Abstract
Myocardial ischemia-reperfusion injury (MIRI) is a life-threatening complication of myocardial infarcts, with inner mitochondrial membrane protein dysfunction involved in MIRI-induced heart injury. The role of outer mitochondrial membrane protein mitochondrial antiviral signaling protein (MAVS) is unknown. Here, we show that MAVS expression increases in infarcted myocardium of male wild-type mice. Global MAVS-knock-out or myocardial-specific MAVS knockdown protects male mice from acute and chronic MIRI. MIRI induces double-stranded RNA in affected myocardium, activating intracellular retinoic acid-inducible gene I (RIG-I) signaling, which leads to MAVS aggregation and subsequent non-canonical downstream signaling. MAVS aggregates recruit tumor necrosis factor-associated factor family 6 (TRAF6) and transforming growth factor-β-activated kinase 1 (TAK1), the activating mitogen-activated protein kinase (MAPK) pathway and apoptosis. MAVS-knock-out reduces c-jun-NH2 terminal kinase (JNK) phosphorylation and apoptosis. JNK inhibition protects against MIRI in wild-type male mice, whereas JNK agonist impairs protection in MAVS-knock-out male mice. MIRI activates RIG-I/MAVS pathway and subsequently triggers the TAK1/TRAF6 complex, leading to the activation of the MAPK/JNK signaling cascade. This sequential activation cascade may serve as a potential therapeutic target for MIRI.
Similar content being viewed by others
Introduction
Acute myocardial flow restriction caused by coronary artery occlusion triggers myocardial infarction. Timely reperfusion of occluded arteries can improve systolic function, reduce ventricular fibrillation, and the survival rate of patients during the acute post-myocardial infarction period as well as during long-term time windows1,2,3. However, acute therapeutic intervention leading to reperfusion of the occluded artery segment may cause myocardial injury, i.e., myocardial ischemia-reperfusion injury (MIRI), which often results in acute life-threatening complications, including ventricular fibrillation resulting in sudden death, infiltration of inflammatory cells due to cell necrosis, and late adverse ventricular remodeling, such as fibrosis and angiogenesis4,5,6. Indeed, 25–40% of deaths subsequent to a myocardial infarct are believed to be associated with MIRI. MIRI is largely due to mitochondrial damage of myocardial cells in the infarct and peri-infarct myocardium7,8. Mitochondria are the main source of adenosine triphosphate in cardiac cells and regulate a wide variety of cellular functions9. They also play an important role in innate immune signaling pathways to control injurious impacts of exogenous agents10,11,12. It is well established that mitochondrial membrane proteins participate in major mitochondrial functions13. However, while the role of the inner mitochondrial membrane during oxidative respiration is well understood during MIRI, the outer mitochondrial membrane proteins have received less attention14.
The mitochondrial antiviral signaling protein (MAVS) is a major constituent of the outer mitochondrial membrane15. MAVS consists of an N-terminal cysteinyl aspartate-specific proteinase recruitment domain, a proline-rich region preceding a poorly structured middle segment, and a monotopic transmembrane domain at the C-terminus16. As a key signaling protein activated by viral RNA sensors such as melanoma differentiation-associated protein 5 and retinoic acid-inducible gene I (RIG-I), MAVS promotes the expression of interferon-stimulating genes and inflammatory cytokines through nuclear factor kappa-B and interferon regulatory factor 3 to participate in immune responses against viral infections17,18,19. In this signaling cascade, RIG-I is first activated by both RNA and polyubiquitin chains linked through lysine-63 residues of ubiquitin20. Then, MAVS binds to the conformationally altered RIG-I via its cysteinyl aspartate specific proteinase recruitment domain forming prion-like filaments on the outer mitochondrial membrane through lysine-63 residues-linked polyubiquitination, which constitutes a critical event of MAVS activation20,21,22,23. Moreover, the middle proline-rich region domain of MAVS can bind several members of the tumor necrosis factor-associated factor family including tumor necrosis factor associated-factor family 2, tumor necrosis factor-associated factor family 3, tumor necrosis factor associated-factor family 5 and tumor necrosis factor-associated factor family 6 to promote downstream signaling24,25. Among them, tumor necrosis factor associated-factor family 6 has been associated with target cell apoptosis after virus infection26. Besides being expressed in immune cells, MAVS is ubiquitously expressed in multiple mesenchymal cells. Studies of the cardiovascular system have shown that nucleotide-binding oligomerization domain protein 1/ receptor-interacting protein kinase 2 signaling is critically involved in MAVS activity during cardiac hypertrophy27 and MAVS deletion contributed to the pathogenesis of non-hypertrophic cardiac dysfunction in aged mice28. However, the role of MAVS in MIRI remains unknown.
The mitogen-activated protein kinase family plays important and diverse roles in signal transduction during heart development, physiological adaptation and pathological conditions29,30. Mitogen-activated protein kinases constitute four subfamilies including extracellular signal-regulated kinases (extracellular signal-regulated protein kinases 1, −2), p38-mitogen-activated protein kinases, the big mitogen-activated protein kinase and c-jun-NH2 terminal kinases (JNK1, 2, and 3)31,32. Being a stress-activated protein kinase, JNK can be activated by mitogen-activated protein kinase kinase kinases in response to inflammatory cytokines and cellular stress following MIRI, DNA damage, and endoplasmic reticulum perturbation32,33. Moreover, transforming growth factor-β-activated kinase 1, encoded by the Map3k7 gene, can regulate cardiomyocyte necrosis and affect ventricular remodeling in cardiac overload in mice and during clinically significant stages of atherosclerosis. However, transforming growth factor-β-activated kinase 1’s involvement in MIRI remains to be determined34.
Here, we observed that MIRI triggers RIG-I resulting in stimulation of MAVS-regulated myocardial mitogen-activated protein kinase/JNK signaling via the transforming growth factor-β-activated kinase 1/tumor necrosis factor-associated factor family 6 axis at the outer mitochondrial membrane. The MIRI-RIG-I signaling cascade exacerbates the extent of MIRI-triggered injury. Here, we provide a comprehensive mechanistic studies of the RIG-I/MAVS/JNK cascade during MIRI using genetic and pharmacological approaches in vitro and a wide variety of in vivo models. Our data reveal that signaling molecules of the RIG-I cascade are activated during myocardial injury and may qualify as potential novel therapeutic targets to interfere the immediate, clinically significant period after myocardial infarction.
Results
Global MAVS deficiency in male mice protects the heart against MIRI
To study the role of MAVS in MIRI, we first examined hearts of male WT mice by western blot analyses. MIRI was induced in WT mice by coronary artery ligation for 30 min followed by reperfusion for 6 h. We observed that protein levels of MAVS were elevated in both the area at risk and in the infarcted areas when compared to the remote area or sham mice (Fig. 1a, b). MAVS expression also increased in the murine cardiomyocyte HL-1 cell line in vitro following hypoxia-reoxygenation (Supplementary Fig. 1a), with more pronounced increases in mitochondria preparations (Fig. 1c, d). This data showed that MAVS protein expression was up-regulated in mitochondria under hypoxia-reoxygenation conditions in vivo and in vitro. To further explore the roles of MAVS in MIRI, global MAVS knockout (MAVS-KO) mice were generated (Supplementary Fig. 1b). Examining hearts male vs female MAVS-KO mice no significant gender-related differences as determined by several parameters using cardiac ultrasound, myocardial enzyme release and infarct sizes were observed (Supplementary Fig. 1c–g). Male mice were used for future studies.
a MAVS expression in remote area, area at risk and infarct area of WT hearts in sham vs 6-hour reperfusion mice. b Statistical analyses in (a). c MAVS expression in mitochondrial preparations of HL-1 cells after 6 h hypoxia and 8 h reoxygenation, with mitochondrial cytochrome coxidase IV (COX-IV) as the mitochondrial internal reference. d Statistical analyses in (c). e Echocardiography of WT vs MAVS-KO mice at 6 h reperfusion. Yellow line shows the left ventricle anterior and posterior wall position, white double-tailed arrow shows the inside diameter. LVIDS is left ventricular internal diameter at end systole, LVIDD at end diastole. Scale bar, 1 mm. f Cardiac contractility parameters of WT vs MAVS-KO mice at 6 h of reperfusion. Left ventricular ejection fraction (LVEF), left ventricular fraction shortening (LVFS), left ventricular end-systolic volume (LVESV), left ventricular end-diastolic volume (LVEDV). n = 10. g 2, 3, 5-triphenyltetrazolium chloride + Evans blue staining of WT vs MAVS-KO mice at 1 day of reperfusion. Scale bar, 2 mm. h Infarct volume ratio from staining in (g). n = 8. i Pathophysiological characteristics by hematoxylin-eosin staining in WT vs MAVS - KO mice at 3 days reperfusion. Black line shows the infarct area. Scale bar, 1 mm. j Infarct size quantification in i. n = 5. k Ultrastructure of heart infarct area in WT vs MAVS-KO mice at 6 h reperfusion by transmission electron microscopy. Red arrows indicate damaged mitochondria. Scale bar, 500 nm. l Fold change of damaged mitochondria in k. n = 8. m Terminal deoxynucleotidyl transferase-mediated 2’-deoxyuridine 5’-triphosphate nick end labeling (TUNEL) staining in WT vs MAVS-KO heart sections at 6 h after reperfusion. Wheat germ agglutinin (WGA) stains cardiomyocytes. Scale bar, 50 μm. n Apoptotic cell quantification in (m). n = 5 mice. o Serum cardiac enzymes levels at 6 h reperfusion or sham. n = 5 mice. b, d Data from 3 independent samples are presented as means ± SD. Statistical tests used: unpaired 2-tailed Student t test for (d, h, j, l, n); one-way ANOVA with Tukey’s test for (b, f, o). Significance levels: *p < 0.05, **p < 0.01, ***p < 0.001, ****p < 0.0001, ns (p ≥ 0.05). Source data are in the Source Data file.
Next, heart phenotypes of WT versus MAVS-KO mice were evaluated. Echocardiography (Fig. 1e) was performed to determine myocardial contractility in untreated mice (sham mice) or mice subjected to ischemia reperfusion. In MAVS-KO sham vs WT sham mice, no difference in myocardial contractility was observed (Fig. 1e). However, MAVS-KO mice which underwent ischemia reperfusion showed markedly improved cardiac contractility versus WT controls as determined by multiple echocardiographic parameters: increased left ventricular ejection fraction and left ventricular fraction shortening, and decreased left ventricular end-diastolic volume as well as left ventricular end-systolic volume (Fig. 1f). This data revealed a significant role of MAVS to regulate heart contractility in mice (Fig. 1e, f). Next, to assess longer term consequences, MIRI was induced in WT and MAVS-KO mice by coronary artery ligation for 30 min followed by reperfusion for 24 h or 3 days. MAVS-KO mice showed significantly reduced cardiac infarct sizes at 24 h post-reperfusion (Fig. 1g, h) as well as at 3 days after reperfusion (Fig. 1i, j) vs WT mice. Moreover, MAVS-KO mice showed significantly decreased burdens of CD45 leukocyte infiltration in infarcted areas and area at risk areas vs their controls (Supplementary Fig. 1h). Next, transmission electron microscopy was used to examine cardiomyocytes at the subcellular level including mitochondrial integrity at 6 h post-reperfusion. Significant swelling, rupture, and collapse of mitochondrial cristae was observed in WT mice but to a lesser extent in MAVS-KO mice (Fig. 1k, l). In addition, terminal deoxynucleotidyl transferase-mediated 2’-deoxyuridine 5’-triphosphate nick end labeling staining showed that the number of apoptotic cells in the injured myocardium was significantly reduced in MAVS-KO mice vs controls (Fig. 1m, n). Other myocardium-specific parameters of MIRI were also significantly affected as shown by elevation of myocardial enzyme levels in the circulation including cardiac troponin I, creatine kinase, creatine kinase isoenzyme and α-hydroxybutyrate dehydrogenase in WT mice, while MAVS-KO showed markedly attenuated levels (Fig. 1o). These results showed that MAVS deficiency protects the heart against acute MIRI in mice.
Myocardium-specific MAVS knockdown in male mice alleviates heart injury in MIRI
MAVS is expressed in multiple mesenchymal cells and immune cells. To detail the role of myocardium-specific MAVS in MIRI, we isolated primary cardiomyocytes and non-cardiomyocytes from adult hearts that had been reperfused for 6 h and then determined MAVS expression in both heart cell subtypes in male WT mice (Supplementary Fig. 2a, b). This data showed that MAVS expression was largely but not exclusively expressed by cardiomyocytes and its levels increased significantly in both cardiomyocytes and non-cardiomyocytes.
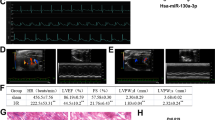
Next, we isolated immune and non-immune cells in adult male WT mice to determine MAVS levels in leukocytes that may participate in MIRI (Supplementary Fig. 2c). Surprisingly, we found that the increase of MAVS was striking in non-immune cells but that MAVS protein expression in immune cells indeed decreased during MIRI (Supplementary Fig. 2d–g). This data raised the important question regarding the interpretation of the global MAVS KO phenotype in the myocardium versus heart immune cells during MIRI (shown in Fig. 1). To specifically address this issue, we generated myocardium-specific MAVS knockdown male mice using adeno-associated virus serotype 9 transfer short hairpin RNA with a cardiomyocyte-specific promoter targeting MAVS and mice with negative control short hairpin RNA knockdown vector. Myocardium-specific short hairpin RNA knockdown of MAVS protein was first confirmed by both immunofluorescent staining and western blot (Supplementary Fig. 2h–j). Similar to the phenotype of global MAVS-KO male mice (Fig. 1 above), MAVS knockdown mice showed improved cardiac functions when compared to the negative control short hairpin RNA knockdown mice as analyzed by increased left ventricular ejection fraction and left ventricular fractional shortening, and decreased left ventricular end-diastolic volume and left ventricular end-systolic volume (Fig. 2a, b). Furthermore, specific knockdown of MAVS in cardiomyocytes effectively reduced the infarct size (Fig. 2c, d, Supplementary Fig. 2k). Moreover, MAVS-sh mice also displayed reduced immune cell infiltration compared to control hearts at day 3 (Supplementary Fig. 2l). Furthermore, the number of apoptotic cells was significantly reduced in the myocardium of MAVS knockdown mice at day 3 (Fig. 2f, g). In addition, quantitative transmission electron microscopy analyses revealed that MAVS knockdown mice showed markedly reduced damage of mitochondria membranes (Fig. 2h, i). Moreover, the levels of myocardial enzymes, i.e., cardiac troponin I, creatine kinase, creatine kinase isoenzyme and α-hydroxybutyrate in sera and reactive oxygen species of MAVS knockdown mice were significantly reduced when compared to those of the control mice (Fig. 2j, k). Thus, this data demonstrated that MAVS expressed by the cardiomyocytes rather than MAVS expressed by extramyocardial cells mediated the protection against multiple types of injury in response to MIRI.
