Abstract
Multiple sclerosis (MS) is an immune-mediated demyelinating disease. Epstein-Barr virus (EBV) encodes for the EBNA-1381-452 region that induces autoreactive antibody responses, which are likely critically involved in MS pathogenesis. Here we investigate whether these EBNA-1381-452-specific antibodies can serve as a biomarker to identify at-risk individuals for MS. We quantify EBNA-1381-452-specific antibody titers from 324 relapsing-remitting MS patients and 324 matched controls in longitudinal follow-up plasma samples, starting from the individual’s EBV-seroconversion. In MS patients, significantly elevated EBNA-1381-452-specific IgG titers are identified that are increased already as early as nine months after EBV-seroconversion (OR:5.7; 95% CI: 4.1-8.1; P < 0.0001) and a median 5.4 years prior to MS diagnosis. Especially, the presence of continuously high EBNA-1381-452-specific antibody titers is associated with a more rapid MS diagnosis after EBV-seroconversion (P < 0.0001). Thus, the quantification of EBNA-1381-452-specific IgG antibody levels may provide a prognostic biomarker to determine the individual’s risk for the diagnosis of MS.
Similar content being viewed by others
Introduction
Multiple sclerosis (MS) is a chronic, autoinflammatory and demyelinating disease of the central nervous system (CNS) and the most common disabling neurological disorder in young adults1. Despite a globally rising prevalence and an estimated 2.8 million (35.9/100,000) people living with MS2, no reliable screening strategy currently exists for the identification of individuals at risk of future MS.
The pathology of MS, i.e., demyelination and axonal damage, are the result of an initial autoimmune-mediated inflammation, and it has been suggested that Epstein-Barr virus (EBV) may be critically involved in these processes3,4,5. Especially, it has been shown that specific immune responses directed against a highly conserved peptide sequence within the EBV nuclear antigen (EBNA)−1 region, EBNA-1381-452, cross-react with distinct CNS-derived proteins and may thus elicit autoreactive immune processes6. Recent studies have demonstrated that MS patients have developed elevated antibody titers against specific peptides within the EBNA-1381-452 region7, and that these antibodies cross-react with the distinct CNS-derived proteins, such as the Glial Cell Adhesion Molecule (GlialCAM), Alpha-Crystallin B Chain (CRYAB), Myelin Basic Protein (MBP), and Anoctamin 2 (ANO2), respectively8,9,10,11. Based on these findings, we have investigated whether the quantification of EBNA-1381-452-specific IgG antibody titers could serve as a biomarker for the identification of individuals who are at risk of future MS.
Results
Establishment of EBNA-1381-452-specific IgG ELISA
First, the EBNA-1381-452-specific IgG ELISA was established and validated using an EBNA-1381-452-derived peptide pool as antigen. The test showed low inter- and intra-assay variability, as assessed by repeated testing of plasma samples from 15 EBV-seropositive and 15 EBV-seronegative healthy blood donors (Table S4). Then, the test cut-off for the detection of EBNA-1381-452-specific IgG antibodies was calculated using plasma samples from an additional 25 EBV-seronegative blood donors. An optical density (OD) of ≥0.32 was determined as cut-off for a positive EBNA-1381-452-specific IgG antibody titer. We then tested the plasma samples, obtained from all 704 EBV-EBNA-1-seropositive MS patients of our cohort at the time point of MS diagnosis, as well as the samples obtained from 5381 EBV-EBNA-1-seropositive control persons by the EBNA-1381-452-specific IgG ELISA. As shown in Figs. 1A, 97.9% of all MS patients and 77.9% of all controls had detectable EBNA-1381-452-specific IgG antibody titers (OR: 12.6, 95% CI: 7.6-219, P < 0.0001).
EBNA-1381-452-specific IgG titers were quantified in N = 704 MS patients and N = 5381 controls by ELISA. A Bars represent the number of MS patients and controls with detectable (OD ≥ 0.32) EBNA-1381-452-specific IgG antibody titers. Groups were compared using the two-sided Fisher’s exact test. B Violin plots represent the EBNA-1381-452-specific IgG antibody titers of EBNA-1381-452-specific IgG antibody seropositive MS patients (N = 689) and controls (N = 4189). Each data point represents one individual control or MS patient. Black lines indicate the median OD as well as the first and third quartiles. Dashed black lines indicate the cut-off for detection of EBNA-1381-452-specific IgG antibody (OD ≥ 0.32). Groups were compared using the two-sided Mann-Whitney Test. C Forest plot for the discrimination of MS patients and controls based on the EBNA-1381-452-specific IgG antibody titers. The number of MS patients (N = 704) and controls (N = 5381) with EBNA-1381-452-specific IgG antibody titers above the indicated cut-offs were compared using Fisher’s exact test. The individual OR (±95% CI) for each cut-off is shown. D Two-sided ROC analysis (not correct for multiple comparisons) to discriminate between EBNA-1381-452 IgG antibody seropositive MS patients (N = 689) and controls (N = 4189). E Distribution of MS patients and controls with high-level (OD ≥ 1.7), low level (OD ≤ 1.69 – ≥0.32), and absent (OD ≤ 0.31) EBNA-1381-452-specific antibody titers. Groups were compared using the Chi-square test. F, G EBNA-1381-452-specific IgG antibody titers are associated with axonal damage and MS disease severity. F Blots represent the number of MRI MS lesion in MS patients with high-level, low level, and absent EBNA-1381-452-specific antibody titers. Groups were compared using the Chi-square test. G Plasma NfL concentrations were quantified in N = 704 MS patients at the time point of MS diagnosis by SIMOA. Blots represent the mean plasma NfL concentrations in MS patients with high-level, low level, and absent EBNA-1381-452-specific antibody titers. Plasma NfL concentrations were compared between the groups using two-sided ANOVA and Dunn’s Post-Test. Source data are provided as a Source Data file. AUC: Area under the curve, EBNA-1: Epstein–Barr Virus Nuclear Antigen 1, MRI: Magnetic Resonance Imaging, MS: Multiple Sclerosis, NfL: Neurofilament Light Chain, OD: Optical Density. OR: Odds Ratio.
