Abstract
Inflammatory diseases are a major source of morbidity and mortality world-wide, the pathogenesis of which are characterised by the interplay of key pro-inflammatory and oxidative enzymes. Here, we report the development of a small molecule dual inhibitor targeting vascular adhesion protein-1 (VAP-1) and myeloperoxidase (MPO), two clinically relevant pro-inflammatory/oxidative enzymes that play complementary pathogenic roles in various inflammatory diseases. This agent, SNT-8370 [(E)-3-(3-((2-(aminomethyl)-3-fluoroallyl)oxy)benzyl)-2-thioxo-1,2,3,7-tetrahydro-6H-purin-6-one)], irreversibly inhibits VAP-1 and MPO activity with equivalent and enhanced nanomolar potency, respectively, when compared to benchmark clinical VAP-1 and MPO inhibitors. SNT-8370 is selective, exhibiting >100-1000-fold more potency for VAP-1 and MPO versus other mammalian (per)oxidases and shows no significant off-target activity in established preclinical screening panels. In vivo, SNT-8370 is metabolically stable, exhibits a favourable pharmacokinetic/pharmacodynamic profile without CNS penetration, and effectively inhibits VAP-1 and MPO activities. Moreover, compared to monotherapy, SNT-8370 more effectively inhibits leukocyte infiltration in mouse peritonitis, carrageenan air pouch, and lipopolysaccharide-induced lung injury models of acute inflammation. SNT-8370 is also protective in preclinical models of myocardial ischemia-reperfusion injury and unilateral-ureteral-obstruction-induced nephropathy. Collectively, our results support SNT-8370 as a first-in-class, mechanism-based dual inhibitor of VAP-1 and MPO, and as a promising therapeutic for the clinical treatment of inflammatory disorders.
Similar content being viewed by others
Introduction
Inflammation is a fundamental physiological process that protects host tissue against infection, foreign irritants and damaged or transformed cells by removing injurious agents or stimuli and precipitating a wound healing process. Under normal conditions, acute inflammatory responses are effectively coordinated by cellular and molecular cues that signal for the temporal resolution of the process and permit the restoration of tissue homoeostasis1,2. However, unregulated, or excessive inflammatory responses can become chronic, ultimately causing host-tissue damage1,2. Chronic inflammation can occur in various organ systems including bone, renal, hepatic, neurological, pulmonary and cardiovascular tissues and is a major cause of morbidity and mortality world-wide3.
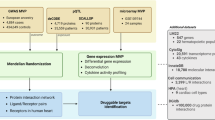
Accordingly, great interest surrounds the discovery and development of therapeutic agents targeting pathogenic chronic inflammatory processes4. As inflammatory responses are coordinated by the complex interplay of multiple proteins and pathways, increasing attention surrounds the discovery of new combinatorial therapeutic approaches that selectively and simultaneously suppress multiple inflammatory pathways5. An innovative approach in combination therapy is the discovery of a new generation of small molecule inhibitors for the simultaneous selective and potent inhibition of multiple molecular targets or proteins. Single-molecule dual inhibitors hold promise in providing synergistic therapeutic efficacy, reduced potential of drug–drug interactions and drug-resistance, and improved pharmacokinetics compared to co-administration of multiple individual drugs6. This study reports on the discovery and characterisation of a small molecule dual inhibitor that simultaneously targets two different but complementary pro-inflammatory and oxidative enzymes capable of driving chronic inflammatory disorders, vascular adhesion protein-1 (VAP-1) and myeloperoxidase (MPO) (Fig. 1).
During inflammation, VAP-1 expressed on the luminal membrane of the activated endothelium facilitates the recruitment, adhesion and transmigration of leucocytes (e.g. neutrophils) into inflamed tissues, via its enzyme activity, which includes the local production of the redox signalling oxidant, hydrogen peroxide (H2O2). Recruited neutrophils release MPO in response to inflammatory stimuli, which upon activation by its co-substrate H2O2 (potentially derived from VAP-1 activity) catalyses a variety of oxidative reactions that result in the oxidation, chlorination and nitration of an array of biomolecules within the inflamed tissue (e.g. atherosclerotic lesion), leading to an inflammatory feedback loop, whereby additional leucocytes are recruited from the circulation. The inhibition of VAP-1 reduces leucocyte influx and the local generation of H2O2, leading to the reduced release of MPO. Inhibition of MPO reduces local oxidative tissue damage and inhibits the inflammatory feedback loop.
VAP-1 (also known as semicarbazide-sensitive amine oxidase [SSAO] and Amine Oxidase Copper-containing 3 [AOC3]) is a plasma membrane expressed adhesion protein involved in the recruitment and transmigration of granulocytes, in particular, neutrophils7 (Fig. 1). VAP-1 is also an ectoenzyme that contains active-site copper and topaquinone co-factors and catalyses the generation of the reactive oxygen species, hydrogen peroxide (H2O2) and aldehydes7. Elevated levels of VAP-1 (both tissue and circulating as a truncated soluble form) are associated with an increased incidence in many inflammatory diseases including cardiovascular, kidney, liver and neurodegenerative disorders7,8,9. VAP-1−/− mice are protected against inflammation and related processes, an effect mirrored by treatment with either pharmacological inhibitors of the enzyme activity or antibodies to the adhesion domain7,8,9. Therefore, VAP-1 has emerged as a potential new target for treating a variety of inflammatory and fibrotic conditions7,8,9. VAP-1 inhibitors, ASP8232 and PXS-4728 (Fig. 2), have advanced into Phase 2 clinical trials with anti-inflammatory properties demonstrated in patients with diabetic kidney disease and non-alcoholic steatohepatitis, respectively10,11. Anti-inflammatory dual inhibitors targeting VAP-1 and monoamine oxidase B have been developed for the treatment of neuroinflammation (NCT05904717) and muscular diseases12. These dual inhibitors target the same amine oxidase family through a common mechanism involving a fluoroallylamine warhead. The dual inhibitor described in this study inhibits two distinct pro-inflammatory enzyme families (amino oxidase and heme peroxidase) through alternative molecular mechanisms by targeting different binding sites via two disparate chemical warheads.
Representative examples of clinically investigated VAP-1 and MPO inhibitors showing the starting templates for drug-drug conjugate design. Selected examples of explored hybrid molecules (Compounds A–E), including the structure of SNT-8370 (Compound E). Colour-coding showing the active warheads for VAP-1 (Blue) and MPO (Green, Pink).
MPO is highly expressed in neutrophils (where it can account for up to 5% of the dry weight), and to a lesser degree in monocytes and macrophages13,14,15. MPO is released in response to inflammatory signals by rapid degranulation and acts in a localised fashion on the immediate tissue environment (Fig. 1), including within neutrophilic extracellular traps. MPO represents a major enzymatic source of reactive biological oxidants in inflammatory tissues that is activated upon reaction of its co-substrate H2O2 with the active-site heme16. For example, MPO generates hypochlorous acid (HOCl) and hypothiocyanous acid, which contribute to the innate immune roles of neutrophils in combating infectious pathogens17. However, uncontrolled and excessive production of MPO-derived oxidants can result in significant host tissue damage, which underscores the strong link between MPO and the pathogenesis of numerous inflammatory disorders15,16. MPO inhibitors PF-06282999, AZD5904, verdiperstat (AZD3241/BHV3241) and more recently mitiperstat (AZD4831) (Fig. 2) have progressed into the clinic, e.g. mitiperstat is currently in studies for heart failure (Phase 2/3)18,19, non-alcoholic steatohepatitis and chronic obstructive pulmonary disease (Phase 2)20,21.
As MPO is released by activated leucocytes that are directed to sites of inflammation by endothelial-expressed VAP-1, these two enzymes play complementary roles in facilitating the recruitment and activation of leucocytes in inflammation, with both enzymes contributing to the local production of reactive oxidants (Fig. 1). Therefore, there is significant overlap with respect to the inflammatory diseases relevant for both enzymes. Inhibitors of these individual enzymes have been shown to be safe in various Phase 1 studies. A single inhibitor of both enzymes therefore has the potential to reduce leucocyte recruitment, oxidative stress, tissue damage and fibrosis, affording a broad anti-inflammatory/anti-fibrotic approach with a lower risk profile compared to the current drugs (e.g. non-steroidal anti-inflammatory drugs, steroids, TNF-α inhibitor).
Herein we describe the discovery and characterisation of SNT-8370, a condensed drug-drug conjugate based on the vast knowledge of single mode inhibitors. SNT-8370 is an irreversible mechanism-based dual inhibitor of both VAP-1 and MPO that shows a superior in vitro and in vivo drug profile compared to benchmark clinical MPO or VAP-1 single mode inhibitors, including enhanced anti-inflammatory activity by SNT-8370 versus single mode inhibitors in various different preclinical models of inflammatory disease. SNT-8370 is metabolically stable, has a good pharmacokinetic/pharmacodynamic (PK/PD) profile and shows no significant off-target activity in preclinical screening, findings in support of its future clinical development as a new anti-inflammatory therapeutic.
Results
Chemical design, development and initial in vitro characterisation of SNT-8370 as a potent and selective dual-inhibitor of VAP-1 and MPO
To obtain a dual VAP-1/MPO inhibitor, the well documented binding motifs (warheads) of a VAP-1 inhibitor (a fluoroallylamine) and an MPO inhibitor (thiouracil or thioxanthine) were combined to form a drug-drug conjugate. Different ways of chemically joining a variety of known MPO inhibitors with templates capable of binding to a VAP-1 inhibitor were explored, and prototype compounds (a selection of which are shown in Fig. 2) were tested for their ability to inhibit VAP-1 and MPO enzymatic activity.
Test compounds were initially profiled against the benchmark clinical compounds by measuring VAP-1-catalysed H2O2 production or MPO-catalysed H2O2 consumption using the Amplex Red assay to generate IC50 values for both VAP-1 and MPO (Table 1). In the uracil scaffold series, attachment of the VAP-1 warhead in the meta position with either 4- or 5-positioning of the chloro atom (Fig. 2; Compounds A & B) afforded compounds with similar MPO potency (to PF0628299922), but reduced VAP-1 potency compared to PXS-4728 (>1000-fold decrease). Interestingly, the para substituted VAP-1 warhead (Fig. 2; Compound C) also showed similar MPO potency but with a reduced drop-off in VAP-1 potency. Moving to the thioxanthine scaffold, the para substituted VAP-1 warhead (Compound D) maintained excellent potency for VAP-1, but the inhibitory activity for MPO was abrogated. The meta-orientated VAP-1 warhead (Compound E), however, seemed optimally placed; potency for VAP-1 was comparable to the benchmark compounds, whilst for MPO the IC50 was ~3-fold more potent than comparator AZD5904, and ~2-fold more potent than the second-generation clinical MPO inhibitor verdiperstat (AZD3241/BHV3241)23,24. Substitution of both the central aryl ring and the thioxanthine, to further optimise the potency of the molecule for both enzyme targets, failed to significantly improve on Compound E, highlighting an extremely narrow structure-activity relationship (outlined in the Supporting Information, Supplementary Table S1). The preferred dual-inhibitor, Compound E, was designated SNT-8370 and progressed for further profiling.