a Echocardiography of MAVS knockdown (MAVS-sh) and negative control knockdown (NC-sh) mice at 6 h reperfusion. Yellow line shows the left ventricle anterior and posterior wall position, white double-tailed arrow shows the inside diameter. LVIDS, Left ventricular internal diameter end systole; LVIDD, Left ventricular internal diameter end diastole. Scale bar, 1 mm. b Cardiac left ventricular ejection fraction (LVEF), left ventricular fraction shortening (LVFS), left ventricular end-systolic volume (LVESV) and left ventricular end-diastolic volume (LVEDV) in MAVS-sh and NC-sh mice at 6 h reperfusion or sham. n = 10 mice per group. c Infarct volume in left ventricle based on 2, 3, 5-triphenyltetrazolium chloride + evans blue staining. n = 7 mice per group. d Pathophysiological features by hematoxylin-eosin staining in MAVS-sh mice and NC-sh mice at 3 days reperfusion. The black line shows the infarct area. Scale bar, 1 mm. e Infarct sizes quantification in (d). n = 7. Data are shown with 7 biologically independent samples. f Terminal deoxynucleotidyl transferase-mediated 2’-deoxyuridine 5’-triphosphate nick end labeling (TUNEL) staining in heart sections of MAVS-sh and NC-sh mice at 3 days reperfusion. Scale bar, 50 μm. g Apoptotic cell percentage in intact 4’,6-diamidino-2-phenylindole (DAPI) positive cells in (f). n = 5 mice. h Ultrastructure of infarct area at 6 h reperfusion by transmission electron microscope. Red arrows indicate damaged mitochondria. Scale bar, 500 nm. i Damaged mitochondria percentage quantified in MAVS-sh and NC-sh mice. n = 10 mice in each group. j Cardiac enzymes detection in the serum at 6 h reperfusion or sham. n = 5 mice. k Reactive oxygen species in cardiac tissue at 6 h reperfusion or sham. n = 5 mice. Data are means ± standard deviation; statistical analyses were conducted by unpaired 2-tailed Student t test (c, e, g, i) and one-way analysis of variance with Tukey’s multiple comparisons test (b, j, k); *p < 0.05, **p < 0.01, ***p < 0.001; ****p < 0.0001, ns, p ≥ 0.05. Source data are provided as a Source Data file.
Myocardial MAVS aggravates cardiac function in male mice at two weeks following induction of MIRI
To study the role of myocardial MAVS on cardiac function at the stage of subacute myocardial healing and scar formation after initiation of MIRI in male mice, we examined myocardial tissue at day 14 after reperfusion. There was no significant difference in heart to body weight ratio between MAVS knockdown mice and WT mice in the sham group, while an increased ratio was observed in WT mice compare to the MAVS knockdown mice in the ischemia-reperfusion group (Fig. 3a). At 2 weeks, we noticed that MAVS knockdown specifically in cardiomyocytes reduced the MIRI-induced enlargement of cardiomyocytes when compared to the WT mice (Fig. 3b, c). Angiogenesis is an important index of cardiac function recovery. Angiogenesis was apparent at different time points after reperfusion in WT mice. This data indicated that newly formed smaller-sized blood vessels appeared at day 7 and increased thereafter within 2 weeks. In addition, somewhat larger-sized blood vessels appeared after 28 days (Supplementary Fig. 3a). Of note, MAVS knockdown mice showed improvement in multiple cardiac function parameters including attenuated fibrosis and increased angiogenesis (Fig. 3d–i). We also examined the myocardial pathology phenotype at day 14 after reperfusion in MAVS-KO mice. These mice showed similar protection such as significantly lower heart/body weight ratios, and reduced cardiomyocyte hypertrophy (Supplementary Fig. 3b, c). Likewise, MAVS-KO mice showed improved cardiac functions (Supplementary Fig. 3d, e), less pronounced myocardial fibrosis and increased angiogenesis at 14 days (Supplementary Fig. 3f, g) when compared to WT control hearts. This data revealed that both MAVS knockdown mice and MAVS-KO mice showed markedly attenuated myocardial injury at late stages of MIRI, providing evidence that MAVS of the myocardium specifically has a detrimental role in MIRI.
a Comparison of heart weight to body weight ratio at 14 days reperfusion in MAVS knockdown (MAVS-sh) mice and control mice (NC-sh). n = 5. b Wheat germ agglutinin staining of cardiac myocytes. Scale bar, 50 μm. c Cardiomyocyte size measured in myocardial tissue sections. n = 20 cells/group. d Echocardiography of MAVS-sh and NC-sh mice at day 14 after reperfusion. Yellow line shows left ventricle wall positions, white double-tailed arrow represents the inner diameter. LVIDS, Left ventricular internal diameter end systole; LVIDD, Left ventricular internal diameter end diastole. Scale bar, 1 mm. e Left ventricular ejection fraction (LVEF), left ventricular fraction shortening (LVFS), left ventricular end-systolic volume (LVESV) and left ventricular end-diastolic volume (LVEDV) were assayed to determine cardiac function in MAVS-sh and NC-sh mice at day 14 after reperfusion or sham. n = 5. f Fibrosis of heart tissue sections at day 14 after reperfusion. Pathological parameters are shown in remote area, area at risk and infarct area. Scale bar, 1 mm (panoramic), 50 μm (enlarged). g Fibrosis proportion in infarct area in f was calculated. n = 8. h Immunofluorescence staining of endothelial cell marker CD31 in cardiac tissues at day 14 after reperfusion. Scale bar, 20 μm. i Blood vessels number in high power fields was counted according to the staining results in (h). n = 8. Data are presented as means ± standard deviation; *p < 0.05, **p < 0.01, ***p < 0.001, ****p < 0.0001 by one-way analysis of variance with Tukey’s multiple comparisons test (a, c, e); *p < 0.05, ***p < 0.001 by unpaired 2-tailed Student t test (g, i); ns, p ≥ 0.05. Source data are provided as a Source Data file.
MAVS mediates cardiomyocyte death during hypoxic injury in vitro
Our data revealed that knockout of MAVS reduces myocardial ischemia and apoptosis in vivo (Fig. 1). To gain mechanistic insight into the role of MAVS during MIRI, we used lentiviral infection to construct a myocardial cell line, i.e., HL-1 cells, with either MAVS overexpression or MAVS-knockdown. We first verified the expression of MAVS in all of the edited HL-1 cell lines we had generated by western blot (Supplementary Fig. 4a, b). HL-1 cells with MAVS overexpression showed significantly increased early and late apoptosis under hypoxia-reoxygenation conditions compared with those in negative control with overexpressing vector (6.83% vs 3.92%; 6.59% vs 3.32%), while HL-1 cells with MAVS knockdown demonstrated decreased apoptosis compared with negative control knockdown cells (1.92% vs 3.55%) (Supplementary Fig. 4c, d). In the normoxic state, HL-1 cells with MAVS knockdown showed a tendency of relatively low numbers of early stage of apoptotic cells, however, without statistical difference, while there was no difference in late stage of apoptosis (Supplementary Fig. 4d). Since mitochondrial membrane potential is a critical parameter involved in mitochondrial function, the mito tracker tetramethylrhodamine ethyl ester was used to evaluate mitochondrial membrane potential. Under normoxic conditions, mitochondrial membrane potential was maintained at relatively high levels, though MAVS knockdown cells showed higher mitochondrial membrane potential values compared to MAVS overexpression cells or control cells (Supplementary Fig. 4e, f). Under hypoxia-reoxygenation conditions, mitochondrial membrane potential levels were markedly reduced when compared to normoxia, while the change of mitochondrial membrane potential reduction in MAVS knockdown cells was attenuated (Supplementary Fig. 4e, f) indicating protection from MAVS-triggered mitochondrial injury under hypoxia-reoxygenation conditions. Glutathione acts as an enzyme-catalyzed antioxidant in oxidative tissue injury35. Under hypoxia-reoxygenation, glutathione levels significantly decreased in MAVS overexpression cells compared to negative control with overexpressing vector cells, while the decline was significantly reduced in the MAVS knockdown cells compared to negative control short hairpin RNA knockdown cells (Supplementary Fig. 4g). Moreover, the level of glutathione in MAVS overexpression cells decreased significantly under hypoxia-reoxygenation conditions compared with that in normoxia, while that glutathione levels in the MAVS knockdown group was not significantly down-regulated in hypoxia-reoxygenation (Supplementary Fig. 4g). These results revealed that deletion of MAVS protects cardiomyocytes from a series of detrimental effects under hypoxia-reoxygenation conditions in vitro.
Endogenous host RNA in MIRI initiate the RIG-I/MAVS pathway in cardiomyocytes in mice
To define the MAVS-activated signaling pathway during MIRI in more detail, we collected infarcted myocardial tissue from mice at 6 h after reperfusion and myocardial tissue from the sham group, and then prepared cardiac tissue lysates for proteomic sequencing. According to Kyoto encyclopedia of genes and genomes analyses, the mitogen-activated protein kinase and RIG-I signaling pathways were enriched in the MIRI hearts vs their sham counterparts, and that oxidative phosphorylation and carbon metabolism also participated in MIRI (Supplementary Fig. 5a). We next used MAVS as a bait in vitro to pull down candidate binding proteins, and analyzed the captured proteins by mass spectrometry from cardiac tissue lysates prepared at 6 h after reperfusion or sham. 1936 proteins were captured in the sham group and 1887 proteins were captured in the MIRI group (Supplementary Fig. 5b). 1559 proteins were identical between the two groups and 328 proteins were differentially expressed in infarcted tissue (Supplementary Fig. 5b). Kyoto encyclopedia of genes and genomes analyses showed that the mitogen-activated protein kinase signaling pathways were enriched within the differentially regulated 328 proteins in MIRI-burdened hearts (Supplementary Fig 5c). Among these proteins, we modeled the protein network that potentially interacts with MAVS using the STRING software (Supplementary material: https://cn.string-db.org/). Mitogen-activated protein kinase kinase kinase 7 (MAP3K7/TAK1) and retinoic acid-inducible gene I (Ddx58/RIG-I) proteins showed the strongest interaction with MAVS (Supplementary Fig. 5d). Previous studies had shown that MAVS can interact with nucleotide-binding oligomerization domain protein 1 (NOD1) and receptor-interacting protein kinase 2 (RIPK2) in failing hearts27 and that melanoma differentiation-associated gene 5 (MDA5) was one of the intracellular sensors that can activate MAVS in virus-infected tissues18 and that the cysteinyl aspartate specific proteinase activation and recruitment domain of RIG-I binds to MAVS to trigger downstream signal transduction21,25. To gain further information on these events during MIRI, we first examined molecules that may be involved in activating MAVS during MIRI in both WT and MAVS-KO mice at the transcriptional level. The results showed that MAVS knockout did not affect MIRI-induced elevated expressions of MDA5, TLR3/7/8 and NOD1/2. And MDA5, TLR3/8 and NOD1/2 were higher in MAVS knockout mice than in WT mice (Supplementary Fig. 5e). And both of RIG-I and RIPK2 in MAVS-KO mice were significantly decreased compared with WT mice (Supplementary Fig. 5e).
Interestingly, RIG-I is known to be involved in MAVS activation during viral infection serving as an intracellular RNA sensor21,36. In view of the kyoto encyclopedia of genes and genomes analysis data and the previously documented impact of RIG-I in virus infection, we focused on RIG-I as an important potential contributor of MIRI. First, we examined both the expression and activation of RIG-I and MAVS in vivo during MIRI. We observed that RIG-I and MAVS expression was increased in the MIRI mice after 6 h of reperfusion compared to the sham group (Fig. 4a–d). Lysine 63 residues-type ubiquitination was also significantly increased in the lysates of cardiac tissue from MIRI mice compared to sham hearts (Fig. 4a–d). This data indicated that both the RIG-I core protein and its lysine 63 residues-type ubiquitinated form were markedly enhanced in vivo following MIRI compared with those in the sham control mice (Fig. 4a, b).
a Co-immunoprecipitation assays were performed to detect lysine 63 residues (K63)-type ubiquitination of RIG-I in vivo at 6 h after reperfusion or sham. The RIG-I protein was used as the bait protein to capture the interaction protein candidates, and immunoprecipitation (IP) and input represent the protein sample to be detected, respectively. b Statistical data of protein expression in (a). c K63-type ubiquitination of MAVS in vivo was determined by co-immunoprecipitation assay. The MAVS protein acts as the bait protein to capture the interaction proteins, and IP and input represent the protein sample to be detected, respectively. d Statistical data of protein expression in (c). e RIG-I and MAVS expression was determined by western blot in HEK293T cells transfected with RNA extracted from heart tissues at remote area, area at risk and infarct area after 6 h post-reperfusion or sham group, and RNA extracted from unrelated normal cells was negative control RNA (NC-RNA). f Statistical data of protein expression in (e). g Transcriptional levels of transforming growth factor-β-activated kinase 1 (TAK1), tumor necrosis factor-associated factor family 6 (TRAF6), interferon-α (IFN-α) and interferon-γ (IFN-γ) in HEK293T cells treated as described in (e). h K63-type ubiquitination of RIG-I was determined by co-immunoprecipitation at 48 h after transfection with total RNA from heart tissues at 6 h after reperfusion versus controls. i Statistical data of protein expression in (h). j Immunofluorescence staining of double-stranded RNA (dsRNA) in myocardial tissue sections in WT mice at 1 day after reperfusion and in sham group. α-actin indicates cardiomyocytes. Scale bar, 20 μm. b, d, f, g, i Data are shown with 3 biologically independent samples. Data are means ± standard deviation; ***p < 0.001, ****p < 0.0001 by one-way analysis of variance statistics with Tukey’s multiple comparisons test (g) and *p < 0.05, **p < 0.01, ***p < 0.001, **** p < 0.0001 by two-way analysis of variance with Tukey’s multiple comparisons test (f, i); ****p < 0.0001 by unpaired 2-tailed Student t test (b, d); ns, p ≥ 0.05. Source data are provided as a Source Data file.
