Abstract
Breast cancer (BC) is a leading cause of death among women, with approximately 30% HER2−positive (HER2+). Although HER2-targeted therapies have improved outcomes for patients with HER2+ metastatic breast cancer (mBC), clinical challenges and prognostic variability remain. Tumor-infiltrating lymphocytes (TILs) have emerged as prognostic and predictive biomarkers in various tumors, including BC, but their role in HER2+ mBC is poorly understood. This multicentric retrospective cohort study evaluated the prognostic significance of TILs in 110 patients with HER2+ mBC treated with pertuzumab, trastuzumab, and taxane-based chemotherapy at two Italian institutes from June 2013 to May 2024. TILs were assessed on metastatic or primary tumor samples. High TILs levels (>5%) were independently associated with longer PFS and OS. TILs levels were higher in primary tumours than in metastases (p = 0.009), with significant variation by metastatic site. These findings underscore the potential of TILs as prognostic biomarkers in HER2+ mBC, necessitating further prospective studies.
Similar content being viewed by others
Introduction
Breast cancer (BC) remains a leading cause of cancer-related morbidity and mortality among women worldwide, with approximately 20–30% of cases exhibiting HER2-positive (HER2+) status1,2,3. HER2+ BCs are known for their aggressive nature and poor prognosis. The clinical outcomes of patients with HER2+ BC have tangibly improved with the advent of HER2-targeted therapies such as trastuzumab and pertuzumab, small molecules, and recently with the novel antibody-drug conjugates such as trastuzumab deruxtecan2,3,4,5. Despite these advances, metastatic HER2+ BC generally remains incurable, with treatment aimed at prolonging survival and improving quality of life6.
Tumor-infiltrating lymphocytes (TILs) have emerged as significant prognostic and predictive biomarkers in different tumor types, including BC7. In early-stage BC, high levels of TILs have been consistently associated with better treatment responses in HER2+ and triple-negative BC, suggesting an active immune environment that contributes to tumor control8,9. Indeed, in HER2+ early BC disease, several studies in the neoadjuvant and adjuvant setting have evaluated TILs as prognostic factors and predictors of response, demonstrating a positive correlation with better clinical outcomes9,10,11,12,13.
However, the role of TILs in metastatic BC (mBC), particularly in the context of HER2+ disease, is less understood. While some studies have suggested that TILs might confer a survival advantage in mBC, others have reported divergent or inconclusive results14,15. Indeed, data about the immunogenicity of HER2+ BC paved the way for clinical trials evaluating immune checkpoint inhibitors (ICIs) in this subtype, with underwhelming results so far15,16,17. These findings may vary widely due to differences in patient populations, methodologies for assessing TILs, and the heterogeneity of metastatic disease. Data on the role and presence of TILs in BC metastatic sites is generally limited, revealing a correlation between TIL percentages in primary tumors and their metastatic counterparts, though the percentages are typically lower in the metastatic setting18,19,20.
Given these complexities, we designed a study that aims to comprehensively evaluate the prognostic value of TILs in a cohort of patients with HER2+ mBC receiving first-line therapy in two reference breast cancer centers. By focusing on this particular patient group and employing rigorous methodologies to assess TILs, we seek to clarify their role in influencing clinical outcomes and explore the potential for TILs as biomarkers to guide therapy choices in advanced disease stages.
Results
Patient characteristics
Our multicentric retrospective study cohort included 110 patients with HER2+ mBC treated at the European Institute of Oncology and the AOU Policlinico Umberto I from June 2013 to May 2024. TILs levels were assessed on hematoxylin and eosin (H&E)-stained slides from metastatic (n = 57) or primary tumor (n = 53) samples. Only for a small subset of patients (n = 13), TIL levels were evaluated in both the primary tumor and metastatic sites. The study population comprised patients with a median age of 49 (interquartile range (IQR) 43.5–56.4) years. Of these, 60 (54.6%) were hormone receptor (HR)-positive (HR+), and 50 (45.4%) were HR−negative (HR-) BC. The majority of patients were premenopausal or perimenopausal at the time of diagnosis (50.9%), and 45.4% had de novo metastatic disease. Additionally, 75 patients (68.2%) presented with visceral disease, and 9 patients (8.2%) had brain metastases (BMs) at the time of diagnosis. Fifty percent of the patients achieved a partial response as the best response to first-line treatment. For the whole cohort, at a median follow-up of 18.4 months, the median progression-free survival (PFS) was 25.1 months (95% CI: 14.7–49.3). Regarding overall survival (OS), the median OS was not reached, with a median follow-up of 37.2 months.
Considering only the cohort of patients where TILs were evaluated on the metastatic site (n = 57 patients), the majority of patients were HR-negative (50.9%), and only 12 patients (21.1%) were metastatic at diagnosis.
The clinical-pathological characteristics of the patients included in our study are shown in Table 1.
TIL levels and correlation with clinicopathological features
TILs were successfully assessed in all 110 samples. Of these, 57 samples were collected from metastatic sites and 53 from primary tumors. The median expression of TILs was 10% (IQR: 5–15%). The correlations between TILs as a continuous variable and the clinicopathological characteristics of patients were evaluated (Table 2).
