Abstract
In the randomized, phase 3 KEYNOTE-119 study, overall survival (OS) was not significantly improved with pembrolizumab 200 mg Q3W versus investigator’s choice of chemotherapy in participants with previously treated metastatic TNBC. In this exploratory analysis, we evaluated associations of tumor-infiltrating lymphocytes (TILs), T-cell‒inflamed gene expression profile (TcellinfGEP), BRCA1/BRCA2 mutation (BRCAm) status, homologous recombination deficiency (HRD) status, and tumor mutational burden (TMB) with clinical outcomes. TIL level was associated with improved objective response rate (ORR), progression-free survival (PFS), and OS with pembrolizumab but not with chemotherapy or after adjusting for TcellinfGEP. Associations were also identified between TcellinfGEP and improved ORR, PFS, and OS with pembrolizumab. Participants with TMB ≥ 10 mut/Mb showed a trend toward increased benefit with pembrolizumab versus chemotherapy. No association was seen between BRCAm/HRD status and treatment response. These findings suggest a positive association between TILs, TcellinfGEP, and TMB with clinical outcomes in patients with metastatic TNBC receiving pembrolizumab. ClinicalTrials.gov Identifier: NCT02555657 (date of registration: September 18, 2015).
Similar content being viewed by others
Introduction
The anti–programmed cell death protein 1 (PD-1) monoclonal antibody pembrolizumab has demonstrated activity as monotherapy in certain tumor types, including in patients with advanced or metastatic disease1. The phase 3, randomized, open-label KEYNOTE-119 study evaluated pembrolizumab monotherapy versus physician’s choice of single-agent chemotherapy treatment as second- or third-line treatment for participants with metastatic triple-negative breast cancer (TNBC)2. Pembrolizumab monotherapy did not significantly improve the primary endpoint of overall survival (OS) compared with chemotherapy. However, among participants with higher programmed cell death ligand 1 (PD-L1) expression, the hazard ratio (HR) for OS favored the pembrolizumab group. Potentially, biomarkers beyond PD-L1 may be employed to identify additional patients likely to benefit from treatment with pembrolizumab monotherapy.
The presence of tumor-infiltrating lymphocytes (TILs) has been shown to be of prognostic significance in TNBC, with greater lymphocytic infiltration associated with better clinical outcomes3,4. In the phase 2 KEYNOTE-086 study (NCT02447003), TIL levels were a surrogate marker of preexisting antitumor immunity and were independent predictors of objective response during monotherapy with pembrolizumab5. Additionally, both T-cell‒inflamed gene expression profile (TcellinfGEP) and BRCA1/BRCA2 mutation (BRCAm) have been associated with improved treatment response in patients with TNBC6,7. For example, in the phase 2 KEYNOTE-086 study of pembrolizumab monotherapy for treatment of metastatic TNBC, TcellinfGEP was associated with objective response rate (ORR) and OS6. In the phase 2 TBCRC009 study, participants with BRCAm metastatic TNBC had higher response rates to chemotherapy than those without mutations7. Tumor mutational burden (TMB), defined as total somatic mutations per coding area of an exon, has also been associated with improved response to treatment with immune checkpoint inhibitors, including anti–PD-1 agents, that enhance antitumor T-cell activity8. In a retrospective analysis, higher TMB was associated with increased response rate during treatment with anti–PD-1 or anti–PD-L1 therapy across a range of tumor types9. In the phase 2 KEYNOTE-158 study, participants with TMB ≥ 10 mutations/megabase (mut/Mb) had a higher ORR than participants with TMB < 10 mut/Mb (29% vs 6%), irrespective of tumor type8.
Additional evidence is needed to understand the ability of these biomarkers to predict response and survival outcomes with antitumor treatments such as pembrolizumab. The current analysis of data from KEYNOTE-119 evaluated associations of TILs, TcellinfGEP, BRCAm/homologous recombination repair deficiency (HRD) status, and TMB as biomarkers with clinical outcomes among participants enrolled in the KEYNOTE-119 study.
Results
Participants
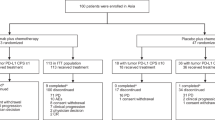
As previously reported2, between November 25, 2015, and April 11, 2017, 622 participants were enrolled at 150 medical centers in 31 countries and randomized to receive pembrolizumab (n = 312) or chemotherapy (n = 310). Baseline demographics for both treatment groups have been previously described2. In brief, among the 622 enrolled participants, 292 (46.9%) had an Eastern Cooperative Oncology Group (ECOG) performance status of 1,405 (65.1%) had PD-L1 combined positive score (CPS) ≥ 1, 194 (31.1%) had PD-L1 CPS ≥ 10, and 109 (17.5%) had PD-L1 CPS ≥ 20. The final data cutoff date was April 11, 2019. Among 601 participants in the all-patients-as-treated population (pembrolizumab, n = 309; chemotherapy, n = 292), TILs were evaluable in 551 treated participants (pembrolizumab, n = 284; chemotherapy, n = 267), TcellinfGEP data were available for 333 treated participants (pembrolizumab, n = 177; chemotherapy, n = 156), BRCAm/HRD status was available for 218 treated participants (pembrolizumab, n = 115; chemotherapy, n = 103), and TMB data were available for 255 participants (pembrolizumab, n = 133; chemotherapy, n = 122).
