Abstract
Long-term delivery of broadly neutralizing antibodies (bnAbs) using adeno-associated virus (AAV) vector is a promising approach for both the prevention and treatment of HIV infection. However, host anti-drug antibody (ADA) responses severely limit the continuous delivery of these anti-HIV bnAbs and have been the most important obstacle for development of this approach for widespread human use. Transient treatment with the immunomodulatory agent rapamycin (sirolimus) allows for continuous long-term delivery of the anti-HIV bnAb 3BNC117 in immunocompetent mice in the absence of detectable ADAs. Use of the agent in monkeys results in 12 of 15 successful deliveries of the bnAbs 3BNC117, 10-1074, and PGT145 following drug cessation across all animals. The results of this 5-monkey trial lend strong support to continuing studies in SHIV-infected monkeys and use of this approach in humans for potential worldwide use.
Similar content being viewed by others
Introduction
Antibody-based strategies for the prevention or treatment of HIV have been made possible by the isolation and availability of dozens of monoclonal antibodies (mAbs) with potent neutralizing activity against a broad range of HIV isolates1,2. Trials in monkeys and in humans have demonstrated potent antiviral effects following passive transfer of such potent broadly neutralizing antibodies (bnAbs), in both prophylactic and therapeutic settings1. While passive transfer may be a first approach to combat HIV infection, it might not be practical on a large scale and long-term. The immense costs associated with mAb production, the need for continuous and repeated infusions, and adherence are likely problems. A one-shot administration event using a viral vector encoding the desired antiviral bnAbs is a potential alternative for achieving lifelong anti-HIV immunity. The adeno-associated virus (AAV) vector system is one such promising alternative. In more than 200 clinical trials, recombinant AAVs have been proven safe and efficacious in treating hereditary disorders3,4. Several groups including our own have shown that AAV-delivered bnAbs and antibody-like molecules can protect against immunodeficiency virus infection and can durably control virus replication5,6,7,8,9. In fact, our group has now achieved a functional cure in seven AIDS virus-infected monkeys including the “Miami monkey”6,10 which has now remained aviremic for over 9 years following AAV vector administration.
Nonetheless, the effectiveness of the AAV-antibody approach is hindered by the emergence of unwanted host immune responses following AAV administration11,12,13,14. These immune responses, including anti-drug antibodies (ADAs), limit the bioavailability of AAV-delivered bnAbs and consequently reduce or eliminate their antiviral effect15,16. The degree of immunogenicity is dependent on a variety of factors. While autologous administered “self” proteins may not be expected to elicit immune responses, they do in patients who have mutations or are missing the protein entirely. Anti-HIV bnAbs may be particularly viewed as foreign/non-self since the variable domain regions are vastly diverged from the host germline, and when the constant regions are from a different species as compared to those of the recipient15,16,17,18. Furthermore, adaptive immune responses to the AAV-delivered bnAb are primed and potentiated by innate immune responses to the AAV vector itself14,19. We have used well-known, well-characterized bnAbs that have been “rhesusized” in their constant regions (C-rh) for our monkey studies6, and in those studies only about 10% of intramuscular (i.m.) AAV vector administrations have resulted in continuous long-term delivery. The vast residual of ~90% have had ADA responses to the AAV-delivered bnAbs which have negated their continuing presence. Other monkey trials20,21 and the two human trials22,23 investigating AAV delivery of anti-HIV bnAbs have also observed ADAs and little or no delivery of the desired bnAbs.
A variety of strategies have been explored by us and other groups to circumvent, lower, or avoid the immunogenicity of the AAV vector delivery system. These strategies include but are not limited to: reduction of CpG dinucleotide content in the recombinant AAV genome (evasion of TLR9 signaling); inclusion of micro RNA binding sites into the recombinant AAV genome (reduction of ectopic expression in antigen presenting cells); AAV capsid engineering and modification (evasion of host antibodies and reduction of immunogenicity); inclusion of Treg epitopes into the coding sequence of the transgene (induction of T cell tolerance); liver-directed AAV gene transfer (liver tolerance induction); oral antigen pre-exposure (mucosal tolerance induction); erythrocyte targeting of antigen (red blood cell tolerance induction)14,24,25,26. While some partial effects were noted with some of these approaches in our previous monkey studies, impressive antigenic-specific tolerization has not been achieved. Immunomodulatory drugs have also been part of the strategies to potentially allow for successful AAV gene therapy27,28. The immunosuppressant rapamycin (sirolimus) is an FDA-approved drug that is mostly used as a prophylaxis to prevent rejection of kidney transplants; in fact, the drug has also been shown to be safe in HIV-infected patients with Kaposi sarcoma29 and in HIV-infected patients receiving kidney transplants30. Here we report that transient treatment with the immunomodulatory agent rapamycin allows for continuous, long-term AAV-mediated delivery of anti-HIV bnAbs in both mice and monkeys.
Results
Transient rapamycin treatment prevents ADAs to AAV-delivered bnAb in mice
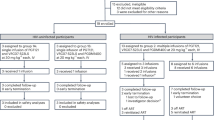
In our experiments, we sought to determine whether extended transient treatment with rapamycin can prevent ADAs toward an immunogenic bnAb delivered by AAV vector. To test that hypothesis, we conducted a 10-mouse experiment. Five immunocompetent B6/129J mice started to receive rapamycin at week −1 relative to the day of AAV administration and treatment with the drug was continued through week 11. Each mouse in the treatment group received 2 mg/kg by the intraperitoneal route three times a week (Monday-Wednesday-Friday). The other five mice served as controls and those animals were only given PBS as mock treatment. At week 0, all 10 mice in both groups were injected with AAV9 encoding the immunogenic bnAb C-rh 3BNC117. The AAV9 vector was administered intramuscularly at a dose of 0.2 × 1013 GC/kg into one gastrocnemius muscle of each mouse.
We performed periodic bleedings and collected plasma to measure levels of AAV-delivered C-rh 3BNC117, ADAs to C-rh 3BNC117, and reactivity to the AAV9 capsid by ELISA. Following AAV administration, none of the five mice in the rapamycin treatment group developed ADAs to C-rh 3BNC117, not during the rapamycin treatment phase (weeks −1 to 11) and not following the cessation of rapamycin in the remaining 17 weeks of continuing measurements (Fig. 1a). ADAs specific to C-rh 3BNC117 were readily detectable as early as week 3 in four of the five control mice and persisted in three of five control mice through week 28. Levels of C-rh 3BNC117 in plasma steadily increased to approximately 50–250 μg/ml following AAV administration in all of the five mice of the rapamycin group during the treatment phase, and those levels decreased but stabilized over the course of time following the cessation of rapamycin (Fig. 1b). In contrast, the five control mice exhibited a peak in C-rh 3BNC117 levels of up to 25 μg/ml at week 3, which then abruptly declined to undetectable levels in three of five mice during the mock treatment phase. In the other two control mice, levels of the bnAb increased and stabilized to approximately 10 and 30 μg/ml by week 28. At that study end point, the five rapamycin animals exhibited higher C-rh 3BNC117 levels that were statistically significant (P = 0.0006) (Fig. 1c).
Ten B6/129J mice were given AAV9-C-rh 3BNC117 at 0.2 × 1013 GC/kg by the intramuscular (i.m.) route in the absence (MO1 animals #9-13 in blue color) and presence of rapamycin (MO1 animals #14-18 in red color). The treatment group received rapamycin at 2 mg/kg three times a week by the intraperitoneal (i.p.) route for the duration of 12 weeks (week −1 to 11). a ADAs to C-rh 3BNC117 in plasma; upper limit of detection = 4. b C-rh 3BNC117 levels in plasma. c Levels of C-rh 3BNC117 at week 28 post AAV; data are presented as mean values ± SD; mean comparison of the control group (blue circles, n = 5 biological samples) with the rapamycin treatment group (red squares, n = 5 biological samples) using the unpaired t-test (two-tailed) with Welch’s correction, with P ≤ 0.001 (***) indicating statistical significance. d Reactivity to AAV9 capsid in plasma. e Reactivity to AAV9 capsid at week 26 post AAV; data are presented as mean values ± SD; mean comparison of the control group (blue circles, n = 5 biological samples) with the rapamycin treatment group (red squares, n = 5 biological samples) using the unpaired t-test (two-tailed) with Welch’s correction with P ≤ 0.05 (*) indicating statistical significance. Abbreviations: LOD limit of detection. Source data are provided as a Source Data file.
