Abstract
There is a relative dearth of research on patients with Parkinson’s disease (PD) from under-represented ethnic groups in the United Kingdom. The East London Parkinson Disease project seeks to understand the clinical manifestations and determinants of PD in a diverse population. Data on clinical features were collected, between 2019 and 2024. We assessed 218 patients with PD and 90 controls. Among them, 50% of patients and 64% controls identified as South Asian or Black. South Asian and Black patients had significantly worse motor scores compared to White patients (mean [SD], 42.2 [18.8], and 47.0 [16.6] vs 35.2 [16.4], p < 0.001 and p < 0.001). Cognitive impairment was more prevalent in South Asian (73%) and Black patients (75%) than in White patients (45%, p = 0.002). Our results suggest that patients with PD from South Asian and Black ethnic groups may have more severe motor and certain non-motor features, including cognitive impairment, compared to White patients.
Similar content being viewed by others
Introduction
Although progress in understanding the clinical types and patterns of Parkinson’s disease (PD) progression have been made using clinical, genetic and transcriptomic data1,2,3, there remains a lack of research in diverse populations4. Most studies, including PD trials5, have focused predominantly on White, relatively affluent, well-educated patients, who attend tertiary neurology services6. Even landmark initiatives seeking to develop markers of PD progression, such as the Parkinson’s Progression Marker Initiative (PPMI) or Parkinson’s Disease Biomarkers Program (PDBP), have enrolled more than 95% White participants7,8. These have failed to recruit patients in a manner that reflects the underlying population structure.
Several large initiatives aimed at population-specific risk factors for Parkinson’s and PD progression, such as LARGE-PD9, BLAAC PD10, and GP26, have started to address diversity in PD research. However, these are predominantly focused on understanding the genetic basis of PD risk.
The East London Parkinson’s Disease (ELPD) project was established to carry out research in a highly diverse population from East London with free access to a publicly funded, free at the point of service, healthcare system (namely the National Health Service - NHS). We aimed to recruit participants so that our sample reflected the underlying population structure in East London, where >40% identify as South Asian and 7% as Black, and ~45% are from the lowest UK deprivation group11. This work complements other initiatives in London to address health inequality in PD research12. The focus of present report was to describe the clinical features by ethnicity in patients and controls recruited to the ELPD project.
Results
Since 2019, a total of 218 patients and 90 controls have been recruited to the ELPD project. Of patients, 85 (39%), and of controls, 56 (62%) identified as South Asian (Table 1). Males represented 137 (63%) of patients and 63 (70%) of healthy controls. The age at assessment was higher in patients than controls (mean [SD], 68.5 [10.8] years vs 62.7 [10.9], p < 0.001). Our patients had an index of multiple deprivation decile of 3.0 [1] (median [IQR]) consistent with being in the most deprived tertile in the UK.
Demographic characteristics
Demographic and disease-related data are presented in Table 1. Our South Asian patients self-identified as 49% (42) Bangladeshi, 25% (21) Indian, 15% (13) Pakistani, and 11% (9) other South Asians. Our Black patients self-identified as 71% (17) Black African and 29% (7) African Caribbean. Age at assessment was higher in Black and White compared to South Asian patients (mean [SD], 71.1 [10.0], and 70.2 [9.5] vs 66.4 [11.4] years), Table 2. Time from diagnosis was 4.8 [6.9] (median, [IQR]) years, and duration of PD symptoms was 6.3 [7.4] years. There were no statistical differences between time from diagnosis and duration of symptoms across ethnic groups.
The index of multiple deprivation decile was higher for White than for South Asian, and Black patients (median [IQR], 4.0 [2.0], vs 3.0 [1.0] and 3.0 [2.0], p = 0.003), Supplementary Table 1. Hypertension was present more frequently in the patients identifying as Black (75%) compared to South Asian (52%) and White (49%), p = 0.069. Type 2 diabetes was more common in patients identifying as South Asian (46%), compared to Black (26%) and White (24%), p = 0.006. Smoking and alcohol consumption were significantly increased in the White patient group (Supplementary Table 2). Caffeine consumption, pesticide exposure, and head injury were very similar between groups (Supplementary Table 2).