Association of TILs with clinical outcomes
Across all evaluable participants, the median TIL level was 5%. ORR was 9.5% (95% CI, 6.4‒13.5%) in the pembrolizumab group (n = 284) and 10.9% (95% CI, 7.4‒15.2%) in the chemotherapy group (n = 267; Fig. 1a). Median TIL levels were higher among responders versus nonresponders in the pembrolizumab group, but not in the chemotherapy group.
a TIL levels in responders and nonresponders. b Overall survival by median TIL cutpoints of < 5% and ≥ 5%. TILs are plotted on a square-root scale. The median TIL level was 20% among responders in the pembrolizumab group and 5% among nonresponders in the pembrolizumab group. Median TIL level was 5% among responders and nonresponders in the chemotherapy group. In these boxplots, the whiskers extend no further than 1.5 times the interquartile range; dots represent values that fall outside 1.5 times the interquartile range. Responses evaluated by blinded independent central review per RECIST version 1.1. HR hazard ratio, RECIST Response Evaluation Criteria in Solid Tumors, TIL tumor-infiltrating lymphocyte.
In the pembrolizumab group, statistically significant associations were identified between TILs and best overall response (BOR; P = 0.0004), PFS (P = 0.0002), and OS (P = 0.0003). Statistical significance was not observed in the chemotherapy group for any outcome (P > 0.05 for all; Table 1).
The median TIL level of 5% was used to stratify participants into 2 groups. Among participants with TILs ≥ 5%, the HR for OS favored the pembrolizumab group (0.75 [95% CI, 0.59‒0.95]), whereas among participants with TILs < 5%, the HR for OS favored the chemotherapy group (1.46 [95% CI, 1.11‒1.92]; Fig. 1b).
Additionally, there was a moderate correlation between TIL level and PD-L1 CPS and between TIL level and TcellinfGEP, with Spearman correlation coefficients of 0.46 and 0.56, respectively (Supplementary Fig. 1). Despite being correlated with one another, TIL level and PD-L1 CPS showed independent predictive ability for clinical outcomes among participants receiving pembrolizumab monotherapy in a multivariate model (TIL: BOR, P = 0.011; PFS, P = 0.003; OS, P = 0.004; PD-L1 CPS: BOR, P = 0.040; PFS, P = 0.038; OS, P = 0.090; Supplementary Table 1).
Association of TcellinfGEP with clinical outcomes
In the pembrolizumab group, statistically significant associations were identified between TcellinfGEP score and BOR (P < 0.001), PFS (P < 0.0001), and OS (P < 0.0001). Statistical significance was not observed in the chemotherapy group for any outcome (P > 0.05 for all; Table 1).
Among participants with a TcellinfGEPlow (< 1st tertile) score, the ORR was 0.0% (95% CI, 0.0‒6.8%) in the pembrolizumab group (n = 52) and 8.5% (95% CI, 2.8‒18.7%) in the chemotherapy group (n = 59). For participants with a TcellinfGEPnon-low (≥ 1st tertile) score, the ORR was 15.2% (95% CI, 9.4‒22.7%) in the pembrolizumab group (n = 125) and 13.4% (95% CI, 7.3‒21.8%) in the chemotherapy group (n = 97; Table 2).
In both treatment groups, median TcellinfGEP scores were higher for responders than for nonresponders, although the range of median TcellinfGEP scores was narrower for the pembrolizumab group than the chemotherapy group (Fig. 2a). Area under the receiver operating characteristic curve (AUROC) analyses indicated a positive association between TcellinfGEP score and ORR for the pembrolizumab group (area under the curve, 0.78 [95% CI, 0.69‒0.87]) but not for the chemotherapy group (area under the curve, 0.60 [95% CI, 0.44‒0.76]; Fig. 2b).
a TcellinfGEP scores in responders and nonresponders. b AUROC analysis of the association between TcellinfGEP score and objective response rate. c OS by TcellinfGEP score with a 1st tertile cutpoint (< 1st tertile vs ≥ 1st tertile). In these boxplots, the whiskers extend no further than 1.5 times the interquartile range; dots represent values that fall outside 1.5 times the interquartile range. aResponders include participants who had a complete or partial response per RECIST version 1.1. AUC area under the curve, AUROC area under the receiver operating characteristic curve, HR hazard ratio, RECIST Response Evaluation Criteria in Solid Tumors, TcellinfGEP T-cell‒inflamed gene expression profile, TPC treatment of physician’s choice chemotherapy.
In the subgroup of participants with a TcellinfGEPlow score, HRs for PFS and OS favored the chemotherapy group. The HR for PFS was 3.63 (95% CI, 2.31‒5.70) and the HR for OS was 1.72 (95% CI, 1.15‒2.55; Table 2). In the subgroup of participants with TcellinfGEPnon-low, the HR for PFS was 1.40 (95% CI, 1.02‒1.93) and the HR for OS was 0.77 (95% CI, 0.58‒1.04; Fig. 2c).
Additional analyses were done to model associations jointly of TcellinfGEP and TILs with clinical outcomes. In the pembrolizumab group, 165 participants had both TcellinfGEP and TIL data available for analysis; in the chemotherapy group, 146 participants had both TcellinfGEP and TIL data available. When TcellinfGEP was modeled jointly with TILs (square-root transformed), statistically significant associations were identified for the pembrolizumab group between TcellinfGEP score and BOR (P = 0.006), PFS (P < 0.001), and OS (P < 0.001), but no statistically significant associations were identified for the chemotherapy group (P > 0.05 for all). However, when TILs were modeled jointly with TcellinfGEP score, no association was identified between TILs and BOR, PFS, or OS for either treatment group (P > 0.15 for all; Table 3).
There was a moderate correlation between TcellinfGEP and PD-L1 CPS with a Spearman correlation coefficient of 0.6 (Supplementary Fig. 1).
Association of BRCAm/HRD status with clinical outcomes
Among 218 participants with evaluable data, 78 of 115 (67.8%) in the pembrolizumab group and 64 of 103 (62.1%) in the chemotherapy group were assessed as BRCAm or HRD-positive (genomic loss of heterozygosity [gLOH] ≥ 16). Forty-five participants had BRCAm (pembrolizumab, n = 26; chemotherapy, n = 19) and 128 had HRD-positive (gLOH ≥ 16; pembrolizumab, n = 69; chemotherapy, n = 59) status. No statistically significant association was observed in either treatment arm among the 3 BRCAm/HRD status categories and BOR, PFS, or OS (P > 0.05 for all).