SNT-8370 potently inhibits MPO-catalysed oxidative reactions
Under (patho)-physiological conditions, MPO employs H2O2 to oxidise chloride ions into the potent biological oxidant HOCl16. Therefore, we next compared the efficacy of SNT-8370 to inhibit MPO-catalysed H2O2 consumption and HOCl production under identical assay conditions with single mode clinically-trialled 2-thioxanthine (verdiperstat/AZD3241)23,24 and thiouracil-based (PF06282999)22 irreversible MPO inhibitors. SNT-8370 inhibited MPO-catalysed H2O2 consumption more significantly when compared to verdiperstat or PF06282999 (Fig. 3A–D). Accordingly, the IC50 value for SNT-8370 of 0.08 μM was ~5-8-fold lower than the IC50 values of verdiperstat (0.41 μM) or PF06282999 (0.63 μM) (Fig. 3D). SNT-8370 also more efficiently inhibited MPO-catalysed HOCl production, compared to verdiperstat or PF06282999 (Fig. 3E). Thus, the IC50 value of SNT-8370 was 0.25 μM, which was ~2–5-fold lower than the corresponding IC50 values for verdiperstat (0.59 μM) or PF06282999 (1.23 μM). Of note, different IC50 values for MPO inhibition of the test compounds were apparent across the different MPO activity assays employed (Table 1, Fig. 3). These differences likely reflect the different experimental conditions and readouts employed to assess MPO activity. Importantly, across all MPO assays SNT-8370 exhibited a significant 2–5-fold reduction in IC50 values when compared to verdiperstat and 5-8-fold reduction when compared to PF06282999.
A–D Inhibitors were added at the indicated concentrations to PBS (pH-7.4) supplemented with 5 mM taurine, followed by incubation at room temperature with mixing. H2O2 (50 μM) was added and the change in H2O2 concentration was continuously monitored using an H2O2-specific electrode. After a maximal steady-state H2O2 concentration was achieved, MPO (10 nM) was added and the rate of MPO-catalysed H2O2 consumption was measured over the ensuing 200–800 s. Representative H2O2 consumption curves for A SNT-8370, B verdiperstat and C PF06282999. D Dose-dependent inhibition curves of MPO-catalysed H2O2 consumption by SNT-8370, verdiperstat and PF06282999. Data is expressed as a % of the rate of MPO-catalysed H2O2 consumption in the absence of inhibitors (control) and represents the mean ± SEM of n = 3 (SNT-8370, verdiperstat) or n = 4 (PF06282999) independent experiments. E MPO (10 nM) was incubated in the absence or presence of the indicated concentrations of inhibitors in PBS (pH-7.4) supplemented with 5 mM taurine. MPO was activated by H2O2 (50 μM) addition, the reaction terminated after 6 min and the level of MPO-catalysed HOCl production assessed by the iodide-catalysed TMB assay. Results show the dose-dependent inhibition curves of MPO chlorination activity. Data is expressed as a % of MPO-catalysed HOCl production in the absence of inhibitors (control) and represents the mean ± SEM of n = 3 (PF06282999, verdiperstat) or n = 7 (SNT-8370) independent experiments. F LDL (0.2 mg/mL) was incubated with 30 nM MPO, 500 μg/mL glucose, 100 ng/mL glucose oxidase and 0.5 mM NaNO2 in the absence (control) or presence of the indicated concentrations of SNT-8370 (n = 4) or verdiperstat (n = 4). Reactions were incubated at 37 °C for 2 h and LDL cholesteryl ester hydro(per)oxides (CE-O(O)H) levels measured. Data is expressed as a % of MPO-dependent CE-O(O)H formation in the absence of inhibitors (control) and represents the mean ± SEM of n = 4 (SNT-8370, verdiperstat) independent experiments. Data was analysed as area under the curve (AUC) by (D, E) one-way ANOVA (Tukey’s post hoc) or (F) Student’s t-test (two-tailed). The p values shown are versus the corresponding SNT-8370 concentration curve.
A key pathogenic oxidative reaction catalysed by leucocyte-derived MPO in the artery wall during atherosclerotic cardiovascular disease is the oxidative modification of low-density lipoprotein (LDL)15,25. For example, in the presence of inflammatory levels of nitrite, MPO-catalyses the generation of the nitrogen dioxide radical (•NO2), which mediates the peroxidation of LDL lipids and conversion of the lipoprotein into a pro-atherogenic form26,27. We therefore next compared the capacity of SNT-8370 to inhibit MPO-mediated LDL lipid peroxidation with verdiperstat. For this, LDL was incubated with MPO in the presence of nitrite and a continuous source of H2O2 to induce LDL lipid peroxidation and resultant formation of cholesteryl ester lipid hydroperoxides26,27. Compared to verdiperstat, SNT-8370 more potently inhibited MPO-mediated LDL lipid peroxidation (Fig. 3F), exhibiting an IC50 of 20 nM, 30-fold lower than the corresponding IC50 value for verdiperstat of 0.6 μM.
Collectively, these data demonstrate that SNT-8370 is a more potent inhibitor of MPO-catalysed oxidative reactions compared to two different classes of clinical benchmark MPO inhibitors.
Molecular modelling of the interaction of SNT-8370 in MPO’s active site
Given the improvements in inhibitory efficacy observed with SNT-8370 for MPO compared to AZD5904 (Table 1) and verdiperstat (Fig. 3), we next sought to understand this by exploring the MPO active site in silico. Our starting point was the structurally related 2-thioxanthine TX2 ligand covalently bound to the MPO active site (PDB 3ZS0)28. Overlay of SNT-8370 was performed to establish an initial pose for the docking experiments. The sulphur of SNT-8370 was covalently attached to the co-factor in analogy to TX2, and then an induced fit docking simulation carried out using the Molecular Operating Environment (MOE®) platform. The top three scoring hits were manually assessed and observed to be very similar in their arrangement in the active pocket. Both the aryl group (in analogy to the TX2) and the vinyl fluoride portions of the structure sit in highly lipophilic regions of the active site (Fig. 4A, B), and a strong interaction between the allylamine group and one of the gatekeeper residues to the MPO pocket, Glu116 residue, was observed (Fig. 4B, C). This additional interaction with the glutamic acid may be responsible for the beneficial increase in MPO inhibitory efficacy of SNT-8370 over the starting MPO inhibitor templates. Supportive of this hypothesis is the observation that if the primary amine VAP-1 warhead is capped with an acyl group, thereby removing the basic nature of the nitrogen, the IC50 for MPO is significantly impacted, dropping from 17 nM (Table 1, SNT-8370) to 128 nM (see Supporting Information, Supplementary Table S1, Compound S13).
In silico modelling of SNT-8370 (yellow) bound to the heme group (purple) in the active site of activated MPO, showing (A) the active site pocket with SNT-8370 orientated in two lipophilic clefts (green, white and yellow colouring), B the molecular interactions as calculated by the Molecular Operating Environment (MOE) platform, showing the interaction between the allylamine portion of the molecule and the Glu116 residue at the entrance to the active site, and C a 3-D representation of this interaction in PYMOL, where a distance of 1.71 Å was measured between the SNT-8370 protonated amine and the negatively charged Glu116 residue acid group (shown in green stick form).
SNT-8370 is an efficient mechanism-based irreversible inhibitor of VAP-1 and MPO
A feature of efficient mechanism-based irreversible MPO inhibitors is their capacity to rapidly react with MPO compound I (Supplementary Fig. S1)28, to form a secondary drug radical that preferentially irreversibly reacts with the heme active site to inhibit the enzyme, versus escape from the active site to potentially undergo off-target reactions29. For SNT-8370, this radical is formed via the 2-thioxanthine moiety through the sulphur atom, which is considered to form a covalent bond with the active site heme (Supplementary Fig. S1)28. For VAP-1, both irreversible and reversible inhibitors of the enzyme have been reported30,31. SNT-8370 belongs to the fluoroallylamine class of VAP-1 inhibitors, which are thought to irreversibly bind to the co-factor via activation upon binding in the active site triggering a reaction cascade leading ultimately to a displacement of the fluorine atom (Supplementary Fig. S2)32.
To further gauge the efficacy of SNT-8370 as an MPO inhibitor we determined the partition ratio (see the Methods Section for experimental details), which is a measure of the efficiency by which mechanism-based irreversible enzyme inhibitors covalently bind to and inactivate the active sites of their target enzymes. The partition ratio therefore provides a comparative rate of turnover between different irreversible inhibitors. If a drug is 100% efficient, then a partition ratio of 1 is expected (i.e. no turnover, one molecule of inhibitor is covalently bound to one molecule of activated enzyme). If inhibitor efficiency is less, then a ratio of >1 is observed. Quantitative measurement of the partition ratio (for >1) is expected to vary across labs as the values are dependent on the experimental conditions including, the specific activity/concentration of enzymatically active protein present in the relevant assay, and so the partition ratio is best measured relative to benchmarked compounds.
For MPO, we followed the assay of Ruggeri and colleagues who previously reported a partition ratio for PF06282999 of 6.522. Under our assay conditions PF06282999 exhibited a partition ratio for MPO inhibition of 43.9 ± 0.6 (mean ± SEM, n = 3) (Fig. 5C), indicating inter-laboratory assay variation. Notably, under our assay conditions SNT-8370 exhibited a significantly lower partition ratio of 15.7 ± 2.4 (n = 3) (Fig. 5A) for MPO inhibition when compared to PF06282999 (p < 0.0001, one-way ANOVA [Tukey’s post-hoc]) or verdiperstat (partition ratio of 28.8 ± 0.8, n = 3; p = 0.0066, one-way ANOVA [Tukey’s post-hoc]) (Fig. 5B). Therefore, the partition ratio data strengthens the conclusion of the concentration-dependent inhibition experiments that SNT-8370 is a more efficient mechanism-based MPO inhibitor when compared to verdiperstat and PF06282999 and is consistent with the molecular modelling results suggesting tighter drug binding of SNT-8370 within the MPO active site.
A–C For partition ratio, MPO (60 nM) was incubated with 2 μM H2O2 in the presence of DMSO (vehicle control) or relevant inhibitor (0.13–5 μM). After 15 min, the mixture was diluted 300-fold into assay buffer containing 2 μM H2O2 and 30 μM Amplex Red, and MPO activity immediately measured as the rate of H2O2 consumption. Data is the mean ± SEM of n = 3 independent experiments and represents % control MPO activity graphed as a function of [inhibitor]/[MPO]. Partition ratios of A SNT-8370 (n = 3), B verdiperstat (n = 3) and C PF06282999 (n = 3) were calculated as the X-axis-intercept of the line of best fit (green). D MPO (500 pM) was incubated with H2O2 (100 μM) in the presence of varying concentrations of BMS-250 and MPO activity measured as the rate of H2O2 consumption by the Amplex Red assay. Data is the mean value of n = 2 independent experiments. E For MPO jump dilution experiments, MPO (30 nM) was incubated with H2O2 (2 μM) in the absence (DMSO) and presence of SNT-8370 or BMS-250 at 300-fold their recorded IC50 to achieve maximal enzyme inhibition. The mixture was diluted 300-fold and the recovery of MPO activity measured upon enzyme reactivation. Data is expressed as % control activity and represents the mean ± SEM of n = 3 independent experiments. F VAP-1 (0.25 μg/mL) was incubated in the presence of varying concentrations of ‘des-fluoro’ SNT-8370 and VAP-1 activity measured as the rate of H2O2 generation by the Amplex Red assay. Data is the mean value of n = 2 independent experiments. G For VAP-1 Jump dilution experiment, VAP-1 (700 nM) was incubated in the absence (DMSO) or presence of SNT-8370 or ‘des-fluoro’ SNT-8370 at 30-fold their recorded IC50 to achieve maximal enzyme inhibition. The mixture was diluted 50-fold, and the recovery of VAP-1 activity measured upon enzyme reactivation. Data is expressed as % control and represents the mean ± SEM of n = 3 independent experiments. Data was analysed by one-way ANOVA (Tukey’s post hoc).