Clinical characteristics
There was weak evidence of an older age at symptom onset in White and Black patients, compared to South Asian patients (mean [SD], 62.6 [11.3], and 64.4 [11.9] vs 59.2 [12.2] years, p = 0.055, p = 0.068 respectively). Similarly, age at diagnosis did not achieve significance, but was lower in the South Asian patients (Table 2).
Time from symptom onset to diagnosis was similar in all three patient groups - White versus South Asian patients, and versus Black patients (median [IQR], 1.2 [1.5], vs 1.0 [1.9] and 1.0 [0.9] years, p = 0.171, and p = 0.247). Symptom duration on assessment in South Asian, Black was similar to White patients (median [IQR], 6.8 [7.3], 6.5 [3.7] vs 6.0 [7.6] years, p = 0.939 and p = 0.952). There was no evidence that median levodopa equivalent daily doses (LEDD) were higher in the South Asian group than White and Black patients (median [IQR], 600 [600], 536 [532], vs 540 [473] mg, p = 0.411 and p = 0.938 respectively).
MDS-UPDRS III motor scores were significantly higher in the South Asian and Black groups compared to White patients (mean [SD], 42.2 [18.8], 47.0 [16.6], vs 35.2 [16.4], p < 0.001 and p < 0.001 respectively). The magnitude of these differences remained when adjusted for age, gender, disease duration and LEDD. Fewer South Asian patients (10%) reported experiencing an ‘OFF’ period during the assessment, compared to White (23%) and Black groups (29%), but this was only nominally significant p = 0.043. The difference in MDS-UPDRS III remained significant between ethnicities when adjusting for ON-OFF status (p < 0.001). Motor complications were also found to be more severe, with a higher MDS-UPDRS IV for the Black patients compared to the White group (median [IQR], 6.0 [5.0] vs 3.0 [6.0], p < 0.001), Fig. 1.
Objective motor assessments - BRAIN test, showed worse scores for ethnically under-represented patients, with akinesia time (AT) significantly slower in the South Asian compared to the White group (median [IQR], 194.5 [102.2] vs 153.0 [90.1] ms, p < 0.001), when adjusted for age, gender, duration of disease, and ON-OFF state (Supplementary Table 3).
Non-motor and motor experiences of daily living are reflected in the MDS-UPDRS I and II (Table 2). A greater number of non-motor symptoms, as assessed by the NMSQ, were reported in South Asian compared to White patients (median [IQR], 13.5 [11.2] vs 11.0 [18.0], p = 0.002).
Cognitive impairment in ELPD
From 218 patients, 91 White, 52 South Asian and 16 Black patients had reliable cognitive scores on the MoCA (n = 159). From 90 controls, only 39 had reliable MoCA scores. For details of participants excluded from this analysis see Supplementary Note 1. There was weak evidence for MoCA scores being higher in controls than patients (mean [SD], 25.6 [3.4] vs 23.8 [4.6], p = 0.024). MoCA scores were lower in patients from South Asian and Black ethnicities, compared to the White patients (mean [SD], 22.2 [4.7], 22.4 [4.8] vs 24.9 [4.2], p < 0.001 and p < 0.001 respectively, Table 2). Based on MoCA scores alone, patients from South Asian and Black groups were identified as having more cognitive impairment than in White groups (38, 73%, and 12, 75%, vs 41, 45%, p = 0.002), Fig. 2 & Supplementary Table 4.
Other clinical characteristics
Using a brief 6-item version of the UPSIT, controls had higher scores compared to patients (median [IQR], 3.0 [2.0] vs 2.0 [2.0], p = 0.007). South Asian and White patients had similar smell scores (median [IQR], 2.0 [3.0] vs 2.0 [1.0], p = 0.911), whereas Black patients had worse scores (median [IQR], 1.0 [1.0], p = 0.002, and p = 0.037). Patients from South Asian backgrounds had worse scores compared to White for depression (HADS-D mean [SD], 8.5 [5.2] vs 6.3 [3.8], p = 0.019), sleep quality (PDSS2 mean [SD] 23.1 [11.7] vs 17.1 [10.2], p = 0.008), quality of life index (EQ5D5L index mean [SD] 0.4 [0.3] vs 0.5 [0.3], p < 0.001) (Supplementary Table 1). Black patients had similar scores compared to White for depression, sleep quality, and quality of life index. There was no significant difference between pain reporting in the three ethnicities in univariate or multivariate analysis (Supplementary Table 1). No statistical differences between all three ethnicities were seen in the daytime somnolence scores (ESS), autonomic dysfunction (SCOPA-AUT), anxiety (HADS-A) and REM sleep behaviour clinical suspicion (RBDSQ) (Supplementary Table 1).
