Abstract
Spatiotemporally-tailored activation of dendritic cells (DC) in lymph nodes (LN) remains a critical challenge for effective cancer vaccination therapy. In this study, we show that photo/sonodynamic effect can trigger the nuclear transcription factor-kappa B (NF-κB) and stimulator of interferon genes (STING) pathways activation in DC. We engineers a library of spatiotemporally-tailored STING nanoadjuvants (SNA) by conjugating the photo/sonosensitizer and STING agonist onto the biodegradable polypeptide, and co-assembling with charge-modified polypeptides. The combination of antigen-loaded SNA vaccine (SNVac) with laser irradiation or ultrasound stimulation (namely SNVac-L or SNVac-US) efficiently facilitates DC activation and induces antigen-specific CD8+ T cell response in vivo comparing to the free mixture of antigen with STING agonist. We further demonstrate that SNVac-L monotherapy or combination therapy with immune checkpoint blockade (ICB) elicits antitumor immunity to reduce tumor size and prevent tumor relapse in multiple mouse tumor models. This study thus provides a potential translational strategy for spatiotemporally-tailored innate immunity stimulation of DC to potentiate cancer immunotherapy.
Similar content being viewed by others
Introduction
Cancer vaccines hold remarkable potential for tumor eradication and long-term prevention by evoking antitumor immune responses and immune memory1,2,3. Dendritic cells (DC) are considered the professional antigen-presenting cells (APC) to phagocytize and process tumor-associated antigens (TAA), and subsequently prime antigen-specific cytotoxic T lymphocytes (CTL)4,5,6. The activation of intracellular inflammatory and DNA-sensing signaling pathways, including nuclear factor kappa B (NF-kB), cyclic GMP-AMP synthase (cGAS)-stimulator of interferon genes (STING) and Toll-like receptors (TLR) can promote the antigen-presentation profile of DC by upregulating pro-inflammatory cytokine and type I interferon (IFN-I) responses7,8,9,10,11. However, the immune responses induced by small-molecule TLR or STING agonizts is highly impeded by their poor lymph nodes (LN)-targeting profile and rapid blood clearance12,13,14. To address these limitations, various agonist delivery systems, including agonist-integrated nanoadjuvants15,16,17, antibody-agonist conjugates18,19,20, and intrinsic adjuvating nanoparticles21,22,23, have been devised to improve vaccination therapy by activating DC in the secondary lymphoid organs24,25. Despite their therapeutic promise in preclinical settings, most of these strategies are still challenged by the insufficient and uncontrollable innate immune stimulation profile in vivo26,27,28,29,30, thereby leading to ineffective spatiotemporal orchestration of antigen cross-presentation with innate immune stimulation in DC, and ultimately limiting the antigen-specific T-cell activation.
Redox homeostasis of DC markedly influence the magnitude and persistence of innate immune response31,32. Moderate intracellular reactive oxygen species (ROS) generation can promote STING pathway activation in DC through metabolic regulation of SUMO-specific protease 3 (SENP3) activity33. However, excessive ROS accumulation can induce abnormal lipid accumulation to impair the antigen presentation capacity of DC34. Given the graded dose-effect of ROS on immune function of DC, it is of high priority to precisely tailor redox homeostasis of DC to enhance innate immune activation and subsequent T-cell activation. Non-invasive manipulation of intratumoral antitumor immunity by external physical stimuli (e.g., laser, ultrasound, magnetic field) have been pursued as attractive strategies for precise cancer immunotherapies35,36,37,38. However, it remains a formidable challenge to non-invasively modulate redox homeostasis of DC in LN, and how to achieve spatiotemporally-tailored orchestration of antigen cross-presentation with efficient innate immune stimulation in DC remains largely unknown.
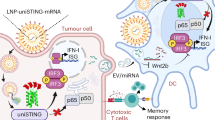
In this work, we first demonstrate that photo/sonodynamic effect can spatiotemporally control the activation of NF-κB and STING pathways in DC through modulating redox homeostasis. We next engineer a library of STING nanoadjuvants (SNA) by conjugating STING agonist onto the photo/sonosensitive polypeptide, and then co-assembling with a set of charge-modified polypeptides. The top-performed SNA with the highest LN-targeting efficacy is further employed for developing STING nanovaccine (SNVac) by loading various types of tumor antigens. Combination treatment of SNVac with LN-localized laser irradiation or ultrasound stimulation (namely SNVac-L or SNVac-US) effectively improves the magnitude and persistence of innate immune responses, and ultimately induces robust and durable antitumor T-cell responses. We further demonstrate that SNVac-L monotherapy or combination therapy with immune checkpoint blockade (ICB) can markedly suppress tumor growth and prevent post-operative tumor relapse in multiple mouse tumor models, including orthotopic liver tumor and breast tumor models.
This study rationally combines the laser or ultrasound stimuli-activatable photo/sonodynamic effects for vaccine adjuvant design, and achieves spatiotemporal orchestration of antigen cross-presentation with innate immune pathways activation in DC, which is crucial for subsequent antigen-specific T cell activation. Since the photo/sonodynamic therapy has been widely utilized for cancer treatment in the clinic, the spatiotemporally-tailored nanoadjuvants can represent a highly translational strategy to exploit laser or ultrasound-guided technique to facilitate region-confined innate immunity stimulation, and thus implement safe and potent cancer vaccination therapy.
Results
Laser or ultrasound-tailored redox homeostasis modulation stimulated innate immune pathways in DC
Inspired by the ability of photo/sonodynamic effect to spatiotemporally tailor ROS generation in target cells39,40, we sought to utilize laser or ultrasound-tailored photo/sonodynamic effect to precisely modulate redox homeostasis of DC. To fabricate the photo/sonosensitive nanovector (PSN) for laser or ultrasound-tailored ROS generation in DC (Fig. 1a), we first synthesized a biodegradable polypeptide (methoxy poly(ethylene glycol)-block-poly-tyrosine, mPEG-b-PTyr) by ring-opening polymerization (ROP) of L-tyrosine N-carboxyanhydrides (NCA). A potent photo/sonosensitizer, pyropheophorbide-a (PPa), was covalently conjugated onto the biodegradable polypeptide (Supplementary Figs. 1, 2).
a Schematic illustration for laser or ultrasound-tailored innate immunity activation in DC by stimulating the NF-κB and STING signaling pathways. IFN-I, Type I interferon. b, c ELISA-determined TNF-α and IL-6 secretion by BMDC after PSN-L or PSN-US treatment (n = 3 biologically independent replicates). The experiment was repeated three times independently with similar results. d Heatmap of the DEG in BMDC after PSN-L treatment (n = 3 biologically independent replicates). The experiment was repeated twice independently with similar results. e GSEA for the altered gene sets in PSN-L group versus PBS group. f Western blot analysis of NF-κB pathway activation in BMDC after PSN-L or PSN-US treatment (n = 3 biologically independent replicates). The experiment was repeated twice independently with similar results. g, h ELISA-determined TNF-α and IL-6 secretion by BMDC after PSN-L + JSH23 or PSN-US + JSH23 treatment (n = 3 biologically independent replicates). The experiment was repeated twice independently with similar results. i Western blot analysis of STING pathway activation in BMDC after PSN-L or PSN-US treatment (n = 3 biologically independent replicates). The experiment was repeated twice independently with similar results. j, k The ISG response produced in RAW264.7-ISG-Luc and THP-1-ISG-Blue cells after PSN-L or PSN-US treatment (n = 3 biologically independent replicates). The experiment was repeated three times independently with similar results. l ELISA-determined IFN-β secretion by BMDC after STINGa + SNA-L or STINGa + SNA-US treatment (n = 3 biologically independent replicates). The experiment was repeated twice independently with similar results. m Western blot analysis of STING pathway activation in BMDC after STINGa + PSN-L or STINGa + PSN-US treatment (n = 3 biologically independent replicates). The experiment was repeated twice independently with similar results. Unless specified otherwise, the data are presented as mean ± SD. Statistical significance was calculated via unpaired two-tailed Student’s t-test (l) or one-way ANOVA with Tukey’s test (b−k), and P-values were indicated. Source data are provided as a Source Data file. The elements in Fig. 1a were created by Adobe Photoshop.
The ROS generation profile of PSN is strictly controlled by the concentration of photo/sonosensitizer, as well as the intensity and duration of laser irradiation or ultrasound stimulation. The high intensity of laser irradiation or ultrasound stimulation can induce additional thermal or mechanical effects to interfere the ROS-mediated innate immune stimulation. Therefore, we selected a low intensity and short duration of laser irradiation (671 nm, 50 mW/cm2, 1 min) or ultrasound stimulation (1 MHz, 0.2 W/cm2, 1 min, 50% duty cycle). In this case, we altered the concentration of photo/sonosensitizer to generate different intracellular ROS levels in bone marrow-derived DC (BMDC) and bone marrow-derived macrophages (BMDM), and then examined the cell viability to screen out the appropriate concentration of photo/sonosensitizer. The result showed that there was no obvious cytotoxicity observed in BMDC or BMDM upon laser irradiation or ultrasound stimulation at the PPa concentration below 1.0 μg/mL (Supplementary Fig. 3).
We subsequently selected the corresponding intensity, duration of laser irradiation or ultrasound stimulation and concentration of photo/sonosensitizer for analyzing the effect and mechanism of ROS generation on innate immune activation of DC. PSN treatment followed with laser irradiation or ultrasound stimulation (namely PSN-L or PSN-US) induced 3.5 or 3.0-fold higher intracellular ROS level in DC, respectively (Supplementary Fig. 4a). It was worth noting that PSN-L or PSN-US significantly triggered the expression of co-stimulatory molecules on DC, with 3.1 or 3.8-fold higher CD80 expression level compared to PSN treatment, respectively (Supplementary Fig. 4b, c). In addition, PSN-L or PSN-US remarkably increased the secretion levels of pro-inflammatory cytokines by DC, including tumor necrosis factor-α (TNF-α) and interleukin-6 (IL-6) (Fig. 1b, c). These data suggested that laser or ultrasound-tailored ROS generation in DC could activate innate immune responses in vitro.
To elucidate the underlying mechanism of intracellular ROS generation on innate immune activation of DC, we examined the transcriptomic features of PSN-L-treated BMDC, and identified 1991 differently expressed genes (DEG) compared to PBS group (Supplementary Fig. 5a). PSN-L-treated DC showed increased expression of immune-related genes (Tnfrsf12, H2-K1, CXCL10 and IL6) (Fig. 1d). The DEG were enriched in immune-associated signaling pathways and cytokine signaling pathways by KEGG enrichment analysis (Supplementary Fig. 5b). Gene set enrichment analysis (GSEA) further identified that the DEG were enriched in NF-κB signaling pathway and cytosolic DNA-sensing signaling pathway (Fig. 1e), implying the activation of the pro-inflammatory immune responses41,42. Western blot assay further verified that PSN-L or PSN-US treatment promoted phosphorylation of NF-κB subunit p65 (p-P65) protein in DC (Fig. 1f). The addition of NF-κB nucleus translocation inhibitor, JSH23, significantly impaired the effect of PSN-L or PSN-US to stimulate TNF-α and IL-6 secretion by DC (Fig. 1g, h), validating that PSN-L or PSN-US activated NF-κB signaling pathway in DC.
Intracellular ROS generation has been demonstrated to induce endoplasmic reticulum stress and trigger cytosolic DNA release43,44. STING is a critical cytosolic pattern recognition receptor for sensing cytosolic DNA and initiating innate immune response45,46. Western blot assay displayed that PSN-L or PSN-US activated STING signaling pathway in DC by promoting phosphorylation of TANK-binding kinase-1 (TBK1) and interferon regulatory factor-3 (IRF3) proteins (Fig. 1i). Furthermore, PSN-L or PSN-US obviously elicited type-I interferon (IFN-I)-related genes (ISG) expression in RAW264.7-ISG-Luc and THP1-ISG-Blue cells, respectively (Fig. 1j, k). Notably, the addition of ROS scavenger, N-acetyl-l-cysteine (NAC), suppressed PSN-L-elicited DC maturation and ISG expression (Supplementary Fig. 6), indicating that PSN-L or PSN-US modulated redox homeostasis of DC to activate innate immune responses.
We further investigated whether laser or ultrasound-tailored ROS generation could enhance the STING agonist (STINGa) activity in DC for amplifying STING signaling pathway activation and IFN-I production. In the presence of a model STINGa, MSA-2, PSN-L or PSN-US treatment 10.2 and 15.0-fold more efficiently promoted IFN-β secretion, respectively, which led to increased DC maturation compared with mono STINGa treatment (Fig. 1l and Supplementary Fig. 7). Western blot assay revealed that PSN-L or PSN-US promoted phosphorylation of TBK1 and IRF3 proteins in STINGa-treated DC (Fig. 1m). The addition of JSH23 also remarkably reversed the effect of PSN-L or PSN-US to promote IFN-β secretion from STINGa-treated DC (Supplementary Fig. 8). These data collectively validated that laser or ultrasound-tailored redox homeostasis modulation could augment the activation of NF-kB and STING signaling pathways in DC, representing a promising approach for spatiotemporally-tailored innate immunity stimulation.
