Abstract
Numerous brain imaging studies have reported white matter alterations in schizophrenia, but the lipidome analysis of the corresponding tissue remains incomplete. In this study, we investigated the lipidome composition of six subcortical white matter regions corresponding to major axonal tracks in both control subjects and schizophrenia patients. All six regions exhibited a consistent pattern of quantitative lipidome alterations in schizophrenia, involving myelin-forming and mitochondria associated lipid classes. While alteration levels of myelin-forming lipids, particularly sphingolipids, aligned with the extent of the myelin changes reported in structural brain imaging studies, a significant decrease of mitochondria in the white matter, indicated by the lipidome alterations, was not previously investigated. To verify this effect, we performed lipidome analysis in a larger set of individuals and in the mitochondria-enriched membrane fraction, as well as directly quantified mitochondrial content. Our results suggest a substantial reduction of the mitochondrial quotient accompanied by the imbalance in myelin lipids in schizophrenia white matter.
Similar content being viewed by others
Introduction
Schizophrenia (SZ) is a multifaceted mental disorder marked by a variety of symptoms and cognitive impairments1,2. With a global prevalence of approximately four per 1000, schizophrenia is relatively widespread and ranks among the top 15 diseases causing the most years of life lost due to disability3,4,5. Schizophrenia significantly impacts an individual’s social life and reduces their life expectancy by 15–25 years due to increased premature mortality rates and a higher risk of suicide compared to the general population6,7,8.
Despite its substantial social and economic implications and more than 130 years of research, the mechanisms underlying schizophrenia remain elusive, while numerous hypothetical ones have been proposed9. These include the classic dopamine hypothesis10,11, based on decrease of schizophrenia symptoms following the pharmacological inhibition of dopamine receptors; the N-methyl-D-aspartate (NMDA) hypothesis12,13, which is based on observed hypofunction of NMDA receptors; the serotonin hypothesis14, which proposes hyperactivation of serotonin receptors; the mitochondrial dysfunction hypothesis15,16, which highlights morphological abnormalities in neocortical mitochondria17 and decreased expression of mitochondrial genes in the brain in schizophrenia18,19; the neuroinflammation hypothesis20,21 incorporating cytokine-associated inflammatory events together with an oxidative stress; and the glial maldevelopment hypothesis22,23 based on, among others, patient-derived organoid studies.
The inherent challenge in consolidating these findings into a comprehensive understanding of the molecular alterations associated with schizophrenia lies in the functional and structural complexity of the human brain. Various brain structures, cell types, and cell interaction circuits may exhibit unique molecular manifestations related to schizophrenia24. However, the majority of molecular studies on schizophrenia have focused predominantly on specific brain regions, such as the prefrontal cortex25,26, and particular cell populations, such as neocortical neurons. At the same time, numerous studies underscore the systemic nature of schizophrenia including alterations in white matter subcortical regions. Some of the relevant findings include decrease of myelin-associated signal and a reduction in fractional anisotropy, indicative of myelin disorganization, detected using structural magnetic resonance imaging (sMRI) in subcortical white matter tracks27,28,29. While this decrease is rather widespread, the degree of effect varies between brain regions, with the most significant schizophrenia-associated changes reported in the corpus callosum and corona radiata30. Other white matter regions showing anisotropy abnormalities in schizophrenia patients include cingulum bundle31,32 interconnecting gray matter structures of the limbic system and was thought to be the core structure in the “circle of emotions”33; uncinate fasciculus connecting temporal and frontal lobes34,35; and internal capsule connecting the cortex, brainstem, basal ganglia, and thalamus36,37.
The structural MRI signal primarily reflects the quantity and integrity of myelin membranes that form axonal sheaths, which are composed of over 70% lipids by dry weight38. Lipids not only form a significant component of the myelin sheath39,40 but also play roles in brain signaling41 and energy metabolism42. However, lipidome studies of the schizophrenic brain are limited, particularly those focusing on white matter regions. Lipid abnormalities identified in these studies include changes in sphingomyelin metabolism43,44, elevated levels of ceramides43,45 and free fatty acids45, and decreased levels of phospholipids45,46,47. As for fatty acid radicals, some studies have found decreased levels of polyunsaturated fatty acids, primarily arachidonic acid, in the schizophrenia brain tissue47,48, although these results were disputed by other studies49.
In summary, these findings suggest the potential for substantial metabolic and structural changes in the subcortical white matter of brains affected by schizophrenia. To further explore this notion, we conducted an analysis of lipidome profiles in six white matter regions in neurotypical individuals and schizophrenia patients. Some of these regions have not been previously studied, while others have not been examined as systematically. Our results corroborate the myelin alterations in these tracts as reported by sMRI, and additionally reveal changes associated with the representation and function of mitochondria in the white matter of schizophrenia patients.
Materials and methods
Brain samples and tissue dissection
Post-mortem human brain samples were obtained from the National BioService (St. Petersburg, Russia). Study included 44 subjects (22 schizophrenia cases (SZ) and 22 healthy controls (HC); Table 1). Informed consent for the use of human brain tissues for research was obtained from all subjects or their next of kin by the tissue provider organization. The protocol was approved by the Skoltech Institutional Review Board №15.1. Human subjects were defined as healthy with respect to the sampled brain tissue by medical pathologists. Diagnosis of SZ was based on ICD-10 criteria and provided by the Moscow Healthcare Department. All human subjects suffered sudden death with no prolonged agony state from causes not related to brain function.
All post-mortem brain slices were stored at −80 °C. The Atlas of the Human Brain50 was used to locate the areas of interest in the human brains. Frozen brain slices were brought to −20 °C before dissection. For lipidomic analysis, tissue pieces weighing approximately 15–25 mg were cut out from selected brain areas using a metal scalpel. After collection, the dissected samples were transferred to cooled 1.5 ml round bottom reinforced Precellys tubes (Bertin Technologies) and stored at −80 °C prior to lipid extraction.
Lipid extraction, mass-spectrometry analysis and lipidomic data processing
For the lipid extraction, MTBE:MeOH:H2O solvent system was used. UPLC-MS analysis was performed on the an QExactive mass spectrometer (Thermo Fisher Scientific, USA) interfaced with the Waters Acquity UPLC chromatographic system (Waters, Manchester, UK). Identification and relative quantification of lipids were performed separately for positive and negative ionization modes using MS-DIAL software51 (version 4.90). Detailed parameters of the lipidomic analysis and data processing are described in supplementary materials.
Mitochondria isolation and analysis
Mitochondria were isolated from cingulum bundle samples according to a modified protocol52,53. Briefly, 100–140 mg of brain tissue was dissected and divided into two equal parts. After stratified randomization, the first part of the samples was mixed with 1.25 mL of ice-cold homogenization buffer (210 mM mannitol, 70 mM sucrose, 5 mM Tris-HCl, and 1 mM EDTA, pH 7.5) and manually homogenized in a Potter-Elvehjem homogenizer with 30–40 strokes. The homogenizer was then washed with 0.25 mL of cold buffer, and the suspensions were pooled and centrifuged (10 min, 1300 × g, 4 °C). The supernatant was removed, and the pellet was washed with 500 mL of cold homogenization buffer and centrifuged again (10 min, 1300 × g, 4 °C). The supernatants were combined and subjected to centrifugation (2 × 10 min, 1300 × g, 4 °C). Finally, the supernatants were centrifuged (20 min, 12,700 × g, 4 °C) to obtain a crude mitochondrial fraction, which was washed twice with 0.01 M PBS (pH 7.4). Lipid extraction was immediately performed following the protocol described in previous section.