Discussion
Here we describe the baseline data in a diverse sample of patients residing in East London receiving ‘free at the point of service’ care via the NHS. Using inclusive recruitment methods, more than 50% of patients and 65% of the control group came from South Asian and Black ethnic groups. We found that motor, non-motor and cognitive features differed by ethnicity, with evidence overall for a more severe burden of disease in under-represented patient groups. There were no differences in time to diagnosis, disease and symptom duration, or treatment differences to account for the worse motor phenotype in South Asian and Black groups.
Our data suggest that South Asian and Black patients had worse motor scores, when adjusting for age, gender, disease duration, and LEDD. We investigated whether assessing patients in ON versus OFF states may be driving the difference in scores. However, MDS-UPDRS III scores were still significantly higher in Black and South Asian patients, when adjusting for this. This is in keeping with other studies that have also shown MDS-UPDRS III reflects disease progression regardless of ON/OFF states13. Similarly, motor fluctuations were worse in Black patients compared to the White group, when adjusting for age, gender, disease duration, and LEDD.
The severity of motor scores suggests a requirement for higher doses of medication, or a heavier burden of disease in under-represented patient groups. This may hold true especially in the South Asian patients, as their age at onset was significantly younger. Worse motor severity and fluctuations could be explained by genetic factors, with more atypical motor features having been reported by Chaudhuri et al. in under-represented communities, such as UK-based South Asian and Afro-Caribbean populations14. Factors, such as concomitant diabetes, hypertension, or other cardiovascular risk factors could also be an explanation14, as well as language/cultural barriers in accurately ascertaining motor fluctuations. Another explanation for ethnic differences in disease severity could be a lower socio-economic status in our Black and South Asian patients. However, one of the strengths of our study was the inclusion of participants of low socio-economic status in all three ethnic groups. In keeping with worse motor symptoms, the subjective assessment of motor activities of daily living (MDS-UPDRS II) in patients from South Asian groups were also found to be more severe compared to White patients.
An objective motor assessment, the BRAIN test, only showed a worse dwell time (AT) when pressing keys on a computer keyboard in South Asian patients. Both our HCs and patients had worse KS compared to other publications15,16. This finding, alongside low computer literacy, could explain the less pronounced differences between the groups. More work is needed to understand if the BRAIN test can be used in diverse populations.
There is significant interest in whether the prevalence of dementia/cognitive impairment differs in patients from different ethnic groups17. The results from the current study suggest higher rates of cognitive impairment in the Black and South Asian groups compared to White patients. However, the MoCA18 has been shown to have language, literacy and cultural biases19,20. MoCA was shown to perform better when translated and culturally adapted21. We used the validated Bengali MoCA for best outcomes in the Bengali-speaking participants. Therefore, we are confident that our study did correctly identify worse cognitive scores in under-represented patients. However, the threshold for defining cognitive impairment required adjustments in translated versions, compared to White population groups20,21,22, with lower cut-offs being proposed for older age and/or lower education groups23. Our findings confirm that screening tests developed in White, English-speaking countries, may not be the most appropriate tools to investigate cognitive impairment in diverse populations.
Although there were no significant differences between non-motor scores in all three ethnicities, as reported by the NMSQ, we did find significantly worse depression (HADS-D), sleep quality (PDSS2) in South Asian patients, as well as diminished quality-of-life measures (EQ5D5L) in both South Asian and Black patients. We also found that patients from South Asian ethnic groups had a slightly higher MDS-UPDRS II score, reflective of a higher non-motor burden in this group.