Engineering STING nanoadjuvants for laser or ultrasound-tailored innate immunity stimulation in LN
LN serve as the dominant secondary lymphoid organs, where a substantial population of APC reside to recognize innate immune stimuli and initiate protective immune responses against cancer and infections47,48. We sought to engineer a library of STING nanoadjuvants (SNA) to implement laser or ultrasound-tailored innate immunity stimulation in LN, for inducing safe and robust antitumor immune responses. The STINGa was covalently conjugated onto the backbone of mPEG-b-PTyr-PPa polypeptide to obtain STINGa-conjugated polypeptide (SAP) (Supplementary Fig. 9). We next synthesized a set of charge-modified polypeptides (CMPn) (Supplementary Figs. 10–13), which were co-assembled with SAP to obtain a series of STING nanoadjuvants (SNA1-13) displaying particle size ranging from 108.1 nm to 168.4 nm and surface charge ranging from -44.2 mV to + 30.1 mV (Fig. 2a).
a Schematic illustration for engineering of the SNA library with tunable physicochemical properties for laser or ultrasound-tailored innate immunity activation in the idLN. b Representative fluorescence images of the idLN and major organs examined at 12 h post SNA1-13 injection (n = 3 biologically independent mice). The experiment was repeated twice independently with similar results. c Semi-quantification of the fluorescence signal in the idLN at 12 h post SNA1-13 injection. (n = 3 biologically independent mice). The experiment was repeated twice independently with similar results. d The absolute number of CD11c+ DC and the CD86 expression level of DC in the idLN after SNA treatment followed with indicated conditions of laser irradiation (n = 3 biologically independent mice). The experiment was repeated twice independently with similar results. e The absolute number of CD11c+ DC and the CD86 expression level of DC in the idLN after SNA treatment followed with indicated conditions of ultrasound stimulation (n = 3 biologically independent mice). The experiment was repeated twice independently with similar results. f The absolute number of CD11c+ DC and CD11b+ macrophages in the iLNs after indicated treatments (n = 3 biologically independent mice). The experiment was repeated twice independently with similar results. g The maturation levels of CD11c+ DC and CD11c+CD8α+ DC in the iLNs after indicated treatments (n = 3 biologically independent mice). The experiment was repeated twice independently with similar results. h The IFN-β and IL-12P70 production in the idLN after SNA or SNA-L treatment (n = 3 biologically independent mice). The experiment was repeated twice independently with similar results. i The IFN-β and IL-12P70 production in the idLN after SNA or SNA-US treatment (n = 3 biologically independent mice). The experiment was repeated twice independently with similar results. Unless specified otherwise, the data are presented as mean ± SD. Statistical significance was calculated via unpaired two-tailed Student’s t-test (h, i) and P-values were indicated. Source data are provided as a Source Data file. The elements in Fig. 2a were created by Adobe Photoshop.
To optimize the LN-targeting efficacy of SNA library, SNA1-13 were subcutaneously injected into the tail base of mice. Ex-vivo fluorescence imaging displayed that SNA1-13 effectively accumulated in inguinal draining LN (idLN) with minimal distribution in major organs (heart, liver, spleen, lung and kidney) (Fig. 2b and Supplementary Fig. 14). Semi-quantification of fluorescence signal screened out the SNA4 nanoadjuvant, with an averaged particle size of 135.0 nm and a surface charge of +10.2 mV, exhibited the highest idLN-targeting efficacy (unless noted, all SNA mentioned below refer to SNA4) (Fig. 2c). We also examined the biodistribution of SNA in tumor-bearing mice, and found that SNA effectively accumulated into idLN at 12 h post injection, while marginally accumulated into tumor tissues (Supplementary Fig. 15).
We next investigated which types of conventional DC (cDC) or macrophages in idLN mainly take up the SNA. The result showed that the CD8α+CD11c+ resident cDC1 could effectively uptake the nanoadjuvant, while the CD103+CD11c+ migratory cDC1 and CD11b+CD11c+ cDC2 showed significantly lower uptake efficiency. The frequency of SNA+ in CD8α+ cDC1, CD103+ cDC1 and CD11b+ cDC2 was about 18.2%, 4.64% and 1.58%, respectively. Notably, we found the CD169+ SCS macrophages also participated in the uptake of SNA, and the frequency of SNA+ in CD169+ SCS macrophages was about 8.33%. (Supplementary Fig. 16). We also investigated the cell-specificity of SNA in idLN of tumor-bearing mice, and similar cell-targeting profiles were observed (Supplementary Fig. 17). These results demonstrated that SNA effectively targeted the CD8α+ resident cDC1 rather than the CD103+ migratory cDC1 or cDC2 in idLN.
We next investigated whether the spatiotemporal control of laser irradiation or ultrasound stimulation could amplify SNA-mediated innate immune responses in idLN. The idLN of mice were locally irradiated with different power intensity of 671 nm laser (0, 100, 200, 300 mW/cm2) or stimulated with different power intensity of ultrasound (0, 0.5, 1.0, 1.5 W/cm2) at 3 h, 6 h or 12 h post SNA injection. The findings demonstrated that at 6 h post SNA injection, 200 mW/cm2 of laser irradiation or 1.0 W/cm2 of ultrasound stimulation effectively enhanced SNA-mediated innate immune responses, and elicited the highest levels of DC recruitment and maturation in idLN (Fig. 2d, e). Laser irradiation or ultrasound stimulation alone showed no obvious immune stimulatory effect, and only marginally affected DC recruitment and maturation in idLN. SNA injection moderately increased the absolute number of CD11c+ DC and CD11b+ macrophages in idLN, as well as increased the maturation levels of CD11c+ DC and CD11c+CD8α+ DC. In contrast, the combination of SNA with idLN-localized laser irradiation or ultrasound stimulation (namely SNA-L or SNA-US) sustainedly promoted DC recruitment and maturation over 5 days (Fig. 2f, g and Supplementary Fig. 18). In addition, compared with SNA injection that only induced short-lived production of IFN-I and proinflammatory cytokine in idLN, SNA-L or SNA-US induced abundant and sustained IFN-β and IL-12P70 secretion for over 48 h (Fig. 2h, i).
Given the potent ability of SNA-L and SNA-US to activate innate immunity in idLN, we next examined their performance to elicit intratumoral antitumor immunity (Fig. 3a and Supplementary Fig. 19). SNA injection moderately increased the tumor-infiltration levels of CD8+ T cells and IFN-γ+CD8+ T cells, while SNA-L and SNA-US both enhanced the CD8+ T cells and IFN-γ+CD8+ T cells infiltration into tumors (Fig. 3b, c). The frequency of IFN-γ+ in CD8+ T cells in SNA-L and SNA-US groups were 3.8 and 4.2-fold higher than the PBS group, respectively (Supplementary Fig. 20a, b). In addition, SNA-L and SNA-US not only decreased the frequency of tumor-infiltrating regulatory T cells (Treg) (Fig. 3g and Supplementary Fig. 20c), but also alleviated the suppressive function of Treg, as indicated by the decrease of IL10+ Treg and IL4+ Treg when compared with PBS group (Fig. 3h, i and Supplementary Fig. 20d, e). Moreover, SNA-L and SNA-US remarkably decreased the frequency of tumor-infiltrating M2-type tumor-associated macrophages (TAM), while increased the frequency of M1-type TAM (Fig. 3d–f and Supplementary Fig. 20f). In contrast, laser irradiation or ultrasound stimulation alone marginally activated intratumoral immune responses.
a Experimental schedule for evaluating the antitumor immunity induced by SNA-L or SNA-US in 4T1 tumor-bearing mice in vivo. b Quantitative analysis of the frequency of CD8+ T cells in tumor (CD8+ in CD3+CD45+ cells) (n = 5 biologically independent mice). c Quantitative analysis of the frequency of IFN-γ+CD8+ T cells in tumor (IFN-γ+ in CD8+CD3+CD45+ cells) (n = 5 biologically independent mice). d Quantitative analysis of the frequency of M1-TAM in tumor (CD86+ in F4/80+CD11b+CD45+ cells) (n = 5 biologically independent mice). e Quantitative analysis of the frequency of M2-TAM in tumor (CD206+ in F4/80+CD11b+CD45+ cells) (n = 5 biologically independent mice). f Quantitative analysis of the ratio of M1-TAM to M2-TAM in tumor (n = 5 biologically independent mice). g Quantitative analysis of the frequency of Treg in tumor (CD25+FOXP3+ in CD4+CD3+CD45+ cells) (n = 5 biologically independent mice). h Quantitative analysis of the frequency of IL-10+ Treg in tumor (IL-10+ in CD25+FOXP3+CD4+CD3+CD45+ cells) (n = 5 biologically independent mice). i, Quantitative analysis of the frequency of IL-4+ Treg in tumor (IL-4+ in CD25+FOXP3+CD4+CD3+CD45+ cells) (n = 5 biologically independent mice). j Averaged 4T1 tumor growth curves and the photographs of the tumors after SNA or SNA-L treatment (n = 6 biologically independent mice). Scale bar = 10 mm. k Averaged 4T1 tumor growth curves and the photographs of the tumors after SNA or SNA-US treatment (n = 6 biologically independent mice). Scale bar = 10 mm. l Western blot analysis of the STING pathway activation in the idLN (n = 3 biologically independent mice). The experiment was repeated two times independently with similar results. m Schematic illustration to show SNA-L-mediated innate immune activation and immune microenvironment reprograming in the idLN. dsDNA, double stranded DNA. n GO enrichment analysis of DEG in the idLN after SNA-L treatment (n = 3 biologically independent mice). The experiment was repeated twice independently with similar results. o KEGG enrichment analysis of DEG in the idLN after SNA-L treatment (n = 3 biologically independent mice). The experiment was repeated twice independently with similar results. p Heatmap of DEG in tdLN after SNA-L treatment (n = 3 biologically independent mice). The experiment was repeated twice independently with similar results. Unless specified otherwise, the data are presented as mean ± SD. Statistical significance was calculated via one-way ANOVA (b−k) with Tukey’s test, and P-values were indicated. Source data are provided as a Source Data file. The elements in Fig. 3a were created by Adobe Illustrator, and the elements in Fig. 3m were created by Adobe Photoshop.
We next examined the performance of SNA-L or SNA-US to inhibit established tumor growth in different tumor-bearing mouse models. SNA injection moderately delayed the progression of CT26 colorectal tumor and 4T1 breast tumor, and only inhibited CT26 tumor growth and 4T1 tumor growth by 53.1% and 45.1%, respectively. In contrast, SNA-L inhibited 85.4% of CT26 tumor growth and 80.0% of 4T1 tumor growth (Fig. 3j and Supplementary Figs. 21, 22). Similar results were observed in SNA-US treatment, and SNA-US inhibited MC38 tumor growth and 4T1 tumor growth by 74.8% and 74.6%, respectively, while SNA injection only moderately inhibited tumor growth (Fig. 3k and Supplementary Figs. 23, 24).
To elucidate the mechanism of antitumor immunity induced by SNA-L in vivo, we examined the innate and adaptive immune responses in idLN. The findings showed that SNA-L treatment more efficiently promoted DC influx into idLN and induced DC maturation compared to SNA treatment (Supplementary Fig. 25a). Similar trends were observed in the influx of CD11b+ macrophages and CD3+ T cells into idLN (Supplementary Fig. 25b). In addition, compared with SNA treatment, SNA-L treatment not only increased the percentage of activated CD8+ T cells (Supplementary Fig. 25c), but also decreased the percentage of Treg and M2-type macrophages in idLN (Supplementary Fig. 25d, e). Western blot assay further indicated that SNA-L treatment more efficiently activated STING signaling pathway in idLN (Fig. 3l).
We next evaluated the transcriptomic features of idLN collected from SNA-L-treated mice, and identified 737 DEG compared to that of SNA group mice (Supplementary Fig. 26a). SNA-L treatment upregulated the immune-activation-related genes (Ccl4, Ccl2, Igfbp6, and Tnfaip6) and downregulated the immune-suppression-related genes (Foxp3, Tgfbr1, Smad4 and CD274) (Fig. 3p). Most DEG were enriched in immune response-associated signaling pathways and cytokine signaling pathways (Fig. 3n and Supplementary Fig. 26b). Moreover, KEGG enrichment analysis identified that DEG were enriched in multiple immune-response-associated signaling pathways, such as cytokine-cytokine receptor interaction and chemokine signaling pathway (Fig. 3o). Collectively, these results demonstrated that SNA-L provided a spatiotemporally-tailored strategy for innate immunity stimulation in idLN and eliciting potent antitumor immune responses (Fig. 3m).