We next assessed the reactivity to the AAV9 capsid in plasma. Following AAV administration, humoral responses were readily detectable in all ten animals, which were uniformly strong in the five mock-treated mice and low or modest in the five rapamycin-treated mice (Fig. 1d). While rapamycin avoided ADAs to the AAV-delivered bnAb C-rh 3BNC117 during and after the treatment phase, the drug did not prevent humoral responses to the AAV9 capsid during the treatment phase. However, it was noted that the reactivity to AAV9 capsid was significantly lower following the treatment phase in the rapamycin group as compared to the mock group at week 26 (Fig. 1e).
We then analyzed T cell subsets in peripheral blood mononuclear cells (PBMC) and in the spleen (Supplementary Figs. 1 and 2). CD4+ T cells among PBMC were significantly lower in the rapamycin group vs. the control group during the treatment phase at week 10 (Supplementary Fig. 2a) but had recovered to levels similar to controls after rapamycin withdrawal at week 24 (Supplementary Fig. 2b), suggesting transient changes of CD4+ T cell counts during rapamycin treatment. To examine if rapamycin treatment alters regulatory T cell (Treg) and T follicular helper cell (Tfh) differentiation, we repeated the experiment in additional animals and sacrificed the mice 3 weeks after rapamycin treatment. As expected, we observed lower CD4+ T cell counts in splenocytes (Supplementary Fig. 2c) in the rapamycin treated group (n = 5) as compared to the controls (n = 3). Interestingly, Treg counts were significantly elevated among CD4+ T cells of the spleen in the rapamycin group vs. the control group during the treatment phase. We also observed a modest but not significant decrease of Tfh counts among CD4+ T cells in the rapamycin group (Supplementary Fig. 2d).
Transient rapamycin treatment allows for long-term AAV-antibody delivery in monkeys
Given the impressive results that were achieved in immunocompetent mice, we initiated a 5-monkey trial in which we set out to test the immunomodulatory effect of transient treatment with rapamycin on the AAV-antibody deliverability in nonhuman primates. Five AAV9-negative rhesus monkeys that were not infected with AIDS virus began rapamycin treatment at week −2. The monkeys then received three intramuscularly administered AAV9 vectors (encoding the bnAbs C-rh 3BNC117, C-rh 10-1074, and C-rh PGT145) at 0.2 × 1013 GC/kg each at week 0, where each of the three vectors was injected separately into a distinct muscular site. Meanwhile, the monkeys continued to receive rapamycin up until week 12 post AAV administration. Intramuscular rapamycin injections were performed daily at a dose of 0.2 mg/kg between weeks −2 and 0, and injections continued three times a week (Monday-Wednesday-Friday) with adjusted dosages of 0.15–0.4 mg/kg between weeks 0 and 12. Following AAV9 administration at week 0, serum levels of AAV-delivered C-rh 3BNC117, C-rh 10-1074, and C-rh PGT145 rose and remained in the therapeutic range of approximately 15–55 μg/ml by week 12 post AAV (Fig. 2a–c). Most importantly, following the cessation of rapamycin at that time, bnAb levels were maintained in a therapeutic range of approximately 5–55 μg/ml in the 12 of 15 successful bnAb delivery attempts by week 56 post AAV.
Five rhesus macaques were injected intramuscularly (i.m.) with three AAV9 vectors encoding the bnAbs C-rh 3BNC117, C-rh 10-1074, and C-rh PGT145 at a dose of 0.2 × 1013 GC/kg of each vector. Rapamycin was given daily and then three times a week by the intramuscular (i.m.) route for the duration of 14 weeks (week −2 to 12 relative to AAV administration). The dosages ranged between 0.15 and 0.4 mg/kg to accommodate individual adjustments. Serum levels of the AAV-delivered bnAbs a C-rh 3BNC117, b C-rh 10-1074, and c C-rh PGT145. d Rapamycin levels in whole blood. Source data are provided as a Source Data file.
The minimal therapeutic range of rapamycin is considered to be trough levels of 5–15 ng/ml in whole blood31,32,33,34. Our initial dosage regimen resulted in rapamycin levels of up to 60 ng/ml at week 0 (Fig. 2d). To reduce or avoid potential adverse events while maintaining a therapeutic range, we adjusted the dosage in individual monkeys and performed rapamycin injections three times a week beyond week 0. Most animals maintained therapeutic rapamycin levels around 15 ng/ml of whole blood between weeks 5 and 12. Nonetheless, early adjustments to the drug regimen resulted into unfavorable rapamycin fluctuations leading to subtherapeutic drug levels at week 2 post AAV in at least two of the monkeys. The monkeys that were mostly affected by the drop of rapamycin levels at that time were r20073 (4 ng/ml) and r21082 (3 ng/ml) (Fig. 2d).
As in our mouse experiment, we analyzed the frequency of T cell subsets in the PBMCs of our five rapamycin-treated monkeys (Supplementary Figs. 3 and 4). We observed no changes in CD8+ T cell counts when comparing paired samples collected before (2 weeks pre AAV) and during rapamycin treatment (8 weeks post AAV). However, CD8+ T cells expanded significantly between 8 and 20 weeks post AAV, by which time rapamycin had already been discontinued for eight weeks (Supplementary Fig. 4a). We then plotted the serum levels of the three bnAbs against the CD8+ T cell counts from weeks 8 and 20 post AAV and found a significant negative correlation (Supplementary Fig. 4b). Blood CD4+ T cell counts remained unchanged when comparing paired samples from before (2 weeks pre AAV) and during rapamycin treatment (8 weeks post AAV), but those counts dropped significantly after rapamycin cessation (20 weeks post AAV) (Supplementary Fig. 4c). Within the CD4+ T cell population, the frequency of Treg cells initially dropped significantly when comparing paired samples from before (2 weeks pre AAV) and during rapamycin treatment (8 weeks post AAV). However, Treg counts more than doubled in three of the five monkeys after rapamycin cessation (20 weeks post AAV). No changes were observed in the other two monkeys (r20073 and r21082), which had previously exhibited subtherapeutic rapamycin levels at week 2 post AAV (Supplementary Fig. 4d and Fig. 2d).
Following AAV9 administration at week 0, no ADAs specific to C-rh 3BNC117, C-rh 10-1074, and C-rh PGT145 were detected in all five monkeys up until week 16 (Fig. 3a–c). Rapamycin treatment was discontinued at week 12 post AAV, which resulted in the expected drop of drug levels in blood to below the therapeutic range by week 13. Following the rapamycin cessation, considerable ADA responses emerged in two of five animals for C-rh 3BNC117 (Fig. 3a), in one of five animals for C-rh 10-1074 (Fig. 3b), and in two of five animals for C-rh PGT145 (Fig. 3c). Four of the five ADA responses were found in the two animals that had subtherapeutic rapamycin levels at week 2 post AAV: r20073 and r21082. And those two animals accounted for two of three unsuccessful continuous deliveries of bnAbs (Fig. 2). Antibody responses to the AAV9 capsid were readily detectable at week 2 post AAV administration (Fig. 3d). While bnAb-specific ADAs remained largely suppressed, AAV9-specific ADAs increased and remained at high levels in all monkeys following the rapamycin cessation at week 12.
The five rhesus macaques from Fig. 2 that received three AAV9 vectors were monitored for ADAs in serum. ADAs to a C-rh 3BNC117, b C-rh 10-1074, and c C-rh PGT145. d Reactivity to the AAV9 capsid in serum. Abbreviations: LOD limit of detection. Source data are provided as a Source Data file.