High-level EBNA-1381-452-specific IgG antibody titers are detectable at the time of MS diagnosis
Subsequently, the difference of EBNA-1381-452-specific IgG antibody titers in patients diagnosed with MS and healthy control persons was assessed by quantifying the EBNA-1381-452-specific IgG antibody titers of all EBNA-1381-452 IgG seropositive MS patients (N = 689, 97.7%) and controls (N = 4189, 77.9%). As shown in Fig. 1B, C, significantly higher EBNA-1381-452-specific IgG antibody titers were detected by the ELISA in MS patients, compared to controls (mean OD: 2.2 vs. 1.2, P < 0.0001).
Based on these data, we further investigated whether there is a specific cut-off that may define an EBNA-1381-452-specific IgG titer that is associated with MS. Using ROC analysis, a cut-off was determined (Fig. 1D, Table S5), and EBNA-1381-452-specific IgG antibody titers exceeding an OD ≥ 1.7 were significantly more often identified in patients at the time of MS diagnosis (Fig. 1E). In contrast, lower EBNA-1381-452-specific IgG titers, between OD ≥ 0.32 and OD ≤ 1.69, were predominantly found in the control cohort. Additionally, specific cut-off-values for male and female, as well as adult and pediatric persons were calculated. As shown in Fig. S2, the same cut-off of OD ≥ 1.7 was calculated for discrimination between MS patients and controls in male and female, as well as in adult and pediatric individuals.
High-level EBNA-1381-452-specific IgG antibody titers are associated with MS disease severity
We next analyzed whether EBNA-1381-452-specific IgG antibody titers are associated with surrogate markers of disease severity at the time of MS diagnosis. Therefore, we correlated the EBNA-1381-452-specific IgG antibody titers with the number of T2 MRI brain lesions in the individual patients at MS diagnosis. As shown in Fig. 1F and Fig. S3, in patients with high-level (OD ≥ 1.7) EBNA-1381-452-specific IgG antibody titers, >10 T2 MRI brain lesions were observed significantly more frequently.
We also determined the plasma concentration of neurofilament light chain (NfL) and plasma glial fibrillary acidic protein (GFAP), biomarkers reflecting acute and chronic axonal damage and astrocytic activation, MRI lesion burden, disability progression, and relapse risk12,13,14, from all MS patients at the time point of MS diagnosis. MS patients with high-level EBNA-1381-452-specific IgG antibody titers had significantly higher NfL (Fig. 1G) and GFAP (Fig. S4A) plasma concentrations, compared to MS patients with low or undetectable EBNA-1381-452-specific IgG titers. Additionally, we compared the EBNA-1381-452-specific IgG antibody titers and the plasma NfL and GFAP concentrations specifically in male and female, as well as adult and pediatric MS patients. As shown in Fig. S4B-E and Fig. S5, higher plasma NfL and GFAP concentrations were observed independent of age and gender, reflecting a higher level of axonal damage in MS patients with high-level EBNA-1381-452-specific IgG antibody titers.
High-level EBNA-1381-452-specific IgG antibody titers develop already early after primary EBV infection
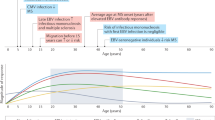
As the level of EBNA-1381-452-specific antibodies was found to be associated with MS, we further investigated the time point of emergence of these antibodies in the individual host after EBV seroconversion. Therefore, we selected all MS patients from the entire study cohort in whom the time point of EBV seroconversion could be retrospectively identified and from whom follow-up plasma samples were available between EBV seroconversion and MS diagnosis (Table 1). A total of 324 patients met these criteria and 324 controls could be matched to these patients according to the sampling time points, gender, age, time to seroconversion, and occurrence of IM (Table S1). From all patients and controls, we tested one plasma sample obtained during the period of EBV seroconversion, and four follow-up plasma samples in median nine-month intervals thereafter employing the EBNA-1381-452-specific IgG ELISA, thus covering an overall period of three years (Fig. 2A).