Combination of STING nanovaccine (SNVac) with laser irradiation elicited robust T-cell immunity
Spatiotemporal orchestration of antigen cross-presentation with efficient innate immune stimulation in DC is critical for inducing robust antigen-specific T-cell immunity24,25. Therefore, we sought to explore the potential of STING nanoadjuvant as an antigen delivery platform for spatiotemporally-tailored antigen cross-presentation and T-cell activation (Fig. 4a). The protein antigen ovalbumin (OVA) was loaded into STING nanoadjuvant via electrostatic interaction to prepare STING nanovaccine (SNVac). The antigen loading ratio and encapsulation efficiency were determined to be about 12.3% and 87.5%, respectively (Supplementary Fig. 27a). DLS and TEM analysis revealed that SNVac exhibited a uniform spherical morphology, with an averaged particle size of 135.1 nm and a surface charge of +6.6 mV (Fig. 4b, c and Supplementary Fig. 27b).
a Schematic illustration to show the preparation of SNVac for spatiotemporally-tailored antigen cross presentation with innate immune stimulation. b, c DLS analysis and representative TEM images of SNVac. OVA was selected as the model antigen (n = 3 biologically independent replicates). The experiment was repeated three times independently with similar results. Scale bar = 500 nm. d Representative CLSM images to show the SNVac distribution in DC. OVA was labeled with FITC (green), the nuclei and endosome were stained with DAPI (blue) and Lyso-Tracker (red), respectively (n = 3 biologically independent replicates). The experiment was repeated twice independently with similar results. Scale bars = 10 μm. e Quantitative analysis of the frequency of matured BMDC (CD86+ in CD11c+ cells) (n = 3 biologically independent replicates). The experiment was repeated three times independently with similar results. f The secretion of IFN-β in the supernatant of BMDC (n = 3 biologically independent replicates). The experiment was repeated three times independently with similar results. g Quantitative analysis of the frequency of antigen-presented DC (SIINFEKL-H2Kb+ in CD11c+ cells) (n = 3 biologically independent replicates). The experiment was repeated three times independently with similar results. h Quantitative analysis of the proliferation level of T cells after co-cultured with BMDC (n = 3 biologically independent replicates). The experiment was repeated twice independently with similar results. i Representative fluorescence images and signal quantification of the idLN after free OVA or SNVac injection (n = 3 biologically independent mice). The experiment was repeated twice independently with similar results. j Representative fluorescence micrographs of the idLN at 6 h after SNVac injection (n = 3 biologically independent mice). The experiment was repeated twice independently with similar results. Scale bars = 100 μm. k Quantitative analysis of the cellular uptake of SNVac by CD11c+ DC and CD11b+ macrophages in the idLN (n = 3 biologically independent mice). The experiment was repeated twice independently with similar results. l Experimental timeline for the evaluation of SNVac-L-elicited antigen-specific immune response in vivo. m Quantitative analysis of the frequency of activated macrophages (CD80+CD86+ in CD11b+ cells) in the idLN (n = 5 biologically independent mice). n Quantitative analysis of the frequency of matured DC (CD80+CD86+ in CD11c+ cells) in the idLN (n = 5 biologically independent mice). o Quantitative analysis of the frequency of antigen-presented DC (SIINFEKL-H2Kb+ in CD11c+ cells) in the idLN (n = 5 biologically independent mice). p Quantitative analysis of the frequency of antigen-specific T cells (SIINFEKL-H2Kb tetramer+ in CD3+CD8+ cells) in the spleen (n = 5 biologically independent mice). q Quantitative analysis of the OVA-specific killing effect in vivo (n = 5 biologically independent mice). The ratio of CFSEhigh to CFSElow cells reflects the level of OVA-specific antitumor immunity. r Heatmap of the secretion of TNF-α and IFN-γ by splenocytes after re-stimulation by SIINFEKL peptide (n = 5 biologically independent mice). s Schematic illustration of the SNVac-L-induced antigen cytosolic release and STING pathway activation to promote antigen cross-presentation and T-cell activation. Unless specified otherwise, the data are presented as mean ± SD. Statistical significance was calculated via unpaired two-tailed Student’s t-test (i, k) or one-way ANOVA with Tukey’s test (e−h, m−q), and P-values were indicated. Source data are provided as a Source Data file. The elements in Fig. 4l were created by Adobe Illustrator, and the elements in Fig. 4a, s were created by Adobe Photoshop.
We next employed a FITC-labeled OVA (OVA-FITC) to detect the intracellular distribution of antigen in DC. Flow cytometry analysis revealed that DC showed marginal uptake of free OVA-FITC due to the poor membrane permeability of antigen. In contrast, SNVac effectively promoted cellular uptake of antigen by DC, and exhibited 3.8-fold higher OVA-FITC uptake efficiency than free OVA-FITC group at 8 h post incubation (Supplementary Fig. 27c). However, it was worth noting that most of the antigen signal (green) in SNVac group was co-localized with the lysosome signal (red), and failed to promote antigen cytosolic release (Fig. 4d). In contrast, the combination of SNVac with 671 nm laser irradiation (namely SNVac-L, 50 mW/cm2, 1 min) significantly facilitated the lysosomal escape of antigen and achieved efficient antigen cytosolic release in DC. This could be attributed to the increase of lysosomal membrane permeability, as validated by the acridine orange staining and Bio-TEM images of SNVac-L-treated DC in vitro (Supplementary Fig. 28).
Based on the remarkable ability of SNVac-L to promote cytosolic delivery of antigen, we next evaluated the performance of SNVac-L to enhance antigen cross-presentation and T-cell activation in vitro. We found that SNVac-L not only induced the highest level of DC maturation among all the treatment groups, but also effectively promoted IFN-β secretion by DC, displaying about 3.6 and 1.4-fold higher than the OVA+MSA-2 and SNVac groups, respectively (Fig. 4e, f and Supplementary Fig. 29a). Flow cytometry analysis revealed that SNVac-L elicited the highest level of antigen presentation on the surface of DC among all the treatment groups, and displayed about 2.5 and 1.7-fold higher percentage of antigen-presented DC than the OVA+MSA-2 and SNVac groups, respectively (Fig. 4g and Supplementary Fig. 29b). CLSM examination further confirmed the remarkable capacity of SNVac-L to promote antigen presentation on the surface of DC (Supplementary Fig. 29c). Moreover, SNVac-L-treated DC showed the highest effect to promote T cell proliferation, and the secreted IFN-γ and TNF-α by T cells in SNVac-L group were about 1.6 and 1.9-fold higher than the SNVac group, respectively (Fig. 4h and Supplementary Fig. 30). Collectively, SNVac-L utilized the laser-tailored ROS generation effect to synchronously promote antigen cytosolic release and NF-κB/STING pathways activation, thus ensuring the spatiotemporal orchestration of antigen cross-presentation with innate immune stimulation in DC to promote T-cell activation.
We next investigated the idLN-targeting efficacy of SNVac in vivo by utilizing the fluorescence imaging capacity of photo/sonosensitizer. Upon subcutaneous injection at the tail base of mice, SNVac could effectively accumulate into idLN and display a gradual increase of fluorescence signal in idLN over time, which peaked at 6 h post injection (Supplementary Fig. 31). We also examined the performance of SNVac for idLN-targeting delivery of tumor antigen in vivo by utilizing the fluorescence imaging capacity of OVA-FITC. Ex-vivo fluorescence imaging displayed minimal distribution of OVA-FITC in idLN in free OVA-FITC group mice. In contrast, SNVac effectively delivered antigen into idLN and exhibited about 5.1-fold higher OVA-FITC signal than free OVA-FITC group at 6 h post injection (Fig. 4i). CLSM examination of idLN section further confirmed the remarkable idLN-targeting antigen delivery efficacy of SNVac (Fig. 4j). Flow cytometry analysis also demonstrated that SNVac 4.0 and 3.1-fold more efficiently delivered antigen to DC and macrophages in idLN than free OVA-FITC group, respectively (Fig. 4k).
We next examined the antigen-specific immune responses induced by SNVac-L in vivo. C57BL/6 mice were vaccinated with SNVac three times at a 7 day interval, followed with idLN-localized laser irradiation (671 nm, 200 mW/cm2, 5 min) at 6 h post per vaccination (Fig. 4l). We found that SNVac-L dramatically promoted the influx of CD11c+ DC, CD11b+ macrophages and CD3+ T cells into idLN (Supplementary Fig. 32d), and triggered the expression of stimulatory markers (CD80, CD86) in DC and macrophages (Fig. 4m, n and Supplementary Fig. 32a, b). In addition, SNVac-L induced the highest level of antigen presentation on the surface of DC, and displayed about 1.6-fold higher percentage of antigen-presented DC than SNVac group (Fig. 4o and Supplementary Fig. 32c). To demonstrate which types of DC were primarily responsible for cross-presenting antigen after SNVac-L treatment, we analyzed the antigen presentation level of CD8α+CD11c+ resident cDC1 and CD103+CD11c+ migratory cDC1 in idLN. We found that SNVac-L treatment markedly promoted antigen cross-presentation by CD8α+ cDC1, and the SIINFEKL-H2Kb expression level exhibited 3.8-fold increase compared with PBS group (Supplementary Fig. 33a). Although the antigen presentation level of CD103+ cDC1 was also increased after SNVac-L treatment, the frequency of SIINFEKL-H2Kb+ in CD103+ DC was only 1.6-fold higher than that of PBS group (Supplementary Fig. 33b). Therefore, CD8α+ cDC1 may played a more essential role in antigen cross-presentation after SNVac-L treatment. We subsequently analyzed the antigen-specific CD8+ T cell response induced by SNVac-L, and found that SNVac-L 17.8 and 4.0-fold more efficiently elicited SIINFEKL-H2Kb tetramer+CD8+ T cell response than OVA+CpG and SNVac groups, respectively (Fig. 4p and Supplementary Fig. 34a). Upon ex-vivo restimulation with SIINFEKL peptide, the splenocytes collected from SNVac-L group mice displayed the highest secretion levels of IFN-γ and TNF-α among all the groups (Fig. 4r and Supplementary Fig. 34c). Furthermore, we performed a cytotoxicity killing assay to detect the antigen-specific cytotoxic T cell response generated by SNVac-L. The result showed that SNVac-L group mice produced the highest antigen-specific cytotoxic T cell response among all the groups, displaying an OVA-specific killing effect reaching over 80% (Fig. 4q and Supplementary Fig. 34b).
SNVac-L reshaped tumor immune microenvironment to suppress established tumor growth
Given the promising efficacy of the SNVac-L to elicit robust T-cell immune response in vivo, we continued to evaluate the therapeutic performance of SNVac-L in established tumor models. C57BL/6 mice were subcutaneously inoculated with B16-OVA cells in the right flank and treated with indicated formulations 7 days later (Fig. 5a). OVA+CpG and OVA+MSA-2 only moderately inhibited tumor growth and all the mice succumbed to tumors within 30 days. SNVac extended the median survival of mice from 16 days (PBS group) to 36 days, while all the mice succumbed to tumors within 40 days (Fig. 5d). In contrast, SNVac-L markedly inhibited tumor growth and prolonged the median survival of mice, with 2/6 of the mice produce complete tumor regression over 60 days (Fig. 5b, c). The body weight of all mice did not change notably when exposed to the current regimen (Supplementary Fig. 35). H&E staining of the tumor sections showed that SNVac-L induced notable apoptosis/necrosis of tumor cells, as indicated by the presence of nuclear collapse and cytoplasmic rupture (Supplementary Fig. 36).
a Experimental schedule for evaluating the therapeutic efficacy of SNVac-L in the B16-OVA tumor model. b, c Averaged B16-OVA tumor growth curves and corresponding survival curves of mice in indicted groups (n = 6 biologically independent mice). d Individual B16-OVA tumor growth curves of mice (n = 6 biologically independent mice). e Quantitative analysis of the frequency of matured DC (CD80+CD86+ in CD11c+ cells) in the idLN (n = 5 biologically independent mice). f Quantitative analysis of the frequency of activated macrophages (CD80+CD86+ in CD11b+ cells) in the idLN (n = 5 biologically independent mice). g Quantitative analysis of the frequency of CD8+ T cells in tumor (CD8+ in CD3+CD45+ cells) (n = 5 biologically independent mice). h Heatmap of the frequency of M1-TAM (CD86+F4/80+CD11b+CD45+) and M2-TAM (CD206+F4/80+CD11b+CD45+) in tumor (n = 5 biologically independent mice). i Quantitative analysis of the frequency of Gzmb+CD8+ T cells in tumor (Gzmb+ in CD8+CD3+CD45+ cells) (n = 5 biologically independent mice). j Quantitative analysis of the frequency of Treg in tumor (FOXP+CD25+ in CD4+CD3+CD45+ cells) (n = 5 biologically independent mice). k Quantitative analysis of the frequency of MDSC in tumor (Ly6C+ in CD11b+CD45+ cells) (n = 5 biologically independent mice). l Heatmap of the intratumoral secretion of TNF-α and TGF-β (n = 5 biologically independent mic). m Immunofluorescence staining of tumor-infiltrating CD8+ T cells (red) and CD4+ T cells (green) (n = 3 biologically independent mice). The experiment was repeated twice independently with similar results. Scale bar = 100 μm. n Experimental schedule for evaluating the influence of CD8+ T cell blockade on antitumor efficacy of SNVac-L in the B16-OVA tumor model. o, p Averaged B16-OVA tumor growth curves and corresponding survival curves of mice after SNVac-L + anti-CD8 treatment (n = 6 biologically independent mice). q Experimental schedule for evaluating the influence of IFNAR blockade on antigen-specific T cell response induced by SNVac-L. r Representative flow cytometry plots and quantitative analysis of the frequency of antigen-specific T cells (SIINFEKL-H2Kb tetramer+ in CD3+CD8+ cells) in the spleen (n = 5 biologically independent mice). Unless specified otherwise, the data are presented as mean ± SD. Statistical significance was calculated via one-way ANOVA with Tukey’s test (b, e−k, o, r) or log-rank (Mantel-Cox) test (c, p) and P-values were indicated. Source data are provided as a Source Data file. The elements in Fig. 5a were created by Adobe Illustrator.