In a similar fashion, oxidative turnover studies were carried out with VAP-1 (Supplementary Fig. S3). No oxidative turnover was observed for SNT-8370, suggesting a low partition ratio, similar to previous reports from the fluoroallylamine class of inhibitors30.
To further confirm the irreversible nature of VAP-1 and MPO inhibition, we next performed jump dilution experiments following published methods for MPO29. In each experiment, data with SNT-8370 was compared with reversible enzyme inhibitors in the same experiment. For MPO, a reversible inhibitor referred to here as BMS-250 was employed (WO2017040449)33. For VAP-1, the des-fluoro analogue of SNT-8370 was used. As expected, addition of BMS-250 (Fig. 5D) or des-fluoro SNT-8370 (Fig. 5F) to the relevant enzyme dose-dependently inhibited MPO (IC50 13 nM) and VAP-1 (IC50 1.4 μM), respectively. Initial addition of inhibitors at concentrations 300-fold (for MPO) or 30-fold (for VAP-1) higher than the relevant IC50 value followed by rapid dilution to wash out the enzyme active site afforded a measure of reversibility of each compound against the relevant enzyme target. Despite enzyme wash-out, SNT-8370 maintained its potent inhibitory activity for MPO (Fig. 5E) and VAP-1 (Fig. 5G), indicative of minimal post-dilution recovery of enzyme activity for SNT-8370. In contrast, post-dilution enzyme activity was significantly recovered by 50-60% for MPO pre-treated with BMS-250 (Fig. 5E) and 70–80% for VAP-1 pre-treated with des-fluoro SNT-8370 (Fig. 5G). These findings support SNT-8370 irreversibly inhibits MPO and VAP-1.
Selectivity of SNT-8370 for VAP-1 and MPO versus other human mammalian (per)oxidase enzymes
Both VAP-1 and MPO belong to extended families of related oxidative enzymes, with structurally similar active sites. VAP-1 is a member of the amine oxidase family, which contains several important off-targets such as the monoamine oxidases (MAOs; MAO-A & MAO-B), involved in the metabolism of key neurotransmitters; diamine oxidase (DAO), involved in the metabolism of histamine; and the lysyl oxidases (LOX), involved in the cross-linking of collagen. MPO is a member of the heme peroxidase family, members of which include eosinophil peroxidase (EPO)34, involved in eosinophil driven inflammatory processes with a preference for bromide and iodine ions as substrates; lactoperoxidase (LPO), involved in the innate immune system in milk and mucosal secretions34; thyroid peroxidase (TPO), involved in the production of key thyroid hormone proteins16,35; and peroxidasin (PXDN; also referred to as vascular peroxidase or VPO1) that plays a role in vascular wall development by forming a covalent link in collagen IV in the basement membrane36 and increasingly recognised to contribute to cardiovascular inflammation and disease37. A summary of the profile of SNT-8370 against these related off-targets is shown in Table 2. For both the amine oxidase and the heme peroxidase enzyme families, compared to MPO or VAP-1, SNT-8370 exhibited a selectivity index of >100-fold over most off-targets and importantly >1000-fold over MAO-A and LOX.
ADME and off-target profiling of SNT-8370
Due to its excellent in vitro pharmacology SNT-8370 was advanced for profiling in preclinical absorption, distribution, metabolism and excretion (ADME) assays, the results of which are summarised in Supplementary Table S2. SNT-8370 was found to have good metabolic stability in microsomes and hepatocytes and exhibited excellent plasma stability with equal partitioning between whole blood and plasma. Screening for potential drug-drug interactions (DDI) against seven common cytochrome (CYP) p450 isoforms indicated no significant CYP inhibition at concentrations up to 10 μM. Screening of a transporter protein panel (14 off-targets), also showed no significant inhibition at 30 μM (Supplementary Table S3).
Analysis using a cell health assay for potential cytotoxicity showed no toxicity up to 100 μM SNT-8370. Furthermore, SNT-8370 presented no significant inhibition of sodium, calcium, or potassium ion channels at the same test concentration (Supplementary Table S2). Potential for oxidation of the allylamine in SNT-8370 by the related copper-dependent amine oxidase off-targets (plasma amine oxidase using canine AOC438 and human DAO) was assessed, with no turnover observed (Supplementary Fig. S3). No significant off-targets were identified in the Eurofins PanLabs screen (68 off-targets, Supplementary Table S4) at a concentration of 10 μM.
In vivo tissue distribution of SNT-8370
The encouraging in vitro ADME profile led to an in vivo time-tissue distribution study in the mouse (Supplementary Table S5). SNT-8370 was quickly absorbed with the highest drug concentrations measured 1 h after oral gavage. SNT-8370 was cleared comparatively rapidly with a half-life of 2–4 h. High concentrations of the drug in both the kidney and the liver indicate these organs may serve as primary routes of clearance of the parent compound. No drug was detectable in the brain.
SNT-8370 effectively inhibits VAP-1 and MPO activities in vivo
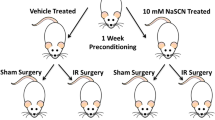
To examine the in vivo target engagement of SNT-8370 as a dual-inhibitor of VAP-1 and MPO, two peritonitis models of acute inflammation were employed.
First, mice were treated with thioglycolate broth intraperitoneally (i.p.) to recruit leucocytes into the peritoneum over 20 h, which was followed by oral administration of SNT-8370 or verdiperstat at different doses. One hour later, i.p. administration of zymosan A activated the recruited leucocytes resulting in their degranulation and release of MPO over 4 h (Fig. 6A). MPO activity (measured ex vivo by the MPO Activity on a Polymer Surface [MAPS] bioluminescence assay39) and drug concentrations in the isolated peritoneal lavage fluid were determined to establish a pharmacokinetic/pharmacodynamic (PK/PD) relationship. Lavage fluid isolated from mice treated with thioglycolate and zymosan A had a markedly elevated MPO enzyme activity (Fig. 6B). SNT-8370 at oral doses of 10 and 30 mg/kg had no effect on MPO activity (Fig. 6B—only 30 mg/kg dose shown), which corresponded to the detection of very low concentrations (1.1 ng/mL and 1.5 ng/mL respectively; equivalent to <4 nM drug) of SNT-8370 in the peritoneal lavage fluid (Fig. 6D). However, an oral dose of 60 mg/kg of SNT-8370 reduced peritoneal MPO activity in thioglycolate broth/zymosan A-treated mice by >50%, consistent with a higher lavage drug concentration of ~60 ng/mL (170 nM; equivalent to ~10× the IC50 in vitro). Verdiperstat demonstrated a similar PK/PD relationship with significant inhibition of MPO activity of >50% also only observed at a dose of 60 mg/kg (Fig. 6B), consistent with the detection of peritoneal drug concentrations of >10 ng/mL (Fig. 6E). Treatment with SNT-8370 or verdiperstat had no effect on the thioglycolate broth/zymosan A-induced increase in lavage fluid MPO protein concentration (Fig. 6C), verifying that in vivo MPO inhibition by both compounds reflects direct inhibition of enzyme activity.
A Peritoneal inflammation and leucocyte recruitment was induced in male C57Bl/6J mice by i.p. injection of thioglycolate broth for 20 h. Control mice (Con) received i.p. injection of PBS (n = 7). After 20 h, thioglycolate broth-treated mice received SNT-8370 by oral gavage at 30 (n = 4) or 60 mg/kg (n = 6), verdiperstat at 30 (n = 3) or 60 mg/kg (n = 6), or vehicle control (n = 7). One hour later, mice were administered zymosan A i.p. to promote leucocyte activation and MPO release. After 4 h, the inflammatory exudates were collected via peritoneal lavage and analysed for MPO activity and protein levels. B Effect of oral drug treatment on peritoneal MPO activity in thioglycolate broth/zymosan A-treated mice with peritonitis. Results are expressed as a % of MPO activity apparent in thioglycolate broth/zymosan A, vehicle-treated mice with peritonitis and represent the mean ± SEM for non-treated, control (Con) mice (n = 7) or peritonitis mice treated with vehicle control (n = 7), SNT-8370 at 30 mg/kg (n = 4) or 60 mg/kg (n = 6), and verdiperstat at 30 mg/kg (n = 3) or 60 mg/kg (n = 6). Data was analysed by one-way ANOVA (Dunnett’s post hoc). p values shown are versus vehicle control mice with peritonitis. C MPO protein levels in the peritoneum were determined by ELISA. Data represents the mean ± SEM (n = 3 for all treatments). The concentrations of D SNT-8370 and E verdiperstat present in the peritoneal lavage fluid at 5 h after oral gavage were measured by mass spectrometry. Data represent the mean ± SEM for D SNT-8370 at 10 (n = 3), 30 (n = 3), or 60 (n = 3) mg/kg and E verdiperstat at 10 (n = 3), 30 (n = 3) or 60 (n = 6) mg/kg.
In a second peritonitis model, animals were administered the test drugs 1 h prior to i.p. administration of thioglycolate broth. Total leucocytes and neutrophil infiltration into the inflamed peritoneum were then assessed at 6 h (Supplementary Fig. S4A). SNT-8370 and verdiperstat were dosed at 60 mg/kg as this was efficacious in the previous model. The VAP-1 inhibitor PXS-4707 (see Supporting Information, Supplementary Table S6 for the profile of PXS-4707 as a potent and selective VAP-1 inhibitor), a PXS-4728 analogue with similar PK/PD profile, was dosed at 6 mg/kg, an efficacious in vivo dose previously documented for PXS-472840,41. Only SNT-8370 significantly reduced the thioglycollate broth-induced elevation in total immune cells (Supplementary Fig. S4B) and neutrophils (Supplementary Fig. S4C) into the peritoneum. Neither of the monotherapy treatments showed a significant effect. Analysis of in vivo VAP-1 activity in the adipose tissue showed >90% inhibition for SNT-8370 and PXS-4707 treated groups (Supplementary Fig. S4D), confirming efficacious in vivo target engagement for VAP-1 had been achieved by both compounds. The lack of efficacy observed with PXS-4707 is in line with reports by Noonan et al.42 showing that VAP-1 oxidase null mice also show no significant reduction in peritoneal leucocyte trafficking into the thioglycolate broth inflamed peritoneum, and suggests that the inflammatory response present in this in vivo model is only attenuated by a strong anti-inflammatory therapy such as that provided by the simultaneous dual-inhibition of VAP-1 and MPO with SNT-8370.
SNT-8370 exhibits enhanced and sustained in vivo anti-inflammatory activity in the carrageenan air pouch model
The murine air pouch model of carrageenan-induced oedema is a standard model of acute inflammation driven by a predominantly neutrophilic response43. At 30 min prior to application of λ-carrageenan solution into the air pouch, the animals were given a single oral dose of either vehicle, SNT-8370, verdiperstat or the VAP-1 inhibitor PXS-4707. Dexamethasone was used as a positive anti-inflammatory control. The impact of the drugs on carrageenan-induced leucocyte infiltration was assessed at (i) 4-h or (ii) 12-h post-carrageenan challenge with the test drugs re-administered at 8 h (Fig. 7A). Figure 7B shows that dexamethasone and all three test treatments significantly reduced leucocyte influx into the air pouch at 4-h. However, at the 12-h time point, whilst the potent anti-inflammatory dexamethasone significantly suppressed air pouch leucocyte levels, neither of the mono-therapy treatments (verdiperstat or PXS-4707) showed a significant effect (Fig. 7C). In contrast to monotherapy, SNT-8370 significantly reduced leucocyte influx at 12-h (at 30 mg/kg). Moreover, dexamethasone and SNT-8370 (at 10 and 30 mg/kg), but neither verdiperstat nor PXS-4707, significantly reduced the carrageenan-induced increase in exudate volume at 12-h as a measure of inflammatory oedema (Fig. 7D).
