Abstract
Beta-adrenoceptor-blockers and agonists have been associated with an increased and decreased risk of Parkinson’s disease (PD), respectively. We aimed to investigate whether these medications are linked to clinical heterogeneity and progression in PD. Longitudinal data from the Parkinson’s Incident Cohorts Collaboration (n = 1107) were analysed. Baseline clinical status and progression to Hoehn & Yahr stage 3 (H&Y3) or dementia were compared in beta-blocker or beta-agonist users versus non-users of each drug. Baseline motor and cognitive variables were similar in beta-blocker users (n = 195) versus non-users and beta-agonist users (n = 68) versus non-users, following adjustment for relevant confounders. Beta-blocker users (n = 156) progressed faster to H&Y3 (p = 0.002), accounting for relevant confounders (Hazard Ratio (HR) = 1.538; p = 0.011), while beta-agonist users (n = 54) progressed similarly to non-users. Neither drug was associated with progression to dementia. These findings support the possibility that beta-adrenoceptor drugs may have potential in modifying aspects of PD progression. Further investigation is essential to identify any causative component in the relationship.
Similar content being viewed by others
Introduction
Parkinson’s disease (PD) is characterised by the pathological accumulation of alpha-synuclein positive Lewy bodies and neurites in the brain, with associated changes in the immune system both within the central nervous system (CNS) and the periphery. Beta-adrenoceptor modulation has been found to influence alpha-synuclein gene expression, with blockade leading to increased expression, and stimulation leading to decreased expression1. Beta-adrenoceptors are also present on immune cells, with stimulation related to immune-regulatory effects, and blockade related to immune activation2.
Epidemiological studies, including meta-analyses, have linked the use of beta-blockers and beta-agonists with an increased and decreased risk of PD, respectively1,3,4,5,6,7,8. However, some studies have found inconsistent results, and confounding factors and reverse causation may also contribute to these associations9,10,11,12,13.
Amongst those who have PD, relationships between beta-adrenoceptor modulating drugs and progression to major PD milestones such as postural instability and dementia, features which are relatively resistant to dopaminergic therapy and have important implications on quality of life and care14, have not been fully explored. Only one study has investigated these medications in relation to progression in PD and suggested that short-acting beta-agonist use was not associated with progression to dementia, but was associated with reduced time to death in PD, which was considered to reflect the effect of chronic obstructive pulmonary disease (COPD)/asthma severity in users of these medications6. Links between the use of these medications at the time of PD diagnosis and baseline clinical heterogeneity or subsequent motor progression to postural instability have not been investigated. This study sought to investigate these relationships using baseline and longitudinal data from the Parkinson’s Incidence Cohorts Collaboration (PICC)15, since beta-adrenoceptor modulation could potentially be a modifiable risk factor for PD progression. We hypothesised that beta-blockers would be associated with faster disease progression, while beta-agonists would display the opposite relationship.
Results
The overall PICC cohort consisted of 1107 patients with newly diagnosed idiopathic PD16,17,18,19,20,21. Demographic and baseline clinical details are shown in Table 1. The combined cohort had an average time from diagnosis to last visit of 5.5 (SD 3.1) years (Table 1).
Beta-adrenoceptor drugs and baseline clinical heterogeneity
At the baseline visit, 195 (17.6%) of patients were on beta-blockers, 68 (6.1%) were taking beta-agonists, 4 (0.40%) were on both beta-agonists and beta-blockers, and 848 (76.6%) were not prescribed either of these drug classes (non-users). A detailed breakdown of specific drugs is provided in Supplementary Table S1.
Demographic and baseline clinical characteristics of groups stratified according to beta adrenoceptor drug use are summarised in Table 2. Beta-blocker users were significantly older, had a shorter disease duration at baseline, and higher baseline MDS-UPDRS motor and H&Y scores than non-users (Table 2). Frequency of cardiovascular disease and Cumulative Illness Rating Scale (CIRS) category scores were also higher in beta-blocker users than non-users, as anticipated given their typical clinical indications for use (Table 2). Beta-agonist users were significantly older and had fewer years of education compared to non-users (Table 2). The presence of autoimmune/inflammatory disease, percentage of ex/current smokers and CIRS category score were significantly higher in beta-agonist users compared to non-users, as anticipated given the typical clinical indications for these medications. (Table 2).
Multivariate regression analysis was performed to assess the contribution of potential confounding factors to the observed group differences in baseline motor disease severity (Table 3). This analysis did not include the NYPUM and ParkWest cohorts due to the absence of CIRS data (Table 3). The results revealed that the associations between beta-blocker use and higher baseline MDS-UPDRS motor scores and H&Y stage were not statistically significant when accounting for relevant covariates (age at diagnosis, disease duration, comorbidities and study cohort) (Table 3).
Beta-adrenoceptor drugs and motor and cognitive progression
There were no significant differences in follow-up duration for groups stratified by beta-blocker use/non-use and beta-agonist use/non-use (Table 2). Patients who were already at H&Y3 at baseline (n = 159) were excluded from the H&Y3 survival analyses. Following these exclusions, the higher baseline MDS-UPDRS motor score and H&Y stage in the beta-blocker use group and the higher age at diagnosis in the beta-agonist use group did not remain statistically significant (Supplementary Table S2).
