Abstract
Breast cancer is a heterogeneous disease with global reach. Basigin (BSG) is a transmembrane protein with multifunctional roles in the breast tumor microenvironment. Using the hallmarks of cancer, we explore the pleiotropic roles of BSG in breast cancer. Further, we examine the cellular interactants of BSG and the molecular regulators of BSG. BSG has the potential to play a prognostic role and is a candidate target for new therapeutic interventions.
Similar content being viewed by others
Introduction
Human mammary tissue is particularly complex, with glands (ducts and lobules) developing from epithelial tissue interspersed with adipose and fibrous connective tissue1. These glands are highly dynamic, undergoing dramatic morphological changes that occur at the onset of puberty, during embryogenesis/pregnancy, and in involution following the cessation of lactation2. Numerous and diverse molecular regulators tightly control this dynamic environment3, dysregulation of which can lead to cellular dysfunction and cancer. Breast cancer (BC) is the most common type of cancer in women worldwide, with over 2.3 million new diagnoses in 2022 and 670,000 concurrent deaths4,5. BC is an umbrella term for a heterogeneous group of malignancies that has been categorized into several discrete subgroups through genomic and transcriptomic analysis6. Much like the highly heterogeneous breast tissue, malignancies of the breast are composed of varying cell types7. This heterogeneity is responsible, in part, for resistance to therapies, disease progression, and recurrence8,9.
While mortality due to the malignancy has declined due to screening programs and more advanced therapies10, early detection still remains key to treatment and survival11. Mammography is the most widely employed tool in the detection of lesions, and is able to differentiate between breast epithelium/stroma and fat12. This approach, however, suffers from a high rate of false positives, low sensitivity, misdiagnosis of calcifications as tumors, and significant discomfort to patients13,14,15. Liquid biopsies screened for aberrant expression of cancer-specific biomarkers (proteins and molecular markers) have gained interest as a more specific, less invasive technique for the diagnosis and management of this malignancy16,17,18,19.
Cancer cells are previously healthy cells that have undergone dysregulation with transformations both at the cellular and molecular levels, making the cells undetectable by the immune system, which fails to differentiate “healthy self-cells” from the mutated cancer cells6. The altered cell surface markers also hold prognostic potential as indicators of susceptibility and response to various treatment approaches20. Identifying, characterizing, and exploiting such markers holds a key role in the future of oncology. One such marker is the transmembrane protein basigin (BSG), also known as extracellular matrix metalloproteinase inducer (EMMPRIN) or cluster of differentiation protein 147 (CD147). BSG is well recognized for its role as a “chaperone protein,” ensuring proper localization of other proteins to the plasma membrane and enabling their function21,22,23,24,25,26,27,28,29. In cancer, it has been shown to support proliferation, migration, metastasis, and chemoresistance of tumor cells while promoting an oncogenic niche30,31. Due to the many-sided functions of BSG and its primary role as a cell surface protein, this protein has become an attractive target for therapeutic interventions in numerous cancers32.
In addition to cell surface markers, small non-coding RNAs called microRNAs (miRNAs or miRs) considered as accessible molecular biomarkers have been reported as crucial regulators of BC progression18,33,34,35,36. MiRNAs are short nucleotide sequences that regulate gene expression post-transcriptionally and also play an important role in regulating cell states, providing insight into disease states and progression37,38,39. They have been flagged as optimal biomarkers due to their detection and high stability in a myriad of body fluids, including blood, urine, and saliva40. As regulators of gene expression, miRNAs have diverse functions in the breast tissue during normal and malignant development41 and numerous miRs have been identified as aberrantly expressed in BC42. It is known that miRNAs regulate oncogenesis through their tumor-suppressive or oncogenic activities, with ample evidence of anomalous miRNA expression in a variety of malignancies17,43,44. The roles of miRNAs in mediating the various hallmarks of cancer progression in BC are areas of ongoing investigation, with considerable research specifically on miRs as inhibitors of growth suppression, enhancers of proliferation, promoters of angiogenesis and eventual activation of invasion and metastasis in particular18. A few miRNAs have been reported to directly bind to the 3’-UTR of the BSG mRNA transcript, thereby suppressing disease progression and metastasis45,46,47.
This review is a collective exploration of the role of BSG, interacting proteins, and miRNA mediators in the initiation, promotion, and metastatic transformation of BC cells. The prospective implications of targeting BSG, associated molecular interactants, and miRNAs for therapeutic and prognostic purposes in BC is also explored.
Cellular and molecular marker profiles of BC subtypes
BC can be classified in a number of different ways: location (ductal carcinoma in situ (DCIS)/lobular carcinoma in situ (LCIS) and stages), immunohistochemical (IHC) markers, and recently with molecular markers that include miRNAs and mutations of key oncogenic genes (BC antigen gene 1 and 2, BRCA1, BRCA2, tumor suppressor protein 53, TP53)48. The most common method of classification relies on IHC screening of the hormone receptors (HRs) for estrogen (ER) and progesterone (PR) as well as the expression levels of the human epidermal growth factor receptor-2 (HER2, also known as ERBB2 or HER2/neu)48,49. Introduction of gene expression profiling organized BC into different molecular subtypes: normal-like, luminal-like, HER2-enriched, and basal-like were identified by Perou and colleagues in 200049; the triple negative (TNBC) subtype was later included to denote those that lacked expression of any of these surface antigens and thus were only able to avail of the non-specific chemotherapeutic interventions50. The various classification systems of BC are summarized below [Table 1].
Studies have shown that the presence of multiple cell types in normal mammary epithelia that acquire distinct features when transitioning to a disease state can become markers of disease and are key in identifying and delivering targeted therapy to the malignant cells44,51,52. With the evolution of genomic studies and open access to published large “-omics” data sets, more specific molecular markers of disease have been identified53,54,55,56,57. The availability of polymerase chain reaction (PCR) tests has also made categorization easier, as absolute quantification of gene expression can be measured more precisely than the conventional classification based on the expression analysis of histological markers58,59. As our understanding of the complex tumor microenvironment (TME) evolves further and the technology advances to detect more minuscule markers (in both quantity and size), miRNAs emerge as one of the preeminent signals in BC subclassification60. For instance, miRNA-4728 has been identified as a surrogate marker for HER2 expression60, miR-21 and the miR-200 family are involved in BC stem cells (CSCs)61, and the accumulation of miR-21 and miR-181a in bone marrow of BC patients has significant prognostic implications34. The inclusion of these biomolecules in testing strata clarifies the heterogeneous nature of the TME and the tumor itself, while providing further insight into the prognosis and potential therapeutic response of patients as well as in real-time monitoring of the disease37,62. Multiple gene expression profile panels have been designed and released to market for determining therapeutic strategies and to predict patient responses to therapies [Table 2].
With advanced technologies providing us with a better understanding of the numerous diseases affecting individuals, we have also come to understand the great inter-individual variability that stems from environmental, physiological, molecular, and socioeconomic factors unique to each person63,64. This led to the transformation of clinical investigations into “personalized medicine,” or “precision medicine,” which takes into account the individual clinicopathological features to improve efficacy of treatments and limit the side-effects65. In order for these efforts to be effective, biomarkers that reflect the state of disease must be clearly identified for diagnosis, prognosis predictions, monitoring of disease progression, and monitoring patient responses to therapies66. Classical markers in breast cancer include histological biomarkers (hormone receptors Estrogen (ER) and progesterone (PR), HER2 and Ki-67 expression) and genetic biomarkers (TP53), GATA-binding protein 3 (GATA3), mitogen-activated protein kinase kinase kinase 1 (MAP3K1), BRCA1)67. Biomarkers in the form of microRNAs68 and circulating tumor cells (CTCs)69 are also gaining traction in cancer research and hold the potential to inform the therapeutic courses of action. However, they both tell an incomplete story. Most miRNAs can bind to multiple messenger RNAs (mRNAs)70 and are expressed in multiple tissues concurrently71, making it difficult to elucidate the role each miRNA plays in physiology. In addition, the heterogeneous expression of neoantigens within the TME makes neoantigen-directed therapies an imperfect targeting mechanism72.
Expression significance of BSG in BC
While the methods of BC classification are diverse and evolving with our understanding of the neoplasm, surface markers will remain key players in early detection and treatment of this malignancy. Most patients still receive treatment plans revolving around the classical disease markers (IHC and pathological classification), leading to under or over-treatment of the disease73. The delayed recurrence of BC represents a unique challenge in assuring disease-free survival of patients74, making the identification of cells that facilitate minimal residual disease that leads to long term relapse increasingly important73,75. Emerging biomarkers such as trophoblast cell surface antigen 2 (TOP2)76, sera carbohydrate antigen 15–3 (CA15-3), HER2 levels77, and circulating trefoil factor (TFF) 1, TFF2, and TFF3 have shown promise in identifying BC78. However, dual-purpose biomarkers and drug targets present a holy grail of sorts for BC diagnosis and treatment.
As a surface marker that has been implicated in tumor-initiating breast cancer stem cells (BCSCs), the transmembrane glycoprotein BSG has the potential to play a role in the next generation of cancer biomarkers79,80. Upon initial discovery over 40 years ago, BSG was named “tumor cell-derived collagenase stimulatory factor” (TCSF), due to an overexpression of the protein on tumor cells22,24,81. Later renamed as extracellular matrix metalloproteinase inducer (EMMPRIN)23, the protein is today commonly referred to as “Basigin” (BSG), or cluster of differentiation 147 (CD147)82. BSG is a glycoprotein with two immunoglobulin-like domains encoded by the CD147 gene located on chromosome 19p13.383. Reports of abnormal CD147 expression across multiple solid tumors, in addition to breast tumors, are extensively reviewed by Li. Y. et al.84. BSG is involved in a number of functions: cytoskeletal remodeling, migration and invasion, therapy resistance in cancer treatment, angiogenesis, and pro-inflammatory signaling85. Regulation of matrix metalloproteinases (MMPs) in adjacent fibroblasts modifies the extracellular microenvironment in an oncolytic manner86. Proper localization of BSG is essential for the function of the monocarboxylate transport proteins (MCTs) MCT1 and MCT4, which are key for lactate transport in glycolysis87,88,89. BSG has also been identified as a stemness marker in multiple carcinomas90,91, where the protein appears to confer chemoresistant properties to a subpopulation of cells. BSG has been found to promote the epithelial to mesenchymal transition (EMT) in numerous solid cancers, thereby promoting metastasis92. As a versatile protein, it is useful to look at the pleiotropic roles BSG plays in cancer by examining the involvement in key hallmarks of cancer, as outlined by Hanahan and Weinberg, and highlighted in [Fig. 1]93,94,95.
The Hallmarks of cancer, first introduced by Hanahan and Weinberg in 200095 and updated in 201194 and 202293 provide a useful way of framing the various roles BSG plays in the oncogenic environment. Notably, BSG influences non-mutational epigenetic reprogramming, invasion and metastasis, angiogenesis, cellular energetics, and phenotypic plasticity. These hallmarks, highlighted amongst the current hallmarks, form the basis of this review. Created in BioRender. Richard, V. (2025) https://BioRender.com/8ttjnxe.
Role of BSG in nonmutational epigenetic programming
Epigenetic modifications—including DNA methylation, histone modification, noncoding RNA (ncRNA) modulation of gene expression, and epi-transcriptomic regulation of RNAs to modulate gene expression have been identified as key drivers of cancer development and progression96,97. These changes lead to aberrant biochemical pathways and metabolomics, which form the oncogenic niche98. To date, there are no genetic mutations that have been identified as metastatic triggers, suggesting that this progression is driven by epigenetic and epi-transcriptomic changes96. Acquisition of oncogenic and metastatic phenotypes are the result of post-translational modifications to mRNAs and transcription pathways99.