Mechanistic studies were performed to investigate the antitumor immunity induced by SNVac-L in vivo. We found that SNVac-L effectively promoted the maturation of DC and activation of macrophages in idLN (Fig. 5e, f and Supplementary Fig. 37). We next analyzed intratumoral infiltration of different immune cells after SNVac-L treatment (Supplementary Fig. 38). The results showed that the tumor-infiltration level of CD4+ T cells was marginally changed after SNVac-L treatment, while the infiltration levels of CD8+ T cells and NK cells were both significantly increased, showing about 3.4 and 2.0-fold higher than the PBS group, respectively (Fig. 5g and Supplementary Fig. 39). The frequencies of tumor-infiltrating IFN-γ+CD8+ T cells and GZMB+CD8+ T cells were effectively increased after SNVac-L treatment, showing about 2.6 and 3.5-fold higher than the PBS group, respectively (Fig. 5i and Supplementary Fig. 40a, b). In comparison, the frequencies of IFN-γ+ NK cells and IFN-γ+CD4+ T cells were marginally improved after SNVac-L treatment (Supplementary Fig. 40c, d). These findings indicated that cytotoxic CD8+ T cells might play a dominant role for tumor cell killing.
We next measured the tumor-infiltration level and suppressive function of Treg after SNVac-L treatment. Compared with PBS group, SNVac-L treatment significantly decreased the frequency of tumor-infiltrating Treg, and inhibited the production of Treg-derived suppressive cytokines (IL-4, IL-10). The frequencies of tumor-infiltrating IL10+ Treg and IL4+ Treg in SNVac-L group displayed 2.8 and 2.5-fold decrease than PBS group (Fig. 5j and Supplementary Fig. 41). Interestingly, SNVac-L also reversed the immunosuppressive tumor microenvironment by reducing myeloid-derived suppressor cells (MDSC) (Fig. 5k and Supplementary Fig. 42a), and repolarizing tumor-supportive M2-type TAM to the tumor-suppressive M1-type TAM (Fig. 5h and Supplementary Fig. 42b–d). SNVac-L treatment also increased the intratumoral secretion level of TNF-α, while suppressed TGF-β secretion (Fig. 5l and Supplementary Fig. 43). Immunofluorescence staining of tumor sections displayed that SNVac-L treatment significantly promoted the tumor-infiltration of CD8+ T cells compared to SNVac group (Fig. 5m).
To validate the contribution of CD8+ T cell response for SNVac-L therapy, we performed CD8+ T cell blocking experiment through systemic injection of anti-CD8 antibody (αCD8) (Fig. 5n). Almost all CD8+ T cells in spleen were blocked while CD4+ T cells were unaffected (Supplementary Fig. 44a). CD8+ T cells blockade significantly abrogated the antitumor performance of SNVac-L in B16-OVA tumor model (Fig. 5o, p and Supplementary Fig. 44b), indicating the antitumor efficacy of SNVac-L could be mainly attributed to CD8+ T cell activation.
Next, we investigated the role of IFN-I, a pivotal cytokine produced by STING activation, in promoting SNVac-L-mediated antigen-specific T cell response in vivo. We blocked the IFN-I pathway using an antibody against IFN-α receptor (anti-IFNAR) (Fig. 5q), and found that IFNAR blockade dramatically suppressed antigen-specific CD8+ T cell response induced by SNVac-L (Fig. 5r). These results together demonstrated that SNVac-L activated STING-IFN-I pathway to elicit potent CD8+ T-cell immunity, and reverse the immunosuppressive tumor microenvironment.
Combination of membrane antigen-loaded nanovaccine (M-SNVac) with laser irradiation prevented post-operative tumor recurrence and metastasis
Autologous tumor cell membrane antigen-loaded cancer vaccines hold promising potential for personalized cancer immunotherapy49. However, it remains a formidable challenge to elicit robust therapeutic benefits due to the weak immunogenicity of autologous tumor cell membrane antigen, insufficient stimulation of innate immunity and immunosuppressive tumor microenvironment50. To demonstrate the therapeutic potential of SNVac-L for personalized cancer vaccination therapy, we extracted tumor cell membrane (Mem) as the antigen51,52, and selected STING nanoadjuvant as the delivery platform to prepare membrane antigen-loaded nanovaccine (M-SNVac) (Fig. 6a). The co-assembly of M-SNVac was effectively driven by the electrostatic interaction of negatively-charged Mem with positively-charged nanoadjuvant. The B16F10 cell membrane-based M-SNVac displayed a uniform particle size of 159.9 nm and a surface charge of 6.62 mV. The 4T1 cell membrane-based M-SNVac displayed a uniform particle size of 142.9 nm and a surface charge of 8.02 mV (Supplementary Fig. 45). The protein antigen concentration of Mem loaded in M-SNVac was quantified by the bicinchoninic acid assay. Compared to the mixture of Mem with two TLR adjuvants (Mem+CpG+MPLA), the combination of M-SNVac with idLN-localized laser irradiation (namely M-SNVac-L, 200 mW/cm2, 5 min) displayed more potent antitumor efficacy, and inhibited 93.5% of B16F10 tumor growth (Fig. 6b–e).
a Schematic illustration for tumor cell membrane antigen-based M-SNVac preparation and the laser-tailored M-SNVac-L treatment for personalized cancer vaccine therapy. b, c Individual and averaged B16F10 tumor growth curves of mice in indicated groups (n = 6 biologically independent mice). d, e The photographs of collected B16F10 tumors and corresponding tumor weight in indicated groups (n = 6 biologically independent mice). f Experimental schedule for evaluating the therapeutic efficacy of autologous tumor cell membrane antigen-based M-SNVac-L in the postoperative 4T1-Luc tumor model. g Representative bioluminescence images of 4T1-Luc tumor-bearing mice at different time points (n = 6 biologically independent mice). h, i Averaged 4T1-Luc tumor growth curves and corresponding survival curves of mice in indicated groups (n = 6 biologically independent mice). j Representative bioluminescence images and H&E staining images of the lung tissue on day 30 post tumor inoculation. Scale bar = 2 mm. k, l The corresponding quantitative analysis of bioluminescence intensity and absolute number of tumor lung metastatic foci (n = 4 biologically independent mice). The experiment was repeated twice independently with similar results. m−o Representative bioluminescence images, average 4T1-Luc tumor growth curves and corresponding survival curves of mice in the tumor-rechallenge model (n = 4 biologically independent mice). The experiment was repeated twice independently with similar results. p Representative flow cytometry plots and quantitative analysis of the frequency of TCM (CD44+CD62+ in CD8+CD3+ T cells) and TEM (CD44+CD62L− in CD8+CD3+ T cells) in the spleen examined on day 120 post tumor inoculation (n = 4 biologically independent mice). The experiment was repeated twice independently with similar results. Unless specified otherwise, the data are presented as mean ± SD. Statistical significance was calculated via unpaired two-tailed Student’s t-test (p), one-way ANOVA with Tukey’s test (c−l) or log-rank (Mantel-Cox) test (i, o) and P-values were indicated. Source data are provided as a Source Data file. The elements in Fig. 6f were created by Adobe Illustrator, and the elements in Fig. 6a were created by Adobe Photoshop.
We further investigated the therapeutic potential of M-SNVac-L for postoperative immunotherapy of triple negative breast cancer (TNBC), which is an aggressive breast cancer subtype with rapid disease progression and high risk of metastasis53,54. 4T1-Luc cells were subcutaneously inoculated into the right flank of mice, and 90% of tumor tissues were surgically resected when tumor volume reached about 300 mm3. We extracted Mem from collected tumor tissues to prepare M-SNVac. Personalized M-SNVac vaccination, followed with idLN-localized laser irradiation were conducted three times at 7 day interval (Fig. 6f), and 4T1-Luc tumor recurrence was monitored by in vivo bioluminescence imaging (Fig. 6g). Compared with Mem+CpG+MPLA treatment that only moderately suppressed 4T1-Luc tumor recurrence, M-SNVac-L displayed remarkable efficacy to prevent tumor recurrence, and enabled 4/6 of mice to be tumor-free and survive up to 90 days (Fig. 6h, i and Supplementary Fig. 46). In addition, ex-vivo bioluminescence imaging of lung tissues further demonstrated that M-SNVac-L suppressed the post-operative lung metastasis of breast tumor (Fig. 6j–l and Supplementary Fig. 47).
To assess the induction of long-term immune memory effect after M-SNVac-L treatment, M-SNVac-L-cured mice were rechallenged with 4T1-Luc cells at day 90 post primary tumor inoculation. M-SNVac-L-cured mice completely resisted secondary tumor challenge over 120 days (Fig. 6m–o), and maintained high levels of effector CD8+ T memory cells and central CD8+ T memory cells (Fig. 6p). Collectively, personalized M-SNVac-L vaccination could elicit potent and durable immune memory effect to prevent post-operative tumor recurrence and metastasis.
Combination of neoantigen-loaded nanovaccine (Ne-SNVac) with laser irradiation potentiated ICB therapy in orthotopic tumors
Hepatocellular carcinoma (HCC) remains one of the most diagnosed solid tumors with poor survival in the clinic55. Unfortunately, advanced HCC patients marginally benefit from current ICB therapy due to insufficient tumor-infiltration of effector T cells56,57. To demonstrate the potential of neoantigen-based STING nanovaccine (Ne-SNVac) for boosting ICB therapy of HCC, our previously identified Hepa1-6 tumor-specific neoantigen sequence (RWLYWQPTL) was selected and synthetized as the neoantigen peptide58. The therapeutic performance of combination of Ne-SNVac with idLN-localized laser irradiation (namely Ne-SNVac-L, 200 mW/cm2, 5 min) was investigated in the orthotopic Hepa1-6-Luc liver tumor model (Fig. 7a). In vivo bioluminescence imaging result found that mono PD-L1 antibody (αPD-L1) only moderately inhibited Hepa1-6-Luc tumor growth and all the mice lost within 45 days (Fig. 7b). In contrast, Ne-SNVac-L remarkedly inhibited orthotopic liver tumor growth and prolonged the median survival of mice. It was worth noting that combination of Ne-SNVac-L with αPD-L1 further enhanced antitumor efficacy, and enabled 4/5 of mice to be tumor-free and survive up to 80 days (Fig. 7c, e).
a Schematic illustration to show the experimental timeline for evaluating the therapeutic efficacy of neoantigen peptide-based Ne-SNVac-L+anti-PD-L1 in orthotopic Hepa1-6-Luc liver tumor model and orthotopic 4T1-Luc breast tumor model. b Representative bioluminescence images of orthotopic Hepa1-6-Luc tumor-bearing mice at different time points (n = 5 biologically independent mice). c Representative photographs and corresponding H&E-stained slices of the liver tissue on day 30 post tumor inoculation. Scale bar = 100 μm. d Quantitative analysis of the frequency of neoantigen-specifc T cells (Ptpn2-tetramer+ in CD3+CD8+ cells) in tumor (n = 5 biologically independent mice). e The survival curves of orthotopic Hepa1-6-Luc liver tumor-bearing mice in indicated treatment groups (n = 5 biologically independent mice). f Representative immunofluorescence micrographs of tumor-infiltrating CD8+ T cells (red) and CD206+ M2-TAM (green) (n = 3 biologically independent mice). The experiment was repeated twice independently with similar results. Scale bar = 100 μm. g Averaged orthotopic 4T1-Luc tumor growth curves and corresponding survival curves of the tumor-bearing mice (n = 5 biologically independent mice). h Representative bioluminescence images of orthotopic 4T1-Luc breast tumor-bearing mice at different time points (n = 5 biologically independent mice). i Quantitative analysis of the frequency of CD8+ T cells in tumor (CD8+ in CD3+CD45+ cells) (n = 5 biologically independent mice). j, k Quantitative analysis of the frequency of Gzmb+CD8+ T cells (Gzmb+ in CD8+CD3+CD45+ cells) (j) and IFN-γ+CD8+ T cells (IFN-γ+ in CD8+CD3+CD45+ cells) (k) in tumor (n = 5 biologically independent mice). l Heatmap of the frequency of Treg (FOXP+CD25+ in CD4+CD3+CD45+ cells), M1-TAM (CD86+F4/80+CD11b+CD45+) and M2-TAM (CD206+F4/80+CD11b+CD45+) in tumor (n = 5 biologically independent mice). Unless specified otherwise, the data are presented as mean ± SD. Statistical significance was calculated via one-way ANOVA with Tukey’s test (d, i–k) or log-rank (Mantel-Cox) test (e, g), and P-values were indicated. Source data are provided as a Source Data file. The elements in Fig. 7a were created by Adobe Illustrator.