A Illustration of the included time points. EBNA-1381-452-specific IgG antibody titers were quantified from N = 324 MS patients and N = 324 controls at the time point of EBV seroconversion, median 8.9 months after EBV seroconversion (time point 1), median 17.8 months after EBV seroconversion (time point 2), median 26.9 months after EBV seroconversion (time point 3), median 36 months after EBV seroconversion (time point 4), and at the MS diagnosis or a matched time point for controls (median 97.2 months after EBV seroconversion). Created in BioRender. Vietzen, H. (https://BioRender.com/o5v1dep). (B) EBNA-1381-452-specific IgG antibody titers from individual MS patients (N = 324) and controls (N = 324) are shown for each individual time point. Boxes represent the mean EBNA-1381-452-specific IgG antibody titer for each individual time point. EBNA-1381-452-specific IgG antibody titers were compared between individual MS patients and controls for each individual time point using two-sided ANOVA and Dunn’s post-hoc test. C Distribution of high-level (OD ≥ 1.7), low level (OD ≤ 1.69 – ≥0.32), and absent (OD ≤ 0.31) EBNA-1381-452-specific IgG antibody titers is shown for each individual time point. The frequency of high-level, low level, and absent EBNA-1381-452-specific antibody titers was compared using the Chi-square test. D Forest plot for the discrimination of MS patients and controls based on the EBNA-1381-452-specific antibody titers: For each individual time point, the number of MS patients and controls with high-level EBNA-1381-452-specific antibody titers was compared to MS patients and controls with low-level and absent EBNA-1381-452-specific antibody titers (Fig. 2C) using the Fisher’s exact test. The individual ORs (±95% CI) for each comparison is shown Source data are provided as a Source Data file. EBNA-1: Epstein–Barr Virus Nuclear Antigen 1, EBV: Epstein-Barr virus, MS: Multiple Sclerosis, OR: Odds Ratio, T: Time point.
As shown in Fig. 2B and Fig. S6, EBNA-1381-452-specific IgG antibodies were undetectable at the time of EBV seroconversion, but developed thereafter and were detectable at all time points (T1-T4) after symptomatic (IM) and asymptomatic EBV seroconversion. EBNA-1381-452-specific IgG antibody titers of MS patients significantly exceeded those of controls. The distribution of high-level, low-level, and negative EBNA-1381-452-specific IgG antibody titers for all time points is presented in Fig. 2C. MS patients showed a significantly higher frequency of high-level EBNA-1381-452-specific IgG antibody titers for all time points than controls (Fig. 2D). These high-level EBNA-1381-452-specific IgG antibody titers were identified in MS patients up to 12.23 years and a median 5.4 years (interquartile range (IQR) of 3.4–8.63 years) prior to the MS diagnosis (Fig. S7).
Repeated High-Level EBNA-1381-452-Specific IgG Antibody Titers over Time Predict the Development of MS
Although the majority of MS patients developed high-level EBNA-1381-452-specific IgG antibody titers after EBV seroconversion, high-level antibody levels were identified also in individual samples of control persons, which did not allow a clear identification of individuals with an MS diagnosis in the follow-up from a single test result. Therefore, we further analyzed, whether MS patients show a more continuous presence of high-level EBNA-1381-452-specific IgG antibody titers over time compared to controls.
In Fig. 3A, the number of high-level EBNA-1381-452-specific IgG antibody titers, detected in the four follow-up samples of MS patients and controls, is presented. In 96% of the MS patients, high-level EBNA-1381-452-specific IgG titers were present in ≥2/4 samples taken within three years after EBV seroconversion, while this was the case only in 5.6% of the controls. The detection of high-level EBNA-1381-452-specific IgG antibody titers in two or more samples was thus associated with a highly increased risk for further MS diagnosis (OR: 406.7; 95%CI: 197.2-829.9; P < 0.0001). Presence of high-level EBNA-1381-452-specific IgG antibody titers at three or four time points in the follow up was even exclusively found in MS patients.
EBNA-1381-452-specific IgG antibody titers from N = 324 MS patients and N = 324 controls were quantified at time point of EBV seroconversion, median 8.9 months after EBV seroconversion (time point 1), median 17.8 months after EBV seroconversion (time point 2), median 26.9 months after EBV seroconversion (time point 3), and median 36 months after EBV seroconversion (time point 4). The number of MS patients and controls with high-level EBNA-1381-452-specific IgG antibody titers (OD ≥ 1.7), was then assessed for time point 1, time point 2, time point 3 and time point 4. A Data are shown as the cumulative number of time points with high-level EBNA-1381-452-specific IgG antibody titers. Groups were compared using the Chi-square test. B The time point of MS diagnosis was compared to the cumulative numbers of time points with high-level EBNA-1381-452-specific IgG antibody titers using the two-sided Gehan-Breslow-Wilcoxon Test. C The time point of MS disease onset was compared to the cumulative numbers of time points with high-level EBNA-1381-452-specific IgG antibody titers using the two-sided Gehan-Breslow-Wilcoxon Test. EBNA-1: Epstein–Barr Virus Nuclear Antigen 1, EBV: Epstein-Barr virus, MS: Multiple Sclerosis, T: Time point.
Thus, the repeated detection of high-level EBNA-1381-452-specific IgG antibody titers in an individual, already within three years after EBV seroconversion, is highly predictive for the later MS diagnosis.
Continuously high-level EBNA-1381-452-specific IgG antibody titers predict the time to MS disease onset diagnosis
We then also assessed whether the repeated detection of high-level EBNA-1381-452-specific IgG antibody titers in all samples after EBV seroconversion is associated with the time to the MS diagnosis as well as the MS disease onset. As shown in Fig. 3B, the presence of high-level EBNA-1381-452-specific IgG antibody titers in all four samples tested was associated with a significantly shorter time to the MS diagnosis (median 4.38 years after EBV seroconversion) in contrast to patients in whom not always high-level EBNA-1381-452-specific IgG antibody titers were detected (median 7.88 years after EBV seroconversion, P < 0.0001) as well as compared to 4% of the MS patients in whom these antibodies were never detected (median 9.6 years after EBV seroconversion, P < 0.0001).