Multiple types of myocardial injury are known to be associated with myocardial death and therefore may be associated with endogenous DNA or RNA degradation37,38. Therefore it was of major interest to study the possibility that myocardial injury and in particular MIRI involves endogenous RNA as a potential activator of RIG-I. Previous studies had shown that viral RNA is crucial to activate RIG-I to trigger downstream signaling pathways20,39,40. In order to obtain evidence using endogenously generated RNA from various tissues of the hearts during MIRI, we performed in vitro studies using HEK293T cells which were found to express RIG-I constitutively. First, total RNA was extracted from the remote area, risk area and infarction area of hearts at 6 h after reperfusion, and total RNA from sham hearts and unrelated cells served as controls. We found that total RNA extracted from both the infarct and risk areas induced elevated expression of RIG-I and MAVS in HEK293T cells in vitro compared to the sham group and remote area group under RNA stimulation conditions (Fig. 4e, f). In addition, total RNA increased the expression of transforming growth factor-β-activated kinase 1, tumor necrosis factor-associated factor family 6 and interferon-α and interferon-γat the transcriptional level, further confirming that the pathological tissue total RNA may activate the RIG-I/MAVS pathway (Fig. 4g) similar to virus infection. Next, we prepared cell lysates from HEK293T cells that had been transfected with total RNA from heart tissues after reperfusion or sham at 6 h. Enhanced lysine-63 residues-type ubiquitination of RIG-I was observed in the reperfused mice’s RNA transfection group (Fig. 4h). All this data is consistent with the possibility that intracellular RNA of injured cardiomyocytes may be involved in the activation of the RIG-I-MAVS cascade during MIRI. We speculated that myocardial injury and in particular MIRI would generate endogenous double-stranded RNA as a candidate molecule to activate RIG-I. For this important possibility, we determined the presence of double-stranded RNA in the hearts during MIRI by using an antibody against double-stranded RNA. The results showed that marked amounts of double-stranded RNA could be detected in the infarction area compared with the sham group and remote area (Fig. 4i). This data provided evidence that endogenous host double-stranded RNA produced during MIRI may be the trigger to activate and initiate the RIG-I cascade as reported36,40,41. Further work is required to expand this MIRI-associated pathway and its kinetics.
MAVS forms an active complex with tumor necrosis factor-associated factor families and transforming growth factor-β-activated kinase 1 during MIRI in mice
Next, we aimed to identify the protein partners of MAVS in MIRI. Based on the outcomes of mass spectrometry sequencing, MAVS exhibited a stronger interaction with RIG-I and transforming growth factor-β-activated kinase 1 during MIRI (Supplementary Fig. 5d). Previous studies had shown that tumor necrosis factor-associated factor families can be recruited by MAVS to form a signal complex21,25. We then examined the interaction among MAVS, transforming growth factor-β-activated kinase 1 and the candidate interacting protein, i.e., tumor necrosis factor-associated factor family 2/3/5/6, by co-immunoprecipitation. Our data revealed that pairwise interactions occurred between MAVS and transforming growth factor-β-activated kinase 1, MAVS and tumor necrosis factor-associated factor family 2/3/6, transforming growth factor-β-activated kinase 1 and tumor necrosis factor-associated factor family 3/5/6, tumor necrosis factor-associated factor family 6 and tumor necrosis factor-associated factor family 2/3/5 in vivo (Fig. 5a). Tumor necrosis factor-associated factor family 5/6 was up-regulated during MIRI, while tumor necrosis factor-associated factor family 2/3 was down-regulated in MIRI (Fig. 5a). It has been reported that tumor necrosis factor-associated factor family 6 is involved in the activation of transforming growth factor-β-activated kinase 1 and triggers the activation of downstream apoptosis-related pathways42. Tumor necrosis factor-associated factor family 2 has been reported to suppress necroptotic cell death under several pathological conditions such as doxorubicin-induced mitochondrial defects and cardiac dysfunction43 or cerebral ischemia-induced brain injury44. Tumor necrosis factor-associated factor family 3 acts as a negative regulator, and its degradation is required for mitogen-activated protein kinase activation45. Tumor necrosis factor-associated factor family 5 was reported to be up-regulated in heart tissues of ischemia-reperfusion injury mice and hypoxia/reoxygenation-stimulated cardiomyocytes and inhibits inflammation and apoptosis of hypoxia/reoxygenation-stimulated cardiomyocytes46. Therefore, tumor necrosis factor-associated factor family 6 may be a protein that promotes MIRI. The role of transforming growth factor-β-activated kinase 1 in MIRI remained unknown. Therefore, we further examined its interaction among MAVS, transforming growth factor-β-activated kinase 1 and the candidate protein tumor necrosis factor-associated factor family 6 in vitro (Supplementary Fig. 6a, b). Fluorescence resonance energy transfer assays further and independently confirmed the direct pairwise interactions of MAVS with transforming growth factor-β-activated kinase 1 and tumor necrosis factor-associated factor family 6 (Supplementary Fig. 6c, d).
a Co-immunoprecipitation was performed to determine interaction among MAVS, tumor necrosis factor-associated factor family 2/3/5/6 (TRAF2/3/5/6), transforming growth factor-β-activated kinase 1 (TAK1) in WT mice during MIRI. The experiment was repeated 3 times independently with similar results. b Immunofluorescence staining was used to detect the intracellular localization of overexpressed MAVS-S-peptide-tag (MAVS-S-tag), transforming growth factor-β-activated kinase 1-human influenza hemagglutinin (HA)-tag (TAK1-HA) and tumor necrosis factor-associated factor family 6-Flag-peptide-tag (TRAF6-Flag) proteins. Scale bar, 5 μm. c Intracellular localization of MAVS-S-tag, TAK1-HA and TRAF6-Flag proteins in HEK293T cells was determined by immunofluorescence after co-transfection with corresponding plasmids. The yellow arrow indicates the colocalization of the protein partners. Scale bar, 5 μm. d Oligomerization of MAVS in co-expression with TAK1 and TRAF6 in vitro was determined by semi-denaturing detergent agarose gel electrophoresis (SDD-AGE). MAVS and mitochondrial cytochrome coxidase IV (COX-IV) expression were determined by western-blot with sodium dodecyl sulfate polyacrylamide gel electrophoresis (SDS-PAGE). COX-IV was used as the mitochondrial internal reference protein. The experiment was repeated 3 times independently with similar results. e Lysine 63 residues (K63)-type ubiquitination of MAVS co-expressed with TAK1 and TRAF6 was determined by co-immunoprecipitation assay in vitro. IP and input represent the protein sample to be detected, respectively. f Statistical data of protein expression in e, data are shown with 3 biologically independent samples. Data are means ± standard deviation; *p < 0.05, **p < 0.01, ***p < 0.001, ****p < 0.0001 by two-way analysis of variance with Tukey’s multiple comparisons test (f); ns, p ≥ 0.05. Source data are provided as a Source Data file.
Next, we determined their intracellular localization in HEK293T cells overexpressing MAVS, transforming growth factor-β-activated kinase 1 and tumor necrosis factor-associated factor family 6 under homeostatic conditions: tumor necrosis factor-associated factor family 6 and transforming growth factor-β-activated kinase 1 were located uniformly in the cytoplasm, while MAVS was largely localized in the mitochondria compartment in a non-aggregated form, indicating that MAVS are in an inactive state (Fig. 5b). However, we found that the distribution of transforming growth factor-β-activated kinase 1 or tumor necrosis factor-associated factor family 6 changed from a predominant cytoplasmic expression to a mitochondria-bound condition revealing co-localization with MAVS when both were co-expressed with MAVS (Fig. 5c). Furthermore, when transforming growth factor-β-activated kinase 1 and tumor necrosis factor-associated factor family 6 were co-expressed with MAVS, the three proteins could form apparent co-localization complexes, and MAVS also presented as punctuated aggregates, i.e., a phenomenon termed prion-like aggregation, indicating the active form of MAVS (Fig. 5c). However, when transforming growth factor-β-activated kinase 1 and tumor necrosis factor-associated factor family 6 were co-overexpressed in cells by transfection, such punctuated appearance and mitochondria bound did not occur (Fig. 5c). To further identify the potential interaction patterns among MAVS, transforming growth factor-β-activated kinase 1 and tumor necrosis factor-associated factor family 6, we analysed the protein partners in overexpressed cells. This data showed that MAVS overexpression led to induction of RIG-I (Supplementary Fig. 6e, f), indicating that MAVS induces RIG-I in an apparent positive feedback loop. Furthermore, phosphorylated transforming growth factor-β-activated kinase 1 was enhanced when it was co-expressed with MAVS or when it was overexpressed (Supplementary Fig. 6e, f). Moreover, MAVS co-overexpressed with transforming growth factor-β-activated kinase 1 and tumor necrosis factor-associated factor family 6 showed a gel mobility shift indicating a higher molecular weight of the protein, indicating the possibility of post-translational modification of MAVS, i.e., ubiquitination (Supplementary Fig. 6e, f). In addition, we observed oligomerization of MAVS by semi-denaturing detergent agarose gel electrophoresis (Fig. 5d). We found that co-expression of transforming growth factor-β-activated kinase 1 and tumor necrosis factor-associated factor family 6 with MAVS could induce modification and polymerization of MAVS (Fig. 5d, Supplementary Fig. 6e, f). Additionally, lysine-63 residues-type ubiquitination of MAVS was enhanced consistent with functional activation of the protein in vitro (Fig. 5e, f). Lysine-63 residues-type ubiquitination and the protein level of RIG-I was also increased when MAVS was co-expressed with transforming growth factor-β-activated kinase 1 or tumor necrosis factor-associated factor family 6 in transfected cells (Supplementary Fig. 6g, h). These results indicated that MAVS forms a biological protein-protein interaction platform triggering the accumulation of transforming growth factor-β-activated kinase 1 and tumor necrosis factor-associated factor family 6 complex to allow MAVS further activation during MIRI.
MAVS regulates the myocardial mitogen-activated protein kinase/JNK pathway through the transforming growth factor-β-activated kinase 1/tumor necrosis factor-associated factor family 6 axis in MIRI in mice
To further explore how MAVS regulates downstream signaling pathways in cardiomyocytes, we next examined further components of the presumed RNA-RIG-I-MAVS-dependent signaling cascade in MAVS-overexpressing or MAVS-deficient HL-1 cells (Supplementary Fig. 7a). Overexpression of MAVS in cardiomyocytes enhanced phosphorylated transforming growth factor-β-activated kinase 1 and up-regulated tumor necrosis factor-associated factor family 6 and RIG-I expression, while MAVS knockdown cells showed same level as controls (Supplementary Fig. 7b). In addition, phosphorylated tumor necrosis factor-associated factor family-associated nuclear factor kappa-B activator-binding kinase 1, phosphorylated interferon regulatory factor 3 and p-P65, p-JNK and phosphorylated p38-mitogen-activated protein in the mitogen-activated protein kinase pathway were enhanced in MAVS-overexpressed cardiomyocyte cell line while in MAVS knockdown cells showed no change except for p-P65 (Supplementary Fig. 7c, d). Since the mitogen-activated protein kinase/JNK signaling pathway plays an important role in cell death, we determined apoptosis-related proteins to obtain independent parameters for functional apoptosis events. Overexpression of MAVS led to up-regulation of pro-apoptotic-related proteins poly-ADP-ribose polymerase and B-cell lymphoma-2-associated X protein, and down-regulation of anti-apoptotic protein B-cell lymphoma-2 and the cleavage of apoptotic protein cysteinyl aspartate specific proteinase 3 in cardiomyocytes, while in MAVS knockdown cells pro-apoptotic-related proteins showed not significant change as in MAVS overexpression cells (Supplementary Fig. 7e).
Furthermore, relevant proteins were examined in cell damage model induced by hydrogen peroxide and confirmed the in vivo data at mechanistic levels of a cultured cell line. The results showed that under hydrogen peroxide treatment conditions, MAVS knockdown inhibited the overexpression of RIG-1, transforming growth factor-β-activated kinase 1 and tumor necrosis factor-associated factor family 6, and inhibited the phosphorylation of tumor necrosis factor-associated factor family-associated nuclear factor kappa-B activator-binding kinase 1, interferon regulatory factor 3 and P65 in the nuclear factor kappa-B pathway compared with the control groups and the MAVS overexpression group (Supplementary Fig. 8a, b). Moreover, MAVS knockdown significantly inhibited the phosphorylation of JNK and p38-mitogen-activated protein in the mitogen-activated protein kinase pathway, and effectively protected apoptosis induced by hydrogen peroxide compared with the control groups, which was manifested by the reduction of poly ADP-ribose polymerase, B-cell lymphoma-2-associated X protein and cleaved cysteinyl aspartate specific proteinase 3 (Supplementary Fig. 8c, d).
All this data led us to focus on the mitogen-activated protein kinase/JNK pathway. To examine the possibility that the MAVS/transforming growth factor-β-activated kinase 1/tumor necrosis factor-associated factor family 6 axis-induced cardiomyocyte apoptosis in vivo, we examined protein expression in remote area, infarct area and area at risk of hearts from MAVS-KO and WT mice in the MIRI and sham hearts. MAVS expression was significantly higher in infarcted area and area at risk, accompanied by up-regulation of RIG-I, transforming growth factor-β-activated kinase 1, phosphorylated-transforming growth factor-β-activated kinase 1 and tumor necrosis factor-associated factor family 6 protein in WT mice (Fig. 6a). These proteins were significantly down-regulated or inhibited in MAVS-KO mice (Fig. 6a). Importantly, the expression of p-JNK was increased in the infarcted area of WT mice and it was markedly inhibited in MAVS-KO mice (Fig. 6b), while phosphorylated p38-mitogen-activated protein and phosphorylated extracellular regulated protein kinases were increased in the infarcted area of MAVS-KO mice, although they were significantly lower relative to the WT group (Supplementary Fig. 9a). The expression of p-P65, phosphorylated tumor necrosis factor-associated factor family-associated nuclear factor kappa-B activator-binding kinase 1 and phosphorylated interferon regulatory factor 3 were also increased in the infarcted area of both WT mice and MAVS-KO mice although they were significantly lower in the MAVS-KO group (Supplementary Fig. 9b). This data provided evidence that MAVS regulates the downstream proteins of the non-canonical mitogen-activated protein kinase/JNK signaling pathways through transforming growth factor-β-activated kinase 1/tumor necrosis factor-associated factor family 6 followed by activation of p38, extracellular regulated protein kinases, as well as canonical pathway including tumor necrosis factor-associated factor family-associated nuclear factor kappa-B activator-binding kinase 1, interferon regulatory factor 3 and p65 activation. Subsequently, we evaluated the expression of proteins related to apoptosis and observed an increase of cysteinyl aspartate specific proteinase 3 cleavage, poly ADP-ribose polymerase and B-cell lymphoma-2-associated X protein, and a decrease of B-cell lymphoma-2 in the infarcted area of WT mice (Fig. 6c). However, in MAVS-KO mice, the poly ADP-ribose polymerase and B-cell lymphoma-2-associated X protein expression were inhibited and expression of B-cell lymphoma-2 was promoted (Fig. 6c). We next assayed the signaling pathway-related proteins RIG-I, transforming growth factor-β-activated kinase 1, phosphorylated transforming growth factor-β-activated kinase 1, tumor necrosis factor-associated factor family 6, tumor necrosis factor-associated factor family-associated nuclear factor kappa-B activator-binding kinase 1, interferon regulatory factor 3, and nuclear factor kappa-B pathway protein, as well as mitogen-activated protein kinase pathway protein JNK, p38-mitogen-activated protein, and apoptosis related protein poly ADP-ribose polymerase, B-cell lymphoma-2-associated X protein, B-cell lymphoma-2, cleaved cysteinyl aspartate specific proteinase 3 (Supplementary Fig. 9c) in MAVS knockdown and control mice, and similar results were obtained (Supplementary Fig. 9d–g). Taken together, these results provided evidence that MAVS participated in apoptosis of heart cells in MIRI in vivo. This injurious effect links the RIG-I-MAVS signaling pathway to the recruitment of transforming growth factor-β-activated kinase 1 and tumor necrosis factor-associated factor family 6 resulting in phosphorylation of transforming growth factor-β-activated kinase 1 and activation of mitogen-activated protein kinase/JNK pathway, ultimately triggering injurious apoptosis of heart cells. Finally, deficiency of MAVS significantly inhibited the activation of mitogen-activated protein kinase/JNK pathway and the apoptosis cascade.