We next investigated the intratumoral T-cell immunity induced by Ne-SNVac-L + αPD-L1 in the orthotopic liver tumor model. Compared with αPD-L1 that only marginally promoted tumor-infiltration of CD8+ T cells, Ne-SNVac-L + αPD-L1 not only elicited 4.2-fold higher the frequency of tumor-infiltrating neoantigen-specific CD8+ T cells (Fig. 7d and Supplementary Fig. 48a, c), but also efficiently increased the frequency of cytotoxic CD8+ T cells, including IFN-γ+CD8+ T cells and TNF-α+CD8+ T cells (Supplementary Fig. 48b). Immunofluorescence staining of tumor sections further verified that Ne-SNVac-L + αPD-L1 significantly increased tumor-infiltration of CD8+ T cells, while decreasing tumor-infiltration of CD206+ M2-type TAM compared with αPD-L1 group (Fig. 7f).
To demonstrate the genericity of Ne-SNVac-L vaccination strategy for potentiating ICB therapy in solid tumors, we further evaluated the combination treatment of Ne-SNVac-L with αPD-L1 in the orthotopic TNBC model. The 4T1 tumor-specific neoantigen sequence (SHRSCSHQTSAPSPKALAHNGTPRNAI) was selected and synthetized as the neoantigen peptide. In vivo bioluminescence imaging result demonstrated that αPD-L1 only moderately inhibited 4T1-Luc tumor growth and all the mice succumbed to tumors within 35 days (Fig. 7g, h). In contrast, Ne-SNVac-L + αPD-L1 markedly inhibited tumor growth and prolonged the median survival of mice from 22 days (PBS group) to 54 days (Supplementary Fig. 49).
We next measured the tumor-infiltration level and cytotoxic effect of CD8+ T cells after Ne-SNVac-L + αPDL1 treatment. Compared with αPD-L1 group, Ne-SNVac-L + αPD-L1 treatment significantly increased the frequency of tumor-infiltrating CD8+ T cells (Fig. 7i and Supplementary Fig. 50), and promoted production of T cell-derived cytotoxic cytokines (IFN-γ, Gzmb). The frequency of tumor-infiltrating IFN-γ+CD8+ T cells and Gzmb+CD8+ T cells in Ne-SNVac-L+αPD-L1 group displayed 2.4 and 2.7-fold increase than αPD-L1 group (Fig. 7j, k and Supplementary Fig. 51). Interestingly, Ne-SNVac-L + αPD-L1 also effectively alleviated the immunosuppressive tumor microenvironment by inhibiting the tumor-infiltration of Treg (Fig. 7l and Supplementary Fig. 52a), and repolarizing M2-type TAM to M1-type TAM (Supplementary Fig. 52b–d). These results together demonstrated that Ne-SNVac-L vaccination was highly promising to elicit robust intratumoral T-cell immunity to potentiate ICB therapy in solid tumors.
Combination of SNVac with ultrasound stimulation enhanced T-cell immunity to mitigate tumor burden
To demonstrate the genericity of spatiotemporally-tailored cancer vaccination strategy, we further investigated the combination of SNVac with idLN-localized ultrasound stimulation (namely SNVac-US, 1 MHz, 50% duty cycle, 1.0 W/cm2, 5 min) to achieve ultrasound-boosted cancer vaccination therapy (Fig. 8a). SNVac-US significantly promoted the influx of CD11c+ DC, CD11b+ macrophages and CD3+ T cells into idLN (Fig. 8b), and triggered the expression of stimulatory markers (CD80, CD86) in DC (Fig. 8c). In addition, SNVac-US induced the highest level of antigen presentation on the surface of DC, and displayed 2.8-fold higher percentage of antigen-presented DC than OVA+MSA-2 group (Fig. 8d). We subsequently analyzed the antigen-specific T-cell immunity induced by SNVac-US, and found that SNVac-US 3.8 and 1.9-fold more efficiently elicited antigen-specific CD8+ T cell response than OVA+MSA-2 and SNVac groups, respectively (Fig. 8f, g). The in vivo cytotoxicity killing assay showed that SNVac-US group mice produced the highest antigen-specific cytotoxic T cell response among all the groups (Fig. 8h). These findings validated that SNVac-US offered an ultrasound-boosted vaccination strategy to enhance antigen-specific T-cell immunity in vivo (Fig. 8e).
a Schematic illustration of the ultrasound-boosted vaccination induced by SNVac-US to inhibit tumor growth and metastasis. b The absolute number of CD11c+ DC, CD11b+ macrophages and CD3+ T cells in the idLN after indicated treatments (n = 5 biologically independent mice). c Quantitative analysis of the frequency of matured DC (CD80+CD86+ in CD11c+ cells) in the idLN (n = 5 biologically independent mice). d Representative flow cytometry plots and quantitative analysis of the frequency of antigen-presented DC (SIINFEKL-H2Kb+ in CD11c+ cells) in the idLN (n = 5 biologically independent mice). e Schematic illustration of the ultrasound-boosted antigen cytosolic release and STING pathway activation induced by SNVac-US to promote antigen cross-presentation and T-cell activation. f, g Representative flow cytometry plots and quantitative analysis of the frequency of antigen-specific T cells (SIINFEKL-H2Kb tetramer+ in CD3+CD8+ cells) in the spleen (n = 5 biologically independent mice). h Representative flow cytometry plots and quantitative analysis of the OVA-specific killing effect in vivo (n = 4 biologically independent mice). The experiment was repeated twice independently with similar results. i Experimental timeline for evaluating the therapeutic efficacy of SNVac-US in the B16-OVA tumor model. j, k Averaged B16-OVA tumor growth curves and corresponding survival curves of mice in indicated groups (n = 6 biologically independent mice). l Individual B16-OVA tumor growth curves of mice in indicated groups (n = 6 biologically independent mice). m Representative TUNEL and Ki-67 staining images of the B16-OVA tumor sections collected from indicated groups (n = 3 biologically independent mice). The experiment was repeated twice independently with similar results. Scale bars = 100 μm. Unless specified otherwise, the data are presented as mean± SD. Statistical significance was calculated via one-way ANOVA with Tukey’s test (b−d, g−j) or log-rank (Mantel-Cox) test (k), and P-values were indicated. Source data are provided as a Source Data file. The elements in Fig. 8i were created by Adobe Illustrator, and the elements in Fig. 8a, e were created by Adobe Photoshop.
We next evaluated the therapeutic performance of SNVac-US in established tumor model. C57BL/6 mice were subcutaneously inoculated with B16-OVA cells in the right flank and treated with indicated formulations 7 days later (Fig. 8i). OVA+CpG and OVA+MSA-2 only moderately inhibited tumor growth and all the mice succumbed to tumors within 26 days. SNVac extended the median survival of mice from 18 days (PBS group) to 28 days, while all the mice succumbed to tumors within 32 days (Fig. 8j). In contrast, SNVac-US markedly inhibited tumor growth and prolonged the median survival of mice, with 1/6 of the mice produce complete tumor regression over 60 days (Fig. 8k, l). Terminal deoxynucleotidyl transferase-mediated dUTP nick end labeling (TUNEL) and Ki67 staining of tumor sections showed that SNVac-US markedly inhibited tumor cell proliferation and induced tumor cell apoptosis (Fig. 8m).
We further evaluated the therapeutic efficacy of SNVac-US to inhibit lung metastases of B16-OVA tumor. OVA+CpG and OVA+MSA-2 afforded modest therapeutic effect against tumor metastasis compared to PBS group. In contrast, SNVac-US showed the highest anti-metastasis effect among all the groups, and almost completely suppressed the formation of metastatic foci in lungs (Supplementary Fig. 53). These results collectively demonstrated the remarkable therapeutic efficacy of SNVac-US against established tumor growth and metastasis.
H&E staining of idLN and major organs showed negligible histopathological damage, and no inflammatory lesions were observed after SNVac-L and SNVac-US treatment (Supplementary Fig. 54). Biochemical analysis of serum further confirmed the favorable biosafety of SNVac-L and SNVac-US treatment in vivo (Supplementary Fig. 55). Collectively, these results suggested that SNVac-L and SNVac-US offered spatiotemporally-tailored vaccination strategies to achieve safe and effective cancer immunotherapy.
Discussion
Cancer vaccines hold great promise to elicit protective immune response for long-term tumor regression and metastasis prevention. Various types of immune agonizts or delivery systems have been developed to boost cancer vaccine immunotherapy by stimulating innate immune pathways in DC. Despite their therapeutic promise in preclinical settings, most of these strategies were found to induce less potent antitumor immunity while potential dose-limiting toxicity in clinical trials. In this study, we utilized the clinically accessible photo/sonodynamic effect to precisely tailor redox homeostasis of DC, and amplify innate immune pathways activation in a spatiotemporally-tailored manner. Through the co-assembly of STINGa-conjugated polypeptide with charge-modified polypeptides, we established a library of STING nanoadjuvants and optimized the top-performed formulation for idLN-targeting antigen delivery. The combination of antigen-loaded STING nanovaccine with idLN-localized laser irradiation or ultrasound stimulation significantly enhanced the magnitude and persistence of innate immune responses in a region-specific manner, and induced robust and durable antitumor T-cell immunity in different tumor models mimicking a range of clinical scenarios (Supplementary Fig. 57).
Various types of STING nanoadjuvant delivery systems have been developed to promote the activation of STING agonizts in a region-specific manner59,60,61,62. For instance, Moon et al. identified the metal element Mn2+, as the effective STING enhancer to synergize with STING agonist c-di-AMP for combination cancer immunotherapy. They developed a lipid nanoparticle based on the coordination complex between Mn2+ and c-di-AMP. The resultant STING nanoadjuvant efficiently co-delivered Mn2+ and c-di-AMP for tumor-specific STING activation and antitumor immunity induction63. Besides, Irvine et al. covalently conjugated the STING agonist, cGAMP, to PEGylated lipids and developed a lipid nanodisc-based STING nanoadjuvant for tumor-specific STING activation. The lipid nanodisc exhibited tumor-penetration profile and induced potent antitumor immunity in multiple mouse models of tumors64. Apart from the lipid-based STING nanoadjuvants, the polymeric STING nanoadjuvants also exhibited promising potential for cancer immunotherapy. Sun et al. synthesized a cationic and amphiphilic copolymer for complexation of the anionic STING agonist DMXAA. After intravenous injection, the polymeric STING nanoadjuvant reprogrammed the immunosuppressive tumor microenvironment and significantly inhibited primary tumor growth and distant metastasis in mice65.
Compared to the previously reported STING nanoadjuvants, our reported spatiotemporally-tailored STING nanoadjuvant exhibits some advantages for safe and effective cancer immunotherapy. First, the photo/sonosensitizer is innovatively introduced into the STING nanoadjuvant platform, which ensures the innate immunity stimulation of DC can be spatiotemporally tailored by the external laser or ultrasound stimuli. Second, the physicochemical properties, including particle size and surface charge, of STING nanoadjuvant is rationally optimized through modification with charge-modified polypeptides, which endows STING nanoadjuvant with excellent idLN-targeting efficacy. Third, polypeptide-based delivery systems are of satisfying biosafety and biodegradability, and have been widely applied for clinical setup. Therefore, polypeptide-based STING nanoadjuvant can serve as a highly biocompatible platform for cancer vaccine therapy. Furthermore, the STING nanoadjuvant not only effectively co-delivers various types of tumor-specifc antigens into idLN, but also shows great promise to promote cytosolic release of antigens in DC, which enables efficient antigen cross-presentation and T-cell activation to potentiate personized cancer vaccine immunotherapy.
It was worth noting that extensive efforts remain to be conducted for addressing the limitations of STING nanoadjuvant for future clinical translation. First, surface targeting ligands (CLEC9A antibody, mannose) are encouraged to be modified onto the STING nanoadjuvant for improving DC-targeting delivery efficacy. Second, although conventional innate immune stimuli contribute to DC activation, uncontrollable stimulation of innate immunity can lead to DC dysfunction. Therefore, the potential and underlying mechanism of spatiotemporally-tailored STING nanoadjuvant for addressing DC dysfunction should be more extensively investigated. Third, the photoacoustic imaging and high-frequency ultrasound imaging technique should be combined to effectively visualize the biodistribution of STING nanoadjuvant in idLN that located at superficial internal, and thus can guide us to perform precise idLN-specific laser irradiation or ultrasound stimulation.