A Male BALB/c mice were injected with a sterile air pouch on the nape of their necks at day 0 and 3. On day 6, at 30 min prior to administration of the λ-carrageenan solution into the sterile air pouch, the animals were given a single oral dose of either control vehicle (n = 8), SNT-8370 (3 [n = 8], 10 [n = 8] or 30 [n = 8] mg/kg), verdiperstat (15 mg/kg [n = 8]) or PXS-4707 (6 mg/kg [n = 8]). Dexamethasone (10 mg/kg [n = 8]) was used as a positive anti-inflammatory control. Mice were re-dosed with vehicle or test drugs at 8 h post-λ-carrageenan challenge. Untreated control (Con) mice received de-ionised water i.p (instead of λ-carrageenan). The impact of the test drugs on λ-carrageenan-induced leucocyte infiltration into the inflamed sterile air pouch was assessed at (B) 4 h or (C) 12 h post-λ-carrageenan challenge and (D) sterile air pouch exudate volume at 12 h post-λ-carrageenan challenge. B, C Data is expressed as mean ± SEM of the total number of white blood cells (WBC) in the sterile air pouch at (B) 4 h for Con (n = 8), λ-carrageenan alone (n = 8), dexamethasone (n = 6), PXS-4707 (n = 8), verdiperstat (n = 8), SNT-8370 at 30 mg/kg (n = 7) and (C) 12 h for Con (n = 7), λ-carrageenan alone (n = 8), dexamethasone (n = 8), PXS-4707 (n = 7), verdiperstat (n = 8) and SNT-8370 at 3 (n = 7), 10 (n = 8), or 30 (n = 7) mg/kg. D Data is expressed as mean ± SEM of sterile air pouch exudate volume at 12 h post-λ-carrageenan challenge (n = 8 mice for all treatments). Data was analysed by a one-way ANOVA (Dunnett’s post hoc).
SNT-8370 shows augmented in vivo anti-inflammatory activity in a mouse model of acute lung injury
To further investigate the in vivo anti-inflammatory activity of SNT-8370 we next studied its capacity to suppress pulmonary immune cell infiltration in a mouse model of acute lung injury. For this, mice were orally treated with SNT-8370, verdiperstat or PXS-4707 1 h prior to intranasal installation of lipopolysaccharide (LPS). At 6 h post-LPS administration the lung levels of total leucocytes and neutrophils were measured in the bronchoalveolar lavage fluid (Fig. 8A). Of the treatments, SNT-8370 significantly reduced lung infiltration of total leucocytes (Fig. 8B) and neutrophils (Fig. 8C) in LPS-treated mice, while verdiperstat and PXS-4707 exhibited non-significant downward trends in these cell parameters. This data further confirms the augmented in vivo anti-inflammatory activity provided by the simultaneous dual-inhibition of VAP-1 and MPO with SNT-8370 versus monotherapy.
A–C Acute Lung Injury. A Female BALB/cJUnib mice were non-treated (control, con) or treated with vehicle, SNT-8370 (30 mg/kg), verdiperstat (30 mg/kg) or PXS-4707 (10 mg/kg) 1 h prior to intranasal administration of LPS. Mice were then euthanised at 6 h after LPS instillation and the impact of the drugs on lung infiltration (BALF) of (B) total leucocytes (con n = 6, vehicle n = 5, SNT-8370 n = 6, verdiperstat n = 6, PXS-4707 n = 6) and (C) neutrophils (con n = 6, vehicle n = 5, SNT-8370 n = 5, verdiperstat n = 6, PXS-4707 n = 6) measured. Data is expressed as the number of cells/mL of BALF and represents the mean ± SEM. Data was analysed by one-way ANOVA (Tukey’s post hoc). p values shown are versus LPS + vehicle group. D–I Myocardial Infarction. D Male Sprague Dawley rats were administered control vehicle or SNT-8370 (60 mg/kg) by oral gavage just prior to LAD occlusion or sham surgery. The LAD occlusion was released after 30 min and rats were treated twice daily with vehicle or SNT-8370 (60 mg/kg) by oral gavage for a further 28 days before E ejection fraction and F fractional shortening were measured via cardiac ultrasound. E, F Data represents the mean ± SEM (Sham n = 5, LAD/control vehicle n = 6, LAD/SNT-8370 n = 5). Data was analysed by one-way ANOVA (Dunnett’s post-hoc). Cardiac fibrosis was measured in left ventricle tissue sections by G picrosirius red (LAD/control vehicle n = 7, LAD/SNT-8370 n = 6), H Masson’s trichrome (LAD/control vehicle n = 8, LAD/SNT-8370 n = 5) and I periostin (LAD/control vehicle n = 5, LAD/SNT-8370 n = 5) staining. Data is expressed as a % of positive staining per left ventricle tissue area and represents the mean ± SEM. Data was analysed by Student’s t test (two-tailed). p values shown are versus the LAD/control group.
SNT-8370 protects against myocardial infarction and obstructive nephropathy
Finally, we tested the potential protective actions of SNT-8370 in two distinct pre-clinical inflammatory disease models: (i) myocardial infarction and (ii) tubulointerstitial renal fibrosis in the obstructed kidney.
For myocardial infarction (MI), we employed the widely studied rat myocardial ischaemia/reperfusion (I/R) injury model, which is characterised by a complex multicellular immune/inflammatory reaction that is a pre-requisite for cardiac healing and fibrotic scar formation and critical determinant of infarct size and the degree of cardiac dysfunction post-MI44,45. For this, an MI in rats was surgically induced by transient (30 min) ligation of the left anterior descending coronary artery (LAD) followed by release of the ligature to restore LAD blood flow. Rats received SNT-8370 immediately prior to the LAD procedure and subsequently twice-daily via oral gavage for a further 4 weeks post-MI induction (Fig. 8D). After 4 weeks, cardiac function was measured by echocardiography and correlated with the degree of cardiac fibrosis. Rats subject to LAD ligation exhibited cardiac dysfunction as indicated by decreased ejection fraction (Fig. 8E) and fractional shortening (Fig. 8F), which correlated with increased cardiac fibrosis, as judged by picrosirius red (Fig. 8G), masons trichrome (Fig. 8H) and periostin (Fig. 8I) staining. Notably, SNT-8370 treatment prevented the significant post-MI reduction in ejection fraction and fractional shortening that occurred in vehicle-treated rats receiving LAD ligation (Fig. 8E, F). The preserved cardiac function afforded by SNT-8370 treatment correlated with the dual-inhibitors capacity to significantly reduce the LAD-induced increase in cardiac fibrosis across all three fibrotic indices measured (Fig. 8G–I).
For renal fibrosis, mice were subjected to unilateral ureteral obstruction (UUO) surgery involving the ligation of the left ureter followed by twice-daily oral administration of SNT-8370 or the angiotensin-converting enzyme inhibitor captopril (a current effective treatment for obstructive renal fibrosis46) for the next 14 days (Supplementary Fig. S5A). As expected, compared to the control right kidney, UUO surgery induced the development of fibrosis (Supplementary Fig. S5B) and atrophy (indexed as kidney/body weight ratio) (Supplementary Fig. S5C) in the left kidney. SNT-8370 significantly inhibited the development of UUO-induced fibrosis and atrophy in the left kidney, with similar efficacy as captopril (Supplementary Fig. S5).
Discussion
Inflammatory diseases are a major health burden with their pathogenesis commonly underpinned by the reciprocity of pro-inflammatory and oxidative stress enzymes and pathways47,48,49. The current study describes the design and development of SNT-8370 as an orally bioavailable small molecule. SNT-8370 is a potent and selective mechanism-based dual-inhibitor that successfully targets two critical pro-inflammatory, oxidative stress enzymes, VAP-1 and MPO, which play complimentary pathogenic roles in a range of inflammatory disorders7,16. SNT-8370 equipotently inhibited VAP-1 and inhibited MPO with superior efficacy when compared to recent clinically-trialled benchmark VAP-1 and MPO inhibitors. Thus, compared to verdiperstat, SNT-8370 inhibited MPO-catalysed H2O2-consumption and HOCl production by 2–5-fold greater efficacy and MPO-mediated LDL lipid peroxidation with 30-fold greater potency. Molecular modelling combined with in vitro mechanistic studies indicated that the enhanced MPO inhibition reflects a stronger binding of SNT-8370 within the MPO active site pocket, potentially involving interaction with a key gatekeeper residue Glu116 at the entry of the MPO pocket. This results in tighter inhibitor binding and reduced turnover. SNT-8370 was selective for VAP-1 and MPO, exhibiting >100–1000-fold more potency versus other mammalian amine oxidase or heme peroxidase family members. Standard preclinical ADME assays and a tissue distribution assay in mice, showed that SNT-8370 exhibited favourable safety and PK profiles. Studies in mice also showed that SNT-8370 effectively inhibited MPO and VAP-1 activities in vivo. Notably, compared to monotherapy, SNT-8370 provided an enhanced and sustained inhibition of leucocyte infiltration in three different mouse models of acute inflammation and provided protection in pre-clinical models of myocardial ischaemia-reperfusion injury and UUO-induced nephropathy. Together these studies identify SNT-8370 as a mechanism-based dual inhibitor of VAP-1 and MPO that holds significant potential as a broad-range anti-inflammatory therapeutic.
VAP-1 and MPO belong to the broader mammalian amine oxidase and heme peroxidase families, respectively. SNT-8370 inhibited VAP-1 and MPO by >100–1000-fold potency versus physiologically important family members as well as other macromolecular targets typically tested in secondary pharmacology50 further strengthening its excellent pre-clinical properties. In vitro ADME assays and in vivo tissue distribution analysis revealed that SNT-8370 is metabolically stable, shows no specific DDI and distributes well into the kidney, liver and lung, but not the brain (in contrast to verdiperstat).
To study the PK/PD relationship with respect to MPO activity we employed a model of acute inflammatory peritonitis previously employed by Tiden et al., for the in vivo characterisation of 2-thioxanthines as effective MPO inhibitors28. An oral dose of 60 mg/kg afforded sufficient drug bioavailability within the inflamed peritoneum necessary for SNT-8370 or verdiperstat to outcompete an array of endogenous reactive MPO substrates and effectively inhibit peritoneal MPO activity by >50%. Separate studies also showed that at this dose SNT-8370 afforded >90% inhibition of in vivo VAP-1 activity, measured in adipose tissue where high levels of the enzyme are expressed7. Together these pre-clinical studies confirmed that SNT-8370 can effectively inhibit both MPO and VAP-1 enzyme activities in vivo.
Drug-drug conjugates are made by combining recognised binding motifs for each protein through a linker. However, the issue with such approaches (e.g. PROTAC) is that they often produce molecules with suboptimal physiochemical properties (e.g., high molecular weight, high lipophilicity, low structural rigidity), leading to poor ADME properties such as low oral bioavailability, and increased risk of metabolism and DDI51,52,53. Key to the success of producing dual-inhibitors with oral bioavailability is identification of common pharmacophores so that molecules can be truncated and remain within typical small molecule drug-like dimensions, adhering to the principles that guide drug design (e.g. Lipinski’s rule-of-five). SNT-8370 was designed based on a maximum overlap approach that combines the active warhead moieties of a VAP-1 inhibitor PXS-472840,41 and an MPO inhibitor AZD590428 joined through a common aromatic ring. The unexpected finding that this central aromatic core could be attached directly to both warheads, maintaining (and in the case of MPO, augmenting) potency for each target, whilst preserving mechanism-of-action and selectivity for the relevant target proteins, led to a dual inhibitor that has a low molecular weight (361.4 amu) and low lipophilicity (cLogP −0.03), affording oral bioavailability, good metabolic stability and low risk of DDI.