BSG is able to induce the synthesis of hyaluronan, the primary ligand for cell surface receptor CD44, which has been previously implicated in BC stem cells85. Grass and colleagues have shown that an upregulated expression of BSG activates EGFR-Ras-ERK signaling pathway via increased hyaluronan expression, and also hypothesize that this may explain the aberrant Ras activity in cancer, despite the absence of oncogenic Ras85. While this was the result of an adeno-associated virus (AAV)-mediated BSG amplification, it was noteworthy that the effect was observed at levels commonly detected in BC. In a manner not yet fully understood, BSG expression stimulated the production of all three hyaluronan synthases (HS1, HS2, and HS3) and hyaluronan production100, thereby promoting anchorage-independent growth, an indicator of malignant transformation101. One proposed method for this is the stimulation of hyaluronan production via lactate efflux facilitated by MCTs which are trafficked by BSG to the cell membranes102,103,104. ERK signaling is a key regulator of cell proliferation, survival, growth, metabolism, migration and differentiation105.
BSG-mediated activation of invasion and progression to metastasis
Hyaluronan is ubiquitous throughout the extracellular matrix and a key element of the TME that influences tumor growth and disease progression106. Stimulation of hyaluronan is well documented to promote anchorage-independent growth in cancer100,107 and resistance to cancer therapies108,109,110,111,112,113. The effect is mediated by CD44, which co-localizes with BSG in lipid rafts in the plasma membrane to form a positive feedback loop amplifying invasion85,104,109,114,115. High levels of BSG resulted in an increased localization of CD44 and epidermal growth factor receptor (EGFR) proteins to the cell surface and specifically to protein rafts compared to BSG low cells21. Additionally, increased BSG on the surface of MCF10A cells was observed without a corresponding increase in mRNA levels/protein synthesis, indicating that retention or recycling of the protein may be at play85. CD44, when overexpressed in murine BC models, has been shown to induce apoptosis, thereby inhibiting growth, local invasion, and metastasis111.
While the precise roles of MMPs in cancer metastasis are debated due to their involvement in numerous contradictory pathways, the interactions between BSG and MMPs are worth examining. BSG has been observed to mediate the activity and expression of MMP-1, MMP-2, MMP-3, MMP-9, MMP-14, and MT2-MMP116,117,118. These proteases are responsible for modifications of the TME, which promote EMT and are attractive targets for therapeutic interventions119,120. Research on somatic mutations of TNBC samples in The Cancer Genome Atlas-Breast Invasive Carcinoma (TCGA-BRCA) data has shown that MMP9 is significantly upregulated in TNBC compared to other subtypes in a manner that may explain the proclivity of TNBC to proceed down EMT pathways and metastasize earlier than other subtypes121. Martin and colleagues observed that MMP-9 ablation in the lungs reduced metastasis of BC to the lungs, while MMP-7 deletion did not produce a similar effect122. This was observed in mice in a manner dependent on their lineage, suggesting there is a genetic component to the effect of MMP-9 ablation. MMP14, identified as membrane-type-1 matrix metalloproteinase (MT1-MMP) also present in the lipid-rafts of invadopodia, promotes invasion in otherwise non-transformed, non-invasive BC cells123. BSG is a member of the cell membrane protein rafts, and has been shown to be negatively correlated with caveolin-1, thus reducing BSG-dependent MMP induction124. Tang and Hemler found that clustering of BSG in protein rafts was important for effective induction of MMPs, indicating that expression levels of BSG alone may be an insufficient indicator for the effect of BSG on tumor cell behavior. With the ability to enhance MMP activity, BSG promotes tumor invasion and metastasis, facilitating the establishment of local expansion and distant metastasis in BC.
BSG-regulated cell proliferation and inflammation
It is interesting to note that when released from the cell membrane, soluble BSG inhibits migration of BC cells, but promotes cellular proliferation125. As a cell-surface-bound protein, BSG functions as a receptor protein for many secreted molecules, including peptidylprolyl isomerase A (PPIA), also known as cyclophilin A or rotamase A (CypA)126. As a pro-inflammatory cytokine, PPIA stimulates phosphorylation of extracellular kinases, thereby promoting migration, proliferation, and differentiation of cells127. The upregulation of PPIA by NAD(P)H quinone dehydrogenase 1 (NQO1) has been identified as a promoter of BC metastasis to the lungs via activation of BSG128. PPIA and BSG are both upregulated in multiple cancers, including BC, where higher expression levels are correlated with an advanced disease stage129. Acting via the phosphorylated signal transducer and activator of transcription 3 (pSTAT3) pathway with PPIA, BSG can induce transformation of non-stem cells into a cancer stem cell phenotype, promoting metastasis and therapeutic resistance130. Overexpression of PPIA has been correlated with poor outcomes for patients, including disease progression and relapse127.
MCT-4 overexpression has been observed in the metastatic BC cell line MDA-MB-231131, where silencing of either BSG or MCT4 decreased surface localization of the other and reduced in vivo metastasis. In the BC cell line MDA-MB-436, induced BSG expression increased tumorigenic abilities and invasion in vivo, while human xenografts of BC in murine models were observed to generate minimal stromal and inflammatory cell reactions132. There is emerging evidence that many of the growth factors which promote tumor growth and metastasis are manufactured by peritumoral fibroblasts, rather than cancer cells themselves133. These cells, which are part of the TME, play a significant role in the growth and metastasis of neoplasms. As such, BSG is a candidate for promoting the proliferation of tumors via the induction of MMP synthesis132. Modification of the ECM plays a key role in facilitating or inhibiting access of immune cells to the TME, likewise inhibiting or enabling migration, differentiation, and cytokine production in an oncogenic manner134.
BSG-mediated inducing or accessing of vasculature
Vasculature within the TME is essential for the survival and metastasis of cancer, enabling the delivery of nutrients to cancer cells and metastasis from the primary site throughout the body. Experimentally, BSG has been proven to promote angiogenesis via inducing the expression of vascular endothelial growth factor (VEGF) in both MMP-dependent and independent manner135. BSG expression has been shown to increase angiogenesis in the TME by stimulating the expression of VEGF and MMPs in tumor cells and the neighboring stroma136. Additionally, identified as a coreceptor of VEGF receptor 2 (VEGFR2) in tumor and endothelial cells, BSG enhances VEGF functions and supports angiogenesis137,138,139. Soluble BSG expressed by fibroblasts following induction via tumor cell-BSG expression140 also activates the PI3K-Akt pathway to produce VEGF in neighboring fibroblasts136.
BSG in the deregulation of cellular energetics
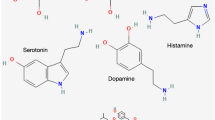
BSG has been shown to play a role in glycolysis in numerous cancers141, a key pathway for tumor cell energy and proliferation. Supporting the localization of the monocarboxylate transporter proteins MCT1, MCT3, and MCT4, BSG facilitates lactate transport across the plasma membrane89,111,142. Interaction between BSG and MCTs is necessary for MCT trafficking to the plasma membrane111 and, in some instances, for the proper functioning of MCTs143. MCT activity is, in turn, essential for the maintenance of a glycolytic phenotype, termed the “Warburg effect,” found in most malignant cancers, emerging as a measure of resistance to therapy31,111. As cancer cells shift to this glycolytic phenotype, they generate cytotoxic levels of intracellular lactate that are exported by MCTs144,145. The exported lactate can then be taken up by nearby normal cells and used for oxidative phosphorylation (OXPHOS), freeing up glucose for cancer cells to utilize144. Upregulation of MCTs and BSG in cancers facilitates this “metabolomic symbiosis” between normal and tumor cells and contribute to an oncogenic microenvironment, allowing cancer to continue to proliferate144,146,147,148.
At the leading edge of a tumor, lactate efflux acidifies the TME, which in turn enhances invasion, metastasis, and drug resistance111. MCT4 and BSG show strong co-localization and compounding effect on ECM degradation, invasion and metastasis in MDA-MB-231 cells149. Work in the MDA-MB-231 and MCF-7 cell lines as well as Xenopus oocytes has shown that the small molecule Beta-Galactose 2 C (BGal2C) blocks the interactions between MCT-1 or MCT-4 and carbonic anhydrase IX (CAIX) by binding to BSG, thereby inhibiting lactate efflux from the cells150,151. This effect was only observed in BC cells, and not in healthy tissue152. Disruption of MCT1/4 blocks lactate transport and reduces glycolysis, thereby reducing tumor cell proliferation [Fig. 2].
The multifunctional roles of BSG in the TME enable tumor growth and progression to distant metastases by (i) enabling lactate efflux to promote an acidic environment that inhibits the growth of normal cells and promotes tumor expansion, (ii) by stimulating VEGF production BSG promotes the delivery of nutrients to the TME and the development of vasculature through which CSCs can metastasize, and (iii) by disrupting tumor ECM through CD44/MMP production, BSG promotes anchorage-independent growth and EMT transformation. BSG enriched cells form a population of CSCs, which intravasate blood vessels, circulate, and extravasate to a distance site. Created in BioRender. Richard, V. (2025) https://BioRender.com/5gpaf4a.
BSG unlocks the stemness and phenotypic plasticity of cancer cells
CSCs are a small subpopulation of tumor cells with the ability to proliferate extensively and establish malignant lesions153,154. As few as 200 cells with the CSC phenotype are able to form tumors, whilst 10,000 non-CSC tumor cells fail to generate tumors when injected in immune-suppressed mice models154. CSCs are as heterogeneous as cancer cells themselves, with different markers used to identify CSCs across different cancer types. The CD44 + /CD24- population of cells has come under increasing scrutiny for their ability to resist therapeutic interventions and establish a resurgent, more aggressive population155,156. In BC, this fraction highlights the cells more likely to go down the pathway of EMT and metastasis92,157.
In BC, CD44+ expression is consistently cited as a marker of BCSCs, with some authors going so far as to suggest that it alone is sufficient for classification of BCSCs158. Ongoing work to study this subpopulation of cells currently uses multiple markers, including expression of CD133, CD90, CD44 with low or no expression of CD24153,159. BSG has been identified in oral carcinoma as a marker of CSCs90, and the multitude of roles it plays in the BC TME suggests it may be a valuable marker of BCSCs as well38. Research into the CD44+ subpopulation of BC cells has revealed that exposure to chemotherapy can induce non-BCSCs to revert to the BCSC phenotype, including an overexpression of BSG protein, which promotes CSC detachment from the ECM in advance of metastasis130. As “master regulators of gene expression,” numerous microRNAs have also been identified as BSG regulators, and may be considered regulators of CSC state by extension38,160.
MicroRNAs as molecular interactants of BSG
First discovered in C. elegans in 1994 by Lee and colleagues161, microRNAs have now been identified as “master regulators of gene expression”162. These small (22–26 nt) transcripts regulate gene expression post-transcription to control fundamental cellular processes163. The microRNA lin-4 discovered by Lee and colleagues in 1994 and lethal-7 (let-7) discovered by Reinhart and colleagues in 2000 were identified based on their role in embryonic development as “heterochronic genes” which temporally regulated gene expression161,164. The first implication of microRNAs involved in cancer came from study of chronic lymphocytic leukemia in 2002, where Crocer and colleagues identified downregulated or deleted miR15a and miR16-1 associated with the disease165. A number of miRs termed “oncomiRs” which promote tumor growth and metastasis have also been identified in BC166,167. As studies of miRNAs in BC have advanced, it has become clear that miRNA profiles are linked to disease state, with studies showing that the removal of malignant lesions reverts expression profiles of miRs in circulation and in the TME to a precancerous profile168. Developing clear miRNA expression profiles that relate to disease state and elucidating the relationship between dysregulated miRs and their interactants holds significant promise for diagnosing and treating cancers in general and BC specifically.