The second part of brain samples, with the same wet weight, was extracted in parallel with the mitochondrial fraction. Prior to mass spectrometry analysis, the dried lipid extracts were resuspended in ice-cold ACN:IPA (7:3, v:v) (400 µl for brain samples and 100 µl for mitochondria samples). 25 µl of the supernatant was transferred to a 350 µl autosampler vial and diluted 1:2 with ACN:IPA (7:3, v:v) for positive measurements, and no dilution was done for negative measurements. The parameters of the mass spectrometry analysis were as described above.
Mitochondria staining and imaging
Isolated mitochondria were stained using IraZolve-Mito (GlpBio, GC43908) dye54. The suspension of crude mitochondria or unbroken cells was washed three times with 0.01 M PBS (pH 7.4), fixed with 10% formaldehyde at room temperature for 5 min, washed three times with PBS, and then incubated with IraZolve-Mito (50 µM in 0.01 M PBS) at 35 °C for 30 min. After that, the pellets were washed three times with PBS. To measure fluorescence intensity, mitochondria or unbroken cells were suspended in PBS, and 200 µL of the suspension was added in triplicate to a 96-well plate and measured using a spectrofluorometer (Infinite® 200 PRO, TECAN, Switzerland) at excitation wavelength (λex) of 403 nm and emission wavelength (λex) of 590 nm. Fluorescence intensities were calculated as the mean of three measurements and normalized by the wet weight. To balance fluorescence intensity between mitochondrial and unbroken cell fractions, fluorescence intensities were additionally normalized by measuring absorbance at λ = 600 nm.
To track mitochondria shape and size, confocal scanning microscopy was performed. The stained mitochondria were resuspended in PBS and 20 µl drops were applied to Thermo Scientific SuperFrost microscope slides. The slides were briefly dried at +37 °C on the Leica HI1220 hotplate and coverslipped with Fluoromount aqueous mounting medium (Sigma-Aldrich-F4680). Mitochondria were imaged using an inverted confocal laser scanning microscope, Zeiss LSM 880 with AiryScan, equipped with a 32-channel GaAsP-PMT area detector and a 40×/1.3 Oil DIC M27 (WD = 0.2 mm), (UV)VIS-IR objective with Scan zoom 3. A z-stack of 5–8 µm depth was scanned for one field of view in two randomly chosen locations for each drop, with a pixel size of 0.07 µm × 0.07 µm × 0.30 µm and an image size of 70.85 µm × 70.85 µm in AiryScan SR mode, with a pixel time of 2.05 µs. To detect IraZolve-Mito (GlpBio, GC43908) fluorescence, 405 nm excitation wavelength and 595 nm emission wavelength were used. AiryScan processing, z-stack maximal intensity projection, and histogram Min/Max correction were performed using Zeiss ZEN 2.3 software. Zeiss LSM 880 with Airyscan is the equipment of the Core Centrum of the Institute of Developmental Biology RAS, Moscow, Russia.
Correlation with MRI data
Structural MRI data were obtained from the open-source dataset COBRE (The Center for Biomedical Research Excellence) and consisted of 82 patients with schizophrenia (SZ, mean age 38.5 ± 13.3) and 86 healthy controls (HC, mean age 38.6 ± 11.9). The data were acquired with the following parameters: TR/TE/TI = 2530/[1.64, 3.5, 5.36, 7.22, 9.08]/900 ms, flip angle = 7°, FOV = 256 × 256 mm, slab thickness = 176 mm, matrix = 256 × 256 × 176, voxel size = 1 × 1 × 1 mm, number of echoes = 5, pixel bandwidth = 650 Hz, total scan time = 6 min. The SZ group consisted of Schizophrenia Strict (71 subjects) and Schizoaffective (11 subjects), and for the analysis, only data related to Schizophrenia Strict subjects were utilized.
For each T1w and T2w MRI scan, alignment to the anatomical and normalization to standard Montreal Neurological Institute (MNI) space were performed using a symmetric image normalization method with affine and rigid transformations (Nipype library 1.8.3). Subsequently, bias field correction (N4 nonparameteric nonuniform normalization) was applied to remove intensity gradients caused by bias field inhomogeneity within the image. To segment white matter volumes, the FreeSurfer library (6.0.0)55 was employed with default settings.
To compare changes in white matter (WM) between healthy controls and schizophrenia patients, T1w and T2w signal intensities were extracted from six previously selected regions for lipid analysis. As the subjects for lipid analysis and MR signal intensity analysis were not the same, it is possible that the coordinates for lipid analysis may not precisely correspond to those for MR signal analysis. To mitigate this potential inaccuracy, a 7 × 7 × 7 mm cube was taken around each coordinate, the intersection of this cube with a three-dimensional white matter mask was determined, and the intensity value over this intersection was averaged to obtain the spatially-smoothed WM intensity value for specific coordinates.
The described algorithm was implemented using the Python programming language (version 3.8.3) and can be found in the provided git repository56. To compare with lipidomic data, the obtained T1/T2 intensities were log2-transformed, and the differences between means in the SZ and HC subsets were calculated. SZ-related Diffusion Tensor Imaging (DTI) changes were obtained from published data30 and used without any additional transformation.
Data analysis
Statistical analyses and data visualization were performed in R (version 4.2.2). Principal component analysis (PCA) was applied for the visualization of the total lipid intensity variation. Significant lipid features were assessed using analysis of variance (ANOVA, exploratory stage, intensity ~ region*diagnosis model) or Student’s t tests (verification stage and mitochondria fraction analysis). In the exploratory stage, ANOVA was additionally accompanied with the permutation test. The normality of the distribution of the lipid intensities was indicated with the Shapiro-Wilk test. The hypergeometric test was applied to identify significant lipid classes or fatty acid residues among the lipid species selected by ANOVA or t-test. To evaluate the significance of the correlation between lipidomic data or between lipidomic and sMRI data, Pearson’s coefficient R was calculated; correlations with R > 0.25 or R < −0.25 and p < 0.05 were considered to be significantly positive and negative, respectively). Correction for multiple testing (Benjamini–Hohberg procedure) was applied in all cases where multiple comparisons were made, and all analyses presented in the paper are conducted using lipids significant after the multiple testing comparison, except specifically indicated cases were all detected lipids were used. Data analysis and visualization utilized “MixOmics”, “ggplot2”, “ggplot”, “ggpubr”, “gridExtra”, “dplyr”, “purrr”, “reshape2”, “ggrepel”, “igraph”, “stringr”, “tidyr”, “matrixStats” and other standard R packages.
Results
Experimental design
We examined alterations in the lipid composition associated with schizophrenia within six white matter regions of the human brain (Fig. 1A). Specifically, we chose brain regions from the left hemisphere’s frontal and temporal lobes, corresponding to the following anatomical structures: the corpus callosum body (ccb), which forms interhemispheric tracts; the cingulum bundle (cgb), which connects frontal, parietal, and medial temporal sites; the superior portion of the corona radiata (cor); the middle longitudinal fasciculus (mlf), a subcortical tract linking the superior temporal gyrus (STG) to the angular gyrus (AG); the uncinated fasciculus (unf), which connects limbic regions in the temporal lobe to the frontal lobe; and the external capsule (ext). Most of these regions have been reported as significantly altered in schizophrenia patients in MRI studies.
A A schematic representation of the anatomical locations of the six white matter regions analyzed in our study. B The scheme for experimental pipeline. C The numbers of lipid compounds detected in our study, with annotation confirmed by fragment spectra in DDA analysis, sorted according to lipid class annotation. Colors indicate lipid structural categories.