Non-motor symptoms have been documented to differ in various regions around the globe, with more frequent symptoms present in certain populations. A systematic review from 2020 showed that gastrointestinal symptoms are more prevalent in the East Asian population, whilst depression is worse in East Asian patients17. This was in contrast to our data, where we only found that depression, sleep quality and quality-of-life were worse in South Asian patients. However, the systematic review included only two mono-ethnic Indian studies, whereas our study was a head-to-head comparison of the three ethnic groups. Interestingly, a cross-sectional analysis between continents showed a lower burden of non-motor symptoms in Asian patients, especially related to sleep and sexual activity24. Unfortunately, this study did not distinguish between South and East Asian groups and included participants with longer disease duration in the White PD group. Our study had a consistent methodology, and better balanced clinical characteristics of PD in all three ethnic groups. This disparity between studies could also be explained by cultural differences with fewer primary care consultations in under-represented groups, as explored in Simonet et al. in UK-based populations25,26. Fortunately, in East London, similar times to diagnosis and levels of treatment between ethnicities suggest an equality of access to primary care, and an unbiased standard of care in secondary settings. A cultural factor that could explain these differences could be related to biased self-reporting in under-represented populations27,28.
South Asian patients may have a younger age at diagnosis. Large international studies including >90% White European participants show that age at onset in the White patient group is 60 years (COURAGE-PD, 23andMe, IPDGC)29,30. Little is known about the age at onset in South Asian countries31, with one study reporting median age at onset as 54 years in Pakistan32. To date, there is relatively low confidence in the reported age of the participants from Bangladesh33. In 2020, only 67% of household members had birth certificates, with only 54% validated female birth certificates in Bangladesh34. However, the age at onset/diagnosis would need further investigation with dedicated prospective incidence studies. Reassuringly, symptom duration at diagnosis in all three major ethnic groups (White, South Asian and Black) was similar, suggesting that in East London, there is an equivalent awareness of PD symptoms in the community and in primary care. This was a positive finding, as other studies show delays in diagnosis and more advanced disease at the time of diagnosis for under-represented patients25,35,36. These studies have also shown a higher prevalence in PD in White populations compared to Asian or Black populations35,36.
One limitation of our study is that this is a case-control study, therefore it may be affected by sampling bias. A second inherent limitation was the recall bias of patients for their first symptoms and age at diagnosis. However, in most cases, we were able to corroborate with GP records of ‘tremor’, or ‘gait disturbance’, or other movement disorder symptoms. A third limitation in our study is the possibility of diagnostic error. However, as seen from previous studies,37,38 diagnostic errors in a specialist movement disorder service are lower than in non-specialist centres. In addition, our patient cohort was around the 5-year mark from diagnosis, therefore less likely to experience a diagnostic error.
Another limitation in our study was the use of different raters over time, which may have introduced inter-rater variability. We mitigated this by undertaking the same clinical training for MDS-UPDRS, MoCA and attending the same movement disorders clinics. Sampling bias and lack of confidence in reported age may be partly responsible for the younger age at assessment for the South Asian group. Despite this, age was not a relevant covariate in most of the statistical models. Future work in our cohort is needed. A final limitation, when analysing the MoCA data, was that we have not used a gold standard to define cognitive impairment in patients with PD dementia. Steps have been taken to amend this for future analyses.
The present study has included White, South Asian, and Black patient and control groups from East London, in an attempt to increase representation in research. We aimed to define the clinical phenotype of patients with PD from White, South Asian and Black ethnic groups. Our findings highlight that, despite an apparent younger age at assessment and similar PD duration and treatment burden, South Asian patients seem to have worse motor and cognitive phenotypes. A more severe motor and non-motor phenotype was also found in the Black patient group, although these patients were less well represented than South Asians in the present study. Further work is needed to understand if these differences arise as part of the natural course of the disease, or if socio-demographic factors lead to these differences.
Methods
Study design and participants
Research Ethics Board approval for the ELPD case-control study was received on 29th November 2018 from the South West - Central Bristol Research Ethics Committee, under the reference 39/SW/0255, IRAS ID 242395. A register of patients with PD and parkinsonism was created locally at the Barts Health NHS Trust. This was then used to recruit patients from the Movement Disorder outpatient clinic at the Royal London Hospital.