a Expression and analysis of RIG-I, MAVS, phosphorylated transforming growth factor-β-activated kinase 1 (p-TAK1), transforming growth factor-β-activated kinase 1 (TAK1), and tumor necrosis factor-associated factor family 6 (TRAF6) in heart tissues of sham, remote area, area at risk and infarct area after 6 h of reperfusion in MAVS-KO and WT mice. b Expression and analysis of p-JNK and JNK in hearts after 24 h of reperfusion in MAVS-KO and WT mice. c Expression and analysis of poly ADP-ribose polymerase (PARP), B-cell lymphoma-2 (BCL2), B-cell lymphoma-2-associated X protein (BAX), and cysteinyl aspartate specific proteinase 3 (cleaved caspase3) in the hearts of MAVS-KO and WT mice after 3 days reperfusion. d The determination of oxygen consumption rate (OCR) on neonatal mouse cardiac myocytes derived from WT and MAVS-KO mice. Different color-labeled region denotes corresponding OCR parameters. e The determination of OCR in neonatal mouse cardiac myocytes treated with hypoxia for 2 h and reoxygenation for 6 h. Different color-labeled region denotes corresponding OCR parameters. f Analysis of parameters involved in mitochondrial bioenergetics, including basal respiration, adenosine triphosphate (ATP) production, maximal respiration, spare respiratory capacity, proton leak, non-mitochondrial respiration, spare respiratory capacity as a% and coupling efficiency. n = 10 tests/group. a–c Data are shown with 3 biologically independent samples. Data are presented as mean ± standard deviation;*p < 0.05, **p < 0.01, ***p < 0.001, ****p < 0.0001 by two-way analysis of variance with Tukey’s multiple comparisons test (a–c); ns, p ≥ 0.05; by one-way analysis of variance with Tukey’s multiple comparisons test (f). *p < 0.05, **p < 0.01, ***p < 0.001, ****p < 0.0001, ns, p ≥ 0.05. Source data are provided as a Source Data file.
Reactive oxygen species participates in the activation of the MAVS/JNK pathway in mice during MIRI
MIRI may induce elevation of reactive oxygen species and knock down MAVS may inhibit reactive oxygen species elevation in vivo (Fig. 2k). To investigate the effect of MAVS in response to reactive oxygen species stimulation, we examined the reactive oxygen species levels in HL-1 cell lines induced by hydrogen peroxide or in control cells. The results showed that under normal conditions, the intracellular total reactive oxygen species level and mitochondrial reactive oxygen species level in MAVS overexpression group were significantly higher than those in MAVS knockdown group (Supplementary Fig. 10a, b). After hydrogen peroxide stimulation, the intracellular total reactive oxygen species levels in the MAVS knockdown group was also significantly lower than that in MAVS overexpression group, and the mitochondrial reactive oxygen species levels in the MAVS knockdown group was lower than that in the negative control knockdown group, but there was no significant difference between MAVS knockdown and MAVS overexpression groups (Supplementary Fig. 10a, b). To follow a potential role of reactive oxygen species during MIRI we conducted mitochondrial stress tests on neonatal mouse cardiac myocytes derived from WT and MAVS-KO mice. The results indicated that under normal oxygen circumstances, MAVS knockout significantly increased mitochondrial maximum respiration, spare capacity, and non-mitochondrial respiration, yet, there was no substantial alteration in basic respiration, adenosine triphosphate productivity, and proton leakage between WT and MAVS-KO mice group (Fig. 6d, f). However, under hypoxia and reoxygenation conditions, MAVS knockout significantly enhanced mitochondrial function, encompassing basic respiration, adenosine triphosphate production, maximum oxygen consumption rate, spare capacity, proton leakage rate and non-mitochondrial respiration (Fig. 6e, f), suggesting that MAVS knockout enhanced mitochondrial respiratory metabolism and thereby mitigated mitochondrial damage. Also, we performed mitochondrial stress tests in hypoxia- and reoxygenation- induced HL-1 cell lines. The results showed MAVS knock down did not affect basal respiration, maximal respiration and non-mitochondrial respiration under normal conditions (Supplementary Fig. 10c, e). However, after hypoxia and reoxygenation, maximal respiration and spare capacity in the MAVS knockdown group were lower than those in the MAVS overexpression group, but there were no differences in mitochondrial basic respiration, adenosine triphosphate production capacity and non-mitochondrial respiration between MAVS knockdown and MAVS overexpression group (Supplementary Fig. 10d, e).
Targeting the MAVS/JNK pathway is indispensable to block the effect of MAVS on MIRI in mice
Since the expression of MAVS is affected by reactive oxygen species stimulation (Supplementary Fig. 8), we conducted in vivo reactive oxygen species clearance experiments to understand reactive oxygen species’ impacts mechanistically. The results showed that the reactive oxygen species scavenger mitoquinone mesylate significantly reduced the level of total reactive oxygen species in WT mice, and also showed a significant decrease in MAVS-KO mice (Fig. 7a). The effect on mitochondrial reactive oxygen species levels decrease was more significant in WT mice (Fig. 7b). Serum myocardial enzyme detection showed that mitoquinone mesylate significantly reduced creatine kinase, creatine kinase isoenzyme and α-hydroxybutyrate dehydrogenase release in WT mice and creatine kinase isoenzyme level in MAVS-KO mice (Fig. 7c). 2, 3, 5-triphenyltetrazolium chloride + Evans blue staining also showed that the myocardial infarction size of mitoquinone mesylate treated mice was significantly reduced (Fig. 7d). These results suggest that reducing reactive oxygen species levels in MIRI can effectively protect short-term myocardial injury. As reported, inhibition of mitochondrial reactive oxygen species by the mitochondria-targeted antioxidant mitoquinone mesylate prevented MAVS oligomerization and type I interferon production47. To obtain further mechanistic insight of reactive oxygen species during MIRI, we studied the effects of mitoquinone mesylate on RIG-I/MAVS activation. The results showed that mitoquinone mesylate significantly inhibited IR-induced MAVS and RIG-I lysine-63 residues ubiquitination (Fig. 7e–h). Importantly, mitoquinone mesylate inhibited the activation of RIG-I/MAVS pathway. Furthermore, phosphorylation of JNK was significantly reduced in vivo (Fig. 7i, j). These results indicate that reactive oxygen species promote activation of RIG-I/MAVS/JNK during MIRI.
a The total reactive oxygen species (ROS) was determined in heart tissue at 6 h post-reperfusion in the mitoquinone mesylate (MitoQ)-treated and untreated MIRI group and sham group in WT mice and MAVS-KO mice. b The expression levels of mitochondrial reactive oxygen species (mitoROS) was determined in heart tissue at 6 h post-reperfusion in the MitoQ-treated and untreated MIRI group and the sham group in WT mice and MAVS-KO mice. c Serum levels of myocardial injury markers creatine kinase, α-hydroxybutyrate and creatine kinase isoenzyme were determined in WT mice and MAVS-KO mice treated with or without mitoquinone mesylate at 6 h post-reperfusion. n = 8. d WT mice treated with or without MitoQ underwent 30 min of ischemia and 24 h of reperfusion. 2, 3, 5-triphenyltetrazolium chloride + Evans blue staining was performed. The ratio of infarct area to left ventricle was analyzed. n = 6. Scale bar, 2 mm. e Lysine-63 residues (K63)-type ubiquitination of MAVS in WT mice treated with or without MitoQ at 6 h post-reperfusion was determined by co-immunoprecipitation assay. f Statistical data of protein expression in (e). g K63-type ubiquitination of RIG-I in WT mice treated with or without MitoQ at 6 h post-reperfusion was determined by co-immunoprecipitation assay. h Statistical data of protein expression in (g). i Phosphorylation of JNK in WT mice treated with or without MitoQ at 6 h post-reperfusion was determined by co-immunoprecipitation assay. j Statistical data of protein expression in (i). f, h, j Data are shown with 3 biologically independent samples. Data are presented as mean ± standard deviation; ****p < 0.0001 by unpaired 2-tailed Student t test (d). **p < 0.01, ***p < 0.001, ****p < 0.0001 by one-way analysis of variance statistics with Tukey’s multiple comparisons test (f, h, j), *p < 0.05, **p < 0.01, ***p < 0.001, ****p < 0.0001 by two-way analysis of variance with Tukey’s multiple comparisons test (a–c); ns, p ≥ 0.05. Source data are provided as a Source Data file.
JNK inhibitors exert cardio-protective effects in MIRI in mice
To further confirm the role of mitogen-activated protein kinase/JNK pathway in MAVS-mediated injury on myocardium in MIRI, the inhibitors AS601245 and SP600125, and the agonists anisomycin and juglanin which target the JNK pathway were used in WT mice and MAVS-KO mice, respectively. First, we verified that treatment of AS601245 negatively regulated the expression of p-JNK in myocardial tissues after MIRI in WT mice (Fig. 8a, b). Importantly, AS601245 and SP600125 treatment significantly reduced the infarct area of WT mice with MIRI compared to control mice at 1day after reperfusion (Fig. 8c, Supplementary Fig. 11a). Furthermore, cardiac function parameters at 24 h after reperfusion were improved by the pharmaceuticals compared to non-treated mice, as evidenced by increased left ventricular ejection fraction and left ventricular fractional shortening, and decreased left ventricular end-systolic volume and left ventricular end-diastolic volume (Fig. 8d, e). We also performed the treatment in MAVS-KO mice during MIRI, and found that the AS601245 treatment improved cardiac function but there was no significance difference between the untreated mice (Supplementary Fig. 11b). AS601245 administration markedly reduced the levels of myocardial enzymes in the circulation of WT mice, as evidenced by decreased creatine kinase, creatine kinase isoenzyme and α-hydroxybutyrate levels (Fig. 8f), indicating a protective effect against injury in myocardial tissues. Furthermore, both AS601245 or SP600125 treatment effectively reduced the infarct size at day 3 after reperfusion (Fig. 8g, Supplementary Fig. 11c, d), decreased the number of apoptotic cardiomyocytes compared with control mice (Fig. 8h, Supplementary Fig. 11e, f); and the apoptosis-related proteins poly ADP-ribose polymerase, B-cell lymphoma-2-associated X protein and cysteinyl aspartate specific proteinase 3 cleavage in the infarction area of WT mice were decreased compared with those in untreated control mice with AS601245 administration (Fig. 8i, j). Moreover, mice treated with SP600125 or AS601245 showed reduced myocardial damage, improved cardiac function, reduced fibrosis, and increased angiogenesis (Supplementary Fig. 11c, d, Supplementary Fig. 12a–f), suggesting that JNK inhibitors protect against MIRI.
a JNK and p-JNK levels measured in infarct area at 24 h post-reperfusion in AS601245-treated/untreated MIRI and sham group. b Statistical data of protein expression in (a). c WT mice with/without AS601245 underwent 30 min of ischemia and 24 h of reperfusion. 2, 3, 5-triphenyltetrazolium chloride + Evans blue staining was performed. The infarct area ratio to left ventricle was analyzed. n = 7. Scale bar, 2 mm. d Echocardiography in WT mice with/without AS601245 treatment at 6 h post-reperfusion. Yellow line shows left ventricle wall positions, white arrow the distance. LVIDS, Left ventricular internal diameter end systole; LVIDD, Left ventricular internal diameter end diastole. Scale bar, 1 mm. e Left ventricular ejection fraction (LVEF), left ventricular fraction shortening (LVFS), left ventricular end-systolic volume (LVESV) and left ventricular end-diastolic volume (LVEDV) assessed in MAVS-KO mice treated with/without AS601245 for 6 h post-reperfusion. n = 5. f Serum myocardial injury markers were determined in WT mice with/without AS601245 at 6 h post-reperfusion. n = 5. g Hematoxylin-eosin staining and analysis of WT mice sections with/without AS601245 at day 3 post-reperfusion. n = 8. Scale bar, 1 mm. h Terminal deoxynucleotidyl transferase-mediated 2’-deoxyuridine 5’-triphosphate nick end labeling (TUNEL) and wheat germ agglutinin (WGA) staining and analysis of heart sections from WT mice treated with or without AS601245 at day 3 post-reperfusion. n = 7. Scale bar, 20 μm. i Apoptosis-related proteins determined by western-blot in heart tissue areas of WT mice treated with/without AS601245 at day 3 post-reperfusion. j Statistical analysis of protein expression in (i). b, j Data are shown with 3 biologically independent samples. Data are presented as mean ± standard deviation; ****p < 0.0001 by unpaired 2-tailed Student t test (c, g, h). **p < 0.01, ***p < 0.001, ****p < 0.0001 by one-way analysis of variance statistics with Tukey’s multiple comparisons test (e, f), *p < 0.05, **p < 0.01, ***p < 0.001, ****p < 0.0001 by two-way analysis of variance with Tukey’s multiple comparisons test (b, j); ns, p ≥ 0.05. Source data are provided as a Source Data file.
To further study the involvement of JNK in MIRI, we applied the JNK agonists juglanin on MAVS-KO mice following MIRI. Juglanin significantly enhanced p-JNK expression in MAVS-KO mice heart tissues of both sham group and ischemia reperfusion group (Supplementary Fig. 11g, h). The infarct area of MAVS-KO mice treated with juglanin during MIRI was significantly increased compared to the untreated mice (Supplementary Fig. 11i, j). The creatine kinase, creatine kinase isoenzyme and α-hydroxybutyrate were increased in both MAVS-KO and WT mice by juglanin administration (Supplementary Fig. 11k, l). The number of TUNEL+ apoptotic cardiomyocytes was elevated in the agonist treated mice (Supplementary Fig. 11m, n), accompanied with an increase of poly ADP-ribose polymerase, B-cell lymphoma-2-associated X protein, cleaved cysteinyl aspartate specific proteinase 3 protein levels which are all related to apoptosis in the infarct area, compared to those in untreated mice (Supplementary Fig. 11o, p). Moreover, administration of juglanin led to an increase of infarct size, myocardial fibrosis and decrease of angiogenesis (Supplementary Fig. 12g–k). Furthermore, we evaluated whether the inhibitors and agonists could cause possible side effect on mice, and detectable toxicities were not observed (Supplementary Fig. 13a).