The median time to reach H&Y3 was 3.52 (Interquartile Range (IQR) 1.77–5.49) years in beta-blocker users and 4.10 (IQR 2.22–6.04) years in beta-blocker non-users. Beta-blocker users progressed to H&Y3 significantly earlier than non-users (Kaplan-Meier analysis; Log Rank (Mantel–Cox), (χ2) = 9.286, df = 1; p = 0.002) (Fig. 1A). Cox regression analysis confirmed this significant relationship between beta-blocker use and increased progression to H&Y3 (Hazard Ratio (HR) = 1.538, p = 0.011), with the inclusion of relevant variables as potential confounders (age at diagnosis, disease duration, comorbidities (CIRS score, cardiovascular disease, diabetes, smoking status) and study cohort) (Table 4).
For beta-agonist users, median time to reach H&Y3 was 4.57 (IQR 1.69–5.57) years, compared to 4.02 (IQR 2.11–5.89) years for non-users. There was no significant difference in rate of progression to H&Y3 between beta-agonist users and non-users (Log Rank (Mantel–Cox), (χ2) = 0.544, df = 1; p = 0.461) (Fig. 1B). This was confirmed by Cox regression analysis (HR = 0.772, p = 0.420) with relevant confounders (Table 4).
During the course of the study, 29.6% of patients developed dementia, with a mean duration from PD diagnosis to dementia onset of 4.50 (IQR 2.56–6.17) years amongst this group. Time to dementia did not differ in beta-blocker users versus non-users on Kaplan–Meier analysis (Log Rank (Mantel–Cox), (χ2) = 3.242, df = 1; p = 0.072) (Fig. 2A) or Cox regression (HR = 1.017, p = 0.926) with relevant baseline confounders (Table 5). Similarly, Kaplan–Meier analysis indicated that time to dementia did not differ in beta-agonist users compared to non-users (Log Rank (Mantel–Cox), (χ2) = 0.084, df = 1; p = 0.772) (Fig. 2B). This was confirmed on Cox regression analysis (HR = 1.091, p = 0.793) with relevant confounders (Table 5).
Study cohort was included as a categorical covariate, with the largest cohort (PICNICS) as the reference category (Tables 3–5), in all multivariate regression analyses. (Use of each of the other cohorts as the reference category had no significant effect on the relationships and significance of the other covariates in the model (data not shown)). The inclusion of the study cohort as a covariate in regression analyses revealed heterogeneity in the effect size and significance of each cohort on the dependent variables (baseline motor severity and progression to H&Y3 and dementia). However, such adjustment for study cohort did not alter our primary finding of a significant relationship between beta blocker use and faster progression to H&Y3.
Discussion
This study demonstrates an association between the use of beta-blocker medications in early PD and subsequent motor progression in a large population-based incident PD cohort. Regular beta-blocker use was associated with more rapid progression to H&Y stage 3 over a mean of 5.5 years of follow-up. However, we observed no significant association between beta-agonist use and progression to H&Y3, and no significant relationship between beta-adrenoceptor drug use and progression to dementia.
Most patients on beta-blockers were prescribed these drugs for cardiovascular disease. This could potentially confound the relationship between beta blocker use and motor impairment, given that postural instability, gait dysfunction and impaired mobility in PD are also linked with increased cerebral white matter disease due to vascular risk factors and poor cardiovascular health22. Cardiovascular disease is also associated with older age, and this can itself be a risk factor for motor progression to H&Y316 and may also be linked with a more severe baseline motor subtype subsequently predictive of prognosis23. In keeping with this, we found that although baseline motor impairment was higher in beta-blocker users compared to non-users, this was confounded by age and comorbidity. However, in terms of axial motor progression, the association between time to H&Y3 and beta blocker use remained significant even accounting for age at diagnosis, baseline H&Y stage, cardiovascular disease, smoking, diabetes and comorbidity score in Cox regression analysis. This suggests that the association between beta-blockers and faster progression to H&Y3 in this cohort is not simply explained by the confounding effects of baseline H&Y stage, age and key comorbidity factors. However, data available in this study may not cover all possible aspects of cardiovascular co-morbidity (e.g. undiagnosed disease) and we cannot exclude the possibility that some residual confounding due to cardiovascular co-morbidity contributes towards the observed association.
Both beta-blockers and beta-agonists are known to cross the blood-brain-barrier (BBB) to different extents and may be mediating effects via central and/or peripheral mechanisms24,25. Brain concentrations of beta-blockers following oral intake have been found to be higher for the relatively lipophilic beta-blockers such as propranolol and metoprolol compared to atenolol24. However, separate analysis of those taking medium-high versus low BBB penetrating beta-blockers was not feasible due to inadequate numbers in each group and lack of data for fair dose equivalent comparisons.
