjugates or isomers that shared similarities with the matched compound in the IESL. Signals matching with MS (<5 ppm) and exhibiting a strong resemblance in experimental MS/MS (similarity score >30) to public databases received a public database (PDa) label. Metabolites confirmed with OL2b and PDa labels were considered as confidently annotated in this study, while those with less confidence were not included in subsequent analyses.
Meet-in-the-middle analysis
The MITM approach has been used by previous research to search for early biological effects and potential intermediate biomarkers in studies of environmental contaminants and reproductive health58,70,71. First, the population used in the larger MWAS was a subset of those with the NNNS score outcome available (Visit 1 n = 81; Visit 2 n = 71). MWAS were run to determine which of the newborn DBS signals were associated with prenatal phthalate exposure and NNNS score. First, the exposure-metabolomic relationships were determined for each urinary phthalate metabolite using a linear model controlling for the same covariate set as the larger MWAS model. A linear model was then run to investigate the metabolomic signal-outcome relationship for NNNS scores, controlling for the same covariate set, except for creatinine, as there were no urinary measures in the model. Chemical identification followed the same procedural steps as outlined in the larger MWAS; however, due to the limited sample size, unadjusted p values (p < 0.05) were used in this exploratory MITM analysis. The metabolites that were identified are indicators of a potential intermediate mechanism that could be explored further in future research.
All analyses were conducted using R (Version 4.3.0, https://www.R-projects.org) or Python (Version 3.9, https://www.python.org).
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Data availability
The raw and processed metabolomics data from this study have been archived in the Metabolomics Workbench (https://www.metabolomicsworkbench.org/, Study ID ST002692) through the UNC HHEAR Laboratory. Due to privacy considerations, outcome and PFAS exposure data are accessible only through restricted access; requests can be directed to the corresponding author, Dr. Liang, and will be addressed within 10 business days. Demographic covariate data are not publicly available due to data privacy regulations. Source data for figures and tables, along with coding materials and data protocols, are provided in the Supplementary Information/Source Data file. Source data are provided with this paper.
Code availability
Specific code is available from the corresponding author, Dr. Liang, and the request will be responded to within 10 business days.
References
Phthalates factsheet | National Biomonitoring Program | CDC. https://www.cdc.gov/biomonitoring/Phthalates_FactSheet.html (2021).
Krais, A. M. et al. Excretion of urinary metabolites of the phthalate esters DEP and DEHP in 16 volunteers after inhalation and dermal exposure. Int. J. Environ. Res. Public Health 15, 2514 (2018).
Silva, M. J. et al. Urinary levels of seven phthalate metabolites in the U.S. population from the National Health and Nutrition Examination Survey (NHANES) 1999-2000. Environ. Health Perspect. 112, 331–338 (2004).
Varshavsky, J. R., Zota, A. R. & Woodruff, T. J. A novel method for calculating potency-weighted cumulative phthalates exposure with implications for identifying racial/ethnic disparities among U.S. reproductive-aged women in NHANES 2001–2012. Environ. Sci. Technol. 50, 10616–10624 (2016).
Welch, B. M. et al. Racial and ethnic disparities in phthalate exposure and preterm birth: a pooled study of sixteen U.S. cohorts. Environ. Health Perspect. 131, 127015 (2023).
Wesselink, A. K. et al. Correlates of urinary concentrations of phthalate and phthalate alternative metabolites among reproductive-aged Black women from Detroit, Michigan. J. Expo. Sci. Environ. Epidemiol. 31, 461–475 (2021).
Zota, A. R. & Shamasunder, B. The environmental injustice of beauty: framing chemical exposures from beauty products as a health disparities concern. Am. J. Obstet. Gynecol. 217, 418.e1–418.e6 (2017).
Hlisníková, H., Petrovičová, I., Kolena, B., Šidlovská, M. & Sirotkin, A. Effects and mechanisms of phthalates’ action on reproductive processes and reproductive health: a literature review. Int. J. Environ. Res. Public Health 17, 6811 (2020).
Vandenberg, L. N. et al. Hormones and endocrine-disrupting chemicals: low-dose effects and nonmonotonic dose responses. Endocr. Rev. 33, 378–455 (2012).
Eales, J. et al. Human health impacts of exposure to phthalate plasticizers: an overview of reviews. Environ. Int. 158, 106903 (2022).
Benjamin, S. et al. Phthalates impact human health: epidemiological evidences and plausible mechanism of action. J. Hazard Mater. 340, 360–383 (2017).