The inclusion criteria for the patient group were as follows: patients over the age of 18, with a clinical diagnosis of Parkinson’s, able to consent or have appropriate next-of-kin/proxy for consent. The clinical diagnosis of PD was made by movement disorder consultants according to MDS 2015 criteria37. The exclusion criteria for the patient group included: secondary parkinsonism (such as vascular or drug-induced parkinsonism), alternative neurological or psychiatric diagnoses (other movement disorders, including stroke and motor neurone disease, and unrelated dementia). Controls were recruited through several approaches: spouses of patients, people attending outpatient clinics for indications other than neurological symptoms, as well as public involvement events in East London. Inclusion criteria for controls were: age above 35 years, absence of parkinsonism, ability to consent. Exclusion criteria for controls were: neurological or psychiatric diagnoses, with the exception of idiopathic intracranial hypertension.
Enrolment strategies were focused on increasing participation from under-represented populations, such as participants from South Asian and Black ethnic backgrounds, and reducing barriers to research. To achieve this, we recruited a diverse, multi-lingual team with researchers that represented the same communities we sought to enrol in the study. We offered home visits, at varied times of the day, as an alternative to scheduled clinic-based visits. We translated relevant study materials (information sheets, consent forms and certain scales). Patient and public involvement events were organised to increase awareness of PD in the East London community, keep research participants up-to-date on study progress and aid recruitment of healthy controls.
Data collection
Data collection for the study started in January 2019. Study visits were undertaken at the Royal London Hospital, or in the participant’s home. Ethnicity was recorded as per ONS by ‘self-identification’39. We classified the self-reported data into geographical regions according to the Global Burden of Disease40.
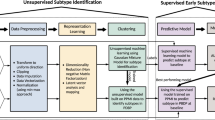
The study protocol consists of one mandatory clinical visit for both patients and controls (Fig. 3). Demographic data, clinical motor and non-motor assessments (e.g. hearing and vision performance captured by computerised psychophysical tests), and biological samples for biomarkers and genetic analysis of PD were collected (Fig. 3). The participant postcode was used to derive the IMD - Index of Multiple Deprivation41, with 1 representing most deprived, and 10 least deprived decile.
MDS-UPDRS MDS-Unified Parkinson’s Disease Rating Scale, MoCA Montreal Cognitive Assessment, RBDSQ REM sleep disease screening questionnaire, VH visual hallucinations, WOQ9 Wearing OFF questionnaire, EQ-5D-5L QoL Quality of Life Questionnaire, HADS Hospital Anxiety and Depression Questionnaire, NMSQ Non-Motor Symptoms Questionnaire, EPS Epworth Sleepiness Questionnaire, PDSS2 Parkinson’s Disease Sleep Scale 2, MERQ-PD-B Mini-environmental Risk factor Questionnaire in Parkinson’s Disease version B, SCOPA-AUT Scales for Outcomes in Parkinson’s Disease - Autonomic Dysfunction, PD Parkinson’s disease. Created with Canva54.
At the mandatory clinical visit, the following assessments & questionnaires were used: motor symptoms (MDS-UPDRS - Movement Disorders Society - Unified Parkinson’s Disease Rating Scale42, BRAIN test - BRadykinesia Akinesia INcoordination test43, DFT - Distal Finger Tapping test44), non-motor symptoms (NMSQ - Non-Motor Symptoms Questionnaire45, EPS - Epworth Sleepiness Questionnaire46, PDSS2 - Parkinson’s Sleep Scale 247, RBDSQ - REM-sleep behaviour disease screening questionnaire48, an abbreviated 6-item version of the UPSIT - University of Pennsylvania Smell Identification Test49), cognitive symptoms (MoCA - Montreal Cognitive Assessment18), quality-of-life (EQ-5D-5L Quality-of-Life Questionnaire50), psychiatric symptoms (HADS - Hospital Anxiety and Depression Questionnaire51), risk factors (MERQ-PD-B - Mini-environmental Risk factor Questionnaire in Parkinson’s Disease version B52). For the BRAIN test, the following were described: KS - kinesia score, number of taps in 30 s, AT - akinesia time, mean dwell-time on each key, IS - incoordination score, variance of travelling time between key taps15. The hemibody with the higher MDS-UPDRS III score for patients, and the lowest KS for controls, were used. A second and third optional visits for patients can be found in Supplementary Fig. 1.
Pseudo-anonymised data were stored securely on Queen Mary University of London servers for analysis and are available upon request.
Data analysis and statistical methods
Data were recorded in Microsoft Access database format and exported as ‘CSV’ files. We defined normal cognition (MoCA > 25), mild cognitive impairment (MoCA = 19–25), and dementia (MoCA < 19)18. This was either administered in English or a validated Bengali translation by our team’s Bengali-speaking team members.