Beta-agonist use at baseline was not associated with altered progression to H&Y3 in this cohort. However, the study may have been underpowered due to the relatively low number of individuals on beta agonist medications. Beta-agonists have been detected in the brain, with nasal administration leading to higher brain concentrations than intravenous administration26. It is possible to speculate that the lack of effect on progression to H&Y3 seen with beta-agonists in this study could be partially due to inadequate systemic and CNS concentrations achieved using inhaled beta-agonists. Thus, further studies investigating different routes of administration and brain pharmacokinetics will be important.
Whilst previous studies have not examined the relationship between beta-adrenoceptor drug use at baseline and subsequent motor progression, the prospective use of beta-blockers and beta-agonists has been associated with an increased and decreased PD risk, respectively1,3,4,5. However, further studies have suggested there may be confounding factors such as reverse causation, and association of the drugs with underlying diseases and risk factors (e.g. chronic obstructive lung disease and smoking) contributing towards these findings9,10,11,12. One study by Alexander et al. suggested a beneficial influence of the beta-agonist albuterol on some PD motor symptoms27, but no prior studies have assessed these aspects longitudinally. The evaluation of associations between beta-adrenoceptor use and subsequent clinical progression within PD (as in this study) is less likely to be influenced by reverse causation compared to studies assessing beta-adrenoceptor use and PD risk, thus also strengthening the current findings linking beta-blocker use with increased axial motor progression in PD.
The potential mechanisms underlying the association between beta-blockers and increased motor progression in PD are complex and multifactorial. Increased axial motor impairment and progression to H&Y3 may be mediated by pathology outside the nigrostriatal tract, including cortical Lewy body pathology 28,29. Beta-adrenoceptor stimulation has been found to decrease expression of alpha-synuclein, and hence beta-adrenoreceptor blockade may be a risk factor for increased cortical alpha-synuclein accumulation and pathological aggregation1. Another potential mechanism of relevance is immune modulation, given that beta-adrenergic modulation has considerable effects on the immune system2. Both innate and adaptive immune cells have beta-adrenergic receptors and are likely to be modulated by beta-agonists and beta-blockers2,30. Generally, beta-adrenergic stimulation is associated with modulating overtly excessive immune responses and has demonstrated dopaminergic neuroprotective effects via inhibitory effects on microglia30. Consequently, beta-blockade would be expected to have opposing effects, leading to increased immune activation, which may be detrimental in the context of PD2. In addition, beta-agonists have also been shown to enhance brain extraction of levodopa, although this may be less relevant to relatively dopamine-resistant axial motor dysfunction25. However, these proposed underlying mechanisms, including alterations in alpha-synuclein expression and/or immune activation, remain speculative and require further investigation.
In keeping with a previous study6, beta-adrenoreceptor modulating drugs were not significantly associated with progression to PD dementia. One possible explanation is that the pathology of PD dementia is more multifactorial, and related to Alzheimer’s type pathology as well as alpha synuclein aggregates31, whereas the pathology of the axial motor features of PD may be more dependent on alpha-synuclein pathology.
A strength of our study is that it has used a large, comprehensive dataset comprising population-based, incident PD cohorts with an average 5.50-year prospective follow-up, with the ability to adjust for some of the potentially confounding influence of key comorbid conditions. However, it is important to acknowledge the limitations. Patients had different time periods of follow-up, although there were no significant differences between groups in the time from diagnosis to last visit (Table 2). Details of the duration and exact daily dose of beta-agonists and beta-blockers taken prior to PD onset and data on commencement or discontinuation of these drugs during the follow-up period were not available for all cohorts. Also, as with all drug studies, the accuracy of drug intake as per prescription could not be guaranteed, and all this limits the ability to confirm conclusions on the true causal influence of these drugs. Additionally, the relative effects of high and low BBB-penetrating beta-blockers/beta-agonists were not assessed due to low numbers of each drug type within the cohort and the lack of feasibility of fair dose comparisons. As previously discussed, the potential residual confounding of any uncaptured cardiovascular and other comorbid factors is also a possible limitation, while factors such as regular exercise, which may potentially have beneficial effects on disease progression32, are also not included as covariates in the analysis. Furthermore, regular use of some beta-blockers has been linked to dizziness, light-headedness and increased risk of falls, thus possibly confounding the relationship between beta-blockers and increased progression to postural instability/H&Y333. Formal assessment of orthostatic hypotension for inclusion as a potential confounder would be important in future studies.
While the inclusion of several different study cohorts from different parts of the UK and Europe is a strength, the inclusion of study cohort in the regression analyses indicated that there may be some heterogeneity among cohorts in terms of both disease severity at baseline and progression to H&Y3 and dementia (e.g. greater and less progression to H&Y3 in CamPaIGN and ICICLE cohorts respectively). Such variability may be due to additional population-level genetic and environmental factors unaccounted for in the data, and further characterisation of such additional relevant features would be valuable in future studies. A formal sensitivity analysis using a sub-cohort of the data was not performed due to the limited size of the individual cohorts and the absence of similar general comorbidity data to be used as a covariate in all cohorts. In addition, while details of ethnicity were not included in this study analysis, the cohorts in this study were mainly recruited from Caucasian majority populations, and further studies including cohorts from other countries and ethnicities will be important.