Association of TMB with clinical outcomes
Overall, 26 of 255 participants (10.2%) had TMB ≥ 10 mut/Mb assessed using the FoundationOne®CDx comprehensive genomic profiling assay (Foundation Medicine, Inc., Cambridge, MA, USA). Among all participants, though small in numbers, the association between higher TMB and better clinical outcomes was statistically significant for PFS (P = 0.015) and OS (P = 0.025) but not BOR (P = 0.154) with pembrolizumab. Median TMB was similar among responders versus nonresponders in the pembrolizumab group (albeit with a higher interquartile range for responders), whereas the median TMB was slightly lower among responders versus nonresponders in the chemotherapy group (Fig. 3a). The AUROC for the association between TMB and ORR was 0.58 (95% CI, 0.43‒0.73) for pembrolizumab and 0.43 (95% CI, 0.27‒0.60) for chemotherapy (Fig. 3b).
a TMB in responders and nonresponders. b AUROC analysis of the association between TMB and objective response rate. c Overall survival in participants with TMB ≥ 10 mut/Mb and participants with TMB < 10 mut/Mb. Median TMB was 3.78 mut/Mb among both responders and nonresponders in the pembrolizumab group; median TMB was 2.52 mut/Mb among responders in the chemotherapy group and 3.78 mut/Mb among responders in the chemotherapy group. In these boxplots, the whiskers extend no further than 1.5 times the interquartile range; dots represent values that fall outside 1.5 times the interquartile range. aResponders include participants who had a complete or partial response per RECIST version 1.1. AUROC area under the receiver operating characteristic curve, mut/Mb mutations per megabase, RECIST Response Evaluation Criteria in Solid Tumors, TMB tumor mutational burden.
There was no association between TMB and ORR, PFS, or OS with pembrolizumab or with chemotherapy (P > 0.05 for all). OS was longer for participants with TMB ≥ 10 mut/Mb treated with pembrolizumab than for all other groups (Fig. 3c).
Discussion
In these exploratory analyses from the phase 3 KEYNOTE-119 study of pembrolizumab monotherapy versus chemotherapy in participants with metastatic TNBC, we evaluated associations between clinical outcomes and a range of potential biomarkers of response to treatment. We identified important associations between these biomarkers and ORR, PFS, and OS among participants receiving pembrolizumab monotherapy; these results may inform the design of future studies evaluating pembrolizumab treatment in patients with advanced or metastatic TNBC.
In the exploratory analysis of TIL expression and clinical outcomes, TIL ≥ 5% was significantly associated with better ORR, PFS, and OS with pembrolizumab monotherapy but not with single-agent chemotherapy. As with CPS, efficacy estimates at the median TIL cutpoint (≥ 5%) suggest that a subset of patients with metastatic TNBC necessitating later-line therapy can derive prolonged survival benefit from pembrolizumab over chemotherapy. Although TIL expression and CPS were moderately correlated, they were independently predictive of clinical outcomes. Understanding which patients with later-line metastatic TNBC would benefit from pembrolizumab would need to be tested in a prospective study; however, TIL expression represents a pragmatic and globally accessible technique that seems to evaluate patients for a pre-existing immune response.
Findings from exploratory analyses also suggest a positive association between TcellinfGEP score and objective response, PFS, and OS for patients with metastatic TNBC who were treated with pembrolizumab, but not in those treated with chemotherapy. A more favorable treatment effect was observed for PFS and OS in the TcellinfGEP-enriched population. Our results are consistent with those from other studies that have evaluated associations between TcellinfGEP score and clinical outcomes among patients receiving pembrolizumab. In particular, in the phase 2 KEYNOTE-086 study, which evaluated pembrolizumab monotherapy in participants with metastatic TNBC who received 1 or 2 prior lines of therapy, statistically significant associations between a higher TcellinfGEP score and improved ORR and OS were identified6. Statistically significant associations between TcellinfGEP score and improved clinical outcomes with pembrolizumab treatment have also been identified for participants with advanced urothelial carcinoma10, head and neck squamous cell carcinoma11, advanced gastric cancer (in KEYNOTE-061)12, and non‒small-cell lung cancer13. The current results, taken together with prior findings in other tumor types, support the association of TcellinfGEP score with response to pembrolizumab treatment across multiple tumor types.
The 18 genes that comprise TcellinfGEP were identified based on their association with response among 1188 participants receiving pembrolizumab in clinical trials14. Results from our study support the hypothesis that increased expression of genes associated with T-cell activation and recruitment within the tumor microenvironment may play a key role in modulating response to immune checkpoint blockade in metastatic TNBC. However, at present, the mechanisms mediating associations between tumor inflammatory pathways assessed by TcellinfGEP score and outcomes in patients with metastatic breast cancer are not fully understood and require further elucidation. Notably, we observed that the associations between TcellinfGEP score and efficacy outcomes were independent of TILs, as determined by joint modeling, which have previously been shown to be associated with response to pembrolizumab (but not chemotherapy), as demonstrated in participants enrolled in the KEYNOTE-119 trial6. Importantly, after adjusting for TcellinfGEP score, the association between TILs and clinical response to pembrolizumab was no longer statistically significant. Taken together, these findings suggest a potential quantitative and biologic relationship between TILs and TcellinfGEP, where TILs do not provide additional predictive value beyond that provided by TcellinfGEP. Further studies will be needed to elucidate the nature of such a relationship.