At the time of the initiation of this 5-monkey trial (study # IS-218), we had no access to additional AAV9-negative monkeys that could be used as control animals. However, prior to the start of IS-218, we had conducted a separate monkey trial (study # IS-160) that utilized four control animals that were given only AAV9 encoding C-rh 3BNC117 without any immunomodulatory treatment. That study employed the same AAV9 stock at the same dose as the one we used in IS-218. We therefore compared the levels of AAV-delivered C-rh 3BNC117 among the two studies at different time points post AAV administration (Fig. 4). In the historical control group of IS-160, the four monkeys reached a mean C-rh 3BNC117 concentration in serum of approximately 25 μg/ml at week 2 post AAV. However, those levels plummeted to zero in all four animals by week 4. While on rapamycin treatment, the five animals in this monkey trial exhibited levels of approximately 30 μg/ml of the bnAb at week 4 post AAV. At week 17, the latest available time point of the historical IS-160 study, the C-rh 3BNC117 levels remained at zero in all four animals. The five animals of this IS-218 monkey trial stabilized to a mean of approximately 15 μg/ml at week 16, which was the closest matched time point to the historical controls. The week 16 levels of IS-218 were 4 weeks following rapamycin cessation and were significantly different than the weeks 4 and 17 after the administration of AAV vector in IS-160.
A previous monkey trial from our group that employed no drug treatment in four monkeys (study # IS-160) was compared to the current monkey trial that employed transient treatment with rapamycin in five monkeys (study # IS-218). Both trials utilized the same AAV9-C-rh 3BNC117 stock at the same dose of 0.2 × 1013 GC/kg in naive rhesus monkeys. The levels of C-rh 3BNC117 in serum were compared among the two trials at weeks 2, 4, and 17/16 post AAV9 administration. Week 17 in IS-160 was the latest time point available and compared to the closest time point available in IS-218, which was week 16 post AAV9 (week 4 post rapamycin cessation). Data are presented as mean values ± SD; mean comparison of the historical control group (black circles, n = 4 biological samples) with the rapamycin treatment group (black squares, n = 5 biological samples) using the unpaired t-test (two-tailed) with Welch’s correction, with P ≤ 0.05 (*), P ≤ 0.01 (**), and P ≤ 0.001 (***) indicating statistical significance. Source data are provided as a Source Data file.
To further illustrate the consistency of the problem with ADAs, (Fig. 5) shows our earlier results using AAV to deliver the exact same C-rh bnAbs (3BNC117 and 10-1074) to six monkeys and the exact same C-rh PGT145 bnAb to six different monkeys in our prior animal study “IS-84”6. Intramuscular deliveries identical to the ones described here in our studies with rapamycin were used in the IS-84 trial. Six of six monkeys exhibited strong ADAs to C-rh 3BNC117 and no continuous delivery of that bnAb (Fig. 5a). Five of six monkeys exhibited considerable ADAs to C-rh 10-1074 and only one of the six exhibited continuous delivery of that bnAb (Fig. 5b). Five of six monkeys exhibited strong ADAs to C-rh PGT145 and none of the six exhibited continuous delivery of that bnAb (Fig. 5c).
a C-rh 3BNC117, b C-rh 10-1074, and c C-rh PGT145. A historical monkey study (IS-84) conducted by our lab is shown to highlight the immunogenicity problem that is associated with AAV-mediated delivery of bnAbs. Following AAV vector administration to monkeys, levels of rhesus constant regions (C-rh) 3BNC117, C-rh 10-1074, and C-rh PGT145 were readily detectable, but those levels dropped to near or below the limit of detection coincidentally with the rise of ADAs to the three bnAbs by weeks 4–12 post AAV. Source data are provided as a Source Data file.
Discussion
Transient treatment with rapamycin resulted in the successful delivery of anti-HIV bnAbs following AAV gene transfer to mice and to monkeys. Five of five long-term deliveries of the C-rh 3BNC117 bnAb were achieved in mice and 12 of 15 long-term deliveries of C-rh 3BNC117, C-rh 10-1074, and C-rh PGT145 were achieved in monkeys. The results of this 5-monkey trial stand in stark contrast to the results of our previous monkey trials in which we observed little or no AAV-mediated antibody deliverability.
Multiple studies have demonstrated the potential for the AAV-antibody gene transfer technology to effectively block viral infection and durably suppress an ongoing viral infection5,6,7,8,9. Nonetheless, the technology has been hampered by the emergence of unwanted immune responses that are frequently observed in most treatment recipients, both monkeys and humans6,15,16,20,22,23. In fact, our group has conducted over 20 monkey trials within the last 13 years and ADAs negated antibody delivery in most cases, as we highlighted here in two of our historical trials. Our studies in monkeys have utilized human anti-HIV bAbs that have been “rhesusized” in their constant regions6,15. However, the two human trials using AAV to deliver human anti-HIV bnAbs have also shown a high frequency of ADAs and a lack of continuous long-term delivery22,23. It is perhaps not surprising that anti-HIV bnAbs are viewed as foreign by the host immune system. Their variable domains typically take about 2–3 years to develop and are very highly diverged from germline. Martinez-Navio et al. have shown that both the propensity and magnitude of ADA responses are directly correlated with the variable domain’s distance from germline15. Klenchin et al. observed long-term continuous delivery of the ITS61.01 and ITS103.01 mAbs with reasonably high frequency8. This is likely due at least in part to closer similarity to the germline. For example, the heavy chain variable domain of ITS61.01 shares 95.6% identity with the rhesus monkey germline, compared to 72.9% for 3BNC117, 78.8% for PGT145, and 82.8% for 10-1074.
In our mouse experiment described here, we treated mice with rapamycin for 12 weeks (week −1 to 11 relative to AAV administration). In our monkey experiment, we treated monkeys with rapamycin for 14 weeks (week −2 to 12 relative to AAV administration). Both experiments resulted in the avoidance of ADAs to the AAV-delivered bnAbs in most treatment recipients during and, most importantly, following cessation of rapamycin administrations. Those extended drug treatments allowed for successful bnAb delivery in the vast majority of cases. A previous mouse experiment showed that a transient 3-week treatment with rapamycin did not prevent ADAs toward the immunogenic antigen, keyhole limpet hemocyanin, following protein infusion35. However, another mouse study showed that a transient 4-week treatment with rapamycin mitigated ADAs to coagulation factor VIII during and after the immunomodulatory treatment phase36. While our experiments, which employed anti-HIV bnAbs, may not be directly comparable to previous studies conducted by other groups who employed different immunogenic antigens, our results here may serve to exemplify that a longer rapamycin treatment may help to induce better tolerance to a highly immunogenic antigen.
During and following rapamycin treatment, we observed that ADAs to the transgene products were largely suppressed in both our mouse and monkey experiments presented here. Rapamycin has been shown to promote expansion and differentiation of Tregs37,38,39,40. Nayak et al. reported that antigen presentation to CD4+ T cells in the presence of rapamycin resulted in the activation-induced cell death of T effector cells (Teff) as well as the induction of Treg cells that was associated with the avoidance of an antibody response to the Factor IX protein in a strain of hemophilia B mice41,42. We also observed decreased CD4+ T cell counts, decreased Tfh counts, and elevated Treg counts in mice on rapamycin treatment, which may have contributed to the induction of tolerance toward the AAV-delivered transgene product C-rh 3BNC117. However, antibody responses to the AAV9 capsid were only decreased modestly. This may be due to differences in antigen persistence and presentation between the transgene product and the AAV capsid; the capsid protein is likely presented transiently by professional antigen presenting cells (APC) that promote immune responses including ADAs, while transgene products are presented persistently by AAV gene-modified muscle cells that do not express high level of co-stimulatory molecules43,44. Higher levels of rapamycin or combination with other immunomodulatory drugs may be needed to induce tolerance to both the AAV capsid and the transgene product45. Previous reports that utilized nanoparticle-encapsulated rapamycin (ImmTOR) were successful at inhibiting immune responses to both the immunogenic antigen and the AAV capsid protein35,46. While the underlying mechanism responsible for the immunomodulatory effects of free rapamycin drug vs. rapamycin delivered in a nanoparticle format is not entirely clear47, it is possible that ImmTOR allows for a more targeted delivery and a higher concentration of rapamycin in AAV gene-modified cells and APCs.
