Abstract
Spaceflight missions represent a new exposome, unpredicted by evolution. Life-threatening agents activate non-specific stress responses involving the psycho-immune-neuroendocrine network. The main molecular pathways regulating this network and those affected by spaceflight exposome/microgravity are reported in various experimental setups. They include gut microbiota-derived metabolites, potentially valuable for countermeasure development. Meaningfully, the application of neuromodulation techniques, like the non-invasive transcutaneous vagal stimulation, for the prevention of pathophysiological alterations related to stress responses, is discussed.
Similar content being viewed by others
Introduction
The immune system (IS) oversees and regulates whole-body homeostasis at many levels. The most recognized function is coordinating the host defense against invading pathogens and, more broadly, against all types of stressors. The concept of the exposome1 aptly encompasses the various agents/stressors, both internal and external to the body, to which the IS must respond in order to prevent or mitigate bodily injuries.
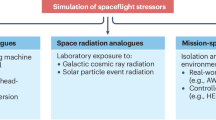
Spaceflight missions, however, present a novel type of exposome that evolution force did not face. These missions have to counteract numerous agents, including psychosocial and physical stressors: G-force variability, exposure to solar particle events and/or galactic cosmic rays, confinement, sleep deprivation, persistent circadian misalignment, and dietary factors, among others. When the organism faces this unique exposome2,3 attempts to cope with it to restore homeostasis4,5 with processes of adaptation or maladaptation6.
IS has a close molecular relationship with the neuroendocrine system, interacting with psychological and cognitive functions. Together, these systems form the Psycho-Immune-Neuro-Endocrine (PINE) network, in which each component can influence the others, ultimately affecting the entire organism. Figures 1 and 2 depict all molecular patterns and signaling able to mediate and regulate the four integrated systems, i.e., IS, Autonomic Nervous System, Psychological and Cognitive function and, Neuro-Endocrine System. In particular, Fig. 2 depicts the classical activation of the stress system, which is located in the central nervous system (amygdala, limbic system), whose major effectors are the Hypothalamic-Pituitary-Adrenal (HPA) axis and the Autonomic Nervous System (ANS)7.
All the involved molecular signaling is depicted to highlight the pathways that may be modulated to counteract or adapt the spaceflight exposome/microgravity effects. Red color for endogenous signaling with examples of mediators inside the parenthesis. HPA axis activation with Autonomic Nervous System interaction is described in the Fig. 2. HPA Hypothalamic-Pituitary-Adrenal axis, CRH corticotropin-releasing hormone, ACTH adrenocorticotropic hormone, VIP vasoactive intestinal peptide, NPY Neuropeptide Y, AEA anandamide, 2-AG 2-arachidonoylglycerol.
HPA is activated in response to physical, emotional, or environmental stressors. The hypothalamus detects stress through sensory inputs and integrates signals from the limbic system (emotional processing). It releases CRH (corticotropin-releasing hormone) and AVP (arginine vasopressin) into the hypophyseal portal system. CRH and AVP stimulate the anterior pituitary to secrete ACTH (adrenocorticotropic hormone) into the bloodstream. ACTH targets the adrenal cortex, prompting the release of glucocorticoids (e.g., cortisol in humans). Cortisol helps mobilize energy by increasing glucose availability, suppressing non-essential functions (like digestion and immunity), and facilitating adaptation to stress. The ANS (Autonomic Nervous System), particularly the SNS (Sympathetic Nervous System), is the body’s rapid-response system during stress. It closely interacts with the HPA axis. Stress triggers the hypothalamus to activate the SNS. The SNS stimulates the adrenal medulla to release catecholamines (e.g., adrenaline and noradrenaline). Catecholamines cause immediate physiological changes: increased heart rate, blood pressure, pupil dilation, and energy mobilization (the “fight or flight” response). Catecholamines can modulate hypothalamic activity, influencing CRH release. Similarly, glucocorticoids can enhance or suppress SNS activity depending on the context. The SNS provides a quick response, while the HPA axis sustains the stress response over minutes to hours. After the stressor is resolved, the PNS (Parasympathetic Nervous System) counteracts the SNS, promoting “rest and digest” functions. Glucocorticoid feedback to the hypothalamus and pituitary inhibits the HPA axis, facilitating recovery. The prefrontal cortex, involved in stress regulation, also responds to endocannabinoid signaling to modulate HPA axis activity, enhancing adaptive responses to stress.
This review explores the emerging and recently identified effects of short- and long-term spaceflight exposome/microgravity (SEM). Specifically, studies on in vivo and in vitro models, both on ground and in Low Earth Orbit (LEO), which focus on the effects on PINE network, are considered, highlighting valuable convergences with gut microbiota-derived signaling.
The activation of the Psycho-ImmunoNeuroEndocrine (PINE) system
Spaceflight exposome represents life-threatening and synergic stressors that require new modalities of adaptation8,9,10,11. Exposure to any stressor, irrespective of its nature, activates an undifferentiated physiological pattern to cope with the threat, the so-called “General Adaptation Syndrome”12. In the first phase, the brain’s amygdala, which is involved in emotional processing, sends a distress signal to the hypothalamus, inducing a massive activation of the HPA axis and the sympathetic branch of the ANS, called the Sympathetic Nervous System (SNS)13 (Fig. 2). This activation is essential for survival, as it enables the mobilization of resources necessary to counteract the stressor through the corticosteroid release by the HPA axis. As a consequence, there is an acceleration of heart rate, increase in blood pressure, increase in breathing rate and pattern, and activation of the inflammatory response, via SNS activation14, that tightly depend on type, duration, and intensity of stressors, with a different effect on PINE system and particularly immune system15. If the threat has been effectively counteracted, the body returns to a pre-stress condition. On the contrary, if the stressor is still present, this prolonged or repeated activation loses its biological value, becoming pathological16 and inducing the so-called “resistance phase”: the body remains in a state of activation, eventually adapting to a higher-than-usual level of metabolic and physiological functioning. Thus, it sets a new level of homeostasis, which, however, is too costly to be maintained17, running out all the organism’s physical and mental resources12. This dysregulation may lead to an increased risk of chronic, cardiovascular, or neuropsychiatric disease18,19,20. In particular, a sustained activation of SNS, without an effective counteraction by the parasympathetic branch of the autonomic nervous system (called PNS), and a steadly increased cytokine production leads to increased cardiovascular morbidity and mortality21, anxiety and depression22, as well as to immune dysregulation17,23.
The complexity of this integrated system places it at the center of homeostasis, allowing it to counteract stress responses of varying intensities and durations, whatever is the stressor. Recent data from animal models and human studies suggest a close relationship between this system and gut microbiota signaling24. This relationship enhances the modulation of PINE activation and regulation, as discussed later in this review. In this context, part of the integrated system will be reviewed as a target of the spaceflight exposome.