Taken together, this data indicated that the JNK inhibitors AS601245 and SP600125 exerted cardio-protective effects on the hearts in MIRI, while the administration of its agonists had the opposite effect strongly suggesting that the MAVS-JNK signaling pathway plays an indispensable role in heart injury during MIRI.
Discussion
Using a combination of in vivo models of MIRI-triggered heart injury together with a series of in vitro approaches, the study detailed above supports several major conclusions: MIRI triggers the RIG-I signaling cascade and markedly induces the expression of MAVS in vivo; MAVS acts as a signaling hub for MIRI-dependent downstream events by recruiting transforming growth factor-β-activated kinase 1 and tumor necrosis factor-associated factor family 6 to the outer mitochondrial membrane and generation of biologically active MAVS/transforming growth factor-β-activated kinase 1/tumor necrosis factor-associated factor family 6 complexes followed by transforming growth factor-β-activated kinase 1 phosphorylation (phosphorylated -transforming growth factor-β-activated kinase 1) and phosphorylation of its downstream targets; during MIRI, MAVS participates in activation of the myocardial mitogen-activated protein kinase/JNK cascade via the transforming growth factor-β-activated kinase 1/tumor necrosis factor-associated factor family 6 axis; MAVS-KO or myocardium-specific knockdown of MAVS protect mice from acute and chronic complications of MIRI; and pharmacological inhibition of the final RIG-I-MAVS cascade target, i.e., JNK, reduces myocardial injury in WT mice whereas pharmacological JNK activation eliminates cardio-protection in MAVS-KO mice. It has been reported that the isoform-specific and cell type-specific impacts of JNK proteins appear to be important for progression of some diseases48. The latter data should be interpreted with caution as JNK-related pharmaceuticals may exert off-target effects. Therefore, it cannot be ruled out that the observed protective effects of SP600125/AS601245 during ischemia/reperfusion are associated with the inhibition of other kinases. And the specificity concerning JNK subtypes targeted by two inhibitors in our study remains to be investigated further. When taken together, this data shows that MAVS/tumor necrosis factor-associated factor family 6/transforming growth factor-β-activated kinase 1 complexes at the outer mitochondrial membrane are an obligatory and functionally significant component of MIRI-triggered heart injury and that several downstream signaling molecules of RIG-I may represent a pharmacological targets to treat both acute and chronic outcomes of MIRI (Fig. 9).
MIRI-induced reactive oxygen species (ROS) activates the RIG-I signaling cascade - at least in part - by RNA generated during myocardial death, in which MAVS plays the role of a hub to regulate downstream signaling: MAVS recruits and interacts with transforming growth factor-β-activated kinase 1 (TAK1) and tumor necrosis factor-associated factor family 6 (TRAF6), and participates in the mitogen-activated protein kinase/JNK signaling pathway, which triggers apoptosis-related pathways that induce cardiomyocyte apoptosis, immune cell infiltration and adverse ventricular remodeling such as increased fibrosis and impaired angiogenesis in vivo. MAVS deficiency prevents cardiomyocyte apoptosis and reduces immune cell infiltration and fibrosis, while promoting angiogenesis. JNK inhibition protects against MIRI. The graphics were generated with BioRender (https://app.biorender.com).
MAVS has been recognized for its role in antiviral immune responses, where it induces the expression of proinflammatory cytokines and antiviral genes such as interferon and interferon-stimulating genes to inhibit viral replication and transmission21,49. Moreover, recent evidence in non-viral diseases suggests that MAVS may also be activated under conditions of mitochondrial reactive oxygen species release, promoting host defense and initiating inflammatory responses through the oligomerization of MAVS and subsequent type I interferon production in systemic lupus erythematosus50. However, the pathophysiological roles of MAVS in the absence of viral infection are less well understood49,50. Studies have shown that MAVS is involved in stress-induced cardiac hypertrophy and it regulates cardiomyocyte metabolism by affecting mitochondrial function where it is essential for nucleotide-binding oligomerization domain protein 1 and receptor-interacting protein kinase 2 interactions and activation of the downstream nuclear factor kappa-B-P65 signaling pathway27. However, identification of the specific mechanism by which MAVS affect cardiomyocyte functions require further work. Here, we made attempts to comprehensively delineate the outcomes and define the underlying signaling pathways following MIRI. These studies uncovered a series of potential signals underlying MIRI in mice.
Previous studies had shown that MAVS can form prion-like aggregates on the outer membrane of mitochondria upon activation and that these aggregates are important for their biological functions21. In view of the body of data obtained here, we propose that MAVS functions as a binding platform for transforming growth factor-β-activated kinase 1 and tumor necrosis factor-associated factor family 6, which trigger biologically active complexes. Tumor necrosis factor-associated factor family 6 is linked to the degradation of poly ADP-ribose polymerase, a molecule involved in DNA damage-related apoptosis and specifically activate transforming growth factor-β-activated kinase 1 leading to cell death26,49,51,52. Our data not only demonstrates MAVS’ involvement in ischemia-reperfusion-induced cardiomyocyte pathologies, but also sheds light on its unconventional biological function: participating in the innate immune response during MIRI.
The mitogen-activated protein kinase-mediated JNK pathway is a stress-induced signaling pathway that responds strongly to inflammatory cytokines and cellular stress, and promotes apoptosis in ischemia-reperfusion29,53. However, the mechanism of JNK pathway activation during MIRI in vivo has remained unclear. Here, we demonstrate that the JNK pathway is likely critically involved in hypoxia-induced cardiomyocyte apoptosis and that JNK activation is dependent on MAVS-mediated activation in vivo. Our study further reveals that MAVS knockdown in vivo still promotes the phosphorylation of downstream proteins, such as p38-mitogen-activated protein, extracellular regulated protein kinases, interferon regulatory factor 3, tumor necrosis factor-associated factor family-associated nuclear factor kappa-B activator-binding kinase 1 and P65. This indicats that mitogen-activated protein kinases and nuclear factor kappa-B pathways can be activated independently of MAVS during MIRI. For example, the cyclic guanine monophosphate–adenosine monophosphate synthase–stimulator of interferon genes (cGAS-STING) pathway has been reported to activate the tumor necrosis factor-associated factor family-associated nuclear factor kappa-B activator-binding kinase 1 (TBK1)-interferon regulatory factor 3 (IRF3)-nuclear factor kappa-B (NF-κB) signaling pathway54,55. However, JNK and transforming growth factor-β-activated kinase 1 (TAK1) phosphorylation are not completely inhibited in MAVS knockdown mice, possibly due to MAVS expression in cardiac fibroblasts rather than cardiomyocytes.
In preliminary studies, we speculated that MIRI-triggered apoptosis and other forms of cell death may involve the formation of myocardium-derived endogenous host RNA (intracytoplasmic double-stranded RNA or single stranded RNA or mitochondrial double-stranded RNA; Fig. 9) as candidates for MIRI-specific initiation of RIG-I activation. Our data provide circumstantial evidence that nonviral endogenous RNA species of still unknown origin are selectively generated during the initial time window of MIRI, and that this RNA triggers RIG-I activation including its lysine 63 residues -type ubiquitination in vivo and in vitro. Moreover, our data show that injured cardiomyocytes produce abundant double-stranded RNA selectively in infarct tissues, which may initiate lysine 63 residues ubiquitination of RIG-I and activation of the interferon pathway in vitro. We recognize, however, that further studies are needed to obtain more direct evidence for the veracity of the important possibility that the RIG-I activator(s) may critically involve the action of MIRI-dependent RNA molecules and possibly other activators.
In conclusion, the present study provides substantial evidence of the deleterious effect of MAVS and its associated mechanism of activation via RIG-I in myocardial injury. Our data indicate the potential of targeting MAVS itself and a series of previously not recognized signaling molecules in the RIG-I-activated signaling cascade as therapeutics during MIRI.
Methods
Animals
All animal care procedures and experiments were performed in accordance with the guidelines of the Animal Ethics and Experimentation Committee of the Union Hospital of Tongji Medical College, Huazhong University of Science and Technology, and in accordance with the Guide for the Care and Use of Laboratory Animals. All animal experiments were approved by the Laboratory Animal Management and Welfare Ethical Review Committee of Huazhong University of Science and Technology (Permission No.: #IACUC-4143). All mice were housed under a controlled 12-hour light-dark diurnal cycle with regulated temperature (20 °C to 25 °C) and relative humidity (40% to 60%). They had ad libitum access to food (Laboratory Rodent Diet, LabDiet, 5001) and water. C57BL/6 wild type (WT) mice were purchased from Vital River Laboratory (Beijing China), while global MAVS-knockout mice were a gift of Huazhong Agricultural University. Cardiomyocyte-specific MAVS-deficient mice were generated by injecting the adeno-associated virus 9 (AAV9) via the tail vein of 6-week-old WT male mice, which knock down the MAVS gene by RNAi under the control of the myocardial-specific promoter cardiac troponin I (cTNT): pAV-cTnT-shRNA-MAVS-GFP, short hairpin RNA (shRNA) sequences: AGCAACCAGACTGGACCAAATATAGTGAAGCCACAGATGTATATTTGGTCCAGTCTGGTTGCC), resulting in the knockdown of MAVS in cardiomyocytes after three weeks. Control mice were obtained with the negative control shRNA sequences that had no homology with MAVS (NC-sh) as described before.
To establish the mouse model of myocardial ischemia-reperfusion injury (MIRI), male mice weighing between 24 g and 27 g and aged 8–10 weeks were intraperitoneally injected with sodium pentobarbital. The chest was then debrided, and the heart exposed by opening the chest on the left side. The left anterior descending coronary artery was ligated with a 7-0 suture, and after 30 min, the occlusion was removed, and the myocardium was allowed to reperfuse. In the sham-operated group, the same surgery was performed without left anterior descending coronary artery ligation. The mice utilized in this study adhered strictly to the ethical standards for animal anesthesia and euthanasia as established by relevant guidelines. For anesthesia, 4% isoflurane was administered in a closed chamber until the loss of the righting reflex, followed by maintenance at 1.5–2% via a nose cone. Vital signs were continuously monitored throughout the procedure, and body temperature was maintained at approximately 37 °C using heating pads. Euthanasia was conducted via intravenous injection of sodium pentobarbital at a dose of 150 mg/kg following light isoflurane anesthesia. Death was confirmed when vital signs ceased for more than 5 min. All procedures were approved by the institutional ethics committee and complied with applicable regulations.
Cell lines and viruses
HL-1 cells (ATCC-CVCL0303) are derived from mice myocardial cells and HEK293T cells (ATCC-CRL-3216) were obtained from American type culture collection, USA. Lentiviral vectors overexpressing target protein and negative control vector (NC-oe), lentiviral knock-down vector expressing short hairpin RNA target genes, and knock-down vector expressing negative control short hairpin RNA (NC-sh), were constructed to overexpress or knockdown the mouse MAVS gene (NM 144888.2). These lentivirus vectors were then packaged into HEK293T cells as the following steps56. Seed HEK293T cells 1 days before transfection to reach 70–80% confluency. Mix lentiviral vector plasmid with packaging plasmids (pSPAX2 and pMD2.G) and transfection reagent PEI (sigma, #408719)), then transfect cells. Change medium 12–18 h post-transfection, harvest viral supernatant 48–72 h later, centrifuge at low speed and filter through 0.45 μm filter. MAVS over-expressed or knockdown HL-1 cells were infected with the respective lentiviruses and the infected cells were selected using purinamycin (MCE, 5 μg/mL).
Hypoxia- reoxygenation protocol in vitro
To mimic MIRI, cells were exposed to hypoxic chambers using pure N2 at 37 °C for 16 h, followed by reoxygenation at 17% O2 and 5% CO2 at 37 °C for 8 h or in hypoxic for 2 h and reoxygenation for 6 h as required. During hypoxia, serum-free medium was used, while complete medium with 10% fetal bovine serum Dulbecco’s Modified Eagle Medium was used for reoxygenation or normoxia controls. For normoxia controls, cells were incubated in 10% fetal bovine serum Dulbecco’s Modified Eagle Medium with 17% O2 and 5% CO2 at 37 °C for 24 h before analysis.
Stress injury model induced by hydrogen peroxide in vitro
HL-1 cells were exposed to 600 μM hydrogen peroxide in serum-free medium for 8 h. The serum-free Dulbecco’s Modified Eagle Medium without hydrogen peroxide treated cells was used for controls. Cell lysates were prepared for the western-blotting as described.
Detection of apoptosis in myocardial cell lines
HL-1 cells were exposed to hypoxic chambers using pure N2 at 37 °C for 16 h, followed by reoxygenation at 17% O2 and 5% CO2 at 37 °C for 8 h. Cells were then subjected to apoptosis staining using an apoptosis kit (Beyotime) according to the manufacturer’s instructions, 7-Aminoactinomycin D (7-AAD) and Allophycocyanin-labeled-Annexin V were used in combination to to label apoptotic cells. Data was analyzed using flow cytometry (Beckman).
Detection of mitochondrial membrane potential
HL-1 cells were exposed to 16 h hypoxia and 8 h reoxygenation and subsequently stained using Tetramethylrhodamine Ethyl Ester kit (Beyotime) at 37 °C for 30 min, in accordance with the manufacturer’s instructions. The mean fluorescence intensity was measured using flow cytometry (Beckman).
Glutathione detection
HL-1 cells were subjected to 16 h hypoxia and 8 h reoxygenation and the intracellular level of reduced glutathione was assessed using a glutathione kit (Beyotime) according to the manufacturer’s instructions. The absorbance was measured at 450 nm using a microplate reader.
Isolation of cardiomyocytes and non-cardiomyocytes from adult mouse heart
8 weeks old male WT mice were utilized for isolating primary cardiomyocytes after 6 h of reperfusion or in the sham group. The isolation protocol was based on previously published studies57. Briefly, mice were anesthetized to expose the heart followed by injection of 7 mL ethylene diamine tetraacetic acid buffer (5 mM, PH 7.8) into the right ventricle after cutting the descending aorta. The ascending aorta was clamped with Reynolds forceps, and the heart was transferred to a 35-mm dish. 10 mL ethylene diamine tetraacetic acid buffer, 3 mL perfusion buffer, and 30 to 50 mL collagenase II buffer were sequentially injected into the left ventricle. The heart was gently pulled into 1-mm pieces using forceps, and cellular dissociation was achieved by gentle trituration. Cell suspensions were passed through a 100-μm filter, and cells were subjected to four sequential rounds of gravity settling. The cardiomyocyte-enriched cell pellet from each round formed a highly enriched cardiomyocyte fraction, while the supernatant from each round was combined to produce a non-cardiomyocyte population.