In the entire cohort, the percentage of TILs in patients with visceral disease was significantly lower than in those without visceral disease (median 10% vs 15%, P = 0.048). HER2+/HR− tumors showed a trend toward significantly higher TIL levels compared to HR+ tumors (mean 14.3 vs 11.9, p = 0.08). No statistically significant difference was observed when comparing estrogen receptor-positive/progesterone receptor-positive (ER+/PR+) vs ER+/PR-negative (p = 0.845).
Furthermore, the site of metastases where TILs were evaluated was associated with TILs values. Lung metastases had higher TIL levels compared to liver metastases (median TILs: 15% vs 5%, unadjusted p-value (p) <0.001, adjusted p = 0.01). A similar trend was observed for bone metastases (median TILs: 15% vs 7.5%, adjusted p = 0.145 and unadjusted p = 0.016) (Fig. 1).
The box plot graph shows the distribution of TILs across various metastatic sites in the cohort of patients whose TILs were evaluated at the metastatic site. Each box represents the IQR of TIL percentages, with the line inside the box indicating the median. The whiskers extend to the minimum and maximum values within 1.5 times the IQR from the quartiles, and individual points outside this range are plotted as outliers. Only significant p-values were reported. IQR interquartile range, LN lymph nodes, TILs tumor-infiltrating lymphocytes, p p-value.
Association of TILs with survival outcomes in all cohort (n = 110 women)
Regarding survival outcomes, we evaluated the correlation between TILs levels and PFS. Since there is no consensus on a high/low TIL score cut-off14, we explored the prognostic role of TILs in mBC using the 25th, 50th, and 75th percentiles of TILs distribution (5%, 10%, and 15%, respectively). We identified the 25th percentile (TILs value of 5%) as a potential cut-off for prognosis differentiation (Fig. 2). The high TILs group had a significantly longer PFS than the low TILs group (median: 49.3 vs. 18.5 months; p = 0.022). Notably, high TILs (cut-off >5%) were more common in HR− patients (74% HR− vs. 55% HR+, p = 0.048).
The images consist of Kaplan–Meier survival curves illustrating the PFS of HER2+ mBC enrolled patients according to the TILs level. The green curves represent those patients with low TILs levels, while the orange curve represents those with high TIL levels. The number of patients at risk at various time points is displayed below the survival curves for both TIL groups. a Kaplan–Meier survival curves using the 25° percentile (5%) as a cut-off for a high/low TIL score. The median PFS for patients with high TIL levels is significantly longer than for those with low TIL levels, as indicated by the p-value of 0.022. b Kaplan–Meier survival curves using the 50° percentile (10%) as a cut-off for a high/low TIL score. The median difference in PFS between the two groups is not statistically significant, with a p-value of 0.45. c Kaplan–Meier survival curves using the 75° percentile (15%) as a cut-off for a high/low TIL score. The median difference in PFS between the two groups is not statistically significant, with a p-value of 0.16. These plots demonstrate the potential prognostic value of TIL levels in predicting the PFS of patients, highlighting a significant association when using a 5% threshold for TIL levels. mBC metastatic breast cancer, PFS progression-free survival, TILs tumor-infiltrating lymphocytes.
We examined the correlation between TILs levels and PFS, adjusting for clinical variables such as age, visceral disease involvement, HR status, and TILs evaluation site. Univariate analysis showed that low TILs were associated with worse PFS (HR = 1.74, 95% CI: 1.08–2.81, p = 0.024). This association remained significant when adjusting for the aforementioned clinical variables (HR = 1.77, 95% CI: 1.08–2.90, p = 0.024) (Table 3). When considering TILs as a continuous variable (per 10% increments), higher TILs were related to a better prognosis, though not statistically significant (Supplementary Table 1).
Analyzing OS outcome, the 25th percentile (TILs value of 5%) was a significant prognostic cut-off (Fig. 3). In the univariate analysis, low TILs were associated with worse OS (HR = 2.02, 95% CI: 1.02–4.00, p = 0.044) and when adjusting for age, visceral disease, HR status, and TILs evaluation site, an association of TILs with OS showed a similar trend at the limit of statistical significance (Table 4). When considering TILs as a continuous variable (per 10% increments), higher TILs were associated with a better prognosis but did not reach statistical significance (HR = 0.81, 95% CI: 0.56–1.16, p = 0.252) (Supplementary Table 1). Moreover, there was no association between HER2 status (HER2 2 + FISH amplified vs HER2 3+) and PFS or OS (data not shown).