Dual inhibitors that simultaneously target VAP-1 and MAO B proteins have been previously described for the treatment of neuroinflammatory (NCT05904710) and muscular disorders12. The dual VAP-1/MAO B inhibitors exhibit CNS penetration and target two related members of the same amine oxidase enzyme family via the same fluoroallylamine binding site. In contrast, SNT-8370 does not cross the blood brain barrier and constitutes a more general anti-inflammatory agent that inhibits two distinct but functionally complementary pro-inflammatory enzyme families in VAP-1 and MPO by simultaneously targeting two disparate enzyme binding motifs via two different chemical warheads.
Endothelial-expressed VAP-1 plays a critical role in facilitating the recruitment of leucocytes into inflammatory tissues or organs7. MPO also plays a complex and contextual role in controlling leucocytes, which depending on the inflammatory stimulus and environment can promote or suppress leucocyte recruitment54,55. In the current study, we examined the anti-inflammatory activity of dual VAP-1/MPO inhibition by SNT-8370 by measuring its in vivo inhibitory capacity on leucocyte recruitment in three distinct models of acute inflammation, i.e. thioglycollate-mediated peritonitis, carrageenan-mediated air pouch and LPS-induced acute lung injury inflammation models. The effect of SNT-8370 was compared with monotherapies that individually target VAP-1 or MPO. Compared to single-target inhibitors SNT-8370 exhibited heightened anti-inflammatory activity in all three models. Thus, SNT-8370, but not single VAP-1 (PXS-4707) and MPO (verdiperstat) inhibitors, significantly reduced total leucocyte and neutrophil infiltration into the inflamed peritoneum. Moreover, compared to single inhibitors, SNT-8370 provided a significantly robust and sustained inhibition of leucocyte infiltration and oedema formation in the carrageenan-induced inflammatory air pouch model. Notably, in the air pouch model SNT-8370 exhibited similar anti-inflammatory activity as the potent anti-inflammatory corticosteroid, dexamethasone. Finally, SNT-8370, but not monotherapies, significantly suppressed pulmonary leucocyte and neutrophil infiltration in the mouse model of acute lung injury. We envisage that the superior in vivo anti-inflammatory activity of SNT-8370 versus VAP-1 or MPO monotherapies reflects the capacity of the dual-inhibitor to potently inhibit both targets combined with improved pharmacokinetic and pharmacodynamic properties.
We also showed that SNT-8370 provided significant protection in two different inflammatory disease models characterised by tissue fibrosis and injury, i.e. myocardial ischaemia/reperfusion injury model and UUO-induced nephropathy. In the myocardial ischaemia/reperfusion model SNT-8370 potently inhibited the development of cardiac fibrosis and preserved normal myocardial function post-MI. In the nephropathy model SNT-8370 showed similar efficacy as a current clinical agent, captopril, in protecting against renal fibrosis and atrophy.
Together these findings highlight the excellent anti-inflammatory activity achieved in vivo by the simultaneous inhibition of VAP-1 and MPO with SNT-8370 across multiple animal models of tissue inflammation highlighting the discovery of a versatile dual inhibitor anti-inflammatory therapeutic. Our findings are also congruent with a recent report studying an inflammatory model of vasculitis that concluded that effective anti-inflammatory therapy in this model requires the targeting of leucocyte effector functions in addition to MPO56. Therefore dual-inhibition of MPO and VAP-1 with SNT-8370 is a promising anti-inflammatory therapeutic strategy with a low safety risk and high benefit.
Considering the significant clinical trial interest in the discovery of selective VAP-1 and MPO inhibitor drugs for the treatment of various inflammatory diseases and the wealth of clinical data showing that inhibition of either target is safe and efficacious, the discovery of SNT-8370 as a potent and selective drug-drug conjugate targeting both VAP-1 and MPO, therefore, holds promise as a versatile anti-inflammatory therapeutic.
Methods
Chemistry for the synthesis of SNT-8370
SNT-8370 was synthesised using the protocol outlined in Steps i - vii in Supplementary Fig. S6 (See Supporting Information for full details).
VAP-1 activity assay
Human recombinant VAP-1/SSAO amine oxidase activity was determined using the coupled fluorometric method for monoamine oxidase, copper-containing amine oxidases and related enzymes following published protocols30,57 (See Supporting Information for full details).
Monoamine oxidase (MAO; MAO-A/MAO-B), diamine oxidase (DAO) and lysyl oxidase (LOX) activity assays
Similar to VAP-1, enzymatic activity in the related amine oxidases was carried out using the coupled fluorometric method (See Supporting Information for full details).
MPO activity assays
To study the impact of inhibitors on MPO activity, purified human MPO from polymorphonuclear leucocytes (Calbiochem; Cat# 475911-100 µg) was employed.
MPO-catalysed H2O2 consumption assays
The effect of inhibitors on MPO-catalysed H2O2 consumption was assessed using a high-throughput Amplex Red fluorescent-based assay or an H2O2-specific microelectrode (ISO-HPO-2, World Precision Instruments) assay following published methods29,58 (See Supporting Information for full details).
MPO chlorination assay
To examine the effect of inhibitors on MPO-catalysed chlorination activity the production of HOCl was measured spectrophotometrically by quantitating the conversion of taurine into taurine mono-chloramine using the iodide-catalysed 3,3’,5,5’ tetramethylbenzidine (TMB) assay following published methods59,60 (See Supporting Information for full details).
MPO partition ratio assay
The MPO partition ratio of inhibitors was determined following published methods22. Assay mixtures (total volume 150 μL) contained 50 mM Na2PO4 (pH 7.4), 1 mM diethylenetriaminepentaacetic acid (DTPA), test inhibitor (titrated 0–5 μM), or DMSO vehicle in the absence or presence of H2O2 (2 μM). Reactions were initiated by the addition of MPO (60 nM), followed by incubation for 15 min at room temperature. After this time, 5 μL of the MPO/inhibitor reaction mixture was diluted 300-fold into new MPO assay mixture consisting of 50 mM Na2PO4 (pH 7.4), 1 mM DTPA, 2 μM H2O2 and 30 μM Amplex Red (Invitrogen). The final DMSO concentration in all reactions was 2% (v/v). The reaction mixture was rapidly vortexed and 100 μL transferred into a 96-well, black, nonbinding surface, polystyrene plate (Corning) and the changes in Amplex Red fluorescence monitored at room temperature every 20 s on a Spectramax M3 Microplate Spectrophotometer (Molecular Devices) with excitation and emission filters set at 530 nm and 580 nm, respectively. The initial linear rate of change in Amplex Red fluorescence was determined over ~200 s, which provided a readout of MPO-catalysed H2O2 consumption or activity. MPO enzyme activity was expressed as a percentage of control and plotted as a linear function of the ratio of the concentration of test inhibitor to MPO enzyme concentration (i.e. [inhibitor]/[enzyme]). The partition ratio was calculated as the point at which the straight line intersected the x-axis22.
Rapid jump dilution assays
The following jump dilution assays for MPO and VAP-1 were based on the protocol outlined by Ward and colleagues29.
MPO jump dilution
MPO (30 nM) was pre-incubated in the presence of 2 μM H2O2 and inhibitors at a concentration ~300-fold higher than the IC50 value, or DMSO as a vehicle control for 15 min at room temperature. The reaction mixture was then rapidly diluted 300-fold into the assay buffer containing 50 mM sodium phosphate buffer (pH 7.4), 1 mM DTPA, 2 μM H2O2 and 30 μM Amplex Red. The reaction was mixed and 100 μL transferred to a 96-well assay plate. The target percentage activity was measured as a function of time after the dilution event, averaging the slope over the period between 6-18 min.
VAP-1 jump dilution
For VAP-1 the measurement of the residence time was based on the detection of H2O2 with an Amplex Red oxidation assay in a 96 well format. The VAP-1 protein (700 nM) was incubated with inhibitors at 30-fold the IC50 for 60 min at 37 °C in SnapStrip PCR vials. After the incubation, a 50-fold dilution was carried out by adding the assay buffer (0.1 M sodium phosphate buffer, pH 7.4), immediately followed by a 1:2 dilution with an equal volume of reaction mixture (a mixture of 600 μM benzylamine [Sigma Aldrich], 120 μM Amplex Red [Sigma Aldrich] and 1.5 U/mL horseradish peroxidase [Sigma Aldrich] prepared in 0.1 M sodium phosphate buffer, pH 7.4) and subjected to measurement as described in the VAP-1 enzymatic assay detailed above. The remaining percentage activity was measured as a function of time after the dilution event, averaging the slope over the period between 21 and 30 min.
MPO LDL lipid peroxidation assay
Isolation of LDL
Human LDL was rapidly isolated from human blood following published methods61,62 (See Supporting Information for full details). Blood was collected from informed and consenting healthy, non-fasted donors (University of New South Wales, Human Research Ethics Committee [UNSW HREC], Protocol Number HC13212).
Lipoprotein oxidation
LDL oxidation reactions were carried out following published methods26,27. Briefly, LDL (0.2 mg protein/mL) in 50 mM sodium phosphate buffer (pH 7.4) supplemented with 100 μM DTPA was incubated at 37 °C in the presence of 30 nM MPO, 0.5 mM NaNO2 and 500 μg/mL glucose plus 100 ng/mL glucose oxidase (Sigma Aldrich) for 2 h in the absence or presence of test inhibitors (0–10 μM) in a final reaction volume of 100 μL. The concentrations of glucose/glucose oxidase employed generated a constant flux of H2O2 of ~1 μM/min, as verified by an H2O2-specific electrode (ISO-HPO-2, World Precision Instruments). After 2 h, the reactions were terminated by addition of 300 nM catalase and 40 μM butylated hydroxytoluene (BHT). Aliquots (100 μL) of reaction mixtures were extracted and analysed by HPLC for neutral lipids (free cholesterol and cholesteryl esters), and cholesteryl ester hydro(per)oxides (CE-O(O)H), following published methods61,63,64 (See Supporting Information for full details).
LPO, EPO, TPO and PXDN assays
LPO activity
Inhibitors were diluted to desired concentrations in phosphate buffer (50 mM Na2HPO4, 140 mM NaCl, pH 7.4), and added to a glass tube supplemented with sodium thiocyanate (SCN−, 100 μM) and GSH (100 μM), with rapid mixing following published methods28. A stable reading for H2O2 concentration was established after H2O2 (50 μM) addition. Subsequently, 10 nM bovine LPO (Sigma-Aldrich) was added to the reaction buffer (final reaction volume was 1 mL) and H2O2 consumption continuously recorded for a further 8 min using an H2O2-specific electrode (ISO-HPO-2) interfaced to an Apollo 4000 Free Radical Analyser (World Precision Instruments) and LabScribe software (iWorx Systems Inc.). The initial rate of LPO-catalysed H2O2 consumption was determined from 140 s after LPO addition, and measured via linear regression over a further 100 s.