Latini, G. Monitoring phthalate exposure in humans. Clin. Chim. Acta 361, 20–29 (2005).
Hlisníková, H., Kolena, B., Šidlovská, M., Mlynček, M. & Petrovičová, I. Urinary phthalate biomarkers during pregnancy, and maternal endocrine parameters in association with anthropometric parameters of newborns. Child 9, 413 (2022).
Yolton, K. et al. Prenatal exposure to bisphenol A and phthalates and infant neurobehavior. Neurotoxicol. Teratol. 33, 558–566 (2011).
Kim, Y. et al. Prenatal exposure to phthalates and infant development at 6 months: prospective mothers and children’s environmental health (MOCEH) study. Environ. Health Perspect. 119, 1495–1500 (2011).
Parenti, M. et al. Maternal serum and placental metabolomes in association with prenatal phthalate exposure and neurodevelopmental outcomes in the MARBLES cohort. Metabolites 12, 829 (2022).
Zhang, X. et al. Assessment of metabolic perturbations associated with exposure to phthalates among pregnant African American women. Sci. Total Environ. 818, 151689 (2022).
C. D. C. Fourth national report on human exposure to environmental chemicals: updated tables. Vol. 1, https://stacks.cdc.gov/view/cdc/75822/cdc_75822_DS1.pdf (2019).
Li, S. et al. Predicting network activity from high throughput metabolomics. PLoS Comput. Biol. 9, e1003123 (2013).
Murphy, R. C. & Gijón, M. A. Biosynthesis and metabolism of leukotrienes. Biochem. J. 405, 379–395 (2007).
Wilcox, A. J. Chapter 16. Birth defects. In: Fertility and pregnancy: an epidemiologic perspective (Oxford University Press, Inc., 2010).
Bloemendaal, M. et al. Neuro-cognitive effects of acute tyrosine administration on reactive and proactive response inhibition in healthy older adults. eNeuro 5, 0035–17.2018 (2018).
Ye, L., Sun, Y., Jiang, Z. & Wang, G. L-serine, an endogenous amino acid, is a potential neuroprotective agent for neurological disease and injury. Front. Mol. Neurosci. 14, 726665 (2021).
Heine, W. E. The significance of tryptophan in infant nutrition. Adv. Exp. Med. Biol. 467, 705–710 (1999).
Vanhole, C. et al. L-thyroxine treatment of preterm newborns: clinical and endocrine effects. Pediatr. Res. 42, 87–92 (1997).
Brownlee, M. et al. Chapter 33 - complications of diabetes mellitus. In: Williams Textbook of Endocrinology (Thirteenth Edition) (eds. Melmed, S., Polonsky, K. S., Larsen, P. R. & Kronenberg, H. M.) 1484–1581 (Elsevier, Philadelphia). https://doi.org/10.1016/B978-0-323-29738-7.00033-2 (2016).
Demmelmair, H., Baumheuer, M., Koletzko, B., Dokoupil, K. & Kratl, G. Metabolism of U13C-labeled linoleic acid in lactating women. J. Lipid Res. 39, 1389–1396 (1998).
Berger, M., Gray, J. A. & Roth, B. L. The expanded biology of serotonin. Annu. Rev. Med. 60, 355–366 (2009).
Maffei, M. E. 5-Hydroxytryptophan (5-HTP): natural occurrence, analysis, biosynthesis, biotechnology, physiology and toxicology. Int. J. Mol. Sci. 22, 181 (2020).
Kapalka, G. M. Chapter 6 - Depression. In: Nutritional and Herbal Therapies for Children and Adolescents (ed. Kapalka, G. M.) 141–187 (Academic Press, San Diego). https://doi.org/10.1016/B978-0-12-374927-7.00006-6 (2010).
Braun, J. M. et al. A prospective cohort study of biomarkers of prenatal tobacco smoke exposure: the correlation between serum and meconium and their association with infant birth weight. Environ. Health 9, 53 (2010).
Huang, C.-C. J., Li, C.-M., Wu, C.-F., Jao, S.-P. & Wu, K.-Y. Analysis of urinary N-acetyl-S-(propionamide)-cysteine as a biomarker for the assessment of acrylamide exposure in smokers. Environ. Res. 104, 346–351 (2007).
Gray, J. P. & Hall, G. J. Cotinine. In: Encyclopedia of Toxicology (3rd Edn.) (ed. Wexler, P) 1050–1051 (Academic Press, Oxford). https://doi.org/10.1016/B978-0-12-386454-3.00294-3 (2014).