MicroRNA let-7b has been identified as a prognostic marker in ovarian169 and BC170, and has been proposed as a regulator of BSG170,171. The let-7 family has been identified as a tumor-suppressor that inhibits BC migration and metastasis172. In BC, miR-22 has been shown to play a regulatory role in BSG expression46. Xu and colleagues identified miR-22 as a senescence inducer in fibroblasts and observed a decrease in miR-22 expression in epithelial and BC cell lines47. Restoration of miR-22 in these cells facilitated a change to a senescent state in breast and cervical cancer cells47. Others reported that miR-22 was able to bind to Sp1, which is a transcriptional enhancer of BSG46. Kong and colleagues also observed the binding of miR-22 and Sp1 directly to BSG mRNA, thus inhibiting protein expression both in a direct and indirect manner46, shown in [Fig. 3]. Both groups report that miR-22 inhibited invasion, metastasis, and proliferation via targeting BSG46,47. Kong and colleagues found that downregulated miR-22 levels also correlated with increased tumor size, nodal involvement, and metastasis (TNM) in patients as well46. Zhang, Chen, and Ding found a similar association in cervical cancer, where low miR-22 expression was correlated with increased TNM while being negatively correlated with five year and overall survival173. Conversely, Pandley and colleagues have shown that the silencing of Tat-interactive protein 60 kDa (TIP-60), a lysine acetyl-transferase, upregulated the expression of miR-22 to suppress EMT and disease progression in BC174. The authors suggest that miR-22 and TIP-60, when taken together, may serve as effective prognostic for BC [Fig. 3].
When uninhibited (a), the transcription and translation of BSG facilitates remodeling of the ECM via enhanced lactate efflux caused by MCTs, CD44-mediated hyaluronan synthesis, and MMP-modulated TME, enabling EMT and metastasis. Interruption of BSG transcription (b) by miR-22 (green color) – via competitive binding to transcriptional promoter Sp1 or translational inhibition (c) when miR-22 or miR-890 (red color) – bind to BSG mRNA interrupt BSG-mediated BC progression. Both miRs have been identified as onco-suppressors and are downregulated in breast cancer. Created in BioRender. Richard, V. (2025) https://BioRender.com/3pvuezw and https://BioRender.com/n95jnw5.
An enrichment of miR-22 in MCF-7 BC cells repressed glucose metabolism and suggested that restoration of miR-22 in BC may be an effective treatment modality175. While the authors do not specify the role BSG plays in this circumstance, their focus was on genes specifically involved in glucose metabolism175. Given the role BSG plays in MCT localization and the glycolytic phenotype, future research is likely to further establish their interaction as a key pro-tumor pathway. Wang and colleagues have reported that miR-890 also binds to the 3’-UTR of BSG, inhibiting disease progression in TNBC45 (Fig. 3c).
While used to treat Rheumatoid Arthritis (RA), Tocilizumab – an anti-IL6 monoclonal antibody – has been effective at decreasing angiogenesis and the level of circulating soluble form of BSG while increasing hsa-miR-146a-5p and hsa-miR-150-5p in RA patients176. Further work treating endothelial cells with a miR-146a mimic reduced the secretions of BSG, VEGF, and MMP9176. Authors identified a potential mechanistic relationship in epithelial cells where BSG secretion was increased and miR-146a levels decreased when NF-Κβ or JAK/STAT pathways were inhibited176. Zisman and colleagues further support the regulatory role of miR-146a on BSG, finding that JAK/STAT inhibition decreased BSG secreted protein, but did not affect BSG mRNA; rather, miR-146a levels increased to inhibit BSG177. In their most recent work in RA models and patient sera, Zisman and colleagues determined that BSG is able to perform dual functions of increasing the angiogenic factors and decreasing anti-angiogenic factors, specifically endostatin and proteasome 20S, via MMP9178. While these experiments were not performed in BC cells or patients, the interaction is worth further research. There are a handful of miRs acting as promising candidate biomarkers for detection and targeted therapeutics in breast cancer, meriting further investigation. A pan-BC study of BSG and regulating miRNA expression levels needs to be conducted and presents an interesting aspect for future investigation.
The clinical potential of BSG
Prognostic implications in BC
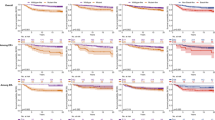
There is evidence to support a prognostic role for BSG in multiple cancers, such as BC84, pancreatic cancer179, primary cutaneous malignant melanoma180, and liver cancer181, where studies have even identified specific isoforms of the protein with increasing prognostic value182. Meta analyses support the findings that BSG overexpression has poor prognostic implications141,183,184,185 and predicts patient response to therapies186. Given a cyclical interaction between BSG, CD44, and hyaluronan, the overexpression of BSG may be indicative of malignancy in cancer and resistance to therapies111. Shi and colleagues found an increased expression of BSG in tumor tissue compared to normal tissue. Xin, Zeng et al. highlighted that resistance to both radiation and chemotherapy can be predicted based on high BSG levels186. Resistance and disease progression may be influenced by the aforementioned ability of BSG to induce stemness in non-stem cells in BC130. Lui, Xu, and colleagues noted that enhanced mRNA expression levels of BSG in BC are specifically related to tumor recurrence, metastasis, and patient survival84. In TNBC, high BSG expression correlated with advanced TNM, elevated Ki-67 levels, and positive p53 expression141, which in turn, indicated poor prognosis in TNBC patients187. In TNBC, high expression of hypoxia-inducible factor-1alpha (HIF-1α) and BSG also allied with high Ki67 levels, histological grade, and lymph node involvement188 proving valuable for both prognostic and diagnostic use.
Given that BSG is able to promote anchorage-independent growth, a key characteristic of malignant cancer cells100 the expression levels of BSG may be able to predict the aggressive level of tumors when enriched with the protein. BSG protein is expressed on the cell surface and in extracellular vesicles (EVs) secreted throughout the human body21,189,190,191,192. BSG has been identified as a marker of (1) EVs secreted specifically by cancer cells, and (2) cancer cell EVs rich in miRNAs193. EVs protect the cargo – miRNAs – in circulation194 and cancer cell EVs are likely to be more reflective of the oncogenic phenotype than other cell-free sources of nucleic acids80,195,196. Isolating a sub-population of circulating EVs originating from cancer cells is a key area of interest in cancer research because these vesicles offer targeted snapshots of the TME, enhancing the specificity and sensitivity of liquid biopsy100. Yoshioka and colleagues developed a protocol to isolate extracellular vesicles (EVs) expressing BSG/CD9 from the serum of colorectal cancer patients without prior purification197. This technique combined with the findings of Ko and colleagues193, who identified BSG-positive EVs as enriched with tumor miRs, may present a highly specific avenue for biomarker investigation. BSG has time and again been shown to correlate with breast cancer progression198. While numerous studies have been conducted to identify miRs as biomarkers in cancers199, translation to the clinic has been challenging, due in part to variation in sample preprocessing200. The ability to isolate breast cancer cell-derived EVs, which protect breast cancer-specific miR contents from degradation while in circulation, may enable future clinical translation of sensitive diagnostic and prognostic tests.
Therapeutic interventions in breast cancer- antibody-drug conjugates (ADC)
Neither surgery, radiotherapy, nor chemotherapy can be described as a precise intervention; each removes or kills off collateral healthy cells in the vicinity and can cause severe, off-target affects which debilitate cancer patients201. Hormone therapy likewise falls short of targeted intervention in many cases: from 2015 to 2019, approximately 15% of new breast cancer diagnoses in US women were negative for one of the two hormone markers used to target therapy202. Thus, new and more personalized methods of drug interventions are necessary. Inhibition of BSG production in vitro and in vivo has seen promise for the treatment of hepatocellular carcinoma and may be applicable in the treatment of breast cancer203. Further, Li, Xu, and colleagues have noted that BSG expression is significantly upregulated in breast cancer compared to sarcomas and matched breast tissue samples enriched with normal epithelium84. BSG comes in forms with differing levels of glycosylation, which correlate with the ability to induce MMP production. The oncogenic membrane protein caveolin-1 has been shown to selectively associate with the highly-glycosylated form of BSG, which is responsible for MMP induction, and inhibit this activity124,204,205. The association between BSG, MCTs, MMPs, and CD276, for example, presents an avenue for highly specific targeting to the TME181,206. Given the numerous studies that find a role for BSG in EMT and metastasis92, BSG may be even better suited for an ADC target than other candidates, as it can be a marker of aggressive carcinomas. Enrichment of BSG within the TME has already led to the development of BSG-mediated therapies.
Combining the precision of monoclonal-antibody-directed targeting and the therapeutic efficacy of a range of treatments, antibody-drug conjugates (ADCs) are the next big thing in cancer therapies. These “magic bullets” as some have described them are guided to target sites by tumor-specific antigens201,207. Target antigen selection is one of the key parameters when designing a new ADC: the antigen target can inform the method of drug delivery (endocytosis) and should ensure that tumor cells and those in the nearby pro-oncogenic microenvironment receive the cytotoxic payload201. The target antigen should also be a surface protein to enable recognition of the site by the ADC. Additionally, ADCs can be developed with specific drug to antigen ratios (DARs) which allow for precise dosing and improve therapeutic safety201. While targeting of the cancer cells themselves is ideal, ADCs that disrupt the pro-oncogenic TME also hold clinical potential207. Given that the cells in the TME have a more stable genome, the chance of them developing therapy resistance is lower than that of tumor cells208. Proteins such as HER2 in breast cancer, CD20 in B cell lymphoma, and Nectin-4 in urothelial cancer have proven viable targets for the delivery of a cytotoxic payload207. In the initial development of ADCs, antibodies were synthesized using murine hybridomas; however, these monoclonal antibodies (mAbs) were highly immunogenic209. As recombinant DNA technology advanced, mAbs were then synthesized in chimeric forms and then in fully human forms, building the base of most ADCs available on the market today207,209. Improved ADCs integrate traditional small-molecule drugs, multiple pharmacological agents, statin and kinase inhibitor-based enhancers have opened new avenues in targeted therapeutics207,210.
In hepatocellular carcinoma (HCC)—where the majority of translational research on the protein to date has occurred—BSG has proven a valuable target for therapeutic applications211,212. The approval of Metuximab (Licartin brand name), a 131-I/anti-CD147 conjugate213, has been used as an effective treatment in HCC since the early 2000s214. The mAb target, HAb18G, has been mapped to specific residues of BSG—39LTCSLNDSATEV50—which are part of domain B of the extracellular portion of BSG215,216. While soluble BSG has been observed in multiple cancers, it appears that the highly glycosylated form of BSG is present in circulation204, and Hab18G binds to a portion of BSG, which becomes glycosylated216. This explains the selectivity of Metuximab for the tumor site, rather than interacting with circulating BSG. Despite the dramatic success of BSG-targeted therapy in HCC217, investigation into potential therapeutic approaches in breast cancer is sparse. Ma and colleagues described the use of Iodide 124 labeled anti-CD147 antibody for tumor detection in colon, pharyngeal squamous, prostate, and pancreatic cancer models in vivo218. Bispecific antibodies that target two moieties have seen early success in improving lysosomal localization of a HER2-targetting ADC via CD63 targeting219, which may prove to be the first in a new line of multi-target ADC studies. Likewise, dual drug ADCs have been more effective in treating heterogenous breast cancer tumors than dual administration of two individual drugs when studies in a murine model220. As a surface antigen, BSG is a prime target for future development of Antibody-Drug Conjugates (ADCs).