The investigation was conducted in two stages (Fig. 1B). During the first, exploratory stage, we examined lipidomic changes associated with SZ across six selected regions of white matter using a smaller sample size (exploratory stage; n = 12; 6 HC and 6 SZ). Next, we selected two brain regions exhibiting the largest and smallest amplitude of lipidome changes in SZ and repeated the analysis within a larger cohort to test the validity of our results (verification stage; n = 44; 22 HC and 22 SZ). The verification cohort included subjects from the exploratory cohort (n = 12; 6 HC and 6 SZ), as well as additional ones (n = 32; 16 HC and 16 SZ). Samples of the 12 overlapping subjects were dissected anew at the verification stage and the entire experiment was repeated along with the additional 32 samples. In both stages, cohorts were matched by age, sex, post-mortem interval (PMI), and tissue preservation, approximated using RNA integrity assessment (p > 0.05; Table 1). The dissected brain areas were identified using the Allen Brain Atlas50, followed by lipid fraction isolation and analysis conducted using mass spectrometry coupled with ultra-performance liquid chromatography (UPLC-MS/MS) in both positive and negative ionization modes. For both the exploratory and verification stages, the mass spectrometry measurements yielded 537 lipid features annotated by fragment spectra and belonging to 24 biochemically defined lipid classes57 (Fig. 1C, Supplementary Table S2).
Identification of schizophrenia-associated white matter lipidome alterations
At the exploratory stage of the project, statistical analysis of the lipidome data measured in six white matter regions identified 154 lipids with the significant abundance differences between schizophrenia and control groups remaining after the multiple testing correction (ANOVA, Benjamini-Hochberg (BH)-corrected p < 0.05 with a model intensity ~ diagnosis*region; permutation p = 0.0004). Further, the same analysis identified 17 lipids with significant differences among white matter regions, but none for the diagnosis*region interaction term (ANOVA, BH-corrected p < 0.05; permutation p = 0.042 for regions and p = 0.59 for diagnosis*region). Biochemical characterization of the lipids displaying significantly different abundance levels in the SZ white matter (ANOVA, BH-corrected p < 0.05, with a model intensity ~ diagnosis) revealed elevated levels of PCO and decreased levels of PG, LPE, BMP, and CAR in SZ (hypergeometric test, BH-corrected p < 0.0001 for PG and LPE; <0.05 for PCO, BMP and CAR; Fig. 2A).
A The average schizophrenia-associated alterations in the lipid classes in each of the six white matter regions represented as log2-transformed lipid abundance differences between schizophrenia and control samples (log2 fold changes). Shaded areas indicate lipid classes with the overall abundance significantly altered in schizophrenia (hypergeometric test, BH-corrected p < 0.05). B Correlations of lipid abundance level alterations (log2 fold changes) in schizophrenia among white matter regions, calculated based on significantly altered lipids (n = 154, ANOVA, BH-corrected p < 0.05). Colors and numbers indicate Pearson correlation coefficients. The dendrogram and the brain section scheme on the right show the clustering of white matter regions using correlation-based distances. C Distributions of schizophrenia effect amplitudes (Cohen’s d values) of significantly altered lipids (n = 154, ANOVA, BH-corrected p < 0.05) within the six white matter regions. Lipids that represent an overall significant abundance increase (mean Cohen’s d > 0) or decrease (mean Cohen’s d < 0) are colored in red and blue, respectively. The histogram below shows the average effect size of the significant schizophrenia-associated alteration for each white matter region.
Aligning with the ANOVA outcome, general analysis of SZ effects on the white matter lipidome revealed similar alteration patterns for all six regions, but with variation related to the region anatomy and the amplitude of schizophrenia-associated effects (Fig. 2B, C). Specifically, we observed a significant positive correlation of the schizophrenia-associated lipid alterations (log2-transformed fold changes) of the 154 lipids significant in the ANOVA test between all six white matter regions (Pearson correlation, mean R = 0.82, maximal p < 0.05; Fig. 2B). While ANOVA model used in our study biases results towards differences shared among all white matter regions, we observed a very similar correlation distribution using all 537 lipids detected in our study in the correlation analysis (Pearson correlation, mean R = 0.62, maximal p < 0.05; Supplementary Fig. S2). In both analyses, the one based on significant and another – on all detected lipids, however, we observed an evident separation of dorsomedial and ventrolateral axonal tracks into distinct clusters, suggesting a partial anatomical specificity of schizophrenia-associated effects. Further, the cingulum bundle and middle longitudinal fasciculus displayed the largest amplitude of the lipid alteration profiles, calculated as Cohen’s effect size values, both for lipids significantly increased and significantly decreased in schizophrenia. Conversely, the external capsule and the uncinate fasciculus changed the least (Fig. 2C).
To test the validity of observed schizophrenia-associated lipidome alterations, we conducted additional measurements in 22 SZ and 22 HC individuals in two white matter regions, cingulum bundle and uncinate fasciculus, regions with the largest and the smallest amplitude of the lipidome alterations. Of the 88 samples, four samples, each from a different HC subject, with two samples representing cgb region and two representing unf region, showed abnormal total lipid signal intensity (Supplementary Fig. S3) and were removed from further analyses. Visualization of the lipid variations among the remaining 84 samples indicated a trend towards separating schizophrenia patients from the control group (Fig. 3A).
A Visualization of lipidome-based distances between white matter samples using PCA. Colors distinguish schizophrenia (SZ) and control (HC) samples. Shapes distinguish unf and cgb regions. Correlation between schizophrenia-associated lipid alterations in cgb (B) region and unf (C) region between exploratory (n = 12) and verification (n = 44) stages. Solid points represent mean differences for lipid classes. Colors indicate lipid structural categories. D A volcano plot visualizing the results of the statistical analysis of schizophrenia-associated alterations in cgb region. Significant changes (t-test, BH-corrected p < 0.05) are color-coded according to lipid categories. E Distributions of schizophrenia-associated alterations, represented as log2-transformed lipid abundance differences between schizophrenia and control samples (log2 fold change), in each assessed fatty acid residue. Colors highlight residues with a significantly decreased (blue) overall abundance in schizophrenia (hypergeometric test, BH-corrected p < 0.05). Only residues which were assessed in more than 5 different lipid features are shown. F Distributions of schizophrenia-associated alterations, represented as log2-transformed lipid abundance differences between schizophrenia and control samples (log2 fold change), in each assessed lipid class. Colors highlight residues with an overall abundance significantly decreased (blue) or increased (red) in schizophrenia (hypergeometric test, BH-corrected p < 0.05).
Analysis of schizophrenia-associated lipid level alterations in the verification dataset reproduced the schizophrenia-associated effects detected at the exploratory stage. Specifically, lipid level differences between SZ and HC groups in the exploratory dataset analysis correlated positively and significantly with the differences detected in the verification dataset (Pearson correlation, R = 0.851, p < 0.0001 for cgb region and R = 0.639, p < 0.0001 for unf region; Fig. 3B, C). Furthermore, we observed a similar strength of correlation for comparisons involving either 32 new or 12 remeasured individuals, suggesting a high robustness of the detected SZ-associated alterations (Supplementary Fig. S4). In addition, verification stage analysis confirmed the difference in SZ-effect amplitudes between the white matter regions. In both datasets, cingulum bundle region displayed much more pronounced SZ-associated differences compared to uncinate fasciculus (Supplementary Fig. S4). As a consequence, due to smaller difference amplitude, uncinate fasciculus showed reproducibly lower correlations between the two exploratory and verification datasets, and yielded zero significantly different lipids in a statistical analysis restricted to this region (two-sided t-test, BH-corrected p < 0.05). By contrast, in the same analysis, cingulum bundle region yielded 67 significantly different lipids (two-sided t-test, BH-corrected p < 0.05, Fig. 3D).