The images consist of Kaplan–Meier survival curves illustrating the OS of HER2+ mBC enrolled patients according to the TILs level. The green curves represent those patients with low TILs levels, while the orange curve represents those with high TIL levels. The number of patients at risk at various time points is displayed below the survival curves for both TIL groups. a Kaplan–Meier survival curves using the 25° percentile (5%) as a cut-off for a high/low TIL score. The median OS for patients with high TIL levels is significantly longer than for those with low TIL levels, as indicated by the p-value of 0.04. b Kaplan–Meier survival curves using the 50° percentile (10%) as a cut-off for a high/low TIL score. The median difference in OS between the two groups is not statistically significant, with a p-value of 0.58. c Kaplan–Meier survival curves using the 75° percentile (15%) as a cut-off for a high/low TIL score. The median difference in OS between the two groups is not statistically significant, with a p-value of 0.38. mBC metastatic breast cancer, OS overall survival, TILs tumor-infiltrating lymphocytes.
Association of TILs with survival outcomes in the cohort TILs on metastatic site (n = 57)
We assessed the prognostic impact of TILs in patients whose TILs were evaluated at the metastatic site. The median PFS was 25.1 months for the low TILs group (≤5%) and 60.6 months for the high TILs group (>5%) (p = 0.032) (Fig. 4). In the univariate analysis, low TILs were associated with inferior PFS (HR = 2.09, 95% CI: 1.05-4.15, p = 0.036). After adjusting for age, visceral disease, HR status, and the metastatic site where TILs were evaluated, the significant association between TILs and PFS was confirmed (HR = 2.26, 95% CI: 1.01–5.06) (Table 5). When considering TILs as a continuous variable (per 10% increments), higher TIL levels were associated with better PFS, though this was not statistically significant (HR = 0.62, 95% CI: 0.38–1.02, p = 0.061). However, in the adjusted model, higher TILs values were significantly associated with better PFS, suggesting a potential prognostic role for TILs (HR = 0.57, 95% CI: 0.32–0.98, p = 0.045). (Supplementary Table 2).
The images consist of Kaplan-Meier survival curves illustrating the PFS of patients whose TILs were evaluated at the metastatic site according to the TILs level. The green curves represent those patients with low TILs levels, while the orange curve represents those with high TIL levels. The number of patients at risk at various time points is displayed below the survival curves for both TIL groups. a Kaplan–Meier survival curves using the 25° percentile (5%) as the cut-off for a high/low TIL score. The median PFS for patients with high TIL levels is significantly longer than for those with low TIL levels, as indicated by the p-value of 0.032. b Kaplan–Meier survival curves using the 50° percentile (10%) as a cut-off for a high/low TIL score. The median difference in PFS between the two groups is not statistically significant, with a p-value of 0.78. c Kaplan–Meier survival curves using the 75° percentile (15%) as a cut-off for a high/low TIL score. The median difference in PFS between the two groups is not statistically significant, with a p-value of 0.18. PFS progression-free survival, TILs tumor-infiltrating lymphocytes.
Patients with TILs >5% had a significantly longer median OS compared to those with TILs ≤5%, as shown in Fig. 5. In univariate analysis, low TILs (≤5%) were associated with poorer OS (HR = 3.18, 95% CI: 1.19–8.50, p = 0.021). After, adjusting for clinical variables, the association of TILs with OS was at the limit of statistical significance (HR = 2.97, 95% CI: 0.90–9.87, p = 0.075), (Table 6) but in a subsequent model, the significant association was confirmed (HR = 3.17, 95% CI: 1.17–8.65, p = 0.024). As a continuous variable (per 10% increments), higher TIL levels were significantly associated with better OS (HR = 0.45, 95% CI: 0.20–0.99, p = 0.048). When controlling for clinical variables, a similar trend was observed but did not reach statistical significance (HR = 0.44, 95% CI: 0.17–1.18, p = 0.104) (Supplementary Table 2).
The images consist of Kaplan–Meier survival curves illustrating the OS of patients whose TILs were evaluated at the metastatic site according to the TILs level. The green curves represent those patients with low TILs levels, while the orange curve represents those with high TIL levels. The number of patients at risk at various time points is displayed below the survival curves for both TIL groups. a Kaplan–Meier survival curves using the 25° percentile (5%) as a cut-off for a high/low TIL score. The median OS for patients with high TIL levels is significantly longer than for those with low TIL levels, as indicated by the p-value of 0.015. b Kaplan–Meier survival curves using the 50° percentile (10%) as a cut-off for a high/low TIL score. The median difference in OS between the two groups is not statistically significant, with a p-value of 0.43. c Kaplan–Meier survival curves using the 75° percentile (15%) as a cut-off for a high/low TIL score. The median difference in OS between the two groups is not statistically significant, with a p-value of 0.32. OS overall survival, TILs tumor-infiltrating lymphocytes.
Paired samples
For a small subset of patients (n = 13), TIL levels were evaluated in both the primary tumor and metastatic sites. The comparison revealed that the percentage of TILs in the metastatic site was significantly lower (median: 10%) than in the primary tumors (median: 15%) (P = 0.008) (Fig. 6).
For n = 13 patients TILs are available in primary tumors and corresponding metastases, which are distributed as follows: n = 4 liver, n = 3 lung, n = 3 lymph node, n = 2 soft tissue, and n = 1 bone. The percentage of TILs in the metastatic site was significantly lower (median:10%) than in the primary tumors (median: 15%) (Wilcoxon paired test, P = 0.008). prim primary site, MT metastatic site, TILs tumor-infiltrating lymphocytes.