The future of BSG in personalized cancer research
Leveraging the interplay between BSG and hyaluronan-promoting therapy resistance111, inhibition of BSG may improve patient response to current interventions. Interrupting the cycle of BSG/CD44/hyaluronan feedback may provide an avenue to reinvigorate the therapeutic response, providing a potential method for recovery of cells that have initiated progression down the CD44-hylauronan escape pathway of receptor-oriented therapeutic evasion221. Targeting of CD44 via BSG in breast cancer cells may be an effective way to attenuate the efflux of lactate from breast cancer cells, which promotes TME acidosis and therapy resistance104. Treatment with anti-hyaluronan oligomers is an effective method for the internalization of CD44 and dissociation of MCT1 and MCT4 from the surface of breast cancer cells104. This may also be a method for re-sensitization of therapy resistant breast cancer110. Targeting of CD44 has already seen some promise in clinical trials in skin, colon, and solid cancers109, though emergence of unacceptable toxicity caused at least one trial to be discontinued. CD44 has been identified as a possible CSC marker, with evidence in breast cancer that as few as 100 CD44+ patient cells are able to form tumors in mice, while tens of thousands of cells lacking this phenotype failed to produce similar results154,222,223. Inhibition of CD44 has already increased trastuzumab efficacy in vitro and in vivo by improving binding of trastuzumab to HER2224. CD44 has been regarded as a marker of stem-cell phenotypes in cancer, correlating with reduced survival rates in TNBC patients121,187,225. Improved targeting of tumor cells directed by BSG expression may re-enable research into the failed anti-CD44 mAb drug scenario.
The case of targeting BSG-mediated interactions
As previously reported, BSG/MCT complexes can be found in breast cancer, specifically in tumor cells in distinct patters compared to normal cells150,152. The pivotal role they play in lactate transport and cell proliferation makes them interesting targets for therapeutic interventions226. BSG targeted therapies have been proposed for leukemia227, and may have applications in breast cancer as well. Expression of MCTs is significantly upregulated in breast cancer147, disruption of which leads to cytotoxic levels of lactate and H + . Combined with impeding the regeneration of NAD+ to inhibit ATP regeneration, interruption of MCT activity may present an avenue for cancer intervention145,228,229. Targeting MCT disruptors to the TME by conjugating them to BSG would improve the specificity of these drugs. Research into MCT interactants such as β1-integrin has shown that MCT4 specifically is involved in cell migration and disruption of MCT4 trafficking to the cell membrane may halt the metastases of cancer cells as well230. Recent research has revealed that miR-342-3p is able to modulate MCT1 expression and is downregulated in TNBC231. Delivery of miRNA-mimics or exogenous miR-342-3p to TNBC tumors may be able to abrogate elevated MCT levels. RNA interference (RNAi) of BSG has been found to inhibit invasion and metastasis in breast cancer in vitro232. Numerous miRs, as outlined previously, regulate BSG expression and may be candidates for miRNA-mediated therapies233. Some have argued that any approaches for targeting BSG to inhibit functionality should disrupt protein-protein interfaces with peptides or monoclonal antibodies instead of small molecules, due to the large binding surface area of the protein137.
Barriers to BSG-mediated therapies
While ADCs improve on the tumor targeting potentials of earlier therapeutics, off-site effects still occur and necessitate monitoring for severe adverse events. In the case of HER2-targeted therapies for breast cancer, interstitial lung disease (ILD, pneumonitis) has been reported in some patients234,235. While high-grade events were rare (0.7% for grade 3+ among 9886 patients), widespread use of the therapy may lead to more common occurrences. Hackshaw and colleagues did identify that patterns of incidence wherein combination therapies – patients treated with trastuzumab in combination with everolimus and paclitaxel – saw the highest incidence of ILD234.
Though ADCs show great promise, the administration routes are hampered because they rely on surface antigens for endocytosis and payload delivery. To be effective, ADCs must circulate from the site of their injection (usually intravenous) to the tumor vasculature, permeate through the vesicular membrane, and bind with the surface antigen target236. ADCs are notably hampered by limited penetration into the tumor mass, restricting the efficacy of these potential “Trojan Horses”237,238. Often hampered by size, some studies have found that less than 1% of ADCs reach the target site in the tumor239. Increasing the permeability of tumor vasculature and ADC persistence may overcome this barrier240 and some research has suggested that ADCs can be viable therapies even without internalization by disrupting the TME241. Like traditional therapies, ADC interventions can fail due to evolved drug resistance in tumors – either by mutations of the drug target, or mutations to the antigen targeted by the ADC207,242,243.
Concluding remarks
Initial categorization of breast cancer relied on clinical-pathological data244; the start of the millennium saw widespread adoption of the use of biomarkers in the form of antigens on the surface of tumor cells to detect the disease via histological analysis49,245. Traditional markers for breast cancer diagnosis include the estrogen and progesterone hormone receptors and the HER2 protein. These markers were attractive because they were easy to detect using established methodologies of IHC and FISH, and are relatively easy to perform246. While these techniques are less precise than quantification of nucleic acids, such as PCR and next-generation sequencing (NGS), they do exemplify features to seek out when identifying new biomarkers.
BSG, as a transmembrane protein, has the potential to play a role in the next generation of breast cancer markers. BSG has been shown to have prognostic implications32,141,182,247,248 and its role in cancer stem cells makes it a particularly attractive target61,130,153,155,158,177,206,222,249. The complex interactions between BSG and MMPs, MCTs, and the TME suggest there are numerous ways BSG-targeted interventions may be effective84,86,129189,212,213,214,218,250: in the form of ADCs, BSG-targeted miR delivery, or disruptions to the BSG/CD44/hyaluronan axis113. Despite this promise, BSG-BC therapies have not yet been introduced to the clinical research scene.
MicroRNAs have seen increasing interest as potential vectors for therapeutic application. While there has been significant work to identify miRs aberrantly expressed in each subtype of breast cancer160,168,251, a consensus has not yet been reached on clear expression profiles. There a frequent conflicting reports of expression levels of specific miRNAs in cancer, which is compounded by numerous miRNAs playing roles in both healthy and disease states, often with minuscule differences in expression levels252. It is unlikely that a single miRNA will be sufficiently informative to definitively diagnose any disease253. Additional challenges come in the form of detecting sufficient quantities of microRNAs in circulation, compounded by irregularities in collection, storage, and isolation techniques254,255,256,257,258,259. CTCs are a sign of metastatic cancer, but are often difficult or impossible to detect at early stages69. While research in these areas is promising, further work is still needed to improve on the current status quo in breast cancer diagnosis and monitoring. While the molecular profile of each breast cancer subtype will vary from individual to individual (inter-tumoral heterogeneity) and even varies between tumor cells within lesions (intra-tumoral heterogeneity), breast cancer by its very nature is a disease of excessive cell growth. As such, cell-surface proteins, growth factors, and microRNAs which promote cell growth or modification of the naïve environment are key in the perpetuation of these malignant lesions.
Data availability
No datasets were generated or analyzed during the current study.
References
Thomas, P. A. Breast cancer and its precursor lesions. In Current Clinical Pathology (Humana Press, 2011).
Perrella, S. et al. Human milk composition promotes optimal infant growth, development and health. Semin. Perinatol. 45, 151380 (2021).
Biswas, S. K., Banerjee S., Baker G. W., Kuo C. Y. & Chowdhury I. The mammary gland: basic structure and molecular signaling during development. Int. J. Mol. Sci. 23, 3883 (2022).
WHO Breast Cancer Fact Sheet. Fact Sheets [Web page] 2024 13 March 2024 [cited 2025; Available from: https://www.who.int/news-room/fact-sheets/detail/breast-cancer
Curbing the climb in cancer incidence. Lancet Oncol. 25, 529 (2024).
Blenkiron, C. et al. MicroRNA expression profiling of human breast cancer identifies new markers of tumor subtype. Genome Biol. 8, 214 (2007).
Skibinski, A. & Kuperwasser, C. The origin of breast tumor heterogeneity. Oncogene 34, 5309–5316 (2015).
Koren, S. & Bentires-Alj, M. Breast tumor heterogeneity: source of fitness, hurdle for therapy. Mol. Cell 60, 537–546 (2015).
Lüönd, F., Tiede, S. & Christofori, G. Breast cancer as an example of tumour heterogeneity and tumour cell plasticity during malignant progression. Br. J. Cancer 125, 164–175 (2021).
Huang, J. et al. Global incidence and mortality of breast cancer: a trend analysis. Aging13, 5748–5803 (2021).
Broeders, M. et al. The impact of mammographic screening on breast cancer mortality in Europe: a review of observational studies. J. Med. Screen. 19, 14–25 (2012).
Albeshan, S. M., Almuqbil, M. M., Elsharkawi, M. M., Nassri, H. & Khoumais, N. A. Outcomes of the Saudi breast cancer early detection program: a nine-year analysis (2012–2020). Breast Cancer Res. Treat. 211, 185–193 (2025).
Boyd, N. F. et al. Breast tissue composition and susceptibility to breast cancer. JNCI J. Natl. Cancer Inst. 102, 1224–1237 (2010). Aug 18.
Subelack, J. et al. Risk factors for interval breast cancer: insights from a decade of a mammography screening program. Breast Cancer Res. Treat. 211, 23–33 (2025).
Bleyer, A. & Welch, H. G. Effect of three decades of screening mammography on breast-cancer incidence. N. Engl. J. Med. 367, 1998–2005 (2012).
Loke, S. Y. & Lee, A. S. G. The future of blood-based biomarkers for the early detection of breast cancer. Eur. J. Cancer 92, 54–68 (2018).
Zou, R. et al. Development and validation of a circulating microRNA panel for the early detection of breast cancer. Brit. J. Cancer126, 472–481 (2022).
Hayes, J., Peruzzi, P. P. & Lawler, S. MicroRNAs in cancer: biomarkers, functions and therapy. Trends Mol. Med. 20, 460–469 (2014).
Cohen, J. D. et al. Detection and localization of surgically resectable cancers with a multi-analyte blood test. Science 359, 926–930 (2018).
Garcia, S. J., Mike E. V., Zhang J., Cuda C. M. & Putterman C. Patterns of immune evasion in triple-negative breast cancer and new potential therapeutic targets: a review. Front. Immunol. 15, 1466868 (2024).
Muramatsu, T. Basigin (CD147), a multifunctional transmembrane glycoprotein with various binding partners. J. Biochem. 159, 481–490 (2016).
Kataoka, H. et al. Tumor cell-derived collagenase-stimulatory factor increases expression of interstitial collagenase, stromelysin, and 72-kDa gelatinase. Cancer Res. 13, 3157–3158 (1996).
Chitra, B. et al. The human tumor cell-derived collagenase stimulatory factor (Renamed EMMPRIN) is a member of the immunoglobulin superfamily. Cancer Res. 55, 434–439 (1995).
Biswas, C. Tumor cell stimulation of collagenase production by fibroblasts. Biochem. Biophys. Res. Commun. 109, 1026–1034 (1982).
Guo, H. et al. Characterization of the gene for human EMMPRIN, a tumor cell surface inducer of matrix metalloproteinases. Gene 220, 99–108 (1998).
DeCastro, R. et al. Human Keratinocytes Express EMMPRIN, an Extracellular Matrix Metalloproteinase Inducer. J. Invest. Dermatol. 106, 1260–1265 (1996).