Statistical analysis and figure generation were completed with Python 3.10.5 in Jupyter Notebook 6.4.8. Statistical analysis included T-test, Mann–Whitney U, Χ2 and Fisher’s exact tests, for continuous and categorical values. Logistic regression was adjusted for age, gender and disease duration. The MDS-UPDRS III, was also adjusted for levodopa-equivalent daily dose (LEDD)53. Bonferroni correction for multiple comparisons was used as follows: 3 ethnic groups (White, South Asian, and Black) & 4 main analyses (MDS-UPDRS III, IV, MoCA and NMSQ), significance cut-off p < 0.004.
Data availability
The raw data will be made available by request.
Code availability
The code for analysis will be publicly available on GitHub: https://github.com/Wolfson-PNU-QMUL/ELPD_Baseline.
References
Makarious, M. B. et al. Multi-modality machine learning predicting Parkinson’s disease. NPJ Parkinsons Dis. 8, 35 (2022).
Fereshtehnejad, S. M. & Postuma, R. B. Subtypes of Parkinson’s disease: what do they tell us about disease progression?. Curr. Neurol. Neurosci. Rep. 17, 34 (2017).
Vijiaratnam, N., Simuni, T., Bandmann, O., Morris, H. R. & Foltynie, T. Progress towards therapies for disease modification in Parkinson’s disease. Lancet Neurol. 20, 559–572 (2021).
Towns, C. et al. Defining the causes of sporadic Parkinson’s disease in the global Parkinson’s genetics program (GP2). NPJ Parkinsons Dis. 9, 131 (2023).
Lau, Y. H. et al. Does ethnicity influence recruitment into clinical trials of Parkinson’s disease?. J. Parkinsons Dis. 12, 975–981 (2022).
Global Parkinson’s Genetics Program GP2: the global Parkinson’s genetics program. Mov. Disord. 36, 842–851 (2021).
Parkinson Progression Marker Initiative The Parkinson progression marker initiative (PPMI). Prog. Neurobiol. 95, 629–635 (2011).
Elkurd, M., Wang, J. & Dewey, R. B. Jr Lateralization of motor signs affects symptom progression in Parkinson disease. Front Neurol. 12, 711045 (2021).
Velez-Pardo, C. et al. The distribution and risk effect of GBA variants in a large cohort of PD patients from Colombia and Peru. Parkinsonism Relat. Disord. 63, 204–208 (2019).
Bandres-Ciga, S. & Black and African American Connections to Parkinson’s Disease (BLAAC PD) Study Group Black and African American Connections to Parkinson’s disease study: addressing missing diversity in Parkinson’s disease genetics. Mov. Disord. 37, 1559–1561 (2022).
Tower Hamlets Borough Profile. https://www.towerhamlets.gov.uk/Documents/Borough_statistics/Tower-Hamlets-Borough-Profile-2024.pdf (2024). Accessed August 5, 2024.
Ray Chaudhuri, K. et al. Addressing the gap for racially diverse research involvement: The King’s Model for minority ethnic research participant recruitment. Public Health Pr. 6, 100426 (2023).
Skorvanek, M. et al. Differences in MDS-UPDRS scores based on Hoehn and Yahr stage and disease duration. Mov. Disord. Clin. Pr. 4, 536–544 (2017).
Chaudhuri, K. R., Hu, M. T. & Brooks, D. J. Atypical parkinsonism in Afro-Caribbean and Indian origin immigrants to the UK. Mov. Disord. 15, 18–23 (2000).
Hasan, H. et al. The BRadykinesia Akinesia INcoordination (BRAIN) tap test: capturing the sequence effect. Mov. Disord. Clin. Pr. 6, 462–469 (2019).
Simonet, C. et al. The emergence and progression of motor dysfunction in individuals at risk of Parkinson’s disease. Mov. Disord. 38, 1636–1644 (2023).
Ben-Joseph, A., Marshall, C. R., Lees, A. J. & Noyce, A. J. Ethnic variation in the manifestation of Parkinson’s disease: a narrative review. J. Parkinsons Dis. 10, 31–45 (2020).