Effects of spaceflight exposome/microgravity on the immune system signaling
Accumulated evidence has convincingly demonstrated that SEM significantly impacts on the immune response, by acting on both innate and adaptive immunity. SEM may affect all cells that participate in the inflammatory response, as it modulates the soluble mediators released by them, such as cytokines/chemokines and bioactive lipids6. Additionally, membrane molecules, such as MHC class I molecules, crucial for immune response, exhibited long-term suppression25. Some alterations also became apparent upon acute exposure to SEM, and recovered afterwards, as suggested by investigations showing that reduced interferon (IFN)-γ production from T cells was associated only with short duration flights (i.e., on the Space shuttle), while being absent in long-term missions (i.e., on board the International Space Station, ISS)26. Interestingly, a system biology-based meta-analysis of published data has shown that SEM acts on the different cells involved in inflammation, by acting on a core signature of roughly 100 conserved signaling pathways27. In particular, repression of the tumor necrosis factor (TNF)-α/NF-kB/Rel transduction axis, as well as of T-cell receptor (TCR)-mediated signals, was found in omics array datasets of various studies28,29. Moreover, SEM impairs immune tolerance by significantly enhancing the production of inflammatory cytokines, such as IFN-γ and IL-17, the latter molecule being engaged in the pathogenesis of autoimmune conditions30,31. This effect apparently depends on the depletion of T regulatory (Treg) cells through the repression of the IL-2/CD25 axis31. Interestingly, the number of the latter cells has been recently found to be unaffected by confinement alone32. This evidence suggests that confinement is unlikely to trigger, per se, Treg cell number reduction observed in space31.
SEM can also act on the processes that orchestrate inflammation and its resolution, a rather complex series of events that are schematically depicted in Fig. 3. Indeed, SEM impairs macrophage differentiation and overall polarization33 and alters complement system activation34, while eliciting metabolic reprogramming and altering cytokine production33. Recent studies have also reported a direct effect of SEM on endothelial cells, with a down-regulation of adhesion molecules responsible for the recruitment of immunocytes at the inflamed site35, as well as the activation of iNOS/NO-NF-κB/IκB and the NLRP3 inflammasome signaling pathway in vitro cell model with simulated microgravity36. In this context, SEM can also affect membrane fluidity37, modifying membrane microdomain (e.g., lipid raft) distribution and signaling thereof, which in turn might lead to the production of pro-inflammatory mediators, most notably bioactive lipids and cytokines.
Upon tissue injury or trauma, pathogens penetrate the organism via the disrupted endothelium. LTB4 and a number of specific PGs are first produced from arachidonic acid as part of the vascular response, and PMNs migrate towards the site of injury. During the acute inflammatory cascade, the production of lipid mediators shifts from LTs and PGs—made by neutrophils, platelets, and pro-inflammatory MФ—to lipoxins—by neutrophils, platelets, and pro-resolving/efferocytic MФ (a process called “lipid mediators class switch process”). As a consequence, non-inflammatory monocytes and MФ are recruited, which produce SPMs and LXs as crucial lipid signals for efferocytosis, i.e., removal by MФ of apoptotic cells - the key process for resolution of inflammation. Additionally, within the bloodstream, LXA4 controls MCP-1 and prevents the LTB4-dependent PMNs migration, thus creating an anti-inflammatory milieu. Whenever the resolutive process fails and/or PGs and LTs production is excessive, chronic inflammation takes place. Thus, PGD2 is synthesized in the attempt to transition from a chronic process to a resolutive one. PGD2 has indeed the ability to bind to and activate the DP1 receptor, which causes the release of IL-10, a well-known cytokine with anti-inflammatory properties. Alternatively, PGD2 can be converted into PGJ2, which directly binds to PPARγ and prevents the synthesis of pro-inflammatory mediators, in order to restore homeostasis. LTB4 leukotriene B4, PG prostaglandin, PMN polymorphonucleate cell, MФ macrophages, SPM pro-resolving mediator, LXA4 lipoxin A4, MCP-1 (or CCL2) monocyte chemoattractant protein-1, DP1 prostaglandin D2 receptor 1, PPARγ peroxisome proliferator-activated receptor γ, TGF-α/β transforming growth factor α/β, IL-6 interleukin 6, TX thromboxane, PLA2 phospholipase A2, COX cyclooxygenase, RvD1 resolving D1.
SEM can induce atrophy of both bone marrow and thymus, which control generation and maturation of T and B cells38. Even though several groups have recently investigated the molecular mechanisms behind spaceflight-induced immune alterations, the full array of molecular actors behind them remains mostly elusive, with the biggest part of the published literature having focused on cytokines. Instead, the role of endogenous bioactive lipids, which are produced by the cells that orchestrate inflammation39, has been poorly addressed40. These molecules represent the fulcrum of the immune response, governing the initiation, extent, and outcome of the inflammatory event40,41.
In particular, endogenous bioactive lipids can be grouped into five main classes, which include widely investigated molecules like eicosanoids and endocannabinoids (eCBs), as well as other compounds such as specialized pro-resolving mediators (SPMs), sphingolipids, and glycerophospholipids41,42,43,44. These substances are produced by virtually all the cells of the body as major pro-homeostatic factors and, during phlogistic events, they control recruitment, removal, and turnover of the immune cells (Fig. 3), thus attracting growing attention as main drivers of all inflammatory processes. In particular, while proper inflammation is governed by arachidonic acid (AA)-derived eicosanoids (i.e., prostaglandins, leukotrienes and thromboxanes), which control recruitment and activation of pro-inflammatory immune cells, resolution is organized in the aftermath of acute events to control and keep at bay the excessive inflammatory surge, and is mainly controlled by ω-6 polyunsaturated fatty acids (PUFA)-derived SPMs. As the tissue needs to return to physiological conditions, neutrophils, platelets, and non-phlogistic monocytes/macrophages undergo a lipid mediator class switch that leads to the production of SPMs, namely resolvins (Rvs), maresins (MaRs), protectins (PDs), and lipoxins (LXs). These lipid mediators are produced by innate immune cells through the concerted action of 5-, 12-, and 15-lipoxygenase (LOX) on docosahexahenoic, docosapentaenoic, eicosapentaenoic acid (DHA, DPA, EPA, respectively), as well as on AA. As they are produced, SPMs antagonize AA-derived autacoids and pro-inflammatory cytokines, stop the ingress of neutrophils and the activation of pro-inflammatory macrophages and lymphocytes, while inducing macrophage-mediated efferocytosis (i.e., the removal of apoptotic bodies and debris), which is crucial to both avoid aberrant inflammation and to favor trans-cellular biosynthesis of SPMs45. On the other hand, eCBs have been shown to control immune functions both by acting directly on recruitment and activation of lymphocytes and monocytes/macrophages41, as well as by engaging SPM receptors (i.e., GPR18) and inducing SPM production46. Despite the critical role of endogenous lipids in inflammatory homeostasis, the biggest part of SEM-related research has focused on eicosanoids and eCBs40, and showed that microgravity increases leukotriene (LT) B4 biosynthesis and 5-LOX activity. Furthermore, authentic microgravity upregulates the expression of the prominent eCB-biosynthetic enzyme N-acylphosphatidylethanolamines-specific phospholipase D (NAPE-PLD), while downregulating that of the prominent eCB-degrading enzyme fatty acid amide hydrolase (FAAH). Conversely, simulated microgravity during parabolic flights can depress the production of bona fide eCBs such as N-arachidonoylethanolamine (AEA) and 2-arachidonoylglycerol (2-AG). To date, the effects of SEM on other signaling lipids have been largely neglected, except a recent study addressing such effects on SPMs46. In particular, it was shown that simulated microgravity impairs RvD1 production, modulates LOX activity, and downregulates the expression of prominent SPM receptors GPR32 and GPR1846.
The available data on SEM effects on eicosanoids, eCBs, and SPMs during the immune response are summarized in Table 1. Thus, molecular signals such as AEA, cyclooxygenase-2 (COX-2), LOXs, NAPE-PLD, FAAH, and more recently RvD1 were shown to be affected by SEM in different experimental setups. Overall, these findings are consistent with a SEM-induced increase of the pro-inflammatory response.