Biswas, C. & Nugent, M. A. Membrane association of collagenase stimulatory factor(s) from B-16 melanoma cells. J. Cell. Biochem. 35, 247–258 (1987).
Biswas, C. Tumor cell stimulation of collagenase production by fibroblasts. Biochem. Biophys. Res. Commun. 109, 1026–1034 (1982). /12/15.
Nabeshima, K., Biswas, C. & Ellis, S. M. Monoclonal antibody preparation and purification of a tumor cell collagenase-stimulatory factor. Cancer Res. 49, 3385–3391 (1989).
Xiong, L., Edwards, I. C. arlK. & Zhou, L. The biological function and clinical utilization of CD147 in human diseases: a review of the current scientific literature. Int. J. Mol. Sci. 15, 17411–17441 (2014). Sep 29.
Nyalali, A. M. K. et al. CD147: an integral and potential molecule to abrogate hallmarks of cancer. Front. Oncol. 13, 1238051 (2023).
Landras, A. et al. CD147 is a promising target of tumor progression and a prognostic biomarker. Cancers 11, 1803–1803 (2019).
Wang, J., Chen, J. & Sen, S. microRNA as biomarkers and diagnostics. J. Cell. Physiol. 231, 25–30 (2016).
Wang, J., Zhang, K. Y., Liu, S. M. & Sen, S. Tumor-associated circulating microRNAs as biomarkers of cancer. Molecules 19, 1912–1938 (2014).
Fogazzi, V. et al. The role of MicroRNAs in HER2-positive breast cancer: where we are and future prospective. Cancers14, 5326 (2022).
Iorio, M.V. et al. MicroRNA gene expression deregulation in human breast cancer. Cancer Res. 65, 7065–7070 (2005).
Richard, V. et al. MicroRNAs in molecular classification and pathogenesis of breast tumors. Cancers 13, 5332 (2021).
Richard, V. et al. Cell state transitions and phenotypic heterogeneity in luminal breast cancer implicating MicroRNAs as potential regulators. Int. J. Mol. Sci. 24, 3497 (2023).
Serpico, D., Molino, L. & Cosimo, S. D. microRNAs in breast cancer development and treatment. Cancer Treat. Rev. 40, 595–604 (2014).
Schwarzenbach, H., Nishida, N., Calin, G. A. & Pantel, K. Clinical relevance of circulating cell-free microRNAs in cancer. Nat. Rev. Clin. Oncol. 11, 145–156 (2014).
Wu, D., Thompson, L. U. & Comelli, E. M. MicroRNAs: a link between mammary gland development and breast cancer. Int. J. Mol. Sci. 23, 15978 (2022).
Condrat, C. E. et al. miRNAs as biomarkers in disease: latest findings regarding their role in diagnosis and prognosis. Cells 9, 276 (2020).
Kent, O. A. & Mendell, J. T. A small piece in the cancer puzzle: microRNAs as tumor suppressors and oncogenes. Oncogene 25, 6188–6196 (2006).
Kumar, T. et al. A spatially resolved single-cell genomic atlas of the adult human breast. Nature 620, 181–191 (2023).
Wang, C. et al. MiR-890 inhibits proliferation and invasion and induces apoptosis in triple-negative breast cancer cells by targeting CD147. BMC Cancer 19, 577 (2019).
Kong, L.M. et al. A regulatory loop involving miR-22, Sp1, and c-Myc modulates CD147 expression in breast cancer invasion and metastasis. Cancer Res. 74, 3764–3748 (2014).
Xu, D. et al. miR-22 represses cancer progression by inducing cellular senescence. J. Cell Biol. 193, 409–424 (2011). /04/18.
Orrantia-Borunda, E. et al. Subtypes of Breast Cancer. In Breast Cancer (ed HN, M.) Exon Publications: Brisbane (AU, 2022).
Perou, C. M. et al. Molecular portraits of human breast tumours. Nature 406, 747–752 (2000).
Brenton, J. D., Carey L. A., Ahmed A. A. & Caldas C. Molecular classification and molecular forecasting of breast cancer: ready for clinical application? J. Clin. Oncol. 23, 7350–7360 (2005).
Santagata, S. et al. Taxonomy of breast cancer based on normal cell phenotype predicts outcome. J. Clin. Investig. 124, 859–870 (2014).
Cardiff, R. D. & Borowsky, A. D. At last: classification of human mammary cells elucidates breast cancer origins. J. Clin. Investig. 124, 478–480 (2014).
Mathews, J. C. et al. Robust and interpretable PAM50 reclassification exhibits survival advantage for myoepithelial and immune phenotypes. npj Breast Cancer 5, 30 (2019).
Parker, J. S. et al. Supervised risk predictor of breast cancer based on intrinsic subtypes. J. Clin. Oncol. 27, 1160–1167 (2009).
Prat, A. et al. Phenotypic and molecular characterization of the claudin-low intrinsic subtype of breast cancer. Breast Cancer Res. BCR 12, 68 (2010).
Prat, A. & Perou, C. M. Deconstructing the molecular portraits of breast cancer. Mol. Oncol. 5, 5–23 (2010).
Bach, K. et al. Differentiation dynamics of mammary epithelial cells revealed by single-cell RNA sequencing. Nat. Commun. 8, 2128 (2017).
Mendoza, G., Portillo, A. & Olmos-Soto, J. Accurate breast cancer diagnosis through real-time PCR HER-2 gene quantification using immunohistochemically-identified biopsies. Oncol. Lett. 5, 295–298 (2012).
Ayatollahi, H. et al. Chromogenic in situ hybridization compared with real time quantitative polymerase chain reaction to evaluate HER2/neu status in breast cancer. Iran. J. Pathol. 12, 128–134 (2017).
Søkilde, R. et al. Refinement of breast cancer molecular classification by miRNA expression profiles. BMC Genomics 20, 503 (2019).
Ali, K. et al. Recent developments in targeting breast cancer stem cells (BCSCs): a descriptive review of therapeutic strategies and emerging therapies. Med. Oncol. 41, 112 (2024).
Jiang, H. Latest research progress of liquid biopsy in tumor-a narrative review. Cancer Manag. Res. 16, 1031–1042 (2024).
Goetz, L. H. & Schork, N. J. Personalized medicine: motivation, challenges and progress. Fertil. Steril. 109, 952–963 (2018).
Seong, H., Izutsu, R., Osaki, M. & Okada, F. Cancer prevention: past challenges and future directions. Genes Environ. 47, 4 (2025).
Singh, D. et al. Personalized medicine: an alternative for cancer treatment. Cancer Treat. Res. Commun. 42, 100860 (2024).
Ho, D. et al. Enabling technologies for personalized and precision medicine. Trends Biotechnol. 38, 497–518 (2020).
Lopez-Gonzalez, L. et al. Exploring biomarkers in breast cancer: hallmarks of diagnosis, treatment, and follow-up in clinical practice. Medicina 60, 168 (2024).
Souza, K. C. B. et al. Identification of cell-free circulating MicroRNAs for the detection of early breast cancer and molecular subtyping. J. Oncol. 2019, 8393769 (2019).
Thery, L. et al. Circulating tumor cells in early breast cancer. JNCI Cancer Spectr. 3, 026 (2019).
Krützfeldt, J., Poy, M. N. & Stoffel, M. Strategies to determine the biological function of microRNAs. Nat. Genet. 38, 14–19 (2006).
Rupaimoole, R., Han, H. D., Lopez-Berestein, G. & Sood, A. K. MicroRNA therapeutics: principles, expectations, and challenges. Chin. J. Cancer 30, 368–370 (2011).
Lybaert, L. et al. Challenges in neoantigen-directed therapeutics. Cancer Cell 41, 15–40 (2023).
van Amerongen, R. et al. Imagine beyond: recent breakthroughs and next challenges in mammary gland biology and breast cancer research. J. Mammary Gland Biol. Neoplasia 28, 17 (2023).
Pan, H. et al. 20-year risks of breast-cancer recurrence after stopping endocrine therapy at 5 years. N. Engl. J. Med. 377, 1836–1846 (2017).
Havas, K. M. et al. Metabolic shifts in residual breast cancer drive tumor recurrence. J. Clin. Investig. 127, 2091–2105 (2017).
Shastry, M., Jacob, S., Rugo, H. S. & Hamilton, E. Antibody-drug conjugates targeting TROP-2: clinical development in metastatic breast cancer. Breast 66, 169–177 (2022).
Di Gioia, D. et al. Serum HER2 in combination with CA 15-3 as a parameter for prognosis in patients with early breast cancer. Clin. Chim. Acta 440, 16–22 (2015).
Ishibashi, Y. et al. Serum TFF1 and TFF3 but not TFF2 are higher in women with breast cancer than in women without breast cancer. Sci. Rep. 7, 4846 (2017).
Kong, L.-M. et al. Promoter hypomethylation up-regulates CD147 expression through increasing Sp1 binding and associates with poor prognosis in human hepatocellular carcinoma. J. Cell. Mol. Med. 15, 1415–1428 (2011).
Bandu, R., Oh, J. W. & Kim, K. P. Extracellular vesicle proteins as breast cancer biomarkers: Mass spectrometry-based analysis. Proteomics 24, 2300062 (2024).
Polette, M. et al. Tumor collagenase stimulatory factor (TCSF) expression and localization in human lung and breast cancers. J. Histochem. Cytochem.45, 703–709 (1997).
Muramatsu, T. & Miyauchi, T. Basigin (CD147): a multifunctional transmembrane protein involved in reproduction, neural function, inflammation and tumor invasion. Histol. Histopathol. 18, 981–987 (2003).
Kaname, T. et al. Mapping basigin (BSG), a member of the immunoglobulin superfamily, to 19p13.3. Cytogen. Genome Res. 64, 195–197 (1993).
Li, Y. et al. HAb18G (CD147), a cancer-associated biomarker and its role in cancer detection. Histopathology 54, 677–687 (2009).
Grass, G. D., Tolliver, L. B., Bratoeva, M. & Toole, B. P. CD147, CD44, and the epidermal growth factor receptor (EGFR) signaling pathway cooperate to regulate breast epithelial cell invasiveness. J. Biol. Chem. 288, 26089–26104 (2013).
Asgari, R. et al. CD147 and MMPs as key factors in physiological and pathological processes. Biomed. Pharmacother. 157, 113983 (2023).
Nabeshima, K. et al. Emmprin (basigin/CD147): matrix metalloproteinase modulator and multifunctional cell recognition molecule that plays a critical role in cancer progression. Pathol. Int. 56, 359–367 (2006).
Park, S. J. et al. An overview of MCT1 and MCT4 in GBM: small molecule transporters with large implications. Am. J. Cancer Res. 8, 1967–1967 (2018).
Kirk, P. et al. CD147 is tightly associated with lactate transporters MCT1 and MCT4 and facilitates their cell surface expression. EMBO J. 19, 3896–3896 (2000).
Richard, V. et al. Multiple drug resistant, tumorigenic stem-like cells in oral cancer. Cancer Lett. 338, 300–316 (2013).
Dai, L. et al. CD147-dependent heterogeneity in malignant and chemoresistant properties of cancer cells. Am. J. Pathol. 182, 577–585 (2013).
Li, F., Wang, J., Yan, Y. Q., Bai, C. Z. & Guo, J. Q. CD147 promotes breast cancer migration and invasion by inducing epithelial-mesenchymal transition via the MAPK/ERK signaling pathway. BMC Cancer 23, 1214 (2023).
Hanahan, D. Hallmarks of cancer: new dimensions. Cancer Discov. 12, 31–46 (2022).