Isolation of immune cells from the heart
Heart tissues obtained from mice after 6 hours of reperfusion were digested using collagenase 2 (1 mg/mL, Solarbio) for 20 min at 37 °C. The cell suspensions were transferred to 10% fetal bovine serum, followed by sequential passage through 70 μm cell strainers. Density gradient centrifugation using Percoll solution (Sigma) with 40% and 80% density in the upper and lower layers, respectively, was performed. The middle layer containing immune cells was collected using pipettes for subsequent lysis and detection.
Isolation of neonatal mouse cardiomyocytes
Neonatal mouse hearts without determination of sex of the donor mouse were collected from neonatal mice 1 day after delivery and primary mouse ventricular cardiomyocytes were isolated. The isolation protocol was based on previously published studies27. The harvested heart was snipped in Ca2+ and Mg2+ free Hank’s Balanced salt solution and then digested in 0.125% pancreatic enzymesfor 10 min at 37 °C. Cells released after the first digestion were discarded and subsequently digested in collagenase 2 (1 mg/mL, Solarbio), cells were transferred to Dulbecco’s Modified Eagle Medium supplemented with 10% fetal bovine serum until all cardiomyocytes have been isolated (about 3–4 times). The cell mixture was rerouted in Dulbecco’s Modified Eagle Medium at 500 × g for 5 min and inoculated in a 35-mm dish. The non-cardiomyocytes adhere to the dish more rapidly, so the cardiomyocytes were in the upper layer of the medium. The cardiomyocytes were incubated in laminin-coated dishes at 37 °C and 5% CO2 for 48 h, and then collected for further biochemical analysis.
Western-blotting
Cultured cells or heart tissues were washed with ice-cold phosphate-buffered saline and subsequently homogenized in Radio Immunoprecipitation Assay Lysis Buffer (Beyotime) containing 1 mM phenylmethylsulfonyl fluoride and 1% (v/v) protease and phosphorylase inhibitor cocktail (Roche, USA). Tissue lysates were prepared from remote areas, areas at risk and infarcted areas. Protein concentrations were determined by employing the bicinchoninic acid assay kit (Beyotime). Equal amounts of cell lysates were separated by 10% or 12% sodium dodecyl sulfate-polyacrylamide gel electrophoresis and subsequently transferred onto polyvinylidene difluoride membranes (Millipore, Merck, Darmstadt, Germany). Polyvinylidene difluoride membranes were blocked in 5% non-fat milk tris buffered saline with tween 20 (Tris-buffered saline with 0.1% Tween 20) for 1 h at room temperature and then incubated overnight at 4 °C with primary antibodies. Membranes were incubated with horseradish peroxidase-conjugated secondary antibodies (Protech, #SA00001-1/2, 1:3000) for 1.5 h at room temperature. Finally, the blots were visualized using an enhanced chemiluminescence (ECL) reagent (Invitrogen, USA). The imageJ software was used to calculate the gray value of the band, and the corresponding control group was selected as the homogenization. The primary antibodies employed were as follows: MAVS-rabbit- monoclonal antibody (CST, #83000, 1:1000), MAVS-rabbit-polyclonal antibody (Protech, #14341-1-AP, 1:2000), Lysine 63 residues (K63)-type-ubiquitination antibody (CST, #5621, 1:1000), β-actin (Protech, #81115-1-RR, 1:2000), α-actin (Protech, #23660-1-AP, 1:1000), COX-IV (Protech, #11242-1-AP, 1:1000), TAK1 (Protech, #12330-2-AP, 1:1000), p-TAK1 (Abcam, ab109404), TRAF6 (Abmart, #T55175, 1:1000), TRAF3 (Protech, # 18099, 1:1000), TRAF2 (Abclone, #A19129, 1:1000), TRAF5 (Protech, # 12868, 1:1000), TBK1 (CST, #3504, 1:1000), p-TBK1 (CST, #5483, 1:1000), IRF3 (CST, #4302, 1:1000), p-IRF3 (CST, #4947, 1:1000), P65 (CST), p-P65 (CST, #3033, 1:1000), RIG-I (Protech, #20566-1-AP, 1:1000), JNK (Abmart, #T40073, 1:1000), p-JNK (Abmart, #T40072S, 1:1000), p-JNK (CST, #4668, 1:1000), P38 (Abmart, #T55600, 1:1000), p-P38 (Abmart, #TP56391, 1:1000), ERK (Abmart, #T40071, 1:1000), p-ERK (Abmart, #T40072, 1:1000), PARP (Protech, # 66520-1-Ig, 1:1000), BAX (Abmart, #T40051, 1:1000), BCL2 (Abmart, #T40056, 1:1000), Cleaved-Caspase3 (Abmart, #TA7022, 1:1000), HA-tag (Abmart, #TU281749, 1:1000), S-tag-mouse-monoclonal antibody (Abmart, #MU118305, 1:1000), S-tag-rabbit-polyclonal antibody (CST, #12774, 1:1000), Flag-tag (Abmart, #M20008, 1:1000).
Infarct size measurements
The surgical procedure of ischemia/reperfusion was conducted following established protocols. At 24 h, mice were euthanized and the heart was immediately excised. The coronary artery was re-occluded at the site of initial occlusion and 2 mL 1% Evans-blue (Sigma) was continuously perfused into the inferior vena cava for 3 min. The heart was removed and washed twice. Subsequently, it was frozen at −80 °C for 10 min and cut into 1 mm-thick sections. Sections were incubated with 1% solution of 2,3,5-triphenyltetrazolium chloride (TTC; Sigma) at 37 °C for 30 min, followed by fixation with 4% paraformaldehyde (PFA, Servicebio) for 2 h at room temperature. Finally, hearts were photographed under a microscope and analyzed using Image J software (version 1.38×, National Institutes of Health, Bethesda, MD, USA) to quantify the area of cardiac infarction and risk area. The remote area is indicated by blue, the area at risk by red and the infarct area by white. The left ventricular area was determined using Image J software.
Echocardiography
Transthoracic echocardiography was performed with a Vevo 2100 instrument (Visual Sonics, Toronto, Ontario, Canada) equipped with an MS-400 Imaging transducer. Mice were gently anesthetized with isoflurane, and the hair on their chest was removed to expose the heart. Mice were immobilized in a supine position on an echogenic pad to minimize data bias, and kept anesthetized during echocardiography. Echocardiography was performed at 6 h, 24 h and 14 days after initiation of reperfusion in the MIRI group. The left ventricular end-diastolic volume and left ventricular end-systolic volume were assessed by direct measurement of B-mode tracings of the left ventricular endocardial border in the parasternal long axis. In addition, the left ventricular ejection fraction and left ventricular fractional shortening were determined. LVEF is the ratio of systolic to diastolic output of the heart. LVFS is the ratio of left ventricular end-diastolic diameter minus left ventricular end-systolic diameter to left ventricular end-diastolic diameter. Acquisition and analyses of echocardiograms were performed by a technician who was blinded to the subgroup.
Histological and immunofluorescence staining
Hearts obtained were fixed with 4% paraformaldehyde and embedded in paraffin at various time points post-MIRI or sham surgery (6 h, 1 days, 3 days, 14 days and 28 days) and tissue sections of 5 μm at 3 d post-MIRI were prepared and stained with hematoxylin-eosin staining. Infarct size was quantified by Image J software. The fibrotic lesions of tissue sections at 14 d post-MIRI were visualized using Masson staining. The percentage of collagen fiber staining area in entire visual field in infarct area was quantified using Image J software and be analyzed. Cardiomyocytes were stained with fluorescein isothiocyanate -labeled wheat germ agglutinin lectin (Gene Tex, #GTX01502, 1:200) with tissue sections at 14 d post-MIRI, and more than three visual fields were selected to measure the area of a total of 20 cells. The size of cardiomyocytes was measured using image J. Tissue slices from MAVS knockdown and control mice at 28 d post-infection were stained with MAVS-rabbit- monoclonal antibody (CST, #83000, 1:200) and green fluorescent protein (GFP)-mouse- monoclonal antibody (Protech, #66002-1-Ig, 1:150) and fluorescein isothiocyanate -labeled wheat germ agglutinin lectin, respectively. Double-stranded RNA was stained with K1-mouse-monoclonal antibody (CST, #28764, 1:400) in tissues slices from WT mice at 1day after reperfusion. Tissues slices from WT mice at 3day, 7day, 14day, 28day after reperfusion were stained with Phospho-Histone H3 (Protech, #66863-1, 1:200) and CD31 (CST, #77699, 1:200). Slices incubated with Alexa Fluor 647- Goat-anti-mouse secondary antibodies (Abcam, ab150115, 1:500), and Alexa Fluor 594 anti-mouse secondary antibodies (Abcam, ab150116, 1:500), Alexa Fluor 594 anti-rabbit secondary antibodies (Abcam, ab150080, 1:500), or Alexa Fluor 488 anti-rabbit secondary antibodies (Abcam, ab150077, 1:500), Alexa Fluor 488 anti-mouse secondary antibodies (Abcam, ab150113, 1:500) as required. Images were captured using a Pannoramic scanner (3DHISTECH Pannoramic MIDI, Hungary) or a fluorescence microscope (Nikon A1 plus).
Terminal deoxynucleotidyl transferase-mediated 2’-deoxyuridine 5’-triphosphate nick end labeling assay of myocardial tissue
Terminal deoxynucleotidyl transferase-mediated 2’-deoxyuridine 5’-triphosphate nick end labeling (TUNEL) assays were performed using the One-step TUNEL In Situ Apoptosis Kit (Elabscience, #E-CK-A422) in accordance with the manufacturer’s instructions. Cardiomyocytes were stained fluorescein isothiocyanate-labeled wheat germ agglutinin lectin. TUNEL-positive cells were quantified from five different fields of > three mice per experimental group, and the sections were subsequently photographed using a Pannoramic scanner (3DHISTECH Pannoramic MIDI, Hungary). Statistical analysis was performed using Image J and GraphPad Prism6.
Transmission electron microscopy
At 6 h after reperfusion, myocardial tissue was fixed with glutaraldehyde overnight. Then it was fixed with 1% osmic acid at 4 °C for 2–3 h, dehydrated with gradient alcohol (50%, 70%, 80%, 85%, 90%, 95%, 100%), soaked overnight with acetone and epoxy resin, and finally embedded and cured with epoxy resin. The tissue was cut into 100 nm thickness and stained with lead and uranium. The mitochondrial morphology of cardiomyocytes was observed using a frozen transmission electron microscopy (Thermo Fisher, Glacios). The damaged and undamaged mitochondria were counted in a field of view with a magnification of 1700 times within non-repeating unit areas in the infarct area and quantified using Image J.
Biochemical and ELISA assays
Blood was collected at 6 h after reperfusion and left at room temperature for 1 h before centrifugation at 3000 rpm at 4 °C for 10 min. The concentrations of creatine kinase and creatine kinase isoenzyme, α-hydroxybutyrate dehydrogenasein serum were determined according the manufacturer’s instructions (Nanjing JianCheng). Cardiac troponin I was detected using an Enzyme linked immunosorbent assay kit (Elabscience, #E-EL-M1203).
Angiogenesis assessment
At 14 days post-reperfusion, heart tissues were embedded in paraffin, sectioned and immunostained with CD31 antibody (CST, #77699, 1:200) and phosphorylated Histone H3 antibody (Protech, #66863-1, 1:200) which is a marker of cell division and regeneration to label vascular endothelial cells using a fluorescence microscope (Nikon A1 plus). The diameter of vessels was generally equal to or greater than 5μm were defined as new blood vessels. The number of blood vessels within five non-repeating unit areas in the high power fieldswas quantified using Image J.
Immunofluorescence assay
Plasmids to overexpress MAVS (NM_144888.2), tumor necrosis factor-associated factor family 6 (NM_009424.3), and transforming growth factor-β-activated kinase 1 (NM_00936.1) were constructed using the pCDNA3.1 vector. The C-terminal of each gene and different tag peptides (S-peptide-tag, Flag-peptide-tag, hemagglutinin (HA)-tag) were expressed by fusion. HEK293T cells were transfected separately or together with MAVS-S-peptide-tag (MAVS-S-tag), tumor necrosis factor-associated factor family 6-Flag-peptide-tag (TRAF6-FLAG), transforming growth factor-β-activated kinase 1-human influenza hemagglutinin (HA)-tag (TAK1-HA) plasmids. After 48 h, cells were fixed by 4% paraformaldehyde for 10 min at room temperature and blocked for 1 h at room temperature using 5% bovine serum albumin. MAVS-S-tag overexpressing cells were incubated with S-tag-mouse-monoclonal antibody (Abmart, #MU118305, 1:200) overnight, and then incubated with Alexa Fluor 647-Goat-anti-mouse secondary antibodies (Abcam, ab150115, 1:500), and Alexa Fluor 594 Azide / Alexa Fluor 488 Tetrafluorophenyl Ester-Flag (Protech, CL594-66008/CL488-66008, 1:500) or Alexa Fluor 488 Tetrafluorophenyl Ester / Alexa Fluor 594 Azide-HA (Protech, CL488-66006/CL594-51064, 1:500) antibodies, as required, at room temperature for 1.5 h. Cells were stained with 4’,6-Diamidino-2-phenylindole dihydrochloride (DAPI, Beyotime # C1005) at room temperature for 10 min and then Mito-Tracker Green (Beyotime, #C1048, 1:200) at 37 ˚C for 30 min. After washing, cells were imaged using a confocal microscope (Leica STELLARIS 8 WLL).
Fluorescence resonance energy transfer experiment
HEK293T cells were transfected with the MAVS-pEGFP-C1, MAVS-pEBFP-C1, TRAF6-pEGFP-C1, and TAK1-pEBFP-C1 plasmids, and donor and acceptor plasmids were co-transfected. Co-transfections included donor plasmid MAVS-pEBFP-C1 and the acceptor plasmid TRAF6-pEGFP-C1, donor plasmid MAVS-pEGFP-C1 and acceptor plasmid TAK1-pEBFP-C1, donor plasmid TRAF6-pEGFP-C1 and acceptor plasmid TAK1-pEBFP-C1. The vector plasmids pEGFP-C1 and pEBFP-C1 were co-transfected as control. After 24 h post-transfection, cells were observed for photoreceptor bleaching using a confocal microscope (Nikon A1R MP).