Spaceflight exposome/microgravity effects on the immune-neuroendocrine system
Both innate and adaptive immunity have a well-documented connection with neuroendocrine system involving adrenergic receptors47, glucocorticoid receptors (GC)48, and other relevant molecular signaling and pathways49.
Beta-adrenergic and glucocorticoid receptors (GC) are expressed on NK cells and can inhibit their function50. These receptors may be the cause of a compromised NK cell function during spaceflight51. In particular, the in-flight exposome decreases number and function of NK associated not only with virus reactivation, but also with excessive systemic release of glucocorticoids/cortisol due to persistent stress conditions. This finding was also reported after flight52,53,54, suggesting a prolonged weakness of immune surveillance with potential health risk for astronauts.
The activity of neutrophils and monocytes/macrophages occurs through oxidative bursts, producing radical oxygen/nitrogen species. Taken together, astronauts exhibit elevated oxidants and reduced antioxidants55. Consistently, animal models aboard the ISS demonstrated significant inhibition of gene-metabolite networks linked to oxidative stress, emphasizing mitochondrial dysfunction56 and increased oxidative phosphorylation25,57. Noteworthy, oxidative-stress balance is crucial not only as an immune activity marker but also as a potential pro-inflammatory marker with neuro-endocrine effects when disrupted58.
Long-term spaceflight exposure increases the expression of PAMPs/DAMPs (Pathogen Associated Molecular Patterns/Danger Associated Molecular Patterns) receptors, such as Toll-Like Receptors (TLRs), in astronauts’ peripheral blood granulocytes/monocytes and serum concentrations of their ligands. TLRs remain elevated post-flight but recover after seven days15. The rise in DAMP receptors may result from augmented self-alarmin molecules in stressed conditions, able to fuel inflammatory state. In this perspective, the increase of autophagic cell death has been shown in in vitro cell models, as cellular stress response after 28 days on board the ISS59, suggesting a need for further ex vivo evaluation.
Spaceflight also reduces thymopoiesis and raises plasma/urinary cortisol levels, indicating a link between glucocorticoids and immune suppression60,61. While T lymphocyte percentages are preserved post-flight, memory T lymphocytes increase54, and delayed T cell activation occurs54,62, thus reflecting immunosenescence effects observed in aging. This acceleration may affect neuroendocrine regulation of inflammation and increase the risk of disease onset.
B cell compartment appeared to be preserved during long-term spaceflight, even though B lymphocyte count was increased54. Importantly, serum immunoglobulins A (sIgAs) increased in astronauts63, in agreement with the single-cell expression data suggesting possible up-regulation of BCR signaling genes in B cells immediately post-flight25. Since sIgAs mostly represent the mucosal humoral immune system, this finding may suggest an adaptive immune response in those districts and particularly in the Gut Associated Lymphoid Tissue (GALT), which tightly communicates with neuro-endocrine mediators64.
Similarly, the brain may be involved in a systemic response to various stressors through different pathways, such as cytokine/chemokine signaling, p38 mitogen-activated protein kinase (MAPK) and NF-κB signaling, indoleamine 2,3 dioxygenase and its downstream metabolites (kynurenine, quinolinic acid and kynurenic acid), and the neurotransmitters serotonin, dopamine and glutamate65. In this perspective, some cytokines/chemokines are also produced at neuroglia level. Notably, plasma cytokine/chemokine level is affected by long-term spaceflight. Pro-inflammatory molecules such as IL-8 (or CXCL8) and troponins from muscle tissues were increased in astronauts during long-duration missions onboard the ISS, even though both recovered on Earth66. The NASA Twin Study reported changes in the 50-cytokine profile of a homozygous twin astronaut during a one-year spaceflight mission on the ISS compared with the other ground-based twin67. However, different trends of cytokine levels may be different in other spaceflights. For instance, IL-6, a systemic pro-inflammatory cytokine that affects the hypothalamus as the central thermo-regulator, and Leptin, an adipokine mediator of the immune-neuroendocrine system, showed different trends comparing the NASA Twin Study with other astronauts/missions68. This indicates a relevant inter-individual variability2. Likewise, a decrease of regulatory/inhibitory cytokines after return to Earth54 may support a systemic pro-inflammatory status after landing.
However, the overall impact on these different molecular patterns/signaling and their downstream protein deserves further investigation to better understand the systemic pro-inflammatory effect, the neuro-endocrine system activation, and its recovery.
Spaceflight exposome/microgravity effects on PINE and gut microbiome (GM)
Molecules involved in the PINE network, not only have been studied in spaceflight exposome as reported in Table 2 (including GM in a few cases), but have also been investigated in the context of terrestrial analogs, such as isolation/confinement campaigns (Table 3), head-down bed rest (HDBR) studies (Table 4) and dry immersion studies (Table 5), that represent cheaper and logistically simpler settings, where the effects of single or multiple variables of the spaceflight exposome can be evaluated. On the whole, several studies have observed a predominance of sympathetic cardiac activity and elevated cortisol levels during spaceflight69,70,71, in HDBR72,73,74, and in situations of prolonged confinement and isolation75,76,77. These modifications are acceptable for the body in the short term, as hypothesized by Selye12. If prolonged, they give rise to a cascade of further multisystem alterations that impact the physical and mental health of the astronaut. Depressive symptoms and anxiety disorders, alteration of sleep, suppression of antiviral response, and establishment of a pro-inflammatory state are among the main maladaptive symptoms that may emerge78,79.
All these alterations sustain each other in a detrimental loop, due to the tight relationship of the PINE network. The SNS innervates lymphoid organs including the spleen and lymph nodes and, its neurotransmitters epinephrine and norepinephrine, secreted by the adrenal gland and local sympathetic neurons, can be recognized by adrenergic receptors on immune cells and in particular by the β2-adrenergic receptor47. Depending on the cell type, adrenergic signaling regulates a variety of functions in immune cells ranging from cellular migration to cytokine secretion80. Furthermore, due to the diurnal oscillation of systemic norepinephrine levels, various immune functions follow a circadian rhythmic pattern.
Sleep deficiency, common among astronauts due to circadian rhythm disruption during spaceflight81,82, can activate the HPA axis and enhance SNS neurotransmitters, impacting the IS via neurotransmitter receptors and NF-κB-mediated inflammatory signaling83. Persistent sleep disturbances or deprivation may trigger norepinephrine release in lymphoid organs and adrenal epinephrine release, stimulating leukocyte adrenergic receptors (e.g., ADRB2) and activating NF-κB-mediated inflammation, significantly affecting inflammatory status83.
Psychological stress, also manifested as sleep disturbances and prolonged anxiety, can chronically activate the inflammatory response. This may lead to a chronic low-grade inflammation, known as inflammaging84, which is associated with the aging process and age-related onset on Earth. Additionally, this process may be accelerated during long-term spaceflight missions2,85.
Cortisol typically has anti-inflammatory effects and inhibits the immune response. However, chronic elevation of cortisol can lead to IS resistance. This results in an accumulation of stress hormones and increased production of inflammatory cytokines, which further compromise the immune response41,86,87. It is well established that astronauts exhibit significantly increased salivary cortisol concentrations during spaceflight52 and cortisol spikes in plasma and urine after return to Earth. This response was more pronounced after long-term missions as compared to short-term missions71. A recent study also demonstrated an increased in-flight endocannabinoid blood levels as biological compensation of stress response54. Thus, various IS components are secondary modified to prolonged psychological and physiological stressors which in turn may generate effects on the immune system.