No association was found between BRCAm/HRD status and clinical outcomes in either treatment group. To our knowledge, 2 other studies have evaluated the association between BRCAm/HRD status and clinical outcomes in advanced solid tumors treated with pembrolizumab. In the phase 2 TOPACIO study of niraparib plus pembrolizumab in women with advanced or metastatic TNBC, the ORR was 47% for participants with BRCAm tumors and 11% for those without confirmed tumor BRCAm15. Median PFS was 8.3 and 2.1 months, respectively. Similarly, initial results from the phase 2 KEYLYNK-007 study of olaparib plus pembrolizumab in advanced solid tumors showed an ORR of 29% for participants with BRCAm tumors and 21% for participants with HRD-positive tumors. Confirmed responses were reported for participants with breast, cervical, endometrial, prostate, duodenal, ovarian, peritoneal, and non‒small-cell lung cancers. The duration of response was not reached for both participant subgroups; the median PFS was not reached in the BRCAm subgroup and 4.1 months in the HRD-positive subgroup16. Yet, since pembrolizumab was combined with a PARP inhibitor in both studies, no clear conclusion could be drawn.
In the exploratory analysis of TMB and clinical outcomes, there was a trend toward a positive association between TMB and clinical response with pembrolizumab but not with chemotherapy. Although the association between TMB and ORR was not statistically significant, those with PFS and OS were. Notably, OS was longer for participants with TMB ≥ 10 mut/Mb with a clear and consistent separation of Kaplan-Meier curves for OS, and a similar trend was also observed in participants with TMB < 10 mut/Mb, albeit less pronounced. However, it must be noted that there were relatively few participants with TMB ≥ 10 mut/Mb (10.2%), which may have limited the ability to assess the predictive value of TMB in this setting. Our findings are broadly consistent with those from the KEYNOTE-158 study, in which TMB ≥ 10 mut/Mb was associated with response to pembrolizumab among participants with advanced solid tumors (none of whom had breast cancer)8.
Other studies have evaluated biomarkers for immunotherapy in patients with TNBC and provide important context for our findings. The phase 3 IMpassion130 study showed a clinical benefit with atezolizumab (an anti–PD-L1 antibody) plus chemotherapy versus chemotherapy alone in patients with locally advanced or metastatic TNBC with PD-L1 expression on tumor-infiltrating immune cells (PD-L1 IC+) but not in the intent-to-treat population (ie, irrespective of PD-L1 IC status)17. In exploratory analyses from IMpassion13018, tumor CD8 positivity and stromal TIL positivity were associated with improved outcomes. However, these biomarkers were highly correlated with PD-L1 IC+ and improvements in outcomes were confined to patients who were also PD-L1 IC+, suggesting these biomarkers did not add predictive value beyond PD-L1 status. In the ALICE study (a phase 2b trial evaluating the addition of atezolizumab to anthracycline-based chemotherapy in patients with metastatic TNBC), there was no evidence of an association between PD-L1 status and PFS or between TMB and PFS among patients receiving atezolizumab plus chemotherapy; however, in exploratory analyses, there was evidence of greater PFS benefit among patients with an above-median tumor inflammation signature19. In a combined analysis of circulating tumor cells (CTCs) from patients in the ALICE study and the ICON study (a phase 2b trial evaluating immunogenic chemotherapy combined with ipilimumab and nivolumab in patients with metastatic hormone receptor positive HER2− breast cancer), presence of CTCs was associated with poor prognosis: 6 out of 17 CTC-positive patients showed PD-L1 expression, which was associated with significantly shorter OS20. Results from the single-arm TONIC study (a phase 2 trial evaluating efficacy of nivolumab after short-term induction with low-dose chemotherapy in patients with metastatic TNBC) showed that patients who exhibited clinical benefit had higher levels of stromal TILs and higher levels of CD8 and PD-L1 expression on immune cells21. Finally, results from the SAFIR02-BREAST IMMUNO study showed that, among patients with metastatic TNBC durvalumab versus maintenance therapy, there was no association between OS and tumor infiltration by lymphocytes, although there was an association between OS and CD274 amplification/gain and efficacy22.
A range of novel biomarkers are currently being evaluated for their potential to predict response to immunotherapy in patients with breast cancer. Emerging evidence has suggested there may be associations between efficacy outcomes and potential biomarkers, including gene-signature scores for T helper 1 cells, B cells, and neutrophils21, and gut microbiota diversity23.
A key strength of the current findings is that they are based on data from a randomized, phase 3 trial. The presence of a comparator group allowed us to demonstrate that the association between TILs and TcellinfGEP scores and outcomes was only observed in participants receiving pembrolizumab. An additional strength of the analysis is the large size of the biomarker-evaluable populations; among the 601 participants enrolled and treated in KEYNOTE-119, approximately a little more than half in both treatment arms had TcellinfGEP data, and a little more than one-third of participants had BRCAm/HRD data available for analysis. However, these descriptive results should be interpreted with caution due to the retrospective, exploratory nature of the analysis and the small numbers of participants in several of the subgroups. In addition, the tissue samples reflect a mix of newly obtained (~56%) and archival (~39%) samples collected at different times throughout a participant’s treatment history, which may have affected biomarker analysis24.
In summary, TcellinfGEP score, TIL quantity, and TMB status may be predictive of treatment response to pembrolizumab among patients with metastatic TNBC. Further investigation will be needed to ascertain how these biomarkers may be used along with PD-L1 immunohistochemistry to ensure all patients who will benefit from pembrolizumab can receive it.