As shown in Fig. 3C, the presence of high-level EBNA-1381-452-specific IgG antibody titers in all four samples tested was also associated with a significantly shorter time to the MS disease onset (median 3.99 years after EBV seroconversion), compared to MS patients in whom not always high-level EBNA-1381-452-specific IgG antibody titers were detected (median 7.06 years after EBV seroconversion, P < 0.0001) as well as compared to the MS patients in whom EBNA-1381-452-specific IgG antibodies were never detected (median 9.09 years after EBV seroconversion, P < 0.0001).
Additionally, we compared the time to the MS diagnosis as well as the MS disease onset, specifically between male and female, as well as adult and pediatric MS patients. As shown in Fig. S8 and Fig. S9, the presence of high-level EBNA-1381-452-specific IgG antibody titers in all four samples tested was associated with a significantly shorter time to the MS diagnosis (Fig. S8) as well as the MS disease onset (Fig. S9) in male and female, as well as adult and pediatric MS patients.
Thus, continuous presence of high-level EBNA-1381-452-specific IgG antibody titers in individuals within three years after EBV seroconversion is associated with an early MS diagnosis and MS disease onset.
Comparison of the high-level EBNA-1381-452-specific IgG antibody titers with plasma NfL and GFAP in predicting MS
We then aimed to compare the increase of plasma NfL and GFAP to our newly established EBNA-1381-452-specific IgG ELISA, allowing the prognosis of MS by detection of high-level EBNA-1381-452-specific IgG antibody titers. We therefore determined the plasma NfL and GFAP levels in the longitudinal cohort at the time point of EBV seroconversion, all four follow-up time points post-EBV seroconversion (T1–T4), and at the time point of MS diagnosis, or at matched time points for controls. As shown in Fig. 4A–B, neither plasma NfL nor GFAP levels were significantly different between MS patients and controls at time point 1 and time point 2, when EBNA-1381-452-specific IgG antibody titers of MS patients already significantly exceeded those of controls (Fig. 2B–C). Thus, EBNA-1381-452-specific IgG antibody titers seem to allow for the earlier prediction of MS than plasma NfL and GFAP levels.
EBNA-1381-452-specific IgG antibody titers, plasma NfL and plasma GFAP concentrations were quantified from N = 324 MS patients and N = 324 controls at the time point of EBV seroconversion, median 8.9 months after EBV seroconversion (time point 1), median 17.8 months after EBV seroconversion (time point 2), median 26.9 months after EBV seroconversion (time point 3), and median 36 months after EBV seroconversion (time point 4). Plasma (A) NfL and (B) GFAP concentrations from individual MS patients and controls are shown for each individual time point. Boxes represent the mean (A) NfL and (B) GFAP concentration for each individual time point. Plasma (A) NfL and (B) GFAP concentrations were compared between the groups using two-sided ANOVA and Dunn’s Post-Test. C, D Plasma (C) NfL and (D) GFAP concentrations were compared between controls and MS patients with 0/4, 1/4, 2/4, 3/4, and 4/4 time points with high-level (OD ≥ 1.7) EBNA-1381-452-specific IgG antibody titers using two-sided ANOVA and Dunn’s Post-Test. Source data are provided as a Source Data file.EBNA-1: Epstein–Barr Virus Nuclear Antigen 1, EBV: Epstein-Barr virus, GFAP: Glial Fibrillary Acidic Protein, MS: Multiple Sclerosis, NfL: Neurofilament Light Chain, T: Time point.
As we have shown that a more continuous presence of high-level EBNA-1381-452-specific IgG titers is associated with earlier MS diagnosis, we also investigated whether this is also associated with higher axonal damage and astrocytic activation in MS patients, as reflected by the plasma NfL and GFAP concentrations at time point 4. As shown in Fig. 4C-D, continuous presence of high-level EBNA-1381-452-specific IgG antibody titers at three and especially four time points after EBV seroconversion was associated with significantly increased NfL and GFAP plasma levels at time point 4 in MS patients.
Thus, in individuals with constantly present high-level EBNA-1381-452-specific IgG antibody titers, there is already a high-level of axonal damage and astrocytic activation three years post EBV-seroconversion.
The development of high-level EBNA-1381-452-specific antibodies precedes axonal damage and astrocytic activation in MS
We finally analyzed to which extent the development of high-level EBNA-1381-452-specific IgG antibody titers precede the axonal damage and astrocytic activation in MS patients. Therefore, we collected retrospective longitudinal follow-up plasma samples from all 324 MS patients and controls in median 9- or 18-month intervals from the time point of MS diagnosis, or a matched time point for controls, to time point 1, i.e., the first included time point in which EBNA-1381-452-specific IgG antibody titers were detectable (Table S2). We then determined in all samples the EBNA-1381-452-specific IgG antibody titer as well as the NfL and GFAP plasma levels. As shown in Fig. S10, the first detection of high-level EBNA-1381-452-specific IgG antibody titers preceded the increase of plasma NfL and GFAP levels in the individual MS patients by median 3.6 years (IQR: 2.2–7 years) and 3.8 years (IQR: 1.8–7 years), respectively, thus defining a time frame between the increase of EBNA-1381-452-specific IgG antibody titers and the occurrence of axonal damage and astrocytic activation in MS patients.
Discussion
Here, we show that the longitudinal and quantitative detection of distinct EBNA-1381-452-specific IgG antibodies by ELISA allows for the early identification of individuals at risk for MS. This serologic biomarker allows the early, reliable, and non-invasive identification of people likely to be diagnosed with MS.