While we cannot directly compare the separate mouse and monkey experiments regarding T cell analyses, we can emphasize the findings of the monkey trial data. We noted a negative correlation of bnAb levels in serum and CD8+ T cell counts between weeks 8 and 20 post AAV. While AAV-delivered bnAb levels dropped following an initial peak during the rapamycin treatment phase in the absence of detectable ADAs (weeks −2 to 12), that decrease was inconsistent among the three bnAbs. It is unclear whether a higher number of CD8+ T cells had an influence on bnAb levels through their cytotoxic activity or whether that decay resulted from the loss of transgene expression in non-target cells48. Furthermore, since increased CD8+ T cell counts persisted by week 20 while bnAb levels started levelling off, those T cells may have become exhausted or may have possibly gained a regulatory function49,50,51. We also observed reduced CD4+ T cell counts and increased Treg counts following the cessation of rapamycin, which both may have contributed to the induction of immune tolerance toward the AAV-delivered bnAbs.
Immunomodulatory drugs such as rapamycin are aimed at suppressing or lowering the body’s normal immune response against self and non-self antigens. Therefore, such drugs are mainly used in patients with autoimmune disorders (e.g., Crohn’s disease, lupus, and rheumatoid arthritis) and in organ transplant recipients to prevent organ transplant rejection52. However, use of immunosuppressive agents has also been extended to the gene therapy field. Initial clinical trials that employed AAV gene transfer were faced with elevated liver enzyme levels which were treated with transient administrations of corticosteroids (e.g., prednisone, prednisolone, and methylprednisolone). Other immunosuppressants that have been used in the AAV gene therapy field include mycophenolate mofetil, calcineurin inhibitors (cyclosporine, tacrolimus), and rituximab28. A variety of single-drug regimens and drug combinations have been tested in pre-clinical trials over the last decades with varying degrees of success20,46,53,54,55,56,57,58,59. In a recent clinical trial, the combined use of rapamycin and rituximab significantly reduced the magnitude of anti-capsid antibodies following AAV9 gene transfer60. It is perhaps desirable to investigate the optimal duration of rapamycin treatment and whether synergistic combination with other drugs can establish complete immune tolerance in the shortest time possible.
Rapamycin is used extensively in the context of kidney transplantation and for treatment of Kaposi sarcoma. The duration of use in these contexts is typically much longer than what we have used here. Rapamycin is typically administered for the duration of the recipient’s life after a kidney transplant to prevent rejection. However, the exact duration and dosage may vary based on individual patient needs and other factors. Use of rapamycin has been shown to be safe as well in HIV-infected patients in these contexts29,30. Nonetheless, further mouse and monkey trials are warranted to help inform and guide the use of AAV-bnAbs in humans for both treatment and prevention purposes. What may be an optimal duration of rapamycin dosing for this purpose? Is the recommended optimal range of rapamycin concentration in blood of 5–15 ng/ml also optimal for optimizing consistency of bnAb delivery and concentration of bnAb delivered? Might use of a second immunomodulatory agent increase the level of continuously delivered bnAb and thus decrease the cost of this therapeutic approach?
The tolerized AAV gene transfer by transient treatment with rapamycin represents a highly promising achievement toward consistent delivery of anti-HIV antibodies at therapeutic levels to humans. Such levels are typically considered therapeutic when serum concentrations of those antibodies are at least 100-fold higher than their IC50s using in vitro neutralization assays61. In our 5-monkey trial, the bnAb levels in serum were in that therapeutic range in the vast majority of animals6. Furthermore, the combined presence of at least two to three bnAbs in serum potentiates their antiviral effect while minimizing the outgrowth of viral escape mutants62. Long-term virologic suppression has been achieved in monkeys with successful delivery of only two antibodies6,8. The long-term presence of AAV-delivered bnAbs can also complement the host’s own immune response against AIDS virus infection which may act in conjunction to suppress viral replication63. The recombinant AAV vector system has become the preferred gene therapy platform due to its overall safety profile and versatile use, with seven governmental-approved gene therapies already on the market4. Rapamycin, which is an FDA-approved drug that has been mostly used in transplantation medicine, could become a useful tool for limiting unwanted host immune responses toward successful AAV-antibody delivery. Given the fact that multiple anti-HIV mAbs have been successfully used in short-term human clinical trials, use of rapamycin for tolerized AAV gene transfer could become a game changer by allowing continuous long-term delivery of bnAbs from a single day’s AAV administration.
Methods
Anti-HIV antibodies
In our mouse and monkey studies, 3BNC11764, 10-107465, and PGT14566 were selected based on their recognition of three different categories of envelope spike target regions, their neutralization potency against SHIV-AD8, and their general neutralization breadth6. Antibody sequences of 3BNC117 (RRID: AB_2491033) and 10-1074 (RRID: AB_2491062) were kindly provided by Michel C. Nussenzweig (The Rockefeller University), and the antibody sequence of PGT145 (RRID: AB_2491054) was kindly provided by Dennis R. Burton (The Scripps Research Institute). To “rhesusize” the constant domains (C-rh) of all mAbs used in our studies, the variable domains of both heavy and light chains were identified using the IMGT/V-QUEST software67,68, and human constant domains were replaced with the corresponding rhesus monkey IgG1 and rhesus monkey light chain sequences based on published sequences (GenBank: AAQ57550.1 for the heavy chain, AAD02577.1 for the kappa chain, and ADX62855.1 for the lambda chain)69,70. The bnAbs 3BNC117 and PGT145 bore a rhesus kappa constant domain, while 10-1074 bore a rhesus lambda constant domain. The IgG1 Fc was selected because of its enhanced effector functions. The “LS mutation” (M428L/N434S) was included in the Fc portion of each antibody to increase the half-life in vivo71,72. Further modification to the IgG Fc portion of PGT145 was introduced to allow for quantification of the AAV-delivered bnAb in vivo: the C-terminus of the heavy chain was extended by a “Strep-tag II” (SAWSHPQFEK) from (IBA Lifesciences). The Fc portions of 3BNC117 and 10-1074 were left untagged.
rAAV vector constructs and AAV production
Coding sequences of the three bnAbs were all designed in silico, codon-optimized and gene-synthesized (Genscript). Heavy and light chains of each bnAb were expressed from one bicistronic cassette that included an F2A “self-processing” peptide from foot-and-mouth disease virus, the furin cleavage sequence (RKRR) for the cellular protease furin, and the linker sequence (SGSG) for improved furin enzyme-mediated cleavage6,73. The synthesized fragments were then cloned into the EcoRI (NEB, cat. # R3101L) and/or NotI (NEB, cat. # R3189L) site of our ssAAV vector backbone containing AAV2 ITRs, CMV promoter, SV40 intron, SV40 polyA signal as previously described6,73. To minimize off-target expression in professional antigen-presenting cells, four tandem repeats of the miRNA binding site miRNA-142-3p and four tandem repeats of miRNA-126-3p were included in the 3′ untranslated region of the AAV vector plasmid74,75,76. Recombinant AAV9 vectors (bearing the AAV9 capsid) were then produced as described previously77,78,79. In short, HEK-293 cells were transfected with a select rAAV vector plasmid and two helper plasmids to allow for generation of infectious AAV particles. After harvesting transfected cells and cell culture supernatant, rAAV was purified by sequential CsCl centrifugation. Vector genome number was measured by digital droplet PCR, and the purity of the preparation was verified by silver-stained SDS-PAGE.
Production of recombinant mAbs
Recombinant mAbs were produced in suspension cells using the ExpiCHO expression system. In short, ExpiCHO-S cells (Thermo Fisher Scientific, cat. # A29127) were cultured in expression medium (Thermo Fisher Scientific, cat. # A29100-01) at 37 °C, 8% CO2, and ≥ 80% relative humidity in an orbital shaking incubator at 125 rpm (Eppendorf, New Brunswick S41i). On the day of transfection, cells were diluted to a density of 6 × 106/ml and transfected with previously cloned rAAV-bnAb vector plasmids following the manufacturer’s instructions. Cell culture supernatant was then harvested by centrifugation and subsequent sterile-filtration 8–10 days post transfection. Recombinant mAbs were then purified from the clarified supernatant using HiTrap recombinant protein A columns (Cytiva, cat. # 17-5079-01). The purified mAbs were subsequently used as standards or coating reagents in ELISA experiments.