Semidenaturing detergent agarose gel electrophoresis
The methodology of semidenaturing detergent agarose gel electrophoresis was conducted in accordance with previous protocols21. Crude mitochondria were isolated from HEK293T cells overexpressing MAVS-S-peptide-tag (MAVS-S-tag), tumor necrosis factor-associated factor family 6-Flag-peptide-tag (TRAF6-FLAG), transforming growth factor-β-activated kinase 1-human influenza hemagglutinin (HA)-tag (TAK1-HA) and control by differential centrifugation, using the Cell Mitochondria Isolation Kit (Beyotime, #C3601). Mitochondria were resuspended in 1×semidenaturing detergent agarose gel electrophoresis sample buffer (0.5×Tris-borate-ethylene diamine tetraacetic acid buffer, 10% glycerol, 2% sodium dodecylsulfate and 0.0025% bromophenol blue) and loaded onto a vertical 1.5% agarose gel containing 0.1% sodium dodecylsulfate. Electrophoresis was carried out in a running buffer (1×Tris-borate-ethylene diamine tetraacetic acid buffer and 0.1% sodium dodecylsulfate) for approximately one hour at a constant voltage of 100 voltage and a temperature of 4 °C and subsequently transferred onto polyvinylidene difluoride membranes. Polyvinylidene difluoride membranes were blocked with 5% non - fat milk in Tris - buffered saline containing 0.1% Tween 20 at room temperature for 1 h, then incubated with primary antibodies overnight at 4 °C. After that, membranes were incubated with horseradish peroxidase - conjugated secondary antibodies (Protech, #SA00001 − 1/2, 1:3000) for 1.5 h at room temperature. Finally, blots were visualized using an enhanced chemiluminescence (ECL) reagent (Invitrogen, USA). The gray value of the band was calculated by ImageJ software, with the corresponding control group used for normalization.
Tissue RNA extraction
After 6 h of reperfusion, 30–40 mg myocardial tissue of remote area, infarcted area and area at risk from MIRI mice and sham group were collected and homogenized with 1 mL TRIZOL reagent (Takara) using a grinder (Servicebio). The vortexed tubes were incubated for 5 min at room temperature. A mixture of 200 μL phenol, chloroform, and isoamyl alcohol (25: 24: 1) was added to the tissue lysis solution, violently shaken for 15 s, and left at room temperature for 3 min. Then the tissue lysis was centrifuge at 4 °C at 12,000 g for 15 min. The upper water phase was transferred to a new 1.5 mL eppendorf tube, mixed with 200 μL chloroform and centrifuged at 4 °C at 12,000 g for 10 min. Transfer the top water phase to a new 1.5 mL eppendorf tube, add 1.5 times the volume of isopropyl alcohol and leave for 10 min at room temperature. Centrifuge at 4 °C at 12,000 g for 10 min and remove the supernatant. Then RNA precipitate at the bottom was washed with 1 mL 75% ethanol, and then centrifuged at 7500 g for 5 min. The supernatant was discarded and the RNA was dried at room temperature. 50 μL of RNase-free water was added and the precipitate was dissolved at 60 °C for 10 min. RNA samples were kept at −80 °C.
RNA transfection
On the day before transfection, 1.0 × 106 HEK293T cells were seeded in cell culture dishes with a diameter of 5 cm and 5 mL of antibiotic-free growth medium was added to each plate. Transfection was initiated when the cell density was 50–60%. Replace 4.25 mL fresh serum-free Dulbecco’s Modified Eagle Medium medium in the plate. For each transfection plate, the mixture of RNA and transfection reagent polyethylenimine (PEI, sigma, #408719) was prepared as follows: 10 μg RNA was added to Opti-Minimum Essential Medium (Gibico), and the final volume was 300 μL; 30 μL transfection reagent polyethylenimine (3 times the volume of total RNA) was added into another 2 mL eppendorf tube, and supplemented with Opti-Minimum Essential Mediumto 300 μL, gently mixed, and left at room temperature for 5 min. The medium mixture containing RNA was added to the medium mixture containing polyethylenimine with thoroughly mixed by vortex, and incubated at room temperature for 15 min. The mixture was added into plates containing HEK293T cells, with a final volume of 5 mL, and gently mixed. The cells were cultured in a carbon dioxide incubator at 37 °C for 5–6 h. The medium containing serum was changed and the cells were cultured for 24–48 h. Conduct follow-up treatment and detection according to experimental requirements.
Quantitative real-time polymerase chain reaction
After 6 h of reperfusion, 30–40 mg myocardial tissue from remote, infarcted and risk areas of MIRI mice and sham group were collected. HL-1 control cells were collected. Homogenize the tissue from mice and HL-1 cells with 1 mL TRIZOL reagent using a grinder. Incubate the vortexed tubes for 5 min at room temperature. Add 200 μL mixed solution of phenol, chloroform and isoamyl alcohol with the ratio 25:24:1, shake vigorously for 15 s, and let stand for 3 min. Centrifuge at 4 °C, 12,000 g for 15 min. Transfer the upper water phase, mix with 200 μL chloroform, and centrifuge again. Transfer the top water phase, add 1.5 - fold isopropyl alcohol, incubate, centrifuge, and discard the supernatant. Wash the RNA precipitate with 75% ethanol, centrifuge, discard the supernatant, and dry. Dissolve the RNA in 50 μL RNase - free water at 60 °C for 10 min. HEK293T cells were transfected with 10 μg RNA extracted from heart tissue of MIRI mice and sham group, and HL-1 control cells. Complementary DNA (cDNA) was obtained for a template according to the instructions of reverse transcription kit (Takara). Quantitative Real-time Polymerase Chain Reaction was performed with primers.
The primer sequences were as follows:
TRAF6 forward (human): CAATGCCAGCGTCCCTTCCAAA,
TRAF6 reverse (human): CCAAAGGACAGTTCTGGTCATGG.
TAK1 forward (human): CAGAGCAACTCTGCCACCAGTA,
TAK1 reverse (human): CATTTGTGGCAGGAACTTGCTCC.
IFN-α forward (human): AGAAGGCTCCAGCCATCTCTGT,
IFN-α reverse (human): TGCTGGTAGAGTTCGGTGCAGA.
IFN-γ forward (human): GAGTGTGGAGACCATCAAGGAAG,
IFN-γ reverse (human): TGCTTTGCGTTGGACATTCAAGTC.
MDA5 forward (mouse): TGCGGAAGTTGGAGTCAAAGCG,
MDA5 reverse (mouse): CACCGTCGTAGCGATAAGCAGA.
RIG-I forward (mouse): AGCCAAGGATGTCTCCGAGGAA,
RIG-I reverse (mouse): ACACTGAGCACGCTTTGTGGAC.
NOD1 forward (mouse): CCTGAAGCAGAACACCACACTG,
NOD1 reverse (mouse): CTTGGCTGTGATGCGATTCTGG.
NOD2 forward (mouse): CCTAGCACTGATGCTGGAGAAG,
NOD2 reverse (mouse): CGGTAGGTGATGCCATTGTTGG.
TLR3 forward (mouse): GTCTTCTGCACGAACCTGACAG,
TLR3 reverse (mouse): TGGAGGTTCTCCAGTTGGACCC.
TLR7 forward (mouse): GTGATGCTGTGTGGTTTGTCTGG,
TLR7 reverse (mouse): CCTTTGTGTGCTCCTGGACCTA.
TLR8 forward (mouse): AAGTGCTGGACCTGAGCCACAA,
TLR8 reverse (mouse): CCTCTGTGAGGGTGTAAATGCC.
RIPK2 forward (mouse): TCGTGTGGATCCTCTCTGCTCT,
RIPK2 reverse (mouse): TTCCAGGACAGTGGTGTGCCTT.
Co-immunoprecipitation assay
For co-immunoprecipitation assay, cell or heart tissue lysates were mixed with ice-cold immune-precipitation buffer (Beyotime, #P0013J) containing protease and phosphorylase inhibitor cocktail (Roche, USA). The mixture was then incubated with the target antibody at 4 °C overnight under constant agitation. Protein A/G agarose beads (Beyotime, #P2012) were incubated with the lysates for 3 h at 4 °C followed by washing, and then lysed with 1×sodium dodecyl sulfate polyacrylamide gel electrophoresis sample buffer. The supernatant was subsequently used for western-blotting with corresponding antibodies.
K63 ubiquitination detection
The expression plasmids or total RNA were transfected into HEK293T cells according to the manufacturer’s instructions. After 24 h, 10 μM of the proteasome inhibitor MG132 (MCE, #133407-82-6) was added, and the cells were collected and mix with immunoprecipitation buffer containing protease and phosphorylase inhibitor cocktail, and supplemented with 10 mM N-ethylmaleimide (NEM, MCE, #128-53-0) after an additional 12-h incubation period. Heart tissues were homogenized with IP buffer containing protease and phosphorylase inhibitor cocktail, and supplemented with 10 mM N-ethylmaleimide at 6 h after reperfusion. The resulting cell lysates were mixed with ice-cold immunoprecipitation buffer (Beyotime, #P0013J) containing protease/phosphorylase inhibitors (Roche). The mixture was incubated with the target antibody at 4 °C overnight with constant agitation. Protein A/G agarose beads (Beyotime, #P2012) were added and incubated for 3 h at 4 °C. After washing, beads were lysed with 1×SDS-PAGE sample buffer. The supernatant was used for western blotting with K63 ubiquitination antibodies.
Mass spectrometry
After 6 h of reperfusion, myocardial tissue from MIRI mice and sham group were collected and homogenized using a grinder (Servicebio). The western and immunoprecipitation cell lysis buffer (Beyotime) was used to prepare the cell lysate for co-immunoprecipitation assay. The supernatant was incubated with primary MAVS antibody (CST, #83000, 1:100) overnight at 4 °C. Protein A/G agarose beads were added and incubated for 3 hours at 4 °C followed by washing, and then lysed with lysate buffer. The protein lysate was centrifuged at 12,000 rpm for 10 min at 4 °C, and the resulting supernatant was used for western-blotting detection and mass spectrometry. The sample was sequencing by Beijing Genomics Institute (BGI) and analyzed. The experiment was repeated 3 times independently. Protein gel strips were identified by separating sample proteins via gel electrophoresis, obtaining strips at different film positions, extracting peptides post-enzymatic digestion. Mass spectrometry was used to get protein mass spectra in these strips, followed by protein identification with software. Dried peptide samples were run on Thermo UltiMate 3000 UHPLC. Liquid -separated peptides were ionized by nanoESI and detected in DDA mode on Q - Ex X massactive HF spectrometer. Search engine results were pre-processed and re-scored by Percolator. Output was filtered at 1% FDR (PSM - level FDR ≤ 0.01) to get significant identified spectra and peptide lists.
Proteomics sequencing
After 6 h of reperfusion, myocardial tissue from MIRI mice and sham group were collected. The whole extracts was sequencing by Beijing Genomics Institute (BGI). In this isobaric tags for relative and absolute quantification (iTRAQ) quantification project, three groups of samples were set up in ischemia-reperfusion group and sham group, and each group contained three heart tissue samples. Peptides and proteins were identified with 1% false discovery rate. Proteins with 1.2 fold change and Q-value less than 0.05 were determined as differentially expressed protein in single replicate. For experimental design with more than one replicate, proteins with 1.2 fold change (mean value of all comparison groups) and P-value (t-test of all comparision groups) less than 0.05 were defined as differentially expressed proteins. We use coefficient of variation to evaluate the reproducibility. Coefficient of variation is defined as the ratio of the standard deviation to the mean.
Flow cytometry
Heart tissues obtained 3 days after reperfusion were digested using collagenase 2 (Solarbio) at a working concentration of 1 mg/mL for 20 min at 37 °C. The resulting heart suspensions were supplemented with 10% fetal bovine serum Vitaland passed sequentially through 70 μm cell strainers to obtain isolated cells. The cells were then stained with antibodies to identify immune cells. CD45 subsets were gated using CD45 (BD, clone: 104). The dead cells were eliminated with Fixable Viability Stain 510 (BD, Cat# 564406). Samples were acquired using a flow cytometer (Beckman) and analyzed using CytExpert software (Beckman).
Oxidant /antioxidant experiment in vivo
WT and MAVS-KO mice were intraperitoneally administered with mitoquinone mesylate (MCE) at a dosage of 10 mg/kg 30 min prior to surgery and 2 h after reperfusion. Six hours subsequent to reperfusion, cardiac infarction tissues of mice were collected. The cardiac tissues were digested using collagenase 2 at a working concentration of 1 mg/mL for 20 min at 37 °C, and the cardiomyocyte suspension was isolated. Reactive oxygen species probe DCFH-DA (MCE, #4091-99-0) and mitochondrial probe MitoRed (MCE, #HY-KD1029) were utilized for staining, and dead and living cells labeled by Fixable Viability Dye eFluor™ 780 (Invitrogen, #65-0865) were stained, and intracellular reactive oxygen species levels and mitochondrial reactive oxygen species levels were examined by flow cytometry (Beckman) and analyzed using CytExpert software (Beckman).
Mitochondrial bioenergetics determination
Mitochondrial bioenergetics was measured in neonatal mouse cardiac myocytes derived from WT and MAVS-KO mice and HL-1 cells using Seahorse XFe96 analyzer (Agilent, US) as described27. Cells were seeded at a density of 20,000 cells per well in laminin-coated (Sigma, L2020, 5 μg/mL, incubated at 37 °C for 2 h) Seahorse Bioscience XFe96 cell culture plates. Following a 2-h hypoxic exposure and subsequent 6-h reoxygenation period, the cells underwent washes and were then incubated in an unbuffered assay medium (Dulbecco’s Modified Eagle Medium supplemented with 5.5 mM glucose, 10 mM galactose, 2 mM L-glutamine, 1 mM sodium pyruvate, 100 U/mL penicillin, 100 μg/mL streptomycin, pH 7.4) at 37 °C in a non-humidified, CO2-free incubator. After establishing the basal oxygen consumption rate, a Seahorse XF Cell Mito Stress Test was performed to evaluate mitochondrial respiration. This included measuring ATP-linked respiration by assessing changes in oxygen consumption rate following the addition of 1.5 μM oligomycin. Maximal respiration was induced using 1.0 μM carbonyl cyanide-p-trifluoromethoxyphenylhydrazone (FCCP), an uncoupler. Mitochondrial respiration was subsequently halted by adding 0.5 μM rotenone and 0.5 μM antimycin A. Parameters related to mitochondrial bioenergetics were calculated based on oxygen consumption rate readings.
Inhibition and agonist experiments in vivo
WT mice or MAVS-KO mice were administered with JNK inhibitor AS601245 (MCE, # 345987-15-7) through the tail vein at a dose of 15 mg/kg 30 min prior to ischemia and 3 h after reperfusion. SP600125 (MCE, #129-56-6) was administered orally at a dose of 30 mg/kg 30 min prior to ischemia and 5 min after reperfusion. MAVS-KO or WT mice mice were administered with JNK agonist anisomycin (MCE, #22862-76-6) through the tail vein at a dose of 30 mg/kg immediately following reperfusion. Juglanin (MCE, # 5041-67-8) was subjected to intraperitoneal injection at a dose of 30 mg/kg 30 min prior to ischemia and 5 min after reperfusion. Untreated mice served as controls. At 6 h, 24 h, 3days and 14 days post-reperfusion, echocardiography, serum myocardial enzymogram, 2, 3, 5-triphenyltetrazolium chloride staining, terminal deoxynucleotidyl transferase-mediated 2’-deoxyuridine 5’-triphosphate nick end labeling staining, and cardiac tissue protein were evaluated as described before. The inhibitor SP600125 or agonist anisomycin or juglain was administered orally, intraperitoneally and by tail vein at a dose of 30 mg/kg per day, respectively. The inhibitor AS601245 was administered by tail vein at a dose of 15 mg/kg per day.