Methods
Materials
All chemicals were purchased from J&K Chemical unless otherwise listed. Pyropheophorbide-a (PPa) (cat. HY-128973) and MSA-2 (cat. HY-136927) were purchased from MedChemExpress. OVA, OVA257-263 (SIINFEKL) peptide, FITC-labeled OVA257–264 peptide and Hepa1-6 tumor-specifc neoantigen (RWLYWQPTL) peptide were synthesized by BankPeptide Biological Technology Co., Ltd. JSH-23 (cat. M2786) was purchased from AbMole. CpG-ODN was synthesized by Synbio Tech (Suzhou/NJ). Serum free cell freezing solution (cat. PB180436) was purchased from Procell. DAPI (cat. MA0128) and Lysotracker Red (cat. MB6041) were purchased from Meilun Biotech CO., Ltd. The D-Luciferin (cat. 40902ES01) was purchased from Yeasen. Glutamic-oxalacetic transaminase activity assay kit (cat. BC1560) was purchased from Beijing Solarbio Science & Technology Co., Ltd. ELISA kits for mouse TNF-α (cat. EMC102a), mouse IFN-β (cat. EMC016), mouse IFN-γ (cat. EMC101g) and mouse TGF-β (cat. EMC107b) were purchased from NeoBioscience Technology Co., Ltd. ELISA kits for mouse IL-6 (cat. KTE7009) was purchased from Abbkine. Mouse Lymphocyte Separation Medium (cat. DKW33-R0100) was purchased from Shenzhen Dakewe Bio-engineering Co., Ltd.
Cell lines and animals
DC2.4 cells (cat. GNM51), RAW264.7 cells (cat. TCM13), B16-OVA cells (cat. TCM2), CT-26 cells (cat. TCM37) and 4T1 cells (cat. TCM32) were all purchased from the Cell Bank of Shanghai, Chinese Academy of Sciences. Hepa1-6 cells were provided by Prof. XL Liu from Mengchao Hepatobiliary Hospital of Fujian Medical University. RAW264.7-Lucia ISG cells and THP1-Blue ISG cells were provided by Prof. MY Zheng from Shanghai Institute of Material Medica, Chinese Academy of Sciences. The construct expressing luciferase was introduced into Hepa1-6, and 4T1 cells by lentiviral transduction for bioluminescence imaging. All the cells were maintained in DMEM medium containing 10% FBS (cat. SX1500, SORFA) and 1% penicillin/streptomycin, and maintained at 37 °C in a humidified incubator with 5% CO2 supply.
BALB/c mice (cat. SM-003, 4–5 weeks, female) and C57BL/6 mice (cat. SM-001, 4–5 weeks, female) were purchased from Shanghai Model Organisms Center, Inc. All mice were housed and maintained under specific pathogen-free (SPF) conditions in groups of 4–5 mice per cage, and maintained at a temperature of 25 °C in a humidity-controlled environment with a 12 h light/dark cycle, with free access to standard food and water. All animal procedures were performed under the guidelines approved by the Institutional Animal Care and Use Committee (IACUC) of the Shanghai Institute of Materia Medica, Chinese Academy of Sciences. For animal studies, the mice were earmarked before grouping and randomly separated into groups by an independent person, and experimental/control animals were bred separately. According to the animal ethics of institute and animal welfare, animals were euthanized by carbon dioxide inhalation when their tumor volumes exceeded 1500 mm3 in all the antitumor studies.
Synthesis of mPEG-b-PTyr polypeptide
mPEG-b-PTyr polypeptide was synthesized by ROP of L-tyrosine N-carboxyanhydride (Tyr NCA) using macroinitiator PEG-NH2. Typically, NH2-PEG5k (100 mg, 0.018 mmol) and Tyr NCA (183 mg, 0.885 mmol) were dissolved in anhydrous DMF under argon. The reaction was stirred for 3 days at room temperature and precipitated with cold diethyl ether to obtain mPEG-b-PTyr as white powder (yield 89.1%).
Synthesis of mPEG-b-PTyr-PPa polypeptide
To prepare mPEG-b-PTyr-PPa, PPa (6.9 mg, 0.013 mmol), DMAP (8.0 mg, 0.33 mmol), EDCI (12.6 mg, 0.33 mmol), and DIEA (8.8 mg, 0.33 mmol) were dissolved in anhydrous DMF. After stirring for 1 h, the DMF solution of mPEG-b-PTyr (100.0 mg, 0.0087 mmol) was added dropwise into the mixture, and stirred continued for 24 h at room temperature. Then, the reaction was precipitated with cold diethyl ether to obtain mPEG-b-PTyr-PPa as black powder.
Synthesis of STINGa-conjugated polypeptide
To prepare STINGa-conjugated polypeptide, MSA-2 (101.8 mg, 0.34 mmol) and DIPC (49.6 mg, 0.34 mmol) were dissolved in anhydrous DMF and pyridine (v/v = 5/1). After stirring for 1 h, the DMF solution of mPEG-b-PTyr-PPa (100.0 mg, 0.0086 mmol) was added dropwise into the mixture, and stirred continued for 48 h at room temperature. Then, the reaction was precipitated with cold diethyl ether to obtain mPEG-b-PTyr-MSA-PPa as black powder.
Synthesis of charge-modified polypeptides
Four types of charge-modified polypeptides, including mPEG-b-P(Lys40), mPEG-b-P(Tyr10-Lys30), mPEG-b-P(Tyr30-Lys10) and mPEG-b-P(Tyr40), were synthesized by ROP of lysine N-carboxyanhydride (Lys NCA) and Tyr NCA using macroinitiator PEG-NH2. Typically, NH2-PEG5k (100 mg, 0.018 mmol) and indicated mass of Lys NCA and Tyr NCA were dissolved in anhydrous DMF under argon. The reaction was stirred for 3 days at room temperature and precipitated with cold diethyl ether to obtain indicated polypeptides as white powder.
mPEG-b-P(Lys30-Tyr-PO32−10), mPEG-b-P(Lys10-Tyr-PO32−30) and mPEG-b-P(Tyr-PO32−40) polypeptides were synthesized via phosphorylation of phenolic hydroxyl groups of tyrosine. For example. mPEG-b-P(Tyr-PO32−40) (100 mg, 0.0087 mmol) was suspended in anhydrous N-methylpyrrolidone under ice bath. Anhydrous triethylamine (200 μL) and phosphorus oxychloride (200 μL) were then slowly added. The mixture was stirred in the darkness overnight and saturated NaHCO3 solution was added. After stirring for another 3 h, the mixture was dialyzed against DI water and lyophilized to obtain mPEG-b-P(Tyr-PO32−40) as yellow solid.
Culture of BMDC and BMDM
Primary BMDC and BMDM were isolated from female C57BL/6 mice. Briefly, bone marrow was flushed from isolated femurs using PBS. For BMDC isolation, the marrow was seeded in petri dishes containing RPMI 1640 medium (cat. L210KJ, BasalMedia Co., Ltd) supplemented with 10% FBS, 1% penicillin-streptomycin, 5 ng/mL interleukin-4 (cat. CK15), and 20 ng/mL murine granulocyte macrophage colony-stimulating factor (cat. CK02, Novoprotein). For BMDM isolation, the marrow was seeded in petri dishes containing RPMI 1640 medium supplemented with 10% FBS, 1% penicillin-streptomycin and 10 ng/mL macrophage colony-stimulating factor (cat. CB34, Novoprotein). Half the culture medium volume was refreshed on day 3. The nonadherent cell fractions of these cultures were used for experiments between days 6 and 8 of culture.
BMDC maturation in vitro
To investigate the adjuvant effect of PSN-L or PSN-US for promoting BMDC maturation, 2 × 105 BMDC were cultured in 12-well plate and incubated with PSN (PPa, 1.0 μg/mL) and MSA-2 (10 μM) for 6 h, and irradiated with 671 nm laser (50 mW/cm2, 1 min) or stimulated with ultrasound (1 MHz, 50% duty cycle, 0.2 W/cm2, 1 min). The cells were continually cultured for 24 h, and stained with corresponding antibodies to analyze BMDC maturation by flow cytometry.
Western blot assay
Western blot was performed to analyze innate immune pathways activation in BMDC. Briefly, 5 × 105 BMDC were cultured in 6-well tissue culture plate and incubated with PSN (PPa, 1.0 μg/mL) and MSA-2 (0, 5, 10 μM) for 6 h, and irradiated with 671 nm laser (50 mW/cm2, 1 min) or stimulated with ultrasound (1 MHz, 50% duty cycle, 0.2 W/cm2, 1 min). The cells were continually cultured for 24 h, and then lysed using RIPA buffer containing 1% protease inhibitors. The protein concentration of the samples was quantified using a bicinchoninic acid assay kit according to the manufacturer’s instructions (New Cell & Molecular Biotech). Equal amounts of protein were mixed with an equal volume of 5 × loading buffer and boiled at 100 °C for 20 min. Gel electrophoresis and protein transformation were then performed. The protein marker (EC1019-A) was purchased from Shandong Sparkjade Biotechnology Co., Ltd. The target proteins were then probed with specific primary antibodies followed by secondary antibodies conjugated with horseradish peroxidase. Immunoreactive proteins were visualized using enhanced chemiluminescence reagents.
ELISA assay
To determine cytokine secretion in vitro and in vivo, 3 × 104 BMDC were cultured in 96-well plate and incubated with PSN (PPa, 1.0 μg/mL) and MSA-2 (0, 5, 10 μM) for 6 h, and irradiated with 671 nm laser (50 mW/cm2, 1 min) or stimulated with ultrasound (1 MHz, 50% duty cycle, 0.2 W/cm2, 1 min). The cells were continually cultured for 24 h, and the supernatant was collected for analyzing IFN-β, TNF-α, IL-6 secretion by indicated ELISA kits. To detect cytokine secretion in vivo, the idLN and tumor tissues were harvested and homogenized in cold PBS and centrifuged to collect the supernatant. All the samples were frozen and stored at −80 °C before ELISA analysis.
ISG-reporter assay
3 × 104 RAW264.7-ISG-Lucia cells were cultured in 96-well plate and incubated with PSN (PPa, 1.0 μg/mL) for 6 h, and irradiated with 671 nm laser (50 mW/cm2, 1 min) or stimulated with ultrasound (1 MHz, 50% duty cycle, 0.2 W/cm2, 1 min). The cells were continually cultured for 24 h. Subsequently, 20 μL of supernatant and 50 μL of QUANTI-Luc detection reagent (cat. rep-qlc4lg1) were added into 384-well white plate. The bioluminescence intensity was measured by SpectraMAX Paradigm.
Preparation and characterization of STING nanoadjuvants
The STING nanoadjuvants were prepared by a nanoprecipitation method. Typically, 1.0 mg of STINGa-conjugated polypeptide in 50 μL of DMSO and indicated mass of charge-modified polypeptides was drop by drop added into 1.0 mL deionized water under supersonic vibration (85 W, on 5 s, off 2 s, 3 min). The resultant nanoadjuvants were purified through ultrafiltration tube (Mw = 100 kDa) and dispersed in PBS for further use. The particle size and zeta potential of nanoadjuvants were measured in pH 7.4 buffer solution by Zeta-sizer Nano ZS90 (Malvern Instruments, England).
Lymph node-targeting of SNA library
C57BL/6 mice were subcutaneously injected at the tail base with SNA1-13 at an identical PPa dose of 5.0 mg/kg. Fluorescence signal in inguinal draining lymph nodes (idLN) and major organs including heart, liver, spleen, lung and kidney were examined 12 h post-injection with an IVIS Spectrum Imaging System. Semi-quantification of the fluorescence signal in idLN and major organs was conducted to screen out the top-performed nanoadjuvant. To investigate the distribution of SNA in tumor-bearing mice, B16-OVA tumor-bearing mice and 4T1 tumor-bearing mice were subcutaneously injected at the tail base with SNA at an identical PPa dose of 5.0 mg/kg. Fluorescence signal in idLN, tumor tissues and major organs were examined 12 h post-injection with an IVIS Spectrum Imaging System.
RNA-seq analysis
Total RNA was extracted with a Trizol reagent kit according to the manufacturer’s protocol. The RNA purification, reverse transcription, library construction and sequencing were performed at Shanghai Majorbio Bio-pharm Biotechnology Co., Ltd. (Shanghai, China) according to the manufacturer’s instructions (Illumina, San Diego, CA). To identify DEG between two different samples, the expression level of each transcript was calculated according to the transcripts per million reads (TPM) method. Differential expression analysis was performed using the DESeq2. DEG with log2FC ≧ 1 and FDR ≤ 0.05 (DESeq2) were considered to be significantly different expressed genes. The SRA accession of RNA-Seq data in the NCBI: SRR32624204, SRR32624205, SRR32624206, SRR32624207, SRR32624208, SRR32624209, SRR32620524, SRR32620525, SRR32620526, SRR32620527, SRR32620528, SRR32620529, SRR32620530, SRR32620531, SRR32620532.