In addition to the general agreement between two sample cohorts, analysis of significant schizophrenia-associated differences found in cingulum bundle revealed the same significant lipid classes as at the exploratory stage. Specifically, we detected elevated levels of PCO and decreased levels of PG, LPE, BMP, and CAR in SZ (hypergeometric test, BH-corrected p < 0.0001 for PG; <0.001 for PCO; <0.05 for BMP, LPE and CAR; Fig. 3F). At the fatty acid residue level, palmitoleic (16:1) and linoleic acid (18:2) acids were significantly decreased in the cingulum bundle of schizophrenia patients (hypergeometric test, BH-corrected p < 0.0001 for FA 18:2; <0.05 for FA 16:1; Fig. 3E)
The relationship between schizophrenia-associated white matter lipidome alterations and alterations reported by brain imaging studies
The observed variation in the magnitude of schizophrenia-associated differences among the six white matter regions provides an avenue to link these differences with alterations of white matter organization and volume reported in schizophrenia patients by structural magnetic resonance imaging (sMRI) studies. For this comparison, we utilized two previously published datasets: a diffusion tensor imaging (DTI) study30 based on functional anisotropy of 1963 schizophrenia patients and 2359 control individuals, and a T1/T2 signal-based study involving 82 schizophrenia patients and 86 controls. By grouping lipid classes into five widely recognized categories - glycerophospholipids, glycerolipids, sphingolipids, fatty acyls, and sterols - we discovered a significant positive correlation between the extent of lipid alteration in schizophrenia and the sMRI signal, specifically within the sphingolipid category for both DTI and T1/T2 sMRI datasets (Pearson correlation, R = 0.6 and p < 0.001 (DTI), R = 0.42 and p < 0.001 (T1/T2); Fig. 4A, B, Supplementary Table S3).
Distribution of the Pearson correlation coefficients for the comparisons between schizophrenia-associated lipid alterations represented by Cohen’s d values and sMRI schizophrenia-associated signal changes detected using DTI (A) or T1/T2 (B) protocols. Distributions include all detected lipids. Colors indicate lipid categories. Vertical dashed lines mark the average correlation value of a distribution. The sterol category, represented by fewer than five lipid compounds detected in our study, is not shown. C Relationship between correlations of lipid class alterations and structural brain alterations measured using either T1/T2 or DTI protocols. Symbols mark average Pearson correlation values calculated within each lipid class. Colors indicate lipid categories.
This finding is consistent with the known overrepresentation of sphingolipids, mainly glycosphingolipids, in myelin forming the axonal sheath compared to other brain cell membranes40,58,59. More broadly, this result highlights the concurrence between the extent of schizophrenia-associated changes in the abundance of myelin-forming lipids identified in our study and myelin alterations demonstrated by large-scale sMRI studies. Lipid class level analysis also revealed a positive correlation with both DTI and T1/T2 signal variations for hexosylceramides, sphingomyelin, cholesterol, and triacylglycerols (Fig. 4C). Within sphingolipids, we further established a relationship between fatty acid residue lengths and correlation strength of the corresponding lipid abundance variation and sMRI signal, irrespective of the extent of unsaturation. Specifically, we demonstrate that the positive correlation between alterations in sphingolipid levels and sMRI signal was limited, with sphingomyelin being the only exception, to compounds with a total fatty acid chain length of 38–46 carbons (Supplementary Fig. S5).
The relationship between schizophrenia-associated white matter lipidome alterations and mitochondrial disfunction
Of the four lipid classes that demonstrated significantly decreased abundance levels in the white matter of individuals with schizophrenia, three, namely PG, BMP, and CAR, have been identified as associated with mitochondrial membranes. Therefore, the observed decrease in these lipid classes suggests a potential breakdown of mitochondria in the white matter tissue of individuals with schizophrenia. This observation aligns with reported abnormalities in mitochondrial shape found in the neocortex, caudate, and hippocampus18,60,61. No studies to date, however, have investigated mitochondrial alterations in the white matter tracts of the schizophrenia brain.
To determine whether the detected decrease in PG, BMP, and CAR levels reflects a decrease in mitochondrial representation or functionality in schizophrenic white matter, we conducted a lipidome analysis following the isolation of mitochondria from the cingulum bundle samples of six schizophrenia patients and six control individuals (Fig. 5A). Simultaneously, we examined the lipidome composition of whole tissue samples extracted from the same brain areas using an identical UPLC-MS protocol. The lipidome measurements of whole tissue samples and mitochondrial isolates resulted in the detection and annotation of 535 lipids representing 22 lipid classes (Supplementary Table S4, Supplementary Fig. S6). Of these, 209 demonstrated significant abundance differences between whole tissue samples and mitochondrial isolates (paired t-test, p < 0.05; permutation p = 0.0024). As anticipated, the mitochondrial fraction was significantly enriched in lipid classes previously associated with mitochondrial membranes62,63,64,65, such as PE, PG, DG, LPC and CARs (hypergeometric test, log2 fold change >0.2, BH-corrected p < 0.0001 for PE, PG and LPE; p < 0.01 for DG; p < 0.05 for LPC and CAR; Fig. 5B). The sole exception was the enrichment of the LPE class in our isolates, which has not been previously linked to mitochondria.
A Schematic of the experimental design. B Differences in lipidome composition between mitochondrial isolates and untreated cingulum bundle tissue samples, represented as log2-transformed lipid abundance differences (log2 fold change), in each assessed lipid class. Colors highlight lipid classes with significantly increased (red) or decreased (blue) abundance in mitochondrial isolates (hypergeometric test, BH-corrected p < 0.05). Areas shaded in red indicate lipid classes reported as characteristic to mitochondria. C Volcano plot visualizing results of statistical analysis of schizophrenia-associated alterations in the cingulum bundle mitochondrial isolates. Significant changes (t-test, BH-corrected p < 0.05) are colored according to the lipid categories. The background volcano plot (transparent red) visualizes results of the parallel statistical analysis conducted on the whole tissue cingulum bundle samples. D Correlation between schizophrenia-associated lipidome alterations detected in mitochondrial isolates and untreated cingulum bundle tissue samples. Colors indicate lipid categories as in panel D. E Schizophrenia-associated differences in cingulum bundle mitochondrial isolates, represented as log2 fold change, in each assessed lipid class. Colors highlight lipid classes with significantly decreased (blue) abundance in mitochondrial isolates derived from schizophrenia specimens (hypergeometric test, BH-corrected p < 0.05). F Fluorescent intensity of mitochondria stained with IraZolve-Mito dye in cingulum bundle mitochondrial fraction and remaining fraction from schizophrenia (SZ) and control (HC) samples.
We identified 158 lipids as significantly decreased in schizophrenia-derived mitochondria isolates (t-test, BH-corrected p < 0.05; Fig. 5C). Additionally, the overall lipid quantity decreased sharply for almost all lipids and lipid classes in schizophrenia-derived mitochondrial isolates compared to mitochondrial isolates obtained from control samples. By contrast, there was no disproportionate decline in overall lipid quantity in untreated cingulum bundle schizophrenia samples dissected from the same anatomical region and extracted and measured concurrently with the mitochondrial isolates (Fig. 5C). Further, despite overall shift in lipid quantity, schizophrenia-associated effects correlated well between the mitochondrial isolates and untreated cingulum bundle tissue samples (Pearson correlation, R = 0.65, p < 0.0001; Fig. 5D).