Hanahan, D. & Weinberg, R. A. Hallmarks of cancer: the next generation. Cell 144, 646–674 (2011).
Hanahan, D. & Weinberg, R. A. The hallmarks of cancer. Cell 100, 57–70 (2000).
Janin, M., Davalos, V. & Esteller, M. Cancer metastasis under the magnifying glass of epigenetics and epitranscriptomics. Cancer Metastasis Rev. 42, 1071–1112 (2023).
Costa, P.M.D.S., et al. Epigenetic reprogramming in cancer: from diagnosis to treatment. Front. Cell Develop. Biol. 11, 1116805 (2023).
Ilango, S. et al. Epigenetic alterations in cancer. Front. Biosci. Landmark 25, 1058–1109 (2020).
Patel, S. A., Rodrigues, P., Wesolowski, L. & Vanharanta, S. Genomic control of metastasis. Br. J. Cancer 124, 3–12 (2020).
Marieb, E. A. et al. Emmprin promotes anchorage-independent growth in human mammary carcinoma cells by stimulating hyaluronan production. Cancer Res. 64, 1229–1232 (2004).
Deng, Z., Wang, H., Liu, J., Deng, Y. & Zhang, N. Comprehensive understanding of anchorage-independent survival and its implication in cancer metastasis. Cell Death Dis. 12, 629 (2021).
Stern, R., Shuster, S., Neudecker, B. A. & Formby, B. Lactate stimulates fibroblast expression of hyaluronan and CD44: the Warburg effect revisited. Exp. Cell Res. 276, 24–31 (2002).
Grass, G. D., Dai, L., Qin, Z., Parsons, C. & Toole, B. P. CD147: regulator of hyaluronan signaling in invasiveness and chemoresistance. Adv. Cancer Res. 123, 351–373 (2014).
Slomiany, M. G. et al. Hyaluronan, CD44, and emmprin regulate lactate efflux and membrane localization of monocarboxylate transporters in human breast carcinoma cells. Cancer Res. 69, 1293–1301 (2009).
Lavoie, H., Gagnon, J. & Therrien, M. ERK signalling: a master regulator of cell behaviour, life and fate. Nat. Rev. Mol. Cell Biol. 21, 607–632 (2020).
Parnigoni, A. et al. Effects of hyaluronan on breast cancer aggressiveness. Cancers 15, 3813 (2023).
Ghatak, S., Misra, S. & Toole, B. P. Hyaluronan oligosaccharides inhibit anchorage-independent growth of tumor cells by suppressing the phosphoinositide 3-Kinase/Akt cell survival pathway. J. Biol. Chem. 277, 38013–38020 (2002).
Misra, S., Ghatak, S. & Toole, B. P. Regulation of MDR1 expression and drug resistance by a positive feedback loop involving hyaluronan, phosphoinositide 3-kinase, and ErbB2. J. Biol. Chem. 280, 20310–20315 (2005).
Chen, C. et al. The biology and role of CD44 in cancer progression: therapeutic implications. J. Hematol. Oncol. 11, 64 (2018).
Yang, C. et al. The use of HA oligosaccharide-loaded nanoparticles to breach the endogenous hyaluronan glycocalyx for breast cancer therapy. Biomaterials 34, 6829–6838 (2013).
Toole, B. P. & Slomiany, M. G. Hyaluronan, CD44 and emmprin: partners in cancer cell chemoresistance. Drug Resistance Updates Rev. Commentaries Antimicrobial Anticancer Chemother. 11, 110–121 (2008).
Misra, S., Ghatak, S., Zoltan-Jones, A. & Toole, B. P. Regulation of multidrug resistance in cancer cells by hyaluronan. J. Biol. Chem. 278, 25285–25288 (2003).
Toole, B. P. The CD147-hyaluronan axis in cancer. Anat. Rec. 303, 1573–1583 (2020).
Al-Othman, N. et al. Role of CD44 in breast cancer. Breast Dis. 39, 1–13 (2019).
Woods, E. L. et al. CD147 mediates the CD44s-dependent differentiation of myofibroblasts driven by transforming growth factor-β1. J. Biol. Chem. 297, 100987 (2021).
Grass, G. D. & Toole, B.P. How, with whom and when: an overview of CD147-mediated regulatory networks influencing matrix metalloproteinase activity. Biosci. Rep. 36, e00283 (2016).
Heppner, K. J., Matrisian, L. M., Jensen, R. A. & Rodgers, W. H. Expression of most matrix metalloproteinase family members in breast cancer represents a tumor-induced host response. Am. J. Pathol. 149, 273–282 (1996).
Polette, M. et al. Tumor collagenase stimulatory factor (TCSF) expression and localization in human lung and breast cancers. J. Histochem. Cytochem. Off. J. Histochemistry Soc. 45, 703–709 (1997).
Kwon, M. J. Matrix metalloproteinases as therapeutic targets in breast cancer. Front. Oncol. 12, 1108695 (2023).
Radisky, E. S. & Radisky, D. C. Matrix metalloproteinases as breast cancer drivers and therapeutic targets. Front. Biosci.20, 1144–1163 (2015).
Błaszczak, E. et al. Triple-negative breast cancer progression and drug resistance in the context of epithelial–mesenchymal transition. Cancers 17, 228 (2025).
Martin, M. D. et al. Effect of ablation or inhibition of stromal matrix metalloproteinase-9 on lung metastasis in a breast cancer model is dependent on genetic background. Cancer Res. 68, 6251–6259 (2008).
Grass, G. D., Bratoeva, M. & Toole, B. P. Regulation of invadopodia formation and activity by CD147. J. Cell Sci. 125, 777–788 (2012).
Tang, W. & Hemler, M. E. Caveolin-1 regulates matrix metalloproteinases-1 induction and CD147/EMMPRIN cell surface clustering. J. Biol. Chem. 279, 11112–11118 (2004).
Knutti, N., Kuepper, M. & Friedrich, K. Soluble extracellular matrix metalloproteinase inducer (EMMPRIN, EMN) regulates cancer-related cellular functions by homotypic interactions with surface CD147. FEBS J. 282, 4187–4200 (2015).
Yurchenko, V. et al. Active site residues of cyclophilin A are crucial for its signaling activity via CD147. J. Biol. Chem. 277, 22959–22965 (2002).
Wang, S. et al. High expression level of peptidylprolyl isomerase A is correlated with poor prognosis of liver hepatocellular carcinoma. Oncol. Lett. 18, 4691–4691 (2019).
Wang, X. et al. NQO1 triggers neutrophil recruitment and NET formation to drive lung metastasis of invasive breast cancer. Cancer Res. 84, 3538–3555 (2024).
Han, J. M. & Jung, H. J. Cyclophilin A/CD147 interaction: a promising target for anticancer therapy. Int. J. Mol. Sci. 23, 9341 (2022).
Meng, Y. et al. Detachment activated CyPA/CD147 induces cancer stem cell potential in non-stem breast cancer cells. Front. Cell Develop. Biol. 8, 543856 (2020).
Gallagher, S. M., Castorino, J. J., Wang, D. & Philp, N. J. Monocarboxylate transporter 4 regulates maturation and trafficking of CD147 to the plasma membrane in the metastatic breast cancer cell line MDA-MB-231. Cancer Res. 67, 4182–4189 (2007).
Zucker, S. et al. Tumorigenic potential of extracellular matrix metalloproteinase inducer. Am. J. Pathol. 158, 1921–1928 (2001).
Li, J. J., Tsang, J. Y. & Tse, G. M. Tumor microenvironment in breast cancer—updates on therapeutic implications and pathologic assessment. Cancers 13, 4233 (2021).
Yang, J., Tang, S., Saba, N. F., Shay, C. & Teng, Y. Tumor secretome shapes the immune landscape during cancer progression. J. Exp. Clin. Cancer Res. 44, 47 (2025).
Tang, Y. et al. Extracellular matrix metalloproteinase inducer stimulates tumor angiogenesis by elevating vascular endothelial cell growth factor and matrix metalloproteinases. Cancer Res. 65, 3193–3199 (2005).
Tang, Y. et al. Regulation of vascular endothelial growth factor expression by EMMPRIN via the PI3K-Akt signaling pathway. Mol. Cancer Res. 4, 371–377 (2006).
Chuliá-Peris, L. et al. Matrix metalloproteinases and their inhibitors in pulmonary fibrosis: EMMPRIN/CD147 comes into play. Int. J. Mol. Sci. 23, 6894 (2022).
Bougatef, F. et al. EMMPRIN promotes melanoma cells malignant properties through a HIF-2alpha mediated up-regulation of VEGF-receptor-2. PloS ONE 5, 12265 (2010).
Khayati, F. et al. EMMPRIN/CD147 is a novel coreceptor of VEGFR-2 mediating its activation by VEGF. Oncotarget 6, 9766–9780 (2015).
Tang, Y., Kesavan, P., Nakada, M. T. & Yan, L. Tumor-stroma interaction: positive feedback regulation of extracellular matrix metalloproteinase inducer (EMMPRIN) expression and matrix metalloproteinase-dependent generation of soluble EMMPRIN. Mol. Cancer Res. 2, 73–80 (2004).
Shi, S., et al. CD147 expression as a clinicopathological and prognostic indicator in breast cancer: a meta-analysis and bioinformatics analysis. BMC Cancer 24, 1429 (2024).
Payen, V. L., Mina, E., Van Hée, V. F., Porporato, P. E. & Sonveaux, P. Monocarboxylate transporters in cancer. Mol. Metab. 33, 48–66 (2019).
Philp, N. J. et al. Loss of MCT1, MCT3, and MCT4 expression in the retinal pigment epithelium and neural retina of the 5A11/basigin-null mouse. Invest. Ophthalmol. Vis. Sci. 44, 1305–1311 (2003).
Sun, X., et al. Role of proton-coupled monocarboxylate transporters in cancer: from metabolic crosstalk to therapeutic potential. Front. Cell Develop. Biol. 8, 651 (2020).
Benjamin, D. et al. Dual inhibition of the lactate transporters MCT1 and MCT4 is synthetic lethal with metformin due to NAD+ depletion in cancer cells. Cell Rep. 25, 3047–3058 (2018).
Pinheiro, C. et al. Expression of Monocarboxylate Transporters 1, 2, and 4 in Human Tumours and Their Association with CD147 and CD44. J. Biomed. Biotechnol. 2010, 427694 (2010).
Pinheiro, C. et al. Monocarboxylate transporter 1 is up-regulated in basal-like breast carcinoma. Histopathology 56, 860–867 (2010).
Wilde, L. et al. Metabolic coupling and the reverse warburg effect in cancer: implications for novel biomarker and anticancer agent development. Semin. Oncol. 44, 198–203 (2017).
Meng, S. et al. MCT4 and CD147 colocalize with MMP14 in invadopodia and support matrix degradation and invasion by breast cancer cells. J. Cell Sci. 137, 261608 (2024).
Combs, J. E. et al. Disruption of the physical interaction between carbonic anhydrase IX and the monocarboxylate transporter 4 impacts lactate transport in breast cancer cells. Int. J. Mol. Sci. 25, 11994 (2024).
Jamali, S. et al. Hypoxia-induced carbonic anhydrase IX facilitates lactate flux in human breast cancer cells by non-catalytic function. Sci. Rep. 5, 13605 (2015).
Ames, S., Andring, J. T., McKenna, R. & Becker, H. M. CAIX forms a transport metabolon with monocarboxylate transporters in human breast cancer cells. Oncogene 39, 1710–1723 (2019).