It has been shown earlier that antibodies against different EBNA-1381-452-derived peptides may develop after EBV infection7, and that these are cross-reactive against distinct CNS-derived proteins8,9,10,11. The EBNA-1381-452-specific IgG ELISA applied in this study allows the quantitative detection of a specific panel of these antibodies that cross-react with the CNS GlialCAM370–389– (EBNA-1386–4057,9), CRYAB2–21– (EBNA-1393–4127,10), MBP205–224– (EBNA-1409–4287,11), and ANO2135–154– (EBNA-1426–4457,8) derived epitopes, and revealed that persons may develop repeatedly high-level antibodies against this broad range of peptides already within nine months after EBV primary infection.
So far, studies have analyzed only the total EBNA-1-specific antibody titers and found a moderate or even absent association between high overall EBNA-1-specific antibody titers, in blood or cerebrospinal fluid (CSF) and the diagnosis of MS15,16,17,18. Here, we demonstrate that, in contrast, a peptide-specific, EBNA-1381-452-derived antibody assay is needed to significantly predict MS diagnosis. And, importantly, it is the repeated longitudinal analysis of these EBNA-1381-452-peptide-derived antibody titers rather than single-point measurements, which is highly predictive for the diagnosis of MS.
In particular, our data revealed that nearly all persons, in whom high-level EBNA-1381-452-specific IgG were detected repeatedly in plasma within three years after EBV seroconversion, were diagnosed with MS in the follow-up. In addition, all individuals in whom high-level antibody titers were detected continuously at all time points analyzed were diagnosed with MS already within seven years after EBV infection. This confirms that the EBNA-1381-452-specific IgG antibody titers are an excellent marker predicting the diagnosis of MS.
From a practical point of view, the EBNA-1381-452-specific IgG ELISA could be applied as a follow-up serological investigation in populations at risk for MS, such as individuals after a clinically apparent IM. Subsequent screening for MS lesions via MRI in individuals with repeated high-level EBNA-1381-452-specific IgG titers within 27 months after EBV-seroconversion might be a useful first step to identify individuals at risk for MS at an early time point.
In our study cohort, EBNA-1381-452-specific antibody titers were detectable in the majority of all EBNA-1 seropositive controls. Interestingly, nearly all female controls had detectable EBNA-1381-452-specific antibody titers, while males were more often EBNA-1381-452 seronegative. Although our study found no significant differences in the EBNA-1381-452-specific antibody titers between EBNA-1381-452 seropositive males and females, these data are of special interest, as the female gender is a known risk factor for MS19,20. Therefore, higher EBNA-1381-452 seroprevalence may contribute to some extent to the increased risk of MS in females.
Biological sex and sex hormones are thought to influence MS by affecting immune responses, inflammation, myelination, and neurodegeneration21. While studies on the influence of sex hormones in MS patients are predominantly involving cisgender populations, in our study, one MS patient was identified as non-binary. This highlights the need for further research that includes transgender and gender-diverse individuals.
Until now, reliably identifying individuals at risk for MS has not been possible. Pre-symptomatic patients have been so far only incidentally identified because of an MRI examination done for reasons other than MS, such as brain trauma, headaches or fear of brain tumor. However, it is for a plethora of reasons highly unlikely that MRI examinations will enter routine practice as a screening tool for MS. Moreover, even if it is speculated that MRI will serve for this purpose, pre-clinical MRI diagnosis is limited to those individuals with already morphological changes on MRI, thus, being unable to identify those individuals at risk in a prodromal phase of MS.
In our study, high-level EBNA-1381-452-specific IgG antibody titers emerged, however, not only years before the first clinical MS symptoms, but also substantially prior to the increase of NfL and GFAP in plasma, which are markers of axonal damage and astrocytic activation12,13,14. These data are of special interest as high-level EBNA-1381-452-specific IgG antibody titers seem to develop early in the asymptomatic prodromal stage of MS, which may represent a window for early treatment to delay or even prevent conversion to clinical MS. Going along with our finding, a recently published study identified a highly specific, though not sensitive, antibody-based biomarker for high-risk MS patients with clinically or radiologically isolated syndrome22. Future studies are thus needed to compare the development of high-level EBNA-1381-452-specific IgG antibody titers with other potential biomarkers to identify patients at high risk for MS.
The detection of high-level EBNA-1381-452-specific IgG antibody titers cannot replace, but may be integrated as a valuable additional tool in validated standard diagnostic techniques for MS diagnosis to enhance sensitivity and specificity for MS risk prediction.
Our study had some limitations. Although we included only EBV EBNA-1 seropositive study participants, 2.1% of all MS patients did not develop detectable EBNA381-452-specific antibody responses between EBV seroconversion and MS diagnosis. Our findings are consistent with recently published studies that demonstrated that in rare cases MS may develop in EBV EBNA-1 seronegative MS patients23,24,25,26,27, highlighting that there is a minority of MS cases based on an EBV-independent pathogenesis. Future studies are needed to evaluate additional biomarkers, e.g., genetic risk factors, especially for these EBNA381-452-specific antibody-seronegative MS patients.
In addition, in our study, we focused on relapsing remitting MS (RRMS) patients. A recently published study demonstrated that EBV seropositive RRMS patients have significantly higher overall EBNA-1-specific antibody titers compared to primary progressive MS (PPMS) patients28. Further studies are thus needed to specifically evaluate the prognostic value of EBNA381-452-specific antibody responses in patients with PPMS and other MS subtypes.
Furthermore, our study was limited by its retrospective case-control design. Future research involving prospective validation cohorts is thus needed to confirm the predictive potential of elevated EBNA-1381-452-specific IgG antibody titers for the early identification of individuals at risk of developing MS.