Given that there was no difference in tissue material weight between specimens dissected from schizophrenia and control brains (t-test, p > 0.05), these results suggest a substantial mitochondrial deficit in the white matter of individuals with schizophrenia. This could potentially explain the decrease in mitochondria-associated lipid classes across six white matter regions. Supporting this hypothesis, the mitochondrial fraction derived from schizophrenia samples was particularly depleted in the same mitochondria-associated lipid classes, PGs, CARs, and BMP, which also showed decreased abundance levels in the cingulum bundle whole-tissue samples (hypergeometric test, BH-corrected p < 0.0001 for PG and p < 0.05 for CAR and BMP; Fig. 5E).
To further substantiate the notion of mitochondrial depletion in the schizophrenia white matter, we directly stained mitochondria in the cingulum bundle mitochondria isolates and remaining tissue homogenates derived from six schizophrenia patients and six control individuals using the IraZolve-Mito dye. We first confirmed the selectiveness of staining by examining mitochondria isolates using confocal microscopy (Supplementary Fig. S7). We then used fluorescence spectroscopy to quantify the mitochondria-associated fluorescent signal in mitochondria isolates and tissue homogenates. Consistent with our predictions, the measurements showed a significant decrease in mitochondria-associated fluorescence in schizophrenia samples compared to controls for both tissue homogenates and, especially, mitochondria isolates (paired t-test (one-sided), p < 0.05 for mitochondria and p < 0.1 for tissue; Fig. 5F).
Discussion
Our study presents a systematic analysis of the lipidome alterations associated with schizophrenia in six anatomically and functionally diverse subcortical white matter regions. Among white matter regions of the human brain, existing lipidomic studies of schizophrenia-associated effects cover only the corpus callosum, with results suggesting substantial lipidome alterations in this region44,47,49. Our findings corroborate this, while going beyond the lipidome coverage of previous studies, demonstrating both shared and diverse effects of schizophrenia on the brain’s white matter.
Although our study broadens the analysis of schizophrenia-associated effects to multiple white matter regions and additional lipid classes, it has a number of limitations. Most prominently, the sample size of the study does not allow us to identify region-specific alterations, as well as to achieve a statistically significant level for differences shared among regions for individual white matter tracks displaying small different amplitude. Further, all participating patients were not drug-naïve, introducing a systematic confounder separating SZ and HC groups. Previous studies have indeed identified particular lipid classes, such as FA and PC, affected by antipsychotic medication intake66. Absence of overlap between these lipid classes and the ones altered in schizophrenia in our study indicates that medication was not the main driving force behind the detected alterations. Similarly, our study did not take into account individuals’ diets, although there were no evident dietary differences between SZ and HC groups.
Despite these limitations, our study demonstrates a robust signal of schizophrenia-associated lipidome alterations that are well correlated among all six white matter regions. This observation aligns well with the current understanding of systemic alterations in structural and functional brain connectivity in schizophrenia67. While our study does not identify statistically significant schizophrenia-associated lipid level alterations in specific white matter regions, it certainly does not exclude their presence. Our results, however, indicate that the prevalence of such region-specific alterations is substantially lower compared to the shared ones. Nonetheless, even shared lipidome alterations display features highlighting variation in schizophrenia-associated effects among the regions. Firstly, patterns of schizophrenia-associated lipidome aligned more closely among white matter regions located within the same brain lobe than between the frontal and temporal lobes. Secondly, the extent of schizophrenia-associated alterations varied by more than two-fold among the assessed white matter regions. Specifically, we observed that out of the six regions, the cingulum bundle and middle longitudinal fasciculus exhibited the most significant alterations, whereas the alteration pattern was least pronounced in the external capsule and uncinated fasciculus. These regions are anatomically scattered, with the cgb located near the medial cingulate cortex, the mlf adjacent to the superior temporal gyrus, and the ext positioned in between. This observation further underscores the widespread nature of schizophrenia-associated alterations and indicates a need for a more concentrated focus on white matter regions in molecular studies of this disorder.
Lipidome alterations we detected in the white matter regions of schizophrenia patients involve particular lipid classes, pointing towards two components of the brain tissue: axonal myelin sheath and mitochondria. With respect to myelin, our analysis shows a significant increase in PCO levels across white matter regions in SZ, a result not reported by previous studies. PCO lipids are one of the major constituents of myelin and influence its structural properties59,68. Cholesterol, another major component of the myelin38,59, was also significantly increased in cingulum bundle, a region showing most pronounced schizophrenia-associated changes. Moreover, the intensity levels of other structural myelin lipid classes, such as PEO, HexCer, SHexCer59, were also increased in this region, albeit not significantly. Combined, these results point towards dysregulated myelination in schizophrenia, an observation aligning with MRI-based schizophrenia brain studies69,70. To test this notion, we took advantage of the variation in schizophrenia-associated lipidome alterations among brain regions to align the lipidome data with results from brain imaging studies. Specifically, we examined data generated using two different sMRI techniques: T1/T2 signal and DTI. The T1/T2 signal reflects the ratio of water-poor and water-rich brain structures, with lipid-rich myelin tracks representing the former. The DTI method evaluates axonal track integrity by examining water molecule diffusion differences along and across the myelinated fibers. We found that schizophrenia-associated changes in levels of sphingolipids and cholesterol, known myelin constituents71, correlated positively with alterations detected in the same six brain regions using both types of sMRI data. We further found that among sphingolipids, compounds containing fatty acid residues within a particular intermediate length range contributed most to the positive correlation with both T1/T2 and DTI data. In addition to sphingolipids, schizophrenia-associated changes in triacylglycerol levels also positively correlated with anatomical changes detected by both T1/T2 and DTI signals. Triacylglycerols have not been shown to contribute substantially to myelin, but rather accumulate in fat droplets found in astrocytes72, this implicating them in schizophrenia-associated axonal track alterations detected by sMRI studies. Furthermore, we found that changes in the abundance of several major glycerophospholipid classes commonly associated with plasma membranes, such as PE, LPE, and PC, positively correlated with T1/T2 but not with DTI signal variation. This suggests that, in addition to myelin, T1/T2 signals also reflect variation in general lipid membrane density and that this membrane density is altered in schizophrenia.
Among the lipid classes showing marked decrease in schizophrenia, the majority have been previously linked to mitochondrial membrane metabolism, lending support to the mitochondrial dysfunction hypothesis. Specifically, PGs serve a crucial role in mitochondrial metabolism as precursors of cardiolipins (CL), a class of lipids specific to mitochondria that are believed to shield mitochondria from oxidative stress62,73. Further, decreased PG levels in schizophrenia were previously reported both in white and gray matter45,47. In conjunction with PGs, BMPs also participate in cardiolipin metabolism74,75. CARs represent another class of lipids linked with mitochondria, playing an important role in the transportation of fatty acids for beta-oxidation63,76,77. These lipid classes are involved in astrocyte metabolism78, which may indicate dysregulation of this cell type in schizophrenia. CoenzymeQ10, which supports oxidative phosphorylation process in mitochondria79, was also decreased. This notion was further supported by changes in the levels of fatty residues, as we detected significant deficit of linoleic acid (LA, 18:2) and palmitoleic acid (PA, 16:1). While PA is probably involved into anti-neuroinflammatory metabolism80, its complete functions in brain are unclear. LA is hypothesized to present neuroprotective properties by preventing the activation of microglia81,82,83. LA is also a major component of CL and their precursor PG84, which are, as was stated previously, involved into mitochondria metabolism and protection from the oxidative stress. It worth mentioning that we did not detect significant changes in the level of other PUFAs, such as docosapentaenoic acid (DPA, 22:5) or docosahexaenoic (DHA, 22:6) acids. This result is in contrast with reports on fatty acid proportions in schizophrenia in several brain regions, including amygdala85, orbitofrontal cortex86, prefrontal cortex87,88 and prefrontal white matter89, where decreased levels of some of the PUFAs, mainly, DPA, were detected.