Preparation and characterization of STING nanovaccines
The protein antigen (OVA), membrane antigen (Mem) and neoantigen peptide were selected as tumor antigens to prepare SNVac, M-SNVac and Ne-SNVac, respectively. The tumor antigen solution (100 μL, 0.3 mg) was added into 1.0 mL of the prepared SNA solution. The resultant mixture was kept stirring at room temperature for 60 min. The obtained STING nanovaccines were purified through ultrafiltration tube (Mw = 100 kDa) and dispersed in PBS for further use. The loading capacity of OVA or Mem in SNVac or M-SNVac was determined by BCA. The loading capacity of neoantigen peptide in Ne-SNVac was determined by HPLC. The particle size and zeta potential of SNVac, M-SNVac and Ne-SNVac were evaluated in PBS (pH 7.4) by Zeta-sizer Nano ZS90.
Antigen presentation and T cell proliferation in vitro
BMDC were incubated with various formulations at equivalent concentration of OVA (10 μg/mL). At 6 h post incubation, BMDC in SNVac-L group were irradiated with 671 nm laser (50 mW/cm2, 1 min). The cells were continuously cultured for 24 h and then stained with corresponding antibodies to analyze the antigen presentation level on BMDC by flow cytometry. For analyzing T cell proliferation in vitro, BMDC were treated with the same formulations as described above, and then co-cultured with CFSE-stained T cells for 48 h (T cell: BMDC = 10:1). The T cell proliferation and cytokine release was assessed by flow cytometry and ELISA assay, respectively.
Laser irradiation or ultrasound stimulation in vivo
At 6 h post subcutaneous injection of STING nanoadjuvant or nanovaccine, the idLN region of injected mice was locally irradiated with 671 nm laser (Modulation: 1 MHz, Wavelength: 671 ± 1 nm, Output intensity: 200 mW/cm2, Duration: 5 min) or stimulated with ultrasound (Frequency: 1 MHz, Duty cycle: 50%, Output intensity: 1.0 W/cm2, Duration: 5 min, Transducer type: COLLIMATING, Effective radiating area: 4 cm2). The ultrasound device was purchased from DJO France S.A.S. (DJO 2776). The 671 nm laser device was purchased from Changchun New Industries Optoelectronics Technology Co., Ltd (MRL-FN-671-1W, Polarization ratio > 100:1, Beam diameter at the aperture <2.5 mm) (Supplementary Fig. 56).
Lymph node-targeting and cellular uptake of SNVac in vivo
To demonstrate the lymph node-targeting of SNVac in vivo, C57BL/6 mice were subcutaneously injected at the tail base with free OVA-FITC or SNVac-FITC at an identical OVA-FITC dose of 5.0 mg/kg. Fluorescence signal in idLN were examined 6 h or 12 h post injection with an IVIS Spectrum Imaging System. To determine the cellular uptake of SNVac-FITC in vivo, the idLN were harvested and digested to obtain single-cell suspensions. The cells were washed with PBS three times and then stained with corresponding antibodies to analyze the cellular uptake of SNVac-FITC by DC and macrophages by flow cytometry.
Vaccination and antigen-specific immune response in vivo
To evaluate the antigen-specific immune responses in vivo, C57BL/6 mice were vaccinated at the identical dose of OVA (1.0 mg/kg), MSA-2 (2.0 mg/kg), PPa (1.0 mg/kg) and CpG (1.0 mg/kg) in indicated formulations three times at 7 day interval. idLN-localized laser irradiation or ultrasound stimulation was conducted at 6 h post per SNVac injection. The idLN were harvested 3 day after the final vaccination, and mechanically disrupted into single cell suspension as descried above. The cells were stained with corresponding antibodies to analyze the maturation and antigen presentation levels of DC in the idLN by flow cytometry. The spleen was harvested 7 day after the final vaccination, and mechanically disrupted into single cell suspension. The red blood cells (RBC) were lysed using RBC lysis buffer. The cells were stained with corresponding antibodies to analyze the frequency of OVA antigen-specific CD8+ T cells using the tetramer staining assay according to the standard protocol. To evaluate the cytotoxic effect of CD8+ T cells, 1 × 106 splenocytes were incubated with 10 μg/mL SIINFEKL peptide for 24 h. The secretion of IFN-γ and TNF-α by splenocytes were then analyzed by indicated ELISA kits.
In vivo cytotoxicity killing assay
In vivo cytotoxicity killing assay was performed to detect the OVA-specific cytotoxic T cell response generated by SNVac-L. Briefly, half of splenocytes from untreated mice were labeled with OVA peptide and high concentration of CFSE (5.0 μM), denoted as OVAp+ target cells. Meanwhile, the other half of splenocytes were labeled with low concentration of CFSE (0.5 μM) and not labeled with OVA peptide, denoted as OVAp− un-target cells. Then, the target cells and un-target cells were equally mixed and injected intravenously into the SNVac-L-treated mice. The OVAp+ target cells could be specifically killed by the OVA-specific cytotoxic T cells in vivo, while the OVAp− un-target cells remain be unaffected. At 24 h post injection of CFSE-labeled splenocytes, the spleen of treated mice were harvested, and the CFSE fluorescence signal of CFSE+ cells was analyzed by flow cytometry. The specific killing ratio was calculated using the equation below.
Antitumor efficacy in multiple murine tumor models
To evaluate the antitumor effect of SNA-L or SNA-US in CT26, MC38 and 4T1 tumor models, 1 × 106 CT26 cells or 4T1 cells were subcutaneously inoculated into the right flank of BALB/c mice, and 1 × 106 MC38 cells were subcutaneously inoculated into the right flank of C57BL/6 mice on day 0. The mice were subcutaneously injected with PBS or SNA on days 4, 7 and 10, at an identical PPa dose of 1.0 mg/kg and MSA-2 dose of 2.0 mg/kg. At 6 h post per injection, the idLN of SNA-L or SNA-US group mice were irradiated with 671 nm laser (200 mW/cm2, 5 min) or stimulated with ultrasound (1.0 W/cm2, 5 min, 1 MHz, 50% duty cycle), respectively.
To evaluate the effect of SNVac-L or SNVac-US to inhibit tumor growth, 1 × 106 B16-OVA cells were subcutaneously inoculated into the right flank of C57BL/6 mice on day 0. B16-OVA tumor-bearing C57BL/6 mice were randomly grouped on day 7, and treated on the day 7, 14, 21 by subcutaneous injection of PBS, OVA+CpG, OVA+MSA-2, SNVac-L or SNVac-US at identical dose of OVA (1.0 mg/kg), MSA-2 (2.0 mg/kg), PPa (1.0 mg/kg) and CpG (1.0 mg/kg). At 6 h post per injection, the idLN of SNVac-L or SNVac-US group mice were irradiated with 671 nm laser (200 mW/cm2, 5 min) or stimulated with ultrasound (1.0 W/cm2, 5 min, 1 MHz, 50% duty cycle), respectively.
To evaluate the therapeutic effect of SNVac-US against tumor metastasis, 1 × 106 B16-OVA cells were intravenously inoculated into the C57BL/6 mice on day 0, and indicated formulations were subcutaneously injected on the day 7, 14 and 21. At 6 h post per injection, the idLN of SNVac-US group mice were stimulated with ultrasound (1.0 W/cm2, 5 min, 1 MHz, 50% duty cycle). The lungs of all group mice were isolated on day 24 and lung metastasis nodules were counted.
To evaluate the antitumor effect of M-SNVac-L in the post-operative 4T1-Luc breast tumor model, 1 × 106 4T1-Luc cells were subcutaneously inoculated into the right flank of BALB/c mice on day 0. Most of the tumor tissue from each mouse was resected when the tumor volume reached about 300 mm3 on day 12, with about 5% remaining to mimic residual micro-tumors after surgery in the clinic. The operated tumor-bearing mice were randomly divided into three groups, and mice were subcutaneously injected with PBS, Mem + CpG + MPLA or M-SNVac-L on day 16, 23, 30, at identical dose of MSA-2 (2.0 mg/kg), PPa (1.0 mg/kg), CpG (1.0 mg/kg) and MPLA (0.5 mg/kg). At 6 h post per injection, the idLN of M-SNVac-L group mice were irradiated with 671 nm laser (200 mW/cm2, 5 min).
To evaluate the combination antitumor effect of Ne-SNVac-L with PD-L1 blockade therapy in the orthotopic liver tumor model, 2 × 106 Hepa1-6-Luc cells were injected into the liver of C57BL/6 mice on day 0. Tumor-bearing C57BL/6 mice were randomly grouped on day 7, and treated on day 7, 14, 21 by subcutaneous injection of Ne-SNVac-L at identical dose of neoantigen (1.0 mg/kg), MSA-2 (2.0 mg/kg), PPa (1.0 mg/kg), or intraperitoneal injection of αPD-L1 (5.0 mg/kg). At 6 h post per injection, the idLN of Ne-SNVac-L and Ne-SNVac-L+αPD-L1 group mice were irradiated with 671 nm laser (200 mW/cm2, 5 min).
To evaluate the combination antitumor effect of Ne-SNVac-L with PD-L1 blockade therapy in the orthotopic breast tumor model, 1 × 106 4T1-Luc cells were injected into the breast pad of BALB/c mice on day 0. Tumor-bearing mice were randomly grouped on day 7, and treated by Ne-SNVac-L and αPD-L1 as described above. The body weight and tumor size were monitored every 2 days, and the tumor volume (V) was calculated by the formula below. The tumor-bearing mice were considered dead when the tumor volume reached 1500 mm3.
Tumor rechallenge assay
M-SNVac-L-cured mice were subcutaneously inoculated with 1 × 106 4T1-Luc cells on day 90 post primary tumor inoculation. Tumor growth was monitored up to 130 days. The splenocytes were harvested on day 130 to determine the frequency of central memory T cells (CD44+CD62L+) or effector memory T cells (CD44+CD62L−) in CD8+CD3+ T cells by flow cytometry.
CD8+ T cell blocking assay
To block CD8+ T cells in vivo, 100 μg of anti-CD8α (53-6.7) (BioXcell) was administered to the B16OVA tumor-bearing mice by intraperitoneal injection 1 day before SNVac-L treatment and every 4 day thereafter for five times. The depletion of CD8+ T cells in spleen was confirmed by flow cytometry.
IFNAR blocking assay
For the IFNAR blocking, 100 µg of anti-IFNARα (MAR1-5A3) (BioXcell) was administered to the C57BL/6 mice by intraperitoneal injection 1 day before SNVac-L treatment and every 4 day thereafter for five times.
Analysis of tumor-infiltrating immune cells
The B16-OVA, Hepa1-6-Luc or 4T1-Luc tumor-bearing mice were treated as described above, and tumor tissues were collected at indicated time points. Tumor tissues were processed through mechanical disruption and digested by collagenase IV (0.2 mg/mL), hyaluronidase (0.2 mg/mL) and DNase I (0.1 mg/mL) for 90 min at 37 °C. The cells were then filtered through 200 mesh nylon filters and washed three times with PBS to obtain single-cell suspension. The RBC were then lysed using RBC lysis buffer. The collected cells were stained with corresponding antibodies to analyze tumor-infiltrating CD4+ T cells and CD8+ T cells, NK cells, IFN-γ+CD8+ T cells, IFN-γ+CD4+ T cells, IFN-γ+ NK cells, Treg, MDSC, M2-TAM and M1-TAM (Supplementary Table 1).
Statistical analysis
All data were presented as mean ± SD. Statistical analysis was performed using GraphPad Prism software 8.2.1. Two-tailed Student’s t-test and one-way analysis of variance (ANOVA) with a Tukey post-hoc test were used for the statistical comparison between the two groups and among multiple groups, respectively. The survival study was analyzed through log-rank (Mantel-Cox) test. No statistical method was used to predetermine sample size. No data were excluded from the analyses. The investigators were not blinded to allocation during experiments and outcome assessment.
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Data availability
The RNA-seq data generated in this study have been deposited in the NCBI SRA database under accession code PRJNA1232983 and PRJNA1233188. All data are included in the Supplementary Information or available from the authors, as are unique reagents used in this Article. The raw numbers for charts and graphs are available in the Source Data file whenever possible. Source data are provided with this paper.
References
Saxena, M., van der Burg, S. H., Melief, C. J. M. & Bhardwaj, N. Therapeutic cancer vaccines. Nat. Rev. Cancer 21, 360–378 (2021).
Shemesh, C. S. et al. Personalized cancer vaccines: clinical landscape, challenges, and opportunities. Mol. Ther. 29, 555–570 (2021).
Sahin, U. & Tureci, O. Personalized vaccines for cancer immunotherapy. Science 359, 1355–1360 (2018).