EPO activity
Inhibitors were diluted to desired concentrations in phosphate buffer (100 mM Na2HPO4, 100 mM NaCl, pH 7.4) and added to a glass tube supplemented with NaBr (100 μM), DTPA (20 μM), and GSH (30 μM), with rapid mixing following published methods65. A stable reading for H2O2 concentration was established after addition of H2O2 (30 μM). Reactions were intiated by addition of 8 nM human EPO (Planta) to the reaction buffer (final reaction volume was 1 mL), and H2O2 consumption was continuously recorded for a further 8 min using an H2O2-specific electrode (World Prescision Instruments). The initial rate of EPO-catalysed H2O2 consumption was determined from 140 s after the addition of EPO, and measured via linear regression over a further 100 s.
TPO activity
TPO activity was assessed by the peroxidase-mediated ascorbate oxidation assay following published methods28,66. Inhibitors were diluted to desired concentrations in phosphate buffer (10 mM Na2HPO4, 140 mM NaCl, pH 7.4) supplemented with ascorbic acid (100 μM), DTPA (100 μM) and NaI (50 μM). Human TPO (200 nm, Abacus dx) was added to each tube and the mixture incubated for 5 min at room temperature. Reaction mixtures were transferred to UV-transparent 96-well assay plates (UV-Star®, Sigma-Aldrich) and reactions initiated by addition of H2O2 (25 μM), and rapidly mixed (final reaction volume was 210 μL). TPO-catalysed ascorbate oxidation was continuously monitored every 20 s for 6 min at 266 nm with the rate of reaction calculated over the initial 200 s of the reaction (Spectramax M3; Molecular Devices).
PXDN activity
Inhibitors were diluted to the desired concentration in 100 μL of 50 mM phosphate buffer (pH 7.4) containing recombinant human PXDN (0.2 μg; cloned, purified and characterised following published methods67) in a 96-well plate. The reaction was started by adding 100 μL of Amplex™ UltraRed (50 μM), H2O2 (20 μM) and sodium bromide (NaBr; 50 mM) in 50 mM phosphate buffer (pH 7.4) resulting in the final concentrations of 0.1 μg of PXDN, 25 μM Amplex Red, 10 μM H2O2, 25 mM NaBr and an inhibitor concentration range of 0–60 μM. The plate was incubated in the dark for 15 min at 37 °C before fluorescence of resorufin, the resulting Amplex Red oxidation product, was detected using a SpectraMax iD3 fluorescent plate reader from Molecular Devices (λex 544 nm, λem 590 nm, end-point measurement).
Molecular modelling of SNT-8370 as an inhibitor of MPO
Molecular modelling of SNT-8370 in the MPO active site was carried out by Evotec (Verona) using the Molecular Operating Environment (MOE®) drug discovery software platform under license from the Chemical Computing Group. Details of the operations carried out are outlined in the main Results text.
Absorption, distribution, metabolism, excretion (ADME) and off-target profiling assays
The following studies were carried out at GVK Bio, Hyderabad, India.
Microsomal stability in the presence of human, rat and dog microsomes was carried out in duplicate at a concentration of 1 μM in the absence and presence of NADPH. The amount of test article remaining was monitored by LC/MS over time.
Hepatocyte stability in the presence of human, rat and dog cryo-preserved hepatocytes was carried out in duplicate at a concentration of 1 μM. The amount of test article remaining was monitored by LC/MS over time.
Plasma protein binding in human, rat and dog plasma was carried out in duplicate at a concentration of 10 μM using the commercially available rapid equilibrium dialysis (RED) kit (ThermoFisher). SNT-8370 was incubated for 5 h at 37 °C in the presence of plasma. The amount of test article recovered was calculated by LC/MS.
Plasma stability in the presence of human, rat and dog plasma was carried out in duplicate at a concentration of 1 μM. The amount of test article remaining was monitored by LC/MS over time.
Whole blood/plasma partitioning was carried out by incubation of SNT-8370 at 1 μM in pooled blood and plasma samples for 60 min with thorough mixing. Blood sample was centrifuged, and the plasma supernatant obtained was compared to the plasma control sample via LC/MS analysis.
Inhibition of the cytochrome p450 enzymes was measured using pooled human liver microsomes, incubating SNT-8370 for 10 min at different concentrations, and the respective CYP isoform activity measured using an LC/MS assay with the appropriate substrates (CYP1A2 (Tacrine), CYP2C9 (Diclofenac), CYP2C19 (S-Mephenytoin), CYP2D6 (Dextromethorphan), CYP3A4 (Midazolam), CYP2B6 (Bupropion Hcl) and CYP2C8 (Paclitaxel)) in the presence of NADPH.
SNT-8370 was tested in vitro for the potential to affect cell health following published methods outlined by Fujimura et al.68 at concentrations up to 100 μM.
Ion channel assessment was carried out at Evotec (Verona) using Rapid ICE™ hERG, hCav1.2 and hNav1.5 current recordings in stably transfected cells at concentrations of 10, 30 and 100 μM of SNT-8370.
Oxidative (substrate) turnover by recombinant human VAP-1, human DAO and AOC4 (from diluted dog serum) was measured by a fluorometric assay30,57 over a period of 40 min at 37 °C in HEPES buffer in the presence of Amplex Red (20 μM), horse radish peroxidase (HRP, 4 U/mL) and the test compound (at a final concentration of 30 μM). The total formation of resorufin over time was measured using an Optima reader (BMG Labtech GmbH, Ortenburg, Germany) at 37 °C. Benzylamine (at 600 μM) was used as the positive control.
Off-target activity was assessed at Eurofins Panlabs Taiwan, Ltd. using the Eurofins Discovery Lead Profiling Screen® panel of 68 enzymes, receptors, ion channels and transporters and measuring the percentage inhibition at a single 10 μM concentration.
Potential transporter activity was assessed at Eurofins Panlabs Taiwan, Ltd. using the Eurofins Transporter Protein Screen panel of 14 common transporters and measuring the percentage inhibition at a single 30 μM concentration.
In vivo testing of SNT-8370
General animal husbandry
In general, experimental animals were housed in SPF conditions on a routine 12-h day/12-h night cycle with food and water available ad libitum. Animals were housed in conventional caging and given standard chow for the study duration. Unless specified, experimental animals were euthanized by CO2 asphyxiation.
Acute peritonitis
The acute peritonitis studies were performed in accordance with the National Health and Medical Research Council of Australia guidelines with approval by the Animal Care and Ethics Committee at the University of New South Wales (Application no.17/8A). In this model, following published methods28, male C57BL/6J mice (8–10 weeks of age; Australian Bioresources, Moss Vale, NSW, Australia) initially received a 1 mL intraperitoneal injection of 4% (w/v) thioglycolate broth, to induce leucocyte recruitment into the peritoneum. The broth was prepared by adding 4% (w/v) thioglycolate medium (Becton Dickinson) to distilled water, and the solution was brought to boil with constant mixing. Once dissolved, the solution was cooled to room temperature. At 20 h after thioglycolate broth administration, mice received a single dose (via oral gavage) of test drug at 10, 30, or 60 mg/kg of body weight dissolved in vehicle (0.5% hydroxypropyl methyl cellulose [HPMC, Sigma-Aldrich], with 0.1% [w/v] Tween 80 in water). One hour after oral gavage, the recruited leucocytes were activated by intraperitoneal injection of 0.5 mL of zymosan A (10 mg/mL) (from Saccharomyces cerevisiae, Sigma-Aldrich) in 0.9% sterile saline (Baxter). Four hours after zymosan A treatment, mice were euthanised by CO2 asphyxiation, and the peritoneal cavity was lavaged with 5 mL of ice-cold PBS. Peritoneal exudate cells were pelleted by centrifugation (2000 × g, 5 min at 4 °C), and supernatants analysed for MPO activity using a bioluminescence assay, measuring MPO Activity on a Polymer Surface (MAPS)39. For this assay, lavage supernatants were diluted with MAPS loading buffer (130 mM NaCl, 6.28 mM Na2HPO4, 18.7 mM NaH2PO4 and 50 ppm v/v Tween 20) to a total volume of 500 μL. Samples were thoroughly mixed and 100 μL/well loaded into a black-walled, tissue culture-treated 96-well microtiter plate (Corning). The plate was covered and shaken at 1,000 rpm for 30 min at room-temperature, to facilitate protein binding to the well surfaces. Each well was then aspirated and washed three-times with MAPS loading buffer (twice with 150 μL, then once with 300 μL). Each well then received 75 μL of freshly prepared MAPS imaging solution (3.1 mM citric acid, 21.9 mM trisodium citrate, 20 mM NaBr, 200 mM (NH4)2SO4 and 100 ppm v/v Tween 20) supplemented with 50 μM L-012 (Wako), and 100 μM H2O2 (added immediately before measurements). The plate was briefly shaken at 1000 rpm and read immediately. Bioluminescence was continuously monitored every 20 s for 16 min, using an EnSpire® Multimode Plate Reader (PerkinElmer). Area Under Curve (AUC), of Relative Luminescence Units (RLU) over 16 min, was calculated and the data expressed as a percentage of positive control. The MPO protein content in lavage supernatants was determined by ELISA (Hycult).
Peritonitis leucocyte trafficking model
These studies were performed in accordance with the National Health and Medical Research Council of Australia guidelines with approval by the Animal Care and Ethics Committee at the University of New South Wales (Application no.17/8A). Male C57Bl/6J mice (8–10 weeks of age; Australian Bioresources, Moss Vale, NSW, Australia) received a single dose (via oral gavage) of SNT-8370 (60 mg/kg), verdiperstat (60 mg/kg) or PXS-4707 (6 mg/kg). C57Bl/6J mice then received a 1 mL intra-peritoneal injection of 4% (w/v) thioglycolate broth to induce leucocyte recruitment into the peritoneum. At 6 h post-thioglycolate broth administration, mice were euthanised and the peritoneal cavity was lavaged with 5 mL of ice-cold PBS and the peritoneal exudate cells were pelleted by centrifugation (2000 × g, 5 min at 4 °C) followed by resuspension and enumeration of total peritoneal leucocyte and neutrophil levels.
Carrageenan air pouch model
This study was performed by Washington Bioscience Inc. (USA) (Protocol 1042) with approval from the local ethics committee. For these studies, male mice were employed due to their greater response in this model69. On day 0, male BALB/c mice (Envigo, 6–8 weeks of age) were shaved at the nape of the neck, anaesthetised and 6 mL of sterile air (0.2 μm, Sartorius, Cat. 16532) was injected subcutaneously using a 23G × 1½ inch needle fixed to a 6 mL syringe. The injection site was sealed with flexible collodion (Macron, Cat. 4580-02). On day 3, a further 3 mL of sterile air was injected into the neck. 3% (w/v) λ-carrageenan was prepared by dissolving 3 g λ-carrageenan (FLUKA, Cat. 22049, lot 1408463) in 80 mL of hot de-ionised water. Once dissolved, the solution was cooled to room temperature and the volume made up to 100 mL with de-ionised water. On day 6, SNT-8370, verdiperstat and PXS-4707 in 30% (w/v) (2-hydroxypropyl)-β-cyclodextrin (vehicle) or vehicle-only were administered by oral gavage to the mice. At 30 min after test drug administration, mice were injected with 1 mL 3% (w/v) λ-carrageenan, using a 23G × 2-inch needle fitted to a 1 mL syringe, directly into the air pouch. Sham/control animals were administered 1 mL de-ionised water. Eight hours after carrageenan injection, the mice were re-dosed with either the test articles or vehicle. Twelve hours after carrageenan/de-ionised water injection, the mice were anaesthetised and 3 mL of 10 U/mL heparinized saline was injected into the air pouch. The air pouch was gently massaged, the contents immediately removed using an 18G × 1-inch needle fitted to a 5 mL syringe and the exudate volume recorded. An aliquot of exudate was used to measure total white blood cells.