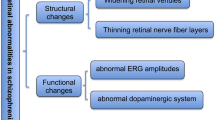
Deficiency of the mentioned fatty acid residues and lipid classes may point out to the increased inflammatory and oxidative status in white matter in schizophrenia, potentially due to increased oxidative stress produced by dysfunctional mitochondria. This is supported by existing proteomic studies, where mitochondria-specific proteins were shown to be downregulated in the schizophrenia brain, in both gray and white matter90,91,92. To further investigate this hypothesis, we isolated and analyzed mitochondrial fraction lipids alongside whole tissue samples. This experiment, coupled with direct quantitation of mitochondrial abundance using specific fluorescent staining, revealed an evident decrease of mitochondria-associated signal in schizophrenia samples compared to controls. This result strongly suggests a reduction in either the number or size of mitochondria in schizophrenia white matter. Such mitochondrial abnormalities have been reported in neocortical gray matter in schizophrenia61,93. Our results indicate that mitochondrial reduction is characteristic of all six investigated white matter regions and could underpin the major lipidome changes we identified in whole tissue samples. One can further speculate that mitochondrial dysfunction may lead to an energy deficit in oligodendrocytes, which could in turn result in abnormalities in the ordered myelin structure created by these cells, as detected by sMRI (Fig. 6). This result is in line with previously reported alterations of oligodendrocytes in prefrontal white matter, accompanied by decrease in mitochondrial number and volume94. While this relationship is hypothetical and requires further confirmation, our study suggests that lipids, as vital components of the brain, may significantly contribute to the mechanisms underlying schizophrenia.
Data availability
Experimental data generated in this study is provided in the Supplementary information.
Code availability
All custom code which was used for the data analysis and visualization is provided in the Supplementary information.
Abbreviations
- SZ:
-
Schizophrenia;
- HC:
-
healthy controls;
- ROS:
-
reactive oxygen species;
- MRI:
-
magnetic resonance imaging;
- DTI:
-
diffusion tensor imaging;
- MTBE:
-
methyl-tert-butyl ether;
- ACN:
-
acetonitrile;
- IPA:
-
isopropyl alcohol;
- QC:
-
quality control;
- UPLC:
-
ultra-performance liquid chromatography;
- PUFA:
-
polyunsaturated fatty acids.
- PC,:
-
Phosphatidylcholines
- LPC,:
-
Monoacylglycerophosphocholines
- LPE,:
-
Monoacylglycerophosphoethanolamines
- LPEO,:
-
Monoalkylglycerophosphoethanolamines
- PC,:
-
Glycerophosphocholines
- PE,:
-
Glycerophosphoethanolamines
- PCO,:
-
Plasmanyl-phosphatidylcholines
- PEO,:
-
Plasmanyl-phosphatidylethanolamines
- PEP,:
-
Plasmalogens
- PG,:
-
Monoacylglycerophosphoglycerols
- BMP,:
-
Bis(monoacylglycero)phosphates
- PI,:
-
Glycerophosphoinositols
- PS,:
-
Glycerophosphoserines
- TG,:
-
Triacylglycerols
- DG,:
-
Diacylglycerols
- MGDG,:
-
Monogalactosyldiacylglycerol
- Cer,:
-
Ceramides
- HexCer,:
-
Hexosylceramides
- SHexCer,:
-
Sulfatides
- AHexCer,:
-
Acyl-hexosylceramides
- SM,:
-
Sphingomyelins
- FA,:
-
Free fatty acids
- CAR,:
-
Acylcarnitines
- NAE,:
-
Anandamides
- ST,:
-
Sterols/Sterol sulfates
References
Habtewold, T. D. et al. A systematic review and narrative synthesis of data-driven studies in schizophrenia symptoms and cognitive deficits. Transl. Psychiatry 10, 244 (2020).
Andreasen, N. C., Arndt, S., Alliger, R., Miller, D. & Flaum, M. Symptoms of Schizophrenia. Methods, Meanings, and Mechanisms. JAMA Psychiatry 52, 341–351 (1995).
Fuller Torrey, E. Prevalence studies in schizophrenia. Br. J. Psychiatry 150, 598–608 (1987).
Saha, S., Chant, D., Welham, J. & McGrath, J. A systematic review of the prevalence of schizophrenia. PLoS Med 2, 0413–0433 (2005).
Vos, T. et al. Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990-2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet 390, 1211–1259 (2017).
Dickerson, F. et al. Mortality in Schizophrenia: Clinical and serological predictors. Schizophr. Bull. 40, 796–803 (2014).
Laursen, T. M. Causes of premature mortality in schizophrenia: A review of literature published in 2018. Curr. Opin. Psychiatry 32, 388–393 (2019).
Bai, W. et al. Worldwide prevalence of suicidal ideation and suicide plan among people with schizophrenia: a meta-analysis and systematic review of epidemiological surveys. Transl. Psychiatry 11, 552 (2021).
Fišar, Z. Biological hypotheses, risk factors, and biomarkers of schizophrenia. Prog. Neuro Psychopharmacol. Biol. Psychiatry 120, 110626 (2023).
Howes, O. D. & Kapur, S. The dopamine hypothesis of schizophrenia: Version III - The final common pathway. Schizophr. Bull. 35, 549–562 (2009).
Davatzikos, C. & Koutsouleris, N. Computational Neuroanatomy of Schizophrenia. Neurobiol. Schizophr 1, 263–282 (2016).
Uno, Y. & Coyle, J. T. Glutamate hypothesis in schizophrenia. Psychiatry Clin. Neurosci. 73, 204–215 (2019).
Stahl, S. M. Beyond the dopamine hypothesis of schizophrenia to three neural networks of psychosis: Dopamine, serotonin, and glutamate. CNS Spectr. 23, 187–191 (2018).
Eggers, A. E. A serotonin hypothesis of schizophrenia. Med. Hypotheses 80, 791–794 (2013).
Clay, H. B., Sillivan, S. & Konradi, C. Mitochondrial dysfunction and pathology in bipolar disorder and schizophrenia. Int. J. Dev. Neurosci. 29, 311–324 (2011).
Rajasekaran, A., Venkatasubramanian, G., Berk, M. & Debnath, M. Mitochondrial dysfunction in schizophrenia: Pathways, mechanisms and implications. Neurosci. Biobehav. Rev. 48, 10–21 (2015).
Ben-Shachar, D. Mitochondrial dysfunction in schizophrenia: A possible linkage to dopamine. J. Neurochem. 83, 1241–1251 (2002).
Ni, P. & Chung, S. Mitochondrial Dysfunction in Schizophrenia. BioEssays 42, 1–12 (2020).
Ben-Shachar, D. Mitochondrial multifaceted dysfunction in schizophrenia; complex I as a possible pathological target. Schizophr. Res. 187, 3–10 (2017).
Meyer, U. Developmental neuroinflammation and schizophrenia. Prog. Neuro-Psychopharmacology. Biol. Psychiatry 42, 20–34 (2013).
Trovão, N. et al. Peripheral biomarkers for first-episode psychosis-opportunities from the neuroinflammatory hypothesis of schizophrenia. Psychiatry Investig. 16, 177–184 (2019).