Animals and ethics statement
The mice used in our studies were immunocompetent B6/129J mice (Jax 101043) that have been bred and maintained at UCLA breeding facility. Animal research involving mice was carried out according to protocols approved by the UCLA Animal Research Committee (ARC) in accordance with all federal, state, and local guidelines. Specifically, all the experiments were carried out in accordance with the recommendations and guidelines80 for housing and care of laboratory animals of the NIH and the Association for the Assessment and Accreditation of Laboratory Animal Care International under UCLA ARC protocol ARC-2020-035.
The five monkeys used in our studies here (study # IS-218) were Indian-origin rhesus macaques (Macaca mulatta) and were tested negative for the presence of antibodies to HIV and AAV981 capsid prior to the start of the experiment at which time the animals weighed between 2.6 kg and 8.3 kg (three females and two males). The four AAV-negative monkeys of our historical controls (study # IS-160) weighed between 5.3 kg and 7.6 kg (two females and two males) at the start of that experiment. The 12 AAV-negative of our other historical controls (study # IS-84) weighed between 3.12 kg and 5.18 kg (seven females and five males) at the start of that experiment. The monkeys were housed at the Wisconsin National Primate Research Center and were cared for in accordance with the standards of Association for Assessment and Accreditation of Laboratory Animal Care International and the University of Wisconsin Research Animal Resources Center and Compliance unit. Animal experiments were approved by the University of Wisconsin College of Letters and Sciences and the Vice Chancellor for Research and Graduate Education Centers Institutional Animal Care and Use Committee (protocol number G006357) and performed in compliance with the principles described in the Guide for the Care and Use of Laboratory Animals80. Fresh water was always available, commercial monkey chow was provided twice a day, and fresh produce was supplied daily. To minimize any distress, ketamine HCl alone or ketamine HCl in combination with dexmedetomidine was used to sedate animals before experimental procedures (e.g., blood collection, AAV inoculations), and animals were monitored twice a day by animal care and veterinary staff. Analgesics and anti-inflammatories were administered to alleviate pain associated with the experimental procedures. The animals were socially housed in pairs or groups of compatible animals whenever possible.
Immunomodulatory treatment and AAV administration
For our mouse experiment, free rapamycin drug (MedChemExpress, cat. # HY-10219) was dissolved in DMSO, and the resulting ready-to-use rapamycin solution was administered by the intraperitoneal (i.p.) route at a dose of 2 mg/kg three times a week (Monday-Wednesday-Friday). The mice in the rapamycin treatment group started to be treated at week −1 relative to AAV and continued to be treated through week 11. The mice of the control group received PBS as mock treatment by the i.p. route, three times a week during the same time frame. At week 0, all mice were given AAV9 encoding the bnAb C-rh 3BNC117 by intramuscular (i.m.) injection into one gastrocnemius muscle of each mouse at a dose of 0.2 × 1013 genome copies (GC)/kg.
For our monkey experiment, free rapamycin drug (MedChemExpress, cat. # HY-10219) was initially dissolved in dimethylacetamide (DMA) (Millipore Sigma, cat. # 270555-100 ML), followed by the serial admixing of Tween-80 (MedChemExpress, cat. # HY-Y1891) and PEG400 (Spectrum Chemical, cat. # P9070-1LT). The ratio of the vehicle components was as follows: 10% (v/v) dimethylacetamide, 10% (v/v) Tween-80, and 80% (v/v) PEG40032. The homogenous rapamycin solution was then clarified by filtration using a 1-micron glass-fiber (J.T. Baker, cat. # SF01-10), followed by sterile-filtration using a 0.2-micron PTFE filter (Cytiva, cat. # 10462300). The resulting 5 mg/ml ready-to-use rapamycin solution was then administered by the i.m. route at a dose of 0.2 mg/kg. The monkeys started to be treated with rapamycin at week −2 relative to AAV on a daily basis. To establish and maintain a minimal therapeutic target of 5–15 ng/ml, we measured the rapamycin trough levels in whole blood (UW core lab). At week 0, we changed the rapamycin regimen to three times a week (Monday-Wednesday-Friday). At week 2, we adjusted the rapamycin dose in individual monkeys (0.15–0.4 mg/kg) to fine-tune the therapeutic target concentration while minimizing potential adverse reactions. At week 0, each of the five rapamycin-treated monkeys were injected by the i.m. route with three AAV9 vectors encoding the bnAbs C-rh 3BNC117, C-rh 10-1074, and C-rh PGT145 at a dose of 0.2 × 1013 GC/kg of each vector. The AAV inoculation sites were as follows: four 0.5 ml injections into the right quadriceps (AAV9-C-rh 3BNC117), four 0.5 ml injections into the left quadriceps (AAV9-C-rh 10-1074), and four 0.5 ml injections across both deltoid and biceps muscles (AAV9-C-rh PGT145-StII).
Quantification of bnAb levels in vivo
AAV-delivered bnAbs in vivo were quantitated by ELISA. Since the bnAbs C-rh 3BNC117 and C-rh 10-1074 were untagged, we utilized anti-idiotype antibodies as coating reagents at 2 μg/ml: “1F1” (Celldex Therapeutics) to capture C-rh 3BNC117 and “3A1” (Celldex Therapeutics) to capture C-rh 10-1074. Following the coating step, ELISA plates were washed, blocked, and then incubated with serial dilutions of serum (monkeys) or plasma (mice). The two bnAbs were then detected with a monkey-specific secondary HRP-conjugated antibody (1:5000) that has little or no cross-reactivity to IgG of other species (Southern Biotech, cat. # 4700-05). Since the C-rh PGT145 bore a Strep-tag II, that bnAb was captured by using Strep-Tactin coated plates (IBA Lifesciences, cat. # 2-5101-001). Following washing and blocking, the plates were incubated with serial dilutions of serum (monkeys). The C-rh PGT145-StII bnAb was then detected with an anti-human kappa chain secondary HRP-conjugated antibody at 1:5000 (Southern Biotech, cat. # 2060-05). Known concentrations of cell-culture produced and purified mAbs were run in parallel and used as standards to calculate the concentrations of the bnAbs in properly diluted serum or plasma samples.
Quantification of ADA responses in vivo
To measure humoral responses to the individual AAV-delivered bnAbs, purified recombinant C-rh 3BNC117, C-rh 10-1074, and C-rh PGT145-StII were used to coat plates at 2 μg/ml. Then, serum samples (monkeys) or plasma samples (mice) were tested at a 1:20 dilution, and anti-antibodies (ADAs) were detected by means of an anti-lambda HRP-conjugated secondary antibody at 1:5000 (Southern Biotech, cat. # 2070-05) for C-rh 3BNC117 and C-rh PGT145 or an anti-kappa HRP-conjugated secondary antibody at 1:5000 (Southern Biotech, cat. # 2060-05) for C-rh 10-1074 in a regular ELISA as previously described15. ADAs to C-rh 3BNC117 in mouse plasma were detected with an anti-mouse (human-adsorbed) secondary HRP-conjugated antibody (Southern Biotech, cat. # 1031-05) at a 1:5000 dilution. To measure humoral responses to the AAV9 capsid, a rAAV9 preparation was used to coat plates at a working concentration of 1 × 1010 genome copies (GC)/ml. Following washing and blocking, the plates were incubated with a 1:200 dilution of serum (monkeys) or plasma (mice). AAV9 capsid-specific host antibodies were then detected with an anti-monkey secondary HRP-conjugated antibody (1:5000) for monkey samples (Southern Biotech, cat. # 4700-05) or an anti-mouse (human-adsorbed) secondary HRP-conjugated antibody (1:5000) for mouse samples (Southern Biotech, cat. # 1031-05).