Nasreddine, Z. S. et al. The Montreal Cognitive Assessment, MoCA: a brief screening tool for mild cognitive impairment. J. Am. Geriatr. Soc. 53, 695–699 (2005).
Milani, S. A., Marsiske, M. & Striley, C. W. Discriminative ability of Montreal cognitive assessment subtests and items in racial and ethnic minority groups. Alzheimer Dis. Assoc. Disord. 33, 226–232 (2019).
Lu, J. et al. Montreal cognitive assessment in detecting cognitive impairment in Chinese elderly individuals: a population-based study. J. Geriatr. Psychiatry Neurol. 24, 184–190 (2011).
Kaul, S. et al. MoCA in five Indian languages: a brief screening tool to diagnose dementia and MCI in a linguistically diverse setting. Int. J. Geriatr. Psychiatry 37, https://doi.org/10.1002/gps.5808 (2022).
Khaw, J. et al. Current update on the clinical utility of MMSE and MoCA for stroke patients in Asia: a systematic review. Int. J. Environ. Res. Public Health. 18, https://doi.org/10.3390/ijerph18178962 (2021).
Carson, N., Leach, L. & Murphy, K. J. A re-examination of Montreal Cognitive Assessment (MoCA) cutoff scores. Int J. Geriatr. Psychiatry 33, 379–388 (2018).
van Wamelen, D. J. et al. Cross-sectional analysis of the Parkinson’s disease Non-motor International Longitudinal Study baseline non-motor characteristics, geographical distribution and impact on quality of life. Sci. Rep. 11, 9611 (2021).
Simonet, C. et al. Assessment of risk factors and early presentations of Parkinson disease in primary care in a diverse UK population. JAMA Neurol. 79, 359–369 (2022).
Schrag, A., Horsfall, L., Walters, K., Noyce, A. & Petersen, I. Prediagnostic presentations of Parkinson’s disease in primary care: a case-control study. Lancet Neurol. 14, 57–64 (2015).
Sauerbier, A. et al. Non-motor symptoms assessed by non-motor symptoms questionnaire and non-motor symptoms scale in Parkinson’s disease in selected Asian populations. Neuroepidemiology 49, 1–17 (2017).
Sauerbier, A., Aris, A., Lim, E. W., Bhattacharya, K. & Ray Chaudhuri, K. Impact of ethnicity on the natural history of Parkinson disease. Med. J. Aust. 208, 410–414 (2018).
Grover, S. et al. Genome-wide association and meta-analysis of age at onset in Parkinson disease: evidence from the COURAGE-PD Consortium. Neurology 99, e698–e710 (2022).
Blauwendraat, C. et al. Parkinson disease age at onset GWAS: defining heritability, genetic loci and α-synuclein mechanisms. Mov. Disord. 34, 866–875 (2019).
Khalil, H. et al. Parkinson’s disease in the Middle East, North Africa, and South Asia: consensus from the International Parkinson and movement disorder society task force for the Middle East. J. Parkinsons Dis. 10, 729–741 (2020).
Khealani, B. A. & Baig, S. M. Clinical spectrum of Parkinson’s disease from Pakistan. Singap. Med. J. 47, 1075–1079 (2006).
Report of the Comprehensive Assessment & Strategic Action Plan on Civil Registration & Vital Statistics (CRVS) System in Bangladesh. https://getinthepicture.org/sites/default/files/resources/Comprehensive%20Assessment%20and%20Strategic%20Action%20Plan%20Report%20Bangladesh_0.pdf (2013). Accessed October 7, 2024.
Faguet, J. P. & Pal, S. Decentralised governance: crafting effective democracies around the world (LSE Press; 2023).
Dahodwala, N., Karlawish, J., Siderowf, A., Duda, J. E. & Mandell, D. S. Delayed Parkinson’s disease diagnosis among African-Americans: the role of reporting of disability. Neuroepidemiology 36, 150–154 (2011).
Wright Willis, A., Evanoff, B. A., Lian, M., Criswell, S. R. & Racette, B. A. Geographic and ethnic variation in Parkinson disease: a population-based study of US Medicare beneficiaries. Neuroepidemiology 34, 143–151 (2010).
Postuma, R. B. et al. MDS clinical diagnostic criteria for Parkinson’s disease. Mov. Disord. 30, 1591–1601 (2015).