Fatemi, S. H. & Folsom, T. D. The neurodevelopmental hypothesis of Schizophrenia, revisited. Schizophr. Bull. 35, 528–548 (2009).
Kalus, P., Senitz, D. & Beckmann, H. Disturbances of corticogenesis in schizophrenia: Morphological findings provide new evidence for the maldevelopmental hypothesis. Neuropsychobiology 40, 1–13 (1999).
Lang, U. E., Puls, I., Müller, D. J., Strutz-Seebohm, N. & Gallinat, J. Molecular mechanisms of schizophrenia. Cell. Physiol. Biochem. 20, 687–702 (2007).
Smucny, J., Dienel, S. J., Lewis, D. A. & Carter, C. S. Mechanisms underlying dorsolateral prefrontal cortex contributions to cognitive dysfunction in schizophrenia. Neuropsychopharmacology 47, 292–308 (2022).
Mirnics, K., Middleton, F. A., Marquez, A., Lewis, D. A. & Levitt, P. Molecular characterization of schizophrenia viewed by microarray analysis of gene expression in prefrontal cortex. Neuron 28, 53–67 (2000).
Carreira Figueiredo, I., Borgan, F., Pasternak, O., Turkheimer, F. E. & Howes, O. D. White-matter free-water diffusion MRI in schizophrenia: a systematic review and meta-analysis. Neuropsychopharmacology 47, 1413–1420 (2022).
Kubicki, M. et al. DTI and MTR abnormalities in schizophrenia: Analysis of white matter integrity. Neuroimage 26, 1109–1118 (2005).
Hoptman, M. J. et al. A DTI study of white matter microstructure in individuals at high genetic risk for schizophrenia. Schizophr. Res. 106, 115–124 (2008).
Kelly, S. et al. Widespread white matter microstructural differences in schizophrenia across 4322 individuals: Results from the ENIGMA Schizophrenia DTI Working Group. Mol. Psychiatry 23, 1261–1269 (2018).
Bubb, E. J., Metzler-Baddeley, C. & Aggleton, J. P. The cingulum bundle: Anatomy, function, and dysfunction. Neurosci. Biobehav. Rev. 92, 104–127 (2018).
Fitzsimmons, J. et al. Cingulum bundle abnormalities and risk for schizophrenia. Schizophr. Res. 215, 385–391 (2020).
Papez, J. W. A proposed mechanism of emotion. Arch NeurPsych 38, 725–743 (1937).
Kawashima, T. et al. Uncinate fasciculus abnormalities in recent onset schizophrenia and affective psychosis: A diffusion tensor imaging study. Schizophr. Res. 110, 119–126 (2009).
Burns, J. et al. Structural disconnectivity in schizophrenia: A diffusion tensor magnetic resonance imaging study. Br. J. Psychiatry 182, 439–443 (2003).
Zhou, S. Y. et al. Decreased volume and increased asymmetry of the anterior limb of the internal capsule in patients with schizophrenia. Biol. Psychiatry 54, 427–436 (2003).
Horga, G. et al. Correlations between Ventricular enlargement and gray and white matter volumes of cortex, thalamus, striatum, and internal capsule in schizophrenia. Eur. Arch. Psychiatry Clin. Neurosci. 261, 467–476 (2011).
O’Brien, J. S. & Sampson, E. L. Lipid composition of the normal human brain: gray matter, white matter, and myelin. J. Lipid Res. 6, 537–544 (1965).
Kister, A. & Kister, I. Overview of myelin, major myelin lipids, and myelin-associated proteins. Front. Chem. 10, 1–9 (2022).
Schmitt, S., Cantuti Castelvetri, L. & Simons, M. Metabolism and functions of lipids in myelin. Biochim. Biophys. Acta Mol. Cell Biol. Lipids 1851, 999–1005 (2015).
Bazan, N. G. Lipid signaling in neural plasticity, brain repair, and neuroprotection. Mol. Neurobiol. 32, 89–103 (2005).
Zhuo, C., Hou, W., Tian, H., Wang, L. & Li, R. Lipidomics of the brain, retina, and biofluids: from the biological landscape to potential clinical application in schizophrenia. Transl. Psychiatry 10, 1–9 (2020).
Zhuo, C. et al. Acid sphingomyelinase/ceramide system in schizophrenia: implications for therapeutic intervention as a potential novel target. Transl. Psychiatry 12, 260 (2022).
Esaki, K. et al. Evidence for altered metabolism of sphingosine-1-phosphate in the corpus callosum of patients with schizophrenia. Schizophr. Bull. 46, 1172–1181 (2020).
Emanuel, S. et al. High throughput lipidomic profiling of schizophrenia and bipolar disorder brain tissue reveals alterations of free fatty acids, phosphatidylcholines, and ceramides. J. Proteome Res. 7, 4266–4277 (2008).
Schmitt, A. et al. Altered thalamic membrane phospholipids in schizophrenia: A postmortem study. Biol. Psychiatry 56, 41–45 (2004).
Shimamoto-Mitsuyama, C. et al. Lipid Pathology of the Corpus Callosum in Schizophrenia and the Potential Role of Abnormal Gene Regulatory Networks with Reduced Microglial Marker Expression. Cereb. Cortex 31, 448–462 (2021).
Yao, J. K., Leonard, S. & Reddy, R. D. Membrane phospholipid abnormalities in postmortem brains from schizophrenic patients. Schizophr. Res. 42, 7–17 (2000).
Hamazaki, K. et al. Fatty acid composition of the postmortem corpus callosum of patients with schizophrenia, bipolar disorder, or major depressive disorder. Eur. Psychiatry 39, 51–56 (2017).
Ding, S. L. et al. Comprehensive cellular-resolution atlas of the adult human brain. J. Comp. Neurol. 524, 3127–3481 (2016).
Tsugawa, H. et al. A lipidome atlas in MS-DIAL 4. Nat. Biotechnol. 38, 1159–1163 (2020).
Clayton, D. A. & Shadel, G. S. Isolation of mitochondria from animal tissue. Cold Spring Harb. Protoc 2014, 1112–1114 (2014).
Wieckowski, M. R. M. R., Giorgi, C., Lebiedzinska, M., Duszynski, J. & Pinton, P. Isolation of mitochondria-associated membranes and mitochondria from animal tissues and cells. Nat. Protoc. 4, 1582–1590 (2009).
Sorvina, A. et al. Mitochondrial imaging in live or fixed tissues using a luminescent iridium complex. Sci. Rep. 8, 1–9 (2018).
FreeSurfer library (6.0.0) (2011). https://github.com/freesurfer/freesurfer.
T1w/T2w processing (2023). https://github.com/maryjis/intensities_T1.
Fahy, E. et al. Update of the LIPID MAPS comprehensive classification system for lipids. J. Lipid Res. 50, S9–S14 (2009).
Poitelon, Y., Kopec, A. M. & Belin, S. Myelin Fat Facts: An Overview of Lipids and Fatty Acid Metabolism. Cells 9, 812 (2020).
Barnes-Vélez, J. A., Aksoy Yasar, F. B. & Hu, J. Myelin lipid metabolism and its role in myelination and myelin maintenance. Innovation 4, 100360 (2023).
Roberts, R. C. Mitochondrial dysfunction in schizophrenia: With a focus on postmortem studies. Mitochondrion 56, 91–101 (2021).
Uranova, N. A., Vikhreva, O. V., Rakhmanova, V. I. & Orlovskaya, D. D. Dystrophy of Oligodendrocytes and Adjacent Microglia in Prefrontal Gray Matter in Schizophrenia. Front. Psychiatry 11, 1–15 (2020).