PubChem. N-Acetyl-S-(3-hydroxypropyl)cysteine. https://pubchem.ncbi.nlm.nih.gov/compound/119083.
Tan, Y. et al. High-resolution metabolomics of exposure to tobacco smoke during pregnancy and adverse birth outcomes in the Atlanta African American maternal-child cohort. Environ. Pollut. 292, 118361 (2022).
Tan, Y. et al. Association between a mixture of per- and polyfluoroalkyl substances (PFAS) and inflammatory biomarkers in the atlanta african american maternal-child cohort. Environ. Sci. Technol. 57, 13419–13428 (2023).
Eick, S. M. et al. Prenatal exposure to persistent and non-persistent chemical mixtures and associations with adverse birth outcomes in the Atlanta African American Maternal-Child Cohort. J. Expo. Sci. Environ. Epidemiol. 1–11 https://doi.org/10.1038/s41370-023-00530-4 (2023).
Liang, D. et al. Metabolic perturbations associated with an exposure mixture of per- and polyfluoroalkyl substances in the Atlanta african american maternal-child cohort. Environ. Sci. Technol. 57, 16206–16218 (2023).
Osborn, L. J. et al. A gut microbial metabolite of dietary polyphenols reverses obesity-driven hepatic steatosis. Proc. Natl. Acad. Sci. USA 119, e2202934119 (2022).
Palau-Rodriguez, M. et al. Metabolomic insights into the intricate gut microbial–host interaction in the development of obesity and type 2 diabetes. Front. Microbiol. 6, 1151 (2015).
Chang, G. Maternal substance use: consequences, identification, and interventions. Alcohol Res. 40, 06 (2020).
Hoppin, J. A., Brock, J. W., Davis, B. J. & Baird, D. D. Reproducibility of urinary phthalate metabolites in first morning urine samples. Environ. Health Perspect. 110, 515–518 (2002).
Eatman, J. A. et al. Exposure to phthalate metabolites, bisphenol A, and psychosocial stress mixtures and pregnancy outcomes in the Atlanta African American maternal-child cohort. Environ. Res. 233, 116464 (2023).
Lehmann, S., Delaby, C., Vialaret, J., Ducos, J. & Hirtz, C. Current and future use of ‘dried blood spot’ analyses in clinical chemistry. Clin. Chem. Lab. Med. 51, 1897–1909 (2013).
Velghe, S., Delahaye, L. & Stove, C. P. Is the hematocrit still an issue in quantitative dried blood spot analysis? J. Pharm. Biomed. Anal. 163, 188–196 (2019).
Vespasiani-Gentilucci, U. et al. Platelet count may impact on lysosomal acid lipase activity determination in dried blood spot. Clin. Biochem. 50, 726–728 (2017).
Jain, A. et al. Hemoglobin normalization outperforms other methods for standardizing dried blood spot metabolomics: a comparative study. Sci. Total Environ. 854, 158716 (2023).
Salisbury, A. L., Fallone, M. D. & Lester, B. Neurobehavioral assessment from fetus to infant: the NICU network neurobehavioral scale and the fetal neurobehavior coding scale. Ment. Retard Dev. Disabil. Res. Rev. 11, 14–20 (2005).
Sucharew, H., Khoury, J. C., Xu, Y., Succop, P. & Yolton, K. NICU network neurobehavioral profiles predict developmental outcomes in a low risk sample. Paediatr. Perinat. Epidemiol. 26, 344–352 (2012).
Liu, J. et al. Neonatal neurobehavior predicts medical and behavioral outcome. Pediatrics 125, e90–e98 (2010).
Bowers, K. et al. Early infant attention as a predictor of social and communicative behavior in childhood. Int. J. Behav. Dev. 43, 204–211 (2019).
Brennan, P. A. et al. Protocol for the Emory University African American maternal stress and infant gut microbiome cohort study. BMC Pediatr. 19, 246 (2019).
Zhao, Y. et al. Prenatal phthalate exposure, infant growth, and global DNA methylation of human placenta. Environ. Mol. Mutagen. 56, 286-292 (2015).
Messerlian, C. et al. Urinary concentrations of phthalate metabolites and pregnancy loss among women conceiving with medically assisted reproduction. Epidemiology 27, 879–888 (2016).
Hornung, R. W. & Reed, L. D. Estimation of average concentration in the presence of nondetectable values. Appl. Occup. Environ. Hyg. 5, 46–51 (1990).
O’Brien, K. M., Upson, K. & Buckley, J. P. Lipid and creatinine adjustment to evaluate health effects of environmental exposures. Curr. Environ. Health Rep. 4, 44–50 (2017).