Discussion
In our multicentric retrospective study from BC referral institutions in Italy, we underscore the complex significance of TILs in HER2+ mBC. While high TIL levels in early-stage BC are consistently linked to better prognosis and response to therapy10, our data highlight the impact of TILs on clinical outcomes in the metastatic setting. In early HER2+ BC, several studies demonstrated that increased TILs positively correlate with response to neoadjuvant therapy and clinical benefit in HER2+ BC, similar to the adjuvant setting, where higher TILs display a reduced risk of recurrence10,13,21. Indeed, high stromal TILs correlate with an improved prognosis and an enhanced response to trastuzumab and chemotherapy9,22.
Our study found no significant difference in terms of PFS or OS when comparing patients with high and low TILs levels using the cut-off of 10% or 15% (the median and 75° percentile of TIL distribution respectively). However, a lower threshold (5%, at the lower 25% percentile) for TILs provided a significant prognostic stratification. Patients with higher TILs levels (>5%) had meaningfully longer PFS and OS compared to those with low TILs levels (≤5%) in univariate models, with somewhat consistent results after adjusting for relevant prognostic variables. These findings align with previous studies suggesting that TILs reflect an ongoing anti-tumor immune response and may further enhance anti-tumor immunity through their functional activity, improving patient outcomes. The Cox regression analysis further supported the prognostic value of TILs. Low TILs levels were associated with poorer PFS and OS, even after adjusting for potential confounders such as age, HR status, and visceral disease. Interestingly, when TILs were considered as a continuous variable, higher TILs levels were associated with better outcomes, though statistical significance was not consistently reached.
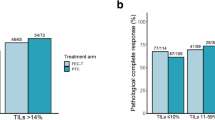
Previous research in metastatic HER2+ BC has produced mixed results. The CLEOPATRA trial found that higher TIL level values were significantly associated with increased OS, irrespective of the treatment group, but only 7% of analyzed samples were from metastatic sites14. One explanation, suggested by the authors for these findings, was that a more functional antitumor immune response, involving various immune subsets such as T-effector cells, B cells, and NK cells, may drive some of the immunomodulating effects of HER2-directed therapies23,24. Conversely, the MA.31 trial, which utilized a 5% threshold, reported no significant prognostic or predictive effects, likely due to the evaluation of TILs in primary tumor samples and a less immunogenic cohort, were found for TILs counts25.
In the PANACEA trial, trastuzumab pre-treated patients with HER2-positive BC received pembrolizumab in combination with trastuzumab and it was observed that the subgroup with higher expression of TILs had a higher objective response rate (ORR). In an exploratory analysis of this trial, authors showed that levels of TILs in the Programmed Death-Ligand 1 (PD-L1)-positive cohort were significantly higher and that there was significantly greater lymphocytic infiltration in objective responders and cases of patients with disease control15. Notably, among all PD-L1+ patients, 41% had TILs level ≥5% and in this cohort, the disease control rate was 47% compared to 5% in patients with TILs <5%26. This discrepancy highlights the potentially divergent roles of the immune environment in different populations and stages of BC.
However, Stover et al. demonstrated a correlation between TILs and both PFS and OS in chemotherapy-treated mBC patients, while adjusting for the treatment arm in those enrolled in the phase III CALGB 40502 trial. The authors selected a 5% TIL threshold based on previous studies in both triple-negative and HER2+ BC, thereby supporting our results27.
In addition, in our study, a small number of patients had TILs data from both the primary tumor and the metastasis. Comparing the percentage of TILs in both samples, the value was much lower in the metastasis. This finding is intriguing, as it suggests that the immune response within the tumor microenvironment may decrease as the disease progresses and metastasizes. The reduced TIL levels in metastatic sites could reflect an immune escape mechanism, where tumors in advanced stages become less responsive to immune infiltration, potentially contributing to poorer outcomes. This underscores the need for further investigation into how the immune microenvironment evolves during cancer progression and how it might be leveraged to improve therapeutic strategies in metastatic settings. Even though the sample size was very small, it is interesting to point out that it confirmed similar findings in other studies including different solid tumors28,29,30. Several factors could influence this variation. First, the immune suppressive mechanisms are likely more pronounced in metastatic disease, possibly due to increased tumor heterogeneity and the evolution of immune evasion strategies as cancer progresses. Moreover, the metastatic niche, especially in “immune sanctuaries” like the brain, may present unique immune challenges that differ fundamentally from those encountered in primary tumor sites.
Indeed, there are differences also according to the site of metastases where TILs were evaluated. The highest mean percentage of TILs was observed in metastatic samples from the lung and lymph node, and lowest in liver, bone, or soft tissue samples, as previously described31,32. It is important to note that, unlike TIL evaluation in primary sites10, there is currently no international consensus on TIL assessment in metastatic sites. Additionally, a higher TIL percentage in lymph nodes can be attributed to the unique characteristics of the lymph node environment, which is naturally enriched with lymphoid cells, potentially distorting the evaluation.