Overall, this study suggests that beta-adrenoceptor modulating drugs may be associated with heterogeneity of axial motor progression in PD. This is a motor feature which is considered to have a non-dopaminergic basis and thus more accurately reflects the underlying disease state than motor symptoms, which are dopa-responsive and confounded by PD medication use34. Further detailed longitudinal epidemiological cohort studies in even larger cohorts, with long-term follow-up and detailed data on medication type, dose, duration, confounding symptoms and comorbidities, will enable investigation into potential dose-response relationships and better correction for confounders. Such detailed studies, together with more experimental studies, will be required to confirm the current findings and, if confirmed, understand the mechanisms and significance of the associations seen.
In general, this work is supportive of previous studies suggesting that beta-adrenoceptor-stimulating drugs warrant further investigation as candidates for drug repurposing trials in PD. Additionally, considering the beneficial use of beta-blockers for the symptomatic control of tremor in PD, as well as for comorbid conditions such as cardiovascular disease and migraine35, further thorough investigation and clarification of any potential negative association between beta-blockers and PD axial motor progression will be important to help prescribers navigate the relative benefits and risks of these drugs for people with PD.
Methods
Participants and data collection
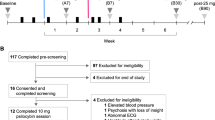
Data was utilised from PICC, a collaboration of 6 population-based PD cohorts in Northern Europe15. Each study obtained demographic and clinical data as near as feasible to the disease diagnosis (baseline (first) visit; mean (standard deviation) disease duration 0.19 (0.32) years; range 0–2.35 years) and during prospective follow-up15. Details have been previously published (Cambridgeshire Incidence of PD from General Practitioner to Neurologist (CamPaIGN))16; Incidence of Cognitive Impairment in Cohorts with Longitudinal Evaluation-PD (ICICLE-PD)17,36; New Parkinson Patient in Umeå (NYPUM)18, The Norwegian ParkWest study (ParkWest)19, Parkinsonism: Incidence, Cognition and Non-motor heterogeneity in Cambridgeshire (PICNICS)20 and Parkinsonism Incidence in North-East Scotland (PINE)21.
In brief, patients were diagnosed with idiopathic PD using UK PD Brain Bank criteria without family history as an exclusion criterion. Patients were followed up at regular intervals and in this study, data from follow-up visits performed every 12, 18 or 24 months were used. All patients had a confirmed clinical diagnosis of idiopathic PD at their last clinic visit or autopsy.
Standard protocol approvals, registrations and patient consents
All studies had ethical approval from their regional Ethics Committees and written informed consent was obtained from all participants. CamPaIGN- Cambridgeshire 3 Research Ethics Committee (08/H0306/26); ICICLE Newcastle- Newcastle and North Tyneside 1 Research Ethics Committee (08/H0906/147); NYPUM- The Regional Ethics Committee of Umeå University, (Um dnr 03-387); Park West- Regional Committee for Medical and Health Research Ethics, Western Norway (REK 131/04); PICNICS- Essex Ethics Committee (REC 07/H0302/138); PINE- Multi-centre Research Ethics Committee for Scotland A (REC05/MRE00/94).
Demographic and clinical assessments
Data acquisition for each study cohort has been previously described in detail15 and included demographic and clinical data. Home visits and/or telephone follow-up to help ascertain key outcomes, as feasible, were offered to minimise attrition bias.
Motor symptoms were evaluated using the Hoehn and Yahr (H&Y) scale and the Unified Parkinson’s Disease Rating Scale (UPDRS) Part III (CamPaIGN, NYPUM, ParkWest, PINE) or the Movement Disorders Society-UPDRS (MDS-UPDRS) Part III (ICICLE-PD, PICNICS). UPDRS-III scores were converted into MDS-UPDRS-III as previously described37. Global cognitive function was assessed using the Mini-Mental State Examination (MMSE)38. Dementia was diagnosed according to Diagnostic and Statistical Manual of Mental Disorders, 4th Edition (PINE, CamPaIGN) or Movement Disorder Society PD dementia criteria39 (PICNICS, ICICLE-PD, NYPUM, ParkWest)15, using appropriate neuropsychological assessments to determine decreased global cognitive ability and impairment in more than one domain and clinical interviews to determine functional impairment and to exclude features making the diagnosis uncertain. Levodopa equivalent daily dose (LEDD) was calculated using published methods40.
Medication and comorbidity data categorisation
Medication history and comorbidity information were collected at the baseline visit based on available details from referral letters, prescriptions and patient interviews. In some cohorts, the patients’ general practitioners were contacted to obtain missing details (ICICLE-PD). Beta-adrenoceptor modulating drug categories were: beta-agonist users (oral or inhaled beta-agonist use) and non-users; beta-blocker users and non-users. Details of the exact daily dose of each drug and prior duration of use were not available for all studies.