Barr, D. B. et al. Urinary creatinine concentrations in the U.S. Population: implications for urinary biologic monitoring measurements. Environ. Health Perspect. 113, 192–200 (2005).
Taibl, K. R. et al. Newborn metabolomic signatures of maternal per- and polyfluoroalkyl substance exposure and reduced length of gestation. Nat. Commun. 14, 3120 (2023).
Petrick, L. et al. An untargeted metabolomics method for archived newborn dried blood spots in epidemiologic studies. Metabolomics 13, 27 (2017).
Zhuang, Y.-J., Mangwiro, Y., Wake, M., Saffery, R. & Greaves, R. F. Multi-omics analysis from archival neonatal dried blood spots: limitations and opportunities. Clin. Chem. Lab. Med. 60, 1318–1341 (2022).
Ward, C. et al. Nontargeted mass spectrometry of dried blood spots for interrogation of the human circulating metabolome. J. Mass Spectrom. 56, e4772 (2021).
NBS Policies and Procedures | Georgia Department of Public Health. https://dph.georgia.gov/NBS/nbs-policies-and-procedures.
Rushing, B. R. et al. Fecal metabolomics reveals products of dysregulated proteolysis and altered microbial metabolism in obesity-related osteoarthritis. Osteoarthr. Cartil. 30, 81–91 (2022).
Lynch, D. H. et al. Baseline serum biomarkers predict response to a weight loss intervention in older adults with obesity: a pilot study. Metabolites 13, 853 (2023).
Lester, B. M. & Tronick, E. Z. History and description of the Neonatal Intensive Care Unit Network Neurobehavioral Scale. Pediatrics 113, 634–640 (2004).
Fink, N. S., Tronick, E., Olson, K. & Lester, B. Healthy newborns’ neurobehavior: norms and relations to medical and demographic factors. J. Pediatr. 161, 1073–1079 (2012).
Hendrix, C. L. et al. Prenatal distress links maternal early life adversity to infant stress functioning in the next generation. J. Psychopathol. Clin. Sci. 131, 117–129 (2022).
Greenland, S., Pearl, J. & Robins, J. M. Causal diagrams for epidemiologic research. Epidemiology 10, 37 (1999).
Benjamini, Y. & Hochberg, Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. J. R. Stat. Soc.: Ser. B 57, 289–300 (1995).
Chang, C.-J. et al. Per- and polyfluoroalkyl substance (PFAS) exposure, maternal metabolomic perturbation, and fetal growth in African American women: a meet-in-the-middle approach. Environ. Int 158, 106964 (2022).
Chadeau-Hyam, M. et al. Meeting-in-the-middle using metabolic profiling – a strategy for the identification of intermediate biomarkers in cohort studies. Biomarkers 16, 83–88 (2011).
Kohlmeier, M. Tyrosine. In: Nutrient Metabolism (ed. Kohlmeier, M) 321–328 (Academic Press, London). https://doi.org/10.1016/B978-012417762-8.50052-1 (2003).
Lee, J. et al. 4-hydroxybenzaldehyde restricts the intracellular growth of toxoplasma gondii by inducing SIRT1-mediated autophagy in macrophages. Korean J. Parasitol. 58, 7–14 (2020).
Byelashov, O. A., Sinclair, A. J. & Kaur, G. Dietary sources, current intakes, and nutritional role of omega-3 docosapentaenoic acid. Lipid Technol. 27, 79–82 (2015).
Marseglia, L. et al. Antioxidant effect of melatonin in preterm newborns. Oxid. Med. Cell Longev. 2021, 6308255 (2021).
Tian, X. et al. Urinary metabolomic study in a healthy children population and metabolic biomarker discovery of attention-deficit/hyperactivity disorder (ADHD). Front. Psychiatry 13, 819498 (2022).
De Jesús, V. R. et al. Examination of xylene exposure in the U.S. population through biomonitoring: NHANES 2005–2006, 2011–2016. Biomarkers 26, 65–73 (2021).
Linagliptin (oral route) side effects - Mayo Clinic. https://www.mayoclinic.org/drugs-supplements/linagliptin-oral-route/side-effects/drg-20074875?p=1.
Chapman, M. J., Wallace, E. C. & Pollock, T. A. 29 - Organic Acid Profiling. In: Textbook of Natural Medicine (Fifth Edition) (eds. Pizzorno, J. E. & Murray, M. T) 236-244.e6 (Churchill Livingstone, St. Louis (MO)). https://doi.org/10.1016/B978-0-323-43044-9.00029-7.(2020)
Ramendra, R. et al. Glutathione metabolism is a regulator of the acute inflammatory response of monocytes to (1→3)-β-D-Glucan. Front. Immunol. 12, 694152 (2021).