Acute lung injury
This study was carried out at the Federal University of Minas Gerais (UFMG, Belo Horizonte, Brazil) with approval from the Ethics Review Committee on the Use of Animals at UFMG (CEUA-UFMG) under approved protocol 54/2016. For these studies, female mice were employed as in our experience no gender-specific differences are noted in this model. Female BALB/cJUniB mice (8–10 weeks of age) were treated by oral gavage with vehicle control, SNT-8370 (30 mg/kg), verdiperstat (30 mg/kg) and PXS-4707 (10 mg/kg). One hour later, the mice were anaesthetised with ketamine and xylazine and then intranasally instilled with lipopolysaccharide (LPS) (E. coli strain 055:B5, Sigma-Aldrich, 25 µg per animal, titrated for potency prior to experiment starting). After 6 h a bronchoalveolar lavage (BALF) was performed. BALF was centrifuged at 4 °C, 250 × g for 8 min and the supernatant was stored and frozen for further analysis. The pellet was resuspended in 100 μL of saline solution with 3% (w/v) of BSA (Bovine Serum Albumin). Cells were diluted in Turk solution (Imbralab®) and counted in a Neubauer chamber. Based on the total count, around 50,000 cells were added to cytospin slides with 3% (w/v) BSA and centrifuged at 20 × g for 5 min (Shandon III). Slides were stained for May-Grunwald-Giemsa with Panótico Rápido (LB Laborclin) and the differential counts were performed using 100× magnification objective. Cells were differentiated into mononuclear cells, neutrophils and eosinophils (as eosinophils represent less than 0.3% of the cells, results were not shown) based on its morphology. The relative percentage for each cell subset was obtained counting 300 events throughout the slide without repeating fields.
Myocardial infarction
This study was approved by the Sydney Local Health District Animal Welfare Committee, Australia (Protocol Number: 2016-026). For these studies, male rats were chosen as cardiovascular disease mortality rates are substantially higher in men than women70. Male Wistar rats (12–15 weeks of age) were randomly assigned to sham-operated, left anterior descending coronary artery (LAD) ligation with vehicle or LAD ligation with SNT-8370 treatment. The LAD rats were subjected to transient (30 min) occlusion of the LAD coronary artery following published methods71. The sham animals underwent identical surgery, except no ligation of the LAD was performed. Immediately prior to surgical intervention and subsequently twice daily for a period of 4 weeks, rats were administered either vehicle alone or SNT-8370 (60 mg/kg) via oral gavage. At the end of the study, a transthoracic echocardiogram was performed under isoflurane/oxygen anaesthesia using a SonoSite Edge II Ultrasound System and a HSL25×/13–6 MHz transducer (Fujifilm Sonosite, Bothell, WA, USA), viewed in M-mode (A) to measure the left ventricular (LV) end-systolic diameter and LV end-diastolic diameter. The rats were then euthanised under isoflurane/oxygen anaesthesia and exsanguinated by cardiac puncture. Hearts were then excised and processed for histological analysis. Following formalin fixation, tissue processing, paraffin embedding and de-paraffinization, 4 μm sections were stained with picrosirius red (Sigma-Aldrich) or Masson’s Trichrome (Sigma-Aldrich) with hematoxylin counterstaining. For periostin staining, sections were subjected to citrate buffer antigen retrieval, permeabilization and blocking in 10% (v/v) goat serum, prior to staining with anti-periostin primary antibody (1:200 dilution; Abcam, Cat# ab215199) and HRP-conjugated secondary antibody (1:250 dilution; Abcam, Cat# ab288151). Antibody staining was visualised by immersion into DAB Immunohistochemistry Substrate (Sigma-Aldrich). Following dehydration and mounting in DPX (Sigma-Aldrich), stained slides were imaged using a Axio Scan.Z1 slide scanner with quantification performed using ImagePro software (Media Cybernetics, Rockville, MD, USA).
Unilateral ureteral obstruction (UUO)
The UUO procedure was performed following published methods46 by Urosphere SAS, Toulouse, France. All experiments were performed according to the European Community Council Directive 2010/63/UE and the French Ministry for Agriculture, Agrifood and Forestry (Decree 2013-118). Experimental protocols were reviewed by CEEA-122 Ethical Committee for Protection of Animals used for Scientific Purposes and approved by French Ministry for National Education, Higher Education and Research under the number CEEA-122 2014-19. Briefly, male C56Bl/6 J mice (8–10 weeks old, Charles River Laboratories, France) were anaesthetised with oxygen-isoflurane (0.2 L/min 1.5–2% isoflurane) and then maintained at 37 °C using a thermo-regulated system during surgery. A cutaneous incision was performed on the left flank, followed by a muscular incision. The left ureter was exposed, and ligated (6/0 silk). Then, the flank incision was sutured (muscle wall and the cutaneous wall) and disinfected with Vetadine® (Centravet, France). After surgery, the animals were returned to their cages. Food and water were given ad libitum. Commencing day 1 post-left ureter ligation, mice were administered vehicle control or SNT-8370 (60 mg/kg) via oral gavage twice a day, or Captopril (Sigma-Aldrich, 32 mg/kg) administered in their drinking water, which continued for the subsequent 13 days. At the end of the protocol (14 days after UUO), mice were weighed and then euthanized. The right and left kidneys were surgically removed, cleaned, rinsed in physiological saline, blotted dry, weighed and the length and thickness measured. The kidney/body weight ratio (mg/g) was then calculated as an index of kidney atrophy. Kidneys were then fixed in 10% formalin at room temperature for 24 h and then transferred in 70% ethanol until histological preparation. Fixed kidneys were embedded in paraffin blocks and two sections (3–5 μm) were stained with hematoxylin eosin or picrosirius red for histological evaluation of fibrosis (interstitial collagen accumulation expressed as a % of picrosirius red stained area per total kidney section surface). Stained tissue sections were imaged at 20× magnification using a Nanozoomer 2.0 HT (Hamamatsu, Japan) and analysed by Image J software.
Statistical analyses
Data are presented as mean ± SEM with the number of independent experiments or determinations indicated. Statistical comparisons were performed between two groups with a student’s t-test (two-tailed). Multiple groups were compared with a one-way ANOVA with a post hoc Tukey’s or Dunnett’s multiple comparisons test. Statistical significance was accepted for p < 0.05. Statistical analyses were performed using GraphPad Prism version 5 (GraphPad Software, La Jolla, CA).
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Data availability
The data sets generated and analysed as part of this study are available upon request from the corresponding authors. The source data for the main manuscript and supplementary information are provided as a Source Data file with this paper. Source data are provided with this paper.
References
Netea, M. G. et al. A guiding map for inflammation. Nat. Immunol. 18, 826–831 (2017).
Kotas, M. E. & Medzhitov, R. Homeostasis, inflammation, and disease susceptibility. Cell 160, 816–827 (2015).
Furman, D. et al. Chronic inflammation in the etiology of disease across the life span. Nat. Med. 25, 1822–1832 (2019).
McInnes, I. B. & Gravallese, E. M. Immune-mediated inflammatory disease therapeutics: past, present and future. Nat. Rev. Immunol. 21, 680–686 (2021).
Monteleone, G., Moscardelli, A., Colella, A., Marafini, I. & Salvatori, S. Immune-mediated inflammatory diseases: common and different pathogenic and clinical features. Autoimmun. Rev. 22, 103410 (2023).
Anighoro, A., Bajorath, J. & Rastelli, G. Polypharmacology: challenges and opportunities in drug discovery. J. Med. Chem. 57, 7874–7887 (2014).
Salmi, M. & Jalkanen, S. Vascular adhesion protein-1: a cell surface amine oxidase in translation. Antioxid. Redox Signal. 30, 314–332 (2019).
Li, H. et al. Vascular adhesion protein-1 (VAP-1)/semicarbazide-sensitive amine oxidase (SSAO): a potential therapeutic target for atherosclerotic cardiovascular diseases. Front. Pharm. 12, 679707 (2021).
Danielli, M., Thomas, R. C., Quinn, L. M. & Tan, B. K. Vascular adhesion protein-1 (VAP-1) in vascular inflammatory diseases. Vasa 51, 341–350 (2022).
de Zeeuw, D. et al. Efficacy of a novel inhibitor of vascular adhesion protein-1 in reducing albuminuria in patients with diabetic kidney disease (ALBUM): a randomised, placebo-controlled, phase 2 trial. Lancet Diabetes Endocrinol. 6, 925–933 (2018).
Newsome, P. N., BI 1467335 NASH Phase IIa trial team et al. A randomised Phase IIa trial of amine oxidase copper-containing 3 (AOC3) inhibitor BI 1467335 in adults with non-alcoholic steatohepatitis. Nat. Commun. 14, 7151 (2023).
Gasparella, F. et al. A novel MAO-B/SSAO inhibitor improves multiple aspects of dystrophic phenotype in mdx mice. Antioxidants 13, 622 (2024).
Nussbaum, C., Klinke, A., Adam, M., Baldus, S. & Sperandio, M. Myeloperoxidase: a leukocyte-derived protagonist of inflammation and cardiovascular disease. Antioxid. Redox Signal 18, 692–713 (2013).
Schultz, J. & Kaminker, K. Myeloperoxidase of the leucocyte of normal human blood. I. Content and localization. Arch. Biochem. Biophys. 96, 465–467 (1962).
Maiocchi, S. L. et al. Myeloperoxidase: a versatile mediator of endothelial dysfunction and therapeutic target during cardiovascular disease. Pharm. Ther. 221, 107711 (2021).
Davies, M. J. Myeloperoxidase: mechanisms, reactions and inhibition as a therapeutic strategy in inflammatory diseases. Pharm. Ther. 218, 107685 (2021).
Klebanoff, S. J., Kettle, A. J., Rosen, H., Winterbourn, C. C. & Nauseef, W. M. Myeloperoxidase: a front-line defender against phagocytosed microorganisms. J. Leukoc. Biol. 93, 185–198 (2013).
Michaelsson, E. et al. Myeloperoxidase inhibition reverses biomarker profiles associated with clinical outcomes in HFpEF. JACC Heart Fail 11, 775–787 (2023).
Lund, L. H. et al. Rationale and design of ENDEAVOR: a sequential phase 2b-3 randomized clinical trial to evaluate the effect of myeloperoxidase inhibition on symptoms and exercise capacity in heart failure with preserved or mildly reduced ejection fraction. Eur. J. Heart Fail 25, 1696–1707 (2023).
A Study in Participants With Non-cirrhotic NASH With Fibrosis. https://classic.clinicaltrials.gov/show/NCT05638737.
An Efficacy and Safety Study of Mitiperstat (AZD4831) (MPO Inhibitor) vs Placebo in the Treatment of Moderate to Severe COPD. https://classic.clinicaltrials.gov/show/NCT05492877.
Ruggeri, R. B. et al. Discovery of 2-(6-(5-Chloro-2-methoxyphenyl)-4-oxo-2-thioxo-3,4-dihydropyrimidin-1(2H)-yl)acet amide (PF-06282999): a highly selective mechanism-based myeloperoxidase inhibitor for the treatment of cardiovascular diseases. J. Med. Chem. 58, 8513–8528 (2015).