Pathological staining score
The degrees of pathological changes in comparison to mock-infected samples were scored by the standard as described58 in with some modifications: 0 = normal; 1 = minimal change (minute quantity of necrosis or inflammatory cells); 2 = mild change (a small quantity of necrosis or inflammatory cells); 3 = moderate change (modest quantity of necrosis or inflammatory cell infiltration); 4 = marked change (large numbers of necrosis or inflammatory cell infiltration); 5 = severe change (diffuse necrosis or inflammatory cell infiltration; almost no remaining normal tissue). Statistical analyses were performed using the SPSS 20.0 software.
Statistical analysis
Continuous variables were expressed as mean ± standard deviation, while categorical variables were presented as number and percentage. To assess differences between two groups, the two-tailed Student’s t-test or Mann–Whitney U test was utilized as appropriate. For multiple group comparison, One-way analysis of variance or Two-way analysis of variance was performed as appropriate. A p < 0.05 is considered statistically significant. All statistical analyses were conducted using SPSS 20.0 software.
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Data availability
The Proteomics sequencing raw data generated in this study have been deposited in the iProX partner repository database under accession code PXD062097 (https://www.iprox.cn/page/project.html?id=IPX0011424000). The protein mass spectrometry raw data used in this study are available in the iProX partner repository database under accession code PXD062096 (https://www.iprox.cn/page/project.html?id=IPX0011419000). The data that support the findings of this study are available within the article and its supplementary information files. Source data are provided with this paper.
References
Ibáñez, B., Heusch, G., Ovize, M. & Van de Werf, F. Evolving therapies for myocardial ischemia/reperfusion injury. J. Am. Coll. Cardiol. 65, 1454–1471 (2015).
Heusch, G. Cardioprotection research must leave its comfort zone. Eur. Heart J. 39, 3393–3395 (2018).
Bansal, S. S. et al. Dysfunctional and proinflammatory regulatory T-Lymphocytes are essential for adverse cardiac remodeling in ischemic cardiomyopathy. Circulation 139, 206–221 (2019).
Hausenloy, D. J. & Yellon, D. M. Ischaemic conditioning and reperfusion injury. Nat. Rev. Cardiol. 13, 193–209 (2016).
Jernberg, T. et al. Association between adoption of evidence-based treatment and survival for patients with ST-elevation myocardial infarction. Jama 305, 1677–1684 (2011).
Valiente-Alandi, I. et al. Inhibiting fibronectin attenuates fibrosis and improves cardiac function in a model of heart failure. Circulation 138, 1236–1252 (2018).
Lesnefsky, E. J., Chen, Q., Tandler, B. & Hoppel, C. L. Mitochondrial Dysfunction and myocardial ischemia-reperfusion: implications for novel therapies. Annu. Rev. Pharmacol. Toxicol. 57, 535–565 (2017).
Wang, J. & Zhou, H. Mitochondrial quality control mechanisms as molecular targets in cardiac ischemia-reperfusion injury. Acta Pharmaceutica Sin. B 10, 1866–1879 (2020).
Bertero, E. & Maack, C. Calcium signaling and reactive oxygen species in mitochondria. Circ. Res. 122, 1460–1478 (2018).
Ramachandra, C. J. A., Hernandez-Resendiz, S., Crespo-Avilan, G. E., Lin, Y. H. & Hausenloy, D. J. Mitochondria in acute myocardial infarction and cardioprotection. EBioMedicine 57, 102884 (2020).
Maack, C. et al. Treatments targeting inotropy. Eur. Heart J. 40, 3626–3644 (2019).
Ferrucci, L. et al. Transcriptomic and proteomic of gastrocnemius muscle in peripheral artery disease. Circ. Res. 132, 1428–1443 (2023).
Robichaux, D. J., Harata, M., Murphy, E. & Karch, J. Mitochondrial permeability transition pore-dependent necrosis. J. Mol. Cell. Cardiol. 174, 47–55 (2023).
Murphy, E. et al. Mitochondrial function, biology, and role in disease: a scientific statement from the american heart association. Circ. Res. 118, 1960–1991 (2016).
Bender, S. et al. Activation of Type I and III interferon response by mitochondrial and peroxisomal MAVS and Inhibition by Hepatitis C Virus. PLoS Pathog. 11, e1005264 (2015).
Meylan, E. et al. Cardif is an adaptor protein in the RIG-I antiviral pathway and is targeted by hepatitis C virus. Nature 437, 1167–1172 (2005).
Thoresen, D. et al. The molecular mechanism of RIG-I activation and signaling. Immunol. Rev. 304, 154–168 (2021).
Bruns, A. M., Leser, G. P., Lamb, R. A. & Horvath, C. M. The innate immune sensor LGP2 activates antiviral signaling by regulating MDA5-RNA interaction and filament assembly. Mol. Cell 55, 771–781 (2014).
Zhong, B. et al. The adaptor protein MITA links virus-sensing receptors to IRF3 transcription factor activation. Immunity 29, 538–550 (2008).
Zeng, W. et al. Reconstitution of the RIG-I pathway reveals a signaling role of unanchored polyubiquitin chains in innate immunity. Cell 141, 315–330 (2010).
Hou, F. et al. MAVS forms functional prion-like aggregates to activate and propagate antiviral innate immune response. Cell 146, 448–461 (2011).
Silva, J. L., De Moura Gallo, C. V., Costa, D. C. & Rangel, L. P. Prion-like aggregation of mutant p53 in cancer. Trends Biochem. Sci. 39, 260–267 (2014).
Liu, B. et al. The ubiquitin E3 ligase TRIM31 promotes aggregation and activation of the signaling adaptor MAVS through Lys63-linked polyubiquitination. Nat. Immunol. 18, 214–224 (2017).
Liu, S. et al. MAVS recruits multiple ubiquitin E3 ligases to activate antiviral signaling cascades. eLife 2, e00785 (2013).
Lee, N. R., Kim, H. I., Choi, M. S., Yi, C. M. & Inn, K. S. Regulation of MDA5-MAVS antiviral signaling axis by TRIM25 through TRAF6-Mediated NF-kappaB Activation. Molecules Cells 38, 759–764 (2015).
Chattopadhyay, S. et al. Viral apoptosis is induced by IRF-3-mediated activation of Bax. EMBO J. 29, 1762–1773 (2010).
Lin, H. B. et al. Innate Immune Nod1/RIP2 signaling is essential for cardiac hypertrophy but requires mitochondrial antiviral signaling protein for signal transductions and energy balance. Circulation 142, 2240–2258 (2020).
Wang, Q. et al. Reduced immunity regulator MAVS contributes to non-hypertrophic cardiac dysfunction by disturbing energy metabolism and mitochondrial homeostasis. Front. Immunol. 13, 919038 (2022).
Rose, B. A., Force, T. & Wang, Y. Mitogen-activated protein kinase signaling in the heart: angels versus demons in a heart-breaking tale. Physiol. Rev. 90, 1507–1546 (2010).
Wang, X. et al. Homocysteine induces cardiomyocyte dysfunction and apoptosis through p38 MAPK-mediated increase in oxidant stress. J. Mol. Cell. Cardiol. 52, 753–760 (2012).
Johnson, G. L. & Lapadat, R. Mitogen-activated protein kinase pathways mediated by ERK, JNK, and p38 protein kinases. Science 298, 1911–1912 (2002).
Davis, R. J. Signal transduction by the JNK group of MAP kinases. Cell 103, 239–252 (2000).
Raman, M., Chen, W. & Cobb, M. H. Differential regulation and properties of MAPKs. Oncogene 26, 3100–3112 (2007).
Li, L. et al. Transforming growth factor β-activated kinase 1 signaling pathway critically regulates myocardial survival and remodeling. Circulation 130, 2162–2172 (2014).
Jain, M. et al. Increased myocardial dysfunction after ischemia-reperfusion in mice lacking glucose-6-phosphate dehydrogenase. Circulation 109, 898–903 (2004).
Rehwinkel, J. & Gack, M. RIG-I-like receptors: their regulation and roles in RNA sensing. Nat. Rev. Immunol. 20, 537–551 (2020).
Yu, H. et al. LARP7 protects against heart failure by enhancing mitochondrial biogenesis. Circulation 143, 2007–2022 (2021).
de Bruin, R., Rabelink, T., van Zonneveld, A. & van der Veer, E. Emerging roles for RNA-binding proteins as effectors and regulators of cardiovascular disease. Eur. Heart J. 38, 1380–1388 (2017).
Goubau, D. et al. Antiviral immunity via RIG-I-mediated recognition of RNA bearing 5’-diphosphates. Nature 514, 372–375 (2014).
Dhir, A. et al. Mitochondrial double-stranded RNA triggers antiviral signalling in humans. Nature 560, 238–242 (2018).
Das, S. et al. The Extracellular RNA Communication consortium: establishing foundational knowledge and technologies for extracellular RNA research. Cell 177, 231–242 (2019).
Sorrentino, A. et al. The type I TGF-beta receptor engages TRAF6 to activate TAK1 in a receptor kinase-independent manner. Nat. Cell Biol. 10, 1199–1207 (2008).
Dhingra, R. et al. Proteasomal degradation of TRAF2 mediates mitochondrial dysfunction in doxorubicin-cardiomyopathy. 146, 934–954, https://doi.org/10.1161/circulationaha.121.058411 (2022).
Li, J. et al. TRAF2 protects against cerebral ischemia-induced brain injury by suppressing necroptosis. Cell Death Dis. 10, 328 (2019).
Häcker, H., Tseng, P. H. & Karin, M. Expanding TRAF function: TRAF3 as a tri-faced immune regulator. Nat. Rev. Immunol. 11, 457–468 (2011).
Xu, W. et al. TRAF5 protects against myocardial ischemia reperfusion injury via AKT signaling. Eur. J. Pharmacol. 878, 173092 (2020).
Buskiewicz, I. A. et al. Reactive oxygen species induce virus-independent MAVS oligomerization in systemic lupus erythematosus. Sci. Signal. 9, ra115 (2016).
Shvedova, M., Anfinogenova, Y., Atochina-Vasserman, E. N., Schepetkin, I. A. & Atochin, D. N. c-Jun N-Terminal Kinases (JNKs) in Myocardial and Cerebral Ischemia/Reperfusion Injury. Front. Pharmacol. 9, 715 (2018).
Ren, Z. et al. Regulation of MAVS expression and signaling function in the antiviral innate immune response. Front. Immunol. 11, 1030 (2020).
Mills, E. L., Kelly, B. & O’Neill, L. A. J. Mitochondria are the powerhouses of immunity. Nat. Immunol. 18, 488–498 (2017).
Landström, M. The TAK1-TRAF6 signalling pathway. Int. J. Biochem. Cell Biol. 42, 585–589 (2010).
Wang, C. et al. TAK1 is a ubiquitin-dependent kinase of MKK and IKK. Nature 412, 346–351 (2001).
Ferrandi, C. et al. Inhibition of c-Jun N-terminal kinase decreases cardiomyocyte apoptosis and infarct size after myocardial ischemia and reperfusion in anaesthetized rats. Br. J. Pharmacol. 142, 953–960 (2004).
Zhong, B. & Shu, H. B. MITA/STING-mediated antiviral immunity and autoimmunity: the evolution, mechanism, and intervention. Curr. Opin. Immunol. 78, 102248 (2022).
Liu, S. et al. Phosphorylation of innate immune adaptor proteins MAVS, STING, and TRIF induces IRF3 activation. Science 347, aaa2630 (2015).
Merten, O. W., Hebben, M. & Bovolenta, C. Production of lentiviral vectors. Mol. Ther. Methods Clin. Dev. 3, 16017 (2016).
Ackers-Johnson, M. et al. A simplified, Langendorff-Free method for concomitant isolation of viable cardiac myocytes and nonmyocytes from the adult mouse heart. Circ. Res. 119, 909–920 (2016).
Groseth, A. et al. The Ebola virus glycoprotein contributes to but is not sufficient for virulence in vivo. PLoS Pathog. 8, e1002847 (2012).
Acknowledgements
This work has been financially supported by the Noncommunicable Chronic Diseases-National Science and Technology Major Project (2023ZD0509900 to R.Z.), National Key Research and Development plan (2023YFC2307003 to R.Z.), National Natural Science Foundation of China (Nos. 82274317, 82474287 to D.H., 82070136 to S.L., 82305194 to Y.D.), the Postdoctoral Science Foundation of China (2020T130040ZX to Z.K.; 2023M73122 to Y.D.), the Foundation of Hubei Key Laboratory of Biological Targeted Therapy (2023swbx017 to Z.K.), Deutsche Forschungsgemeinschaft (DFG, MO 3054/1-1 to S.K.M., SFB1123-Z1 to S.K.M., YI 133/3-5 to C.Y., HA 1083/15-5 to A.J.R.H.), ERA-CVD (PLAQUEFIGHT 01KL1808) to A.J.R.H., and Corona Foundation grant (S199/10087/2022) to S.K.M.
Author information
Authors and Affiliations
Contributions
Z.K. designed and performed the experiments, analyzed the data, and drafted the manuscript. M.Y. performed the in vitro and in vivo experiments. Y.L. participated in the study design and paper writing. C.Y.Y., B.L., M.L., Y.G., Y.D., Z.Z., H.Z., and J.J.L. performed some of the in vivo experiments. C.J.Y. and S.K.M. provided critical insights for the study design and revised the manuscript. J.Y.L., H.F., Y.N., Y.W., F.J., K.H., A.S., F.L., G.Z., Z.L., and X.C. gave suggestions for the study design and paper writing. L.Z. provided the MAVS-KO mice. R.Z gave suggestions for the study design and financed the study. D.H., A.J.R.H., and S.L. designed and financed the study, wrote, and edited the manuscript. All authors have read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Communications thanks Stefanie Doppler and the other anonymous reviewers for their contribution to the peer review of this work. A peer review file is available.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Source data
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Kang, Z., Yang, M., Liu, Y. et al. Myocardial mitochondrial antiviral signaling protein promotes heart Ischemia-reperfusion injury via RIG-I signaling in mice. Nat Commun 16, 5101 (2025). https://doi.org/10.1038/s41467-025-60123-7
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41467-025-60123-7
This article is cited by
-
Old dogs-new tricks: multifaceted functions of MAVS beyond antivirus activity in human health and diseases
Cell & Bioscience (2025)
-
Interferon-stimulated gene screening identifies CCND3 as a host restriction factor against emerging high-pathogenic bandaviruses
Nature Communications (2025)
-
Advances in JNK inhibitor development: therapeutic prospects in neurodegenerative diseases and fibrosis
Archives of Pharmacal Research (2025)