In the neuroendocrine system great relevance has the gut/GALT and brain-gut axis. In particular, enterochromaffin (EC) cells are known as the major source of gut-derived serotonin (5-hydroxytryptamine, 5-HT). Lipid mediated engagement of invariant natural killer T cells with EC cells regulates peripheral 5-HT release via CD1d, indicating an immune-mediated selective neuroendocrine response to lipid antigens64. This circuit is extremely important since connect gut microbiome (GM), lipid antigens and immune-neuroendocrine response. In this context, spaceflight is known to affect gut-microbiota67,88,89, bacteria gene expression in an in vitro model90, and recent evidence in animal model also suggests an effect on host-GM interaction91, thus the advancement of countermeasures for keeping GM homeostasis during spaceflight missions should be pursued for crew members’ health. As well known, diet-derived tryptophan (TRP) and gut microbiota-host interaction significantly influence TRP availability and metabolism, which in turn may affect cognitive function92. TRP either crosses the blood-brain barrier for serotonin synthesis or undergoes metabolism in the gut or liver via the kynurenine pathway. Unbalance of this pathway can lead to neuroprotective kynurenic acid or neurotoxic quinolinic acid, thus potentially impairing cognitive function. Gut microbiota, not only metabolizes TRP, producing indoles that activate aryl hydrocarbon receptor (AhR) signaling, essential for the control of immune response and neuroinflammation93,94,95, but may also synthesizes TRP or convert it into serotonin. These processes can alter TRP availability for the host, with potential effects on the brain.
GM may lead to the acute activation of intestinal sensory neurons, in particular, it has been demonstrated through Bacteroides fragilis polysaccharide A96. Interestingly, Bacteroides species are among those affected by long-term spaceflight97, thus suggesting an important GM-mediated effect potentially able to modify neuroendocrine response. In fact, recent studies confirm the central role not only of the brain-gut axis, but also of the GM in inter-organ communication with the involvement of neurotransmitters (catecholamines, serotonin, gamma-aminobutyric acid), intestinal peptides (cholecystokinin, peptide YY and glucagon-like peptide 1), and bacterial metabolites such as short-chain fatty acids98. Main SCFAs include acetate, propionate, and butyrate. They have anti-inflammatory properties and influence immune cell function, being also able to modulate the brain-gut axis by acting on the vague nerve and influencing neurotransmitter production. GM and their lipid metabolites can affect the HPA axis, which is crucial for stress response and hormonal regulation. SCFAs and bile acids modified by microbiota strains can modulate the release of neurotransmitters like serotonin and dopamine, impacting mood and cognitive functions99. It is noteworthy that changes in intestinal microbial abundance also alter the expression of neurotransmitter receptors within the brain in animal models100,101, suggesting a strong potential for deeper investigation in humans and spaceflight countermeasures.
Holistic approach: countermeasures for PINE network modulation
Space is a hostile environment for humans. Altered gravity or circadian misalignment are just few of the factors that could challenge the maintenance of homeostasis. Indeed, psychological aspects are also involved102. In the context of future long-duration space missions, a holistic approach will be fundamental both to deepen our knowledge on the impact of these variables and to define appropriate countermeasures10,103. The new approach has to overcome the strict distinction among different systems and between body and mind. To this aim, a trans-systemic approach is necessary that takes into account the potential integration of the pathways involved (Figs. 1 and 2). Moreover, there is an important and widely extended inter-individual variability in the perception and intensity of response to stimuli considered stress factors104. A first approach to counteracting the adverse effects of spaceflight exposome could involve a systematic personalized retrospective analysis and the prospective identification of the most resilient psychophysiological profiles, as well as those that respond at the best to interventional countermeasures. Understanding how each astronaut or type of psychophysiological profile, including sex-related variables, copes with spaceflight exposome would help to plan profile-related strategies to reduce or control stress-induced activation and its negative consequences on physical and mental health. On the other hand, a strong and high individual variability may reduce the efficacy of the identification of common psychophysiological profiles to be used as reference target. Recently, advanced strategies to improve mental training, such as mental imagery105, have been developed that could be further implemented for a more personalized training application.
In this context, the ANS, through its multisystemic connections running from the central nervous system (CNS) to the entire organism, represents an important target to study106. While the prolonged dominance of the SNS, a critical component of the stress response, can have harmful effects, the predominance of the PNS, especially vagal modulation, reflects a more adaptive autonomic state at rest. This is associated with greater resilience and faster recovery from stress107. Future studies on terrestrial analogs or space missions will have to verify whether astronauts, who present an ANS modulated by a vagal predominance, are actually more resilient to the induced alterations. In addition, all the interventions aimed at maintaining or restoring the balance between sympathetic and parasympathetic modulation could represent effective countermeasures.
The possibility of vagal stimulation by GM-derived neurotransmitters, such as γ-aminobutyric acid (GABA), serotonin, and dopamine, paves the way for advanced countermeasures able to stimulate vagal afferent neurons and sending signals to the brain. For example, certain Lactobacillus and Bifidobacterium species produce GABA, which can interact with the vague nerve to influence mood and stress responses108. Gut bacteria ferment dietary fibers and are able to produce short-chain fatty acids (SCFAs) like acetate, propionate, and butyrate. In turn, these SCFAs can stimulate the vague nerve either directly or indirectly through their anti-inflammatory effects109. Furthermore, SCFAs can modulate the release of gut hormones such as neuropeptide Y (NPY), peptide YY (PYY), and glucagon-like peptide-1 (GLP-1), which can then activate vagal pathways98. Supplementation with specific probiotics that enhance vagal stimulation may help to improve stress resilience. In this perspective, it should be recalled that both pre-/pro-biotics have been shown to efficiently promote the growth of beneficial gut bacteria producing SCFAs and neurotransmitters88,109, and post-biotics, which supply beneficial bacterial metabolites110, can improve host-GM interaction, and hence human health.
Accordingly, physical personalized exercise, programs of stress management, or more direct intervention such as the vague nerve stimulation (VNS) are all possible strategies to adopt. The first approach has already been introduced and studied, applying different protocols also in terrestrial analogs111. However, it has been observed that subjects display markedly different responses to the same intervention, thus identifying “responders” and individuals that have “low sensitivity” to the physical activity104. These aspects further emphasize the need for a more detailed profiling of the baseline psychophysiological states of the crew for the prediction of the future response both to the spaceflight exposome and to the adopted countermeasures. Furthermore, it is necessary to identify new strategies aiming to modify the perception of stimuli not foreseen by evolution (e.g., cognitive restructuring or positive psychology).
As for VNS, a growing literature data points to it as a powerful technique to normalize an altered sympathovagal balance112, by reducing inflammation106 and improving mood conditions113. A recent study in stress-susceptible mice has shown that chronic VNS restored behavior-relevant neuronal oscillations with the recovery of altered behavioral states, thus again suggesting that physiological vagal-brain communication underlies anxiety and mood disorders114.
It is known that transcutaneous VNS (tVNS) directly engages the nucleus tractus solitarius, which is the primary brainstem target of most afferent vagal projections, and significantly activates areas of the central vagal network, namely the locus caeruleus, amygdala, and nucleus accumbens. Vagal afferent signaling to the nucleus tractus solitarius (NTS) may lead to an indirect reduction of sympathetic activity and a simultaneous increase in parasympathetic activity. Noteworthy, tVNS has recently been proposed as a new powerful non-invasive approach to dysautonomias, such as postural orthostatic tachycardia syndrome (POTS) and cyclic vomiting syndrome115.