Comorbidity burden was quantified by categorising the available medical history data based on the scoring guidelines from the CIRS and using the total number of comorbidity categories affected (CIRS category score)41. Due to the nature of the most common clinical indications for beta-agonists (immune mediated reversible airway obstruction including asthma and COPD) and beta-blockers (ischaemic heart disease, hypertension, cardiac arrhythmias), the presence or absence of the comorbid disease categories encompassing these conditions (autoimmune/inflammatory diseases and cardiovascular diseases respectively) were also separately recorded in cohorts where data was available.
Assessment of outcomes
Motor progression was assessed using time from diagnosis to reaching postural instability, as measured by a score of 3 or higher on the H&Y scale. The H&Y stage is particularly reflective of axial motor dysfunction (including postural instability and gait dysfunction) and reaching H&Y3 is a key motor milestone in PD progression14. The date of reaching H&Y3 was calculated as the midpoint between the first visit at and beyond which the H&Y status was consistently recorded as ≥3, and the preceding visit, based on the available follow-up data. For the purposes of this study, ‘consistent’ recording of the H&Y stage as ≥3 was defined as recording of the H&Y stage as ≥3 for all future visits until the end of follow-up. Censoring was at the time of the last assessment.
Cognitive progression was assessed by measuring the time from diagnosis to the fulfilment of criteria for PD dementia39. The date of dementia was calculated as the midpoint between the visit at which dementia was first diagnosed and the preceding visit16. Where patients were lost to follow-up in the research clinic, dementia diagnoses were determined from clinical records or death certificates, with date of dementia diagnosis being determined by expert consensus of experienced clinical researchers on a case-by-case basis using the midpoint between the date that dementia was first recorded and the preceding clinic visit or research appointment, as appropriate.
Time (years) from PD diagnosis to dementia was calculated and used for survival analysis. Censoring was at the time of the last assessment.
Statistical analysis
Data was analysed using IBM SPSS Statistics (Version 27). Survival plots were generated using GraphPad Prism version 9.
Baseline differences in demographic and clinical (including motor and cognitive) variables between beta-adrenoceptor drug users and non-users groups were evaluated using non-parametric Kruskal–Wallis tests for continuous variables (due to lack of normal distribution indicated by Shapiro–Wilk tests) and Chi-squared tests for dichotomous variables. Regression analyses were used to confirm any observed associations between the drug categories and key baseline cognitive and motor variables, adjusting for relevant covariates. Such analysis only included patients with all the covariates available for analysis.
Associations between beta-agonist users versus non-users and beta-blocker users versus non-users and time to reach H&Y3 or PD dementia were assessed using Kaplan-Meier survival analyses. Pairwise log-rank comparisons were conducted to determine if groups differed in survival distribution. Cox regression analyses were performed to control for relevant covariates. The event per variable ratio was >10 in each analysis, indicating suitability for survival analysis and Cox regression. The proportional hazards assumption was checked by visual inspection of Kaplan–Meier curves and Schoenfeld Residual plots for each covariate. Significance threshold was considered to be p < 0.05, and the available data was estimated to have 80% power to detect an HR of <0.57 and >1.75.
In all multivariate regression analyses, relevant covariates included variables that were significantly different (p < 0.05) between drug user/non-user groups (Table 2) and other relevant variables associated with the drug category or the outcome measure. Study cohort was included as a categorical covariate, with the largest cohort (PICNICS) as the reference category (Tables 3–5). Covariates included in each regression analysis are detailed in the ‘Results’ tables.
Data availability
Anonymised data related to the findings of this study may be shared on request from any qualified investigator for purposes of replicating procedures and results.
References
Mittal, S. et al. β2-Adrenoreceptor is a regulator of the α-synuclein gene driving risk of Parkinson’s disease. Science 357, 891–898 (2017).
Scanzano, A. & Cosentino, M. Adrenergic regulation of innate immunity: a review. Front. Pharmacol. 6, 171 (2015).
Gronich, N. et al. β2-adrenoceptor agonists and antagonists and risk of Parkinson’s disease. Mov. Disord. 33, 1465–1471 (2018).
Koren, G., Norton, G., Radinsky, K. & Shalev, V. Chronic use of β-blockers and the risk of Parkinson’s disease. Clin. Drug Investig. 39, 463–468 (2019).
Noyce, A. J. et al. Meta-analysis of early nonmotor features and risk factors for Parkinson disease. Ann. Neurol. 72, 893–901 (2012).
Marras, C. et al. Beta agonists and progression of Parkinson’s disease in older adults: a retrospective cohort study. Mov. Disord. 35, 1275–1277 (2020).
Chen, C. L., Wang, S. Y., Chen, T. C. & Chuang, C. S. Association between β2-adrenoreceptor medications and risk of Parkinson’s disease: a meta-analysis. Medicina 57, 1006 (2021).
Saengphatrachai, W., Praditukrit, K., Owattanapanich, W., Pitakpatapee, Y. & Srivanitchapoom, P. The association between developing Parkinson’s disease and β-Adrenoceptor acting agents use: a systematic review and meta-analysis. J. Neurol. Sci. 430, 120009 (2021).