Furthermore, evaluating the correlations between TILs as a continuous variable and the clinicopathological characteristics of patients, we observed that HR- patients had higher values of TILs at the limit of statistical significance, confirming previous results that suggested a correlation between ER expression and decreased function of CD8+ T-cells33,34. We found also that the percentage of TILs was lower in patients with visceral disease at diagnosis, suggesting that low TILs correlate with a more aggressive disease.
However, while this study offers valuable insights, it has several limitations. Indeed, its retrospective nature may introduce selection biases. For example, in our cohort, BMs were observed in only 9 patients (8.2%) at the time of diagnosis of metastatic disease. Given the small number of events, this variable was not included in the multivariate model. However, considering the known prognostic impact of brain involvement in HER2+ mBC, this should be acknowledged as a potential limitation of our analysis. An additional limitation of our study is the variability in assessments made by different pathologists. Nevertheless, we attempted to minimize this risk by following standardized protocols for TILs evaluation, and the assessments were carried out by experienced pathologists. Notably, for 10 patients, TILs were evaluated on lymph nodes as metastatic samples. Although another limitation is the small sample size included compared to other publications, TILs were assessed in most cases on tissue samples from metastatic sites, whereas in other studies, nearly all assessments were performed on primary tumor samples. Our findings offer some insights into how the tumor microenvironment and its interaction with the immune system may change from early-stage to metastatic disease. This underscores the need to consider different tissue sources when analyzing TILs and their potential relevance to prognosis and treatment response, while also recognizing that an international consensus on the evaluation of TILs in metastatic sites has yet to be established.
Future prospective studies with standardized TILs evaluation protocols are necessary to validate these findings. Indeed, discrepancies in the role of TILs as prognostic biomarkers in advanced HER2+ BC across different studies necessitate further evaluation due to various methodological concerns, such as differing TILs thresholds, sampling sites (primary vs. metastatic), and patient characteristics. Future research should involve larger cohorts to confirm these observations and investigate the mechanisms behind the differing roles of TILs in primary versus metastatic BC. Biomarker development should focus on aspects of the immune response that correlate with therapeutic outcomes in different contexts and metastatic sites. Understanding the immune landscape in mBC is crucial for optimizing treatment strategies and improving patient outcomes, especially since clinical trials have shown poor results with immunotherapy in advanced disease, even in TIL-enriched cancers15,16,17. In conclusion, despite the limitations of our study, it provides valuable insights into the interaction between the tumor microenvironment and the immune system in HER2+ mBC.
Methods
Study design and patient selection
This multicentric retrospective cohort study included 110 consecutive patients with confirmed HER2+ mBC, treated at the European Institute of Oncology and the AOU Policlinico Umberto I, between June 2013 and May 2024, using pertuzumab, trastuzumab, and taxane-based chemotherapy as first-line therapy. Eligibility criteria were adults aged 18 or older, diagnosed with stage III unresectable and stage IV HER2 + BC, and treated with a first-line regimen of pertuzumab, trastuzumab, and taxane-based chemotherapy. Patients were excluded if they had received prior systemic therapy for metastatic disease, had incomplete medical records, or had no available archival tumor samples. The study was conducted in accordance with Good Clinical Practice guidelines and the declaration of Helsinki. Written informed consent was obtained from all patients. The study received approval from the respective institutional Research Ethics Boards, including the Coordinating Center Ethics Committee (European Institute of Oncology, Approval Number: ID4176) and the Institutional Ethics Committee of AOU Policlinico Umberto I (Protocol n° 805/16, RIF.CE:4181).
Data collection
Clinical features and outcomes were retrieved from electronic medical records in both institutes. This included demographic details, treatment regimens, response rates, date of disease progression, and death. The date of initial diagnosis, the onset of metastasis, and the sites of metastatic disease were also recorded.
Sample collection and TILs assessment
Archival tumor samples were obtained for each patient before the initiation of first-line treatment. TILs, ER and PR status, and HER2 status were assessed on metastatic tissue samples when available, and on primary tumor samples otherwise. ER, PR and HER2 were based on the standardized ASCO/CAP guidelines35. ER and PR positivity were defined with a 1% cut-off at immunohistochemistry (IHC)34. HER2 positivity is defined either by protein overexpression as determined by immunohistochemical score (IHC) 3+ or equivocal protein expression (IHC 2+), with evidence of HER2 gene amplification (defined here as IHC 2+/Amplified)36,37. TILs were locally evaluated on H&E-stained slides by an experienced pathologist of each institute, following the International TILs Working Group criteria8. TILs were quantified as a percentage of the stromal area occupied by lymphocytic infiltrates. Indeed, TILs were analyzed as continuous variables, and their distribution at the 25th, 50th, and 75th percentiles.