Kevat, S. et al. Cancer stem cell regulation as a target of therapeutic intervention: insights into breast, cervical and lung cancer. Cell Biochem. Biophys. 83, 1521–1535 (2025).
Al-Hajj, M., Wicha, M. S., Benito-Hernandez, A., Morrison, S. J. & Clarke, M. F. Prospective identification of tumorigenic breast cancer cells. Proc. Natl. Acad. Sci. USA 100, 3983–3988 (2003).
Chu, X. et al. Cancer stem cells: advances in knowledge and implications for cancer therapy. Signal Transduct. Target. Ther. 9, 170 (2024).
Li, X. et al. Intrinsic resistance of tumorigenic breast cancer cells to chemotherapy. JNCI J. Natl. Cancer Inst. 100, 672–679 (2008).
Dave, B., Mittal, V., Tan, N. M. & Chang, J. C. Epithelial-mesenchymal transition, cancer stem cells and treatment resistance. Breast Cancer Res. 14, 202 (2012).
Bisht, S. et al. Cancer stem cells: from an insight into the basics to recent advances and therapeutic targeting. Stem Cells Int. 2022, 9653244 (2022).
Zhang, X., Powell, K. & Li, L. Breast cancer stem cells: biomarkers, identification and isolation methods, regulating mechanisms, cellular origin, and beyond. Cancers 12, 3765 (2020).
Jimenez-Tellez, N., et al. Biological implications of MicroRNAs as regulators and biomarkers of therapeutic toxicities in breast cancer. Int. J. Mol. Sci. 24, 12694 (2023).
Lee, R. C., Feinbaum, R. L. & Ambros, V. The C. elegans heterochronic gene lin-4 encodes small RNAs with antisense complementarity to lin-14. Cell 75, 843–854 (1993).
Levantini, E. & Rizzo, M. miRNAs: from master regulators of gene expression to biomarkers involved in intercellular communication. Biomedicines 12, 721 (2024).
Nazarov, P.V. et al. Interplay of microRNAs, transcription factors and target genes: linking dynamic expression changes to function. Nucleic Acids Res. 41, 2817–2831 (2013).
Reinhart, B. J. et al. The 21-nucleotide let-7 RNA regulates developmental timing in Caenorhabditis elegans. Nature 403, 901–906 (2000).
Calin, G. A. et al. Frequent deletions and down-regulation of micro- RNA genes miR15 and miR16 at 13q14 in chronic lymphocytic leukemia. Proc. Natl. Acad. Sci. 99, 15524–15529 (2002).
Esquela-Kerscher, A. & Slack, F. J. Oncomirs — microRNAs with a role in cancer. Nat. Rev. Cancer 6, 259–269 (2006).
Hemmatzadeh, M., Mohammadi, H., Jadidi-Niaragh, F., Asghari, F. & Yousefi, M. The role of oncomirs in the pathogenesis and treatment of breast cancer. Biomed. Pharmacother. 78, 129–139 (2016).
Muñoz, J. P., Pérez-Moreno P., Pérez Y., Calaf G. M. The role of MicroRNAs in breast cancer and the challenges of their clinical application. Diagnostics 13, 3072 (2023).
You, K., Liu, Y., Chen, L., Ye, H. & Lin, W. Radix ranunculus temate saponins sensitizes ovarian cancer to Taxol via upregulation of miR-let-7b. Exp. Therapeutic Med. 23, 315 (2022).
Ma, L., Li, G., Wu, Z. & Meng, G. Prognostic significance of let-7b expression in breast cancer and correlation to its target gene of BSG expression. Med. Oncol. 31, 773 (2013).
Fu, T.Y. et al. Let-7b-mediated suppression of basigin expression and metastasis in mouse melanoma cells. Exp. Cell Res. 317, 445–451 (2011).
Hu, X. et al. The heterochronic microRNA let-7 inhibits cell motility by regulating the genes in the actin cytoskeleton pathway in breast cancer. Mol. Cancer Res. MCR 11, 240–250 (2013).
Zhang, L., Chen, B. & Ding, D. Decreased microRNA-22 is associated with poor prognosis in cervical cancer. Int J. Clin. Exp. Pathol. 10, 9515–9520 (2017).
Pandey, A. K. et al. TIP60-miR-22 axis as a prognostic marker of breast cancer progression. Oncotarget 6, 41290–41306 (2015).
Koufaris, C., Papandreou, M. E., Ellis, J. K., Nicolaidou, V. & Keun, H. C. miR-22-enriched breast cancer cells display repressed glycolytic metabolism, increased glycogen synthesis, and reduced survival in low glucose conditions. Mol. Biol. Rep. 50, 5185–5193 (2023).
Zisman, D. et al. Tocilizumab (TCZ) decreases angiogenesis in rheumatoid arthritis through its regulatory effect on miR-146a-5p and EMMPRIN/CD147. Front. Immunol. 12, 739592 (2021).
Zisman, D. et al. Tofacitinib regulates endostatin via effects on CD147 and cathepsin S. Int. J. Mol. Sci. 25, 7267 (2024).
Rahat, M. M. et al. Soluble CD147 regulates endostatin via its effects on the activities of MMP-9 and secreted proteasome 20S. Front. Immunol. 15, 1319939 (2024).
Li, L. et al. HAb18G/CD147 promotes pSTAT3-mediated pancreatic cancer development via CD44s. Clin. Cancer Res. 19, 6703–6715 (2013).
Chen, T. & Zhu, J. Evaluation of EMMPRIN and MMP-2 in the prognosis of primary cutaneous malignant melanoma. Med. Oncol. 27, 1185–1191 (2010).
Xu, Y.-J., He, H. J., Wu, P. & Li, W. B. Expression patterns of cluster of differentiation 147 impact the prognosis of hepatocellular carcinoma. World J. Gastrointest. Oncol. 15, 1412–1423 (2023).
Xiong, W. & Deng, Y. BSG Isoform 2 (ENST00000353555) is a better component than total BSG expression in generating prognostic signature for overall survival of liver cancer. Cureus 16, 62287 (2024).
Bovenzi, C. D. et al. Prognostic indications of elevated MCT4 and CD147 across cancer types: a meta-analysis. BioMed. Res. Int. 2015, 242437 (2015).
Fan, H., Yi, W., Wang, C. & Wang, J. The clinicopathological significance and prognostic value of EMMPRIN overexpression in cancers: evidence from 39 cohort studies. Oncotarget 8, 82643–82660 (2017).
Zhang, J. et al. Large-scale single-cell and bulk sequencing analyses reveal the prognostic value and immune aspects of CD147 in pan-cancer. Front. Immunol. 13, 810471 (2022).
Xin, X. et al. CD147/EMMPRIN overexpression and prognosis in cancer: a systematic review and meta-analysis. Sci. Rep. 6, 1–12 (2016).
Wang, H. et al. CD44+/CD24− phenotype predicts a poor prognosis in triple-negative breast cancer. Oncol. Lett. 14, 5890–5898 (2017).
Chen, M., Liu, Z., Zheng, K., Hu, C. & Peng, P. The potential mechanism of HIF-1α and CD147 in the development of triple-negative breast cancer. Medicine 103, e38434 (2024).
Bai, Y., Huang, W., Ma, L. T., Jiang, J. L. & Chen, Z. N. Importance of N-Glycosylation on CD147 for Its Biological Functions. Int. J. Mol. Sci. 15, 6356–6377 (2014).
Wang, S.-J. et al. CD147 promotes collective invasion through cathepsin B in hepatocellular carcinoma. J. Exp. Clin. Cancer Res. 39, 145 (2020).
Dana, P. et al. CD147 augmented monocarboxylate transporter-1/4 expression through modulation of the Akt-FoxO3-NF-κB pathway promotes cholangiocarcinoma migration and invasion. Cell. Oncol. 43, 211–222 (2020).
Zhang, N., Liu, Z., Lai, X., Liu, S. & Wang, Y. Silencing of CD147 inhibits cell proliferation, migration, invasion, lipid metabolism dysregulation and promotes apoptosis in lung adenocarcinoma via blocking the Rap1 signaling pathway. Respiratory Res. 24, 253 (2023).
Ko, S. Y. et al. The glycoprotein CD147 defines miRNA-enriched extracellular vesicles that derive from cancer cells. J. Extracell. Vesicles 12, 12318 (2023).
Lee, Y.-J., Chae, S. & Choi, D. Monitoring of single extracellular vesicle heterogeneity in cancer progression and therapy. Front. Oncol. 13, 1256585 (2023).
Yin, B. et al. Harnessing microRNA-enriched extracellular vesicles for liquid biopsy. Front. Mol. Biosc. 11, 1356780 (2024).
Lee, Y. et al. Recent advances of small extracellular vesicle biomarkers in breast cancer diagnosis and prognosis. Mol. Cancer 22, 33 (2023).
Yoshioka, Y. et al. Ultra-sensitive liquid biopsy of circulating extracellular vesicles using ExoScreen. Nat. Commun. 5, 3591 (2014).
Liu, F. et al. Expression of HAb18G is associated with tumor progression and prognosis of breast carcinoma. Breast Cancer Res. Treat. 124, 677–688 (2010).
Lakshmi, S., Hughes, T. A. & Priya, S. Exosomes and exosomal RNAs in breast cancer: a status update. Eur. J. Cancer 144, 252–268 (2021).
Saliminejad, K., Khorshid, H. R. K. & Ghaffari, S. H. Why have MicroRNA biomarkers not been translated from bench to clinic? Future Oncol. 15, 801–803 (2019).
Liu, B., Zhou, H., Tan, L., Siu, K. T. H. & Guan, X. Y. Exploring treatment options in cancer: tumor treatment strategies. Signal Transduct. Target. Ther. 9, 175 (2024).
Huang, H. et al. Trends in the incidence and survival of women with hormone receptor-positive breast cancer from 1990 to 2019: a large population-based analysis. Sci. Rep. 14, 23690 (2024).
Rahat, M. A. Mini-review: can the metastatic cascade be inhibited by targeting CD147/EMMPRIN to prevent tumor recurrence? Front. Immunol. 13, 855978 (2022).
Tang, W., Chang, S. B. & Hemler, M. E. Links between CD147 function, glycosylation, and caveolin-1. Mol. Biol. Cell 15, 4043–4050 (2004).
Patani, N. et al. The role of caveolin-1 in human breast cancer. Breast Cancer Res. Treatment 131, 1–15 (2011).
Seo, Y. R. et al. Lateral interactions between CD276 and CD147 are essential for stemness in breast cancer: a novel insight from proximal proteome analysis. Sci. Rep. 13, 14242 (2023).
Fu, Z., Li, S., Han, S., Shi, C. & Zhang, Y. Antibody drug conjugate: the “biological missile” for targeted cancer therapy. Signal Transduct. Target. Ther. 7, 93 (2022).
Rummel, S., Valente, A. L., Kane, J. L., Shriver, C. D. & Ellsworth, R. E. Genomic (In)stability of the breast tumor microenvironment. Mol. Cancer Res. 10, 1526–1531 (2012).
Abdollahpour-Alitappeh, M. et al. Antibody–drug conjugates (ADCs) for cancer therapy: strategies, challenges, and successes. J. Cell. Physiol. 234, 5628–5642 (2019).
Shastry, M. et al. Rise of antibody-drug conjugates: the present and future. Am. Soc. Clin. Oncol. Educ. Book 43, 390094 (2023).
Wu, J. et al. HAb18G/CD147 promotes epithelial–mesenchymal transition through TGF-β signaling and is transcriptionally regulated by Slug. Oncogene 30, 4410–4427 (2011).
Xu, J. et al. HAb18G/CD147 functions in invasion and metastasis of hepatocellular carcinoma. Mol. Cancer Res. 5, 605–614 (2007).