Methods
Eligibility criteria
Full eligibility criteria and study design have been published previously2. Briefly, participants with centrally confirmed metastatic TNBC were eligible if they had an ECOG performance status of 0 or 1; had received 1 or 2 prior systemic treatments for metastatic breast cancer; had received prior treatment with an anthracycline or taxane in the neoadjuvant, adjuvant, or metastatic setting; had documented disease progression on the most recent therapy; and had measurable disease per Response Evaluation Criteria in Solid Tumors (RECIST) version 1.1. Participants were excluded if they had active central nervous system metastases or carcinomatous meningitis, active autoimmune disease requiring systemic treatment in the past 2 years, or history or evidence of noninfectious pneumonitis requiring steroid treatment; had received treatment with an agent directed at PD-1, PD-L1, or another coinhibitory T-cell receptor or with an antineoplastic monoclonal antibody within 4 weeks; or had received chemotherapy, targeted small-molecule therapy, or radiotherapy within 2 weeks. Participants were required to provide a newly obtained tumor tissue sample for central confirmation of TNBC status and PD-L1 expression; archival samples were permitted only with approval from the study sponsor if a new sample could not be obtained.
The study was done in accordance with the principles set forth in the Declaration of Helsinki and with the International Council on Harmonisation Good Clinical Practice guidelines. An independent ethics committee or institutional review board at each site (listed in the Supplementary Materials) approved the protocol before study-related procedures began. All participants provided written informed consent before enrolling. The study was registered with ClinicalTrials.gov (NCT02555657; date of registration: September 18, 2015).
Study treatment
Briefly, participants were randomized 1:1 to receive pembrolizumab or chemotherapy. Randomization was stratified by tumor PD-L1 status (CPS ≥ 1 vs CPS < 1) and by prior neoadjuvant or adjuvant treatment versus de novo metastatic TNBC. Participants randomized to the pembrolizumab group received pembrolizumab 200 mg once every 3 weeks for 35 cycles or until confirmed disease progression, unacceptable toxicity, consent withdrawal, or investigator decision. Participants randomized to the chemotherapy group received the investigator’s choice of capecitabine, eribulin, gemcitabine, or vinorelbine per local guidelines until disease progression, unacceptable toxicity, consent withdrawal, or investigator decision. Participants in the chemotherapy group who had documented disease progression were not permitted to cross over to receive pembrolizumab.
Assessments
The presence of TILs in tumor samples was assessed by light microscopy of hematoxylin and eosin‒stained sections using a predefined method25,26. Tumor RNA profiling was conducted on the RNA-seq platform (Illumina, San Diego, CA). TMB, BRCAm, and HRD status were assessed using the FoundationOne®CDx comprehensive genomic profiling assay (Foundation Medicine, Inc., Cambridge, MA, USA)27,28,29. FoundationOne®CDx is an FDA-approved next-generation sequencing assay that can identify TMB status in tumor samples using a prespecified cutpoint of at least 10 mut/Mb to define TMB-high (≥ 10 mut/Mb) and less than 10 mut/Mb for non–TMB-high (< 10 mut/Mb) tumors8.
BRCAm/HRD status was categorized into 3 groups: BRCAm, BRCA wild-type with gLOH ≥ 16, and BRCA wild-type with gLOH < 16.
Tumor imaging was performed using computed tomography or magnetic resonance imaging at baseline, every 9 weeks for 1 year, and every 12 weeks thereafter until participants had radiologic evidence of disease progression, started a new anticancer treatment, or withdrew consent, or until the end of the study. Tumor response was assessed by a central imaging vendor per RECIST version 1.1.
Statistical analyses
The study’s primary endpoint was OS (defined as time from randomization to death from any cause). ORR and PFS (time from randomization to disease progression or death) were secondary endpoints. Evaluation of the relationships between potential biomarkers and antitumor activity of pembrolizumab was an exploratory endpoint.
Biomarker analyses were performed in the all-patients-as-treated population (ie, those who received ≥ 1 dose of study medication analyzed according to treatment received). This exploratory analysis assessed the associations of TILs, TcellinfGEP, BRCAm/HRD status, and TMB with the clinical outcomes of BOR and PFS per RECIST version 1.1 and with OS. The associations of biomarkers with BOR were evaluated using logistic regression and AUROC analysis; their associations with PFS and OS were evaluated by Cox proportional hazards models. Associations were evaluated within each treatment group (ie, for participants in the pembrolizumab group and participants in the chemotherapy group). Analyses for TcellinfGEP, TMB, and BRCAm/HRD were adjusted for baseline ECOG performance status, and analyses of TILs were adjusted for previous adjuvant or neoadjuvant therapy versus de novo metastatic disease at initial diagnosis.
Relative prognostic and predictive effects of the biomarkers were assessed in subgroups defined as follows: above or below the median TIL score; TcellinfGEPlow (< 1st tertile) versus TcellinfGEPnon-low (≥ 1st tertile); BRCAm/HRD status (BRCAm vs BRCA wild-type and gLOH ≥ 16 vs BRCA wild-type and gLOH < 16); and TMB ≥ 10 mut/Mb versus TMB < 10 mut/Mb. The cutoff for dichotomization of the population by TcellinfGEP (ie, < 1st tertile/≥ 1st tertile) was selected based on prior studies evaluating TcellinfGEP as a biomarker for pembrolizumab30,31.
The 95% CIs for ORRs were estimated using the Clopper and Pearson method32. The 95% CIs for HRs from Cox proportional hazards models were calculated using the log-log method with adjustment for baseline ECOG performance status. No alpha was assigned to these analyses; all P values are descriptive. In multivariate modeling, TcellinfGEP and TILs were jointly modeled with baseline ECOG performance status as a covariate; CPS and TILs were jointly modeled with the stratification variables, previous adjuvant or neoadjuvant therapy versus de novo metastatic disease at initial diagnosis, as covariates. Spearman correlation (ρ) was used to assess the pairwise correlations between TcellinfGEP, PD-L1 CPS, TILs, and TMB.