Statistical analysis
Statistical analysis was conducted using R software environment for statistical computing and graphics (version 4.2.3, R Foundation, Vienna, Austria). All analyses were performed considering all cohort (n = 110) and the cohort with TILs evaluated only in the metastatic site (n = 57). Continuous variables were described using median and IQR, and categorical variables using frequencies and percentages. Shapiro–Wilk test was applied to TIL’s variable to check for distribution normality. Mann–Whitney test or Kruskall–Wallis test was used to analyze the correlations between clinicopathological factors and continuous TILs variable. A paired Wilcoxon test was applied to compare TILs percentage evaluated in both primary and metastatic sites (n = 13). PFS was defined as the time from first-line treatment start to the evidence of progressive disease or death from any cause (whichever occurred first) while OS was defined as the time from first-line treatment start to death from any cause. Data were censored if the disease had not progressed by the last evaluation or if patients were still alive at the last follow-up. The cut-off values were defined as the 25° percentile, median, and 75° percentiles of TILs distribution. The survival curves were generated by Kaplan–Meier method and evaluated by log-rank test. Univariate and multivariate Cox’s proportional hazards models were used to evaluate the association of TILs levels with PFS and OS, adjusted for potential confounders such as age, HR status, and presence of visceral disease. All tests were two-sided and, overall, a threshold of 0.05 for the p-value was considered.
Data availability
The datasets generated and/or analyzed during the current study are not publicly available due to privacy and confidentiality concerns, as they contain sensitive patient information. However, the data can be made available from the corresponding author upon reasonable request, in compliance with relevant data protection regulations.
Code availability
Statistical analysis was conducted using R software environment for statistical computing and graphics (version 4.2.3, R Foundation, Vienna, Austria). No custom code or software was used in this study.
Abbreviations
- BC:
-
breast cancer
- BMs:
-
brain metastases
- ER:
-
estrogen receptor
- ER+:
-
estrogen receptor-positive
- H&E:
-
hematoxylin and eosin
- HER2+:
-
HER2-positive
- HR:
-
hormone receptor
- HR+/−:
-
hormone receptor-positive/negative
- ICIs:
-
immune checkpoint inhibitors
- IHC:
-
immunohistochemistry
- IQR:
-
interquartile range
- mBC:
-
metastatic breast cancer
- OS:
-
overall survival
- ORR:
-
objective response rate
- P:
-
p-value
- PD-L1:
-
Programmed Death-Ligand 1
- PFS:
-
progression-free survival
- PR:
-
progesterone receptor
- PR+:
-
progesterone receptor -positive
- TILs:
-
tumor-infiltrating lymphocytes
References
Łukasiewicz, S. et al. Breast Cancer—Epidemiology, Risk Factors, Classification, Prognostic Markers, and Current Treatment Strategies—An Updated Review. Cancers 13, 4287 (2021).
Slamon, D. J. et al. Human Breast Cancer: Correlation of Relapse and Survival with Amplification of the HER-2/ neu Oncogene. Science 235, 177–182 (1987).
Slamon, D. J. et al. Use of Chemotherapy plus a Monoclonal Antibody against HER2 for Metastatic Breast Cancer That Overexpresses HER2. N. Engl. J. Med. 344, 783–792 (2001).
Swain, S. M. et al. Pertuzumab, Trastuzumab, and Docetaxel in HER2-Positive Metastatic Breast Cancer. N. Engl. J. Med. 372, 724–734 (2015).
Cortés, J. et al. Trastuzumab Deruxtecan versus Trastuzumab Emtansine for Breast Cancer. N. Engl. J. Med. 386, 1143–1154 (2022).
Giordano, S. H. et al. Systemic Therapy for Advanced Human Epidermal Growth Factor Receptor 2–Positive Breast Cancer: ASCO Guideline Update. J. Clin. Oncol. 40, 2612–2635 (2022).
Valenza, C. et al. Tumor Infiltrating Lymphocytes across Breast Cancer Subtypes: Current Issues for Biomarker Assessment. Cancers 15, 767 (2023).
Salgado, R. et al. The evaluation of tumor-infiltrating lymphocytes (TILs) in breast cancer: recommendations by an International TILs Working Group 2014. Ann. Oncol. 26, 259–271 (2015).
Loi, S. et al. Tumor infiltrating lymphocytes are prognostic in triple negative breast cancer and predictive for trastuzumab benefit in early breast cancer: results from the FinHER trial. Ann. Oncol. 25, 1544–1550 (2014).
Salgado, R. et al. Tumor-Infiltrating Lymphocytes and Associations With Pathological Complete Response and Event-Free Survival in HER2-Positive Early-Stage Breast Cancer Treated With Lapatinib and Trastuzumab. JAMA Oncol. 1, 448 (2015).
Hou, Y. et al. PD-L1 expression and CD8-positive T cells are associated with favorable survival in HER2-positive invasive breast cancer. Breast J. 24, 911–919 (2018).
Kuemmel, S. et al. Abstract PD10-11: Keyriched-1- A prospective, multicenter, open label, neoadjuvant phase ii single arm study with pembrolizumab in combination with dual anti-HER2 blockade with trastuzumab and pertuzumab in early breast cancer patients with molecular HER2-enriched intrinsic subtype. Cancer Res. 82, PD10-11-PD10-11 (2022).