Thus, targeting ANS as countermeasure by means of different techniques (from cognitive behavioral therapies and Gut microbiota-derived metabolites, to non-invasive tVNS) might represent a future holistic approach to modulate the PINE network in astronauts, as schematically depicted in Fig. 4.
The main potential countermeasures targeting PINE system are summarized. Dotted arrows indicate potential induction of the specified molecules. BDNF brain -derived neurotrophic factor, GABA γ-aminobutyric acid, SCFAs short chain fatty acids, SNS sympathetic nervous system, PNS parasympathetic nervous system.
Conclusions and perspectives
Recent studies on crew members involved in long-duration space missions have identified potential immune dysfunctions, including immune hyper-activity and hypo-reactivity25,52,54,66. These dysfunctions may impact the PINE network through various molecular pathways, as illustrated in Figs. 1 and 2. Additionally, dysregulated psychophysiological features can negatively affect the integrated system and overall health, leading to arrhythmias, cardiovascular alterations, and depressive symptoms. Therefore, a comprehensive understanding of the role and regulation of molecular signaling within the PINE network is crucial. This knowledge could favor the development of targeted therapies and strategies to mitigate the effects of spaceflight on crew members, enhancing their resilience to threatening agents.
In this context, many ground-based findings suggest the significant role of GM-derived signaling as an exogenous contributor of molecules and mediators likely capable of modulating the PINE network. For instance, SCFAs can reduce the expression of pro-inflammatory cytokines and eicosanoids, which may subsequently decrease the induction of lipoxygenase (LOX) enzymes. Microbiota-induced changes in bile acid metabolites can affect lipid signaling and alter the activity of enzymes involved in lipid metabolism, including LOX. GM-derived signaling can also influence the endocannabinoid system through various mechanisms, such as the production of endocannabinoid-like substances. A research in animal models has shown that certain gut bacteria strains, such as Akkermansia muciniphila, can produce molecules similar to endocannabinoids, like 2-oleoylglycerol (2-OG), which can activate cannabinoid receptors116. GM can influence levels of endocannabinoids such as anandamide (AEA) and 2-arachidonoylglycerol (2-AG) by affecting their synthesis and degradation pathways in the gut and other tissues. This, in turn, may indirectly influence cannabinoid receptor expression and function, thus impacting the endocannabinoid signaling117.
The potential molecular task-force behind GM-derived signaling is illustrated in Fig. 5, based on ground results independently of spaceflight118,119,120,121. This issue deserves further investigations to be exploited for current and future countermeasures that could take into account the interactions of gut microbiota-derived metabolites, pre/pro/postbiotic valuable effects, and ad hoc physical exercise training with ASN interactions (Fig. 4).
The most important gut-derived metabolites are depicted with potential effect on molecular signaling for PINE network. The potential host receptors, which could be modulated, are highlighted in red. D-AAs Amino Acid with D configuration, NAEs N-acylethanolamines, 2-MAGs 2-monoacylglycerols, GABA, γ-aminobutyric acid, BCFAs Branched chain fatty acid, SCFAs short chain fatty acids, AhR aryl hydrocarbon receptor, NMDA N-methyl D-aspartate receptor, DRs Dopamine receptors, PPARs peroxisome proliferator-activated receptors, CB1 cannabinoid receptors type 1, 5-HTRs serotonine receptors, GCPRs/FFARs G-coupled Protein Receptors/Free Fatty Acid Receptors, CB2 cannabinoid receptors type 2, TLRs toll-like receptors.
The comprehensive role of GM-derived signaling and the involvement of specific bacterial strains seems crucial for developing countermeasures that influence PINE network regulation. Further investigation on the changes of GM composition/bacterial metabolites is deemed necessary to confirm the effects of spaceflight exposome and, approaching personalized medicine, to identify pre-/pro-/post-biotic and dietary supplements with a personalized approach for more effective countermeasures. Detecting the individual effects of the spaceflight exposome on PINE-associated molecular pathways and circulating blood mediators represents a new frontier for targeted, personalized therapies to counteract spaceflight exposome and preserve astronauts’ health. Moreover, direct vagal activation, such as non-invasive tVNS, could be explored for preventing pathophysiological alterations related to physical and mental stress responses observed in astronauts during long-term space missions.
References
Wild, C. P. The exposome: from concept to utility. Int J. Epidemiol 41, 24–32 (2012).
Capri, M. et al. Long-term human spaceflight and inflammaging: Does it promote aging? Ageing Res. Rev. 87, 101909, (2023).
Crucian, B. E. et al. Immune system dysregulation during spaceflight: Potential countermeasures for deep space exploration missions. Front. Immunol. 9, 1437 (2018).
Lu, S., Wei, F. & Li, G. The evolution of the concept of stress and the framework of the stress system. Cell Stress 5, 76–85, (2021).
Selye, H. Confusion and controversy in the stress field. J. Hum. Stress 1, 37–44 (1975).
Frippiat, J. P. et al. Towards human exploration of space: The THESEUS review series on immunology research priorities. NPJ Microgravity 2, 16040 (2016).
Chrousos, G. P. Stress and disorders of the stress system. Nat. Rev. Endocrinol. 5, 374–381 (2009).
Marazziti, D., Arone, A., Ivaldi, T., Kuts, K. & Loganovsky, K. Space missions: psychological and psychopathological issues. CNS Spectrums 27, 536–540 (2022).
Basner, M. et al. Psychological and behavioral changes during confinement in a 520-day simulated interplanetary mission to mars. PLoS ONE 9, e93298 (2014).
Antonsen, E. L. et al. Updates to the NASA human system risk management process for space exploration. NPJ Microgravity 9, 72 (2023).
Albornoz-Miranda, M., Parrao, D. & Taverne, M. Sleep disruption, use of sleep-promoting medication and circadian desynchronization in spaceflight crewmembers: Evidence in low-Earth orbit and concerns for future deep-space exploration missions. Sleep Med. X 6, 100080 (2023).
Selye, H. Stress and the general adaptation syndrome. Br. Med. J 1, 1383–1392 (1950).
Charmandari, E., Tsigos, C. & Chrousos, G. Endocrinology of the stress response. Ann. Rev. Physiol. 67, 259–284 (2005).
McEwen, B. S. Protective and damaging effects of stress mediators: central role of the brain. Dialogues Clin. Neurosci. 8, 367–381 (2006).
Ponomarev, S. A. et al. The impact of short-term confinement on human innate immunity. Sci. Rep. 12, 8372 (2022).
Miller, D. B. & O’Callaghan, J. P. Neuroendocrine aspects of the response to stress. Metabolism 51, 5–10 (2002).
McEwen, B. Stress adaptation, and disease. Allostasis Allostatic load. Ann. N. Y Acad. Sci. 840, 33–44 (1998).
Thayer, J. F., Yamamoto, S. S. & Brosschot, J. F. The relationship of autonomic imbalance, heart rate variability and cardiovascular disease risk factors. Int. J. Cardiol. 141, 122–131 (2010).
Won, E. & Kim, Y.-K. Send Orders for Reprints to reprints@benthamscience.ae Stress, the Autonomic Nervous System, and the Immune-kynurenine Pathway in the Etiology of Depression. Curr. Neuropharmacol. 14, 665–673 (2016).