Rizzo, G. et al. Accuracy of clinical diagnosis of Parkinson disease: a systematic review and meta-analysis. Neurology 86, 566–576 (2016).
Ethnic group, national identity and religion. Accessed April 29, 2025. https://www.ons.gov.uk/methodology/classificationsandstandards/measuringequality/ethnicgroupnationalidentityandreligion (2025).
GBD 2015 Geographies. https://www.healthdata.org/sites/default/files/files/Projects/GBD/GBDRegions_countries.pdf (2015).
Ministry of Housing, Communities, Local Government (2018 to 2021). English indices of deprivation 2015. http://www.gov.uk/government/statistics/english-indices-of-deprivation-2015 (2015). Accessed September 4, 2024.
Goetz, C. G. et al. Movement Disorder Society-sponsored revision of the Unified Parkinson’s Disease Rating Scale (MDS-UPDRS): scale presentation and clinimetric testing results. Mov. Disord. 23, 2129–2170 (2008).
Noyce, A. J. et al. Bradykinesia-akinesia incoordination test: validating an online keyboard test of upper limb function. PLoS One 9, e96260 (2014).
Akram, N. et al. Developing and assessing a new web-based tapping test for measuring distal movement in Parkinson’s disease: a Distal Finger Tapping test. Sci. Rep. 12, 386 (2022).
Chaudhuri, K. R. et al. International multicenter pilot study of the first comprehensive self-completed nonmotor symptoms questionnaire for Parkinson’s disease: the NMSQuest study. Mov. Disord. 21, 916–923 (2006).
Johns, M. W. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep 14, 540–545 (1991).
Trenkwalder, C. et al. Parkinson’s disease sleep scale-validation of the revised version PDSS-2. Mov. Disord. 26, 644–652 (2011).
Stiasny-Kolster, K. et al. The REM sleep behavior disorder screening questionnaire-a new diagnostic instrument. Mov. Disord. 22, 2386–2393 (2007).
Bestwick, J. P. et al. Maximising information on smell, quantitative motor impairment and probable REM-sleep behaviour disorder in the prediction of Parkinson’s disease. bioRxiv, https://doi.org/10.1101/2020.03.03.20023994 (2020).
EuroQol Research Foundation. EQ-5D-5L user guide. Available from: https://euroqol.org/publications/user-guides (2019).
Bjelland, I., Dahl, A. A., Haug, T. T. & Neckelmann, D. The validity of the Hospital Anxiety and Depression Scale. Update. Lit. Rev. J. Psychosom. Res. 52, 69–77 (2002).
Report Viewer. http://www.commondataelements.ninds.nih.gov/report-viewer/23351/PD%20DOC%20Mini%20Environmental%20Risk%20Questionnaire%20for%20Parkinson’s%20Disease%20Patients%20Baseline%20(PD%20DOC%20MERQ-PD-B (2024). Accessed July 12, 2024.
Jost, S. T. et al. Levodopa Dose Equivalency in Parkinson’s Disease: Updated Systematic Review and Proposals. Mov. Disord. 38, 1236–1252 (2023).
Canva. https://www.canva.com/ (2024).
Acknowledgements
This study received funding from: Virginia Keiley benefaction, Barts Charity, Michael J Fox Foundation, Parkinson’s UK, Medical College of Saint Bartholomew’s Hospital Trust, and Cure Parkinson’s.
Author information
Authors and Affiliations
Contributions
A.J.N. designed the study. K.D., A.Z., E.C., T.H., A.B.J., J.K. recruited and assessed participants clinically. A.Z. performed the analysis. A.Z. and K.D. wrote the paper. A.J.N., C.R.M., A.J.L. and S.W. reviewed the article. The rest of the authors, E.C., B.H., H.C., N.D., D.A.G., C.B., T.B., C.S., provided critical revisions of the paper.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zirra, A., Dey, K.C., Camboe, E. et al. The East London Parkinson’s disease project – a case-control study of Parkinson’s Disease in a diverse population. npj Parkinsons Dis. 11, 172 (2025). https://doi.org/10.1038/s41531-025-01031-x
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41531-025-01031-x
This article is cited by
-
Idiopathic hyposmia as a marker of prodromal Parkinson’s disease — a cohort study
Scientific Reports (2025)