Data availability
Merck Sharp & Dohme LLC, a subsidiary of Merck & Co., Inc., Rahway, NJ, USA (MSD) is committed to providing qualified scientific researchers access to anonymized data and clinical study reports from the company’s clinical trials for the purpose of conducting legitimate scientific research. MSD is also obligated to protect the rights and privacy of trial participants and, as such, has a procedure in place for evaluating and fulfilling requests for sharing company clinical trial data with qualified external scientific researchers. The MSD data sharing website (available at: https://externaldatasharing-msd.com/) outlines the process and requirements for submitting a data request. Applications will be promptly assessed for completeness and policy compliance. Feasible requests will be reviewed by a committee of MSD subject matter experts to assess the scientific validity of the request and the qualifications of the requestors. In line with data privacy legislation, submitters of approved requests must enter into a standard data-sharing agreement with MSD before data access is granted. Data will be made available for request after product approval in the US and EU or after product development is discontinued. There are circumstances that may prevent MSD from sharing requested data, including country- or region-specific regulations. If the request is declined, it will be communicated to the investigator. Access to genetic or exploratory biomarker data requires a detailed, hypothesis-driven statistical analysis plan that is collaboratively developed by the requestor and MSD subject matter experts; after approval of the statistical analysis plan and execution of a data-sharing agreement, MSD will either perform the proposed analyses and share the results with the requestor or will construct biomarker covariates and add them to a file with clinical data that is uploaded to an analysis portal so that the requestor can perform the proposed analyses.
References
Keytruda (pembrolizumab). Full Prescribing Information, Merck & Co., Inc., Rahway, NJ, USA, 2024.
Winer, E. P. et al. Pembrolizumab versus investigator-choice chemotherapy for metastatic triple-negative breast cancer (KEYNOTE-119): a randomised, open-label, phase 3 trial. Lancet Oncol. 22, 499–511 (2021).
Kashiwagi, S. et al. Use of tumor-infiltrating lymphocytes (TILs) to predict the treatment response to eribulin chemotherapy in breast cancer. PloS one 12, e0170634 (2017).
Loi, S. et al. Tumor-infiltrating lymphocytes and prognosis: a pooled individual patient analysis of early-stage triple-negative breast cancers. J. Clin. Oncol. 37, 559–569 (2019).
Loi, S. et al. Relationship between tumor infiltrating lymphocyte (TIL) levels and response to pembrolizumab (pembro) in metastatic triple-negative breast cancer (mTNBC): results from KEYNOTE-086. Ann. Oncol. 28, LBA13 (2017).
Loi, S. et al. Association between biomarkers and clinical outcomes of pembrolizumab monotherapy in patients with metastatic triple-negative breast cancer: KEYNOTE-086 exploratory analysis. JCO Precis Oncol. 7, e2200317 (2023).
Isakoff, S. J. et al. TBCRC009: a multicenter phase II clinical trial of platinum monotherapy with biomarker assessment in metastatic triple-negative breast cancer. J. Clin. Oncol. 33, 1902–1909 (2015).
Marabelle, A. et al. Association of tumour mutational burden with outcomes in patients with advanced solid tumours treated with pembrolizumab: prospective biomarker analysis of the multicohort, open-label, phase 2 KEYNOTE-158 study. Lancet Oncol. 21, 1353–1365 (2020).
Yarchoan, M., Hopkins, A. & Jaffee, E. M. Tumor mutational burden and response rate to PD-1 inhibition. N. Engl. J. Med 377, 2500–2501 (2017).
Bellmunt, J. et al. Putative biomarkers of clinical benefit with pembrolizumab in advanced urothelial cancer: results from the KEYNOTE-045 and KEYNOTE-052 landmark trials. Clin. Cancer Res. 28, 2050–2060 (2022).
Haddad, R. I. et al. Influence of tumor mutational burden, inflammatory gene expression profile, and PD-L1 expression on response to pembrolizumab in head and neck squamous cell carcinoma. J. Immunother. Cancer 10, e003026 (2022).
Shitara, K. et al. Association between gene expression signatures and clinical outcomes of pembrolizumab versus paclitaxel in advanced gastric cancer: exploratory analysis from the randomized, controlled, phase III KEYNOTE-061 trial. J. Immunother. Cancer 11, e006920 (2023).
Gutierrez, M. et al. Biomarker-directed, pembrolizumab-based combination therapy in non-small cell lung cancer: phase 2 KEYNOTE-495/KeyImPaCT trial interim results. Nat. Med. 29, 1718–1727 (2023).
Cristescu, R. et al. Transcriptomic determinants of response to pembrolizumab monotherapy across solid tumor types. Clin. Cancer Res. 28, 1680–1689 (2022).
Vinayak, S. et al. Open-label clinical trial of niraparib combined with pembrolizumab for treatment of advanced or metastatic triple-negative breast cancer. JAMA Oncol. 5, 1132–1140 (2019).
Maio, M. et al. Olaparib plus pembrolizumab in patients with previously treated advanced solid tumors with homologous recombination repair mutation (HRRm) and/or homologous recombination deficiency (HRD): initial results of the phase 2 KEYLYNK-007 study. Cancer Res. 81, Abstract CT178 (2021).
Schmid, P. et al. Atezolizumab and nab-paclitaxel in advanced triple-negative breast cancer. N. Engl. J. Med 379, 2108–2121 (2018).
Emens, L. A. et al. Atezolizumab and nab-paclitaxel in advanced triple-negative breast cancer: biomarker evaluation of the IMpassion130 Study. J. Natl. Cancer Inst. 113, 1005–1016 (2021).
Rossevold, A. H. et al. Atezolizumab plus anthracycline-based chemotherapy in metastatic triple-negative breast cancer: the randomized, double-blind phase 2b ALICE trial. Nat. Med. 28, 2573–2583 (2022).