Agorastos, A. & Chrousos, G. P. The neuroendocrinology of stress: the stress-related continuum of chronic disease development. Mol. Psychiatry 27, 502–513 (2022).
Hering, D., Lachowska, K. & Schlaich, M. Role of the Sympathetic Nervous System in Stress-Mediated Cardiovascular Disease. Curr. Hypertension Rep. 17, 80 (2015).
Fisher, A. J., Song, J. & Soyster, P. D. Toward a systems-based approach to understanding the role of the sympathetic nervous system in depression. World Psychiatry 20, 295–296 (2021).
Zefferino, R., Di Gioia, S. & Conese, M. Molecular links between endocrine, nervous and immune system during chronic stress. Brain Behav 11, e01960 (2021).
Dinan, T. G. & Cryan, J. F. Regulation of the stress response by the gut microbiota: Implications for psychoneuroendocrinology. Psychoneuroendocrinology 37, 1369–1378 (2012).
Kim, J. K. et al. Single-cell multi-ome and immune profiles of the Inspiration4 crew reveal conserved, cell-type, and sex-specific responses to spaceflight. Nat. Commun. 15, 4954 (2024).
Crucian, B. E., Stowe, R. P., Pierson, D. L. & Sams, C. F. Immune system dysregulation following short- vs long-duration spaceflight. Aviat. Space Environ. Med. 79, 835–843 (2008).
Mukhopadhyay, S. et al. A systems biology pipeline identifies new immune and disease related molecular signatures and networks in human cells during microgravity exposure. Sci. Rep. 6, 25975 (2016).
Versari, S., Longinotti, G., Barenghi, L., Maier, J. A. M. & Bradamante, S. The challenging environment on board the International Space Station affects endothelial cell function by triggering oxidative stress through thioredoxin interacting protein overexpression: the ESA-SPHINX experiment. FASEB J 27, 4466–4475 (2013).
Girardi, C. et al. Integration analysis of MicroRNA and mRNA expression profiles in human peripheral blood lymphocytes cultured in modeled microgravity. Biomed. Res. Int. 2014, 296747 (2014).
McGinley, A. M. et al. Interleukin-17A serves a priming role in autoimmunity by recruiting IL-1β-producing myeloid cells that promote pathogenic T cells. Immunity 52, 342–356.e6 (2020).
Chang, T. T., Spurlock, S. M., Candelario, T. L. T., Grenon, S. M. & Hughes-Fulford, M. Spaceflight impairs antigen-specific tolerance induction in vivo and increases inflammatory cytokines. FASEB J 29, 4122–4132 (2015).
Gallardo-Dodd, C. J. et al. Exposure of Volunteers to Microgravity by Dry Immersion Bed over 21 Days Results in Gene Expression Changes and Adaptation of T Cells (2023).
Shi, L. et al. Spaceflight and simulated microgravity suppresses macrophage development via altered RAS/ERK/NFκB and metabolic pathways. Cell Mol. Immunol. 18, 1489–1502 (2021).
Guéguinou, N. et al. Modulation of iberian ribbed newt complement component C3 by stressors similar to those encountered during a stay onboard the international space station. Int. J. Mol. Sci. 20, 1579 (2019).
Li, N. et al. Microgravity-induced alterations of inflammation-related mechanotransduction in endothelial cells on board SJ-10 satellite. Front. Physiol. 9, 1025 (2018).
Jiang, M. et al. Endoplasmic reticulum stress-dependent activation of iNOS/NO-NF-κB signaling and NLRP3 inflammasome contributes to endothelial inflammation and apoptosis associated with microgravity. FASEB J 34, 10835–10849 (2020).
Kohn, F. P. M. & Hauslage, J. The gravity dependence of pharmacodynamics: the integration of lidocaine into membranes in microgravity. NPJ Microgravity 5, 1–6 (2019).
Akiyama, T. et al. How does spaceflight affect the acquired immune system? npj Microgravity 6, 14 (2020).
Chiurchiù, V., Leuti, A. & Maccarrone, M. Bioactive lipids and chronic inflammation: managing the fire within. Front. Immunol. 9, 38 (2018).
Fava, M. et al. Cellular and molecular effects of microgravity on the immune system: a focus on bioactive lipids. Biomolecules 14, 446 (2024).
Leuti, A. et al. Bioactive lipids, inflammation and chronic diseases. Adv. Drug Delivery Rev 159, 133–169 (2020).
Hishikawa, D., Hashidate, T., Shimizu, T. & Shindou, H. Diversity and function of membrane glycerophospholipids generated by the remodeling pathway in mammalian cells. J. Lipid Res. 55, 799–807 (2014).
Basil, M. C. & Levy, B. D. Specialized pro-resolving mediators: Endogenous regulators of infection and inflammation. Nat. Rev. Immunol. 16, 51–67 (2016).
Maccarrone, M. et al. Goods and Bads of the Endocannabinoid System as a Therapeutic Target: Lessons Learned after 30 Years. Pharm. Rev. 75, 885–958 (2023).
Serhan, C. N. & Levy, B. D. Resolvins in inflammation: Emergence of the pro-resolving superfamily of mediators. J. Clin. Investig. 128, 2657–2669 (2018).
Leuti, A. et al. Simulated microgravity affects pro-resolving properties of primary human monocytes. Cells 13, 100 (2024).
Sharma, D. & David Farrar, J. Adrenergic regulation of immune cell function and inflammation. Semin Immunopathol 42, 709–717 (2020).
Cox, S. S. et al. Adrenergic and glucocorticoid modulation of the sterile inflammatory response. Brain Behav. Immun. 36, 183–192 (2014).
Akinyemi, D. E., Chevre, R. & Soehnlein, O. Neuro-immune crosstalk in hematopoiesis, inflammation, and repair. Trends Immunol 45, 597–608 (2024).
Capellino, S., Claus, M. & Watzl, C. Regulation of natural killer cell activity by glucocorticoids, serotonin, dopamine, and epinephrine. Cell Mol. Immunol. 17, 705–711 (2020).
Bigley, A. B. et al. NK cell function is impaired during long-duration spaceflight. J. Appl. Physiol 126, 842–853 (2018).
Mehta, P. & Bhayani, D. Impact of space environment on stability of medicines: challenges and prospects. J. Pharm. Biomed. Anal 136, 111–119 (2017).
Mehta, S. K. et al. Dermatitis during spaceflight associated with HSV-1 reactivation. Viruses 14, 789 (2022).
Buchheim, J. I. et al. Stress related shift toward inflammaging in cosmonauts after long-duration space flight. Front. Physiol. 10, 85 (2019).
De Luca, C. et al. Monitoring antioxidant defenses and free radical production in space-flight, aviation and railway engine operators, for the prevention and treatment of oxidative stress, immunological impairment, and pre-mature cell aging. Toxicol. Ind. Health 25, 259–267 (2009).
Chakraborty, N. et al. Gene-metabolite network linked to inhibited bioenergetics in association with spaceflight-induced loss of male mouse quadriceps muscle. J. Bone Miner. Res 35, 2049–2057 (2020).
Rudolf, A. M. & Hood, W. R. Mitochondrial stress in the spaceflight environment. Mitochondrion 76, 101855 (2024).
Vitale, G., Salvioli, S. & Franceschi, C. Oxidative stress and the ageing endocrine system. Nat. Rev. Endocrinol. 9, 228–240 (2013).
Tran, V., Carpo, N., Cepeda, C. & Espinosa-Jeffrey, A. Oligodendrocyte progenitors display enhanced proliferation and autophagy after space flight. Biomolecules 13, 201 (2023).