Chen, Z. N. et al. Targeting radioimmunotherapy of hepatocellular carcinoma with iodine (131I) metuximab injection: clinical Phase I/II trials. Int. J. Radiat. Oncol.*Biol.*Phys. 65, 435–444 (2006).
Li, J. et al. Adjuvant 131I-metuximab for hepatocellular carcinoma after liver resection: a randomised, controlled, multicentre, open-label, phase 2 trial. Lancet Gastroenterol. Hepatol. 5, 548–560 (2020).
Ku, X.-M. et al. Epitope mapping of series of monoclonal antibodies against the hepatocellular carcinoma-associated Antigen HAb18G/CD147. Scand. J. Immunol. 65, 435–443 (2007).
Yu, X.-L. et al. Crystal structure of HAb18G/CD147: implications for immunoglobulin superfamily homophilic adhesion. J. Biol. Chem. 283, 18056–18065 (2008).
Chen, H. et al. Hepatic artery injection of 131I-metuximab combined with transcatheter arterial chemoembolization for unresectable hepatocellular carcinoma: a prospective nonrandomized, multicenter clinical trial. J. Nucl. Med. 63, 556–556 (2022).
Ma, X. K. et al. 124I-labeled anti-CD147 antibody for noninvasive detection of CD147-positive pan-cancers: construction and preclinical studies. Acta Pharmacologica Sin. 45, 436–448 (2023).
de Goeij, B. E. et al. Efficient payload delivery by a bispecific antibody–drug conjugate targeting HER2 and CD63. Mol. Cancer Therapeutics 15, 2688–2697 (2016).
Yamazaki, C. M. et al. Antibody-drug conjugates with dual payloads for combating breast tumor heterogeneity and drug resistance. Nat. Commun. 12, 3528 (2021).
Bourguignon, L. Y. W., Xia, W. & Wong, G. Hyaluronan-mediated CD44 interaction with p300 and SIRT1 regulates β-catenin signaling and NFκB-specific transcription activity leading to MDR1 and Bcl-xL gene expression and chemoresistance in breast tumor cells. J. Biol. Chem. 284, 2657–2671 (2009).
Saito, S., et al. Biomarkers of cancer stem cells for experimental research and clinical application. J. Personalized Med. 12, 715 (2022).
Chaffer, C. L. et al. Normal and neoplastic nonstem cells can spontaneously convert to a stem-like state. Proc. Natl. Acad. Sci. USA 108, 7950–7955 (2011).
Pályi-Krekk, Z. et al. Hyaluronan-induced masking of ErbB2 and CD44-enhanced trastuzumab internalisation in trastuzumab resistant breast cancer. Eur. J. Cancer 43, 2423–2433 (2007).
Almási, S. et al. The prognostic value of stem cell markers in triple-negative breast cancer. Pathol. Oncol. Res. 29, 1611365 (2023).
Wilson, M. C. et al. Basigin (CD147) is the target for organomercurial inhibition of monocarboxylate transporter isoforms 1 and 4: the ancillary protein for the insensitive MCT2 is EMBIGIN (gp70). J. Biol. Chem. 280, 27213–27221 (2005).
Spinello, I. et al. The small-molecule compound AC-73 targeting CD147 inhibits leukemic cell proliferation, induces autophagy and increases the chemotherapeutic sensitivity of acute myeloid leukemia cells. Haematologica 104, 973–985 (2018).
Kanekura, T. CD147/basigin is involved in the development of malignant tumors and T-Cell-mediated immunological disorders via regulation of glycolysis. Int. J. Mol. Sci. 24, 17344 (2023).
Koltai, T. & Fliegel, L. Exploring monocarboxylate transporter inhibition for cancer treatment. Explor. Target. Anti-tumor Ther. 5, 135–169 (2024).
Gallagher, S. M., Castorino, J. J. & Philp, N. J. Interaction of monocarboxylate transporter 4 with β1-integrin and its role in cell migration. Am. J. Physiol. - Cell Physiol. 296, 414–421 (2008).
Romero-Cordoba, S. L. et al. Loss of function of miR-342-3p results in MCT1 over-expression and contributes to oncogenic metabolic reprogramming in triple negative breast cancer. Sci. Rep. 8, 12252 (2018).
Li, F. et al. RNA interference targeting CD147 inhibits metastasis and invasion of human breast cancer MCF-7 cells by downregulating MMP-9/VEGF expression. Acta Biochimica et. Biophysica Sin. 50, 676–684 (2018).
Sikder, S., Bhattacharya, A., Agrawal, A., Sethi, G. & Kundu, T. K. Micro-RNAs in breast cancer progression and metastasis: a chromatin and metabolic perspective. Heliyon 10, 38193 (2024).
Hackshaw, M. D. et al. Incidence of pneumonitis/interstitial lung disease induced by HER2-targeting therapy for HER2-positive metastatic breast cancer. Breast Cancer Res. Treat. 183, 23–39 (2020).
Powell, C. A. et al. 289P Risk factors for interstitial lung disease in patients treated with trastuzumab deruxtecan from two interventional studies. Ann. Oncol. 31, S357–S358 (2020).
Jin, Y., Schladetsch, M. A., Huang, X., Balunas, M. J. & Wiemer, A. J. Stepping forward in antibody-drug conjugate development. Pharmacol. Therapeutics 229, 107917 (2022).
Dostalek, M., Gardner, I., Gurbaxani, B. M., Rose, R. H. & Chetty, M. Pharmacokinetics, pharmacodynamics and physiologically-based pharmacokinetic modelling of monoclonal antibodies. Clin. Pharmacokin.52, 83–124 (2013).
Wei, Q. et al. The promise and challenges of combination therapies with antibody-drug conjugates in solid tumors. J. Hematol. Oncol. 17, 1 (2024).
Kondrashov, A., et al. Antibody-drug conjugates in solid tumor oncology: an effectiveness payday with a targeted payload. Pharmaceutics 15, 2160 (2023).
Takakura, T., Shimizu, T. & Yamamoto, N. Antibody-drug conjugates in solid tumors; new strategy for cancer therapy. Jpn. J. Clin. Oncol. 54, 837–846 (2024).
Corso, A. D. et al. A non-internalizing antibody-drug conjugate based on an anthracycline payload displays potent therapeutic activity in vivo. J. Control. Rel. 264, 211–218 (2017).
Loganzo, F., Sung, M. & Gerber, H.-P. Mechanisms of resistance to antibody–drug conjugates. Mol. Cancer Therapeutics 15, 2825–2834 (2016).
Mckertish, C. M. & Kayser, V. Advances and limitations of antibody drug conjugates for cancer. Biomedicines 9, 872 (2021).
La Vecchia, C. et al. Cancer mortality in Europe, 2000–2004, and an overview of trends since 1975. Ann. Oncol. 21, 1323–1360 (2010).
Sørlie, T. et al. Gene expression patterns of breast carcinomas distinguish tumor subclasses with clinical implications. Proc. Natl. Acad. Sci. 98, 10869–10874 (2001).
Mohanty, S. S., Sahoo, C. R. & Padhy, R. N. Role of hormone receptors and HER2 as prospective molecular markers for breast cancer: an update. Genes Dis. 9, 648–658 (2022).
Shi, S. et al. CD147 expression as a clinicopathological and prognostic indicator in breast cancer: a meta-analysis and bioinformatics analysis. BMC Cancer 24, 1429 (2024).
Fu, J. et al. Impact of BSG/CD147 gene expression on diagnostic, prognostic and therapeutic strategies towards malignant cancers and possible susceptibility to SARS-CoV-2. Mol. Biol. Rep. 50, 2269–2281 (2022).
Ghandour, F., Kassem, S., Simanovich, E., Rahat, M. A. Glucose promotes EMMPRIN/CD147 and the secretion of pro-angiogenic factors in a co-culture system of endothelial cells and monocytes. Biomedicines 12, 706 (2024).
Wang, J. et al. Melittin inhibits the invasion of MCF‑7 cells by downregulating CD147 and MMP‑9 expression. Oncol. Lett. 13, 599–604 (2017).
Tariq, M., Richard, V. and Kerin, M. J. MicroRNAs as molecular biomarkers for the characterization of basal-like breast tumor subtype. Biomedicines 11, 3007 (2023).
Wang, M. et al. Circulating microRNAs as potential cancer biomarkers: the advantage and disadvantage. Clin. Epigenet.10, 118 (2018).
Jang, J. Y. et al. Multiple microRNAs as biomarkers for early breast cancer diagnosis. Mol. Clin. Oncol. 14, 31 (2020).
Vahed, S. Z., et al. A microRNA isolation method from clinical samples. Bioimpacts 6, 25–31 (2016).
Shirshova, A. N., Shamovskaya, D. A., Boyarskikh, U. A., Kushlinskii, N. E. & Filipenko, M. L. One-phase phenol-free method for microRNA isolation from blood plasma. MethodsX 5, 737–743 (2018).
Ramshani, Z. et al. Extracellular vesicle microRNA quantification from plasma using an integrated microfluidic device. Commun. Biol. 2, 189 (2019).
Diefenbach, R. J., Lee, J. H., Kefford, R. F. & Rizos, H. Evaluation of commercial kits for purification of circulating free DNA. Cancer Genet. 228-229, 21–27 (2018).
Bracht, J. et al. Choice of size-exclusion chromatography column affects recovery, purity, and miRNA cargo analysis of extracellular vesicles from human plasma. Extracell. Vesicles Circul. Nucleic Acids 5, 497–508 (2024).
Clarissa, E. M., et al. Digital profiling of tumor extracellular vesicle-associated RNAs directly from unprocessed blood plasma. ACS Nano 19, 5526–5538 (2025).
Timbres, J. et al. DCIS and LCIS: are the risk factors for developing in situ breast cancer different? Cancers 15, 4397 (2023).
Herschkowitz, J. I. et al. Identification of conserved gene expression features between murine mammary carcinoma models and human breast tumors. Genome Biol. 8, 76 (2007).
Wallden, B. et al. Development and verification of the PAM50-based Prosigna breast cancer gene signature assay. BMC Med. Genomics 8, 54 (2015).
Krijgsman, O. et al. A diagnostic gene profile for molecular subtyping of breast cancer associated with treatment response. Breast Cancer Res. Treat. 133, 37–47 (2011).
Paik, S. et al. A multigene assay to predict recurrence of tamoxifen-treated, node-negative breast cancer. N. Engl. J. Med. 351, 2817–2826 (2004).
Veer, L. J. et al. Gene expression profiling predicts clinical outcome of breast cancer. Nature 415, 530–536 (2002).
Cardoso, F. et al. 70-gene signature as an aid to treatment decisions in early-stage breast cancer. N. Engl. J. Med. 375, 717–729 (2016).
Acknowledgements
Figures were generated using BioRender. K.B. and V. R. received Research Assistant and Postdoctoral fellowship support respectively and the research was funded by National Breast Cancer Research Institute (NBCRI), grant number FY24001.
Author information
Authors and Affiliations
Contributions
Conceptualization - V.R. and K.B.; writing—original draft preparation, figure generation - K.B.; writing—review and editing - V.R. and M.J.K.; supervision- V.R. and M.J.K.; project administration- V.R. and M.J.K.; funding acquisition- M.J.K. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Bruce, K., Kerin, M. & Richard, V. The pleiotropic roles of non-hormonal receptor basigin and regulatory microRNAs in breast cancer. npj Breast Cancer 11, 104 (2025). https://doi.org/10.1038/s41523-025-00827-7
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41523-025-00827-7