Searles Nielsen, S., Gross, A., Camacho-Soto, A., Willis, A. W. & Racette, B. A. β2-adrenoreceptor medications and risk of Parkinson disease. Ann. Neurol. 84, 683–693 (2018).
Hopfner, F. et al. Use of β2-Adrenoreceptor agonist and antagonist drugs and risk of Parkinson disease. Neurology 93, E135–E142 (2019).
Giorgianni, F., Ernst, P., Dell’Aniello, S., Suissa, S. & Renoux, C. Beta 2 agonists and the incidence of Parkinson’s disease. Am. J. Epidemiol. 189, 801–810 (2020).
de Germay, S., Conte, C., Rascol, O., Montastruc, J.-L. & Lapeyre-Mestre, M. β-adrenoceptor drugs and Parkinson’s disease: a nationwide nested case–control study. CNS Drugs 34, 763–772 (2020).
Chen, W., Sadatsafavi, M., Tavakoli, H., Samii, A. & Etminan, M. Effects of β2-adrenergic agonists on risk of Parkinson’s disease in COPD: a population-based study. Pharmacotherapy 40, 408–415 (2020).
Evans, J. R. et al. The natural history of treated Parkinson’s disease in an incident, community based cohort. J. Neurol. Neurosurg. Psychiatry 82, 1112–1118 (2011).
Szwedo, A. A. et al. GBA and APOE impact cognitive decline in Parkinson’s disease: a 10-year population-based study. Mov. Disord. https://doi.org/10.1002/MDS.28932 (2022).
Williams-Gray, C. H. et al. The CamPaIGN study of Parkinson’s disease: 10-year outlook in an incident population-based cohort. J. Neurol. Neurosurg. Psychiatry 84, 1258–1264 (2013).
Yarnall, A. J. et al. Characterizing mild cognitive impairment in incident Parkinson disease: The ICICLE-PD Study. Neurology 82, 308–316 (2014).
Linder, J., Stenlund, H. & Forsgren, L. Incidence of Parkinson’s disease and Parkinsonism in northern Sweden: a population-based study. Mov. Disord. 25, 341–348 (2010).
Alves, G. et al. Incidence of Parkinson’s disease in Norway: the Norwegian ParkWest study. J. Neurol. Neurosurg. Psychiatry 80, 851–857 (2009).
Evans, J. R. et al. Comparative epidemiology of incident Parkinson’s disease in Cambridgeshire, UK. J. Neurol. Neurosurg. Psychiatry 87, 1034–1036 (2016).
Caslake, R. et al. Age-, gender-, and socioeconomic status-specific incidence of Parkinson’s disease and parkinsonism in northeast Scotland: the PINE study. Parkinsonism Relat. Disord. 19, 515–521 (2013).
Veselý, B., Antonini, A. & Rektor, I. The contribution of white matter lesions to Parkinson’s disease motor and gait symptoms: a critical review of the literature. J. Neural Transm. 123, 241–250 (2016).
Rajput, A. H., Rajput, M. L., Ferguson, L. W. & Rajput, A. Baseline motor findings and Parkinson disease prognostic subtypes. Neurology 89, 138–143 (2017).
Cruickshank, J. M. & Neil-Dwyer, G. Beta-blocker brain concentrations in man. Eur. J. Clin. Pharmacol. 28(Suppl), 21–23 (1985).
Uc, E. Y., Dienel, G. A., Cruz, N. F. & Harik, S. I. β-Adrenergics enhance brain extraction of levodopa. Mov. Disord. 17, 54–59 (2002).
Zhang, R. et al. Spatial distribution of (R)-Salbutamol in rat brain following nasal and intravenous administration using DESI-MS. Pharmaceutics 12, 35 (2020).
Alexander, G. M., Schwartzman, R. J., Nukes, T. A., Grothusen, J. R. & Hooker, M. D. 2-Adrenergic agonist as adjunct therapy to levodopa in Parkinson’s disease. Neurology 44, 1511–1513 (1994).
Virmani, T., Moskowitz, C. B., Vonsattel, J.-P. & Fahn, S. Clinicopathological characteristics of freezing of gait in autopsy-confirmed Parkinson’s disease. Mov. Disord. 30, 1874–1884 (2015).
Kotagal, V., Bohnen, N. I., Müller, M. L. T. M., Frey, K. A. & Albin, R. L. Cerebral amyloid burden and Hoehn and Yahr stage 3 scoring in Parkinson disease. J. Parkinsons Dis. 7, 143–147 (2017).
Qian, L. et al. 2-adrenergic receptor activation prevents rodent dopaminergic neurotoxicity by inhibiting microglia via a novel signaling pathway. J. Immunol. 186, 4443–4454 (2011).
Irwin, D. J. et al. Neuropathological and genetic correlates of survival and dementia onset in synucleinopathies: a retrospective analysis. Lancet Neurol. 16, 55–65 (2017).