Buford, T. W. & Willoughby, D. S. Impact of DHEA(S) and cortisol on immune function in aging: A brief review. Appl. Physiol. Nutrition Metabol. 33, 429–433 (2008).
Benjamin, C. L. et al. Decreases in thymopoiesis of astronauts returning from space flight. JCI Insight 1, e88787 (2016).
Hughes-Fulford, M., Chang, T. T., Martinez, E. M. & Li, C.-F. Spaceflight alters expression of microRNA during T-cell activation. FASEB J 29, 4893–4900 (2015).
Spielmann, G. et al. B cell homeostasis is maintained during long-duration spaceflight. J. Appl. Physiol 126, 469–476 (2019).
Luo, J. et al. Lipids regulate peripheral serotonin release via gut CD1d. Immunity 56, 1533–1547.e7 (2023).
Capuron, L. & Miller, A. H. Immune system to brain signaling: Neuropsychopharmacological implications. Pharmacol. Therapeutics 130, 226–238 (2011).
Crucian, B. E. et al. Plasma cytokine concentrations indicate that in vivo hormonal regulation of immunity is altered during long-duration spaceflight. J. Interferon Cytokine Res 34, 778–786 (2014).
Garrett-Bakelman, F. E. et al. The NASA twins study: a multidimensional analysis of a year-long human spaceflight. Science 364, eaau8650 (2019).
Capri, M. et al. Recovery from 6-month spaceflight at the International Space Station: muscle-related stress into a proinflammatory setting. FASEB J 33, 5168–5180 (2019).
Mandsager, K. T., Robertson, D. & Diedrich, A. The function of the autonomic nervous system during spaceflight. Clin. Autonomic Res. 25, 141–151 (2015).
Mehta, S. K., Stowe, R. P., Feiveson, A. H., Tyring, S. K. & Pierson, D. L. Reactivation and Shedding of Cytomegalovirus in Astronauts during Spaceflight. The Journal of Infectious Diseases 182 https://academic.oup.com/jid/article/182/6/1761/916184 (2000).
Stowe, R. P., Sams, C. F. & Pierson, D. L. Adrenocortical and Immune responses following short- and long-duration spaceflight. Aviat. Space Environ. Med. 82, 627–634 (2011).
Hirayanagi, K. et al. Autonomic cardiovascular changes during and after 14 days of head-down bed rest. Auton. Neurosci. 110, 121–128 (2004).
Liang, X. et al. Changes in the diurnal rhythms during a 45-day head-down bed rest. PLoS ONE 7, e47984 (2012).
Xu, X. et al. Changes of Cytokines during a Spaceflight Analog - a 45-Day Head-Down Bed Rest. PLoS ONE 8, e77401 (2013).
Maggioni, M. A. et al. Reduced vagal modulations of heart rate during overwintering in Antarctica. Sci. Rep. 10, 21810 (2020).
Yi, B. et al. 520-d Isolation and confinement simulating a flight to Mars reveals heightened immune responses and alterations of leukocyte phenotype. Brain Behav. Immun. 40, 203–210 (2014).
Jacubowski, A. et al. The impact of long-term confinement and exercise on central and peripheral stress markers. Physiol. Behav. 152, 106–111 (2015).
Scatà, C. et al. Social isolation: a narrative review on the dangerous liaison between the autonomic nervous system and inflammation. Life 13, 1229 (2023).
Jones, C. W., Basner, M., Mollicone, D. J., Mott, C. M. & Dinges, D. F. Sleep deficiency in spaceflight is associated with degraded neurobehavioral functions and elevated stress in astronauts on six-month missions aboard the International Space Station. Sleep 45, zsac006 (2022).
Devi, S. et al. Adrenergic regulation of the vasculature impairs leukocyte interstitial migration and suppresses immune responses. Immunity 54, 1219–1230.e7 (2021).
Barger, L. K. et al. Prevalence of sleep deficiency and use of hypnotic drugs in astronauts before, during, and after spaceflight: AN observational study. Lancet Neurol 13, 904–912 (2014).
Flynn-Evans, E. E., Barger, L. K., Kubey, A. A., Sullivan, J. P. & Czeisler, C. A. Circadian misalignment affects sleep and medication use before and during spaceflight. NPJ Microgr 2, 15019 (2016).
Irwin, M. R. & Opp, M. R. Sleep health: reciprocal regulation of sleep and innate immunity. Neuropsychopharmacology 42, 129–155 (2017).
Franceschi, C. et al. Inflammaging and anti-inflammaging: a systemic perspective on aging and longevity emerged from studies in humans. Mech. Ageing Dev. 128, 92–105 (2007).
Tobaldini, E. et al. Short sleep duration and cardiometabolic risk: from pathophysiology to clinical evidence. Nat. Rev. Cardiol. 16, 213–224 (2019).
Vitlic, A., Lord, J. M. & Phillips, A. C. Stress, ageing and their influence on functional, cellular and molecular aspects of the immune system. Age 36, 9631 (2014).
Morey, J. N., Boggero, I. A., Scott, A. B. & Segerstrom, S. C. Current directions in stress and human immune function. Curr Opin Psychol. 5, 13–17 (2015).
Turroni, S. et al. Gut microbiome and space travelers’ health: state of the art and possible pro/prebiotic strategies for long-term space missions. Front. Physiol. 11, 553929 (2020).
Voorhies, A. A. et al. Study of the impact of long-duration space missions at the International Space Station on the astronaut microbiome. Sci. Rep. 9, 9911 (2019).
Aunins, T. R. et al. Spaceflight modifies Escherichia coli gene expression in response to antibiotic exposure and reveals role of oxidative stress response. Front. Microbiol. 9, 310 (2018).
Gonzalez, E. et al. Spaceflight alters host-gut microbiota interactions. NPJ Biofilms Microbiol 10, 71 (2024).
Santoro, A. et al. Gut microbiota changes in the extreme decades of human life: a focus on centenarians. Cell. Mol. Life Sci. 75, 129–148 (2018).
Barroso, A., Mahler, J. V., Fonseca-Castro, P. H. & Quintana, F. J. The aryl hydrocarbon receptor and the gut–brain axis. Cell. Mol. Immunol. 18, 259–268 (2021).
Shaw, C., Hess, M. & Weimer, B. C. Microbial-derived tryptophan metabolites and their role in neurological disease: anthranilic acid and anthranilic acid derivatives. Microorganisms 11, 1825 (2023).
Sinha, A. K. et al. Dietary fibre directs microbial tryptophan metabolism via metabolic interactions in the gut microbiota. Nat. Microbiol. 9, 1964–1978 (2024).
Mao, Y. K. et al. Bacteroides fragilis polysaccharide A is necessary and sufficient for acute activation of intestinal sensory neurons. Nat. Commun. 4, 1465 (2013).
Liu, Z. et al. Effects of spaceflight on the composition and function of the human gut microbiota. Gut Microbes 11, 807–819 (2020).
Kasarello, K., Cudnoch-Jedrzejewska, A. & Czarzasta, K. Communication of gut microbiota and brain via immune and neuroendocrine signaling. Front. Microbiol. 14, 1118529 (2023).
Chen, Y., Xu, J. & Chen, Y. Regulation of neurotransmitters by the gut microbiota and effects on cognition in neurological disorders. Nutrients 13, 2099 (2021).