Andresen, N. K. et al. Circulating tumor cells in metastatic breast cancer patients treated with immune checkpoint inhibitors - a biomarker analysis of the ALICE and ICON trials. Mol. Oncol. 19, 2092–2108 (2024).
Voorwerk, L. et al. Immune induction strategies in metastatic triple-negative breast cancer to enhance the sensitivity to PD-1 blockade: the TONIC trial. Nat. Med. 25, 920–928 (2019).
Bachelot, T. et al. Durvalumab compared to maintenance chemotherapy in metastatic breast cancer: the randomized phase II SAFIR02-BREAST IMMUNO trial. Nat. Med. 27, 250–255 (2021).
Ullern, A. et al. Gut microbiota diversity is prognostic and associated with benefit from chemo-immunotherapy in metastatic triple-negative breast cancer. Mol. Oncol. 19, 1229–1243 (2025).
Brennan, L. et al. T-cell heterogeneity in baseline tumor samples: implications for early clinical trial design and analysis. Front Immunol. 13, 760763 (2022).
Salgado, R. et al. The evaluation of tumor-infiltrating lymphocytes (TILs) in breast cancer: recommendations by an International TILs Working Group 2014. Ann. Oncol. 26, 259–271 (2015).
Hendry, S. et al. Assessing tumor-infiltrating lymphocytes in solid tumors: a practical review for pathologists and proposal for a standardized method from the International Immunooncology Biomarkers Working Group. Part 1: assessing the host immune response, TILs in invasive breast carcinoma and ductal carcinoma in situ, metastatic tumor deposits and areas for further research. Adv. Anat. Pathol. 24, 235–251 (2017).
US Food and Drug Administration. Summary of Safety and Effectiveness Data (SSED). FoundationOne®CDx. Available at: https://www.accessdata.fda.gov/cdrh_docs/pdf17/P170019S016B.pdf. Accessed September 16, 2020.
Milbury, C. A. et al. Clinical and analytical validation of FoundationOne®CDx, a comprehensive genomic profiling assay for solid tumors. PloS one 17, e0264138 (2022).
Frampton, G. M. et al. Development and validation of a clinical cancer genomic profiling test based on massively parallel DNA sequencing. Nat. Biotechnol. 31, 1023–1031 (2013).
Cristescu, R. et al. Pan-tumor genomic biomarkers for PD-1 checkpoint blockade-based immunotherapy. Science 362, eaar3593 (2018).
Ayers, M. et al. IFN-gamma-related mRNA profile predicts clinical response to PD-1 blockade. J. Clin. Investig. 127, 2930–2940 (2017).
Clopper, C. & Pearson, E. The use of confidence or fiducial limits illustrated in the case of the binomial. Biometrika 26, 404–413 (1934).
Acknowledgements
We thank the participants and their families and caregivers for participating in this study, along with all investigators and site personnel. Funding for this research was provided by Merck Sharp & Dohme LLC, a subsidiary of Merck & Co., Inc., Rahway, NJ, USA (MSD). Statistical support was provided by Xuan Zhou, PhD, of MSD. Medical writing assistance was provided by Autumn Kelly, MA, of ICON plc (Blue Bell, PA, USA). This assistance was funded by MSD.
Author information
Authors and Affiliations
Contributions
Concept and design: E.W., J.M., P.J., P.S., R.C., S.L., V.K. Acquisition, analysis, or interpretation of data: A.L., A.G., J.M., J.C., K.T., K.S.L., L.T., L.H., M.N., N.H., O.L., P.J., P.S., R.C., R.S., S.A.I., S.L., S.O., V.K. Drafting of the manuscript or critical revision for important intellectual content: all authors. All authors approved the final version of the published manuscript, had full access to all the data in the study, and take responsibility for the integrity of the data and the accuracy of the data analysis.
Corresponding author
Ethics declarations
Competing interests
J. Cortes: Honoraria (self), Advisory/Consultancy, Research grant/Funding (institution), Travel/Accommodation/Expenses: Roche; Honoraria (self), Travel/Accommodation/Expenses: Novartis; Honoraria (self), Advisory/Consultancy: Celgene; Honoraria (self), Advisory/Consultancy: Eisai; Honoraria (self), Research grant/Funding (institution), Travel/Accommodation/Expenses: Pfizer; Honoraria (self): Samsung; Advisory/Consultancy: Cellestia; Advisory/Consultancy, Research grant/Funding (institution): AstraZeneca; Advisory/Consultancy: Biothera Pharmaceutical; Advisory/Consultancy: Merus; Advisory/Consultancy: Seattle Genetics; Advisory/Consultancy: Daiichi Sankyo; Advisory/Consultancy: Erytech; Advisory/Consultancy: Athenex; Research grant/Funding (institution): Ariad Pharmaceuticals; Research grant/Funding (institution): Baxalta; Research grant/Funding (institution): GMBH/Servier Affaires; Research grant/Funding (institution): Bayer Healthcare; Research grant/Funding (institution): F. Hoffman-La Roche; Research grant/Funding (institution): Guardant Health; Research grant/Funding (institution): MSD; Research grant/Funding (institution): Piqor Therapeutics; Research grant/Funding (institution): Puma C; Research grant/Funding (institution): Queen Mary University of London; Shareholder/Stockholder/Stock options: MedSIR. O. Lipatov: None. S.