Ochi, T. et al. Predictive and prognostic value of stromal tumour-infiltrating lymphocytes before and after neoadjuvant therapy in triple negative and HER2-positive breast cancer. Eur. J. Cancer 118, 41–48 (2019).
Luen, S. J. et al. Tumour-infiltrating lymphocytes in advanced HER2-positive breast cancer treated with pertuzumab or placebo in addition to trastuzumab and docetaxel: a retrospective analysis of the CLEOPATRA study. Lancet Oncol. 18, 52–62 (2017).
Loi, S. et al. Pembrolizumab plus trastuzumab in trastuzumab-resistant, advanced, HER2-positive breast cancer (PANACEA): a single-arm, multicentre, phase 1b-2 trial. Lancet Oncol. 20, 371–382 (2019).
Dirix, L. Y. et al. Avelumab, an anti-PD-L1 antibody, in patients with locally advanced or metastatic breast cancer: a phase 1b JAVELIN Solid Tumor study. Breast Cancer Res. Treat. 167, 671–686 (2018).
Emens, L. A. et al. Trastuzumab emtansine plus atezolizumab versus trastuzumab emtansine plus placebo in previously treated, HER2-positive advanced breast cancer (KATE2): a phase 2, multicentre, randomised, double-blind trial. Lancet Oncol. 21, 1283–1295 (2020).
Sobottka, B., Pestalozzi, B., Fink, D., Moch, H. & Varga, Z. Similar lymphocytic infiltration pattern in primary breast cancer and their corresponding distant metastases. Oncoimmunology 5, e1153208 (2016).
Sun, X. et al. Prognostic value and distribution pattern of tumor infiltrating lymphocytes and their subsets in distant metastases of advanced breast cancer. Clin. Breast Cancer 24, e167–e176 (2024).
Cimino-Mathews, A., Ye, X., Meeker, A., Argani, P. & Emens, L. A. Metastatic triple-negative breast cancers at first relapse have fewer tumor-infiltrating lymphocytes than their matched primary breast tumors: a pilot study. Hum. Pathol. 44, 2055–2063 (2013).
Denkert, C. et al. Tumour-infiltrating lymphocytes and prognosis in different subtypes of breast cancer: a pooled analysis of 3771 patients treated with neoadjuvant therapy. Lancet Oncol. 19, 40–50 (2018).
Dieci, M. V. et al. Association of tumor-infiltrating lymphocytes with distant disease-free survival in the ShortHER randomized adjuvant trial for patients with early HER2+ breast cancer. Ann. Oncol. 30, 418–423 (2019).
Griguolo, G., Pascual, T., Dieci, M. V., Guarneri, V. & Prat, A. Interaction of host immunity with HER2-targeted treatment and tumor heterogeneity in HER2-positive breast cancer. J. Immunother. Cancer 7, 90 (2019).
Bianchini, G. & Gianni, L. The immune system and response to HER2-targeted treatment in breast cancer. Lancet Oncol. 15, e58–e68 (2014).
Liu, S. et al. Role of Cytotoxic Tumor-Infiltrating Lymphocytes in Predicting Outcomes in Metastatic HER2-Positive Breast Cancer. JAMA Oncol. 3, e172085 (2017).
Loi, S. et al. Abstract GS2-06: Phase Ib/II study evaluating safety and efficacy of pembrolizumab and trastuzumab in patients with trastuzumab-resistant HER2-positive metastatic breast cancer: Results from the PANACEA (IBCSG 45-13/BIG 4-13/KEYNOTE-014) study. Cancer Res. 78, GS2-06–GS2-06 (2018).
Stover, D. G. et al. Association between tumor-infiltrating lymphocytes and survival in patients with metastatic breast cancer receiving first-line chemotherapy: analysis of CALGB 40502. NPJ Breast Cancer 10, 75 (2024).
Ogiya, R. et al. Comparison of tumor-infiltrating lymphocytes between primary and metastatic tumors in breast cancer patients. Cancer Sci. 107, 1730–1735 (2016).
Baine, M. K. et al. Characterization of tumor infiltrating lymphocytes in paired primary and metastatic renal cell carcinoma specimens. Oncotarget 6, 24990–25002 (2015).
Stover, D. G. et al. Association of tumor infiltrating lymphocyte quantity with survival in patients (pts) with metastatic breast cancer (MBC) receiving microtubule-targeting agents: Post hoc analysis CALGB 40502 (Alliance). J. Clin. Oncol. 41, 1010–1010 (2023).
Li, Y. et al. Abstract PD6-01: Prevalence of PDL1 and tumor infiltrating lymphocytes (TILs) in primary and metastatic TNBC. Cancer Res. 78, PD6-01–PD6-01 (2018).
Loi, S. et al. Relationship between tumor infiltrating lymphocyte (TIL) levels and response to pembrolizumab (pembro) in metastatic triple-negative breast cancer (mTNBC): Results from KEYNOTE-086. Ann. Oncol. 28, v608 (2017).
Criscitiello, C. et al. Tumor-infiltrating lymphocytes (TILs) in ER+/HER2− breast cancer. Breast Cancer Res. Treat. 183, 347–354 (2020).