Sayour, E. J., Boczkowski, D., Mitchell, D. A. & Nair, S. K. Cancer mRNA vaccines: clinical advances and future opportunities. Nat. Rev. Clin. Oncol. 21, 489−500 (2024).
Peri, A. et al. The landscape of T cell antigens for cancer immunotherapy. Nat. Cancer 4, 937–954 (2023).
Fan, T. et al. Therapeutic cancer vaccines: advancements, challenges, and prospects. Signal Transduct. Target Ther. 8, 450 (2023).
Hu, A. et al. Harnessing innate immune pathways for therapeutic advancement in cancer. Signal Transduct. Target Ther. 9, 68 (2024).
Samson, N. & Ablasser, A. The cGAS-STING pathway and cancer. Nat. Cancer 3, 1452–1463 (2022).
Chen, Q., Sun, L. & Chen, Z. J. Regulation and function of the cGAS-STING pathway of cytosolic DNA sensing. Nat. Immunol. 17, 1142–1149 (2016).
Vanpouille-Box, C., Hoffmann, J. A. & Galluzzi, L. Pharmacological modulation of nucleic acid sensors - therapeutic potential and persisting obstacles. Nat. Rev. Drug Discov. 18, 845–867 (2019).
Lind, N. A., Rael, V. E., Pestal, K., Liu, B. & Barton, G. M. Regulation of the nucleic acid-sensing Toll-like receptors. Nat. Rev. Immunol. 22, 224–235 (2022).
Chen, F. et al. Acid-ionizable iron nanoadjuvant augments STING activation for personalized vaccination immunotherapy of cancer. Adv. Mater. 35, e2209910 (2022).
Chen, F. et al. Nanobiomaterial-based vaccination immunotherapy of cancer. Biomaterials 270, 120709 (2021).
Shae, D. et al. Endosomolytic polymersomes increase the activity of cyclic dinucleotide STING agonists to enhance cancer immunotherapy. Nat. Nanotechnol. 14, 269–278 (2019).
Lynn, G. M. et al. Peptide-TLR-7/8a conjugate vaccines chemically programmed for nanoparticle self-assembly enhance CD8 T-cell immunity to tumor antigens. Nat. Biotechnol. 38, 320–332 (2020).
Yang, K. et al. Zinc cyclic di-AMP nanoparticles target and suppress tumours via endothelial STING activation and tumour-associated macrophage reinvigoration. Nat. Nanotechnol. 17, 1322–1331 (2022).
Kuai, R., Ochyl, L. J., Bahjat, K. S., Schwendeman, A. & Moon, J. J. Designer vaccine nanodiscs for personalized cancer immunotherapy. Nat. Mater. 16, 489–496 (2017).
Wu, Y. T. et al. Tumor-targeted delivery of a STING agonist improvescancer immunotherapy. Proc. Natl. Acad. Sci. USA 119, e2214278119 (2022).
Wu, X. et al. A HER2-targeting antibody-MMAE conjugate RC48 sensitizes immunotherapy in HER2-positive colon cancer by triggering the cGAS-STING pathway. Cell Death Dis. 14, 550 (2023).
Duvall, J. R. et al. Discovery and optimization of a STING agonist platform for application in antibody drug conjugates. J. Med Chem. 66, 10715–10733 (2023).
Xu, J. et al. A general strategy towards personalized nanovaccines based on fluoropolymers for post-surgical cancer immunotherapy. Nat. Nanotechnol. 15, 1043–1052 (2020).
Luo, M. et al. A STING-activating nanovaccine for cancer immunotherapy. Nat. Nanotechnol. 12, 648–654 (2017).
Gong, N. et al. Proton-driven transformable nanovaccine for cancer immunotherapy. Nat. Nanotechnol. 15, 1053–1064 (2020).
Zhang, X., Yang, B., Ni, Q. & Chen, X. Materials engineering strategies for cancer vaccine adjuvant development. Chem. Soc. Rev. 52, 2886–2910 (2023).
Ye, T., Li, F., Ma, G. & Wei, W. Enhancing therapeutic performance of personalized cancer vaccine via delivery vectors. Adv. Drug Deliv. Rev. 177, 113927 (2021).
Weiden, J., Tel, J. & Figdor, C. G. Synthetic immune niches for cancer immunotherapy. Nat. Rev. Immunol. 18, 212–219 (2018).
Lee, S. N., Jin, S. M., Shin, H. S. & Lim, Y. T. Chemical strategies to enhance the therapeutic efficacy of toll-like receptor agonist based cancer immunotherapy. Acc. Chem. Res 53, 2081–2093 (2020).
Macagno, A., Napolitani, G., Lanzavecchia, A. & Sallusto, F. Duration, combination and timing: the signal integration model of dendritic cell activation. Trends Immunol. 28, 227–233 (2007).
Napolitani, G., Rinaldi, A., Bertoni, F., Sallusto, F. & Lanzavecchia, A. Selected Toll-like receptor agonist combinations synergistically trigger a T helper type 1-polarizing program in dendritic cells. Nat. Immunol. 6, 769–776 (2005).
Jin, S. M. et al. A nanoadjuvant that dynamically coordinates innate immune stimuli activation enhances cancer immunotherapy and reduces immune cell exhaustion. Nat. Nanotechnol. 18, 390–402 (2023).
Glorieux, C., Liu, S., Trachootham, D. & Huang, P. Targeting ROS in cancer: rationale and strategies. Nat. Rev. Drug Discov. 23, 583–606 (2024).
Li, X. et al. Precise modulation and use of reactive oxygen species for immunotherapy. Sci. Adv. 10, eadl0479 (2024).
Hu, Z. et al. SENP3 senses oxidative stress to facilitate STING-dependent dendritic cell antitumor function. Mol. Cell 81, 940–952 e945 (2021).
Cubillos-Ruiz, J. R. et al. ER stress sensor XBP1 controls anti-tumor immunity by disrupting dendritic cell homeostasis. Cell 161, 1527–1538 (2015).
Miller, I. C. et al. Enhanced intratumoural activity of CAR T cells engineered to produce immunomodulators under photothermal control. Nat. Biomed. Eng. 5, 1348–1359 (2021).
Wu, Y. et al. Control of the activity of CAR-T cells within tumours via focused ultrasound. Nat. Biomed. Eng. 5, 1336–1347 (2021).
Wang, D. et al. Engineering nanoparticles to locally activate T cells in the tumor microenvironment. Sci. Immunol. 4, eaau6584 (2019).
Ma, X. et al. Modular-designed engineered bacteria for precision tumor immunotherapy via spatiotemporal manipulation by magnetic field. Nat. Commun. 14, 1606 (2023).
Feng, B. et al. Self-amplified drug delivery with light-inducible nanocargoes to enhance cancer immunotherapy. Adv. Mater. 31, e1902960 (2019).
Li, Y. et al. Nanosensitizer-mediated augmentation of sonodynamic therapy efficacy and antitumor immunity. Nat. Commun. 14, 6973 (2023).
Sun, S. C. Non-canonical NF-kappaB signaling pathway. Cell Res 21, 71–85 (2011).
Morgan, M. J. & Liu, Z. G. Crosstalk of reactive oxygen species and NF-kappaB signaling. Cell Res 21, 103–115 (2011).
West, A. P. & Shadel, G. S. Mitochondrial DNA in innate immune responses and inflammatory pathology. Nat. Rev. Immunol. 17, 363–375 (2017).
Riley, J. S. & Tait, S. W. Mitochondrial DNA in inflammation and immunity. EMBO Rep. 21, e49799 (2020).
Chen, C. & Xu, P. Cellular functions of cGAS-STING signaling. Trends Cell Biol. 33, 630–648 (2023).
Zhang, L. et al. NF-kappaB activation enhances STING signaling by altering microtubule-mediated STING trafficking. Cell Rep. 42, 112185 (2023).
Ding, Y., Li, Z., Jaklenec, A. & Hu, Q. Vaccine delivery systems toward lymph nodes. Adv. Drug Deliv. Rev. 179, 113914 (2021).
Tian, R., Ke, C., Rao, L., Lau, J. & Chen, X. Multimodal stratified imaging of nanovaccines in lymph nodes for improving cancer immunotherapy. Adv. Drug Deliv. Rev. 161-162, 145–160 (2020).
Fang, L. et al. Engineering autologous tumor cell vaccine to locally mobilize antitumor immunity in tumor surgical bed. Sci. Adv. 6, eaba4024 (2020).
Ochyl, L. J. et al. PEGylated tumor cell membrane vesicles as a new vaccine platform for cancer immunotherapy. Biomaterials 182, 157–166 (2018).
Chen, L. et al. Bacterial cytoplasmic membranes synergistically enhance the antitumor activity of autologous cancer vaccines. Sci. Transl. Med. 13, eabc2816 (2021).
Qiao, G. et al. Surgical tumor-derived nanoplatform targets tumor-associated macrophage for personalized postsurgical cancer immunotherapy. Sci. Adv. 10, eadk7955 (2024).
Bianchini, G., De Angelis, C., Licata, L. & Gianni, L. Treatment landscape of triple-negative breast cancer - expanded options, evolving needs. Nat. Rev. Clin. Oncol. 19, 91–113 (2022).
Garrido-Castro, A. C., Lin, N. U. & Polyak, K. Insights into molecular classifications of triple-negative breast cancer: improving patient selection for treatment. Cancer Discov. 9, 176–198 (2019).
Yang, J. D. et al. A global view of hepatocellular carcinoma: trends, risk, prevention and management. Nat. Rev. Gastroenterol. Hepatol. 16, 589–604 (2019).
Cai, Z. et al. Personalized neoantigen vaccine prevents postoperative recurrence in hepatocellular carcinoma patients with vascular invasion. Mol. Cancer 20, 164 (2021).
Sangro, B., Sarobe, P., Hervas-Stubbs, S. & Melero, I. Advances in immunotherapy for hepatocellular carcinoma. Nat. Rev. Gastroenterol. Hepatol. 18, 525–543 (2021).
Chen, H. et al. Personalized neoantigen vaccine combined with PD-1 blockade increases CD8(+) tissue-resident memory T-cell infiltration in preclinical hepatocellular carcinoma models. J. Immunother. Cancer 10, e004389 (2022).
Guo, J. & Huang, L. Nanodelivery of cGAS-STING activators for tumor immunotherapy. Trends Pharmacol. Sci. 43, 957–972 (2022).
Wang, F. et al. Tumour sensitization via the extended intratumoural release of a STING agonist and camptothecin from a self-assembled hydrogel. Nat. Biomed. Eng. 4, 1090–1101 (2020).
Li, S. et al. Prolonged activation of innate immune pathways by a polyvalent STING agonist. Nat. Biomed. Eng. 5, 455–466 (2021).
Zhou, M. et al. Multifunctional STING-activating Mn(3) O(4) @Au-dsDNA/DOX nanoparticle for antitumor immunotherapy. Adv. Health. Mater. 9, e2000064 (2020).
Sun, X. et al. Amplifying STING activation by cyclic dinucleotide-manganese particles for local and systemic cancer metalloimmunotherapy. Nat. Nanotechnol. 16, 1260–1270 (2021).
Dane, E. L. et al. STING agonist delivery by tumour-penetrating PEG-lipid nanodiscs primes robust anticancer immunity. Nat. Mater. 21, 710–720 (2022).
Liang, J. et al. Nanoparticle-enhanced chemo-immunotherapy to trigger robust antitumor immunity. Sci. Adv. 6, eabc3646 (2020).
Acknowledgements
This work was supported by the National Natural Science Foundation of China (U22A20328 and W2412035 to H.J.Y., 22474042 to Z.A.X), Science and Technology Commission of Shanghai Municipality (23490712700 to Z.A.X., 24430713500 and 23ZR1475000 to H.J.Y.), Shanghai Oriental Talents Program (BJKL2024046 to Z.A.X.), Open Funds of State Key Laboratory of Drug Research (SKLDR-2023-KF-09 to H.J.Y.). The Mass Spectrometry System and the cell sorter BD Influx of the National Facility for Protein Science in Shanghai (NFPS), Shanghai Advanced Research Institute, CAS are gratefully acknowledged. All animal procedures were carried out under the guidelines approved by the Institutional Animal Care and Use Committee (IACUC) of the Shanghai Institute of Materia Medica, CAS.
Author information
Authors and Affiliations
Contributions
F.C., Z.X. and H.Y. designed the study. F.C. and H.Y. wrote the primary manuscript. F.C., H.Z. and S.L. conducted the experiments and analyzed the data. S.R., L.H. and Z.C. assisted with experiments. L.Y., M.Z., X.L., Z.X. and H.Y. revised the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Communications thanks the anonymous reviewer(s) for their contribution to the peer review of this work. A peer review file is available.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Source data
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Chen, F., Zhang, H., Li, S. et al. Engineering STING Nanoadjuvants for spatiotemporally-tailored innate immunity stimulation and cancer vaccination therapy. Nat Commun 16, 5773 (2025). https://doi.org/10.1038/s41467-025-60927-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41467-025-60927-7