The identification of early biomarkers before MS onset is of critical importance. As recent studies with patients with radiologically isolated syndrome highlighted29,30, stratification of the risk for MS before neuroaxonal damage and clinical deficits develop could allow timely intervention and alteration of the outcome for these patients, potentially preventing progression and reducing long-term disability.
In summary, we demonstrate that the quantification of high-level EBNA-1381-452-specific IgG antibody titers is a highly sensitive and reliable biomarker for the early identification of individuals at risk of future MS, which may provide an opportunity for early treatment prior to onset of MS.
Methods
Study design and participants
For this multi-center study, 704 EBV-EBNA-1-seropositive relapsing remitting MS (RRMS) patients were recruited. In all patients, MS was diagnosed according to the McDonald 2017 criteria31 between 2001 and 2023.
All MS patients were part of the part of the Vienna Multiple Sclerosis Database (VMSD) and the BIOMARKER study of the Children’s Hospital Datteln, Germany32,33,34,35. The following demographic and clinical data were included in the study: age, gender (based on self-reporting), and lesion load at disease onset. From each patient, at least one plasma sample was included, which was collected immediately after MS diagnosis (0–14 days) and prior to any MS-specific treatment, including high-dose corticosteroids for acute relapse treatment. At the time of MS diagnosis, T2-weighted magnetic resonance imaging (MRI) scans revealed that 51.1% of patients had between 3–9 brain lesions, while 48.9% had 10 or more brain lesions.
In addition, 5381 EBV-EBNA-1 seropositive control individuals were included in the study. Of these, 4134 (76.8%) were healthy blood donors. From 1247 (23.2%) controls, plasma samples were collected due to prophylactic medical examinations or vaccination titer controls. Details of the study cohort are shown in Table 1.
In 324 (46%) of the MS patients, the time point of EBV seroconversion could be retrospectively identified, and follow-up plasma samples were available in a 6–12 (median: 8.9) month interval from EBV seroconversion to the time point of MS diagnosis. MS was diagnosed 36–156 (median: 76.91) months after EBV seroconversion (Fig. S1A). The MS disease onset, as defined by the first occurrence of symptoms consistent with MS, occurred after 1–19 (mean: 7.92) months before the MS diagnosis.
In 264 of these MS patients with follow-up samples (81.5%), EBV seroconversion occurred in the course of clinically evident infectious mononucleosis (IM), confirmed by the triad of fever, lymphadenopathy, and tonsillitis (Table 1). In all patients with IM, EBV primary infection was further confirmed serologically by the presence of EBV viral-capsid antigen (VCA)-specific IgM in the absence of EBV-VCA- or EBV-EBNA-specific IgG antibodies. In all 264 patients with clinically evident IM, the time point of EBV seroconversion (T0) was defined as the first available plasma sample with VCA-IgM positive, VCA-IgG negative, and EBNA-IgG negative antibodies.
In 60 (18.5%) patients with MS, primary EBV infection had occurred asymptomatically, and, in these individuals, EBV seroconversion was confirmed by an additional plasma sample that was available and obtained at a median of 5.2 (3.2–7.2) months prior to the first detection of EBV-VCA-specific IgM or EBV-VCA- specific IgG. In all 60 patients with an asymptomatic EBV seroconversion, the time point of EBV seroconversion (T0) was defined as the first available plasma sample with VCA-IgM positive or VCA-IgG positive antibodies.
For each of the 324 follow-up MS patients, one healthy control individual was selected from the control cohort matched according to gender, age, time, and occurrence of IM. All MS patients and healthy controls were recruited in Austria and Germany. Furthermore, from all 324 control subjects, a follow-up was available for >5 years after the matching time point, and it was confirmed by follow-up records that none of them was diagnosed with MS or other autoimmune diseases or neuro-inflammatory disorders within this follow-up period. The recruitment of the study participants was recently described in detail36. The study was approved by the Institutional Review Board of the Medical University of Vienna (IRB number: 1339/2022). Details of the study cohort are shown in Table 1. Further details of the plasma samples included are shown in Table S1 and Table S2.
For the validation of the EBNA-1381-452-specific IgG ELISA, additional plasma samples from 15 EBV-VCA-IgG and EBNA-IgG seropositive as well as 40 EBV-VCA-specific IgM, EBV-VCA-specific IgG, and EBV-EBNA-specific IgG seronegative healthy blood donors were included.
EBV serology
EBV-VCA-IgM, EBV-EBNA-IgG and EBV-VCA-IgG antibodies were detected and quantified by ELISA (Euroimmune).
EBNA-1381-452 peptide IgG ELISA
EBNA-1381-452-specific IgG antibodies were detected and quantified by a newly established enzyme-linked immunosorbent assay (ELISA). Briefly, 96-well plates (Thermo Fisher Scientific) were coated in carbonate buffer (1.59 g Na₂CO₃ + 2.93 g NaHCO₃ in 1 L ddH₂O) with 1 μg/mL of an EBNA-1381-452-derived peptide library (Table S3). The plate was washed with PBST (1xPBS + 0.05% Tween-20) and blocked with Blocking Buffer (1xPBS + 1% BSA). Patient plasma samples were diluted 1:100 in Sample Diluent (DRG International) and incubated for 2 h at 37 °C, followed by an additional washing step with PBST. Peptide-specific IgG antibodies were detected using HRP-conjugated goat anti-human IgG (1:12500 in Blocking Buffer) and TMB substrate (Thermo Fisher Scientific). The reaction was stopped after 8 min, using 1 N sulfuric acid. The absorbance was measured at λ = 450 nm and λ = 620 nm using a Synergy HTX multimode reader (BioTek). The difference in absorbance between 450 nm and 620 nm was calculated, followed by the subtraction of the blank. EBNA-1381-452-specific IgG antibody titers were assessed in two independent technical replicates.