Stanton, S. E., Adams, S. & Disis, M. L. Variation in the Incidence and Magnitude of Tumor-Infiltrating Lymphocytes in Breast Cancer Subtypes. JAMA Oncol. 2, 1354 (2016).
Allison, K. H. et al. Estrogen and Progesterone Receptor Testing in Breast Cancer: ASCO/CAP Guideline Update. J. Clin. Oncol. 38, 1346–1366 (2020).
Wolff, A. C. et al. Human Epidermal Growth Factor Receptor 2 Testing in Breast Cancer: American Society of Clinical Oncology/College of American Pathologists Clinical Practice Guideline Focused Update. Arch. Pathol. Lab. Med. 142, 1364–1382 (2018).
Loibl, S. & Gianni, L. HER2-positive breast cancer. Lancet 389, 2415–2429 (2017).
Acknowledgements
This study received no funding. The authors wish to thank all the patients who participate in this study and their families.
Author information
Authors and Affiliations
Contributions
B.T.S. contributed to the conceptualization, data collection, and writing of the original draft. C.C. contributed to the conceptualization, methodology development, validation, and writing of the original draft. G.C. contributed to the conceptualization, methodology development, and project administration. F.G. conducted formal statistical analyses and was responsible for generating the figures and tables. P.P.M.B.G. contributed to data collection. R.S. contributed to data collection. C.P. was responsible for retrieving the tissue samples and evaluating and measuring the tumor infiltrating lymphocytes. B.C. was responsible for retrieving the tissue samples and evaluating and measuring the tumor-infiltrating lymphocytes. N.F. contributed to methodology development. All authors contributed to reviewing and editing the manuscript and approved the final version.
Corresponding author
Ethics declarations
Competing interests
Authors have no conflicts of interest related to the current analyses. B.T.S. received honoraria as speaker from Lilly outside the submitted work and declares no non-financial competing interests. A.M. reported personal fees from Menarini/ Stemline, Roche, Lilly and AstraZeneca outside the submitted work and is supported by the ESMO José Baselga Fellowship for Clinician Scientists sponsored by AstraZeneca, outside the submitted work and declares no non-financial competing interests. A.E. received honoraria as speaker from Novartis and AstraZeneca outside the submitted work and and declares no non-financial competing interests. S.S. received honoraria as speaker from: Novartis, Pfizer, Roche, Lilly, BMS, MSD, outside the submitted work and and declares no non-financial competing interests. A.B. has/had a consultant/advisory role for: Roche-Genentech, MSD, Pfizer, BMS, Amgen, Novartis, Pierre Fabre, Gilead, Eli-Lilly, and Seagen, outside the submitted work and declares no non-financial competing interests. E.M. had consulting or advisory role for: Exact Sciences, MSD Oncology, Daiichi Sankyo/Astra Zeneca, Pfizer, Seagen, Ipsen, and received travel accommodation, registration for international congresses from: Roche, Pfizer, Lilly, Novartis, Gilead Sciences, AstraZeneca, Pierre Fabre, outside the submitted work and declares no non-financial competing interests. N.F. has received honoraria for consulting, advisory roles, speaker bureau, travel, and/or research grants from Merck Sharp & Dohme (MSD), Merck, Novartis, AstraZeneca, Roche, Menarini, Daiichi Sankyo, GlaxoSmithKline (GSK), Gilead, Adicet Bio, Sermonix, Reply, Veracyte Inc., Leica Biosystems, and Lilly, outside the submitted work and declares no non-financial competing interests. G.C. reports financial interests with AstraZeneca, Daiichi Sankyo, Exact Sciences, Lilly, Merck, Novartis, Pfizer, Roche, Veracyte, Ellipsis, Astellas, Blueprint Medicine, BMS, Merck, Novartis, Menarini, Relay Therapeutics, Sanofi; and non-financial interests with the Italian National Health Council as Advisor for Ministry of Health, ESMO as Clinical Practice Guidelines Chair, Europa Donna as Member of the Scientific Council, EUSOMA as member of the Advisory Council, Fondazione Beretta. All the competing interests were outside the submitted work outside the submitted work and he declares no non-financial competing interests. C.C. had consultancy/advisory role/speaker bureau for: Pfizer, Roche, MSD, Novartis, Lilly, Seagen, Gilead Daiichi-Sankyo, outside the submitted work and declares no non-financial competing interestsoutside. All other authors declare no financial or non-financial competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
41523_2025_760_MOESM1_ESM.pdf
Supplementary Table Cox Prognostic Models for TILs as continuous variable (10% of increment) for all cohort and for the cohort of patients whose TILs were evaluated at the metastatic site.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Taurelli Salimbeni, B., Giudici, F., Pescia, C. et al. Prognostic impact of tumor-infiltrating lymphocytes in HER2+ metastatic breast cancer receiving first-line treatment. npj Breast Cancer 11, 41 (2025). https://doi.org/10.1038/s41523-025-00760-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41523-025-00760-9