Johnstrom, P. et al. Development of rapid multistep carbon-11 radiosynthesis of the myeloperoxidase inhibitor AZD3241 to assess brain exposure by PET microdosing. Nucl. Med. Biol. 42, 555–560 (2015).
Jucaite, A. et al. Effect of the myeloperoxidase inhibitor AZD3241 on microglia: a PET study in Parkinson’s disease. Brain 138, 2687–2700 (2015).
Nicholls, S. J. & Hazen, S. L. Myeloperoxidase, modified lipoproteins, and atherogenesis. J. Lipid Res. 50, S346–S351 (2009).
Podrez, E. A. et al. Macrophage scavenger receptor CD36 is the major receptor for LDL modified by monocyte-generated reactive nitrogen species. J. Clin. Investig. 105, 1095–1108 (2000).
Podrez, E. A., Schmitt, D., Hoff, H. F. & Hazen, S. L. Myeloperoxidase-generated reactive nitrogen species convert LDL into an atherogenic form in vitro. J. Clin. Investig. 103, 1547–1560 (1999).
Tiden, A. K. et al. 2-thioxanthines are mechanism-based inactivators of myeloperoxidase that block oxidative stress during inflammation. J. Biol. Chem. 286, 37578–37589 (2011).
Ward, J. et al. Mechanistic characterization of a 2-thioxanthine myeloperoxidase inhibitor and selectivity assessment utilizing click chemistry–activity-based protein profiling. Biochemistry 52, 9187–9201 (2013).
Foot, J. S. et al. PXS-4681A, a potent and selective mechanism-based inhibitor of SSAO/VAP-1 with anti-inflammatory effects in vivo. J. Pharm. Exp. Ther. 347, 365–374 (2013).
Bligt-Linden, E. et al. Novel pyridazinone inhibitors for vascular adhesion protein-1 (VAP-1): old target-new inhibition mode. J. Med. Chem. 56, 9837–9848 (2013).
Findlay, A. D. et al. Identification and optimization of mechanism-based fluoroallylamine inhibitors of lysyl oxidase-like 2/3. J. Med. Chem. 62, 9874–9889 (2019).
Shaw, S. A. et al. Discovery and structure activity relationships of 7-benzyl triazolopyridines as stable, selective, and reversible inhibitors of myeloperoxidase. Bioorg. Med. Chem. 28, 115723 (2020).
Davies, M. J., Hawkins, C. L., Pattison, D. I. & Rees, M. D. Mammalian heme peroxidases: from molecular mechanisms to health implications. Antioxid. Redox Signal. 10, 1199–1234 (2008).
Arnhold J. & Malle E. Halogenation activity of mammalian heme peroxidases. Antioxidants 11, 890 (2022).
Bhave, G. et al. Peroxidasin forms sulfilimine chemical bonds using hypohalous acids in tissue genesis. Nat. Chem. Biol. 8, 784–790 (2012).
Cheng, G. & Shi, R. Mammalian peroxidasin (PXDN): from physiology to pathology. Free Radic. Biol. Med. 182, 100–107 (2022).
Schwelberger, H. G. The origin of mammalian plasma amine oxidases. J. Neural Transm. 114, 757–762 (2007).
Goiffon, R. J., Martinez, S. C. & Piwnica-Worms, D. A rapid bioluminescence assay for measuring myeloperoxidase activity in human plasma. Nat. Commun. 6, 6271 (2015).
Jarnicki, A. G. et al. The inhibitor of semicarbazide-sensitive amine oxidase, PXS-4728A, ameliorates key features of chronic obstructive pulmonary disease in a mouse model. Br. J. Pharm. 173, 3161–3175 (2016).
Schilter, H. C. et al. Effects of an anti-inflammatory VAP-1/SSAO inhibitor, PXS-4728A, on pulmonary neutrophil migration. Respir. Res. 16, 42 (2015).
Noonan, T. et al. The oxidase activity of vascular adhesion protein-1 (VAP-1) is essential for function. Am. J. Clin. Exp. Immunol. 2, 172–185 (2013).
Duarte D. B., Vasko M. R. & Fehrenbacher J. C. Models of inflammation: carrageenan air pouch. Curr Protoc Pharmacol Chapter 5, Unit5 6 (2012).
Swirski, F. K. & Nahrendorf, M. Cardioimmunology: the immune system in cardiac homeostasis and disease. Nat. Rev. Immunol. 18, 733–744 (2018).
Frangogiannis, N. G. The inflammatory response in myocardial injury, repair, and remodelling. Nat. Rev. Cardiol. 11, 255–265 (2014).
Schanstra, J. P. et al. In vivo bradykinin B2 receptor activation reduces renal fibrosis. J. Clin. Investig. 110, 371–379 (2002).
Binder, C. J., Papac-Milicevic, N. & Witztum, J. L. Innate sensing of oxidation-specific epitopes in health and disease. Nat. Rev. Immunol. 16, 485–497 (2016).
Lugrin, J., Rosenblatt-Velin, N., Parapanov, R. & Liaudet, L. The role of oxidative stress during inflammatory processes. Biol. Chem. 395, 203–230 (2014).
Stocker, R. & Keaney, J. F. Jr. Role of oxidative modifications in atherosclerosis. Physiol. Rev. 84, 1381–1478 (2004).
Bowes, J. et al. Reducing safety-related drug attrition: the use of in vitro pharmacological profiling. Nat. Rev. Drug Discov. 11, 909–922 (2012).
Thummel, K. E. & Wilkinson, G. R. In vitro and in vivo drug interactions involving human CYP3A. Annu. Rev. Pharm. Toxicol. 38, 389–430 (1998).
Cantrill, C. et al. Fundamental aspects of DMPK optimization of targeted protein degraders. Drug Discov. Today 25, 969–982 (2020).
Sakaeda, T. et al. Molecular and pharmacokinetic properties of 222 commercially available oral drugs in humans. Biol. Pharm. Bull. 24, 935–940 (2001).
Rehring, J. F. et al. Released myeloperoxidase attenuates neutrophil migration and accumulation in inflamed tissue. Front. Immunol. 12, 654259 (2021).
Haegens, A. et al. Myeloperoxidase deficiency attenuates lipopolysaccharide-induced acute lung inflammation and subsequent cytokine and chemokine production. J. Immunol. 182, 7990–7996 (2009).
Florez-Barros, F. et al. Myeloid expression of the anti-apoptotic protein Mcl1 is required in anti-myeloperoxidase vasculitis but myeloperoxidase inhibition is not protective. Kidney Int. 103, 134–143 (2023).
Holt, A. & Palcic, M. M. A peroxidase-coupled continuous absorbance plate-reader assay for flavin monoamine oxidases, copper-containing amine oxidases and related enzymes. Nat. Protoc. 1, 2498–2505 (2006).
Maiocchi, S. L., Morris, J. C., Rees, M. D. & Thomas, S. R. Regulation of the nitric oxide oxidase activity of myeloperoxidase by pharmacological agents. Biochem. Pharm. 135, 90–115 (2017).
Dypbukt, J. M. et al. A sensitive and selective assay for chloramine production by myeloperoxidase. Free Radic. Biol. Med. 39, 1468–1477 (2005).
Maiocchi, S. et al. Polyamine-conjugated nitroxides are efficacious inhibitors of oxidative reactions catalyzed by endothelial-localized myeloperoxidase. Chem. Res. Toxicol. 34, 1681–1692 (2021).
Sattler, W., Mohr, D. & Stocker, R. Rapid isolation of lipoproteins and assessment of their peroxidation by high-performance liquid chromatography postcolumn chemiluminescence. Methods Enzymol. 233, 469–489 (1994).
Thomas, S. R., Neuzil, J. & Stocker, R. Cosupplementation with coenzyme Q prevents the prooxidant effect of alpha-tocopherol and increases the resistance of LDL to transition metal-dependent oxidation initiation. Arterioscler Thromb. Vasc. Biol. 16, 687–696 (1996).
Thomas, S. R., Davies, M. J. & Stocker, R. Oxidation and antioxidation of human low-density lipoprotein and plasma exposed to 3-morpholinosydnonimine and reagent peroxynitrite. Chem. Res Toxicol. 11, 484–494 (1998).
Witting, P. K., Mohr, D. & Stocker, R. Assessment of prooxidant activity of vitamin E in human low-density lipoprotein and plasma. Methods Enzymol. 299, 362–375 (1999).
van Dalen, C. J. & Kettle, A. J. Substrates and products of eosinophil peroxidase. Biochem. J. 358, 233–239 (2001).
Chesney, J. A., Mahoney, J. R. Jr & Eaton, J. W. A spectrophotometric assay for chlorine-containing compounds. Anal. Biochem. 196, 262–266 (1991).
Paumann-Page, M. et al. Pre-steady-state kinetics reveal the substrate specificity and mechanism of halide oxidation of truncated human peroxidasin 1. J. Biol. Chem. 292, 4583–4592 (2017).
Fujimura, H. et al. Cell-based fluorescence assay for evaluation of new-drugs potential for phospholipidosis in an early stage of drug development. Exp. Toxicol. Pathol. 58, 375–382 (2007).
Delano, D. L., Montesinos, M. C., D’Eustachio, P., Wiltshire, T. & Cronstein, B. N. An interaction between genetic factors and gender determines the magnitude of the inflammatory response in the mouse air pouch model of acute inflammation. Inflammation 29, 1–7 (2005).
Mosca, L., Barrett-Connor, E. & Wenger, N. K. Sex/gender differences in cardiovascular disease prevention: what a difference a decade makes. Circulation 124, 2145–2154 (2011).
Yao Y. et al. Pan-lysyl oxidase inhibitor PXS-5505 ameliorates multiple-organ fibrosis by inhibiting collagen crosslinks in rodent models of systemic sclerosis. Int. J. Mol. Sci. 23, 5533 (2022).
Acknowledgements
This research was carried out as a collaborative venture between UNSW and Syntara Ltd. The authors would like to thank Sally Vuong for technical assistance in the performance of the myocardial infarction model and employees of Syntara Ltd., past and present, for contributions towards in house assays and the synthesis of compounds.
Author information
Authors and Affiliations
Contributions
E.G., J.F., W.J. and S.R.T. contributed to the experimental design/performance, data analysis and interpretation and manuscript writing. B.R. and Y.Z. designed and executed the myocardial infarction studies. H.S. and M.M.T. designed and executed the acute lung injury studies. M.P.P. provided human recombinant peroxidasin (PDXN) and measured IC50 values for SNT-8370. All authors have reviewed and approved the manuscript.
Corresponding authors
Ethics declarations
Competing interests
This study was partly funded by research support of Syntara Limited, Australia (formerly Pharmaxis Limited) to UNSW (S.R.T., E.G.), UFMG (M.M.T.), Heart Research Institute (B.R.) and the University of Otago (M.P.P.). Throughout the course of the work, J.F., H.S. and W.J. were employed by Syntara Limited, and held shares in the company. The remaining authors declare no competing interests.
Peer review
Peer review information
Nature Communications thanks the anonymous reviewer(s) for their contribution to the peer review of this work. A peer review file is available.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Source data
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Glaros, E., Foot, J., Rayner, B. et al. Targeting vascular adhesion protein-1 and myeloperoxidase with a dual inhibitor SNT-8370 in preclinical models of inflammatory disease. Nat Commun 16, 3430 (2025). https://doi.org/10.1038/s41467-025-58454-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41467-025-58454-6
This article is cited by
-
Reversible Myeloperoxidase Inhibition by Benzodioxole Carboxamides: Insights from In Silico and InVitro Studies
Cell Biochemistry and Biophysics (2025)