Flow cytometry analysis of mouse samples
Flow cytometric quantification of CD4⁺ T cells, CD8⁺ T cells, regulatory T cells (Treg), and T follicular helper (Tfh) cells was performed as follows. PBMCs and splenocytes isolated from mice were stained with surface antibodies: CD45 (clone 30-F11; BV785; BioLegend), CD3 (clone 17A2; AF700; BioLegend), CD4 (clone GK1.5; PE-Cy7; BioLegend), and CD8a (clone 53-6.7; APC-eFluor 780; eBioscience) for 20 min at 4 °C in the dark. Cells were washed with FACS buffer (PBS supplemented with 4% FBS) and fixed/permeabilized using Fixation/Permeabilization solution (Miltenyi Biotec) for 30 min at 4 °C in the dark. Following a wash with 1X Permeabilization buffer (Miltenyi Biotec), cells were stained intracellularly with anti-FoxP3 (clone REA788; PE; Miltenyi Biotec) and anti-Bcl6 (clone BCL-DWN; APC; eBioscience) for 30 min at 4 °C in the dark. After staining, cells were washed with Permeabilization buffer and fixed in 1% fixation buffer (PBS containing 10% formaldehyde).
Stained cells were acquired on a BD LSRFortessa flow cytometer (BD Biosciences) and data were analyzed using FlowJo software (version 10.8.1; FlowJo LLC, BD Life Sciences). Initial gating was performed to identify the lymphocyte population based on forward scatter area (FSC-A) versus side scatter area (SSC-A), which reflect cell size and granularity, respectively. Doublets were excluded using FSC-A versus FSC-height (FSC-H) gating. Within the CD45⁺ population, T cells were identified by co-expression of CD3 (CD45⁺CD3⁺). Subsequently, CD4⁺ and CD8⁺ T cell subsets were gated within the CD3⁺ population, and their percentages were quantified. From the CD3⁺CD4⁺ T cell subset, regulatory T cells (Treg) were defined as CD4⁺FoxP3⁺ cells, while T follicular helper (Tfh) cells were identified as CD4⁺Bcl6⁺. All gating strategies were standardized across samples to ensure consistency in analysis.
Flow cytometry analysis of monkey samples
Quantification of CD4+ T cells, CD8+ T cells and CD4+ T regulatory cells by flow cytometry was conducted as follows. Cryopreserved PBMCs were thawed, washed and stained with an antibody cocktail of CD3 (clone SP34-2; A488; BD Biosciences), CD4 (clone OKT4; PE-Cy7; Biolegend), CD8 (clone RPA-T8; BV711; BD Biosciences), CD25 (clone M-A251; BV421; BD Biosciences), and an amine reactive dye; live/dead near IR 633 (ThermoFisher) for 15 min in the dark. Cells were then washed in RPMI with 10% FBS (R10) and fixed with 2% paraformaldehyde (PFA) for 15 min. Cells were washed in R10 and resuspended in Bulk Permeabilization Reagent: Fix and Perm Medium B (Thermofisher) and stained with Fox P3 (clone 150D; A647; Biolegend) for 15 min in the dark. Cells were washed with R10 and fixed in 2% paraformaldehyde.
Stained cells were run on a BD FACSymphony and data were analyzed using FlowJo v10.8.1 (FlowJo, LLC). First, doublets were excluded by eliminating disproportionately high width in a forward scatter (FSC) area vs. FSC height plot. Next, lymphocytes were gated from the single cells based on their forward scatter and side scatter properties. Gated lymphocytes that were negative for the Live/Dead stain were then selected as live cells. Live cells were gated on CD3+ cells and CD3+/CD4+ and CD3+/CD8+ were gated and percentages recorded. CD3+/CD4+ T cells were selected, and T regulatory cells were gated as CD25+/FoxP3+ cells. Absolute cell counts of CD4+ T cells and CD8+ T cells were determine based on complete blood count data and the percentages of the lymphocyte population as determined by flow cytometry. Cell counts were normalized to cells per 1000 lymphocytes. The T regulatory cells were derived from the CD3+ CD4+ T cell population and were normalized to cells per 1000 CD4+ T cells.
Statistical analysis
All analyses were performed in Prism 10 (GraphPad). Comparisons between two groups were performed using the unpaired two-tailed t test with Welch’s correction. All values are expressed as means. P values of ≤0.05 (*), ≤0.01 (**), and ≤0.001 (***) were considered significant. Error bars represent standard deviation of the means of three or more biological samples. Where indicated, individual values of two groups were compared by the paired two-tailed t test where values are expressed as geometric means, with P > 0.05 being not significant (ns) and both P ≤ 0.05 (*) and P ≤ 0.001 (***) indicating statistical significance; error bars represent standard deviation of the geometric means of three or more biological samples. Correlation analysis on 10 biological samples was performed using the one-tailed Spearman correlation test, with P ≤ 0.05 (*) indicating statistical significance.
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Data availability
All data are available in the main text or the supplementary materials. Source data are provided with this paper. Materials are available with an appropriate material transfer agreement. Source data are provided with this paper.
References
Sok, D. & Burton, D. R. Recent progress in broadly neutralizing antibodies to HIV. Nat. Immunol. 19, 1179–1188 (2018).
Kumar, S., Singh, S. & Luthra, K. An overview of human anti-HIV-1 neutralizing antibodies against diverse epitopes of HIV-1. ACS Omega 8, 7252–7261 (2023).
Wang, D., Tai, P. W. L. & Gao, G. Adeno-associated virus vector as a platform for gene therapy delivery. Nat. Rev. Drug Discov. 18, 358–378 (2019).
Wang, J. H., Gessler, D. J., Zhan, W., Gallagher, T. L. & Gao, G. Adeno-associated virus as a delivery vector for gene therapy of human diseases. Signal Transduct. Target. Ther. 9, 78 (2024).
Fuchs, S. P. & Desrosiers, R. C. Promise and problems associated with the use of recombinant AAV for the delivery of anti-HIV antibodies. Mol. Ther. Methods Clin. Dev. 3, 16068 (2016).
Martinez-Navio, J. M. et al. Adeno-associated virus delivery of anti-HIV monoclonal antibodies can drive long-term virologic suppression. Immunity 50, 567–575.e565 (2019).
Gardner, M. R. et al. AAV-expressed eCD4-Ig provides durable protection from multiple SHIV challenges. Nature 519, 87–91 (2015).
Klenchin, V. A. et al. Adeno-associated viral delivery of Env-specific antibodies prevents SIV rebound after discontinuing antiretroviral therapy. Sci. Immunol. 10, eadq4973 (2025).
Gardner, M. R. et al. AAV-delivered eCD4-Ig protects rhesus macaques from high-dose SIVmac239 challenges. Sci. Transl. Med. 11, https://doi.org/10.1126/scitranslmed.aau5409 (2019).
Liberatore, R. A. & Ho, D. D. The Miami monkey: a sunny alternative to the Berlin patient. Immunity 50, 537–539 (2019).
Keeler, A. M., Zhan, W., Ram, S., Fitzgerald, K. A. & Gao, G. The curious case of AAV immunology. Mol. Ther. 33, 1946–1965 (2025).
Kumar, S. R. P., Duan, D. & Herzog, R. W. Immune responses to muscle-directed adeno-associated viral gene transfer in clinical studies. Hum. Gene Ther. 34, 365–371 (2023).
Ertl, H. C. J. Immunogenicity and toxicity of AAV gene therapy. Front. Immunol. 13, 975803 (2022).
Arjomandnejad, M., Dasgupta, I., Flotte, T. R. & Keeler, A. M. Immunogenicity of Recombinant adeno-associated virus (AAV) vectors for gene transfer. BioDrugs 37, 311–329 (2023).
Martinez-Navio, J. M. et al. Host anti-antibody responses following adeno-associated virus-mediated delivery of antibodies against HIV and SIV in rhesus monkeys. Mol. Ther. 24, 76–86 (2016).
Gardner, M. R. et al. Anti-drug antibody responses impair prophylaxis mediated by AAV-delivered HIV-1 broadly neutralizing antibodies. Mol. Ther. 27, 650–660 (2019).