Sarkar, C. & Lipinski, M. M. N-acetyl-L-leucine: a promising treatment option for traumatic brain injury. Neural Regen. Res. 17, 1957–1958 (2022).
Stout, M. B. et al. 17α-estradiol alleviates age-related metabolic and inflammatory dysfunction in male mice without inducing feminization. J. Gerontol. A Biol. Sci. Med Sci. 72, 3–15 (2017).
Ohyama, Y. & Shinki, T. Subchapter 97A - Calcitriol. In: Handbook of Hormones (eds. Takei, Y., Ando, H. & Tsutsui, K) 548-e97A-5 (Academic Press, San Diego, 2016). https://doi.org/10.1016/B978-0-12-801028-0.00236-1.
Mett, J. & Müller, U. The medium-chain fatty acid decanoic acid reduces oxidative stress levels in neuroblastoma cells. Sci. Rep. 11, 6135 (2021).
Substance Details JWH-019. https://www.unodc.org/LSS/Substance/Details/798c1450-2373-422a-a292-d645810d2365.
Perng, W. et al. Associations of cord blood metabolites with perinatal characteristics, newborn anthropometry, and cord blood hormones in project viva. Metabolism 76, 11–22 (2017).
PubChem. Mono(2-ethylhexyl) phthalate(1-). https://pubchem.ncbi.nlm.nih.gov/compound/21924291.
PubChem. Octyl hydrogen phthalate. https://pubchem.ncbi.nlm.nih.gov/compound/79362.
Ohue-Kitano, R. et al. 3-(4-Hydroxy-3-methoxyphenyl)propionic acid produced from 4-hydroxy-3-methoxycinnamic acid by gut microbiota improves host metabolic condition in diet-induced obese mice. Nutrients 11, 1036 (2019).
Kapalka, G. M. Chapter 4 - substances involved in neurotransmission. In: Nutritional and Herbal Therapies for Children and Adolescents (ed. Kapalka, G. M) 71–99 (Academic Press, San Diego, https://doi.org/10.1016/B978-0-12-374927-7.00004-2 (2010).
Duranton, F. et al. Normal and pathologic concentrations of uremic toxins. J. Am. Soc. Nephrol. 23, 1258–1270 (2012).
Gafar, A. A. et al. Lithocholic acid induces endoplasmic reticulum stress, autophagy and mitochondrial dysfunction in human prostate cancer cells. PeerJ 4, e2445 (2016).
Lyons, M. A. & Brown, A. J. 7-Ketocholesterol. Int. J. Biochem. Cell Biol. 31, 369–375 (1999).
Acknowledgements
We thank all members of the Environmental Metabolomics and Exposomics Research Group at Emory (EMERGE) for their valuable input and feedback on this project. S.S.H. and K.R.T. are supported by the NIEHS T32 Training Program in Environmental Health and Toxicology (T32 ES012870). This work was supported by the NIH research grants [R01NR014800, R01MD009064, R24ES029490, R01MD009746, R21ES032117, R01ES035738], NIH Center Grants [P50ES02607, P30ES019776, UH3OD023318, U2CES026560], and Environmental Protection Agency (USEPA) center grant [83615301].
Author information
Authors and Affiliations
Contributions
S.S.H. completed the analysis, interpretation, and writing of the manuscript. D.L., S.S.H., and T.H. generated the study aims and prepared the manuscript. Z.T. completed the code checks, manuscript editing, and preparation. A.D., P.A.B., and E.J.C. were involved in data collection, cohort management, and manuscript editing and preparation. B.R., S.L.M., and S.S. were involved in metabolomics data processing, manuscript editing, and preparation. T.H., S.M.E., K.R.T., Y.T., P.P., G.E.L., J.E., P.B.R., D.B.B., and D.P.J. were involved in manuscript editing and preparation.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Communications thanks Luigi Atzori, who co-reviewed with Martina Spada, Trecia A. Wouldes, and the other, anonymous, reviewer(s) for their contribution to the peer review of this work. A peer review file is available.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Source data
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Hoffman, S.S., Tang, Z., Dunlop, A. et al. Impact of prenatal phthalate exposure on newborn metabolome and infant neurodevelopment. Nat Commun 16, 2539 (2025). https://doi.org/10.1038/s41467-025-57273-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41467-025-57273-z