Neufeld, K. M., Kang, N., Bienenstock, J. & Foster, J. A. Reduced anxiety-like behavior and central neurochemical change in germ-free mice. Neurogastroenterol. Motility 23, 255–64 (2011).
Bravo, J. A. et al. Ingestion of Lactobacillus strain regulates emotional behavior and central GABA receptor expression in a mouse via the vagus nerve. Proc. Natl. Acad. Sci. USA 108, 16050–16055 (2011).
Gatti, M., Palumbo, R., Di Domenico, A. & Mammarella, N. Affective health and countermeasures in long-duration space exploration. Heliyon 8, e09414 (2022).
Antonsen, E. L. et al. Estimating medical risk in human spaceflight. NPJ Microgravity 8, 8 (2022).
Scott, J. P. R., Kramer, A., Petersen, N. & Green, D. A. The role of long-term head-down bed rest in understanding inter-individual variation in response to the spaceflight environment: a perspective review. Front. Physiol. 12, 614619 (2021).
Gatti, M., Palumbo, R., Di Domenico, A. & Mammarella, N. Simulating extreme environmental conditions via mental imagery: the case of microgravity and weight estimation. Front Psychol 13, 913162 (2022).
Bellocchi, C. et al. The interplay between autonomic nervous system and inflammation across systemic autoimmune diseases. Int. J. Mol. Sci. 23, 2449 (2022).
Carnevali, L., Koenig, J., Sgoifo, A. & Ottaviani, C. Autonomic and brain morphological predictors of stress resilience. Front. Neurosci. 12, 228 (2018).
Rajanala, K., Kumar, N. & Chamallamudi, M. R. Modulation of gut-brain axis by probiotics: a promising anti-depressant approach. Curr. Neuropharmacol. 19, 990–1006 (2021).
Moțățăianu, A., Șerban, G. & Andone, S. The role of short-chain fatty acids in microbiota–gut–brain cross-talk with a focus on amyotrophic lateral sclerosis: a systematic review. Int. J. Mol. Sci. 24, 15094 (2023).
Shama, S., Qaisar, R., Khan, N. A., Tauseef, I. & Siddiqui, R. The role of 4-phenylbutyric acid in gut microbial dysbiosis in a mouse model of simulated microgravity. Life 12, 1301 (2022).
Scott, J. P. R., Weber, T. & Green, D. A. Introduction to the frontiers research topic: optimization of exercise countermeasures for human space flight – Lessons from terrestrial physiology and operational considerations. Front. Physiol. 10, 173 (2019).
Carandina, A. et al. Effects of transcutaneous auricular vagus nerve stimulation on cardiovascular autonomic control in health and disease. Auton. Neurosci. 236, 102893 (2021).
Naparstek, S., Yeh, A. K. & Mills-Finnerty, C. Transcutaneous Vagus Nerve Stimulation (tVNS) applications in cognitive aging: a review and commentary. Front. Aging Neurosci. 15, 1145207 (2023).
Okonogi, T. et al. Stress-induced vagal activity influences anxiety-relevant prefrontal and amygdala neuronal oscillations in male mice. Nat. Commun. 15, 183 (2024).
Carandina, A. et al. Transcutaneous vagus nerve stimulation as a potential novel treatment for cyclic vomiting syndrome: a first case report. Clin. Auton. Res. 34, 209–212 (2024).
Coccurello, R., Marrone, M. C. & Maccarrone, M. The endocannabinoids-microbiota partnership in gut-brain axis homeostasis: implications for autism spectrum disorders. Front. Pharmacol. 13, 869606 (2022).
Srivastava, R. K., Lutz, B. & Ruiz de Azua, I. The microbiome and gut endocannabinoid system in the regulation of stress responses and metabolism. Front. Cell. Neurosci. 16, 867267 (2022).
Matsumoto, M. et al. Free D-amino acids produced by commensal bacteria in the colonic lumen. Sci. Rep. 8, 17915 (2018).
O’Riordan, K. J. et al. Short chain fatty acids: microbial metabolites for gut-brain axis signalling. Mol. Cell. Endocrinol. 546, 111572 (2022).
Roussel, C. et al. Human gut microbiota and their production of endocannabinoid-like mediators are directly affected by a dietary oil. Gut Microbes 16, 2335879 (2024).
Zhang, H., Xie, Y., Cao, F. & Song, X. Gut microbiota-derived fatty acid and sterol metabolites: biotransformation and immunomodulatory functions. Gut Microbes 16, 2382336 (2024).
Maccarrone, M., Bari, M., Lorenzon, T. & Finazzi-Agrò, A. Altered gravity modulates prostaglandin H synthase in human K562 cells. J. Gravit. Physiol 7, 61–62 (2000).
Maccarrone, M. & Finazzi-Agro, A. Microgravity increases the affinity of lipoxygenases for free fatty acids. FEBS Lett 489, 283 (2000).
Maccarrone, M. et al. Creating conditions similar to those that occur during exposure of cells to microgravity induces apoptosis in human lymphocytes by 5-lipoxygenase-mediated mitochondrial uncoupling and cytochrome c release. J. Leukoc. Biol 73, 472–481 (2003).
Choukèr, A. et al. Motion sickness, stress and the endocannabinoid system. PLoS ONE 5, e10752 (2010).
Strewe, C. et al. Effects of parabolic flight and spaceflight on the endocannabinoid system in humans. Rev. Neurosci. 23, 673–680 (2012).
Gasperi, V. et al. The fatty acid amide hydrolase in lymphocytes from sedentary and active subjects. Med. Sci. Sports Exerc. 46, 24–32 (2014).
Battista, N. et al. Altered anandamide metabolism in microgravity: the “RESLEM” experiment. Front. Physiol. 9, (2018).
Bersenev, E. Y. et al. Sleep in 21-day dry immersion. are cardiovascular adjustments rapid eye movement sleep-dependent? Front. Physiol. 12, 749773 (2021).
de Abreu, S. et al. Multi-system deconditioning in 3-day dry immersion without daily raise. Front. Physiol. 8, 799 (2017).
Jollet, M. et al. Does physical inactivity induce significant changes in human gut microbiota? New answers using the dry immersion hypoactivity model. Nutrients 13, 3865 (2021).
Lebedeva, S., Shved, D. & Savinkina, A. Assessment of the psychophysiological state of female operators under simulated microgravity. Front. Physiol. 12, 751016 (2022).
Robin, A. et al. Comprehensive assessment of physiological responses in women during the ESA dry immersion VIVALDI microgravity simulation. Nat. Commun. 14, 6311 (2023).
Acknowledgements
MM wishes to thank Dr. Annamaria Tisi and Dr. Noemi De Dominicis (University of L’Aquila, Italy) for their kind help with the artwork. This review paper is based upon work from the Contributors to the topic “Immunology” in the “Integrative Physiology” of the ASI Space Life Sciences Working Groups. The publication of this manuscript is supported by the Italian Space Agency (ASI). M.C. was supported by RFO (Ricerca Fondamentale Orientata) funds and the ASI- contract “MetaMuscle” (CUP) F35F21001800005.
Author information
Authors and Affiliations
Contributions
All authors have contributed to the original writing draft. Conceptualization of the main flow stream was performed by M.C., N.M. and M.M.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Capri, M., Montano, N., Piccirillo, S. et al. Spaceflight exposome/microgravity effects on the psychoimmunoneuroendocrine system. npj Microgravity 11, 66 (2025). https://doi.org/10.1038/s41526-025-00487-8
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41526-025-00487-8