Mosch, R. & Guchelaar, H. J. Immunogenicity of monoclonal antibodies and the potential use of HLA haplotypes to predict vulnerable patients. Front. Immunol. 13, 885672 (2022).
Harris, C. T. & Cohen, S. Reducing immunogenicity by design: approaches to minimize immunogenicity of monoclonal antibodies. BioDrugs 38, 205–226 (2024).
Keeler, A. M., Zhan, W., Ram, S., Fitzgerald, K. A. & Gao, G. The curious case of AAV immunology. Mol. Ther. https://doi.org/10.1016/j.ymthe.2025.03.037 (2025).
Saunders, K. O. et al. Broadly neutralizing human immunodeficiency virus type 1 antibody gene transfer protects nonhuman primates from mucosal simian-human immunodeficiency virus infection. J. Virol. 89, 8334–8345 (2015).
Welles, H. C. et al. Vectored delivery of anti-SIV envelope targeting mAb via AAV8 protects rhesus macaques from repeated limiting dose intrarectal swarm SIVsmE660 challenge. PLoS Pathog. 14, e1007395 (2018).
Priddy, F. H. et al. Adeno-associated virus vectored immunoprophylaxis to prevent HIV in healthy adults: a phase 1 randomised controlled trial. Lancet HIV 6, e230–e239 (2019).
Casazza, J. P. et al. Safety and tolerability of AAV8 delivery of a broadly neutralizing antibody in adults living with HIV: a phase 1, dose-escalation trial. Nat. Med. 28, 1022–1030 (2022).
Gross, D. A., Tedesco, N., Leborgne, C. & Ronzitti, G. Overcoming the challenges imposed by humoral immunity to AAV vectors to achieve safe and efficient gene transfer in seropositive patients. Front. Immunol. 13, 857276 (2022).
Earley, J., Piletska, E., Ronzitti, G. & Piletsky, S. Evading and overcoming AAV neutralization in gene therapy. Trends Biotechnol. 41, 836–845 (2023).
Muhuri, M. et al. Overcoming innate immune barriers that impede AAV gene therapy vectors. J. Clin. Investig. 131, https://doi.org/10.1172/jci143780 (2021).
Chu, W. S. & Ng, J. Immunomodulation in administration of rAAV: preclinical and clinical adjuvant pharmacotherapies. Front. Immunol. 12, 658038 (2021).
Prasad, S. et al. Immune responses and immunosuppressive strategies for adeno-associated virus-based gene therapy for treatment of central nervous system disorders: current knowledge and approaches. Hum. Gene Ther. 33, 1228–1245 (2022).
Krown, S. E. et al. Rapamycin with antiretroviral therapy in AIDS-associated Kaposi sarcoma: an AIDS Malignancy Consortium study. J. Acquir. Immune Defic. Syndr. 59, 447–454 (2012).
Stock, P. G. et al. Reduction of HIV persistence following transplantation in HIV-infected kidney transplant recipients. Am. J. Transpl. 14, 1136–1141 (2014).
Trepanier, D. J., Gallant, H., Legatt, D. F. & Yatscoff, R. W. Rapamycin: distribution, pharmacokinetics and therapeutic range investigations: an update. Clin. Biochem. 31, 345–351 (1998).
Varco-Merth, B. D. et al. Rapamycin limits CD4+ T cell proliferation in simian immunodeficiency virus-infected rhesus macaques on antiretroviral therapy. J. Clin. Investig. 132, https://doi.org/10.1172/jci156063 (2022).
Yatscoff, R. W., Wang, P., Chan, K., Hicks, D. & Zimmerman, J. Rapamycin: distribution, pharmacokinetics, and therapeutic range investigations. Ther. Drug Monit. 17, 666–671 (1995).
Kahan, B. D. et al. Therapeutic drug monitoring of sirolimus: correlations with efficacy and toxicity. Clin. Transpl. 14, 97–109 (2000).
Kishimoto, T. K. et al. Improving the efficacy and safety of biologic drugs with tolerogenic nanoparticles. Nat. Nanotechnol. 11, 890–899 (2016).
Moghimi, B. et al. Induction of tolerance to factor VIII by transient co-administration with rapamycin. J. Thromb. Haemost.9, 1524–1533 (2011).
Battaglia, M. et al. Rapamycin promotes expansion of functional CD4+CD25+FOXP3+ regulatory T cells of both healthy subjects and type 1 diabetic patients. J. Immunol.177, 8338–8347 (2006).
Fraser, H. et al. A rapamycin-based GMP-Compatible process for the isolation and expansion of regulatory T cells for clinical trials. Mol. Ther. Methods Clin. Dev. 8, 198–209 (2018).
Baeten, P. et al. Rapamycin rescues loss of function in blood-brain barrier-interacting Tregs. JCI Insight 9, https://doi.org/10.1172/jci.insight.167457 (2024).
Passerini, L. et al. Treatment with rapamycin can restore regulatory T-cell function in IPEX patients. J. Allergy Clin. Immunol. 145, 1262–1271.e1213 (2020).
Nayak, S. et al. Prevention and reversal of antibody responses against factor IX in gene therapy for hemophilia B. Front. Microbiol. 2, 244 (2011).
Nayak, S. et al. Prophylactic immune tolerance induced by changing the ratio of antigen-specific effector to regulatory T cells. J. Thromb. Haemost.7, 1523–1532 (2009).
Gernoux, G., Wilson, J. M. & Mueller, C. Regulatory and exhausted T cell responses to AAV capsid. Hum. Gene Ther. 28, 338–349 (2017).
Gernoux, G. et al. Muscle-directed delivery of an AAV1 vector leads to capsid-specific T cell exhaustion in nonhuman primates and humans. Mol. Ther.28, 747–757 (2020).
Xiang, Z. et al. The effect of rapamycin and ibrutinib on antibody responses to adeno-associated virus vector-mediated gene transfer. Hum. Gene Ther. 33, 614–624 (2022).
Meliani, A. et al. Antigen-selective modulation of AAV immunogenicity with tolerogenic rapamycin nanoparticles enables successful vector re-administration. Nat. Commun. 9, 4098 (2018).
Kishimoto, T. K. Development of ImmTOR tolerogenic nanoparticles for the mitigation of anti-drug antibodies. Front. Immunol. 11, 969 (2020).
Muhuri, M., Levy, D. I., Schulz, M., McCarty, D. & Gao, G. Durability of transgene expression after rAAV gene therapy. Mol. Ther.30, 1364–1380 (2022).
Liston, A. & Aloulou, M. A fresh look at a neglected regulatory lineage: CD8(+)Foxp3(+) Regulatory T cells. Immunol. Lett. 247, 22–26 (2022).
Sun, J. et al. Efficient therapeutic function and mechanisms of human polyclonal CD8(+)CD103(+)Foxp3(+) regulatory T cells on collagen-induced arthritis in mice. J. Immunol. Res. 2019, 8575407 (2019).
Ando, S. et al. mTOR regulates T cell exhaustion and PD-1-targeted immunotherapy response during chronic viral infection. J. Clin. Investig. 133, https://doi.org/10.1172/jci160025 (2023).
Reyes, A., Mohanty, A., Pharaon, R. & Massarelli, E. Association between immunosuppressive therapy utilized in the treatment of autoimmune disease or transplant and cancer progression. Biomedicines 11, https://doi.org/10.3390/biomedicines11010099 (2022).
Mingozzi, F. et al. Modulation of tolerance to the transgene product in a nonhuman primate model of AAV-mediated gene transfer to liver. Blood 110, 2334–2341 (2007).
Mingozzi, F. et al. Pharmacological modulation of humoral immunity in a nonhuman primate model of AAV gene transfer for hemophilia B. Mol. Ther.20, 1410–1416 (2012).
Jiang, H. et al. Effects of transient immunosuppression on adenoassociated, virus-mediated, liver-directed gene transfer in rhesus macaques and implications for human gene therapy. Blood 108, 3321–3328 (2006).
Cramer, M. L., Shao, G., Rodino-Klapac, L. R., Chicoine, L. G. & Martin, P. T. Induction of T-cell infiltration and programmed death ligand 2 expression by adeno-associated virus in rhesus macaque skeletal muscle and modulation by prednisone. Hum. Gene Ther. 28, 493–509 (2017).