Sharpe, G., Macerollo, A., Fabbri, M. & Tripoliti, E. Non-pharmacological treatment challenges in early Parkinson’s disease for axial and cognitive symptoms: a mini review. Front. Neurol. 25, 576569 (2020).
Ham, A. C. et al. Beta-blocker use and fall risk in older individuals: Original results from two studies with meta-analysis. Br. J. Clin. Pharmacol. 83, 2292–2302 (2017).
Evans, J. R. et al. The factor structure of the UPDRS as an index of disease progression in Parkinson’s disease. J. Parkinsons Dis. 1, 75–82 (2011).
Hopfner, F. et al. β-adrenoreceptors and the risk of Parkinson’s disease. Lancet Neurol. 19, 247–254 (2020).
Lawson, R. A. et al. Which neuropsychological tests? Predicting cognitive decline and dementia in Parkinson’s disease in the ICICLE-PD cohort. J. Parkinsons Dis. 11, 1297–1308 (2021).
Goetz, C. G., Stebbins, G. T. & Tilley, B. C. Calibration of unified Parkinson’s disease rating scale scores to Movement Disorder Society-unified Parkinson’s disease rating scale scores. Mov. Disord. 27, 1239–1242 (2012).
Folstein, M. F., Folstein, S. E. & McHugh, P. R. ‘Mini-mental state’. A practical method for grading the cognitive state of patients for the clinician. J. Psychiatr. Res. 12, 189–198 (1975).
Emre, M. et al. Clinical diagnostic criteria for dementia associated with Parkinson’s disease. Mov. Disord. 22, 1689–1707 (2007).
Tomlinson, C. L. et al. Systematic review of levodopa dose equivalency reporting in Parkinson’s disease. Mov. Disord. 25, 2649–2653 (2010).
Parmelee, P. A., Thuras, P. D., Katz, I. R. & Lawton, M. P. Validation of the Cumulative Illness Rating Scale in a geriatric residential population. J. Am. Geriatr. Soc. 43, 130–137 (1995).
Acknowledgements
We would like to thank all participants, study personnel from each study and funders of individual studies and of PICC. We would like to thank Artur Wozniak and Adrian Martin from the University of Aberdeen, Data Management Department, for their help in developing the PICC database. We acknowledge the contributions of members of the individual study groups as detailed below. CamPaIGN study: Roger A. Barker, Thomas Foltynie, Sarah L. Mason, Caroline H. Williams-Gray. ICICLE-PD Study: David Burn, Lynn Rochester, Alison J. Yarnall, Rachael A. Lawson, Gordon W. Duncan, Tien K. Khoo. NYPUM Study: Lars Forsgren, Jan Linder, Mona Edström, Jörgen Andersson, Linda Eriksson, David Bäckström, Gun-Marie Hariz, Magdalena Domellöf. ParkWest Study: ParkWest Principal investigators: Guido Alves (Norwegian Centre for Movement Disorders, Stavanger University Hospital) and Ole-Bjørn Tysnes (Haukeland University Hospital). Study personnel: Michaela Dreetz Gjerstad, Kenn Freddy Pedersen, Elin Bjelland Forsaa, Veslemøy Hamre Frantzen, Anita Laugaland, Jodi Maple- Grødem, Johannes Lange, Karen Simonsen, Eldbjørg Fiske and Ingvild Dalen (Stavanger University Hospital); Bernd Müller, Geir Olve Skeie and Marit Renså (Haukeland University Hospital); Wenche Telstad, Aliaksei Labusau and Jane Kastet (Førde Hospital); Ineke HogenEsch, Marianne Kjerandsen and Liv Kari Håland (Haugesund Hospital); Karen Herlofson, Solgunn Ongre and Siri Bruun (Sørlandet Hospital Arendal). PICNICS study: Roger A. Barker, Caroline H. Williams-Gray, Jonathan Evans, David P. Breen, Gemma Cummins, Krista Farrell, Ruwani Wijeyekoon, Kirsten Scott, Tom Stoker, Julia Greenland, Marta Camacho, Natalie Valle Guzman, Lucy Collins, Simon Stott and Sarah Mason. PINE Study: Medical: Carl E. Counsell, Kate S. M. Taylor, Robert Caslake, Angus D. Macleod, David J. M. McGhee, Diane Swallow; Research nurse/assistant: Joanne Gordon, Clare Harris, Ann Hayman, Nicola Johannesson, Hazel Forbes; Data management: Valerie Angus, Alasdair Finlayson, David Dawson, Katie Wilde, David Ritchie, Artur Wozniak; Statisticians: Neil Scott, Shona Fielding; Radiology: Prof. Alison Murray; Pathology: Ishbel Gall, Dr James MacKenzie, Prof. Colin Smith; Secretarial: Aileen Sylvester, Susan Mitchell, Pam Rebecca, Ann Christie and Diane McCosh. The CamPaIGN study has received funding from the Wellcome Trust, the Medical Research Council, the Patrick Berthoud Trust and the NIHR Cambridge Biomedical Research Centre. (NIHR203312). The ICICLE-PD study was funded by Parkinson’s UK (J-0802, G-1301, G-1507) and supported by the Lockhart Parkinson’s Disease Research Fund and the NIHR Newcastle Biomedical Research Unit and Centre (BRC). The views expressed are those of the author(s) and not necessarily those of the NIHR or the Department of Health and Social Care. The NYPUM study was supported by grants