NfL and GFAP testing
Plasma neurofilament light chain (NfL), a biomarker reflecting axonal damage, and plasma glial fibrillary acidic protein (GFAP), a biomarker reflecting astrocytic activation associated with disease progression in MS, were quantified using single-molecule array (SIMOA) Neurology 2 Plex B assay kits in the SIMOA SR-X Analyzer (Quanterix) according to the manufacturer’s instructions as described in detail before37.
Statistical analysis
The 95.0% CI cut-off for the detection of EBNA-1381-452-specific IgG antibodies was calculated as described in detail before38. Receiver operating characteristic (ROC) curves were used to define high-level EBNA-1381-452-specific IgG titers. After the ROC analysis, all cut-off values ≥ 70% sensitivity and ≥70% specificity were tested individually in Fisher’s exact tests. The cut-off with the highest Odds Ratio (OD ≥ 1.7) was selected to differentiate between high-level and low-level EBNA-1381-452-specific IgG antibody titers. The EBNA-1381-452-specific IgG antibody seroprevalence and the number of MS lesions were compared using the Chi-square test or Fisher’s exact test. EBNA-1381-452-specific IgG antibody titers as well as the plasma NfL and GFAP levels over time were analysed using robust non-linear regressions and were compared using Mann-Whitney-Test or ANOVA and Tukey’s or Dunn’s post-hoc test. The association between the EBNA-1381-452-specific IgG levels and the MS diagnosis was assessed using the Gehan-Breslow-Wilcoxon Test. All statistical analyses were performed using GraphPad Prism 10.
Ethics declaration
The study was approved by the Institutional Review Board of the Medical University of Vienna (IRB number: 1339/2022). As datasets, including data obtained in routine practice, were exported pseudonymously, the need for written informed consent from study participants was waived by the Institutional Review Board.
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Data availability
The anonymized data supporting the findings of this study are available from the corresponding authors upon request. Due to legal and ethical considerations, access is granted to qualified researchers upon request to the corresponding authors and pending approval by the Data-Clearing Committee of the Medical University of Vienna. Source data for the figures and Supplementary Figs. are provided as a Source Data file. Source data are provided with this paper.
Code availability
This study generated no codes.
References
Reich, D. S., Lucchinetti, C. F. & Calabresi, P. A. Multiple sclerosis. N. Engl. J. Med 378, 169–180 (2018).
Walton, C. et al. Rising prevalence of multiple sclerosis worldwide: insights from the Atlas of MS, third edition. Mult. Scler. 26, 1816–1821 (2020).
Bjornevik, K. et al. Longitudinal analysis reveals high prevalence of Epstein-Barr virus associated with multiple sclerosis. Sci. (N. Y., NY) 375, 296–301 (2022).
Ascherio, A. et al. Epstein-Barr virus antibodies and risk of multiple sclerosis: a prospective study. Jama 286, 3083–3088 (2001).
Cortese, M. et al. Serologic response to the Epstein-Barr virus peptidome and the risk for multiple sclerosis. JAMA Neurol. 81, 515–524 (2024).
Soldan, S. S. & Lieberman, P. M. Epstein-Barr virus and multiple sclerosis. Nat. Rev. Microbiol. 21, 51–64 (2023).
Vietzen H., et al. Accumulation of Epstein-Barr virus-induced cross-reactive immune responses is associated with multiple sclerosis. J. Clin. Invest. 134, e184481 (2024).
Tengvall, K. et al. Molecular mimicry between Anoctamin 2 and Epstein-Barr virus nuclear antigen 1 associates with multiple sclerosis risk. Proc. Natl. Acad. Sci. USA 116, 16955–16960 (2019).
Lanz, T. V. et al. Clonally expanded B cells in multiple sclerosis bind EBV EBNA1 and GlialCAM. Nature 603, 321–327 (2022).
Thomas, O. G. et al. Cross-reactive EBNA1 immunity targets alpha-crystallin B and is associated with multiple sclerosis. Sci. Adv. 9, eadg3032 (2023).
Lünemann, J. D. et al. EBNA1-specific T cells from patients with multiple sclerosis cross react with myelin antigens and co-produce IFN-gamma and IL-2. J. Exp. Med. 205, 1763–1773 (2008).
Gill, A. J., Schorr, E. M., Gadani, S. P. & Calabresi, P. A. Emerging imaging and liquid biomarkers in multiple sclerosis. Eur. J. Immunol. 53, 2250228 (2023).
Benkert, P. et al. Serum neurofilament light chain for individual prognostication of disease activity in people with multiple sclerosis: a retrospective modelling and validation study. Lancet Neurol. 21, 246–257 (2022).
Meier, S. et al. Serum glial fibrillary acidic protein compared with neurofilament light chain as a biomarker for disease progression in multiple sclerosis. JAMA Neurol. 80, 287–297 (2023).
Levin, L. I. et al. Temporal relationship between elevation of Epstein-Barr virus antibody titers and initial onset of neurological symptoms in multiple sclerosis. JAMA 293, 2496–2500 (2005).
Sundström, P. et al. An altered immune response to Epstein-Barr virus in multiple sclerosis. Neurology 62, 2277–2282 (2004).