Samelson-Jones, B. J., Finn, J. D., Favaro, P., Wright, J. F. & Arruda, V. R. Timing of intensive immunosuppression impacts risk of transgene antibodies after AAV gene therapy in nonhuman primates. Mol. Ther. Methods Clin. Dev. 17, 1129–1138 (2020).
Ishii, A. et al. rAAV8 and rAAV9-mediated long-term muscle transduction with tacrolimus (FK506) in non-human primates. Mol. Ther. Methods Clin. Dev. 18, 44–49 (2020).
McIntosh, J. H. et al. Successful attenuation of humoral immunity to viral capsid and transgenic protein following AAV-mediated gene transfer with a non-depleting CD4 antibody and cyclosporine. Gene Ther. 19, 78–85 (2012).
Salabarria, S. M. et al. Thrombotic microangiopathy following systemic AAV administration is dependent on anti-capsid antibodies. J. Clin. Investig. 134, https://doi.org/10.1172/jci173510 (2024).
Burton, D. R. Antiviral neutralizing antibodies: from in vitro to in vivo activity. Nat. Rev. Immunol. 23, 720–734 (2023).
Wagh, K. et al. Optimal combinations of broadly neutralizing antibodies for prevention and treatment of HIV-1 clade C infection. PLoS Pathog. 12, e1005520 (2016).
Schoofs, T. et al. HIV-1 therapy with monoclonal antibody 3BNC117 elicits host immune responses against HIV-1. Science 352, 997–1001 (2016).
Scheid, J. F. et al. Sequence and structural convergence of broad and potent HIV antibodies that mimic CD4 binding. Science 333, 1633–1637 (2011).
Mouquet, H. et al. Complex-type N-glycan recognition by potent broadly neutralizing HIV antibodies. Proc. Natl. Acad. Sci. USA 109, E3268–E3277 (2012).
Walker, L. M. et al. Broad neutralization coverage of HIV by multiple highly potent antibodies. Nature 477, 466–470 (2011).
Giudicelli, V., Brochet, X. & Lefranc, M. P. IMGT/V-QUEST: IMGT standardized analysis of the immunoglobulin (IG) and T cell receptor (TR) nucleotide sequences. Cold Spring Harb. Protoc. 2011, 695–715 (2011).
Lefranc, R. uiz,M. M. P. IMGT gene identification and Colliers de Perles of human immunoglobulins with known 3D structures. Immunogenetics 53, 857–883 (2002).
Calvas, P. et al. Characterization of the three immunoglobulin G subclasses of macaques. Scand. J. Immunol. 49, 595–610 (1999).
Scinicariello, F., Engleman, C. N., Jayashankar, L., McClure, H. M. & Attanasio, R. Rhesus macaque antibody molecules: sequences and heterogeneity of alpha and gamma constant regions. Immunology 111, 66–74 (2004).
Ko, S. Y. et al. Enhanced neonatal Fc receptor function improves protection against primate SHIV infection. Nature 514, 642–645 (2014).
Zalevsky, J. et al. Enhanced antibody half-life improves in vivo activity. Nat. Biotechnol. 28, 157–159 (2010).
Fuchs, S. P., Martinez-Navio, J. M., Gao, G. & Desrosiers, R. C. Recombinant AAV vectors for enhanced expression of authentic IgG. PloS one 11, e0158009 (2016).
Agudo, J. et al. The miR-126-VEGFR2 axis controls the innate response to pathogen-associated nucleic acids. Nat. Immunol. 15, 54–62 (2014).
Boisgerault, F. et al. Prolonged gene expression in muscle is achieved without active immune tolerance using microrRNA 142.3p-regulated rAAV gene transfer. Hum. Gene Ther. 24, 393–405 (2013).
Majowicz, A. et al. Mir-142-3p target sequences reduce transgene-directed immunogenicity following intramuscular adeno-associated virus 1 vector-mediated gene delivery. J. Gene Med. 15, 219–232 (2013).
Su, Q., Sena-Esteves, M. & Gao, G. Production of recombinant adeno-associated viruses (rAAVs) by transient transfection. Cold Spring Harb. Protoc. 2020, 095596 (2020).
Su, Q., Sena-Esteves, M. & Gao, G. Purification of recombinant adeno-associated viruses (rAAVs) by cesium chloride gradient sedimentation. Cold Spring Harb. Protoc. 2020, 095604 (2020).
Sanmiguel, J., Gao, G. & Vandenberghe, L. H. Quantitative and digital droplet-based AAV genome titration. Methods Mol. Biol. 1950, 51–83 (2019).
Garber, J. C. et al. in Guide for the Care and Use of Laboratory Animals 8th edn (National Academies Press, 2011).
Gardner, M. R. et al. High concordance of ELISA and neutralization assays allows for the detection of antibodies to individual AAV serotypes. Mol. Ther. Methods Clin. Dev. 24, 199–206 (2022).
Acknowledgements
The authors would like to thank Desiree E. Mendes and Claudia P. Ramos Muniz for technical assistance. We would also like to thank Qin Su and Ran He of The Horae Gene Therapy Center at UMass Chan Medical School for excellent AAV vector preparation and supportive advice. We thank the staff of the Division of Laboratory Animal Medicine at UCLA for professional animal care and excellent experimental conduct. We are very grateful for the outstanding support by the Wisconsin National Primate Research Center staff (Immunology Core Laboratory, Scientific Protocol Implementation Unit, and Animal Services Unit) for professional animal care and excellent experimental conduct; in particular, we would like to thank Logan Vosler and Matt Reynolds for their help. Additionally, we thank Michel C. Nussenzweig (The Rockefeller University) for generously providing reagents. This project was supported by Miami-Dade County (State of Florida) through the award contract # 24-UMAR (to M. Stevenson and R.C.D.), and by the NIH award U19AI149646 from the National Institute of Allergy and Infectious Diseases (to M. Farzan and R.C.D.). The study was further supported by a pilot award by the HIV/AIDS and Emerging Infectious Diseases Institute (HEIDI) at the University of Miami through the State of Florida Funding Initiative (to S.P.F.) sponsored by the State of Florida, Department of Health (award contract #CODVD to M. Stevenson). This work was also funded by the National Institute of Allergy and Infectious Diseases (R01AI172727 and R01DA059873 to A.Z.), the American Foundation for AIDS Research (grants 110304-71-RKRL to A.Z.). This work was also supported by the UCLA AIDS Institute, the James B. Pendleton Charitable Trust, and the McCarthy Family Foundation.
Author information
Authors and Affiliations
Contributions
>The study was conceived and designed by S.P.F., A.Z. and R.C.D. The study was supervised and monitored by S.P.F., D.M.D., E.A., G.G., A.Z. and R.C.D. The experiments were performed by S.P.F., P.G.M., R.Z., S.T., L.W., E.C., K.L.W., J.F., J.C., E.A., J.M.T. and J.M.M.-N. Critical reagents and input were provided by J.C., J.X. and J.M.M.-N. Data analysis was performed by S.P.F., J.C., G.G., J.M.T., J.M.M.-N., A.Z. and R.C.D. The manuscript was composed by S.P.F., A.Z. and R.C.D.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests. G.G. is a scientific co-founder of Voyager Therapeutics, Adrenas Therapeutics, and Aspa Therapeutics, and holds equity in these companies. G.G. is an inventor on patents with potential royalties licensed to Voyager Therapeutics, Aspa Therapeutics, and other biopharmaceutical companies. R.C.D. is a co-founder of Marguron LLC.
Peer review
Peer review information
Nature Communications thanks Roland Herzog and the other, anonymous, reviewer(s) for their contribution to the peer review of this work. A peer review file is available.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Source data
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Fuchs, S.P., Mondragon, P.G., Zabizhin, R. et al. Transient rapamycin treatment avoids unwanted host immune responses toward AAV-delivered anti-HIV antibodies. Nat Commun 16, 8906 (2025). https://doi.org/10.1038/s41467-025-63970-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41467-025-63970-6