Horvath, S. E. & Daum, G. Lipids of mitochondria. Prog. Lipid Res. 52, 590–614 (2013).
Zammit, V. A., Ramsay, R. R., Bonomini, M. & Arduini, A. Carnitine, mitochondrial function and therapy. Adv. Drug Deliv. Rev. 61, 1353–1362 (2009).
Osman, C., Voelker, D. R. & Langer, T. Making heads or tails of phospholipids in mitochondria. J. Cell Biol. 192, 7–16 (2011).
Chicco, A. J. & Sparagna, G. C. Role of cardiolipin alterations in mitochondrial dysfunction and disease. Am. J. Physiol. Cell Physiol. 292, C33–44 (2007).
Burghardt, K. J., Kajy, M. & Ward, K. M. Metabolomics, Lipidomics, and Antipsychotics: A Systematic Review. Biomedicines 11(12), 3295 (2023).
Van Den Heuvel, M. P. & Fornito, A. Brain networks in schizophrenia. Neuropsychol. Rev. 24, 32–48 (2014).
Dean, J. M. & Lodhi, I. J. Structural and functional roles of ether lipids. Protein Cell 9, 196–206 (2018).
Flynn, S. W. et al. Abnormalities of myelination in schizophrenia detected in vivo with MRI, and post-mortem with analysis of oligodendrocyte proteins. Mol. Psychiatry 8, 811–820 (2003).
Yumerhodzha, S., Duru, D. G., Duru, A. D. & Bebek, N. White matter changes in thalamic stroke. In 18th National Biomedical Engineering Meeting 60, 1–4 (IEEE, 2015).
Koenig, S. H. Cholesterol of myelin is the determinant of gray‐white contrast in MRI of brain. Magn. Reson. Med. 20, 285–291 (1991).
Lee, J. A., Hall, B., Allsop, J., Alqarni, R. & Allen, S. P. Lipid metabolism in astrocytic structure and function. Semin. Cell Dev. Biol. 112, 123–136 (2021).
Houtkooper, R. H. & Vaz, F. M. Cardiolipin, the heart of mitochondrial metabolism. Cell. Mol. Life Sci. 65, 2493–2506 (2008).
Mayr, J. A. Lipid metabolism in mitochondrial membranes. J. Inherit. Metab. Dis. 38, 137–144 (2015).
Scherer, M. & Schmitz, G. Metabolism, function and mass spectrometric analysis of bis(monoacylglycero)phosphate and cardiolipin. Chem. Phys. Lipids 164, 556–562 (2011).
Pande, S. V. A mitochondrial carnitine acylcarnitine translocase system. Proc. Natl. Acad. Sci. USA 72, 883–887 (1975).
Virmani, M. A. & Cirulli, M. The Role of L-Carnitine in Mitochondria, Prevention of Metabolic Inflexibility and Disease Initiation. Int. J. Mol. Sci. 23, 2717 (2022).
Szrok-Jurga, S. et al. The Role of Acyl-CoA β-Oxidation in Brain Metabolism and Neurodegenerative Diseases. Int. J. Mol. Sci. 24, 13977 (2023).
Hidalgo-Gutiérrez, A. et al. Metabolic targets of coenzyme q10 in mitochondria. Antioxidants 10, 1–15 (2021).
Yu, Q. et al. Palmitoleic acid protects microglia from palmitate-induced neurotoxicity in vitro. PLoS One 19, 1–15 (2024).
Vesga‐jiménez, D. J. et al. Fatty Acids: An Insight into the Pathogenesis of Neurodegenerative Diseases and Therapeutic Potential. Int. J. Mol. Sci. 23, 2577 (2022).
Murru, E. et al. Conjugated Linoleic Acid and Brain Metabolism: A Possible Anti-Neuroinflammatory Role Mediated by PPARα Activation. Front. Pharmacol. 11, 1–12 (2021).
Taha, A. Y. Linoleic acid–good or bad for the brain? npj Sci. Food 4, 1 (2020).
Nakagawa, Y. Metabolism and biological function of cardiolipin. Yakugaku Zasshi 133, 561–574 (2013).
Hamazaki, K., Hamazaki, T. & Inadera, H. Fatty acid composition in the postmortem amygdala of patients with schizophrenia, bipolar disorder, and major depressive disorder. J. Psychiatr. Res. 46, 1024–1028 (2012).
McNamara, R. K. et al. Abnormalities in the fatty acid composition of the postmortem orbitofrontal cortex of schizophrenic patients: Gender differences and partial normalization with antipsychotic medications. Schizophr. Res. 91, 37–50 (2007).
Hamazaki, K. et al. Fatty acid composition of the postmortem prefrontal cortex of patients with schizophrenia, bipolar disorder, and major depressive disorder. Psychiatry Res. 227, 353–359 (2015).
Taha, A. Y., Cheon, Y., Ma, K., Rapoport, S. I. & Rao, J. S. Altered fatty acid concentrations in prefrontal cortex of schizophrenic patients. J. Psychiatr. Res. 47, 636–643 (2013).
Ghosh, S., Dyer, R. A. & Beasley, C. L. Evidence for altered cell membrane lipid composition in postmortem prefrontal white matter in bipolar disorder and schizophrenia. J. Psychiatr. Res. 95, 135–142 (2017).
Saia-Cereda, V. M. et al. Proteomics of the corpus callosum unravel pivotal players in the dysfunction of cell signaling, structure, and myelination in schizophrenia brains. Eur. Arch. Psychiatry Clin. Neurosci. 265, 601–612 (2015).
Martins-De-Souza, D. et al. Prefrontal cortex shotgun proteome analysis reveals altered calcium homeostasis and immune system imbalance in schizophrenia. Eur. Arch. Psychiatry Clin. Neurosci. 259, 151–163 (2009).
Prabakaran, S. et al. Mitochondrial dysfunction in schizophrenia: Evidence for compromised brain metabolism and oxidative stress. Mol. Psychiatry 9, 684–697 (2004).
Uranova, N. A., Vikhreva, O. V. & Rakhmanova, V. I. Abnormal microglial reactivity in gray matter of the prefrontal cortex in schizophrenia. Asian J. Psychiatr. 63, 102752 (2021).
Uranova, N. A., Vikhreva, O. V., Rakhmanova, V. I. & Orlovskaya, D. D. Ultrastructural pathology of oligodendrocytes adjacent to microglia in prefrontal white matter in schizophrenia. npj Schizophr. 4, 26 (2018).
Acknowledgements
The research was supported by the Russian Science Foundation grant № 22-15-00474. The work of Maria Osetrova was partially supported by Russian Science Foundation grant № 20-15-00299. We thank the Advanced Mass Spectrometry Core facility and Advanced Imaging Core facility of Skoltech, as well as Core Centrum of the Institute of Developmental Biology RAS for providing the experimental equipment for conducting this study.
Author information
Authors and Affiliations
Contributions
Conceptualization: P.K., O.E.; Sample preparation: O.E., D.S., N.A.; Lipidomic analysis: D.S., E.S.; Mitochondria staining: D.S., O.E.; Data analysis: D.S., M.B., M.S.; Visualization: D.S., M.O.; Resources: A.M., Y.Z., M.K., G.K., P.K.; Supervision: P.K., E.S., O.E., M.O.; Funding: P.K.; Writing – original draft: D.S., P.K., M.S.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Senko, D., Efimova, O., Osetrova, M. et al. White matter lipidome alterations in the schizophrenia brain. Schizophr 10, 123 (2024). https://doi.org/10.1038/s41537-024-00542-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41537-024-00542-5