from the Swedish Medical Research Council, Erling-Persson Foundation, the Swedish Brain Foundation (Hjärnfonden), Umeå University, Västerbotten County Council, King Gustaf V and Queen Victoria Freemason Foundation, Swedish Parkinson Foundation, Swedish Parkinson Research Foundation, Kempe Foundation, Swedish PD Association, the European Research Council and the Knut and Alice Wallenberg Foundation. The Norwegian ParkWest study has received funding from the Research Council of Norway (177966), the Western Norway Regional Health Authority (911218), the Norwegian Parkinson’s Research Foundation and Rebergs Legacy. The PICNICS study was funded by the Cure Parkinson’s Trust, the Van Geest Foundation, the Medical Research Council, Parkinson’s UK and the NIHR Cambridge Biomedical Research Centre (NIHR203312). The PINE study was funded by Parkinson’s UK (grant numbers G0502, G0914 and G1302), the Scottish Chief Scientist Office (CAF/12/05, PCL/17/10), Academy of Medical Sciences, NHS Grampian endowments, the BMA Doris Hillier award, RS Macdonald Trust, the BUPA Foundation and SPRING. The PICC collaboration has been supported by The Chief Scientist Office of the Scottish Government (PCL/17/10), the Academy of Medical Sciences, Parkinson’s UK (initial collaborator meeting) and the Norwegian Association for Public Health. This research was funded in whole or in part by the UKRI Medical Research Council [MR/R007446/1]. R.S.W. was supported by a Fellowship from Addenbrooke’s Charitable Trust (RG77199). R.A.B. was an NIHR Senior Investigator (NF-SI-0616-10011) and is supported by the Cambridge Stem Cell Institute. C.H.W.G. was supported by an RCUK/UKRI Research Innovation Fellowship awarded by the Medical Research Council (MR/R007446/1; MR/W029235/1) and received support from the Cambridge Centre for Parkinson-Plus. J.M.G. and G.A. are supported by the Research Council of Norway (287842). R.A.L. is supported by the Janet Owens Parkinson’s UK Senior Research Fellowship (F-1801). A.J.Y. is supported by the NIHR Newcastle Biomedical Research Centre (BRC) and by grants awarded from Parkinson’s UK, Dunhill Medical Trust, EU IMI, NIHR HTA, Weston Brain Institute, Intercept Pharmaceuticals and Lewy Body Society.
Author information
Authors and Affiliations
Consortia
Contributions
Study conception: Ruwani S. Wijeyekoon. Major role in data collection: Ruwani S. Wijeyekoon, Marta Camacho, David Bäckström, Lars Forsgren, Rachael A. Lawson, Alison J. Yarnall, Angus D. Macleod, Carl E. Counsell, Ole-Bjørn Tysnes, Guido Alves, Jodi Maple-Grødem, Caroline H. Williams-Gray. Data analysis: Ruwani S. Wijeyekoon. Drafting of the manuscript: Ruwani S. Wijeyekoon. Preparation of data for analysis: Marta Camacho, David Bäckström, Angus D. Macleod, Jodi Maple-Grødem. Revision of the manuscript: Marta Camacho, David Bäckström, Lars Forsgren, Rachael A. Lawson, Alison J. Yarnall, Angus D. Macleod, Carl E. Counsell, Ole-Bjørn Tysnes, Guido Alves, Jodi Maple-Grødem, Roger A. Barker, Caroline H. Williams-Gray. Study conception and design: Roger A. Barker, Caroline H. Williams-Gray.
Corresponding author
Ethics declarations
Competing interests
R.S.W. reports no competing interests or disclosures relevant to the manuscript. M.C. reports no competing interests or disclosures relevant to the manuscript. D.B. reports no competing interests or disclosures relevant to the manuscript. L.F. reports no competing interests or disclosures relevant to the manuscript. R.A.L. reports no competing interests or disclosures relevant to the manuscript. A.J.Y. reports no competing interests or disclosures relevant to the manuscript. A.D.M. reports no competing interests or disclosures relevant to the manuscript. C.E.C. reports no competing interests or disclosures relevant to the manuscript. O.T. reports no competing interests or disclosures relevant to the manuscript. G.A. reports no competing interests or disclosures relevant to the manuscript. J.M.-G. reports no competing interests or disclosures relevant to the manuscript. R.A.B. reports no competing interests or disclosures relevant to the manuscript. C.H.W.-G. reports no competing interests or disclosures relevant to the manuscript.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wijeyekoon, R.S., Camacho, M., Bäckström, D. et al. Beta-adrenoceptor drugs and progression to Parkinson’s disease milestones in a large pooled incident cohort. npj Parkinsons Dis. 11, 198 (2025). https://doi.org/10.1038/s41531-025-01014-y
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41531-025-01014-y