Jons, D. et al. Seroreactivity against lytic, latent and possible cross-reactive EBV antigens appears on average 10 years before MS induced preclinical neuroaxonal damage. J. Neurol. Neurosurg. Psychiatry 95, 325–332 (2024).
Ingram, G., Bugert, J. J., Loveless, S. & Robertson, N. P. Anti-EBNA-1 IgG is not a reliable marker of multiple sclerosis clinical disease activity. Eur. J. Neurol. 17, 1386–1389 (2010).
Rommer P. S., et al. Relapsing and progressive MS: the sex-specific perspective. Ther. Adv. Neurol. Disord. 13, 1756286420956495 (2020).
Orton, S. M. et al. Sex ratio of multiple sclerosis in Canada: a longitudinal study. Lancet Neurol. 5, 932–936 (2006).
Nesbitt, C., Van Der Walt, A., Butzkueven, H., Cheung, A. S. & Jokubaitis, V. G. Exploring the role of sex hormones and gender diversity in multiple sclerosis. Nat. Rev. Neurol. 21, 48–62 (2025).
Zamecnik, C. R. et al. An autoantibody signature predictive for multiple sclerosis. Nat. Med 30, 1300–1308 (2024).
Abrahamyan, S. et al. Complete Epstein-Barr virus seropositivity in a large cohort of patients with early multiple sclerosis. J. Neurol. Neurosurg. Psychiatry 91, 681–686 (2020).
Domínguez-Mozo, M. I. et al. Epstein-Barr virus and multiple sclerosis in a Spanish cohort: a two-years longitudinal study. Front Immunol. 13, 991662 (2022).
Nourbakhsh, B. et al. Multiple Sclerosis is rare in Epstein-Barr virus-seronegative children with central nervous system inflammatory demyelination. Ann. Neurol. 89, 1234–1239 (2021).
Pohl, D. et al. High seroprevalence of Epstein-Barr virus in children with multiple sclerosis. Neurology 67, 2063–2065 (2006).
Aloisi, F., Giovannoni, G. & Salvetti, M. Epstein-Barr virus as a cause of multiple sclerosis: opportunities for prevention and therapy. Lancet Neurol. 22, 338–349 (2023).
Farrell, R. A. et al. Humoral immune response to EBV in multiple sclerosis is associated with disease activity on MRI. Neurology 73, 32–38 (2009).
Lebrun-Frenay, C. et al. Radiologically isolated syndrome. Lancet Neurol. 22, 1075–1086 (2023).
Lebrun-Frénay, C. et al. Teriflunomide and time to clinical multiple sclerosis in patients with radiologically isolated syndrome: the TERIS randomized clinical trial. JAMA Neurol. 80, 1080–1088 (2023).
Thompson, A. J. et al. Diagnosis of multiple sclerosis: 2017 revisions of the McDonald criteria. Lancet Neurol. 17, 162–173 (2018).
Bsteh, G. et al. Quantifying the risk of disease reactivation after interferon and glatiramer acetate discontinuation in multiple sclerosis: The VIAADISC score. Eur. J. Neurol. 28, 1609–1616 (2021).
Bsteh, G. et al. Association of disease-modifying treatment with outcome in patients with relapsing multiple sclerosis and isolated MRI activity. Neurology 103, e209752 (2024).
Wendel, E.-M. et al. Serum neurofilament light-chain levels in children with monophasic myelin oligodendrocyte glycoprotein-associated disease, multiple sclerosis, and other acquired demyelinating syndrome. Mult. Scler. J. 28, 1553–1561 (2022).
Wendel, E. M. et al. High association of MOG-IgG antibodies in children with bilateral optic neuritis. Eur. J. Paediatr. Neurol. 27, 86–93 (2020).
Vietzen, H. et al. Ineffective control of Epstein-Barr-virus-induced autoimmunity increases the risk for multiple sclerosis. Cell 186, 5705–5718.e5713 (2023).
Altmann, P. et al. Seven day pre-analytical stability of serum and plasma neurofilament light chain. Sci. Rep. 11, 11034 (2021).
Frey, A., Di Canzio, J. & Zurakowski, D. A statistically defined endpoint titer determination method for immunoassays. J. Immunol. Methods 221, 35–41 (1998).
Acknowledgements
We thank Kathrin Schanda and Philippe Furlano for the excellent technical assistance. The study was funded by the Center for Virology and the Department of Neurology, Medical University of Vienna, Vienna, Austria. H.V. received a research grant from the Austrian MS society.
Author information
Authors and Affiliations
Contributions
Conceptualization: H.V., T.B., P.R., E.P., Methodology: H.V., P.R., E.P., Validation: H.V., P.R., E.P., Formal Analysis: H.V., L.K., S.B., M.P., Investigation: H.V., P.R., E.P., Data collection and analysis: H.V., Resources: M.G., C.P., C.J., M.R., H.S., F.K., E.W., K.R., M.B., B.K., G.B., T.B., Writing–Original Draft: H.V., E.P., Writing–Review & Editing: H.V., T.B., P.R., E.P., Visualization: H.V.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Communications thanks the anonymous reviewers for their contribution to the peer review of this work. A peer review file is available.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Source data
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Vietzen, H., Kühner, L.M., Berger, S.M. et al. Early identification of individuals at risk for multiple sclerosis by quantification of EBNA-1381-452-specific antibody titers. Nat Commun 16, 6416 (2025). https://doi.org/10.1038/s41467-025-61751-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41467-025-61751-9
This article is cited by
-
Towards a prognostic biomarker for multiple sclerosis
Nature Reviews Microbiology (2025)