-A. Im: Advisory/Consultancy, Research grant/Funding (institution): AstraZeneca; Advisory/Consultancy: Eli-Lilly; Advisory/Consultancy/Research grant/Funding (institution): Eisai; Advisory/Consultancy: MSD; Advisory/Consultancy: Novartis; Advisory/Consultancy, Research grant/Funding (institution): Daiichi-Sankyo; Research grant/Funding (institution): Boryung Pharm; Advisory/Consultancy: Novartis; Advisory/Consultancy, Research grant/Funding (institution): Pfizer; Advisory/Consultancy/Research grant/Funding (institution): Roche. A. Goncalves: Honoraria (institution), Advisory/Consultancy, Research grant/Funding (institution): Novartis; Honoraria (institution), Advisory/Consultancy, Research grant/Funding (institution): MSD; Research grant/Funding (institution): AstraZeneca; Research grant/Funding: Roche/Genentech; Research grant/Funding: Sanofi/Aventis; Research grant/Funding: Daiichi Sankyo/AstraZeneca; Travel/Accommodation/Expenses: Menarini; Travel/Accommodation/Expenses: Mylan; Honoraria (institution), Advisory/Consultancy, Research grant/Funding (institution): Gilead. K.S. Lee: Advisory/Consultancy: Roche; Advisory/Consultancy: Lilly; Advisory/Consultancy: Pfizer; Advisory/Consultancy: Novartis; Research grant/Funding (institution), (support of drug): Dong-A Pharm. P. Schmid: Consultant fees/honoraria from AstraZeneca, Bayer, Boehringer Ingelheim, Celgene, Eisai, MSD, Novartis, Pfizer, Puma, Roche. Grant funding to the institution from Astellas, AstraZeneca, Genentech, Medivation, Novartis, Oncogenex, Roche. K. Tamura: Research grant/Funding from Eli Lilly. L. Testa: Advisory/Consultancy, Research grant/Funding (institution): Lilly; Advisory/Consultancy, Research grant/Funding (institution): Novartis; Research grant/Funding (institution): Roche; Travel/Accommodation/Expenses: Libbs; Travel/Accommodation/Expenses: Pfizer. S. Ohtani: Honoraria (institution): Chugai; Honoraria (institution): Eisai; Honoraria (institution): Pfizer; Honoraria (institution): AstraZeneca. N. Harbeck: Speaker Bureau/Expert testimony: AstraZeneca; Advisory/Consultancy, Speaker Bureau/Expert testimony: Daiichi Sankyo; Advisory/Consultancy, Speaker Bureau/Expert testimony: Gilead; Speaker Bureau/Expert testimony: Lilly; Speaker Bureau/Expert testimony: MSD; Advisory/Consultancy, Speaker Bureau/Expert testimony: Novartis; Advisory/Consultancy, Speaker Bureau/Expert testimony: Pfizer; Advisory/Consultancy, Speaker Bureau/Expert testimony: Roche; Advisory/Consultancy: Sandoz/Hexal; Advisory/Consultancy: Seattle Genetics; Shareholder/Stockholder/Stock options, Spouse/Financial dependent, Codirector of West German Study Group (self): West German Study Group; Full/Part-time employment: LMU Munich. S. Loi: Receives research funding to institution from Novartis, Bristol Myers Squibb, AstraZeneca/Daiichi Sankyo, Roche-Genentech, MSD, Pfizer, Gilead Sciences, Nektar Therapeutics, Eli Lilly. Acted as consultant to Roche-Genentech, MSD, Gilead Sciences, AstraZeneca/Daiichi Sankyo, Bristol Myers Squibb, Novartis, Eli Lilly, Amaroq Therapeutics, Mersana Therapeutics, Domain Therapeutics, BioNTech, Bicycle Therapeutics, Exact Sciences, Menari Asia-Pacific, SAGA Diagnostics, Adanate. Supported by the National Breast Cancer Foundation of Australia Endowed Chair and the Breast Cancer Research Foundation, New York. R. Salgado: Advisory Board role for BMS, Roche, AstraZeneca, Daichii Sankyo, Exact Sciences. Research funding by Roche, Puma, Merck, BMS. V. Karantza: Shareholder/Stockholder/Stock options: Merck & Co., Inc., Rahway, NJ, USA; Full-time employment: Merck Sharp & Dohme LLC, a subsidiary of Merck & Co., Inc., Rahway, NJ, USA. J. Mejia: Shareholder/Stockholder/Stock options: Merck & Co., Inc., Rahway, NJ, USA; Full-time employment: Merck Sharp & Dohme LLC, a subsidiary of Merck & Co., Inc., Rahway, NJ, USA. R. Cristescu: Shareholder/Stockholder/Stock options: Merck & Co., Inc., Rahway, NJ, USA; Full-time employment: Merck Sharp & Dohme LLC, a subsidiary of Merck & Co., Inc., Rahway, NJ, USA. A. Loboda: Shareholder/Stockholder/Stock options: Merck & Co., Inc., Rahway, NJ, USA; Full-time employment: Merck Sharp & Dohme LLC, a subsidiary of Merck & Co., Inc., Rahway, NJ, USA. M. Nebozhyn: Shareholder/Stockholder/Stock options: Merck & Co., Inc., Rahway, NJ, USA; Full-time employment: Merck Sharp & Dohme LLC, a subsidiary of Merck & Co., Inc., Rahway, NJ, USA. P. Jelinic: Shareholder/Stockholder/Stock options: Merck & Co., Inc., Rahway, NJ, USA; Full-time employment: Merck Sharp & Dohme LLC, a subsidiary of Merck & Co., Inc., Rahway, NJ, USA. L. Huang: Shareholder/Stockholder/Stock options: Merck & Co., Inc., Rahway, NJ, USA; Full-time employment: Merck Sharp & Dohme LLC, a subsidiary of Merck & Co., Inc., Rahway, NJ, USA. E.P. Winer: None.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Cortes, J., Lipatov, O., Im, SA. et al. Association of potential biomarkers with clinical outcomes in metastatic triple-negative breast cancer treated with pembrolizumab or chemotherapy. npj Breast Cancer 11, 109 (2025). https://doi.org/10.1038/s41523-025-00814-y
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41523-025-00814-y